Abstract
Objective
To evaluate the effects of breastfeeding on maternal weight loss in the 12 months postpartum among U.S. women.
Methods
Using data from a national cohort of U.S. women conducted in 2005-2007 (N=2,102), we employed propensity scores to match women who breastfed exclusively and non-exclusive for at least three months to comparison women who had not breastfed or breastfed for less than three months. Outcomes included postpartum weight loss at 3, 6, 9, and 12 months postpartum; and the probability of returning to pre-pregnancy body mass index (BMI) category and the probability of returning to pre-pregnancy weight.
Results
Compared to women who did not breastfeed or breastfed non-exclusively, exclusive breastfeeding for at least 3 months resulted in 3.2 pounds (95% CI: 1.4,4.7) greater weight loss at 12 months postpartum, a 6.0-percentage-point increase (95% CI: 2.3,9.7) in the probability of returning to the same or lower BMI category postpartum; and a 6.1-percentage-point increase (95% CI: 1.0,11.3) in the probability of returning to pre-pregnancy weight or lower postpartum. Non-exclusive breastfeeding did not significantly affect any outcomes.
Conclusion
Our study provides evidence that exclusive breastfeeding for at least three months has a small effect on postpartum weight loss among U.S. women.
Keywords: breastfeeding, weight loss, obesity, Infant Feeding Practices Study II
Introduction
Failure to lose pregnancy-related weight is an important contributor to long-term obesity and related serious chronic conditions among women (Rooney and Schauberger, 2002, Amorim et al., 2007, Lipsky et al., 2012, Hu, 2003, Cogswell et al., 2001). Breastfeeding may promote postpartum weight loss, due to the caloric expenditures required for lactation (Dewey, 1997) or metabolic changes that are favorable to weight loss (Stuebe and Rich-Edwards, 2009). Previous literature examining the relationship between breastfeeding and weight loss in the postpartum period has produced mixed results (Neville et al., 2013, Ip et al., 2007, Janney et al., 1997, Ostbye et al., 2012, Krause et al., 2010, Gould Rothberg et al., 2011). Currently 41% of U.S. women breastfeed exclusively for 3 months and 19% breastfeed exclusively for 6 months, with considerable variation among states (Centers for Disease Control and Prevention, 2014). More than a third of U.S. women are obese (Flegal et al., 2012), with state obesity prevalence varying from 18.6% to 34.4% (Centers for Disease Control and Prevention, 2010). To the extent that interventions promoting breastfeeding are effective, (Chung et al., 2008, Labarere et al., 2005) it is important to better understand maternal benefits of breastfeeding.
A key shortcoming of the literature among U.S. women is selection; that is, women who choose to breastfeed their infants are systematically different than those women who do not choose to breastfeed their infants on important confounders. Because it is not possible to randomly assign breastfeeding status to women, we use propensity score matching in a national cohort of U.S. women to estimate the effect of breastfeeding on postpartum weight loss. This approach allows us to balance the distribution of covariates between women who do and do not breastfeed, similar to what would be achieved in a study using experimental methods. We hypothesized that women who breastfed for at least 3 months would have greater postpartum weight loss, and would have greater probabilities of returning to their pre-pregnancy body mass index (BMI) category and returning to their pre-pregnancy weight, relative to women who did not breastfeed or breastfed for less than 3 months.
Methods
Data
The Infant Feeding Practices Study II (IFPS II) is a national cohort study that followed U.S. women from the last trimester of pregnancy through 12 months postpartum in order to collect detailed information about infant feeding. The U.S. Food and Drug Administration and Centers for Disease Control and Prevention conducted the study; detailed descriptions of the study design and methods have been previously published (Fein et al., 2008). Briefly, women were sampled during their third trimester of pregnancy from a national consumer opinion panel. Participants completed a prenatal questionnaire during the third trimester of pregnancy, a telephone interview close to the birth of their infant, and 10 postpartum questionnaires during the 12 months postpartum. Questionnaires asked about demographics, health history, social support, infant feeding, and breastfeeding and breast milk pumping practices. Response rates were 77% for the month 1 questionnaire, 79% for the month 3 questionnaire, 71% for the month 6 questionnaire, and 65% for the month 12 questionnaire (Fein et al., 2008).
The Johns Hopkins Bloomberg School of Public Health Institutional Review Board (IRB) determined that this study was a secondary data analysis of an existing, de-identified, publicly available dataset that did not require IRB oversight.
