Abstract
Th subsets are defined according to their production of lineage-indicating cytokines and functions. In this study, we have identified a subset of human Th cells that infiltrates the epidermis in individuals with inflammatory skin disorders and is characterized by the secretion of IL-22 and TNF-α, but not IFN-γ, IL-4, or IL-17. In analogy to the Th17 subset, cells with this cytokine profile have been named the Th22 subset. Th22 clones derived from patients with psoriasis were stable in culture and exhibited a transcriptome profile clearly separate from those of Th1, Th2, and Th17 cells; it included genes encoding proteins involved in tissue remodeling, such as FGFs, and chemokines involved in angiogenesis and fibrosis. Primary human keratinocytes exposed to Th22 supernatants expressed a transcriptome response profile that included genes involved in innate immune pathways and the induction and modulation of adaptive immunity. These proinflammatory Th22 responses were synergistically dependent on IL-22 and TNF-α. Furthermore, Th22 supernatants enhanced wound healing in an in vitro injury model, which was exclusively dependent on IL-22. In conclusion, the human Th22 subset may represent a separate T cell subset with a distinct identity with respect to gene expression and function, present within the epidermal layer in inflammatory skin diseases. Future strategies directed against the Th22 subset may be of value in chronic inflammatory skin disorders.
Introduction
Th subsets play a discriminative role in translating antigen-specific immune responses into tissue functions or immunopathology. The identification of novel T cell subsets, such as Th17 cells, is important in order to define the role of the specific immune response in human disease. Across the board of different pathologies, distinct T cell subsets secrete cytokines that not only function on other immune cells, but also instruct target cells (1–3). Each T cell subset secretes tissue-instructing cytokines such as IFN-γ (Th1), IL-4 (Th2), and IL-17 (Th17), which induce MHC-expression in nonlymphoid cells, mucus secretion in epithelial cells, and IL-6 expression in keratinocytes and/or epithelial cells, respectively (4).
A less well-defined tissue-instructing cytokine is IL-22, which is expressed by Th17 cells (5, 6), but also by NK cells (7). Recent studies have determined that some T cells express IL-22 independently of IL-17, particularly CCR10+ T cells (2, 8–10). IL-22 belongs to the IL-10 cytokine family and binds to a heterodimeric receptor consisting of the IL10 receptor (IL-10R) β chain and the IL-22R. Despite this receptor sharing, IL-22 signaling acts independently of IL-10 (11) and, in contrast to IL-10, also triggers 3 MAPK pathways (12). The IL-22R is expressed almost exclusively on nonimmune cells, such that IL-22, like IL-17, acts primarily on tissue cells (13).
The function of IL-22 is difficult to generalize: It is not antiinflammatory, nor is it necessarily proinflammatory. However, it is consistently described to enable epithelial innate immune responses, which can be detrimental or protective. An example of a detrimental effect is epithelial hyperplasia in psoriasis (PS), which also can be induced by IL-22 in human artificial skin cultures (14). Furthermore, IL-22 synergizes with IL-17 in the induction of proinflammatory cytokines in human bronchial epithelial cells (3) and colonic myofibroblasts (15).
Examples of protective effects of IL-22 were reported in Gram-negative bacterial pneumonia, in which IL-22 induces the secretion of antimicrobial substances in lung epithelial cells (3). In addition, IL-22, but not IL-17, protects from hepatitis-induced liver damage by preventing hepatocyte apoptosis (16, 17). In the skin, IL-22 induces antimicrobial peptides, promotes keratinocyte proliferation, and inhibits differentiation, which suggests a role in remodeling wound healing and in innate defense mechanisms (14). The role of IL-22 in common skin disorders such as atopic eczema (AE) and allergic contact dermatitis (ACD) is currently not known.
Here we describe a Th22 subset of T cells, which was clearly separate from Th17 and other known T cell subsets. Th22 cells expressed several FGFs, were associated with epidermal repair responses, and synergized with TNF-α to induce a characteristic Th22 signature in keratinocytes.
Results
IL-22–expressing cells represent a tissue T cell subset.
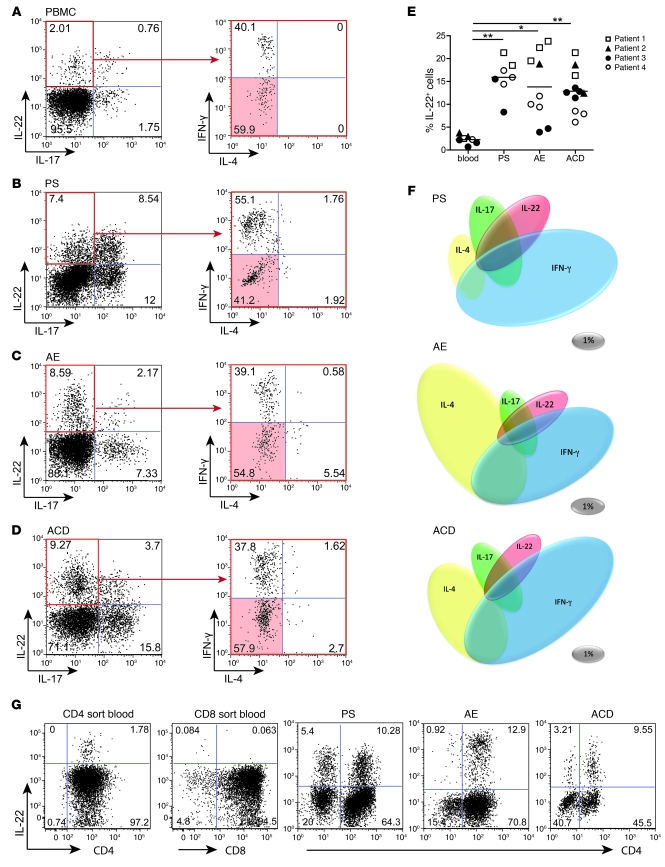
To investigate the cytokine profile of circulating and skin-homing T lymphocytes, we analyzed freshly isolated PBMCs (n = 4) and short-term cultures of skin biopsies obtained from patients with PS (n = 3), AE (n = 4), and ACD (n = 4). T cells were permeabilized, and their cytokine profile was studied by flow cytometry and multicolor intracellular staining. As expected, obvious differences between the samples were observed. AE-derived T cells were characterized by a large proportion of IL-4–expressing T cells (30.5% ± 10.0%), whereas PS- and ACD-derived T cells showed a prevalence of IFN-γ–expressing T cells (PS, 34.3% ± 3.7%; ACD, 36.4% ± 4.8%; Figure 1F and Supplemental Table 1; supplemental material available online with this article; doi: 10.1172/JCI40202DS1). The IL-17–expressing population was largest in PS (17.4% ± 4.2%), followed by ACD (13.1% ± 3.1%) and AE (9.0% ± 1.2%; Figure 1). This IL-17–expressing population overlapped with IFN-γ–producing T cells and, to a lesser degree, with those expressing IL-4, whereas approximately 50% were pure Th17 cells (both IL-4 and IFN-γ negative). IL-22–producing T cells were observed in both PBMCs and inflammatory skin diseases. Although interindividual differences were high, the frequency of IL-22+ T cells was significantly higher in skin-derived T cell lines than in the circulation (PBMCs, 2.3% ± 0.4%; PS, 15.9% ± 2.3%; AE, 13.8% ± 4.0%; ACD, 12.9% ± 2.4%; Figure 1E). Thus, IL-22+ cells were enriched in inflamed skin.
Figure 1. Th22 cells represent a distinct T cell subset enriched in inflammatory skin diseases.
