Abstract
Addiction is complex and multifactorial. Recognition provides the opportunity to provide potentially life-saving treatment. Oncology patients are not excluded from substance use disorders (SUDs) and the opioid epidemic. Patients with current or past SUDs may develop cancer, and an SUD may also develop during cancer treatment. Therefore, this unique subset of patients potentially has two fatal diseases: cancer and an SUD. Most oncology advanced practitioners (APs) are unprepared to care for SUDs in patients with cancer. Pain is one of the most common symptoms in the cancer population, and cancer-related pain is often treated with opioids. Opioid exposure increases the risk of developing an opioid use disorder (OUD). In addition, a cancer diagnosis can have a significant impact on mental health and wellness, and patients may use substances to cope with psychological distress. Drug and alcohol use exists on a continuum and while not all use is problematic, it may have adverse consequences. A cancer diagnosis provides another possibility for patients to engage in services and treatment for their unsafe use and/or addiction. The case study in this article of a patient with cancer and an SUD is an example of the challenges associated with the chronic and relapsing nature of addiction. Oncology advanced practitioners have the opportunity to positively influence outcomes through the assessment of substance use and adoption of harm reduction techniques in all patients with cancer.
CASE STUDY
Jane Doe is a 28-year-old female diagnosed 3 years ago with nodular sclerosis Hodgkin lymphoma. She completed five cycles of doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) chemotherapy; however, she did not return to her original treating oncologist for further care (Figure 1). She never received the recommended radiation therapy. Ms. Doe presented as a new patient to the clinic with a lump in her neck, which had increased in size over the past 6 months. Standard lab work was performed, including human immunodeficiency virus (HIV, nonreactive) and a hepatitis panel (concerning for new hepatitis B infection). Further workup consisted of imaging with CT, PET scans, and mediport placement for IV access. Lymph node biopsy confirmed Hodgkin lymphoma.
Figure 1.
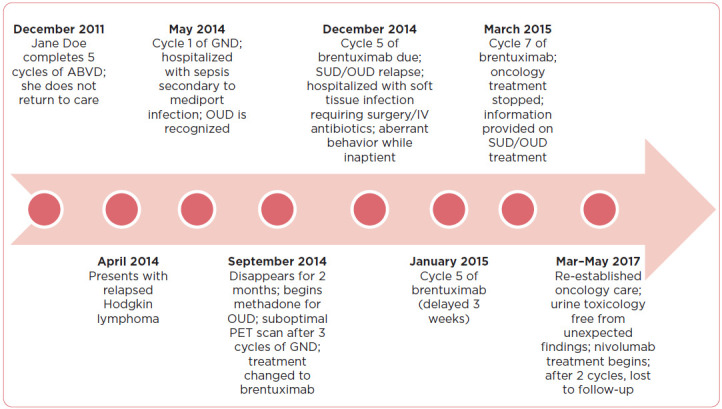
Case study timeline. ABVD = doxorubicin, bleomycin, vinblastine, and dacarbazine; GND = gemcitabine, navelbine, and doxorubicin; OUD = opioid use disorder; SUD = substance use disorder.
Salvage gemcitabine, navelbine, and doxorubicin (GND) chemotherapy was started. Cycle one was complicated by sepsis secondary to mediport infection, with peripheral blood and line cultures demonstrating both Klebsiella and gram-positive cocci in chains (viridans strep). A third culture was positive for Lactobacillus. On physical exam, Ms. Doe had multiple red marks around her mediport site, and her right arm showed evidence of prior needle injury. Infectious disease was consulted. During her hospitalization, she received IV vancomycin and cefepime. Emtricitabine/tenofovir was initiated for her newly recognized hepatitis B infection (hepatitis B DNA > 60,000,000). The mediport was removed due to infection. Ms. Doe was discharged with oral levofloxacin without venous access due to concerns of IV drug use.
Ms. Doe received her second and third cycles of GND without incident, but was lost to follow-up prior to cycle four. Two months later, she resurfaced after beginning treatment for her opioid use disorder at a methadone clinic. A restaging PET scan needed to be rescheduled several times due to hyperglycemia; eventually, it was determined her liquid methadone contained glucose. The PET scan demonstrated an overall mixed response, most likely related to suboptimal therapy. The treating team met with Ms. Doe to discuss goals of chemotherapy. She was told they were trying to treat her lymphoma and save her life, but needed her participation to be successful. This included addressing her heroin use. Missed appointments negatively impacted the efficacy of her treatments. The ultimate goal remained autologous stem cell transplant to cure her Hodgkin lymphoma.