This study was funded by the National Heart, Lung, and Blood Institute (NHLBI) of the U.S. National Institutes of Health. NHLBI had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Outcomes
The primary outcomes were the change in weight from a woman's highest pregnancy weight to her post-pregnancy weight at 3 months, 6 months, 9 months, and 12 months postpartum, measured continuously in pounds. The highest pregnancy weight was reported approximately 2-4 weeks post-delivery. Among women who were not underweight (i.e., had a BMI≥18.5 kg/m2) pre-pregnancy, we also examined the probability of returning to pre-pregnancy BMI category or lower, and the probability of returning to pre-pregnancy weight or lower. Outcomes were calculated based on self-reported weight and height.
Breastfeeding definitions
We defined two breastfeeding variables. The first breastfeeding variable was a binary measure of exclusive breastfeeding, which was defined as a woman reporting feeding her infant breast milk exclusively (either breastfeeding or bottle feeding of expressed breast milk) for at least the first 3 months of the infant's life. For exclusively breastfeeding women, the comparison group was women who reported not feeding their infant any breast milk as well as women who reported non-exclusive feeding of breast milk, during the first 3 months. The second breastfeeding variable was a binary measure of non-exclusive breastfeeding for at least 3 months, defined as a woman reporting non-exclusively feeding her infant breast milk (either breastfeeding or bottle feeding of expressed breast milk) for at least the first 3 months of the infant's life. The comparison group for non-exclusively breastfeeding women included women who never breastfed and women who breastfed non-exclusively for less than three months.
Although the American Academy of Pediatrics (AAP) recommends exclusive breastfeeding for about 6 months, (American Academy of Pediatrics, 2012) we used 3 months' breastfeeding to define the breastfeeding variables. It appears plausible that energy expenditures due to lactation in the first three months are sufficient to promote weight loss (Brewer et al., 1989, Baker et al., 2008). Because U.S. law requires 12 workweeks' medical leave for employed individuals, 3 months of breastfeeding may represent an actionable goal for many women. Additionally, few women in the current dataset (n=91) exclusively breastfed their infants for 6 months.
Statistical analysis
We generated propensity scores (Rosenbaum, 1983) to match women who reported exclusive or non-exclusive breastfeeding for at least the first 3 months of their infant's life (the two breastfeeding groups) to those who did not breastfeed for 3 months (the two comparison groups), conducting the matching separately for each of our two breastfeeding definitions. Propensity score matching provided two major advantages over traditional multivariable regression adjustment approaches (Stuart, 2010). First, propensity score matching allowed us to achieve balance on observed covariates between women who did and did not breastfeed, ensuring that the two groups were comparable on those measures (Dehejia and Wahba, 2002). Second, the matching process was conducted without using data on the outcomes of interest, leading to a study design that was created independently of the expected outcome (Rubin, 2007).
The propensity score model was a logistic regression in which the response variable was a binary measure of breastfeeding (either of the two breastfeeding definitions) and the independent variables were individual-level covariates that have been shown in the literature to be associated with breastfeeding (Scanlon et al., 2010, Liu et al., 2010, Scott et al., 2006). Covariates included maternal demographic factors (age, race/ethnicity, parity, educational attainment, and whether the infant was enrolled in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC)); health/medical factors (pre-pregnancy obesity, prenatal insurance coverage, whether a woman smoked any cigarettes three months postpartum, having a cesarean-section birth, and whether the infant was in the intensive care unit for 3 days or less after birth); and breastfeeding support (whether the infant's pediatrician recommended exclusive breastfeeding, and prenatal breastfeeding intention). We considered including gestational weight gain in the models, however, exploratory data analysis indicated that pre-pregnancy obesity status was a stronger predictor of breastfeeding and was highly correlated with gestational weight gain. Given state variability in breastfeeding rates, we also considered matching on state of residence, but including state indicator variables did not substantially change the results and were therefore not included.
Analyses employed full matching, which is a flexible propensity score matching method that groups all study subjects into matched subclasses, each containing at least one subject from the breastfeeding group and at least one subject from the comparison group (Stuart and Green, 2008). Full matching generates weights for each subject. (See Appendix for a detailed description of propensity score methods). After conducting the propensity score matching, we used a “doubly robust” analysis by fitting regression models in the weighted matched dataset and also controlling for the observed covariates. Controlling for our observed covariates in the final analytic models helps to further adjust for any remaining differences that existed between study groups after matching (Ho, 2007). We used linear regression for the weight loss outcomes as these outcomes were normally distributed. For the two binary outcomes (return to pre-pregnancy BMI category and return to pre-pregnancy weight), we used logistic regression and then derived predicted probabilities from those results.