(A–D) Representative 4-color intracellular cytokine stainings of primary human T lymphocytes derived from PBMCs (A), PS (B), AE (C), and ACD (D) for IL-22, IL-17, IFN-γ, and IL-4. Shown are dot plots for IL-22 and IL-17 and of IL-17–IL-22+ gated cells (red outline) for IFN-γ and IL-4. Th22 cells are shown by red shading. Numbers indicate relative percentages per quadrant. (E) Frequency of IL-22+ cells in PBMCs (n = 4) and in PS (n = 3), AE (n = 4), and ACD (n = 3). Symbols denote individual determinations, and horizontal bars denote mean. *P < 0.05; **P < 0.01. (F) Plasticity in T cell phenotypes, as shown by coexpression of IL-22 with other cytokines in PS (n = 3), AE (n = 4), and ACD (n = 4). Gray ovals denote scale, indicating 1% of total cells. (G) The majority of IL-22+ T cells belongs to the CD4+ subpopulation, as shown for CD4/CD8 sorted cells from PBMCs and skin T cell lines of PS, AE, and ACD. Numbers indicate relative percentages per quadrant.
In addition to distinct IL-4, IFN-γ, and IL-17 populations, a subset of T cells secreting IL-22 alone was present as a robust single-positive entity. Depending on the disease, about one-third of total IL-22+ cells were clear-cut Th22 cells (Supplemental Figure 1), and another third were Th17 cells coproducing Il-22; thus, Th22 and Th17 cells were the major T cell sources of IL-22. The overlap of cytokine expression observed in T cells derived from inflammatory skin disorders is shown in Figure 1F. These data illustrate that the size and likely plasticity from Th1, Th2, Th17, and Th22 subsets toward neighboring phenotypes was distinct for the different diseases.
Because IL-22 is not released solely by T lymphocytes, we investigated IL-22+ cells from blood and skin for their expression of T cell markers. The majority of IL-22+ cells were found within the CD4+ subpopulation in circulating PBMCs and AE, whereas in both PS and ACD, a minor, but substantial, fraction was IL-22+CD4– (Figure 1G). Our data highlight that CD4+ Th cells represent the major source of IL-22 in the skin, although IL-22 was also secreted by other leukocyte subsets, such as NK cells and CD8+ T cells (data not shown).
Characteristics of Th22 clones.
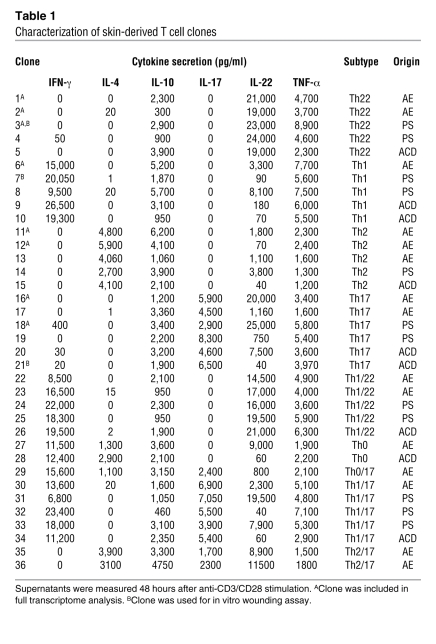
T cell subsets are defined by an epigenetically imprinted cytokine profile that is assumed to be stable over multiple cell divisions, thereby allowing amplification of immune responses by clonal expansion. Starting from T cell lines, as analyzed in Figure 1, we generated 244 distinct T cell clones from 2 donors with AE (143 clones), 44 clones from a patient with ACD, and 57 clones from a patient with PS (Table 1).
Table 1 .
Characterization of skin-derived T cell clones
Consistently with the single-cell analysis from biopsies, multiple Th22 clones were characterized by solitary IL-22 expression, which did not show substantial protein secretion of IL-4, IFN-γ, or IL-17 (Figure 2, A–C, left). As observed for the large majority of T cell clones isolated from skin, Th22 cells were capable of secreting IL-10 and/or TNF-α. The cytokine secretion pattern of isolated Th22 clones was remarkably stable even after 4 restimulations over sequential 10-week cultures. Th22 clones released IL-22 within 6 hours, reaching a peak at 12 hours and persisting at this level for at least 48 hours (Figure 2, A–C, right). Surface expression profiling of Th22 clones confirmed the CD3+CD4+ phenotype of Th22 cells, whereas the CD8 and NK cell markers CD56, NKp44, and NKp46 were negative (Supplemental Figure 2).
Figure 2. Th22 clones show a stable phenotype.
Skin T cell lines were cloned by limiting dilution and analyzed by intracellular cytokine staining and ELISA. Th22 clones 1 (A), 2 (B), and 3 (C; see Table 1) produced exclusively IL-22, as determined by multicolor flow cytometry. Stability of the Th22 phenotype is also shown in a time course after TCR stimulation and over a culture time of 10 weeks with subsequent TCR restimulations. Cytokine content of cell-free supernatant is shown for 1 representative experiment.
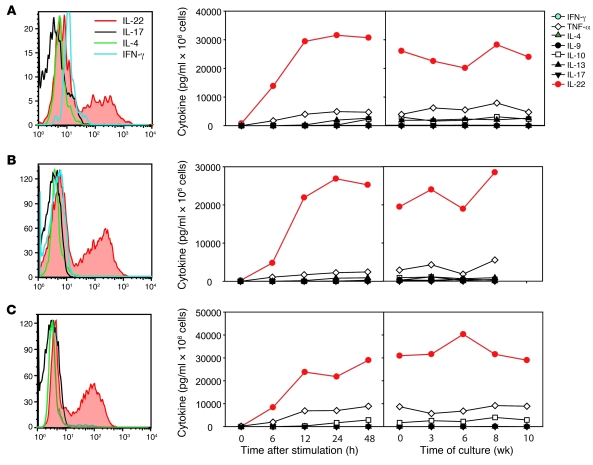
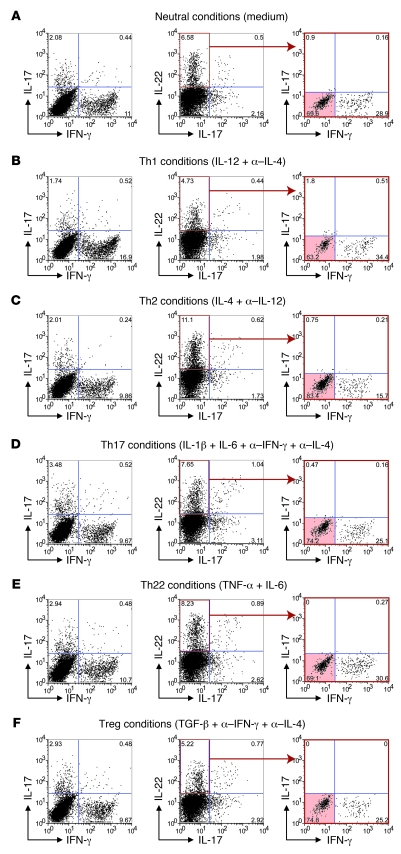
Th22 cells represent an independent and stable lineage of Th cells.
Because Th cell are increasingly understood to differ in plasticity and differentiation status, we investigated the phenotype stability of Th22 cells under different polarizing conditions. Skin-derived memory Th22 clones did not lose the capacity to secrete IL-22 under Th1, Th2, Th17, and Treg conditions, nor did they gain the capacity to produce substantial amounts of an additional subset-defining cytokine, although IFN-γ was slightly induced under different conditions (Supplemental Figure 3). These findings were confirmed in freshly isolated CD45RA–CCR10+ T cell lines from PBMCs of 3 independent donors (Figure 3). CCR10+ sorting enriched IL-22–producing, antigen-experienced T cells (Supplemental Figure 4 and ref. 9). The frequency of IL-22+ T cells and the secretion of IL-22 remained at high levels under all polarizing conditions (Figure 3, B–F, and Supplemental Figure 4), being slightly diminished only under Treg conditions. Importantly, induction of IFN-γ under Th1 conditions and IL-17 under Th17 conditions was not caused by a conversion of Th22 cells into Th1 or Th17 cells, as the number of Th22 cells within the CCR10+ T cell lines was not diminished under different polarizing conditions (Supplemental Figure 4). In contrast, both Th2 and Th22 conditions tended to increase the number of Th22 cells, whereas IL-13 and IL-4 were induced only marginally or not at all (Supplemental Figure 4). Thus, Th22 cells represent a stable T cell lineage, and memory Th22 cells do not convert into another subset.