Addiction is a complex and multifactorial disease (American Society of Addiction Medicine [ASAM], 2019). The opioid epidemic has led to increased concern about substance use disorders (SUDs), especially opioid use disorder (OUD), in patients with cancer (Carmichael et al., 2016). Addiction in oncology patients is not well described; a recent systematic review reported substance use rates ranging from 2% to 35%, with median use rates of 18% for opioids and 25.5% for alcohol (Yusufov et al., 2019). Substances such as alcohol and tobacco are known to increase the risk of certain cancers. Patients with previous or current SUD may develop cancer, related or unrelated to their substance use, and an SUD may also develop after a cancer diagnosis. Cancer-related pain is often treated with opioids, and opioid exposure increases the risk of developing an OUD (Dowell et al., 2016).
Patients with cancer and SUDs often have mental illness, and substances may be used in response to psychological distress. Polysubstance use with opioids, alcohol, marijuana, methamphetamines, and cocaine, is not uncommon (Jones & McCance-Katz, 2019). Serious complications leading to both increased health care utilization and negative outcomes may occur directly related to patients' substance use (Yusufov et al., 2019). For example, patients who inject drugs may experience skin and soft tissue infections, HIV, viral hepatitis, and infective endocarditis (Thakarar et al., 2019). Cancer treatment delays from nonadherence and/or complications may result in disease progression, increased symptoms, and ultimately death (Yusufov et al., 2019).
The ASAM recently updated the definition of addiction, emphasizing the complexity and multifactorial interactions of this treatable chronic disease. Perhaps improved understanding will drive a comprehensive national campaign to improve accessibility of addiction prevention, treatment, remission, and recovery programs for all people (ASAM, 2019). The current cancer care model is not always equipped to provide the extensive treatment necessary to holistically care for this unique patient population.
Most oncology clinicians are not prepared to confront the opioid epidemic or other SUDs. The lymphoma department at The Ohio State University James Cancer Hospital, a large academic cancer center, identified the need to address substance use after multiple patients experienced poor outcomes driven by addiction. This case represents one of our first experiences of addiction in a patient with active cancer. The purpose of the case study is to provide an example of the challenges and opportunities to improve outcomes for this complex patient population.
CASE STUDY CONTINUED
Following the suboptimal PET scan results, Ms. Doe's treatment was changed to brentuximab (Adcetris). Ms. Doe reported a recent car accident and drenching night sweats prior to cycle four; however, the restaging PET scan showed a good response. Before cycle five, Ms. Doe was falling sleep during her history and physical. Physical exam revealed a firm, erythematous mass approximately 12 cm × 8 cm on her right inner thigh and another firm mass on her left chest, approximately 3 cm × 2 cm. She was hospitalized due to concern of infection. Right femur MRI demonstrated an abscess in the sartorius muscle, with adjacent myositis, and superficial and deep fasciitis. General surgery performed emergent incision and drainage. Bacterial culture demonstrated methicillin-resistant Staphylococcus aureus. Intravenous antibiotics were administered. The comprehensive wound team recommended dressing changes twice daily. Liquid dilaudid was only given before dressing changes.
Ms. Doe admitted to drinking in excess and using heroin immediately prior to her hospital stay despite continuing to attend a methadone clinic. Urine toxicology detected heroin, morphine, codeine, diphenhydramine, methadone, and cotinine. Her methadone was continued at 60 mg daily; however, this was changed to liquid after a repeat urine toxicology demonstrated morphine and diphenhydramine (both not prescribed), methadone, and hydromorphone. The emergency response team was called twice during her hospitalization. Early one morning, she was found unconscious; the Code Blue team was alerted and she recovered rather quickly. Security searched the hospital room and found a full syringe of an unknown substance. Following this episode and for her safety, the room door was left open, she was not allowed visitors, and a staff member was present for the remainder of the hospital stay. Due to Ms. Doe's history of IV drug use, she was not prescribed opioids at discharge.
OVERVIEW
Harm reduction, the public health perspective of minimizing risk with the goal of decreasing negative outcomes, is a feasible alternative to begin addressing substance misuse and addiction in patients with cancer (ASAM, 2019). “Harm reduction” in the context of SUDs does not endorse substance misuse, but accepts it as reality and aims to reduce harmful consequences.
