Abstract
Sleep disturbances are widely prevalent following a traumatic brain injury (TBI) and have the potential to contribute to numerous post-traumatic physiological, psychological, and cognitive difficulties developing chronically, including chronic pain. An important pathophysiological mechanism involved in the recovery of TBI is neuroinflammation, which leads to many downstream consequences. While neuroinflammation is a process that can be both beneficial and detrimental to individuals’ recovery after sustaining a TBI, recent evidence suggests that neuroinflammation may worsen outcomes in traumatically injured patients, as well as exacerbate the deleterious consequences of sleep disturbances. Additionally, a bidirectional relationship between neuroinflammation and sleep has been described, where neuroinflammation plays a role in sleep regulation and, in turn, poor sleep promotes neuroinflammation. Given the complexity of this interplay, this review aims to clarify the role of neuroinflammation in the relationship between sleep and TBI, with an emphasis on long-term outcomes such as pain, mood disorders, cognitive dysfunctions, and elevated risk of Alzheimer’s disease and dementia. In addition, some management strategies and novel treatment targeting sleep and neuroinflammation will be discussed in order to establish an effective approach to mitigate long-term outcomes after TBI.
Keywords: traumatic brain injury, headache, concussion, neuroinflammation, microglia, sleep, pain, Alzheimer’s, dementia
1. Introduction
It has been reported that 69 million (95% CI 64–74 million) individuals are estimated to suffer traumatic brain injuries (TBI) from all causes each year, and that such injuries are associated with the development of consequences that may persist for years after the injury, such as pain, psychiatric, neurological, motor, and neurobehavioral issues, as well as with an increased risk of neurodegeneration [1,2,3,4]. Among the possible underlying pathological mechanisms of these consequences is neuroinflammation, which is an inflammatory response within the central nervous system (CNS) thought to be mediated by the production of cytokines, chemokines, reactive oxygen species (ROS) and other secondary messengers [5]. Although neuroinflammation is considered an adaptive and essential response following acquired traumatic injuries, edema, demyelination, and cellular and axonal damage were found to be associated with excessive neuroinflammation in chronic TBI [6]. Furthermore, evidence suggests that neuroinflammation secondary to acquired traumatic injuries, such as TBI, could play a central role in the development of chronic pain and also several tauopathies [7,8], such as Alzheimer’s disease, Parkinson’s disease, and chronic traumatic encephalopathy [6,9]. In this context, whether neuroinflammation could potentially precipitate or even cause neurodegenerative processes requires special attention.
In parallel, an important factor associated with TBI is disrupted sleep [10,11,12,13,14,15,16,17]. A recent meta-analysis showed that 50% of individuals with TBI report sleep disturbances, whereas approximately one-third of these patients report a sleep disorder [14]. Some of the sleep disturbances reported by those individuals include increased need for sleep even up to 6 months following the injury, obstructive sleep apnea, insomnia, narcolepsy-like symptoms, excessive daytime sleepiness, fatigue, and circadian-rhythm disturbances [16]. The causes of sleep disturbances following a TBI vary considerably: some might occur because of changes in patients’ lifestyle, comorbidities caused by the trauma such as pain and mood changes, or CNS structural damage and pathophysiological mechanisms incurred following a TBI [11]. In addition, one cannot exclude the possibility that premorbid sleep disturbances were exacerbated by TBI. Given the known deleterious consequences of sleep disturbances on alertness, concentration, and vigilance, individuals experiencing sleep disturbances following traumatic injuries are also more prone to subsequent traumatic injuries [18]. Sleep disturbances are also associated with poor prognosis following TBI [14,16,19] as well as declining overall health [20]. Understanding the complex interaction between sleep and TBI is not only essential if we aim to design and implement new management strategies, but it may also be instrumental in understanding their potential mediating role on the development of TBI-prone chronic pain diseases and neuropsychiatric conditions. In that context, and based on emerging research, there is reason to believe that neuroinflammation could entail a promising mechanistic linkage underlying poor prognosis in TBI patients experiencing sleep disturbances [21,22].
In this state-of-the-art review, the objective is to explore the putative role of neuroinflammation from fundamental and clinical perspectives into the relationship between sleep and TBI, in particular to their complex interplay with TBI-prone chronic pain and other neuropsychiatric outcomes. For that purpose, the information is organized and grouped into three main sections: “State-of-the-art overview of mechanisms between TBI, neuroinflammation, and sleep”, where a global perspective on mechanisms and outcomes (including chronic pain) of the multifaceted relationship between these conditions is described; “Neuroinflammation and other neuropsychiatric outcomes in the context of sleep disturbances and TBI”, namely mood disorders, cognitive dysfunctions and neurodegeneration; and “Future directions for clinical practice: targeting neuroinflammation”, which include sleep and neuroinflammation specific possible management options.
2. State-of-the-Art Overview of Mechanisms between TBI, Neuroinflammation, and Sleep
2.1. Mechanisms of Neuroinflammation Following TBI
Following tissue or nerve injury caused by a fracture or a TBI, a series of reactions generated by the body are triggered to allow the rapid return to homeostasis [23,24]. This inflammatory process can, in some cases, lead to an excessive and prolonged immune response, thus triggering a complex cascade of events such as chronic inflammation of the CNS (i.e., neuroinflammation) [25,26,27].