Figure 3. Th22 cells are stable and cannot be deformed into other T cell phenotypes.
Freshly isolated CCR10+ T cells did not convert into another Th subset. Shown are intracellular stainings for CCR10+CD45RA– cells after 5 days under nonpolarizing (A), Th1 (B), Th2 (C), Th17 (D), Th22 (E), and Treg (F) conditions and subsequent stimulation with PMA/ionomycin. Shown are dot plots for IL-17 and IFN-γ, for IL-22 and IL-17, and of IL-17–IL-22+ gated cells (red outline) for IFN-γ and IL-4. Th22 cells are shown by red shading. Numbers indicate relative percentages per quadrant. Data are representative for 3 independent donors. Mean values and corresponding IL-22, TNF-α, IL-13, and IL-4 secretion are shown in Supplemental Figure 3.
Transcriptome of Th22 cells.
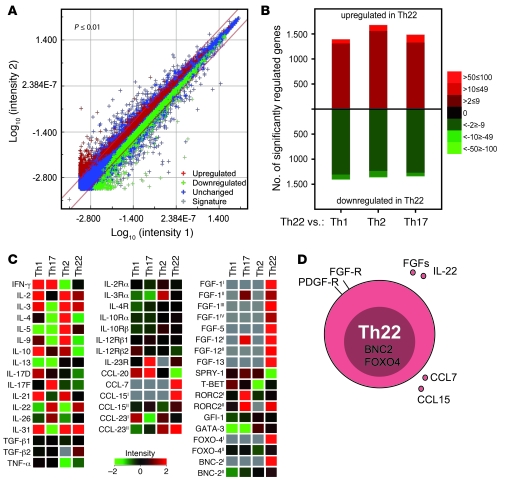
Th22 clones were subjected to full transcriptome analysis to validate the phenotype compared with known T cell subsets, specifically Th17 cells. We compared 3 Th22 cell clones originating from different AE and PS patients with Th1, Th17, and Th2 clones (n = 5; Table 1). To exclude the possibility that Th22 clones derive from Th17 cells, we chose IL-22–producing Th17 clones for gene chip comparison (Table 1). Despite the genetic distance, the Th22 clones showed surprisingly low variance (Figure 4A). The transcriptome for Th22 cells demonstrated similar numbers of up- and downregulated transcripts, whereas the profile for Th22 cells was distinct and not closely related to those of other known T cell subtypes (Figure 4B). The gene chip analysis also confirmed the selectivity of IL-22 expression and the subset-independent nature of TNF-α (Figure 4C). IL-10 was produced substantially less by Th22 clones; however, substantial secretion was observed (Figure 4 and Table 1). Therefore, IL-10 can also be regarded as subset independent. Interestingly, Th22 cells upregulated a number of FGFs upon stimulation. This upregulation seemed to be exclusively limited to Th22 cells, as we observed substantial differences to other known T cell subsets. In contrast, SPRY1, an FGF antagonist, was substantially reduced in Th22 cells compared with Th1, Th2, and Th17 cells. The chemokine expression pattern of Th22 cells provides further evidence for tissue remodeling activity of this subset. Compared with other T cell populations, they produced substantially more transcripts of CCL7, involved in tissue fibrosis, and CCL15 and CCL23 splice variant 2; CCL23 splice variant 1 showed higher expression in Th1 cells (Figure 4C and Supplemental Table 3). In contrast to Th22 cells, Th17 cells strongly upregulated CCL20, a chemokine attracting CCR6+ cells. Furthermore, Th17 cells selectively expressed IL-23R. Transcription factors also underlined the individual expression pattern of Th22 cells, given the reduced RORC2, GATA3, and T-bet expression and the presence of BNC-2 and FOXO4 (Figure 4C). It remains to be demonstrated that these factors are also involved in the polarization process upon Th22 differentiation. The expression profile clearly identified Th22 cells as a separate subset, including subset-specific surface receptors and transcription factors (Figure 4D).
Figure 4. Whole genome transcriptome analysis of Th22 compared with Th1, Th2, and Th17 cells reveals unique functional profiling of Th22.
Th22 clones (n = 3) and Th1, Th2, and Th17 clones (n = 5) were stimulated for 6 hours with a TCR stimulus, and the mRNA expression profile was analyzed in a whole genome microarray approach. (A) Differential Th22 transcriptome, shown as a dLogPlot of Th22 pool genes that were upregulated or downregulated compared with Th1, Th2, and Th17 pools. (B) Th22 transcriptome separation, shown by total up- and downregulated genes in the Th22 pool compared with the single subsets of Th1, Th2, and Th17 clones. (C) Clonal phenotypes. Intensity of immunologically relevant genes of T cell subsets is shown as a heatmap. The Agilent array (single color, technology 14850) contains multiple probe sets for some genes that were empirically observed to differ in intensity from a gene-covering selection of probes. The differential abundance of these probes can originate from alternative splice variants or differential mRNA stability, for example. Alternative probes showing differences in intensity in the present study are indicated by Roman numerals; probe set sequences are available at http://www.agilent.com. Compared with CCL15I (A_23_P218369), CCL15II (A_24_P301501) recognizes an additional splice variant. For FGF1, 16 splice variants are already suggested, and the difference between Th1 and Th22 may originate in differential exon usage (shown are FGF1I, A_23_P136433; FGF1II, A_24_P251969; FGF1III, A_24_P111106; FGF1IV, A_23_P213336). For FGF12, 11 different splice variants are known, and differential signals could reflect differential splicing (shown are FGF12I, A_24_P334300; FGF12II, A_23_P211727). Probe RORC2II (A_23_P372910) binds in the 3′ untranslated region, whereas RORC2I (A_23_P324107) binds in the coding region. FOXO4II (A_24_P379165) binds the 3′ end of the gene, for which up to 3 splice variants may exist (also shown is FOXO4I, A_24_P911066). The more sensitive BNC-2I (A_23_P43690) binds exon 6, whereas BNC-2II (A_23_P43684) binds to the C-terminal exon 7. For CCL23, 2 splice variants are known, of which variant 1 is recognized by CCL23I (A_24_P319088) and both variants by CCL23II (A_24_P133905). (D) Overview of the Th22 phenotype.
Epidermal location of Th22 cells.
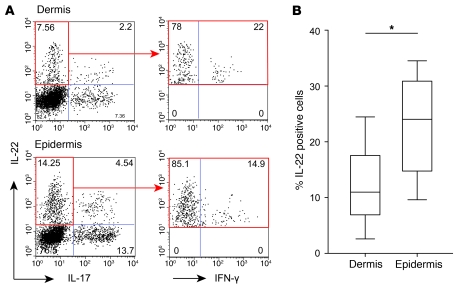
Epidermis and dermis of skin biopsies were separated by dispase treatment, and infiltrated lymphocytes of each fraction were analyzed for the expression of lead cytokines. Figure 5A shows a representative 3-color FACS analysis, which revealed a higher proportion of IL-22+ T cells and Th22 cells in the epidermal compartment. On average, a 2.2-fold enrichment of IL-22+ cells was observed in epidermal compared with dermal isolations of inflamed skin of AE (n = 4) and ACD (n = 4) patients (median [of 8 total] dermis, 10.98; median epidermis, 24.03; P ≤ 0.05; Figure 5B; see Supplemental Figure 1B for disease-separated values).
