Abstract
Objective
To characterize the process of end-of-career attrition among primary care physicians.
Design
Longitudinal, open cohort, population-based study of primary care physicians using health administrative data from ICES.
Setting Ontario.
Participants
All family physicians providing comprehensive care between 1992 and 2013.
Main outcome measures
Changes in workload and scopes of practice over time.
Results
The cohort included 15 552 family physicians who provided comprehensive care at some point during the study period. Physicians reduced workloads and narrowed scopes of practice in advance of full retirement at an average age of 70.5 (95% CI 70.1 to 70.8) years. Female physicians provided fewer clinical services than male physicians did and retired 5 years earlier. Canadian medical graduates provided fewer clinical services and retired 2 years earlier than international medical graduates did. Up to 60% of physicians stopped providing comprehensive primary care before retirement, continuing with other clinical activities, at reduced workloads, for an average of 3 years before retiring fully.
Conclusion
End-of-career practice patterns are characterized by gradual, modest changes in the provision of services rather than abrupt declines, and the retirement process unfolds differently for different physicians. This study highlights the importance of considering physician workload, scope of practice, and demographic factors for more accurate prediction of physician retirement trends and effective work force planning.
Résumé
Objectif
Déterminer le processus de départ à la retraite chez les médecins des soins primaires.
Type d’étude
Une étude démographique longitudinale de cohorte ouverte, effectuée à l’aide des données sanitaires administratives de l’ICES et portant sur des médecins de soins primaires.
Contexte
L’Ontario.
Participants
Tous les médecins de famille qui ont prodigué des soins complets entre 1992 et 2013.
Principaux paramètres à l’étude
Les changements de la charge de travail et du champ de pratique au fil du temps.
Résultats
La cohorte comprenait 15 552 médecins de famille qui prodiguaient des soins complets à certains stades de l’étude. Ces médecins réduisaient leur charge de travail et diminuaient leur champ de pratique en prévision d’une retraite complète prise en moyenne à 70,5 ans (IC à 95 % 70,1 à 70,8). Les femmes offraient moins de services cliniques que les hommes et prenaient leur retraite cinq ans plus tôt. Ceux qui avaient obtenu leur diplôme en médecine au Canada offraient moins de services cliniques et prenaient leur retraite 2 ans plus tôt que ceux qui l’avaient obtenu à l’étranger. Jusqu’à 60 % des médecins cessaient d’offrir des soins complets avant leur retraite, poursuivant d’autres activités cliniques, avec une charge de travail allégée, durant une période moyenne de 3 ans précédant leur retraite complète.
Conclusion
Les modèles de gestion de fin de carrière se caractérisent par des changements modestes et graduels dans la dispensation des soins plutôt que par une diminution brusque; de plus, le processus conduisant à la retraite s’effectue différemment selon les médecins. Cette étude souligne l’importance de tenir compte de la charge de travail des médecins, de leur champ de pratique et des facteurs démographiques afin de mieux prédire les tendances qui caractérisent la prise de retraite chez les médecins et pour s’assurer de disposer d’une force de travail suffisante pour répondre aux besoins futurs.
Understanding attrition through retirement is becoming imperative. Although inputs to the physician work force are well understood, egress from the work force has been less well studied. Estimating attrition from the physician work force has proven to be difficult for a variety of reasons, including unreliability of physicians’ self-reported retirement intentions,1 lack of systematic collection of end-of-career physician information,2 and a multiplicity of definitions of retirement.3 While retirement has typically been considered a categorical end point, evidence is mounting that it is a process that workers go through at the ends of their careers4–6 and that physicians are no exception.7 Although most physician work force planning models incorporate estimates of outflow from the work force, the degree of sophistication in modeling retirement patterns varies,8 and most developed countries struggle to accurately predict physician retirement trends. As a result, the supply of physician services rarely aligns with the population demand for these services, and most health systems experience alternating surpluses and shortages of physicians.
Because primary care physicians have broad scopes of practice and deliver care in a variety of settings, they might have more work options available to them at the ends of their careers and might demonstrate distinct retirement patterns. The objective of this study was to characterize the process of physician attrition from the primary care work force by answering the following questions: How do physicians change their practice patterns as they age? What factors influence changing physician practice patterns?
