Abstract
Gun violence killed over 46,000 Americans in 2021; almost 120,000 suffered gunshot wounds. This epidemic has attracted national attention and increasing concern from medical and surgical organizations, as evident in this special issue. ‘Through and Through History’ explores the surgical management of gunshot wounds from their earliest appearance in 14th-century Europe to the present. Interweaving the civilian and military experience, it details not only the evolution of care directly applied to patients but also the social, political, and scientific milieu that shaped decisions made and actions performed both in and out of the operating room. The article describes how surgeons have pushed the boundaries of medicine and science in each era, developing new therapies for their patients, a historical trend that persists today when such care has the potential to save tens of thousands of lives each year.
Keywords: amputation, GSW, gunshot wound, history, trauma
Patients have suffered from gunshot wounds since at least the 14th century—and medical providers have been trying to treat them for just as long. This article explores the history of the medical management of gunshot wounds from their earliest appearance in Europe to the present, concentrating on the interchanges between military and civilian practice as well as the social, cultural, and scientific milieu that fostered innovation over time.
INTRODUCTION
In 2021, gun violence killed over 46,000 Americans, a tragedy from any perspective.1 While data on shootings are notably less accurate, an estimated 117,166 Americans were shot.2 The staggering discrepancy between these figures—representing 71,116 possible lives saved—chiefly depends on the care our medical system provides. While imperfect, unequal, and constantly evolving, 21st-century medical and surgical management of gunshot wounds (GSWs) makes an irrefutable and significant difference to both the individual and to our society: studies have shown that improved medical treatment is one of the reasons deaths from gun violence decreased in the late 20th century.3 Moreover, it remains one of the few interventions Americans of all political stripes support. These modern therapies have a long history dating to the introduction of firearms in Europe in the late Middle Ages. Over the last 700 years, physicians and surgeons have investigated the pathophysiology of their injuries and developed various remedies to heal GSWs.
The classic account of this subject remains Historical Studies on the Nature and Treatment of Gunshot Wounds from the Fifteenth Century to the Present Time, authored in 1859 by Theodor Billroth, an intimidating name to follow in the surgical literature.4 The few paragraphs below cannot compare to Billroth’s 100-page manuscript and regretfully elide many of the wonderfully illustrative primary quotations he incorporated into his text. As Billroth criticized himself for emphasizing Germanic authors, our article focuses on the West and, in the later years, spotlights the American experience. It includes more social-cultural context to explain the technical discussion. Rather than attempting a comprehensive review, it highlights key episodes over the last 700 years that demonstrate pivotal changes in theory and practice. With many advances arising from war, the article focuses on the close interplay between civilian and military medicine over the centuries that remains critical to trauma care today.
THE INTRODUCTION OF FIREARMS IN THE LATE MIDDLE AGES
The 14th-century ushered in the European experience with medical twindemics—the Black Death and GSWs. While physicians famously struggled with the former, the latter profoundly inspired surgeons to engage with this novel trauma.5 The inspiration for that interplay fell on fecund ground, as the foundation for modern surgery arose in the middle ages. In particular, medieval educational, organizational, and practical-theoretical innovations ranged from disciplinary syntheses, prescient chemical preparations, and instrumental creations.6–8 With the introduction of gunpowder-based firearms in the early-to-mid-14th century, European surgeons were primed for originative action.
Developed from the 10th to the 13th centuries in China (gunpowder first appeared, ironically, as fire medicine (火藥)) and, soon thereafter, spreading widely in Asia and the Arabic world, firearms proved highly adaptable and progressively effective in a variety of military engagements.9 The first documented European examples date from the 1320s (Walter de Milemete’s illustration of a cannon in 1326 (Fig. 1)10,11; Barthélemy de Drach’s reference to powder for cannons in his account books for the king of France), with gunpowder-propellant used in the Battle of Crécy (1346) and the Siege of Calais (1346–1347) during the Hundred Years’ War.12 Initial interest in gunpowder focused on military use. Archeological remains in Denmark suggest the first case of suicide by GSW in the 14th century, while inquest confirms another in the Tower of London in the 16th century.13–15 As the armaments spread, so too did technological support.16 Like that for medical experience, oral directions were followed by 1-page leaflets and thence to manuals for using artillery. Apothecaries, physicians, and other practitioners at times both prepared the chemical components for the propellants and then treated the resulting injuries.17–20
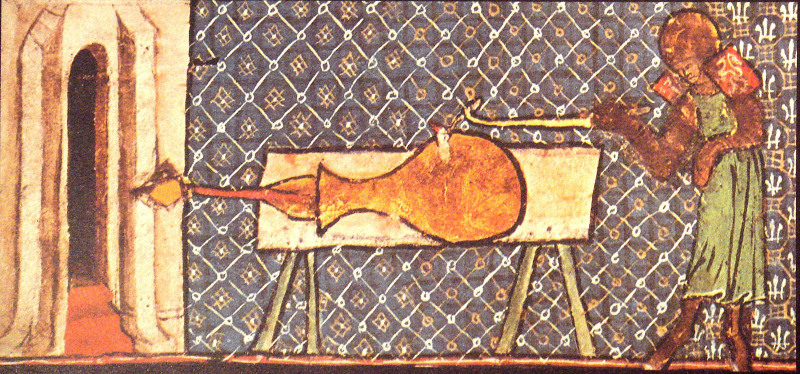
FIGURE 1.
First known western illustration of a firearm, in Walter de Milemete’s 1326 treatise De nobilitatibus, sapientiis et prudentiis regum, depicting a primitive cannon firing at a castle in the 1331 siege of Cividale. Image in the public domain at https://en.wikipedia.org/wiki/Walter_de_Milemete#/media/File:EarlyCannonDeNobilitatibusSapientiiEtPrudentiisRegumManuscriptWalterdeMilemete1326.jpg (accessed December 14, 2022).
As the decades unfurled, handheld firearms were developed and deployed, increasing the frequency and complexity of GSWs through the 15th into the 17th centuries.4,21–26 Novel to the wounds was the combination of the shot’s kinetic energy, the burns and powder from the explosive force, the introduction of foreign bodies (the shot and other particulates from the energy delivery) into the wound, and the crushing results on bones/soft tissue; no prior weapon had presented such an amalgam. Although some scholars have found confusion and irrationality in contemporary surgical responses, a closer reading shows reasonable extensions of prior wound treatments.21,27
Famously, Heinrich Von Pfalzpaint (c. 1415–1465) from Bavaria (Wundarznei, 1497) and Hans von Gersdoff (c. 1455–1529) from Strasbourg (Feldtbuch der Wundartznen newlich getrucht und gebessert, 1517) wrote extensively of GSWs, amputations, and the surgeon’s heroic efforts to mitigate their effects.24,28,29 Less studied, but no less influential over the century, were wound treatises by Bartolemeo Maggi (1477–1552), Francisco Arceo (1493–1571), Mariano Santo (1498–c. 1550), Pierre Franco (c. 1500–1561), and Dionisio Daza Chacón (1510–1596).30–34 While variations occurred, most of the therapeutic approaches mirrored that for other wounds, following 1 of the 2 medieval patterns that had been established by such authorities as Henri de Mondeville and Guy de Chauliac: (a) cleaning the wound, application of an ointment or balm, and either allowance of suppuration (laudable pus) or sutured closure; or (b) cautery with a hot iron.35 Over that first century’s experience with these wounds, the former much more than the latter approach was favored.36 Even while many treatments were familiar, the novelty of the combined crush/burn/poison/penetrate pathology provoked new combinations of old interventions.37 By the late 16th/early 17th century, provocative innovations included using paper instead of linen for wound dressing on British ships.38 Fat, too, became a popular addition to treatment by the late 16th century.39 A rising concern with the perception of wound poisoning was likely incepted with Hieronymus Brunschwig’s Buch der Cirurgia, Hantwirckung der Wundartzny (1497).40
This apprehension over poisoning received substantial support from Giovanni da Vigo (d. c. 1525), who chafed at the difference in quality of the injuries in comparison to those of arrow, halberd, and sword while treating patients for ‘warrior-pope’ Julius II at the 1485 siege of Saluces. He fumbled with language for these lesions, lumping them as wounds caused by ‘arquebuses, bombards, and similar instruments,’ not described by authors ancient or modern (p. 223). Da Vigo summarized wound characteristics to include the contusio of the mechanical impact, the combustio of the shot’s heat and the powder, and a more novel intoxicatio from the powder-shot itself.41 With the last, he hypothesized that gunshots were poisonous, largely from the powder, and, as a consequence, advocated a burning cautery oil to remedy the toxin.21,42–44 It was not surprising, since poisons were expanding as an etiology in medical theory at this time.45–47
Da Vigo’s work spread rapidly throughout Europe, but not without resistance.30,48 Famously, Ambroise Paré, then a ‘lowly’ barber-surgeon, ran out of the oil at the Battle of Turin in 1537 due to supply-chain issues; he was forced to switch to an admixture of turpentine, egg yolk, and rose oil. The resulting radical improvement of his patients sparked his advocacy for an alteration in wound treatment. He would also become a proponent of amputation and of vascular ligation for gunshot-related injuries.49–51 Paré’s subsequent publications made him a celebrity in the 16th century and the so-called ‘father of military surgery.’
INSTITUTIONALIZATION OF GSW MANAGEMENT IN THE EARLY MODERN ERA
Paré more appropriately belongs in the Early Modern Era, a chronologically ambiguous period between the Middle Ages and the modern world that was critical to the evolution of the natural sciences generally and medicine specifically. In the classic example of rejecting boiling oil in the treatment of GSWs, Paré relied on empirical evidence: what he experienced dictated his beliefs rather than what he had read in textbooks. This emphasis on personal knowledge catalyzed advances in anatomy, like Andreas Vesalius’ famous De Humani Corporis Fabrica (1543), and physiology, with William Harvey expostulating on the circulation of blood in De Moto Cordis (1628). It also stimulated the work of John Hunter, often called the father of scientific surgery, as his observations on casualties of the Seven Years War (1756–1763) on Bellisle led to the publication of A Treatise on the Blood, Inflammation, and Gunshot Wounds in 1793.52 Noting that most prior medical authors emphasized early and radical interventions, Hunter instead strongly recommended a more conservative approach. While he recognized the unique nature of GSWs, the increased severity of high-velocity missiles, and their tendency to create necrotic tissue that denied healing by primary intention, he also used multiple case studies from the Seven Years War to illustrate how surgery often caused more harm than good. Specifically, he opposed extensive bloodletting of GSW victims, dilating wounds, and efforts to remove the offending missile in most circumstances. While published posthumously, Hunter’s Treatise garnered immediate attention in the English-speaking world and influenced management for decades.