Integrating harm reduction tactics as universal precautions into routine oncology practice, that is, employing techniques to every patient, not only reduces stigma but also improves clinical care outcomes (Gourlay et al., 2005; Hawk et al., 2017; Paice, 2019; Sager & Childers, 2019). Oncology providers can implement harm reduction principles as a unique strategy to minimize risk while improving treatment adherence and cancer outcomes (Hawk et al., 2017).
All oncology patients should be screened for licit and illicit substance use, either with a formal screening tool or simply by asking every patient directly about their substance use. A neutral, nonjudgmental question can reduce the stigma associated with SUDs. Drug and alcohol use exist on a continuum, from nonproblematic to problematic, and not all use is problematic (Gourley et al., 2005; Sager & Childers, 2019). Although it may be challenging, providers should not be afraid to obtain a more detailed history if current or past use is identified, including asking about the substances used, frequency of use, method(s) of administration, and date of last use. Method(s) of administration (for instance, smoking or injection) may increase the risk of complications such as tissue and bloodstream infections, and may result in multisystem organ dysfunction (Wurcel et al., 2015). Recognition of substance use and a possible SUD provides the opportunity for patients to receive appropriate life-saving treatment (Sager & Childers, 2019). This unique subset of patients potentially has two fatal diseases: cancer and an SUD.
Many harm reduction principles focus on safe prescribing practices to reduce opioid-related risks and aberrant opioid-related behaviors. Suggestions include a single prescriber (individual or team), using only one pharmacy, and checking the state's prescription monitoring database program prior to prescribing a controlled medication.
Providers may also consider using a controlled medication management form or agreement (i.e., contract; McNally et al., 2019; Paice, 2019). Urine toxicology screens should be performed in patients receiving controlled medication prescriptions, noting the absence of the prescribed medication(s) and presence of nonprescribed/illicit substances. Accurate interpretation of results is critical to prevent false accusations of nonadherence or misuse. Unexpected findings should be discussed with the patient (McNally et al., 2019; Paice, 2019). Select patients may necessitate weekly prescriptions, limiting the quantity dispensed, and thus reducing the number of available pills. Refills should be dated (do not fill before [date]), with no early refills (McNally et al., 2019).
Mediports are frequently placed in oncology; a safe alternative for a patient with IV drug use requiring central venous access is a peripherally inserted central catheter, to be placed and removed at each visit or hospitalization (McNally et al., 2019). Additional harm reduction strategies might incorporate referrals to social work, addiction medicine (if available), primary care providers, and mental health providers (McNally et al., 2019). A multidisciplinary team is critical to best reflect the multifactorial nature of substance use, and assists with the identification of available educational, financial, and psychosocial resources to further enhance harm reduction techniques and provide a holistic approach to care. Prescribing medication-assisted treatment when appropriate has demonstrated effectiveness in improving mortality from OUD (Sordo et al., 2017). Substance use may interfere with pain and symptom management, treatment adherence, and may negatively impact quality of life (Yusufov et al., 2019). Implementing harm reduction strategies focusing on enhancing social support and safer alternatives to standard therapy may improve treatment adherence.
Patients with SUDs experience extraordinary stigma. Various terms are used interchangeably, making it challenging. Commonly used terms such as “abuse” convey high perceived fault and control (see Table 1). Language influences perceptions and judgements, even among health-care providers. Clinicians should establish and maintain judgement-free terminology to maximize consistency and accuracy; stigma, characterized by labeling and stereotyping, creates significant barriers to high-quality health care and treatment, leading to detrimental consequences (Ashford et al., 2018; Botticelli, 2016; Nyblade et al., 2019; Parker et al., 2019).
Table 1. Preferred Addiction Terminology.
| Preferred term | Commonly used term | Rationale |
|---|---|---|
Person or patient with a:
|
Someone who is a/an:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Note. Information from National Institute on Drug Abuse (2020).
Oncology providers may experience moral distress supporting patients who make harmful health choices based on personal disapproval of these “behaviors” (Hawk et al., 2017; Nyblade et al., 2019). Substance use disorders, including OUDs, are chronic, relapsing medical illnesses, yet misconceptions still exist that this is a weakness or choice, separating SUD/OUD treatment from the rest of health care (Olsen & Sharfstein, 2014). Recovery often requires both medication and psychosocial treatment and support, and complete abstinence from substance use may be an unrealistic goal (Hoffman et al., 2019; Passik & Kirsh, 2004). These knowledge deficits related to SUDs, combined with preexisting bias, may adversely impact care.