METHODS
This longitudinal, population-based, open cohort study used health administrative data from ICES in Ontario. Demographic characteristics and practice-related data for family physicians were extracted from 6 linked databases for the period between 1992 and 2013: the ICES Physician Database, the Corporate Provider Database, the Ontario Health Insurance Plan (OHIP) Claims Database, the Client Agency Program Enrolment database, the AVGPRICE database, and the CONTACT database. These data sets were linked using unique encoded identifiers and analyzed at ICES. Analyses were conducted using SAS Enterprise Guide 6.1. This study was approved by the institutional review board at Sunnybrook Health Sciences Centre in Toronto, Ont, and by the University of Ottawa Research Ethics Board.
Cohort creation
We included all physicians from the ICES primary care pool (physicians with self-reported or functional specialties of family or general practice) who provided comprehensive primary care services covered by OHIP at any time between 1992 and 2013 in the cohort. Once included, physicians remained in the cohort until the end of the study period. The only physicians excluded from the analyses were those who did not provide comprehensive primary care at any time during the study period.
An algorithm developed at ICES was used to assess physicians’ provision of comprehensive care.9 In order to be considered to have provided comprehensive care in a given year, physicians must have worked at least 44 days that year and billed at least once in at least 7 of 22 activity areas associated with primary care provision (ie, mini or minor assessments, general assessments or reassessments, intermediate assessments, periodic health examinations, geriatric care, mental health or addiction services, hospital care, home visits, chronic care or long-term care, emergency department or equivalent services, vision care, palliative care, flu shots, other immunizations, office laboratory procedures, allergy shots, other injections, Papanicolaou tests, anticoagulant therapy, preoperative assessments, diabetes management, and smoking cessation).
For each physician, we captured information on demographic characteristics, including year of birth, sex, and location of training (the country in which the physician’s medical school was located). In each year, we characterized the rurality of the location of the physician’s practice using the 2008 Rurality Index of Ontario, and the physician’s remuneration model (ie, traditional fee-for-service [FFS], reformed-FFS, capitation, capitation and family health team, community health centre, or other). Table 1 provides descriptions of these models.
Table 1.
Physician remuneration models
| REMUNERATION MODEL | DESCRIPTION |
|---|---|
| FFS | Physicians are compensated by the government for each service rendered |
| Reformed-FFS | Physicians receive a base payment that covers certain services and they bill FFS for other services |
| Capitation | Physicians receive a set fee for each patient on their roster. The fee might be adjusted by age, sex, or morbidity |
| Capitation and family health team | Physicians receive a set fee for each patient, as well as funding to work together with other professionals to provide primary health care for a community |
| Community health centre | Physicians are compensated by salary, often based on units of time |
| Other | This category includes 10 separate and relatively uncommon remuneration models |
FFS—fee for service.
Definition of retirement
We considered physicians to be retired in the year after they were last active, when no billings were generated in that year or in any future years.
Trends for analysis
Trends for analysis included physician workload, retirement age, and practice patterns.
Workload.
Physicians’ annual workload was determined with the following 5 outcome measures: annual OHIP payments, full-time equivalents (FTEs),10 service volume (ie, number of visits), number of days worked, and panel size. (For further description of the workload outcome measures, contact the corresponding author [S.S.]). Stratified analyses of workload by sex, location of training, location of practice, and remuneration model were conducted.
Retirement age.
Our initial analyses showed that attrition from practice occurs across the age spectrum, and that the frequency distribution of attrition is bimodal, with a peak in the early years of practice, the nadir around age 55, and another peak in later years. An aging physician work force lends urgency to the effort to understand attrition patterns of older physicians, and so we chose to focus on physicians in the older age group (aged ≥ 55). We calculated the average age at which these physicians reached retirement. Average retirement ages were compared for statistically significant differences related to sex and location of training using Student t tests, and related to location of practice using ANOVA (analysis of variance).
Practice patterns.