Paré and Hunter are perhaps the most famous examples of early modern practitioners relying on their personal experience to upend dogma around the care of gunshot victims. Albeit exceptional representations, they reflect not only the intellectual change but also the professionalization of surgery in this era. Surgeons increasingly demonstrated singular expertise in this area of medical care, further showcasing valuable skills distinct from those of physicians, apothecaries, and barbers. Historians have shown how through the early modern era surgeons became more familiar with GSWs than other classes of practitioners, with this pathology at times forming their largest focus of treatment.53,54 The contemporaneous rise of the nation state led to sovereigns chartering surgical communities with privileges and responsibilities to the crown, usually related to military surgical training and certification. One of the common privileges was anatomy, highlighting the societal commitment to improving the quality of care. This trend would reach its apogee with the 18th-century French d’Académie Royale de Chirurgie.55 Thus, emerging from the cacophony of military trauma came a symphony of professional and intellectual progression.
Developments in amputation represented one of those advances. Evidence of surgical amputation dates back 31,000 years, with detailed descriptions persisting from antiquity and the Middle Ages, but the surgical practice evolved and expanded in this early modern era.56,57 Indeed, the word ‘amputation’ itself was initially used in a surgical context by Paré in 1564 and was not seen in English-language sources until the 17th century when John Woodall called it ‘the most lamentable part of chirurgery’58,59 (Fig. 2). William Clowes performed the first documented successful above the knee amputation in 1588, and Pierre Verduin’s 1697 manuscript marked the earliest text dedicated exclusively to the subject.60,61 This attention resulted partly from surgeons establishing their identity and expertise as a professional group but mostly from efforts to treat this new pathology: GSWs. Historian John Kirkup noted that amputations following bladed injuries were rare through the ancient and medieval era—patients either exsanguinated before reaching medical care or were able to heal; while amputation was often recommended in the Middle Ages following bites from poisonous animals, examples of practitioners implementing that advice are infrequent.37,58 However, GSWs, as Hunter and other authors recognized, often caused devastating bony and soft tissue damage, prompting doctors to amputate the offended extremity in efforts to save the life of the patient.
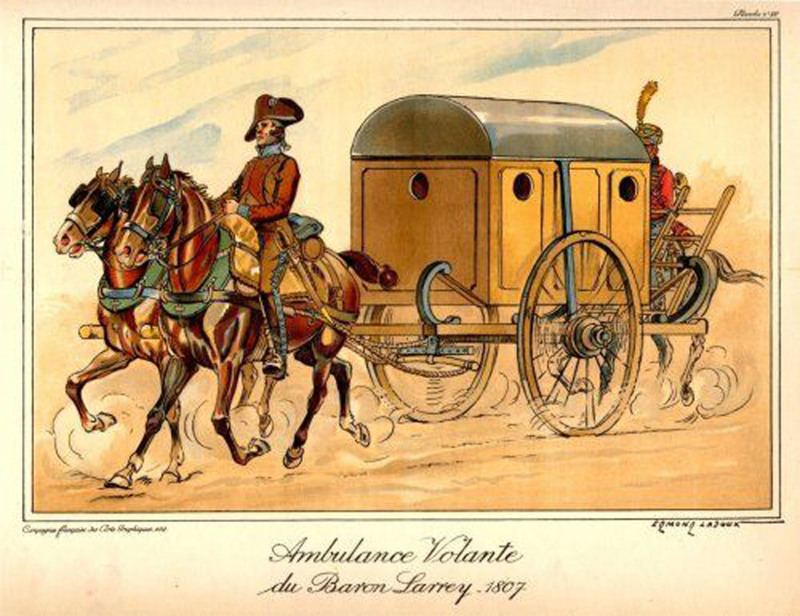
FIGURE 2.
A rare illuminated version of Gersdorff’s classic amputation scene in his 1517 text Feldtbuch der Wundartzney.28 This is the first known portrayal of an amputation, of which Gersdorff himself performed over 200. The patient here is sitting, which was the most common position for amputation until the 19th century. No one holds him down, but a cloth over his head shields his gaze. Despite the presence of a windlass tourniquet above the knee, arterial blood pulsates from the major arteries in the leg; a spare tourniquet and knife lay on the table in the foreground while a patient stands in the back clutching the stump of his recently amputated left hand. Image in the public domain; this version from Reynolds-Finley Historical Library at the University of Alabama Birmingham, used with permission.
As surgeons began amputating more limbs, they developed novel techniques and competing philosophies. Initially, most surgeons performed what today would be called a guillotine amputation and used hot irons to cauterize all bleeding points. Paré famously recommended ligating vessels, using his bec de corbin to grasp arteries and veins, but few doctors adopted his method initially due to the difficulty of visualizing the vasculature in a bloody field.62 In 1718, French surgeon Jean Petit invented the screw tourniquet63 (Fig. 3). For centuries previous, clinicians had used various forms of ligature-like tourniquets, some with the so-called Spanish windlass design, but they were often awkward, challenging to apply efficiently, and rarely worked well (see the pulsating blood in Fig. 2 despite the presence of an older tourniquet).65 Petit’s screw tourniquet revolutionized the field. Easy for a single person to apply and nearly always effective, it endured through the First World War and serves as a model for tourniquets today. The technology catalyzed the transition from cautery to vessel ligation, which became standard of care by the end of the 18th-century. Simultaneously, there was a shift toward circular technique. In 1679, James Yonge described marking out a flap to cover the cut end, an idea he credited to a Mr. C. Lowdher of Exeter.66 But the flap technique did not catch on until the late 19th century, with Yonge himself trying this approach only once. Rather, by the close of the 18th century, the majority of surgeons utilized the circular technique, variously attributed to Petit and/or William Cheseldon.67 In the so-called ‘double-cut’ or circular method, the soft tissue was incised and retracted proximally before transecting the bone such that the soft tissue could then be pulled back down to form a stump more amenable to a prosthesis. This approach spread widely throughout Europe, although it still required 3 to 6 months of healing. By 1800, almost all European surgeons utilized a version of Petit’s tourniquet to practice a circular amputation. They disagreed, however, about the appropriate timing of surgery relevant to wounding, a debate made especially relevant by the ongoing Napoleonic Wars where millions of Europeans sallied against each other in the continent’s largest battles.
FIGURE 3.
Petit’s screw tourniquet. Originally fashioned with a wooden buckle and screw, it quickly adopted the more durable brass. This model dates from the 1820s. Its resemblance to modern tourniquets such as the CAT highlights the persisting influence of this technology. Owen Wangensteen believed ‘it was certainly one of the most important surgical discoveries before the advent of anesthesia.’64 Image in the public domain, courtesy of the Wellcome Collection.
The Wars of the French Revolution and Napoleon (1793–1815) presented an unprecedented number of gunshot victims to the attention of surgeons: famous French surgeon Dominique-Jean Larrey allegedly performed over 200 amputations for GSW in a single 24-hour period following the Battle of Borodino, seemingly extraordinary numbers but ones characteristic of the era.68,69 Overall, clinical care changed minimally: aside from the occasional chest tube or trephination, surgeons rarely intervened on truncal and cranial wounds, preferring to allow them to heal via secondary intention rather than attempting a sutured closure.4,70 Wounded extremities typically resulted in amputation, although by the end of the war, both sides tried to manage some conditions more conservatively: both Larrey and George Guthrie of the British Army came to advocate for immobilization of compound arm and lower leg fractures, with good results.71 In contrast, Guthrie conducted an early clinical trial of sorts that demonstrated the importance of prompt amputation for compound femur fractures resulting from GSW.72,73
With most surgeons favoring the circular method of amputation, they actively discussed when to perform the operation. Some, such as John Hunter and Johann Bilguer, the Surgeon General of the Royal Prussian Army during the reign of Frederick the Great, advocated for delayed amputation—to allow the patient to stabilize (or die) and the wound to declare itself prior to any operation.52,74 Others, including Guthrie and Larrey, promoted prompt intervention, ideally within 1 to 4 hours of injury.69,73 By the end of the Napoleonic Wars, early amputation had achieved wide acceptance among both the British and French medical services. This shift in practice resulted more from organizational changes in military medicine rather than clinical developments. Guthrie and James McGrigor helped professionalize the British military medical system, organizing effective evacuation chains and positioning regimental hospitals directly behind the front lines.75–77 More famously, Larrey introduced his ‘flying ambulances,’ which, along with Pierre-Francois Percy’s administrative reforms, simultaneously brought surgeons closer to the front and transported patients speedily to the rear78,79 (Fig. 4). Whereas Hunter saw patients who had been wounded hours or days prior and correctly deduced their inability to tolerate a capital operation, Larrey and Guthrie encountered them promptly post injury and recognized the benefit immediate intervention would have on their transportation and convalescence. As seen throughout this history, factors outside the operating room significantly influenced what happened within it.