Figure 5. Th22 cells are enriched in the epidermal compartment of the skin.
Skin biopsies were separated into dermal and epidermal parts by dispase treatment. Dermal and epidermal T cell lines were analyzed by flow cytometry. (A) Representative 3-color intracellular staining for IL-22, IL-17, and IFN-γ (on Il-17–IL-22+ gated cells; red outline) of a separated ACD biopsy. Numbers indicate relative percentages in each quadrant. (B) Calculated mean percentage of total IL-22+ cells in dermis and epidermis (n = 4 each of AE and ACD). Lines within boxes denote means; box upper and lower bounds indicate SD; and whiskers indicate minimum and maximum values. *P < 0.05.
The increased number of IL-22–producing T cells in the epidermis was the result of an increase in Th22 cells and in IFN-γ/IL-22–coproducing T cells. The distribution of IL-22+ T cell subpopulations shifted toward IFN-γ/IL-22–coproducing T cells (dermis, 30.5%; epidermis, 42.0%), whereas Th22 cells were comparably distributed in the dermal (35.3%) and epidermal (31.0%) compartments. Accordingly, IL-4/IL-22–coproducing T cells were diminished in the epidermal compartment (dermis, 4.6%; epidermis, 2.8%).
Th22 cells orchestrate potentially novel innate immune responses by keratinocytes.
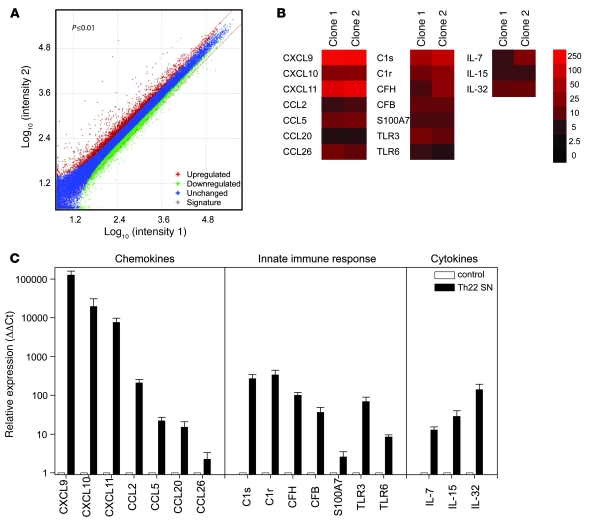
To investigate the potential activities of the Th22 resident within the epidermis on epidermal cells, human primary keratinocytes of healthy donors were exposed for 12 hours to medium or Th22 supernatants of 3 independent and activated Th22 clones. Whole transcriptome analysis of keratinocytes revealed alterations of multiple genes (Figure 6A), including genes involved in the intracellular transport of proteins, genes for chemokines regulating different T cell subsets and cytokines, and genes belonging to the innate immune system (Figure 6B and Supplemental Table 4). The Th1-attracting and antimicrobial chemokines CXCL9, CXCL10, and CXCL11 were induced up to 400-fold. A minor, 10-fold induction was also observed for monocyte-attracting CCL2, the antiviral and antibacterial Th1 chemokine CCL5, the CCR6+ cell–attracting CCL20, and the fibroblast- and eosinophil-attracting CCL26. Furthermore, Th22 supernatants induced T cell growth factors IL-7 and IL-15 and the macrophage differentiation factor IL-32. Surprisingly, Th22 supernatants also substantially induced C1s and C1r, inducible factors of the classical complement pathway, and the initial alternative pathway factor CFB, as well as its regulator, CFH. This Th22-induced pattern of antimicrobial defense also included the antimicrobial peptide S100A7 as well as TLR3 (recognizing double-stranded RNA) and TLR6 (recognizing bacterial lipoproteins).
Figure 6. Th22 cells induce a specific response pattern in primary human keratinocytes.
Primary human keratinocytes (n = 3) were stimulated for 12 hours with supernatants (SN) of activated Th22 clones (n = 2). mRNA was extracted and hybridized to whole genome microarrays. (A) dLogPlot of up- and downregulated genes in primary human keratinocytes in response to Th22 supernatant incubation. (B) Extract of significantly upregulated genes by supernatants of Th22 clones. (C) Confirmation of array results by real-time PCR. Data are representative for at least 3 independent experiments. Error bars indicate SD.
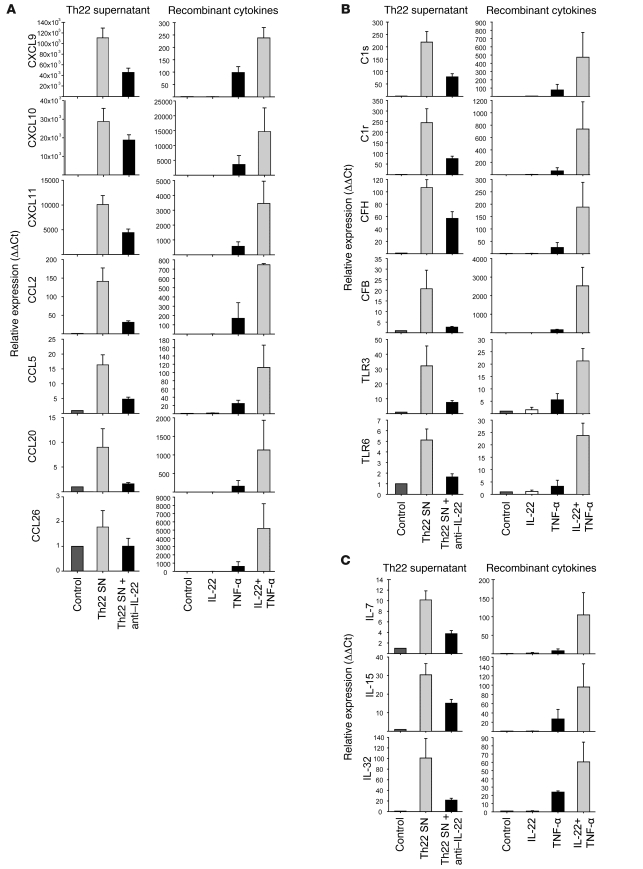
Th22 cells regulate keratinocyte defense mechanisms by an IL-22/TNF-α combination key.
The DNA array analysis was validated using real-time PCR (Figure 6C) and also involved the neutralization of IL-22 in these cultures. A clear reduction was observed in all induced genes, ranging 2- to 10-fold depending on the gene. Because Th22 cells also produce TNF-α, we further hypothesized a synergistic effect of IL-22 and TNF-α in stimulation of keratinocytes. This was tested by the addition of recombinant IL-22, TNF-α, or a combination of both cytokines to primary keratinocyte cultures. Whereas IL-22 alone only marginally induced production of chemokines, complement factors, and cytokines, TNF-α clearly upregulated the expression of all candidate immune genes (Figure 7). However, the combination of IL-22 and TNF-α resulted in a substantially higher stimulation of keratinocytes, multiplying the effects of TNF-α 5- to 15-fold (Figure 7).
Figure 7. Th22 cells influence keratinocyte functions by a combination of IL-22 and TNF-α.
Human primary keratinocytes were stimulated with Th22 supernatants in the presence or absence of neutralizing anti–IL-22 antibodies (left) or with recombinant cytokines (right). mRNA was extracted after 12 hours, and gene expression was analyzed by real-time PCR. (A) Chemokine expression. (B) Innate immune response. (C) Cytokine expression pattern. Data are representative for at least 3 independent experiments. Error bars indicate SD.