First, we examined physicians’ workloads in each of the 10 years before they retired. Next, we examined relative changes in physicians’ scopes of practice—the clinical activities that physicians engage in—in the years before retirement. In addition to office-based comprehensive care, we examined physicians’ participation in anesthesia, emergency department care, inpatient care, home visits, mental health services, nursing home care, obstetrics, on-call anesthesia or surgical assisting, palliative care, and surgical assisting. Table 2 presents service thresholds necessary for characterizing participation in a clinical activity.
Table 2.
Annual service thresholds (billings or service counts) necessary for being characterized as participating in a given clinical activity
| CLINICAL ACTIVITY | SERVICE THRESHOLDS |
|---|---|
| Billing activity, $ | |
| • Anesthesia | > 1000 |
| Service counts activity | |
| • Emergency department | > 50 |
| • Inpatient | > 50 |
| • Home visits | > 10 |
| • Mental health services | > 50 |
| • Nursing home | > 50 |
| • Obstetrics | > 2 |
| • On-call anesthesia or assisting | ≥ 1 |
| • Palliative care | > 10 |
| • Surgical assisting | > 12 |
Finally, we examined the temporal relationship between stopping comprehensive care and retirement, identifying one group of physicians who stopped providing comprehensive care because they retired, and another group of physicians who continued to practise after they stopped providing comprehensive care. We compared the workloads of these 2 groups of physicians, and we looked forward in time to see which clinical activities the latter group of physicians engaged in instead of providing comprehensive care.
RESULTS
We identified 21 240 family physicians, 5688 of whom did not provide comprehensive primary care at any time during the study period and were excluded from the analyses. The study work force cohort included the remaining 15 552 physicians.
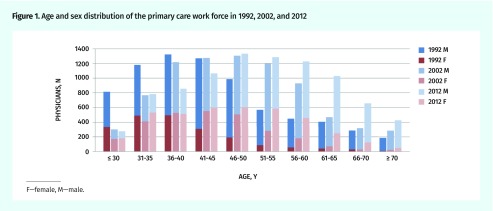
The primary care work force in 1992 was relatively young and male dominated. Over the study period, the primary care work force grew older and included more women (Figure 1).
Figure 1.
Age and sex distribution of the primary care work force in 1992, 2002, and 2012
F—female, M—male.
Results of the trends analysis of physician workload, retirement age, and practice patterns were as follows.
Workload.
Physicians’ workloads generally increase throughout their careers, sharply at first and then more gently, before declining (Figure 2). Physicians begin to reduce their workloads (the slopes of the age-activity curves shift from positive to negative) between the ages of 55 and 61. These patterns are consistent across the 5 workload outcome measures that we examined.
Figure 2.
Average annual workload, by age: Error bars indicate 95% CIs. Workload outcome measures included A) OHIP payments, B) FTEs, C) service volume (ie, number of visits), D) number of days worked, and E) panel size.
FTE—full-time equivalents, OHIP—Ontario Health Insurance Plan.
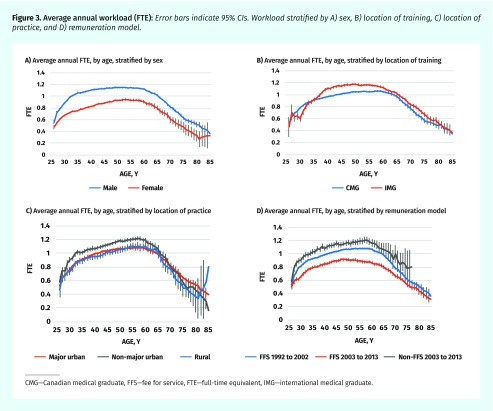
Stratified analyses, shown in Figure 3, revealed differences in workload (as measured by average annual FTE) related to sex, location of training, location of practice, and model of remuneration. On average, workloads of female physicians are smaller than those of male physicians throughout their careers. International medical graduates have larger workloads than Canadian medical graduates for most of their careers. Physicians with practices in non-major urban locations have larger workloads than their colleagues with practices in major urban and rural locations until they are in their late 60s, at which point the workload differences become less pronounced. Physicians working in practices with non–fee-for-service (FFS) remuneration (reformed-FFS, capitation and family health team settings) have larger workloads than their FFS colleagues do. These patterns are also consistent across the 5 measures of workload.