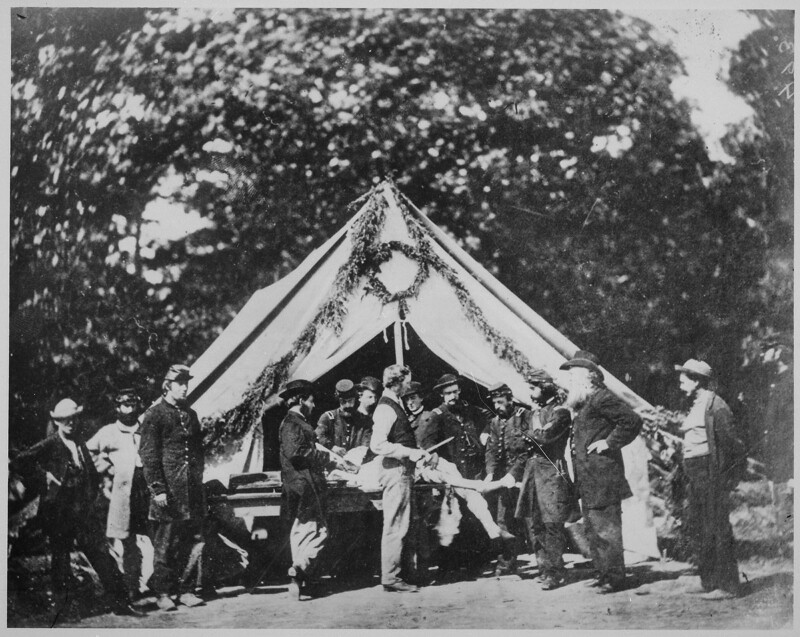
FIGURE 4.
Circa 1920 color rendition of Larrey’s flying ambulance by the French artist Edmond Lajoux. (Original black and white line drawings available in Larrey’s memoirs.69) Note the springs over each wheel base, a rare feature of ambulance before Larrey but one on which he insisted to provide a more comfortable ride to the wounded. Image in the public domain: https://commons.wikimedia.org/wiki/File:Ambulance_of_the_French_Army.jpg (accessed December 14, 2022).
The volume of casualties drew attention to the condition now known as shock. Like amputation, the concept of physiologic depletion following injury dates to antiquity but gained substantial momentum with the introduction of firearms. The word itself originates from French surgeon Henri Ledran who, in 1731, wrote how the body suffered a jarring (secousse) when struck by a bullet; in 1740, John Sparrow translated the text into English, using the word ‘shock.’80,81 The idea of systemic effects resulting from a local wound spread quickly, albeit in various manifestations with numerous explanations. Hunter opined that the body sympathized with the wounded part52; his student Astley Cooper defined it as a constitutional irritation;82 Guthrie dubbed it ‘constitutional alarm.’83 By the mid-19th century, the word ‘shock’ predominated in most European languages, and surgical textbooks of the era usually included a chapter covering the topic. The pathology remained poorly understood, but through the end of the century most medical authorities believed it was due to disturbances in or mediated through the nervous system. Attempts at treating shock with various stimulants largely failed.
The introduction of anesthesia in 1846–1847 benefitted casualties in the American Civil War (1861–1865). Some surgeons initially looked askance at the seemingly miraculous therapy, concerned of its dangerous potential84; Guthrie came to attribute increases in shock to chloroform inhalation, perhaps influenced by the 1848 chloroform death of Hannah Greener.85 These reactions delayed its implementation. By the 1860s, however, surgeons had widely adopted the new drug. Despites Hollywood’s interpretation, it was nearly ubiquitous in the US Civil War: only 254 of the documented 80,000 operations on Union soldiers proceeded without anesthesia.86 It did not, however, substantially change management. Intra-cranial, intra-thoracic, and intra-abdominal operations remained exquisitely rare—and rarely successful. During the Civil War, 62% of patients with penetrating chest wounds and 89% of patients with abdominal wounds died.87 Therapy again focused on managing mangled extremities, now afflicted by the new minié bullet fired at comparatively high velocity and more prone to deformation on impact, causing devastating effects on tissue.
Treatment chiefly comprised of amputation—over 30,000 operations on the Union side alone (Fig. 5). While Civil War surgeons attained a reputation for being over-eager to cleave limbs, both contemporaries and later historians believed the opposite. W.W. Keen, who made tremendous strides diagnosing and treating neurological sequelae of GSW such as neuralgia and later edited the most popular surgical textbook in the United States‚ averred, ‘the popular opinion that the surgeons did a large amount of unnecessary amputating may have been justified in a few cases, but taking the army as a whole, I have no hesitation in saying that far more lives were lost from refusal to amputate.’88,89 With the triage and evacuation system designed and implemented by Jonathan Letterman, by 1863 most Union casualties reached field hospitals relatively quickly, and early, or primary, amputation was again favored.90 Doctors employed both the circular and flap techniques, per personal preference, although circulars from the Surgeon General’s office dictated when and where to amputate in an effort to standardize practice. Overall, about 26% of amputees died from their wounds, with the rate differing dramatically by anatomical location. Hip disarticulations carried a nearly 85% fatality.86 And while still high, these numbers demonstrated significant improvement from the Napoleonic and Crimean Wars.
FIGURE 5.
Amputation being performed in front of a hospital tent—where there was superior lighting compared to indoors—on the Gettysburg battlefield in July of 1863. Given photographic technology of the era, it is unlikely that this is a live-action shot, either being staged or at least a deliberate pause. Note the officer at the head of the bed administering what is likely chloroform anesthesia through a cloth. Image in the public domain from the National Library of Medicine (https://www.nlm.nih.gov/exhibition/lifeandlimb/images/OB1210.jpg), accessed December 14, 2022.
Recognizing the appalling consequences of losing a limb, surgeons attempted more conservative approaches. This included the ‘excision technique,’ an early form of debridement that resected the portion of afflicted bone, although without joining the defect.86 A lengthier procedure than amputation, excision left a floppy and essentially useless limb. The procedure never gained widespread popularity, but it represented surgeons’ quest to utilize less morbid yet still life-saving operations for their patients. Physicians also had the challenge of managing poorly understood conditions such as gangrene and erysipelas that sometimes developed in the hospital wards following seemingly successful procedures. While acceptance of the germ theory remained years in the future, military medical officers came to appreciate the contagious nature of these conditions and associated them with a fetid atmosphere or contamination. They tried various decontamination strategies such as pouring solutions of bromine and nitric acid into the wounds, seemingly with good effect, though with poor understanding as to its mechanism.86,91 Informal trials based on case histories led to active discussions surrounding the optimal treatment but no universally applied guidelines.
More important than any technical or procedural advance, the Civil War catalyzed the union of science and surgery in the United States. The war integrated previously academic disciplines such as anatomical dissection, microscopy, and clinical research into the daily practice of military medical officers by demanding the submission of case reports (Circular No. 5); creating an Army Medical Museum of specimens (Circular No. 2); funding new investigations; and providing an overabundance of research material.91 This new scientific interest manifested itself in the 6-volume tome Medical and Surgical History of the War of Rebellion.92 Building on rising interest in the new field of statistics, it catalogued hundreds of thousands of medical and surgical cases submitted by thousands of military medical officers, creating a resource upon which Americans and Europeans would rely for decades. While there had always been exceptional figures such as John Hunter, the Civil War highlighted the importance of science in surgery for the average practitioners in small town America. In so doing, it prepared a generation of physicians to accept a looming paradigm shift in medicine: the germ theory of disease.
GSWs IN SURGERY IN THE ERA OF THE GERM THEORY
The late 19th century proved an era of rapid advances in all fields of medicine as modern science and technology introduced new theories, devices, and clinical approaches into the discipline.93 In 1867, Joseph Lister published his since-classic article describing the salutary effects of carbolic acid on wound healing—and, critically, linking these empiric results to the fledgling germ theory of disease.94 First accepted widely in Germany, antiseptic and later aseptic surgery slowly spread throughout Europe and the United States.95,96 By 1890, aseptic operations were standard of care in the western world. The technique improved mortality following extremity injuries but did not significantly influence management, which remained chiefly amputation. However, it revolutionized the treatment of intra-cavity and particularly intra-abdominal GSWs.
By the late 19th century, civilian surgical practice changed to exploring patients shot in the abdomen. This trend appeared prominently in the American literature where the post-Civil War West remained an area of active conflict, with cities such as Denver and Phoenix just recently considered the frontier. Notably, Union soldiers were permitted to purchase and keep their service weapons, contributing to a proliferation of firearms, as did the advent of mail-order purchases (eg, Sears began selling revolvers in its catalogs in 1892).97 Presentations on the topic featured prominently in meetings of the American and especially the Southern Surgical Associations (SSA).98,99 After an 1896 SSA paper ‘Bullet Wounds of the Abdomen’ insisted on exploration GSW to the abdomen, Johns Hopkins surgeon Howard Kelly proposed the following resolution: ‘it is the sense of the members of the Southern Surgical and Gynecologic Association that in GSWs penetrating the abdominal cavity, the proper routine procedure is to make an immediate exploratory abdominal incision.’99 This resolution was unanimously carried. While national statistics for the era do not exist, surgical societies, contemporary textbooks, and the published literature in the United States all widely supported exploratory celiotomy. Notably, this shift toward operative interventions for abdominal pathology extended across all realms of surgery, as appendectomies, gastric ulcer repair, and ovariotomies simultaneously rose to prominence; explorations for bullet wounds was part of this larger movement.100 Europe, with lower levels of gun violence, gradually followed the American lead.
The new technology of X-rays facilitated this exploration. Accidentally discovered by William Roentgen in 1895, machines spread rapidly.101 Even with technical limitations of the era, bullets appeared prominently on contemporary radiographs, which quickly replaced the searching fingers and Nélaton probes of yore. While X-rays had little effect on fracture management for years, they immediately impacted the treatment of GSWs.102 In 1898, just three years after their invention, the US military used them extensively when managing casualties in the Spanish American War103 (Fig. 6). They rapidly became a fixture in civilian and military hospitals alike.