To account for loss to follow-up during the study, we conducted analyses including women with complete outcomes data and using multiply imputed outcomes. Results from the complete case and multiple imputation models were consistent in terms of direction, magnitude, and significance; therefore, we present results from the complete case analyses. (See Appendix for imputation model details and results using imputed outcomes).
Results
Baseline characteristics of the study samples are summarized in Table 1. The proportion of women who were overweight or obese increased from 50% pre-pregnancy to 56% at 12 months postpartum, and a plurality of women (46%) gained more weight during pregnancy than recommended by the Institute of Medicine guidelines (Rasmussen et al., 2009). For each of the two breastfeeding definitions (exclusive and non-exclusive breastfeeding for at least 3 months), the breastfeeding and matched control groups were highly comparable on the observed covariates.
Table 1. Characteristics of U.S. women in the two the study samples at baseline, 2005-2007.
| Sample for exclusive breastfeeding analysesa (N=2,102) |
Sample for non-exclusive breastfeeding analysesb (N=1,305) |
|||
|---|---|---|---|---|
|
|
||||
| Exclusive breastfeeding (N=797) |
Non-exclusive or no breastfeeding (N=1,305) |
Non-exclusive breastfeeding (N=521) |
No breastfeeding (N=784) |
|
| Baseline weight characteristics | ||||
| Pre-pregnancy Body Mass Index | ||||
| Underweight (<18.5 kg/m2) | 2.8 (1.5,4.0) | 2.0 (1.2,2.9) | 2.8 (1.6,4.4) | 2.4 (1.1,3.7) |
| Healthy weight (18.5-24.9 kg/m2) | 46.4 (42.7,50.2) | 44.0 (41.0,47.1) | 39.7 (34.9,44.6) | 38.4 (34.2,42.6) |
| Overweight (25-29.9 kg/m2) | 28.6 (25.2,31.9) | 29.5 (26.7,32.2) | 28.3 (23.9,32.8) | 33.4 (29.4,37.5) |
| Obese (≥30 kg/m2) | 22.3 (19.1,25.4) | 24.5 (21.9,27.1) | 29.1 (24.6,33.6) | 25.8 (22.0,29.6) |
| Weight gain during pregnancy | ||||
| Gained≤IOM guidelinesc | 13.3 (10.9,15.6) | 15.6 (13.6,17.5) | 18.7 (15.3,22.1) | 14.4 (11.9,16.9) |
| Gained within IOM guidelinesc | 42.0 (38.5, 45.4) | 41.7 (39.0,44.4) | 36.0 (31.8,40.2) | 37.2 (33.7,40.6) |
| Gained>IOM guidelinesc | 44.8 (41.3,48.3) | 42.7 (40.0,45.4) | 45.3 (40.9,49.6) | 48.4 (44.9,52.0) |
| Other matching variables | ||||
| Demographic characteristics | ||||
| Mean age, years | 30.0 (29.7,30.3) | 29.7 (29.5,30.0) | 29.7 (29.3,30.2) | 29.8 (29.4,30.2) |
| Race | ||||
| White | 90.5 (88.4,92.5) | 89.6 (88.0,91.3) | 80.4 (77.0,83.8) | 80.3 (77.5,83.1) |
| Black | 1.8 (1.0,2.7) | 2.0 (1.3,2.8) | 5.2 (3.2,7.1) | 4.9 (3.4,6.4) |
| Hispanic | 4.1 (3.0,5.2) | 4.1 (3.0,5.2) | 7.7 (5.4,10.0) | 8.8 (6.8,10.8) |
| Other/multiple races | 3.9 (2.5,5.2) | 4.2 (3.1,5.3) | 6.7 (4.6,8.9) | 6.0 (4.3,7.6) |
| Education | ||||
| ≤High school diploma | 11.3 (9.1,13.5) | 10.2 (8.5,11.8) | 15.7 (12.6,18.9) | 15.2 (12.7,17.7) |
| Some college | 33.8 (30.5,37.0) | 32.3 (29.8,34.9) | 39.9 (35.7,44.1) | 42.9 |
| College degree or higher | 55.0 (51.5,58.4) | 57.5 (54.8,60.2) | 44.3 (40.1,48.6) | (39.4,46.4) 41.9 (38.4,45.4) |
| Infant enrolled in WICd | 5.3 (3.7,6.8) | 5.9 (4.7,7.2) | 14.4 (11.4,17.4) | 15.8 (13.2,18.4) |
| At least one previous live birth | 76.9 (74.0,79.8) | 74.3 (71.9,76.6) | 72.0 (68.1,75.8) | 68.0 (64.7,71.3) |