Figure 3.
Average annual workload (FTE): Error bars indicate 95% CIs. Workload stratified by A) sex, B) location of training, C) location of practice, and D) remuneration model.
CMG—Canadian medical graduate, FFS—fee for service, FTE—full-time equivalent, IMG—international medical graduate.
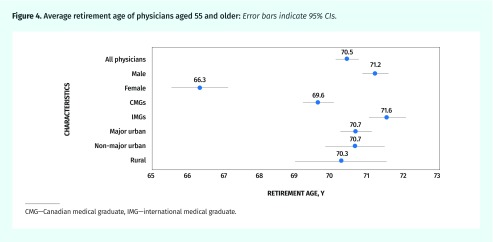
Retirement age.
As noted above, we limited this analysis to physicians aged 55 years and older (Figure 4). The average retirement age is 70.5 (95% CI 70.1 to 70.8). On average, female physicians retire approximately 5 years earlier than male physicians do (P < .05), and Canadian-trained physicians retire 2 years earlier than international medical graduates do (P < .05). The location of practice—major urban, non-major urban, or rural—did not significantly influence retirement age (P < .05). Average retirement ages were stable over time, with no trend toward retirement at older or younger ages between 1992 and 2013.
Figure 4.
Average retirement age of physicians aged 55 and older: Error bars indicate 95% CIs.
CMG—Canadian medical graduate, IMG—international medical graduate.
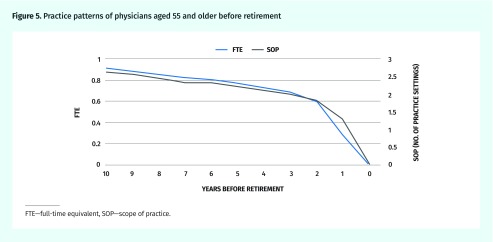
Practice patterns.
We examined the practice patterns of 2142 physicians (aged ≥ 55) who retired during the study period. In the 10 years before retirement, these physicians gradually reduced their workloads and narrowed their scopes of practice (Figure 5). The rate of change in workload is quite uniform until the year immediately preceding retirement. The sudden drop in workload is likely seen because the final year of work for most physicians is a partial one.
Figure 5.
Practice patterns of physicians aged 55 and older before retirement
FTE—full-time equivalent, SOP—scope of practice.
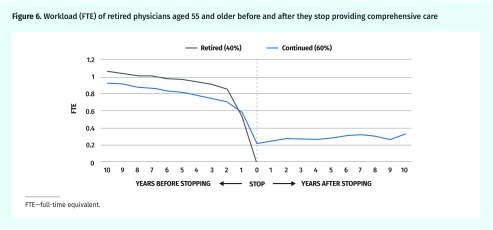
To explore the relationship between workload and scope of practice in advance of retirement, we examined the workloads of retired physicians before and after they stopped providing comprehensive primary care (Figure 6). Approximately 40% of physicians (seen in black) stop providing comprehensive care at the time of retirement. These physicians have higher average FTEs in the years before retirement than the physicians who continue to provide clinical services do. Most physicians continue to practice after they stop providing comprehensive care, working with reduced workloads for an average of 3 years before full retirement. Factors such as sex, location of training, and location of practice did not influence how long physicians continue to work after they stop providing comprehensive care and before they retire; physicians in each group retired, on average, within 6 months of one another. In general, physicians who adopt a phased approach to retirement continue to provide some of the services they did previously (such as inpatient care or surgical assisting), rather than undertaking entirely new practice activities.
Figure 6.
Workload (FTE) of retired physicians aged 55 and older before and after they stop providing comprehensive care
FTE—full-time equivalent.
DISCUSSION
Using 22 years of longitudinal health administrative data, we characterized changes in the end-of-career practice patterns of primary care physicians. We found that practice and retirement behaviour patterns were influenced by physician sex and location of training. Aging resulted in gradual, modest changes in the provision of services, rather than abrupt declines, and physicians reduced their workloads and narrowed their scopes of practice in the years leading up to retirement. Up to 60% of primary care physicians who retired stopped providing comprehensive care but remained in the work force, providing other services with reduced workloads in advance of full retirement from clinical practice.