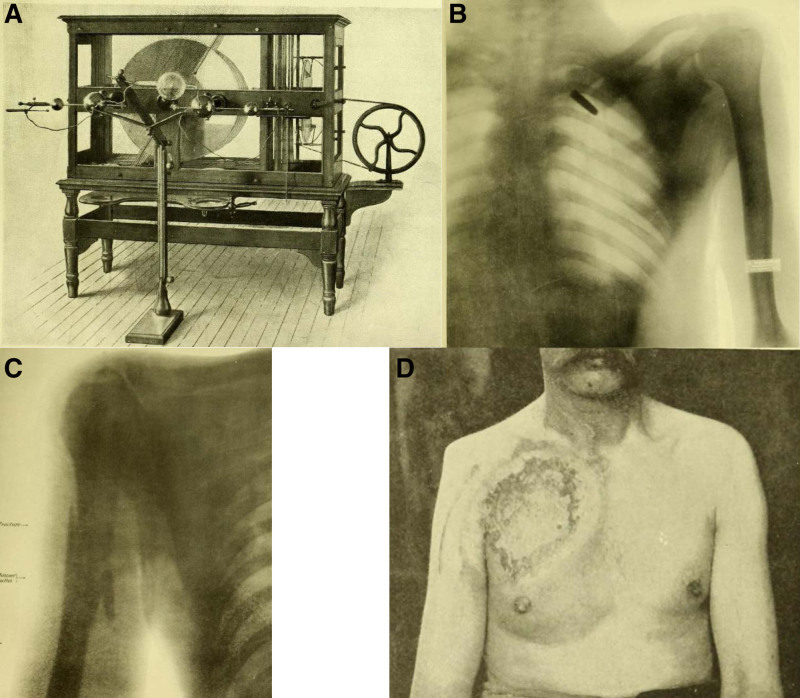
FIGURE 6.
A, Wimshurst-Holtz-type static machine for taking the roentegraphs. They were made by Otis Clapp & Son in Providence, RI and weighed more than 500 pounds each. B, chest X-ray showing a Mauser bullet in Private C. James Edwards. C, Mauser bullet resulting in a humerus fracture in Private Clarence Reed of H Company, 10th US Infantry Division. D, X-ray skin burns on Private Thomas McKenna, of C Company, 6th US Infantry Division, demonstrating how contemporaries still had not mastered the technology, with considerable side effects for patients. All images in the public domain in Borden’s book The Use of the Röentgen Ray….103
Surgeons increasingly studied their discipline in the laboratory as well as the clinic, and these investigations led to the modern field of wound ballistics. Nobel Laureate Theodor Kocher published a series of influential treatises in the late 19th century that, first, rejected the common hypothesis about the roles of bullet heat and centrifugal motion in causing tissue damage; second, highlighted the significance of bullet materials to its deformation on impact—and how that deformation exacerbated morbidity; and third, noted the creation of a hydraulic pressure cavity that formed along the bullet’s trajectory. He also pioneered the use of gelatin as a tissue-substitute for testing, variations of which remain standard to this day. More importantly, Kocher catalyzed the field of wound ballistics as both a legitimate and highly scientific enterprise worthy of surgeons’ attention.104–106 Others followed suit. William MacCormack formalized the concept of cavitation, which Charles Woodruff expanded upon, delineating the relationship between kinetic energy transfer and wounding effects. American surgeon and military officer Louis La Garde published several critical studies on ballistics and definitively proved that bullets are not sterile, despite their high velocities.107,108 These reports eventually contributed to the 1899 Hague Convention, which mandated the use of full metal jacketed rounds in wars between signatories of the treaty. Civilian munitions, and those used against non-European foes, continued to vary widely.
Given these developments, it is perhaps surprising, in hindsight, that military doctrine for abdominal GSWs remained primarily non-operative for fin de siècle conflicts. In the Spanish American (1898), Boer (1899–1902), and Russo-Japanese (1904–1905) Wars, medical doctrine and experience all dictated conservative management for this injury pattern.109–111 Of the 207 abdominal wounds the British suffered in South Africa, surgeons explored only 26, with 18 deaths. Post-operative mortality was so high among Japanese patients that their Surgeon General forbade laparotomy at forward facilities.112 Care of extremity injuries remained essentially unchanged: some efforts at debridement with amputation as necessary. Certainly, medical officers in these 3 conflicts had accepted the germ theory of disease, internalized the importance of aseptic technique, and appreciated the value of novel operations such as appendectomy and gastrectomy. But conditions—and perceptions—in these wars precluded common celiotomies. Military forces used the new, smaller caliber, full metal jacketed bullet, which contemporaries observed/believed to cause clean, through-and-through wounds less in need of operative repair. The battlefields, particularly the South African veldts and Manchurian steppes, were thought to be sterile, theoretically eliminating environmental infection. Military medical services remained disorganized, distances were often vast, and casualty numbers, especially in Manchuria, were excessive, all of which effectively combined to triage patients: those who would have benefited from a laparotomy often died before reaching a surgeon, or presented too weak to tolerate a major operation. Hale appearing casualties with abdominal GSW appeared to recover without intervention. Despite famous exceptions such as Princess Vera Gedroits, most military surgeons left the conflicts strongly recommending non-operative management, including those who previously advocated laparotomies, such as the American Nicholas Senn and Englishman Frederick Treves.113 When these physicians returned to their home countries and reported their experiences, the civilian surgical community often scorned their conclusions.98,114 Thus emerged a separation: in the cities, surgeons were operating on almost all abdominal GSWs, but on the battlefields, patients received little more than an aseptic bandage and hot cup of coffee or tea.
WORLD WAR I
This practice changed in World War I (1914–1919). Medical services of all nations entered the war espousing the conservative doctrine established in prior battles but quickly recognized its failure.115–117 Applying the lessons of Larrey and Letterman, European forces developed a tiered-triage system of forward hospitals that was effectively in place by 1916. While sometimes overwhelmed by the sheer number of casualties, challenging terrain, and near-constant artillery bombardment, these facilities brought surgery temporally closer to the frontlines than in any previous war and contributed to a change in surgical practice.118 Based on doctrine accumulated from earlier conflicts, medical officers initially supported wounded in action medically but offered little surgical intervention. The results were abysmal. Early in the war, 25% of injured extremities required amputation, often due to avoidable infection; mortality from abdominal GSWs exceeded 70%.115 Sepsis caused a significant portion of this morbidity as tetanus and soft tissue infections spread systemically.
The military medical system recognized the problem and returned to a century-old solution: debridement. Fiercely advocated by the likes of Le Dran and later Pierre Deasult in the Napoleonic Wars, debridement had since waned in popularity.119 Bacteriology had the potential to buttress its importance, particularly Paul Friedrich’s classic studies showing how wound infection progresses to septicemia—and the roughly 6-hour window physicians have to intervene to prevent it.120 But before World War I, leaders had taken away the wrong message, believing various antiseptics could replace surgical extirpation. This assumption proved wrong in the manure-laden trenches of Western Europe. British surgeon H.W. Gray, and especially French surgeon Antoine DePage, came not only to appreciate the importance of surgically debriding wounds but also to propagate this practice through their respective armies.121 Cuthbert Wallace and others extended this principle to abdominal wounds, fiercely advocating for exploratory laparotomies.122 By 1917, surgical wound debridement, including laparotomy, became standard of care for GSWs on the Western Front (Fig. 7). Antiseptic systems, most famously the Carrel-Dakin technique, buttressed operative intervention and later saw widespread use at home for civilian injuries.123,124
FIGURE 7.
American frontline hospital in World War I. Note the nurse anesthetists administering general anesthesia; physician-trained anesthesiologists were uncommon before the Korean War. Image courtesy of the US Army Signal Corps and is in the public domain.
Surgical efforts benefited from broader developments in medicine. The aforementioned hospital system and ambulances reduced the time from injury to treatment. Bacteriology brought vaccines and, critically, tetanus anti-toxin. Anesthesia, including the new technique of spinal blocks, was universally applied.125 X-ray machines were positioned at the most forward location surgery was performed. Research into the etiology of shock, while still primitive by modern standards, brought attention to the condition and established the importance of resuscitation.126 It also contributed to blood transfusions, which, while relatively small in both number of transfusions and volume transfused, set the stage for the expansion of this therapy in later years.127 By the end of the First World War, surgeons had established the core tenets of GSW management that applied in civilian and military circumstances alike. Future decades would add supporting therapies and alter the techniques, but the foundation of early resuscitation and aggressive surgical intervention remains unchanged.