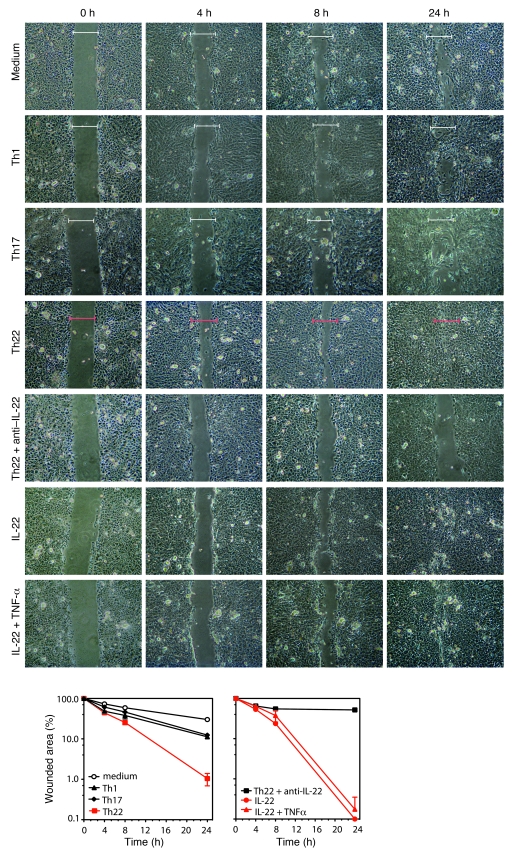
Th22 cells enhance epidermal wound healing in an IL-22–dependent manner.
Besides inducing a defense armory against invading pathogens in keratinocytes, Th22 supernatants effectively enhanced rapid wound healing in a functional keratinocyte in vitro injury model (Figure 8). As soon as 4 hours after wounding, Th22 supernatants had substantial and persistent effects on epithelial layer closure, whereas other supernatants of other T cell subsets were inefficient. Consistent with the data described above, these effects were dependent on IL-22, as IL-22–neutralizing antibodies reverted this effect and recombinant IL-22 restored rapid wound healing. Moreover, in contrast to Th22 supernatant–induced defense genes, IL-22 alone efficiently induced rapid wound healing, and no synergism with TNF-α was observed in that context. These data indicate that IL-22 may function as a biphasic cytokine: protective and regenerative in steady state while amplifying proinflammatory signals given by TNF-α.
Figure 8. Th22 supernatant enhances wound healing in a functional in vitro injury model.
Microscopic photography after wound induction on a confluent monolayer of primary human keratinocytes in a time course from 4 to 24 hours revealed that wound healing was efficiently enhanced by Th22 supernatant and by IL-22, but less so by other T cell subset supernatants. Neutralization of IL-22 in Th22 supernatant reverted this effect. Brackets show initial wound size for comparison. Graphs below show relative wound closure over time, based on the wound gap compared with initial wound size. Error bars indicate SD.
Discussion
We have shown that Th22 cells represent a distinct human T cell subset characterized by a unique expression profile, a functional spectrum that we believe to be novel, and prominence within inflammatory skin diseases. Similar to Th17 cells, Th22 cells were rarely found in PBMCs, while they were clearly detected in T cell populations isolated from the skin of patients with PS, AE, and ACD. This is consistent with the previously suggested role of Th17-related IL-22 in PS (18, 19), atopic dermatitis (20), and contact dermatitis (21, 22).
Although we demonstrated a pure Th22 population, we observed a substantial proportion of Th22 cells that also secreted IFN-γ or IL-17. This plasticity is also observed for other T cell phenotypes, such as Th17 cells expressing IFN-γ or Tregs expressing IL-17 (23, 24). It is of interest that the plasticity expressed by Th22 cells in AE was also apparent in a small percentage of IL-4–expressing cells, but not within PS or ACD. Our present data demonstrated that the extent and composition of this plasticity varied among different inflammatory disease entities even within the same organ. We anticipate that Th22 plasticity is also related to disease severity, as severity-associated factors such as IL-12 (25) are known to modulate T cell plasticity (23, 26).
Although T cell plasticity is now an accepted component of the specific immune system, the stability of a T cell phenotype over multiple cell divisions remains a hallmark of Th subsets, conferring immunologic memory, as we have demonstrated for Th22 cell clones in the current study. Th22 clones responded within 12 hours with maximal IL-22 secretion and were also able to produce moderate amounts of TNF-α and IL-10. Although NK cells show a similar narrow cytokine profile (27–29), the Th22 cells described herein were clearly defined as non-NK cells, demonstrated by CD4 and TCR expression and the absence of NK cell markers. Recent studies indicate that IL-6 and TNF-α, along with the help of plasmacytoid DCs, can promote the Th22 phenotype (9); however, precise culture requirements lacking serum and APCs remain to be defined.
Th22 cells showed distinct differences in the profile of altered genes compared with Th1, Th2, and Th17 cells, confirming an individual signature for the Th22 subset. In contrast to Th17, expression of CCL20 and IL-23R (30) was absent in Th22 clones. Furthermore, RORC, the transcription factor essential for Th17 differentiation (31), was strongly diminished in Th22 cells. This confirms recent reports (9, 10) that highlight the aryl hydrocarbon receptor in the differential regulation of IL-22 over IL-17 (10). The clonal stability; the selective expression of transcription factors, PDGF receptor, and CCR-10 (9); and the fact that naive T cells differentiate in the presence of TNF-α and IL-6 toward the Th22 phenotype (9) provide strong evidence that Th22 cells represent a terminally differentiated and independent T cell subtype.
The Th22 expression profile revealed several FGFs: FGF1 is a powerful mitogen exhibiting strong action on different cell types, including endothelial cells (32, 33), and FGF5 also acts on neuronal differentiation (34) and is associated with inhibition of hair growth (35, 36). These cytokines play a role in various stages of development and morphogenesis as well as in angiogenesis and wound healing processes. Several members of the FGF family have previously been shown to be involved in PS (37, 38). Consistent with this upregulation of fibrogenic factors, the SPRY1 gene, an antagonist of FGFs, was significantly reduced in Th22 cells. A potential role for Th22 in remodeling or repair of the epithelial barrier is further supported by the chemokine expression pattern characterized by CCL7, involved in tissue fibrosis (39), and CCL15 and possibly CCL23 splice variant 2, both implicated in angiogenesis (40, 41). We note that results with CCL23 splice variant 1 contradicted this finding (Figure 4C), but earlier publications did not clarify which isoform was detected.
Th22 cells, like Th17 cells, show an epidermal homing characteristic reflected by a remarkable transcriptome response of primary human keratinocytes in response to Th22 supernatants: namely, the chemokines CXCL9, CXCL10, and CXCL11 are likely to recruit further T cells and also show antimicrobial activity. However, the transcriptome profile also revealed characteristics of keratinocytes that we believe to be previously unknown, including the ability to contribute to expression of complement factors such as C1s, C1r, and CFB and expression of TLR3 and TLR6, in addition to the previously described ability of keratinocytes to express S100 genes and defensins in response to IL-22 (14). Th22 cells also have potential to promote adaptive and innate immunity by virtue of the induction of T cell and NK promoting factors, such as IL-15 and IL-7, in keratinocytes. Of particular interest is the expression of the TNF-α–enhancing cytokine IL-32 by keratinocytes, which corresponds to the ability of Th22 cells to also express TNF-α. We hypothesize that IL-22 and TNF-α represent the key combination of cytokines expressed by Th22 cells that unlocks the activation of keratinocytes, as in vitro cultures using either Th22 supernatants or a combination of IL-22 and TNF-α maximally induced the Th22 signature in keratinocytes, whereas anti–IL-22 did not fully block — and recombinant IL-22 alone was not sufficient to induce — expression of these genes. This dual key is a recurring scheme observed in the lymphoid regulation of tissue cells in inflammatory context, such as the regulation of epithelial cells by IL-17, which is only maximal in synergism with IFN-γ, IL-1, or TNF-α (42, 43). In contrast to major effects on the innate immune response by keratinocytes in a proinflammatory context, IL-22 and TNF-α did not synergize in the enhanced wound healing clearly induced by Th22 cells. This effect was only IL-22 dependent and reflected the induction of promigratory genes in keratinocytes by IL-22 (8, 14, 44, 45). These data indicate a double function of IL-22 in cutaneous immunity: on the one hand, being protective and regenerative, and on the other hand, amplifying TNF-α–induced signals to contribute to a proinflammatory microenvironment during skin immune reactions.