Our observations are consistent with the findings of other studies that have reported a reduction in physician workload11 and scope of practice with age2 and differences in work force participation related to sex and generation.12,13 A recent study of retirement age of primary care providers in the United States found the median retirement age of family physicians to be 65.1 years, with female physicians retiring about 1 year earlier than their male colleagues.14 That study examined a broader spectrum of physicians’ activities, including administration, teaching, and research.
Our findings support the hypothesis that retirement is a transition rather than a sudden all-or-nothing phenomenon. Physicians reduce their workloads and narrow their scopes of practice as they approach the ends of their careers; these changes occur gradually in advance of retirement and are independent of the age at which physicians retire. The zenith of the inverted U-shaped age-activity curve occurs between ages 55 and 61; reductions in average workload seen thereafter likely represent the cumulative effects of physicians’ retirement transitions. In the context of an aging physician work force, consideration must be given to changing workloads so as not to overestimate the capacity of the work force to provide primary care services.
In the face of considerable heterogeneity in the practice patterns of family physicians, we chose to focus on the primary care work force. More than 25% of the physicians in our initial cohort did not provide comprehensive care at any time during the study period and were excluded from the analysis. We argue that these physicians did not substantially contribute to the primary care work force, having been engaged in focused practices or having consistently worked less than 44 days per year. We also used the provision of comprehensive care to track flows into and out of the primary care work force, identifying a substantial number of physicians who transition to retirement through focused practices. In so doing, we have documented important changes in how family medicine is practised over the life course, a pattern that might be seen more commonly as the work force ages.
Our study is the first to document the relationship between workload and scope of practice near the ends of physicians’ careers. In so doing, we identified that most retiring primary care physicians stop providing comprehensive care but remain in the work force with reduced workloads before full retirement. Hence, for these physicians, focused practice is a form of phased retirement. Physicians near the ends of their careers could prove to be an important source of flexibility in the work force by functioning as a work force “buffer,” with the potential to respond to changes in demand for medical care. We have found that after these physicians stop providing comprehensive primary care, they continue with activities that were previously part of their practices. However, in the context of declining comprehensiveness,15 our findings portend a work force that, while interested in maintaining participation in the work force, is potentially less able to provide service in a variety of settings. In order to foster a flexible work force, policy makers might need to provide incentives for physicians of all ages to maintain broad scopes of practice and to continue to practise in settings where future demand is anticipated, such as home visits and long-term care.
Internationally trained physicians have larger average workloads and retire 2 years later than their Canadian-trained colleagues. It seems logical that these physicians work more, and for longer, to compensate for the interruption in their practices while they have their credentials assessed before joining the Canadian work force. However, more in-depth study of international medical graduates is necessary to understand how and why location of training affects practice and retirement behaviour patterns.
The effect of the increasing number of female physicians on the service capacity of the primary care work force is not yet clear. A 2014 systematic review concluded that additional research is necessary to explore career trajectories and retirement patterns of female physicians.16 Evidence from the United States suggests that female physicians maintain higher activity rates for longer than their male colleagues, perhaps to compensate for decreased work activity during child-bearing years.17 However, we found that female primary care physicians in Ontario to date consistently have smaller workloads and retire earlier than their male colleagues do. While the results of our study bring us closer to being able to predict how much service female physicians are likely to provide at any given stage of their careers, we still lack a well-rounded understanding of how other activities these physicians engage in (such as teaching, administration, volunteer work in their profession or outside of medicine, or caregiving for children or elderly parents) affect their participation in clinical work and their retirement decisions.
Our results highlight some of the challenges inherent in predicting physician work force trends. Using retirement age in isolation to predict attrition from the work force risks underestimating or overestimating outflow, depending on whether sex and location of training are considered. Given the considerable number of primary care physicians who choose a phased approach to retirement, failure to consider the scope of practice of physicians at the ends of their careers might result in overestimation of the supply of physicians available to provide primary care services. Ideally, demographic factors, workload, and scope of practice should be considered in tandem when estimating the supply of physician services.
