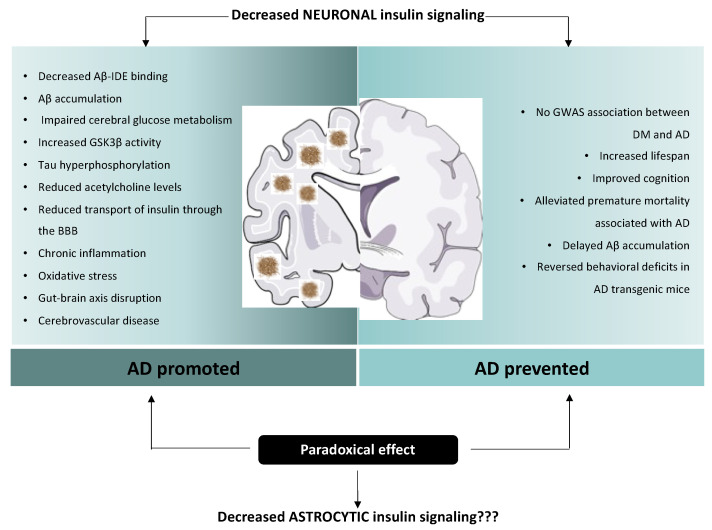
Figure 2.
Paradoxical effect of insulin on Alzheimer’s disease etiopathology. Multiple plausible mechanisms have been proposed to explain the connection between insulin resistance and AD. Insulin and Aβ compete for the binding to IDE, leading to Aβ protein accumulation. Moreover, cerebral glucose metabolism usually precedes AD signs. In situations of insulin resistance, the activity of GSK3β is increased and leads to the hyperphosphorylation of Tau. Furthermore, insulin resistance reduces acetylcholine levels in the brain. Chronic state of hyperinsulinemia interferes with the saturable transport of insulin through the BBB. Other possible mechanisms linking DM and AD have also been described, such as chronic inflammation, oxidative stress, disruption of the gut–brain axis and cerebrovascular diseases. Strikingly, a plausible protective role of diminished neuronal insulin signalling has also been proposed. It has been seen that decreased neuronal insulin signalling has a beneficial effect on lifespan regulation, and can even delay age-related processes. Decreased insulin signalling has also been associated with reduced premature mortality associated with AD and delayed Aβ accumulation. Due to the paradoxical effects of insulin signalling, the current state of our understanding is insufficient to differentiate clearly between the beneficial vs. negative impact on aging and neurodegenerative diseases of reduced insulin signalling. Notably, this debate is fed by results obtained from studies focused exclusively on neuronal insulin signalling; however, the role of insulin action on other brain cell types, such as astrocytes, is still unexplored.