| Health/Medical characteristics | ||||
| Insured during prenatal care | 95.2 (93.4,96.7) | 95.2 (94.1,96.4) | 96.0 (94.3,97.7) | 97.4 (96.3,98.5) |
| Smoked postpartume | 3.8 (2.4,5.1) | 4.6 (3.4,5.6) | 9.6 (7.1,12.1) | 9.5 (7.4,11.6) |
| C-section birth | 24.7 (21.7,27.7) | 26.2 (23.9,28.6) | 27.8 (24.0,31.7) | 24.4 |
| Infant in the NICUf | 2.0 (1.0,3.0) | 1.7 (1.0,2.5) | 3.8 (2.2,5.5) | (21.4,27.5) 2.9 (1.7,4.1) |
| Breastfeeding support | ||||
| Pediatrician recommended breastfeedingg | 59.8 (56.4,63.3) | 59.4 (56.7,62.0) | 49.9 (45.6,54.2) | 48.4 (44.9,51.9) |
| Intended to breastfeedh | 89.7 (87.6,91.8) | 91.4 (89.8,92.9) | 69.5 (65.5,73.4) | 71.8 (68.7,75.0) |
Exclusive breastfeeding defined as feeding an infant breast milk exclusively for at least three months. Matched control group defined as exclusive or non-exclusive feeding of breast milk less than three months or never breastfeeding.
Non-exclusive breastfeeding defined as feeding an infant breast milk non-exclusively for at least three months. Matched control group defined as feeding an infant any breast milk less than three months or never breastfeeding.
a Institute of Medicine (IOM) guidelines recommend gestational weight gain of 28-40 pounds for women with pre-pregnancy BMI<18.5 kg/m2; 25-35 pounds for women who have pre-pregnancy BMI of 18.5-24.9 kg/m2; 15-25 pounds for women with pre-pregnancy BMI of 25-29.9 kg/m2; and 11-20 pounds for women with pre-pregnancy BMI≥30 kg/m2.
The infant was enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) one month after delivery.
Smoking was defined as reporting smoking any amount of cigarettes each day at three months postpartum.
The infant was in an intensive care unit for three days or less after delivery.
Women reported one month after delivery that their infant's pediatrician recommended exclusive breastfeeding of the infant.
Women reported during their third trimester of pregnancy that they intended to breastfeed their infant exclusively for the first few weeks.
Effects of breastfeeding on postpartum weight loss
Exclusive breastfeeding for at least 3 months had a small but significant effect on postpartum weight loss at 6 months postpartum and beyond (Figure 1, Panel A). Women who breastfed exclusively for at least 3 months had a 1.3-pound (0.59 kg) (95% CI: 0.2,2.5 pounds, p<0.05) greater weight loss at 6 months postpartum, relative to those who did not breastfed or breastfed non-exclusively. At 9 months postpartum, exclusive breastfeeding for at least 3 months led to a 3.7-pound (1.68 kg) (95% CI: 2.3,5.2 pounds, p<0.01) greater postpartum weight loss, relative to non-exclusive or no breastfeeding (Table 2). Similarly, at 12 months postpartum, exclusive breastfeeding for at least 3 months led to a 3.2-pound (1.45 kg) (95% CI: 1.7,4.7 pounds, p<0.05) greater postpartum weight loss, relative to non-exclusive or no breastfeeding (Table 2). These results translate into a 2.7-percentage-point greater weight loss at 12 months among women who exclusively breastfed for 3 months, relative to women who did not breastfeed or breastfed non-exclusively.
Figure 1. Effects of exclusive and non-exclusive breastfeeding for three months on weight loss during the 12 months postpartum among U.S. women, 2005-2007.