CASE STUDY CONTINUED
Cycle five of brentuximab was delayed for 3 weeks because of the hospitalization and infection. The multidisciplinary team established firm guidelines: Should Ms. Doe be found using heroin again, her treatment for Hodgkin lymphoma would be discontinued due to safety concerns. She was no longer a candidate for stem cell transplant due to her heroin use, and was able to complete her sixth cycle of treatment. Ms. Doe was provided information on SUD treatment at the cycle seven visit; treating her addiction was made the first priority. She was contacted 2 weeks later, but was then lost to follow-up. Ms. Doe communicated with the team a few times over the next 6 months; however, she continued to actively use heroin.
Two years later, Ms. Doe presented with symptoms of progressive disease. She reported heroin cessation. Urine toxicology indicated only the presence of buprenorphine. Treatment with nivolumab (Opdivo) started once disease workup was completed. After two cycles, Ms. Doe was lost to follow-up.
DISCUSSION
Ms. Doe had an active OUD that was not adequately addressed at the initial visit. Nurses and advanced practitioners (APs) are often the first members of the medical team to suspect an OUD/SUD (Passik & Kirsh, 2004). Ms. Doe was not asked directly about substance use while her health history was reviewed. The clinic nurse first suspected Ms. Doe's IV drug use while obtaining lab work at the conclusion of the initial appointment. Recognition of IV drug use by the oncology team may have prevented mediport placement and Ms. Doe's attempt to access the port, leading to hospitalization with infection and sepsis. This was also a missed opportunity to acknowledge and begin addressing her OUD.
The multidisciplinary oncology team first discussed Ms. Doe's substance use with her after she had disappeared for 2 months. The team was attempting to address Ms. Doe's OUD; in retrospect, the conversation was not helpful. It fails to recognize OUD as a disease, and implies Ms. Doe had control over her actions. This is similar to blaming a person with diabetes for uncontrolled blood sugar. Alternatively, the team could have arranged a multidisciplinary team meeting with Ms. Doe to openly discuss her heroin use, review the goals of care, and provide available resources. Establishing a more open and possibly trusting relationship benefits not only her OUD but her cancer as well. A multidisciplinary consult team specializing in providing medication and linking hospitalized patients to OUD services now exists within our hospital system.
Two years passed before Ms. Doe returned to care. Nivolumab, now approved to treat relapsed Hodgkin lymphoma, was started. This treatment is less immunosuppressive, does not require a central line for administration, and supportive care visits (e.g., labs, etc.) are not necessary between cycles, minimizing the need for more appointments.
CONCLUSION
Oncology is often associated with an empathetic and nonjudgmental setting. Patients with cancer often have assistance navigating the complexities of cancer care, and this help would certainly benefit patients who also have an addiction. This case study provides an example of the chronic and relapsing nature of addiction within the context of a cancer diagnosis. Patients may feel more comfortable confiding substance use to their oncology AP because of their trusting relationship, and APs have the opportunity to improve outcomes through incorporating harm reduction strategies as universal precautions for all patients with cancer. Next steps include developing and implementing SUD educational interventions, including stigma reduction, targeted to oncology APs. Innovation expanding patient access to comprehensive service delivery is critical for addressing substance use and cancer care together.
Acknowledgment
The authors would like to extend a sincere thank you to Carlton Brown for proofreading and providing constructive criticism of this manuscript.
Footnotes
The authors have no conflicts of interest to disclose.