Limitations
Although the data we used in this study were comprehensive, spanning 22 years and including physicians practising in alternate remuneration models, information related to other factors that undoubtedly influence physicians’ retirement decisions (such as spouses and dependants) was not available. And while the use of quantitative measures to examine changes in practice patterns provides a basis for understanding the phenomenon of physician retirement, our conclusions must be informed by the limitations of these measures. For example, the health administrative data used in our study capture only clinical activity, and so we know very little about other work-related activities of family physicians. And, even 2 decades of data did not allow us to characterize differences between generations of physicians that might influence their retirement behaviour patterns. Finally, data about physicians working in community health centres and nurse practitioners providing comprehensive primary care services were not available. A comprehensive understanding of the primary care work force and its role in providing patient care services will only be achieved when complete information about all providers is available.
Conclusion and next steps
This study documented the end-of-career practice patterns of Ontario primary care physicians between 1992 and 2013 and revealed that retirement is a gradual process that unfolds differently for different physicians. For more accurate prediction of physician retirement trends and effective work force planning, our study highlights the importance of considering physician workload, scope of practice, and demographic characteristics. It also sets the stage for further research: multivariate modeling is needed to quantify the effect of various factors on workload and scope of practice. Research using qualitative methods to clarify underlying reasons for the patterns we have observed, and to explore the broader context in which retirement decisions are made, will enrich our understanding of end-of-career issues among physicians. Finally, because the issues we explored are equally relevant to the specialty physician work force, a similar study of medical and surgical specialists is necessary.
Acknowledgments
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. The opinions, results, and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario Ministry of Health and Long-Term Care is intended or should be inferred. Parts of the material in this article are based on data or information compiled and provided by the Canadian Institute for Health Information; however, the analyses, conclusions, opinions, and statements expressed herein are those of the authors and not necessarily those of the Canadian Institute for Health Information. This research was partially funded by the Bruyère Research Institute and by a grant by the Telfer School of Management Research Fund.
Editor’s key points
▸ Using 22 years of longitudinal health administrative data, this study examined the end-of-career practice patterns of primary care physicians. The authors found that physicians’ practice and retirement behaviour patterns were influenced by their sex and location of training. Aging resulted in gradual, modest changes in the provision of services, rather than abrupt declines, and physicians reduced their workloads and narrowed their scopes of practice in the years leading up to retirement. Up to 60% of primary care physicians who retired stopped providing comprehensive care but remained in the work force, providing other services with reduced workloads in advance of full retirement from clinical practice.
▸ Given the considerable number of primary care physicians who choose a phased approach to retirement, failure to consider the scope of practice of physicians at the ends of their careers might result in overestimation of the supply of physicians available to provide primary care services. Ideally, demographic factors, workload, and scope of practice should be considered in tandem when estimating the supply of physician services. In order to foster a flexible work force, policy makers might need to provide incentives for physicians of all ages to maintain broad scopes of practice and to continue to practise in settings where future demand is anticipated.
Points de repère du rédacteur
▸ Cette étude a utilisé des données sanitaires administratives portant sur 22 années pour déterminer comment les médecins responsables de soins primaires géraient leur fin de carrière. Les auteurs ont observé que le sexe et le lieu de formation du sujet avaient une incidence. Le vieillissement donnait lieu à des changements graduels et modestes, plutôt qu’à une brusque diminution, et les médecins réduisaient leur charge de travail et le champ de leurs activités au cours des années précédant la retraite. Jusqu’à 60 % des médecins de famille qui prenaient leur retraite cessaient de dispenser des soins complets, mais continuaient de travailler, offrant des services moins exigeants avant d’abandonner complètement leur pratique.
▸ Étant donné l’important nombre de médecins de soins primaires qui choisissent de prendre une retraite progressive, le fait de ne pas tenir compte du champ de pratique de ces médecins pourrait entraîner une surestimation des médecins susceptibles de fournir des soins primaires. Dans l’idéal, il faudrait tenir compte à la fois des facteurs démographiques, de la charge de travail et du champ de pratique lorsqu’on évalue la quantité de travail que doivent fournir les médecins. Pour favoriser une main-d’œuvre flexible, les responsables des politiques devront peut-être offrir aux médecins de tous les âges des mesures les incitant à maintenir de vastes champs de pratique et à continuer de pratiquer dans des contextes où on s’attend à de plus grands besoins.