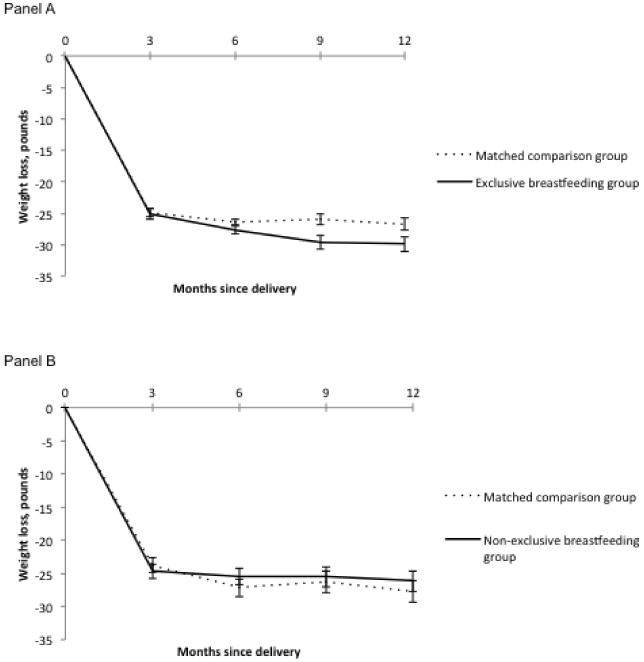
Notes: Exclusive breastfeeding defined as feeding an infant breast milk exclusively for at least three months. Matched control group defined as exclusive or non-exclusive feeding of breast milk less than three months or never breastfeeding. Non-exclusive breastfeeding defined as feeding an infant breast milk non-exclusively for at least three months. Matched control group defined as feeding an infant any breast milk less than three months or never breastfeeding. Doubly robust analyses adjusted for matching covariates shown in Table 2. One pound=0.45 kilogram.
Table 2. Effects of exclusive and non-exclusive breastfeeding for three months on postpartum weight loss, the probability of returning to pre-pregnancy Body Mass Index (BMI) category, and the probability of returning to pre-pregnancy weight during the 12 months postpartum among U.S. women, 2005-2007.
| Outcome | Exclusive breastfeedinga | Non-exclusive or no breastfeeding | Non-exclusive breastfeedingb | No breastfeeding |
|---|---|---|---|---|
| Poundsc (95% CI) | Poundsc (95% CI) | |||
|
|
||||
| 3 month postpartum weight loss | 25.2 (24.3,26.0) | 24.9 (24.3,25.5) | 24.6 (23.5,25.8) | 23.8 (22.9,24.7) |
| 6 month postpartum weight loss | 27.6 (27.7,28.6)* | 26.5 (25.7,27.2)* | 25.4 (24.0,26.7) | 27.1 (26.0,28.3) |
| 9 month postpartum weight loss | 29.6 (28.5,30.7)** | 25.9 (25.0,26.8)** | 25.4 (23.7,27.0) | 26.3 (25.0,27.7) |
| 12 month postpartum weight loss | 29.9 (28.8,31.1)* | 26.7 (25.8,27.7)* | 26.1 (24.5,27.8) | 27.8 (26.4,29.2) |
|
|
||||
| Percentage (95% CI) | Percentage (95% CI) | |||
|
|
||||
| Return to pre-pregnancy BMI categoryd,e | 87.6 (84.9,90.3)** | 81.6 (79.1,84.1)** | 83.9 (80.1,87.8) | 84.0 (80.8,87.2) |
| Return to pre-pregnancy weightd,f | 51.8 (47.8,55.9)* | 45.7 (42.5,47.7)* | 43.0 (37.9,48.0) | 44.0 (39.7,48.3) |
Two groups statistically different, p<0.05
Two groups statistically different, p<0.01
Exclusive breastfeeding defined as feeding an infant breast milk exclusively for at least three months. Matched control group defined as exclusive or non-exclusive feeding of breast milk less than three months or never breastfeeding.
Non-exclusive breastfeeding defined as feeding an infant breast milk non-exclusively for at least three months. Matched control group defined as feeding an infant any breast milk less than three months or never breastfeeding.
One pound=0.45 kilogram.
Excluding women who were underweight (had a BMI<18.5 kg/m2) pre-pregnancy.
Defined as having a greater BMI category 12 months postpartum relative to pre-pregnancy BMI category.
Defined as weight at 12 months postpartum≤pre-pregnancy weight.
Women who breastfed non-exclusively for at least 3 months did not experience significantly greater weight loss during the 12 months postpartum relative to women who did not breastfeed or breastfed non-exclusively for less than 3 months (Figure 1, Panel B; and Table 2). The magnitude of postpartum weight loss appeared to be smaller in non-exclusively breastfeeding women relative to women who did not breastfeed or breastfed for less then three months Figure 1, Panel B); however, differences between groups were not statistically different and were quite small in magnitude (<1.9 pounds/0.86 kg).