In conclusion, our present results demonstrate that Th22 cells represent a T cell subset uniquely able to regulate epidermal responses in inflammatory skin diseases. The subset is not only defined by a stable and distinct expression profile, but also characterized by what we believe to be a novel functional profile. The identification of Th22 cells provides a cellular target for therapeutic intervention and may shed light on thus far unknown pathways in the control of tissue immunity and remodeling.
Methods
Patients.
Adult PS patients (n = 3) suffered from stable, moderate to severe plaque PS, defined by a PS area and severity index (PASI) score of at least 12, a minimum involvement by PS of 10% body surface area, and a history of PS of at least 6 months before sample collection. AE patients (n = 4) were diagnosed according to the criteria of Hanifin and Rajka (46). ACD patients (n = 4) displayed positive patch tests following criteria of the International Contact Dermatitis Research Group (47). Exclusion criteria were local treatment with corticosteroids, phototherapy, or systemic corticosteroid therapy within 4 weeks of sample collection. Before blood or skin samples were taken, each participant gave his informed consent. The study was approved by the ethical committee of the Istituto Dermopatico Dell’Immacolata.
Isolation and expansion of T cells and primary human keratinocytes.
T cell clones derived from inflammatory skin conditions were isolated as previously described (48). Briefly, whole biopsies, or biopsy material treated with 0.5% dispase (Roche) for 1 hour at 37°C in order to separate the epidermis and dermis, were cultured in RPMI 1640 supplemented with 2 mM glutamine, 1 mM sodium pyruvate, 1% nonessential amino acids, 0.05 mM 2-mercaptoethanol, 1% penicillin/streptomycin (all Invitrogen; RPMI complete), and 5% human serum (Sigma-Aldrich) supplemented with 60 U/ml IL-2. Migrated cells were collected after 2–4 days and cloned after 6 days by limiting dilution (0.6 cells/well in 96-well U-bottom microtiter plates) in RPMI complete 5% human serum and 10% heat-inactivated FBS (Hyclone) on a feeder layer of irradiated PBMCs, 30 IU/ml IL-2, and 1% PHA (Sigma-Aldrich). Fresh medium containing IL-2 (Novartis) was added 3 times per week, and clones were restimulated using irradiated feeder PBMCs every 3 weeks. Allergen or hapten reactivity of both T cells lines and clones was determined using the 3H-thymidine incorporation assay. Cytokine content of clone supernatants was analyzed using ELISA in order to identify Th subset identity (see Table 1).
Autologous keratinocytes were isolated using the previously described method of suction blister (43). Briefly, blisters were induced by generating a vacuum on normal skin of the forearms. Epidermal sheets were obtained from blister roofs, treated with 0.05% trypsin (Invitrogen) to obtain single-cell suspension, and seeded on a feeder layer of irradiated 3T3/J2 fibroblasts in modified Green’s medium. At 70%–80% confluence, keratinocytes were detached with 0.05% trypsin, aliquoted, and cryopreserved in liquid nitrogen. Keratinocytes of second and third passage were used in experiments.
Isolation of CCR10+ T cells and phenotype stability.
CCR10+ effector T cells were magnetically isolated from CD45RA depleted PBMC with a combination of a PE-labeled anti-CCR10 antibody (R&D Systems) and anti-PE microbeads (Miltenyi Biotech). CCR10+ cells were restimulated for 5 days in AIMV medium with anti-CD3 and anti-CD28 antibodies and the following cytokines and blocking antibodies: 25 ng/ml IL-12 and 5 μg/ml anti–IL-4 (Th1 condition); 25 ng/ml IL-4, 5 μg/ml anti–IL-12, and anti–IFN-γ (Th2 condition); 20 ng/ml IL-1β, 20 ng/ml IL-6, 20 ng/ml IL-23, 5 ng/ml TGF-β, 5 μg/ml anti–IL-12, and 5 μg/ml anti–IL-4 (Th17 condition); 5 ng/ml TGF-β, 5 μg/ml anti–IL-12, and 5 μg/ml anti–IL-4 (Treg condition); 50 ng/ml TNF-α, 20 ng/ml IL-6, 5 μg/ml anti–IL-12, and 5 μg/ml anti–IL-4 (Th22 condition).
Stimulation of keratinocytes.
A total of 105 keratinocytes were seeded in 6-well microtiter plates in keratinocyte basal medium (KBM) with supplements (Invitrogen) for 5 days. At day of stimulation, medium was replaced by KBM and KBM plus 50 ng/ml recombinant TNF-α and/or 50 ng/ml IL-22. Alternatively, supernatant was obtained from Th22 clones stimulated for 48 hours with anti-CD3 and anti-CD28 (both BD Biosciences) and centrifuged to avoid cellular contamination. Cytokine content was measured by ELISA. Natural IL-22 was neutralized by incubation with 10 μg/ml anti–IL-22 (AF-782; R&D systems) 3 hours prior to keratinocyte stimulation. Full medium served as negative control. After 12 hours of stimulation, period cells were washed, detached with 0.05% trypsin, shock-frozen in liquid nitrogen, and conserved at –80°C until further analysis.
Flow cytometry analysis.
The following antibodies were used in flow cytometry analysis: FITC-conjugated CD4 (clone SK3), PE-conjugated CD4 (clone SK3), PE-conjugated CD8 (clone SK1), and FITC-conjugated CD56 (clone NCAM16.2), all from BD Biosciences; FITC-conjugated IL-4 (clone MP4-25D2), FITC-conjugated IFN-γ (clone B27), and allophycocyanin-conjugated IFN-γ (clone B27), all from BD Biosciences — Pharmingen; PE-conjugated IL-22 (clone 142928) and PE-conjugated IL-4 (clone 3007.11), all from R&D Systems; and PE-conjugated IL-17A (clone SK3) from eBioscience.
Intracellular cytokine staining was performed using a kit (BD Biosciences) according to the manufacturer’s instructions. Briefly, cells were stimulated with PMA and ionomycin for 6 hours in the presence of monensin. After 2 hours, brefeldin A was added. Cells were fixed and permeabilized with Cytofix/Cytoperm (BD Biosciences) and incubated with antibodies. Cells were analyzed using FACS Aria (BD Biosciences), and data were illustrated by FlowJo software (Tree Star Inc.).
ELISA.
Concentrations of IFN-γ, IL-4, IL-10, IL-17, IL-22, and TNF-α in cell-free culture supernatant were measured using commercially available sandwich ELISA kits (all from R&D systems).
RNA extraction, cDNA generation, and real-time PCR analysis.
Total RNA was isolated from frozen cell pellets with a RNeasy Mini kit (Qiagen) and reversely transcribed with random hexamers using the First Strand cDNA Synthesis Kit (Fermentas) according to the manufacturer’s protocols. Primers for real-time PCR, designed with Primer Express software (version 1.2; Applied Biosystems), are listed in Supplemental Table 2. PCR was performed in 384-well plates using EP Motion 5075 (Eppendorf) for pipetting all reagents. The cDNA was amplified with SYBR Green Mastermix (Applied Biosystems) in an ABI Prism 7000HT Sequence Detection System (Applied Biosystems). The comparative ΔΔCt method was used to calculate the relative quantification and the range of confidence.