References
- American Society of Addiction Medicine. (2019). ASAM Releases new definition of addiction to advance greater understanding of the complex, chronic disease. https://www.asam.org/resources/publications/magazine/read/article/2019/10/22/asam-releases-new-definition-of-addiction-to-advance-greater-understanding-of-the-complex-chronic-disease
- Ashford, R. D., Brown, A. M., & Curtis, B. (2018). Substance use, recovery, and linguistics: The impact of word choice on explicit and implicit bias. Drug and Alcohol Dependence, 189, 131–138. 10.1016/j.drugalcdep.2018.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botticelli, M. P. (2016). Changing the language of addiction. JAMA, 316(13), 1361–1362. 10.1001/jama.2016.11874 [DOI] [PubMed] [Google Scholar]
- Carmichael, A. N., Morgan, L., & Del Fabbro, E. (2016). Identifying and assessing the risk of opioid abuse in patients with cancer: An integrative review. Substance Abuse and Rehabillitation, 7, 71–79. 10.2147/SAR.S85409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowell, D., Haegerich, T. M., & Chou, R. (2016). CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016. MMWR, 65(1), 1–49. http://web.a.ebscohost.com/ehost/pdfviewer/pdfviewer?vid=1&sid=24c108a6-5214-4d18-9641-98aff78a1408%40sdc-v-sessmgr01 [DOI] [PubMed] [Google Scholar]
- Gourlay, D. L., Heit, H. A., & Almahrezi, A. (2005). Universal precautions in pain medicine: A rational approach to the treatment of pain. Pain Medicine, 6(2), 107–112. 10.1111/j.1526-4637.2005.05031.x [DOI] [PubMed] [Google Scholar]
- Hawk, M., Coulter, R. W., Egan, J. E., Fisk, S., Friedman, M. R., Tula, M., & Kinsky, S. (2017). Harm reduction principles for healthcare settings. Harm Reduction Journal, 14, 70. 10.1186/s12954-017-0196-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman, K. A., Terashima, J. P., & McCarty, D. (2019). Opioid use disorder and treatment: challenges and opportunities. BMC Health Services Research, 19. 10.1186/s12913-019-4751-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, C. M., & McCance-Katz, E. F. (2019). Co-occurring substance use and mental disorders among adults with opioid use disorder. Drug and Alcohol Dependence, 197, 78–82. 10.1016/j.drugalcdep.2018.12.030 [DOI] [PubMed] [Google Scholar]
- McNally, G. A., Sica, A., & Wiczer, T. (2019). Managing addiction: Guidelines for patients with cancer. Clinical Journal of Oncology Nursing, 23(6), 655–658. 10.1188/19.CJON.655-658 [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. (2020). Words matter-terms to use and avoid when talking about addiction. https://www.drugabuse.gov/nidamed-medical-health-professionals/health-professions-education/words-matter-terms-to-use-avoid-when-talking-about-addiction
- Nyblade, L., Stockton, M. A., Giger, K., Bond, V., Ekstrand, M. L., McLean, R.,…Wouters, E. (2019). Stigma in health facilities: Why it matters and how we can change it. BMC Medicine, 17, 25. 10.1186/s12916-019-1256-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen, Y., & Sharfstein, J. M. (2014). Confronting the stigma of opioid use disorder and its treatment. JAMA, 311(14), 1393–1394. 10.1001/jama.2014.2147 [DOI] [PubMed] [Google Scholar]
- Paice, J. A. (2019). Risk assessment and monitoring of patients with cancer receiving opioid therapy. Oncologist, 24(10), 1294–1298. 10.1634/theoncologist.2019-0301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker, C. M., Hirsch, J. S., Hansen, H. B., Branas, C., & Martins, S. (2019). Facing opioids in the shadow of the HIV epidemic. New England Journal of Medicine, 380(1). 10.1056/NEJMp1813836 [DOI] [PubMed] [Google Scholar]
- Passik, S. D., & Kirsh, K. L. (2004). Opioid therapy in patients with a history of substance abuse. CNS Drugs, 18(1), 13–25. 10.2165/00023210-200418010-00002 [DOI] [PubMed] [Google Scholar]
- Sager, Z., & Childers, J. (2019). Navigating challenging conversations about nonmedical opioid use in the context of oncology. Oncologist, 24(10), 1299–1304. 10.1634/theoncologist.2019-0277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sordo, L., Barrio, G., Bravo, M. J., Indave, B. I., Degenhardt, L., Wiessing, L.,…Pastor-Barriuso, R. (2017). Mortality risk during and after opioid substitution treatment: Systematic review and meta-analysis of cohort studies. BMJ, 357(j1550). 10.1136/bmj.j1550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakarar, K., Rokas, K. E., Lucas, F. L., Powers, S., Andrews, E., DeMatteo, C.,…Cohen, M. (2019). Mortality, morbidity, and cardiac surgery in Injection Drug Use (IDU)-associated versus non-IDU infective endocarditis: The need to expand substance use disorder treatment and harm reduction services. PLOS ONE, 14(11), e0225460. 10.1371/journal.pone.0225460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurcel, A. G., Merchant, E. A., Clark, R. P., & Stone, D. R. (2015). Emerging and underrecognized complications of illicit drug use. Clinical Infectious Diseases, 61(12), 1840–1849. 10.1093/cid/civ689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusufov, M., Braun, I. M., & Pirl, W. F. (2019). A systematic review of substance use and substance use disorders in patients with cancer. General Hospital Psychiatry, 60, 128–136. 10.1016/j.genhosppsych.2019.04.016 [DOI] [PubMed] [Google Scholar]


