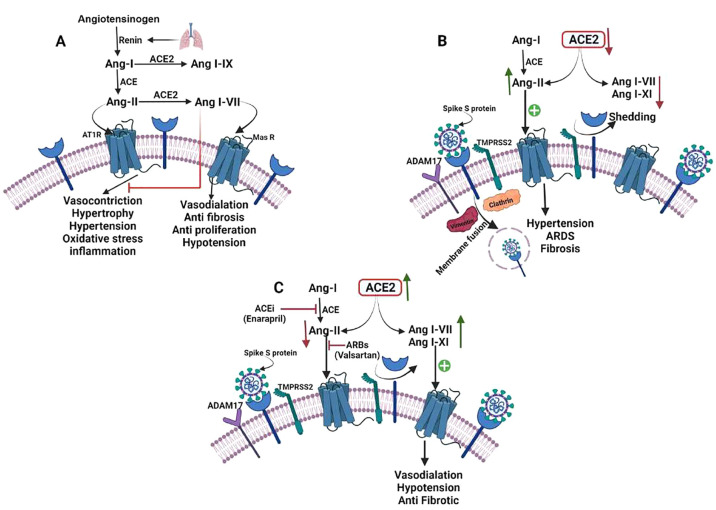
Figure 5.
Possible connection between the pathophysiology of Hypertension and SARS-CoV-2 infection. (A) ACE2/Ang I–VII/Mas axis and the renin-angiotensin system (RAS). Angiotensinogen is transformed to Ang-I by the protease renin, which is then converted to Ang-II by the ACE. Vasoconstriction, hypertrophy, fibrosis, proliferation, inflammation, and oxidative stress can be caused by Ang-II following binding to the AT1 receptor. Ang-I and Ang-II can be converted to Ang I–IX and Ang I–VII respectively by ACE2. Vasodilatation, vascular protection, anti-fibrosis, anti-proliferation, and anti-inflammation are effects of Ang I–VII binding to the Mas receptor. (B) When SARS-CoV-2 binds to ACE2, the virus is internalized with the receptor, and ACE2 is removed via ADAM17. Reduced ACE2 availability causes a decrease in the levels of Ang I–VII, I–IX, and Ang-II degradation, as well as increased AT1 receptor activation, facilitating HTN, ARDS, and fibrosis. (C) Infection with SARS-CoV-2 and therapy with ACEi/ARB. After SARS-CoV-2 binding, ACE2 is upregulated by ACEi and ARB, and free ACE2 persists. Ang I–VII, a favorable metabolite of Ang II, is still destroyed by ACE2, although the AT1 receptor is less activated than Mas receptor-activated through increased levels of Ang I–VII and I–IX resulting in vasodilatation, hypotension, and antifibrotic activity. ARB prevents Ang II binding on the AT1 receptor, while ACE decreases Ang II production, resulting in decreased AT1 receptor activation and sustained interaction with ACE2, preventing ACE2 internalization.