Whole genome microarray analysis.
Quality and integrity of RNA samples was checked with the Agilent 2100 Bioanalyzer platform (Agilent Technologies); 0.5 μg of each total RNA sample was amplified and Cy3 labeled using the Agilent Low RNA Input Linear Amp Kit (Agilent Technologies) following the manufacturer’s protocol. The hybridization procedure was performed according to the Agilent 60-mer oligo microarray processing protocol using the Agilent Gene Expression Hybridization Kit and Agilent Whole Human Genome Oligo Microarrays 4x44K (Agilent Technologies). Fluorescence signals of the hybridized arrays were detected using Agilent’s Microarray Scanner System (Agilent Technologies). The Agilent Feature Extraction Software was used to read out and process the microarray image files, and differential gene expression Feature Extraction Software–derived output data files were further analyzed using the Rosetta Resolver gene expression data analysis system (Rosetta Biosoftware).
Keratinocyte in vitro injury model.
Confluent monolayers of cultured primary human keratinocytes were scratched with the tip of a p-200 pipette to create a uniform cell-free zone in each well. Cellular debris was removed by PBS washing. Wounded monolayers were then incubated in Th1-, Th22-, and Th17-conditioned RPMI media. Recombinant human IL-22 (10 ng/ml; R&D Systems), alone or in combination with recombinant human TNF-α (10 ng/ml; R&D Systems), and Th22 supernatant preincubated with neutralizing anti–IL-22 antibody (AF-782; R&D Systems) served as controls. KBM plus RPMI represented the negative control. Microscopy pictures were taken at different time points after injury with a digital camera. The residual gap between migrating keratinocytes was measured with a computer-assisted image analysis system (Axiovision; Zeiss) and expressed as a percentage of the initial scratched area.
Statistics.
Statistical analysis was performed using 2-tailed Student’s t test. Statistically significant differences were defined as P less than 0.05.
Supplementary Material
Acknowledgments
We wish to thank P. Eyerich (Institute for Computer Science, Faculty of Technical Engineering, University of Freiburg, Freiburg, Germany) for instructions on graphical information transfer. The work was supported by the Bayerische Forschungsstiftung, by Schweizerischer Nationalfonds grant 310000-112329, and by European Commission FP6 Programme grant LSHB-CT-2005-018681.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J. Clin. Invest. 119:3573–3585 (2009). doi:10.1172/JCI40202.
References
- 1.Burgler S., et al. 2009Differentiation and functional analysis of human T(H)17 cells. J. Allergy Clin. Immunol. 123588–595; e581–e587. . 10.1016/j.jaci.2008.12.017 [DOI] [PubMed] [Google Scholar]
- 2.Eyerich K., et al. IL-17 in atopic eczema: linking allergen-specific adaptive and microbial-triggered innate immune response. J. Allergy Clin. Immunol. 2009;123:59–66; e54. doi: 10.1016/j.jaci.2008.10.031. [DOI] [PubMed] [Google Scholar]
- 3.Aujla S.J., et al. IL-22 mediates mucosal host defense against Gram-negative bacterial pneumonia. Nat. Med. 2008;14:275–281. doi: 10.1038/nm1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmidt-Weber C.B., Akdis M., Akdis C.A. TH17 cells in the big picture of immunology. J. Allergy Clin. Immunol. 2007;120:247–254. doi: 10.1016/j.jaci.2007.06.039. [DOI] [PubMed] [Google Scholar]
- 5.Liang S.C., et al. Interleukin (IL)-22 and IL-17 are coexpressed by Th17 cells and cooperatively enhance expression of antimicrobial peptides. J. Exp. Med. 2006;203:2271–2279. doi: 10.1084/jem.20061308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kreymborg K., et al. IL-22 is expressed by Th17 cells in an IL-23-dependent fashion, but not required for the development of autoimmune encephalomyelitis. J. Immunol. 2007;179:8098–8104. doi: 10.4049/jimmunol.179.12.8098. [DOI] [PubMed] [Google Scholar]
- 7.Cupedo T., et al. Human fetal lymphoid tissue-inducer cells are interleukin 17-producing precursors to RORC+ CD127+ natural killer-like cells. Nat. Immunol. 2009;10:66–74. doi: 10.1038/ni.1668. [DOI] [PubMed] [Google Scholar]
- 8.Nograles K.E., et al. 2009IL-22-producing “T22” T cells account for upregulated IL-22 in atopic dermatitis despite reduced IL-17-producing T(H)17 T cells. J. Allergy Clin. Immunol. 1231244.e2–1252.e2. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duhen T., Geiger R., Jarrossay D., Lanzavecchia A., Sallusto F. Production of interleukin 22 but not interleukin 17 by a subset of human skin-homing memory T cells. Nat. Immunol. 2009;10:857–863. doi: 10.1038/ni.1767. [DOI] [PubMed] [Google Scholar]
- 10.Trifari S., Kaplan C.D., Tran E.H., Crellin N.K., Spits H. Identification of a human helper T cell population that has abundant production of interleukin 22 and is distinct from T(H)-17, T(H)1 and T(H)2 cells. Nat. Immunol. 2009;10:864–871. doi: 10.1038/ni.1770. [DOI] [PubMed] [Google Scholar]
- 11.Wolk K., et al. Is there an interaction between interleukin-10 and interleukin-22? Genes Immun. 2005;6:8–18. doi: 10.1038/sj.gene.6364144. [DOI] [PubMed] [Google Scholar]
- 12.Lejeune D., et al. Interleukin-22 (IL-22) activates the JAK/STAT, ERK, JNK, and p38 MAP kinase pathways in a rat hepatoma cell line. Pathways that are shared with and distinct from IL-10. J. Biol. Chem. 2002;277:33676–33682. doi: 10.1074/jbc.M204204200. [DOI] [PubMed] [Google Scholar]
- 13.Wolk K., et al. IL-22 increases the innate immunity of tissues. Immunity. 2004;21:241–254. doi: 10.1016/j.immuni.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 14.Boniface K., et al. IL-22 inhibits epidermal differentiation and induces proinflammatory gene expression and migration of human keratinocytes. J. Immunol. 2005;174:3695–3702. doi: 10.4049/jimmunol.174.6.3695. [DOI] [PubMed] [Google Scholar]
- 15.Andoh A., et al. Interleukin-22, a member of the IL-10 subfamily, induces inflammatory responses in colonic subepithelial myofibroblasts. Gastroenterology. 2005;129:969–984. doi: 10.1053/j.gastro.2005.06.071. [DOI] [PubMed] [Google Scholar]
- 16.Zenewicz L.A., et al. Interleukin-22 but not interleukin-17 provides protection to hepatocytes during acute liver inflammation. Immunity. 2007;27:647–659. doi: 10.1016/j.immuni.2007.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pan H., Hong F., Radaeva S., Gao B. Hydrodynamic gene delivery of interleukin-22 protects the mouse liver from concanavalin A-, carbon tetrachloride-, and Fas ligand-induced injury via activation of STAT3. Cell. Mol. Immunol. 2004;1:43–49. [PubMed] [Google Scholar]
- 18.Ma H.L., et al. IL-22 is required for Th17 cell-mediated pathology in a mouse model of psoriasis-like skin inflammation. J. Clin. Invest. 2008;118:597–607. doi: 10.1172/JCI33263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boniface K., et al. A role for T cell-derived interleukin 22 in psoriatic skin inflammation. Clin. Exp. Immunol. 2007;150:407–415. doi: 10.1111/j.1365-2249.2007.03511.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koga C., Kabashima K., Shiraishi N., Kobayashi M., Tokura Y. Possible pathogenic role of Th17 cells for atopic dermatitis. J. Invest. Dermatol. 2008;128:2625–2630. doi: 10.1038/jid.2008.111. [DOI] [PubMed] [Google Scholar]