THE INTERWAR YEARS
The interwar years saw comparatively little clinical progression. In the 1920s, the Germans invented the first antibiotics, sulfa drugs, and in the Spanish Civil War, Joseph Trueta wrote about the utility of prolonged immobilization in avoiding amputation for GSWs to the extremities.128,129 Scientifically, Alfred Blalock established the critical relevance of hemorrhage to shock, solidifying the value of blood transfusions.130 Far more important were organizational, legal, and cultural changes. First civilian and then military hospitals created blood banks to ensure an adequate supply of this precious commodity.131 The American College of Surgeons inaugurated the Committee on Trauma in 1922, and the American Association for the Surgery of Trauma was founded in 1939, with accompanying meetings and journals, forming legitimate, institutional homes for research in the field.132
These decades also originated gun control in the United States, where gangster-led shootouts such at the famous St. Valentine’s Day Massacre of 1929 captured popular and police attention. Gun homicide rate climbed sharply in cities like Chicago.97 In 1934, Congress passed the National Firearms Act, which limited the sale of automatic weapons, sawed-off shotguns, and silencers.133 A second act in 1938 required all gun dealers to have a Federal license. Whereas various municipalities had patchwork regulations dating back to the 19th century, these laws were the first national response to the problem of gun violence. Gun buyers and sellers were not the only parties with new legal requirements: physicians soon had a mandatory obligation to report GSWs in their hospitals and clinics. Part of a Progressive Era movement in America to measure and thus reduce crime, these statutes spread from state-to-state, commencing in New York in 1926.134 Given the plethora of reporting requirements today (child abuse, communicable disease, etc), relaying gunshot injuries to the police may seem reasonable, but at the time many physicians perceived the regulation as a profound breech in confidentiality of the doctor-patient relationship. An editorial in JAMA condemned the law, warning that wounded individuals would avoid medical attention for fear of arrest.135 These concerns notwithstanding, one US state after another passed a patchwork of laws that generally mandated reporting. This was also a uniquely American phenomenon. The first Canadian province to enact similar legislation was Ontario, in 2005.136
THE SECOND WORLD WAR AND BEYOND
World War II (1939–1945) remains the largest war in history, with millions of casualties, yet the treatment of GSW patients developed only incrementally.137 Evacuation chains sought to bring the wounded to surgeons expeditiously, aiming for arrival times under 6 hours to align with Friedrich’s studies.120 Given the apparent success of dusting sulfa powder into wounds at Pearl Harbor and the promise of the logistically simpler plasma infusions Edwin Cohn had fractionated, the US military initially over-relied on technological fixes to GSWs.128,138 However, the experience in North Africa quickly retaught the lessons from World War I viz, the importance of exploring injuries and debriding devitalized tissue, the utility of delayed primary closure, and the value of blood-based resuscitation. Certainly, ancillary care improved as blood transfusions became far more common with the new understanding of shock, and penicillin replaced sulfa drugs as a much more effective antibiotic.139
Perhaps most importantly, World War II demonstrated the value of specialization. While most American doctors remained general practitioners, residency training for surgeons had slowly spread in the interwar years and begun to create a distinct class of practitioners.140 The military recognized their value with a higher rank and salary, assigning them roles that capitalized on their expertise. In the continental United States, the Army Surgeon General created specialty hospitals in orthopedics, spine injuries, ophthalmic problems, renal disorders and other fields.141 Relaying the specific developments in GSW management for each specialty remains outside the scope of this article, but these centers highlighted the advantages and promise of focusing intellectual and technological resources on particular problems. The number of disfigured casualties from the World Wars also catalyzed the expansion of new disciplines dedicated to rehabilitation.142,143 Medicine—and surgery specifically—had expanded beyond which a single figure like Larrey or Guthrie could master in its entirety. For medical, social, and economic reasons, the World War II experience stimulated a rapid expansion of residencies in all fields.140,144 Surgery residency programs approved by the American College of Surgeons more than doubled between 1945 and 1950. The number of anesthesia residency spots ballooned 10-fold between 1940 and 1960.145,146 Other specialties grew as well.
The post-World War II years fundamentally changed both the doctor and patient experience with trauma from the time of shooting through post-operative care. Following the 1966 Accidental Death and Disability report, the Federal government funded the creation of emergency medical systems, with ambulances, newly certified paramedics, and 911 call-centers providing a coordinated response.147 This evacuation chain brought patients to new hospitals, many of which arose from the 1946 Hill-Burton Act that prioritized the construction of such facilities in rural America; over 550 new hospitals were built between 1946 and 1956 alone.148 Once there, patients were often greeted by physicians working in the nascent but growing field of Emergency Medicine, which triaged and stabilized new admissions.149 Intensive care units, derived from the cardiac care units of the 1950s, deployed a vast array of technology including dialysis machines, ventilators, and an armamentarium of new drugs to help patients recover from their injuries.148,150,151 ICUs and their interventions represented just one facet of an increased reliance on technology in medicine and especially surgery.152 Shaped by military needs (eg, ultrasound; nuclear medicine), economic incentives, and social forces of innovation, new instruments, devices, and drugs soon touched all aspects of patient care.101,153–155 Much of the funding for this technology emanated from the newly prominent National Institutes of Health, which saw its budget explode from a mere $464,000/y in 1939 to $400 million/y by 1960 to over $3 billion/y by 1980. NIH grants catalyzed the creation of the modern surgeon-scientist, whose investigations shaped the evolving management of GSW throughout the 20th century.156 This combination of care led to certification of Trauma Centers by the end of the century that not only specialized in treating these cases but were also dedicated to researching ways to improve that care.
Certainly, surgical techniques for treating GSWs continued to evolve in the post-World War II years. In the Korean War, surgeons progressed from ligating vascular injuries to repairing them, an advance that rapidly spread throughout civilian practice.157 The mandate of colostomies for colon injuries ended a few decades later, with primary repair saving thousands of patients the morbidity of an ostomy.158 Automatically operating all abdominal GSW—international dogma from 1917 onwards—came under investigation as civilian surgeons recognized a difference between military-grade injuries and those from low-velocity weapons common in urban violence. Noting a high number of non-therapeutic laparotomies, pioneers such as Gerald Shaftan at major trauma centers like Kings County Hospital in New York, LA County Hospital in Los Angeles, Charity Hospital in New Orleans, and Groote Shuur Hospital in Cape Town, South Africa, began publishing large series of patients whom they managed non-operatively in the 1960s, with encouraging results.159–163 Initial reception ranged from curious to hostile, but subsequent investigations have repeatedly validated this approach. A recent database study found American hospitals selecting non-operative management of abdominal GSWs in roughly 25% of cases with excellent results, apostasy to an earlier generation of surgeons but now standard of care.164
More systemically, the concept of staged, damage-control surgery emerged from studies on hepatic trauma in Detroit in the 1960s to 1970s to propagate throughout the field.165,166 Other modifications abound in both the literature and on the hospital wards. But far more important than these individualized developments was the environment wounded patients entered. Overarching surgical principles of GSW management changed little from 1918. More importantly, the training surgeons obtained; the hospitals to which patients were admitted; the tools, techniques, technologies, and drugs available for treatment; and the systems put in place all have combined to create a milieu that has revolutionized the care of GSWs in the late 20th century.
GLOBAL WAR ON TERROR AND CONCLUSIONS
The last 20+ years have offered a unique circumstance, with a simmering War on Terror abroad combined with an epidemic of gun violence in the United States. Although injury patterns between the military and civilian populations differ, practitioners in and out of uniform benefitted from the crossover of pathology, particularly in these more recent conflicts with relatively low volumes of casualties compared to prior wars. Surgeons who served overseas brought their combat experience home while hospitals with high rates of penetrating trauma helped train military practitioners before deployments, highlighting the symbiotic relationship between these 2 interrelated clinical realms that has persisted for centuries.167,168 Specific management practices also moved back and forth, with tourniquets, for example, regaining substantial popularity overseas for treating GSWs to the extremity; they have since become ubiquitous in American ambulances and emergency departments.65,169 Resuscitation strategies have also evolved away from large-volume crystalloid infusions that were advocated in the 1960s to the notion of permissive hypotension maintained with a balanced 1:1:1 transfusion protocol, and one that increasingly favors the whole blood used on the battlefields of World War II to Vietnam.170
Tourniquets and transfusion strategies expose the ever-shifting, often cyclic nature of this history. Interventions come and go and come again, passing ‘through-and-through’ history as the epidemiology, culture, technology, and circumstances surrounding GSWs change over time. Throughout, physicians and surgeons have made conscious, dedicated efforts to apply the latest science, technology, and expertise to managing this pathology. Interventions have varied from Jean da Vigo pouring boiling oil into GSW to modern surgeons pouring the latest hemostatic powder into one. In all these cases, the focus has been on the patient. The specifics of how surgeons will treat GSW patients 100 years hence remains to be written, but the general principles will endure. This special issue repeatedly espouses the lack of simple answers to the problem of gun violence in the United States. Prevention clearly remains preferable to treatment. But given the surfeit of firearms in this country, a political climate currently favoring de-regulation, and a culture that tolerates (glorifies?) violence, shootings will continue apace. As physicians and surgeons, we have the responsibility and duty to intervene—as we have done for centuries past.
ACKNOWLEDGMENTS
J.B. participated in research design, writing of the paper, performance of the research, data analysis, and editing and revisions. W.O.S. participated in research design, writing of the paper, performance of the research, data analysis, and editing and revisions. C.B.H. participated in research design, performance of research, data analysis, and editing and revisions. W.S.M. participated in research design, performance of research, data analysis, and editing and revisions. S.D. participated in research design, performance of research, data analysis, and editing and revisions. D.C.S. participated in research design, writing of the paper, performance of research, data analysis, and editing and revisions.
Footnotes
Published online 17 July 2023
Disclosure: The authors declare that they have nothing to disclose.
REFERENCES
- 1.Simon TR, Kegler SR, Zwald ML, et al. Notes from the field: increases in firearm homicide and suicide rates — United States, 2020–2021. MMWR Morb Mortal Wkly Rep. 2022;71:1286–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.BradyCampaign. Gun violence by the numbers. Available at: https://www.bradyunited.org/key-statistics. Accessed September 17, 2022.
