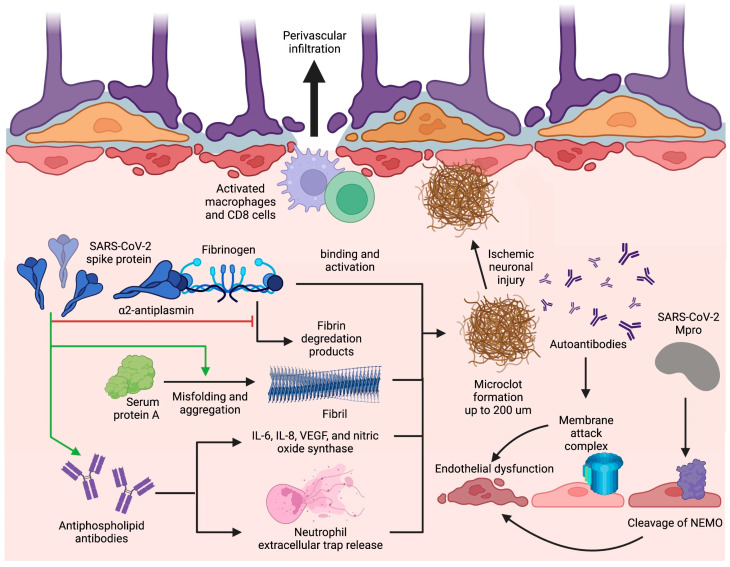
Figure 3.
Blood–brain barrier disruption and microclot formation. SARS-CoV-2 can cause increased microclot formation through spike protein interactions with fibrinogen and serum protein A that promote fibril formation and resist fibrinolysis. Antiphospholipid antibodies are also present in long COVID and can precipitate microclot formation through IL-6, IL-8, VEGF, nitric oxide synthase, and NET release. These microclots also contain α2AP which inhibit plasmin and thus prevent the degradation of fibrin, further contributing to their fibrinolysis-resistant nature. Additionally, SARS-CoV-2 can induce BBB disruption through Mpro cleavage of NEMO in endothelial cells leading to cell death and string vessel formation. Figure was created with the BioRender software.