- 21.Ricciardi L., et al. Increased serum levels of IL-22 in patients with nickel contact dermatitis. Contact Dermatitis. 2009;60:57–58. doi: 10.1111/j.1600-0536.2008.01454.x. [DOI] [PubMed] [Google Scholar]
- 22.Larsen J.M., Bonefeld C.M., Poulsen S.S., Geisler C., Skov L. IL-23 and T(H)17-mediated inflammation in human allergic contact dermatitis. J. Allergy Clin. Immunol. 2009;123:486–492. doi: 10.1016/j.jaci.2008.09.036. [DOI] [PubMed] [Google Scholar]
- 23.Lee Y.K., et al. Late developmental plasticity in the T helper 17 lineage. Immunity. 2009;30:92–107. doi: 10.1016/j.immuni.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siegmund K., et al. Unique phenotype of human tonsillar and in vitro-induced FOXP3+CD8+ T cells. J. Immunol. 2009;182:2124–2130. doi: 10.4049/jimmunol.0802271. [DOI] [PubMed] [Google Scholar]
- 25.Arican O., Aral M., Sasmaz S., Ciragil P. Serum levels of TNF-alpha, IFN-gamma, IL-6, IL-8, IL-12, IL-17, and IL-18 in patients with active psoriasis and correlation with disease severity. Mediators Inflamm. 2005;2005:273–279. doi: 10.1155/MI.2005.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ouaked N., et al. Regulation of the foxp3 gene by the Th1 cytokines: the role of IL-27-induced STAT1. J. Immunol. 2009;182:1041–1049. doi: 10.4049/jimmunol.182.2.1041. [DOI] [PubMed] [Google Scholar]
- 27.Satoh-Takayama N., et al. Microbial flora drives interleukin 22 production in intestinal NKp46+ cells that provide innate mucosal immune defense. Immunity. 2008;29:958–970. doi: 10.1016/j.immuni.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 28.Malmberg K.J., Ljunggren H.G. Spotlight on IL-22-producing NK cell receptor-expressing mucosal lymphocytes. Nat. Immunol. 2009;10:11–12. doi: 10.1038/ni0109-11. [DOI] [PubMed] [Google Scholar]
- 29.Cella M., et al. A human natural killer cell subset provides an innate source of IL-22 for mucosal immunity. Nature. 2009;457:722–725. doi: 10.1038/nature07537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Annunziato F., et al. Phenotypic and functional features of human Th17 cells. J. Exp. Med. 2007;204:1849–1861. doi: 10.1084/jem.20070663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ivanov I.I., et al. The orphan nuclear receptor RORgammat directs the differentiation program of proinflammatory IL-17+ T helper cells. Cell. 2006;126:1121–1133. doi: 10.1016/j.cell.2006.07.035. [DOI] [PubMed] [Google Scholar]
- 32.Almus F.E., Rao L.V., Pendurthi U.R., Quattrochi L., Rapaport S.I. Mechanism for diminished tissue factor expression by endothelial cells cultured with heparin binding growth factor-1 and heparin. Blood. 1991;77:1256–1262. [PubMed] [Google Scholar]
- 33.Winkles J.A., et al. Human vascular smooth muscle cells both express and respond to heparin-binding growth factor I (endothelial cell growth factor). Proc. Natl. Acad. Sci. U. S. A. 1987;84:7124–7128. doi: 10.1073/pnas.84.20.7124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reuss B., Dono R., Unsicker K. Functions of fibroblast growth factor (FGF)-2 and FGF-5 in astroglial differentiation and blood-brain barrier permeability: evidence from mouse mutants. J. Neurosci. 2003;23:6404–6412. doi: 10.1523/JNEUROSCI.23-16-06404.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ota Y., et al. Fibroblast growth factor 5 inhibits hair growth by blocking dermal papilla cell activation. Biochem. Biophys. Res. Commun. 2002;290:169–176. doi: 10.1006/bbrc.2001.6140. [DOI] [PubMed] [Google Scholar]
- 36.Cho Y.M., et al. Hair-cycle-dependent expression of parathyroid hormone-related protein and its type I receptor: evidence for regulation at the anagen to catagen transition. J. Invest. Dermatol. 2003;120:715–727. doi: 10.1046/j.1523-1747.2003.12147.x. [DOI] [PubMed] [Google Scholar]
- 37.Kovacs D., et al. Immunohistochemical analysis of keratinocyte growth factor and fibroblast growth factor 10 expression in psoriasis. Exp. Dermatol. 2005;14:130–137. doi: 10.1111/j.0906-6705.2005.00261.x. [DOI] [PubMed] [Google Scholar]
- 38.Sharpe R.J., Arndt K.A., Bauer S.I., Maione T.E. Cyclosporine inhibits basic fibroblast growth factor-driven proliferation of human endothelial cells and keratinocytes. Arch. Dermatol. 1989;125:1359–1362. doi: 10.1001/archderm.125.10.1359. [DOI] [PubMed] [Google Scholar]
- 39.Varga J., Abraham D. Systemic sclerosis: a prototypic multisystem fibrotic disorder. J. Clin. Invest. 2007;117:557–567. doi: 10.1172/JCI31139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hwang J., et al. Human CC chemokine CCL23, a ligand for CCR1, induces endothelial cell migration and promotes angiogenesis. Cytokine. 2005;30:254–263. doi: 10.1016/j.cyto.2005.01.018. [DOI] [PubMed] [Google Scholar]
- 41.Hwang J., et al. Angiogenic activity of human CC chemokine CCL15 in vitro and in vivo. FEBS Lett. 2004;570:47–51. doi: 10.1016/j.febslet.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 42.Honorati M.C., Cattini L., Facchini A. IL-17, IL-1beta and TNF-alpha stimulate VEGF production by dedifferentiated chondrocytes. Osteoarthritis Cartilage. 2004;12:683–691. doi: 10.1016/j.joca.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 43.Albanesi C., et al. Interleukin-17 is produced by both Th1 and Th2 lymphocytes, and modulates interferon-gamma- and interleukin-4-induced activation of human keratinocytes. J. Invest. Dermatol. 2000;115:81–87. doi: 10.1046/j.1523-1747.2000.00041.x. [DOI] [PubMed] [Google Scholar]
- 44.Wolk K., et al. IL-22 regulates the expression of genes responsible for antimicrobial defense, cellular differentiation, and mobility in keratinocytes: a potential role in psoriasis. Eur. J. Immunol. 2006;36:1309–1323. doi: 10.1002/eji.200535503. [DOI] [PubMed] [Google Scholar]
- 45.Li W., et al. The serine protease marapsin is expressed in stratified squamous epithelia and is up-regulated in the hyperproliferative epidermis of psoriasis and regenerating wounds. J. Biol. Chem. 2009;284:218–228. doi: 10.1074/jbc.M806267200. [DOI] [PubMed] [Google Scholar]
- 46.Hanifin J.M., Rajka G. Diagnostic features of atopic dermatitis. Acta. Derm. Venereol. (Stockh.). 1980;92(Suppl.):44–47. [Google Scholar]
- 47.Andersen K.E., et al. Contact dermatitis. A review. Contact Dermatitis. 1987;16:55–78. doi: 10.1111/j.1600-0536.1987.tb01382.x. [DOI] [PubMed] [Google Scholar]
- 48.Cavani A., et al. Human CD4+ T lymphocytes with remarkable regulatory functions on dendritic cells and nickel-specific Th1 immune responses. . J. Invest. Dermatol. 2000;114:295–302. doi: 10.1046/j.1523-1747.2000.00881.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.