- 3.Chon DS. The Relationship between National Homicide Rates and Medical Care. Indiana University Press; 2002. [Google Scholar]
- 4.Billroth Theodor. Historical studies on the nature and treatment of gunshot wounds from the fifteenth century to the present time. Translated by C. P. Rhoads Yale Journal of Biology and Medicine; vol. 4, issue 1 (1931): 2-36; vol 4, issue 2 (1931): 118-148; vol. 4, issue 3 (1931): 224–257. [PMC free article] [PubMed] [Google Scholar]
- 5.Barr J, Schalick WO, III, Shortell CK. Surgeons in the time of plague: Guy de Chauliac in fourteenth-century France. J Vasc Surg Cases Innov Tech. 2020;6:657–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McVaugh M. The Rational Surgery of the Middle Ages. Firenzae Press; 2006. [Google Scholar]
- 7.Brockliss LWB, Jones C. The Medical World of Early Modern France. Clarendon Press; 1997. [Google Scholar]
- 8.Wallis F. Pre-modern surgery: wounds, words, and the paradox of ‘Tradition’. In: Schlich T, ed. The Palgrave Handbook of the History of Surgery. Palgrave Macmillan; 2018:49–70. [Google Scholar]
- 9.Andrade T. The Gunpowder Age: China, Military Innovation, and the Rise of the West in World History. Princeton University Press; 2016. [Google Scholar]
- 10.Beck RT. The Cutting Edge: Early History of the Surgeons of London. Lund Humphries; 1974. [Google Scholar]
- 11.Clephan RC. The ordnance of the fourteenth and fifteenth centuries. Archaeol J. 1911;68:49–138. [Google Scholar]
- 12.Lalanne L. Recherches sur le Feu Grégeois et sur l’Introduction de la Poudre à Canon en Europe. J. Corréard; 1845. [Google Scholar]
- 13.Lynnerup N, Mikkelsen H, Poulsne K, et al. A firearms fatality from 14th century Denmark. J Paleopathol. 2001;13:11–16. [Google Scholar]
- 14.Gee D. Suicide of a prisoner with multiple missiles: a case report. Med Sci Law. 1996;36:85–90. [DOI] [PubMed] [Google Scholar]
- 15.Lederer D. Suicide in the early modern world. In: Antony R, Carroll S, Pennock CD, eds. The Cambridge History of World Violence. Cambridge University Press; 2020:311–328. [Google Scholar]
- 16.Rogers CJ. (ed). The Military Revolution Debate: Readings on the Military Transformation of Early Modern Europe. Westerview Press; 1995. [Google Scholar]
- 17.Leng R. Anleitung Schiesspulver Zu bereiten, Buechsen Zu be laden und Zu beschiessen: Eine kriegstechnische Bilderhandschrift im clm 600 der Bayerischen Staatsbibliothek. Ludwig Reichert; 2000. [Google Scholar]
- 18.Washa QM. Philosophical Saltpeter: The Origins and Influence of Gunpowder Technology and the Paracelsian Aerial Niter. University of Minnesota; 2019. [Google Scholar]
- 19.Voss MJ. Between the Cannon and the Book: Mathematicians and Military Culture in Sixteenth-Century Italy. Johns Hopkins University; 1994. [Google Scholar]
- 20.Cunningham J. Sickness, disease and medical practitioners in 1640s Ireland. In: Cunningham J, ed. Early Modern Ireland and the World of Medicine: Practitioners, Collectors and Contexts. Manchester University Press; 2019:61–83. [PubMed] [Google Scholar]
- 21.DeVries KR. Military surgical practice and the advent of gunpowder weaponry. Can Bull Med Hist. 1990;7:131–146. [DOI] [PubMed] [Google Scholar]
- 22.Turner WJ, Lee CL. (eds). Trauma in Medeival Society. Brill; 2018. [Google Scholar]
- 23.Hudson GL. Disabled veterans and the state in early modern England. In: Gerber DA, ed. Disabled Veterans in History. University of Michigan Press; 2012:117–144. [Google Scholar]
- 24.Vollmuth R. ‘Von Den Geschosszenen Wunden’: Die Behandlung Von Schusswunden in Deutschsprachigen Chirurgischen Werken Des 15. Jahrhunderts. Orvostört Közl. 1994;40:5–28. [PubMed] [Google Scholar]
- 25.Vollmuth R. Anmerkungen zur Behandlung von Scrwsswunden durch Feuerwaffen in deutschsprachigen chirurgischen Werken des 15.Jahrhunderts. Würzb Medizinhist Mitt. 2001;20:36–42. [PubMed] [Google Scholar]
- 26.Vollmuth R. Anmerkungen zur Behandlung von Scrwsswunden durch Feuerwaffen in deutschsprachigen chirurgischen Werken des 15.Jahrhunderts. Würzb Medizinhist Mitt. 1998;17:205–214. [PubMed] [Google Scholar]
- 27.Eamon W. Pharmaceutical self-fashioning or how to get rich and famous in the renaissance medical marketplace. Pharm Hist. 2003;45:123–129. [PubMed] [Google Scholar]
- 28.Gersdorff Hv. Feldtbůch der Wundartzney: Newlich Getruckt und Gebessert. Hans Schotten zům Thyergarten; 1528. [Google Scholar]
- 29.Vasilopoulos A, Tsoucalas G, Thomaidis V, et al. Hans von Gersdorff and Hans Wechtlin: when battlefield surgery and anatomy met art. Int Medi. 2020;2:74–78. [Google Scholar]
- 30.Maggi B. De Vulnerum Sclopertorum, et Bombardarum Curatione Tractatus. Bartholomeum Bonardum; 1552. [Google Scholar]
- 31.Dusolier M. Aperçu Historique sur la Médecine en Espagne, Particulièrement au XVIe Siècle. Henri Jouve; 1906. [Google Scholar]
- 32.Santo M. La Pratica Universale in Cirugia. Di Nuovo Riformata, et dal Latino Ridotta à la Sua Vera Lettura con le Figure in Disegno de Semplici nel Settimo Libro. Appresso Vi è un Bellissimo Compendio, Che Tratta dell’istessa Materia, Composto per Mariano Santo Barolitano. Con due Trattati di Giovanni Andrea dalla Croce, l’Uno in Materia della Ferite, l’Altro del Cavar l’Armi, e le Saette Fuori della Carne. Et di Nuovo Aggiuntivi Molti Capitoli Estratti dalle Opere dell’Eccellentissimo dottor Signor Leon. Ghirardo & Iseppo Imberti; 1622. [Google Scholar]
- 33.Di Matteo B, Tarabella V, Filardo G, et al. The Renaissance and the universal surgeon: Giovanni Andrea Della Croce, a master of traumatology. Int Orthop. 2013;37:2523–2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de la Rosa S. La Obra Quirurgica de Dionisio Daza Chacón. Universidad de Salamanca; 1958. [Google Scholar]
- 35.Lindskog GE. Some historical aspects of thoracic trauma. J Thorac Cardiovasc Surg. 1961;42:1–11. [PubMed] [Google Scholar]
- 36.Woosnam-Savage RC, DeVries KR. Battle trauma in medieval warfare: wounds, weapons and armor. In: Taylor L, DeVries KR, eds. Wounds and Wound Repair in Medieval Culture. Brill; 2015:1–11. [Google Scholar]
- 37.Kirkup J. Perceptions of amputation before and after gunpowder. Vesalius. 1995;1:51–58. [PubMed] [Google Scholar]
- 38.Leong E. Papering the household: paper, recipes, and everyday technologies in early modern England. In: Bittel CJ, Leong EYT, von Oertzen C, eds. Working with Paper: Gendered Practices in the History of Knowledge. University of Pittsburgh Press; 2019:32–45. [Google Scholar]
- 39.Thomas W. How a defeat became a victory: the siege of Ostend in contemporary Dutch war coverage and post-war chronicles (1601–15). In: Fagel RP, Frnacés LA, Belmonte BS, eds. Early Modern War Narratives and the Revolt in the Low Countries. Manchester University Press; 2020:125–145. [Google Scholar]
- 40.Brunschwig H. Dis ist das Buch der Cirurgia: Hantwirckung der Wund Artzney. Johann Schönsperger; 1497. [Google Scholar]
- 41.de Vigo G. de Vigo en Françoys. La Practique et Cirurgie de Excellent Docteur en Medecine Maistre Jehan de Vigo Nouvellement Imprimee et Recogneue Diligentement sur le Latin avec les Aphorismes et Canons de Cirurgie, Composez par Maistre Nicolas Godin Docteur en Medecine Lesquelz sont Inserez en la Fin de ce Present Livre apres la Partie Compendieuse. Division de Ladicte Practique. La Premiere Partie est Nommee la Copieuse Contenant Neuf Livres Particuliers. La Seconde est Dicte Compendieuse qui Contient Cinq Livres Particuliers: Lesquelz sont Declarez en la Page Sequente. Armoul Langelier; 1542. [Google Scholar]
- 42.Donaldson IML. Ambroise Paré’s accounts of new methods for treating gunshot wounds and burns. J R Soc Med. 2015;108:457–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hernández MM. El Morbo Gálico en la Obra del Doctor Francisco Arceo de Fregenal, un Médico Extremeño del Renacimiento. Universidad de Extremadura; 2017. [Google Scholar]
- 44.da Vigo G. The Whole Worke of that Famous Chirurgion Maister John Vigo. Gale T. T. East; 1586. [Google Scholar]
- 45.Hausse H. Bones of contention: the decision to amputate in early modern Germany. Sixt Century J. 2016;47:327–350. [Google Scholar]
- 46.Gibbs FW. Poison, Medicine, and Disease in Late Medieval and Early Modern Europe. Routledge; 2019. [Google Scholar]
- 47.Manton WI. Lead poisoning from gunshots: a five century heritage. J Toxicol Clin Toxicol. 1994;32:387–389. [DOI] [PubMed] [Google Scholar]
- 48.Siraisi NG. History, Medicine, and the Traditions of Renaissance Learning. University of Michigan; 2007. [Google Scholar]
- 49.Clasper J. The management of military wounds in the middle ages. In: Kirkham A, Warr C, eds. Wounds in the Middle Ages. Ashgate; 2004:17–39. [Google Scholar]
- 50.Malgaigne JF. Surgery and Ambroise Paré. In: Hamby WB, ed. University of Oklahoma Press; 1965. [Google Scholar]
- 51.Hill BH, Jr, Ambroise Paré: sawbones or scientist? J Hist Med Allied Sci. 1960;XV:45–58. [Google Scholar]
- 52.Hunter J. A Treatise on the Blood, Inflammation, and Gun-shot Wounds. John Richardson; 1794. [Google Scholar]
- 53.Jütte R. A seventeenth-century German barber-surgeon and his patients. Med Hist. 1989;33:184–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nutton V. Humanist surgery. In: Wear A, French RK, Lonie IM, eds. The Medical Renaissance of the Sixteenth Century. Cambridge University Press; 1985. [Google Scholar]