Footnotes
Contributors
All authors contributed to the conception and design of the study, analysis and interpretation of the data, and writing and approving the submitted version of the manuscript.
Competing interests
None declared
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.Rittenhouse DR, Mertz E, Keane D, Grumbach K. No exit: an evaluation of measures of physician attrition. Health Serv Res. 2004;39(5):1571–88. doi: 10.1111/j.1475-6773.2004.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pong RW. Putting away the stethoscope for good? Toward a new perspective on physician retirement. Ottawa, ON: Canadian Institute for Health Information; 2011. [Google Scholar]
- 3.Denton FT, Spencer BG. What is retirement? A review and assessment of alternative concepts and measures. Can J Aging. 2009;28(1):63–76. doi: 10.1017/S0714980809090047. [DOI] [PubMed] [Google Scholar]
- 4.Feldman DC, Beehr TA. A three-phase model of retirement decision making. Am Psychol. 2011;66(3):193–203. doi: 10.1037/a0022153. [DOI] [PubMed] [Google Scholar]
- 5.Shultz KS, Wang M. Psychological perspectives on the changing nature of retirement. Am Psychol. 2011;66(3):170–9. doi: 10.1037/a0022411. [DOI] [PubMed] [Google Scholar]
- 6.Wang M, Shultz KS. Employee retirement: a review and recommendations for future investigation. J Manage. 2010;36(1):172–206. [Google Scholar]
- 7.Pannor Silver M. Critical reflection on physician retirement. Can Fam Physician. 2016;62:783–4. (Eng), 792–4 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 8.Ono T, Lafortune G, Schoenstein M. Health work force planning in OECD countries: a review of 26 projection models from 18 countries. OECD Health Working Papers. No. 62. Paris, Fr: OECD Publishing; 2013. [Google Scholar]
- 9.Schultz SE, Glazier RH. Identification of physicians providing comprehensive primary care in Ontario: a retrospective analysis using linked administrative data. CMAJ Open. 2017;5(4):E856–63. doi: 10.9778/cmajo.20170083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan B. Research atlas. Supply of physicians’ services in Ontario. Toronto, ON: Institute for Clinical Evaluative Sciences; 1999. [Google Scholar]
- 11.Joyce CM, Wang WC, McDonald HM. Retirement patterns of Australian doctors aged 65 years and older. Aust Health Rev. 2015;39(5):582–7. doi: 10.1071/AH14176. [DOI] [PubMed] [Google Scholar]
- 12.Watson DE, Reid R, Roos N, Heppner P. Growing old together: the influence of population and work force aging on supply and use of family physicians. Can J Aging. 2005;24(Suppl 1):37–45. doi: 10.1353/cja.2005.0058. [DOI] [PubMed] [Google Scholar]
- 13.Watson DE, Slade S, Buske L, Tepper J. Intergenerational differences in workloads among primary care physicians: a ten-year, population-based study. Health Aff (Millwood) 2006;25(6):1620–8. doi: 10.1377/hlthaff.25.6.1620. [DOI] [PubMed] [Google Scholar]
- 14.Petterson SM, Rayburn WF, Liaw WR. When do primary care physicians retire? Implications for work force projections. Ann Fam Med. 2016;14(4):344–9. doi: 10.1370/afm.1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan BT. The declining comprehensiveness of primary care. CMAJ. 2002;166(4):429–34. [PMC free article] [PubMed] [Google Scholar]
- 16.Hedden L, Barer ML, Cardiff K, McGrail KM, Law MR, Bourgeault IL. The implications of the feminization of the primary care physician work force on service supply: a systematic review. Hum Resour Health. 2014;12:32. doi: 10.1186/1478-4491-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Staiger DO, Auerbach DI, Buerhaus PI. Comparison of physician work force estimates and supply projections. JAMA. 2009;302(15):1674–80. doi: 10.1001/jama.2009.1461. [DOI] [PMC free article] [PubMed] [Google Scholar]