Effects of breastfeeding on return to pre-pregnancy BMI and pre-pregnancy weight
Women who breastfed exclusively for at least 3 months had a 6.0 percentage-point increase (95% CI: 2.3,9.7; p<0.01) in the probability of returning to pre-pregnancy BMI category relative to women who did not breastfeed or breastfed non-exclusively (Table 2). Likewise, women who breastfed exclusively for at least 3 months had a 6.1 percentage-point increase (95% CI: 1.0,11.3; p<0.05) in the probability of returning to pre-pregnancy weight or lower compared to those women who did not breastfeed or breastfed non-exclusively. Consistent with our findings of effects postpartum weight loss, non-exclusive breastfeeding for at least 3 months did not lead to increased probabilities of returning to pre-pregnancy BMI category or pre-pregnancy weight, compared with non-exclusive breastfeeding for less than three months or no breastfeeding (Table 2).
Discussion
This study found that exclusive breastfeeding in the first 3 months postpartum led to a 2.7 percentage-point greater weight loss at 12 months postpartum, relative to not breastfeeding or breastfeeding non-exclusively, among U.S. women. Exclusive breastfeeding increased the probability of returning to pre-pregnancy BMI category and pre-pregnancy weight by about 6 percentage points, relative to no breastfeeding or breastfeeding non-exclusively. In contrast, non-exclusive breastfeeding for at least 3 months did not significantly impact weight loss or weight maintenance. These findings inform efforts to optimize the typical U.S. maternity leave period by providing new evidence of a maternal health benefit of breastfeeding during this window.
Our results were consistent with previous experimental studies in a low-income country (Dewey et al., 2001), suggesting that breastfeeding may lead to greater postpartum weight loss due to increased energy expenditures or hormonal changes. Contrary to expectations, we did not observe any effects of non-exclusive breastfeeding for at least 3 months on postpartum weight loss. These null findings might be due to variation in the intensity of breastfeeding among women who were non-exclusively breastfeeding. Although the increase in postpartum weight loss due to breastfeeding we observed was below the 5%-10% threshold typically used to gauge clinically meaningful weight loss (Moyer, 2012), it is notable that our estimate of weight loss at 12 months postpartum due to exclusive breastfeeding for 3 months exceeds effects observed in a trial of a postpartum weight loss intervention in the U.S. (Ostbye et al., 2009). Because of the small number of women who breastfed exclusively for 6 months, we were not able to conduct an analysis examining the effects of breastfeeding as recommended by the AAP on postpartum weight loss, although future research is needed on this question.
This is the first study to our knowledge to employ propensity score matching to estimate the effect of breastfeeding on postpartum weight loss in a national cohort of U.S. women. Our methods provide advantages over traditional multivariable regression adjustment in that balance was achieved between the breastfeeding and matched comparison groups on a range of covariates, and the matching was conducted in the absence of information about outcomes. A potential limitation in our ability to estimate effects is that there may still be unobserved confounding variables. We have attempted to minimize the likelihood of an unobserved confounder affecting our results by including a range of observed, known confounders in our matching models. We also conducted a sensitivity analysis using bias formulas proposed by Vanderweele and Arah to estimate the “true” results adjusted for a possible unmeasured confounder (Vanderweele and Arah, 2011). Assuming the unmeasured confounder doubled the odds of exclusive breastfeeding for 3 months, we found that our results we robust to confounding with a prevalence of the unmeasured confounder up to three times greater in the exclusive breastfeeding versus matched comparison group (see Appendix for full results).
Several additional limitations to this study should be noted. First, all measures of maternal weight were self-reported, which tends to underestimate weight (Merrill and Richardson, 2009). However, we would not expect under-reporting weight to be differential by study groups or over time. Second, our data are not nationally representative, so results might not be generalizable to the entire population. Third, a substantial proportion of women were lost to follow-up, which resulted in missing outcomes data. We aimed to minimize this limitation by running both complete case analyses and analyses in which the outcomes were imputed, and our findings were consistent using these two approaches. Finally, women were followed for 12 months postpartum, so we were not able to examine longer-term effects of breastfeeding.
Conclusion
Even in the span of a 12-week leave period, exclusive breastfeeding has a small effect on weight loss among U.S. women, which is an important maternal health benefit that should be communicated as part of efforts to promote breastfeeding.
Supplementary Material
Highlights.
It is unclear whether breastfeeding leads to increased postpartum weight loss.
We estimate effects of breastfeeding for 3 months on postpartum weight loss.
Exclusive breastfeeding led to a small increase in postpartum weight loss.
Non-exclusive breastfeeding did not significantly affect postpartum weight loss.