- 55.Gelfand T. Professionalizing Modern Medicine: Paris Surgeons and Medical Science and Institutions in the 18th Century. Greenwood Press; 1980. [Google Scholar]
- 56.Maloney TR, Dilkes-Hall IE, Vlok M, et al. Surgical amputation of a limb 31,000 years ago in Borneo. Nature. 2022;609:547–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Banham D, Voth C. The diagnosis and treatment of wounds in the old English medical collections: Anglo-Saxon surgery? In: Tracy L, DeVries K, eds. Wounds and Wound Repair in Medieval Culture. Brill; 2015:153–174. [Google Scholar]
- 58.Kirkup J. A History of Limb Amputation. Springer; 2007. [Google Scholar]
- 59.Woodall J. The Surgion’s Mate. Edward Griffin; 1617. [Google Scholar]
- 60.Clowes W. A Prooved Practice for All Young Chirurgions, Concerning Burnings with Gunpowder, and Wounds Made with Gunshot, Sward, Halbard, Pyke, Lance or Such Other. Thomas Orwyn; 1588. [Google Scholar]
- 61.Verduin PA. Nouvellle Methode pour Amputer les Membres. Jeam Wolters; 1697. [Google Scholar]
- 62.Paré A. Dix Livres de las Chirurgie, avec Le Magasin des Instruments Necessaires à Icelle. De l’imprimerie de Jean le Royer; 1564. [Google Scholar]
- 63.Petit J-L. D’un Nouvel Instrument de Chirurgie Historie de l’Académie Royale des Sciences; 1718. [Google Scholar]
- 64.Wangensteen OD, Wangensteen SA. The Rise of Surgery: from Empiric Craft to Scientific Discipline. University of Minnesota Press; 1978. [Google Scholar]
- 65.Kragh JF, Swan KG, Smith DC, et al. Historical review of emergency tourniquet use to stop bleeding. Am J Surg. 2012;203:242–252. [DOI] [PubMed] [Google Scholar]
- 66.Yonge J. Currus Triumphalis e Terebintho. 1679. [Google Scholar]
- 67.Lister J. Amputation. In: Holmes T, Packard JH, eds. A System of Surgery, Theoretical and Practical. H.C. Lea’s Son & Co; 1881:51–90. [Google Scholar]
- 68.Skandalakis PN, Lainas P, Zoras O, et al. “To afford the wounded speedy assistance”: Dominique Jean Larrey and Napoleon. World J Surg. 2006;30:1392–1399. [DOI] [PubMed] [Google Scholar]
- 69.Larrey DJ. Mémoires de Chirurgie Militaire et Campagnes. Chez J. Smith; 1812. [Google Scholar]
- 70.Crumplin M. Men of Steel: Surgery in the Napoleonic Wars. Quiller Press; 2007. [Google Scholar]
- 71.Wangensteen SD, Wangensteen OH. Successful pre-Listerian antiseptic management of compound fracture: Crowther (1802), Larrey (1824), and Bennion (ca. 1840). Surgery. 1971;69:811–824. [PubMed] [Google Scholar]
- 72.Malhan NK, Greenslade T, Mitchell PD. George Guthrie’s clinical trial at the Napoleonic war battle of Toulouse in 1814. J Med Biogr. 2009;17:139–143. [DOI] [PubMed] [Google Scholar]
- 73.Guthrie GJ. On Gunshot Wounds of the Extremities Requiring Different Operations of Amputation, with their After-treatment. Longmand, Hurst, Rees, Ornes, and Brown; 1815. [Google Scholar]
- 74.Bilguer JU. A Dissertation on the Intutility of the Amputation of Limbs. Tissot SAD. R. Baldwin; 1764. [Google Scholar]
- 75.Blanco RL. Wellington’s Surgeon General: Sir James McGrigor. Duke University Press; 1974. [Google Scholar]
- 76.Kelly C. War and the Militarization of British Army Medicine, 1793–1830. Pickering and Chatto; 2011. [Google Scholar]
- 77.Cantlie N. A History of the Army Medical Department. Churchill Livingstone; 1974. [Google Scholar]
- 78.Dible JH. Napoleon’s Surgeon. Heinemann; 1970. [Google Scholar]
- 79.Percy P-F. Journal des Campagnes du Baron Percy, Chirurgien en Chef de la Grande Armée, 1754–1825. Plon-Nourrit; 1904. [Google Scholar]
- 80.Le Dran H-F. Observations in Surgery. In: Sparrow J. Printed for James Hodges; 1740. [Google Scholar]
- 81.English PC. Shock, Physiological Surgery, and George Washington Crile: Medical Innovation in the Progressive Era. Greenwood Press; 1980. [Google Scholar]
- 82.Cooper A. The Lectures of Sir Astley Cooper on the Principles and Practices of Surgery. Vol. 3. W. Simpkin and R. Marshall; 1827. [Google Scholar]
- 83.Guthrie GJ. A Treatise on Gunshot Wounds, on Inflammation, Erysipelas, and Mortification, on Injuries of Nerves and on Wounds of the Extremities. Burgess and Hill; 1827. [Google Scholar]
- 84.Pernick MS. A Calculus of Suffering: Pain, Professionalism, and Anesthesia in Nineteenth-Century America. Columbia University Press; 1985. [Google Scholar]
- 85.Guthrie GJ. Treatise on Gun-Shot Wounds, on Inflammation, Erysipelas, and Mortification, on Injuries of Nerves, and on Wounds of the Extremities Requiring the Different Operations of Amputation: in Which the Various Methods of Performing these Operations are Shown, Together with their After Treatment; and Containing an Account of the Author’s Successful Case of Amputation at the Hip Joint... Being a Record of the Opinions and Practice of the Surgical Department of the British Army, at the Termination of the Wars in Spain, Portugal, France, and the Netherlands, in 1814 and 1815, with Additions Relating to those in the Crimea, in 1854–5. 6th ed. Renshaw; 1855. [Google Scholar]
- 86.Bollet AJ. Civil War Medicine: Challenges and Triumphs. Galen Press, Ltd.; 2002. [Google Scholar]
- 87.Gillet MC. The Army Medical Department 1818–1865. Center of Military History; 2000. [Google Scholar]
- 88.Keen WW. Surgical reminiscences of the Civil War. Addresses and Other Papers. W.B. Saunders; 1905:420–441. [Google Scholar]
- 89.Adams GW. Doctors in Blue: the Medical History of the Union Army in the Civil War. H. Schuman; 1952. [Google Scholar]
- 90.Letterman J. Medical Recollections of the Army of the Potomac. D. Appleton and Company; 1866. [Google Scholar]
- 91.Devine S. Learning from the Wounded: the Civil War and the Rise of American Medical Science. University of North Carolina Press; 2014. [Google Scholar]
- 92.Barnes JK, Woodward JJ, Smart C, Otis GA, Huntington DL. The Medical and Surgical History of the War of the Rebellion (1861–65). United States Government Printing Office; 1870–1888. [Google Scholar]
- 93.Bynum WF. Science and the Practice of Medicine in the Nineteenth Century. Cambridge University Press; 1994. [Google Scholar]
- 94.Lister J. On the antiseptic principle of the practice of surgery. Lancet. 1867;91:353–356. [Google Scholar]
- 95.Gariepy TP. The introduction and acceptance of Listerian antisepsis in the United States. J Hist Med Allied Sci. 1994;49:167–206. [DOI] [PubMed] [Google Scholar]
- 96.Gaw JL. “A Time to Heal”: the diffusion of Listerism in Victorian Britain. Transactions of the American Philosophical Society. 1999;89:iii–168. [Google Scholar]
- 97.Weaver GS. Firearm deaths, gun availability, and legal regulatory changes: suggestions from the data. J Crim Law Criminol. 2002;92:823–842. [Google Scholar]
- 98.Ravitch MM. A Century of Surgery: The History of the American Surgical Association. Lippincott; 1981. [Google Scholar]
- 99.Sparkman RS. (ed). The Southern Surgical Association: The First 100 Years. J.B. Lippincott; 1989. [Google Scholar]
- 100.Smith DC. A historical overview of the recognition of appendicitis. N Y State J Med. 1986;86:571–583. [PubMed] [Google Scholar]
- 101.Kevles BH. Naked to the Bone: Medical Imaging in the Twentieth Century. Rutgers University Press; 1987. [Google Scholar]
- 102.Howell JD. Technology in the Hospital: Transforming Patient Care in the Early Twentieth Century. Johns Hopkins University Press; 1995. [PubMed] [Google Scholar]
- 103.Borden WC, Sternberg GM. The Use of the Röntgen Ray by the Medical Department of the United States Army in the War with Spain. Government Printing Office; 1900. [Google Scholar]
- 104.Fackler ML, Dougherty PJ. Theodor Kocher and the scientific foundation of wound ballistics. Surg Gynecol Obstet. 1991;172:153–160. [PubMed] [Google Scholar]
- 105.Bellamy RF, Zajtchuk R. The evolution of wound ballistics: a brief history. In: Bellamy RF, Zajtchuk R, eds. Conventional Warfare: Ballistics, Blast, and Burn Injuries. Office of the Surgeon General; 1991:83–105. [Google Scholar]
- 106.Kocher T. Ueber die Sprengwirkung der Modernen Kleingewehr-Geschosse. Cor Bl Schweiz Aerzte; 1875:5. [Google Scholar]
- 107.La Garde LA. Septic bullets and septic powders. Med Rec. 1895;47:784–785. [Google Scholar]
- 108.La Garde LA. Gunshot Injuries: How They are Inflicted, Their Complications and Treatment. 2nd ed. William Wood and Company; 1916. [Google Scholar]
- 109.Cirillo VJ. Bullets and Bacilli: The Spanish-American War and Military Medicine. Rutgers University Press; 2004. [Google Scholar]
- 110.Makins GH. Surgical Experiences in South Africa, 1899-1900; Being Mainly a Clinical Study of the Nature and Effects of Injuries Produced by Bullets of Small Calibre. 2nd ed. Frowde; 1913. [Google Scholar]
- 111.Barr J. Military medicine of the Russo-Japanese war and its influence on the modernization of the US Army medical department. US Army Med Dep J. 2016:118–128. [PubMed] [Google Scholar]
- 112.Wallace C. War surgery of the abdomen. Lancet. 1917;I:561–568. [Google Scholar]
- 113.Bennett JDC. Princess Vera Gedroits: military surgeon, poet, and author. BMJ. 1992;305:1532–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nancrede CB. The effects of modern small-arm projectiles, as shown by the wounded of the fifth army corps, during the campaign resulting in the capture of Santiago de Cuba. Transactions of the Meeting of the American Surgical Association. 1899;17(43–71). [Google Scholar]