Acknowledgments
Funding Source: This research was supported by a grant from the National Heart, Lung, and Blood Institute of the National Institute of Health (5K01HL096409).
Footnotes
Conflict of Interest: The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Academy of Pediatrics. Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827–41. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- Amorim AR, Rossner S, Neovius M, Lourenco PM, Linne Y. Does excess pregnancy weight gain constitute a major risk for increasing long-term BMI? Obesity. 2007;15:1278–86. doi: 10.1038/oby.2007.149. [DOI] [PubMed] [Google Scholar]
- Baker JL, Gamborg M, Heitmann BL, Lissner L, Sorensen TI, Rasmussen KM. Breastfeeding reduces postpartum weight retention. The American journal of clinical nutrition. 2008;88:1543–51. doi: 10.3945/ajcn.2008.26379. [DOI] [PubMed] [Google Scholar]
- Brewer MM, Bates MR, Vannoy LP. Postpartum changes in maternal weight and body fat depots in lactating vs nonlactating women. The American journal of clinical nutrition. 1989;49:259–65. doi: 10.1093/ajcn/49.2.259. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Breastfeeding Report Card: United States, 2014. Atlanta: 2014. [Accessed August 2 2014]. Online. [Google Scholar]
- Centers for Disease Control and Prevention. Vital signs: state-specific obesity prevalence among adults --- United States, 2009. MMWR Morbidity and mortality weekly report. 2010;59:951–5. [PubMed] [Google Scholar]
- Chung M, Raman G, Trikalinos T, Lau J, Ip S. Interventions in primary care to promote breastfeeding: an evidence review for the U.S. Preventive Services Task Force. Annals of internal medicine. 2008;149:565–82. doi: 10.7326/0003-4819-149-8-200810210-00009. [DOI] [PubMed] [Google Scholar]
- Cogswell ME, Perry GS, Schieve LA, Dietz WH. Obesity in women of childbearing age: risks, prevention, and treatment. Primary care update for Ob/Gyns. 2001;8:89–105. doi: 10.1016/s1068-607x(00)00087-1. [DOI] [PubMed] [Google Scholar]
- Dehejia R, Wahba S. Propensity score matching methods for nonexperimental causal studies. The Review of Economics and Statistics. 2002;84:151–161. [Google Scholar]
- Dewey KG. Energy and protein requirements during lactation. Annual review of nutrition. 1997;17:19–36. doi: 10.1146/annurev.nutr.17.1.19. [DOI] [PubMed] [Google Scholar]
- Dewey KG, Cohen RJ, Brown KH, Rivera LL. Effects of exclusive breastfeeding for four versus six months on maternal nutritional status and infant motor development: results of two randomized trials in Honduras. The Journal of nutrition. 2001;131:262–7. doi: 10.1093/jn/131.2.262. [DOI] [PubMed] [Google Scholar]
- Fein SB, Labiner-Wolfe J, Shealy KR, Li R, Chen J, Grummer-Strawn LM. Infant Feeding Practices Study II: study methods. Pediatrics. 2008;122 Suppl 2:S28–35. doi: 10.1542/peds.2008-1315c. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA: the journal of the American Medical Association. 2012;307:491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- Gould Rothberg BE, Magriples U, Kershaw TS, Rising SS, Ickovics JR. Gestational weight gain and subsequent postpartum weight loss among young, low-income, ethnic minority women. American journal of obstetrics and gynecology. 2011;204:52 e1–11. doi: 10.1016/j.ajog.2010.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho DE, Imai K, King G, Stuart EA. Matching as Nonparametric Preprocessing for Reducing Model Dependence in Parametric Causal Inference. Political Analysis. 2007;15:199–236. [Google Scholar]
- Hu FB. Overweight and obesity in women: health risks and consequences. Journal of women's health. 2003;12:163–72. doi: 10.1089/154099903321576565. [DOI] [PubMed] [Google Scholar]
- Ip S, Chung M, Raman G, Chew P, Magula N, Devine D, Trikalinos T, Lau J. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep) 2007:1–186. [PMC free article] [PubMed] [Google Scholar]
- Janney CA, Zhang D, Sowers M. Lactation and weight retention. The American journal of clinical nutrition. 1997;66:1116–24. doi: 10.1093/ajcn/66.5.1116. [DOI] [PubMed] [Google Scholar]
- Krause KM, Lovelady CA, Peterson BL, Chowdhury N, Ostbye T. Effect of breast-feeding on weight retention at 3 and 6 months postpartum: data from the North Carolina WIC Programme. Public health nutrition. 2010;13:2019–26. doi: 10.1017/S1368980010001503. [DOI] [PubMed] [Google Scholar]