- 115.Harrison M. The Medical War: British Military Medicine in World War I. Oxford University Press; 2010. [Google Scholar]
- 116.van Bergen L. Before My Helpless Sight: Suffering, Dying, and Military Medicine on the Western Front. Walters L. Ashgate; 2009. [Google Scholar]
- 117.Jaffin J. Medical Support for the American Expeditionary Forces in France During the First World War. Command and General Staff College; 1991. [Google Scholar]
- 118.Barr J, Cancio LC, Smith DJ, et al. From trench to bedside: military surgery during World War I upon its centennial. Mil Med. 2019;184:214–220. [DOI] [PubMed] [Google Scholar]
- 119.Reichert FL. The historical development of the procedure termed débridement. Bull Johns Hopkins Hosp. 1928;42:93–104. [Google Scholar]
- 120.Friedrich PL. Die aseptische versorgung frischer wundern. Arch Klin Chir. 1898;57:288–310. [Google Scholar]
- 121.Helling TS, Daon E. In Flanders Fields: the Great War, Antoine Depage, and the resurgence of debridement. Ann Surg. 1998;228:173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bamberger PK. The adoption of laparotomy for the treatment of penetrating abdominal wounds in war. Mil Med. 1996;161:189–196. [PubMed] [Google Scholar]
- 123.Carrel A. Traitement abortif de l’infection des plaies. Bull Acad Med Paris. 1915;74:361–368. [Google Scholar]
- 124.Haller JS, Jr. Treatment of infected wounds during the Great War, 1914 to 1918. South Med J. 1992;85:303–315. [DOI] [PubMed] [Google Scholar]
- 125.Courington FW, Calverley RK. Anesthesia on the western front: the Anglo-American experience of World War I. Anesthesiology. 1986;65:642–653. [DOI] [PubMed] [Google Scholar]
- 126.Archibald EW, McLean W. Observations upon shock, with particular reference to the condition as seen in war surgery. Ann Surg. 1917;66:280–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Pelis K. Taking credit: the Canadian army medical corps and the British conversion to blood transfusion in WWI. J Hist Med Allied Sci. 2001;56:238–277. [DOI] [PubMed] [Google Scholar]
- 128.Lesch JE. The First Miracle Drugs: How the Sulfa Drugs Transformed Medicine. Oxford University Press; 2007. [Google Scholar]
- 129.Trueta J. Treatment of War Wounds and Fractures, with Special Reference to the Closed Method as Used in the War in Spain. Hamish Hamilton Medical Books; 1939. [Google Scholar]
- 130.Blalock A. Shock: further studies with particular reference to the effects of hemorrhage. Arch Surg. 1934;29:837–857. [DOI] [PubMed] [Google Scholar]
- 131.Swanson KW. Banking on the Body: the Market in Blood, Milk, and Sperm in Modern America. Harvard University Press; 2014. [Google Scholar]
- 132.Peltier LF, Davis JH. A history of the American Association for the Surgery of Trauma: the first 50 years. J Trauma. 1989;29:143–151. [DOI] [PubMed] [Google Scholar]
- 133.National Firearms Act, Public Law 474. 1934.
- 134.Robinson LN. History of criminal statistics (1908–1933). J Crim Law Criminol. 1933;24:125–139. [Google Scholar]
- 135.Editorial: Compulsory reporting of gunshot wounds. J Am Med Assoc. 1927;88:404. [Google Scholar]
- 136.Martin AF. The adoption of mandatory gunshot wound reporting legislation in Canada: a decade of tension in lawmaking at the intersection of law enforcement and public health. McGill J Law Health. 2016;9:173–214. [Google Scholar]
- 137.Cowdrey AE. Fighting for Life: American Military Medicine in World War II. Free Press; 1994. [Google Scholar]
- 138.Creager ANH. What blood told Dr Cohn: World War II, plasma fractionation, and the growth of human blood research. Stud Hist Phil Sci Part C. 1999;30:377–405. [Google Scholar]
- 139.Bud R. Penicillin: Triumph and Tragedy. Oxford University Press; 2007. [Google Scholar]
- 140.Barr J. The education of American surgeons and the rise of surgical residencies, 1930–1960. J Hist Med Allied Sci. 2018;73:274–302. [DOI] [PubMed] [Google Scholar]
- 141.Barr J, Cherry KJ, Rich NM. Vascular surgery in World War II: the shift to repairing arteries. Ann Surg. 2016;263:615–620. [DOI] [PubMed] [Google Scholar]
- 142.Linker B. War’s Waste: Rehabilitation in World War I America. University of Chicago Press; 2011. [Google Scholar]
- 143.Anderson J. War, Disability, and Rehabilitation in Britain: ‘Soul of a Nation’. Manchester University Press; 2011. [Google Scholar]
- 144.Ludmerer KM. Let Me Heal: the Opportunity to Preserve Excellence in American Medicine. Oxford University Press; 2015. [Google Scholar]
- 145.Waisel DB. The role of World War II and the European theater of operations in the development of anesthesiology as a physician specialty in the USA. Anesthesiology. 2001;94:907–914. [DOI] [PubMed] [Google Scholar]
- 146.Romanelli T, Bacon DR. The origins of modern anesthesia throughout the American experience spanning the world wars. Bull Anesth Hist. 1999;17:14–17. [DOI] [PubMed] [Google Scholar]
- 147.Simpson AT. Transporting Lazarus: physicians, the state, and the creation of the modern paramedic and ambulance, 1955–73. J Hist Med Allied Sci. 2013;68:163–197. [DOI] [PubMed] [Google Scholar]
- 148.Stevens R. In Sickness and in Wealth: American Hospitals in the Twentieth Century. Johns Hopkins University Press; 1989. [Google Scholar]
- 149.Zink BJ. Anyone, Anything, Anytime: a History of Emergency Medicine. Mosby; 2006. [Google Scholar]
- 150.Fye WB. Caring for the Heart: Mayo Clinic and the Rise of Specialization. Oxford University Press; 2015. [Google Scholar]
- 151.Peitzman SJ. Dropsy, Dialysis, Transplant: a Short History of Failing Kidneys. Johns Hopkins University Press; 2007. [Google Scholar]
- 152.Schlich T, Crenner C. Technological change in surgery: an introductory essay. In: Schlich T, Crenner C, eds. Technological Change in Modern Surgery. Rochester University Press; 2017. [Google Scholar]
- 153.Creager ANH. Life Atomic: a History of Radioisotopes in Science and Medicine. University of Chicago Press; 2013. [Google Scholar]
- 154.Buderi R. The Invention that Changed the World: How a Small Groups of Radar Pioneers Won the Second World War and Launched a Technological Revolution. Simon and Schuster; 1996. [Google Scholar]
- 155.Barr J, Smith DC. The history of trauma. In: Browner B, ed. Skeletal Trauma. Elsevier; 2019:2–24. [Google Scholar]
- 156.Fox DM. The politics of the NIH extramural program, 1937–1950. J Hist Med Allied Sci. 1987;42:447–466. [DOI] [PubMed] [Google Scholar]
- 157.Barr J. Of Life and Limb: Surgical Repair of the Arteries in War and Peace, 1880–1960. University of Rochester Press; 2019. [Google Scholar]
- 158.Chappuis CW, Frey DJ, Dietzen CD, et al. Management of penetrating colon injuries. a prospective randomized trial. Ann Surg. 1991;213:492–497; discussion 497–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.McAlvanah MJ, Shaftan GW. Selective conservatism in penetrating abdominal wounds: a continuing reappraisal. J Trauma Acute Care Surg. 1978;18:206–212. [DOI] [PubMed] [Google Scholar]
- 160.Nance FC, Wennar MH, Johnson LW, et al. Surgical judgment in the management of penetrating wounds of the abdomen: experience with 2212 patients. Ann Surg. 1974;179:639–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Navsaria PH, Nicol AJ, Edu S, et al. Selective nonoperative management in 1106 patients with abdominal gunshot wounds: conclusions on safety, efficacy, and the role of selective CT imaging in a prospective single-center study. Ann Surg. 2015;261:760–764. [DOI] [PubMed] [Google Scholar]
- 162.Velmahos GC, Demetriades D, Toutouzas KG, et al. Selective nonoperative management in 1,856 patients with abdominal gunshot wounds: should routine laparotomy still be the standard of care? Ann Surg. 2001;234:395–402; discussion 402–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Shaftan GW. Indications for operation in abdominal trauma. Am J Surg. 1960;99:657–664. [DOI] [PubMed] [Google Scholar]
- 164.Masjedi A, Asmar S, Bible L, et al. The evolution of nonoperative management of abdominal gunshot wounds in the United States. J Surg Res. 2020;253:224–231. [DOI] [PubMed] [Google Scholar]
- 165.Lucas CE, Ledgerwood AM. Prospective evaluation of hemostatic techniques for liver injuries. J Trauma Acute Care Surg. 1976;16:442–451. [DOI] [PubMed] [Google Scholar]
- 166.Feliciano DV, Mattox KL, Jordan GL, Jr. Intra-abdominal packing for control of hepatic hemorrhage: a reappraisal. J Trauma Acute Care Surg. 1981;21:285–290. [DOI] [PubMed] [Google Scholar]
- 167.Schreiber MA, Holcomb JB, Conaway CW, et al. Military trauma training performed in a civilian trauma center. J Surg Res. 2002;104:8–14. [DOI] [PubMed] [Google Scholar]
- 168.Kellermann A, Elster E, Babington C, et al. Out of the Crucible: How the US Military Transformed Combat Casualty Care in Iraq and Afghanistan. Office of the Surgeon General; 2018. [Google Scholar]
- 169.Schroll R, Smith A, McSwain NE, Jr, et al. A multi-institutional analysis of prehospital tourniquet use. J Trauma Acute Care Surg. 2015;79:10–14. [DOI] [PubMed] [Google Scholar]
- 170.Borgman MA, Spinella PC, Perkins JG, et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma Acute Care Surg. 2007;63:805–813. [DOI] [PubMed] [Google Scholar]