- Labarere J, Gelbert-Baudino N, Ayral AS, Duc C, Berchotteau M, Bouchon N, Schelstraete C, Vittoz JP, Francois P, Pons JC. Efficacy of breastfeeding support provided by trained clinicians during an early, routine, preventive visit: a prospective, randomized, open trial of 226 mother-infant pairs. Pediatrics. 2005;115:e139–46. doi: 10.1542/peds.2004-1362. [DOI] [PubMed] [Google Scholar]
- Lipsky LM, Strawderman MS, Olson CM. Maternal weight change between 1 and 2 years postpartum: the importance of 1 year weight retention. Obesity. 2012;20:1496–502. doi: 10.1038/oby.2012.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Smith MG, Dobre MA, Ferguson JE. Maternal obesity and breast-feeding practices among white and black women. Obesity. 2010;18:175–82. doi: 10.1038/oby.2009.182. [DOI] [PubMed] [Google Scholar]
- Merrill RM, Richardson JS. Validity of self-reported height, weight, and body mass index: findings from the National Health and Nutrition Examination Survey, 2001-2006. Preventing chronic disease. 2009;6:A121. [PMC free article] [PubMed] [Google Scholar]
- Moyer VA. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Annals of internal medicine. 2012;157:373–8. doi: 10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- Neville CE, Mckinley MC, Holmes VA, Spence D, Woodside JV. The relationship between breastfeeding and postpartum weight change-a systematic review and critical evaluation. International journal of obesity. 2013 doi: 10.1038/ijo.2013.132. [DOI] [PubMed] [Google Scholar]
- Ostbye T, Krause KM, Lovelady CA, Morey MC, Bastian LA, Peterson BL, Swamy GK, Brouwer RJ, McBride CM. Active Mothers Postpartum: a randomized controlled weight-loss intervention trial. American journal of preventive medicine. 2009;37:173–80. doi: 10.1016/j.amepre.2009.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostbye T, Peterson BL, Krause KM, Swamy GK, Lovelady CA. Predictors of postpartum weight change among overweight and obese women: results from the Active Mothers Postpartum study. Journal of women's health. 2012;21:215–22. doi: 10.1089/jwh.2011.2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen KM, Yaktine AL Institute of Medicine (U.S.). Committee to Reexamine IOM Pregnancy Weight Guidelines. Weight gain during pregnancy : reexamining the guidelines. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- Rooney BL, Schauberger CW. Excess pregnancy weight gain and long-term obesity: one decade later. Obstetrics and gynecology. 2002;100:245–52. doi: 10.1016/s0029-7844(02)02125-7. [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- Rubin DB. The design versus the analysis of observational studies for causal effects: parallels with the design of randomized trials. Statistics in medicine. 2007;26:20–36. doi: 10.1002/sim.2739. [DOI] [PubMed] [Google Scholar]
- Scanlon KS, Grummer-Strawn L, Li R, Molinari N, Perrine CG. Racial and ethnic differences in breastfeeding initiation and duration, by state - National Immunization Survey, United States, 2004-2008. MMWR Morb Mortal Wkly Rep. 2010;59:327–34. [PubMed] [Google Scholar]
- Scott JA, Binns CW, Oddy WH, Graham KI. Predictors of breastfeeding duration: evidence from a cohort study. Pediatrics. 2006;117:e646–55. doi: 10.1542/peds.2005-1991. [DOI] [PubMed] [Google Scholar]
- Stuart EA. Matching methods for causal inference: A review and a look forward. Statistical science : a review journal of the Institute of Mathematical Statistics. 2010;25:1–21. doi: 10.1214/09-STS313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart EA, Green KM. Using full matching to estimate causal effects in nonexperimental studies: examining the relationship between adolescent marijuana use and adult outcomes. Developmental psychology. 2008;44:395–406. doi: 10.1037/0012-1649.44.2.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuebe AM, Rich-Edwards JW. The reset hypothesis: lactation and maternal metabolism. American journal of perinatology. 2009;26:81–8. doi: 10.1055/s-0028-1103034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanderweele TJ, Arah OA. Bias formulas for sensitivity analysis of unmeasured confounding for general outcomes, treatments, and confounders. Epidemiology. 2011;22:42–52. doi: 10.1097/EDE.0b013e3181f74493. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