In acute and subacute neuroinflammation, microglia, which are the resident macrophages of the CNS, actively monitor the brain microenvironment and react when they encounter various elements of the CNS such as injured cells and pathogens, following TBI [5,28]. In response, microglia become activated and release cytokines (IL-1β, IL-6, TNF-a), nitric oxide (NO), and ROS, which are considered proinflammatory mediators [29]. This release leads to an acute neuroinflammatory response that is postulated to be beneficial to the CNS, in order to clear cellular debris via phagocytosis [28]. The resolution of the neuroinflammatory process is mediated by anti-inflammatory cytokines and the release of anti-inflammatory lipid mediators such as lipoxins, resolvins and neuroprotectins [28]. However, a neuroinflammatory response that persists over time may be detrimental and ultimately lead to neuronal death [30].
A growing body of evidence suggests that microglial activation is associated with synaptic dysfunction/dysregulation, mostly by altering long-term potentiation (LTP) [27]. These LTP, in turn, affect cognitive function, in particular long-term memory [9]. Synaptic dysfunction was also found to precede neuronal pathology such as tauopathies [31], and thus, such that neuroinflammation could be involved in both the onset and the progression of neurodegenerative diseases [6]. For instance, recent animal studies showed that rather than simply activating microglia, neuroinflammation can induce an exaggerated microglial response within the CNS thus “priming”, the inflammatory system for an increased vulnerability to a “second hit”, consequently favoring subsequent neuropsychiatric and neurodegenerative complications [32,33]. This inappropriate neuroinflammatory response activates several self-propagating cycles, causing apoptosis, synaptic dysfunction, impaired regeneration and the production of amyloid-beta (Aβ) and phosphorylated tau, thereby exacerbating behavioral and cognitive impairments [32].
2.2. TBI and Neuroinflammation
Brain damage related to the mechanical force applied to the brain in TBI is referred to as the primary insult (i.e., skull fractures, intracranial hematoma, lacerations, and contusions, diffuse axonal injury) [34]. The secondary insult refers to ischemia caused by various mechanisms, including intracranial hypertension, that compromise the balance between oxygen delivery to neurons and cerebral oxygen consumption [34]. It generates complex and interrelated neurochemical changes, including an extracellular increase in excitatory amino acids, ROS production, increased intracellular sodium and calcium concentration, mitochondrial dysfunction, and a long-lasting inflammatory response that may ultimately lead to cell death [34,35,36]. The significant activation of microglia, as part of the secondary insult, leads to the release of cytokines responsible for neuroprotection (anti-inflammatory process) and neurodestruction (toxic and pro-inflammatory process) [33,37,38]. The balance between the neuroprotective and neurodestructive components is precarious. When a misalignment between these two components occurs to the advantage of the latter, there is an increased risk of progressive brain damage that may persist and progress into chronic neurodegeneration [39]. Indeed, recent studies have found an increased levels of proteins involved in pathological processes of neurodegeneration, such as α-synuclein, Aβ, and tau in TBI patients, which play a major role in the development of neurodegenerative diseases such as Parkinson’s and Alzheimer’s diseases [40,41,42,43]. Given the high prevalence of TBI across the lifespan, understanding the complex interaction between neuroinflammation and its associated neurodegenerative processes is essential to improve patients’ clinical outcomes.
Regarding polytrauma (i.e., the simultaneous traumatic injury of several regions of the body), numerous studies have shown a high incidence of TBI in individuals who have suffered orthopedic trauma, which is not surprising considering that they both share similar causative events (accidental falls, motor vehicle accidents, and accidents in a recreational setting) [44,45]. Therefore, the anatomical proximity of the upper extremities to the head is such that these two types of acquired traumatic injuries inevitably share somewhat comparable biomechanical characteristics [46]. Consequently, the occurrence of a polytrauma brings its share of challenges due to the overlapping pathophysiological mechanisms common to both injuries and their possible interactions. Indeed, the permeability of the blood–brain barrier (BBB) following a TBI facilitates peripheral factors to invade the CNS [47]. Thus, pro-inflammatory cytokines, such as IL-6, IL-1β, and TNF-α, released following a peripheral lesion lead to a significant increase in systemic inflammation [24,35]. Therefore, patients with a TBI and a concomitant peripheral injury are potentially at greater risk for an exacerbation of the ongoing neuroinflammatory response than patients with an isolated TBI or peripheral injury [48]. The latter becomes specially relevant in the context of chronic pain development, as the risk of neural sensitization is increased by the possibility of both peripheral and central neuroinflammation, which may be driving the onset of post-traumatic conditions such as post-traumatic headache and complex regional pain syndrome [49,50,51].
Importantly, attention needs to be directed toward pediatric populations as well, as childhood and adolescence is a time of elevated risk for TBI [52], and prognosis and treatment responses may differ from adults due to the neuronal and brain network developmental status [53,54]. For instance, TBI can influence hippocampal neuro-genesis, which can increase the risk of developing adult neurological and neurodegenerative diseases [55,56]. A recent large-scale study using diffusion-weighted imaging showed that children with persistent post-concussive symptoms (more than 6 months following mild TBI) had more white matter microstructural changes than those with less persistent symptoms or mild orthopedic injury, suggesting more neuroinflammation and axonal swelling [57]. Hence, future research on this population is encouraged, as one might suspect augmented risk for neurocognitive alterations, especially in cases where neuroinflammation persists.
2.3. TBI and Sleep
Sleep–wake disturbances, including excessive daytime sleepiness, fatigue, and insomnia, are frequently reported by patients with TBI [58], and actually patients with TBI are at higher risk of developing chronic sleep–wake disturbances [11,59]. These disturbances can occur immediately after the TBI and tend to persist over time, as longitudinal studies have reported these symptoms are presents 6 months, 12 months, and even 3 years after the TBI [11,60,61,62,63]. For instance, a meta-analysis in patients with chronic TBI (>6 months post-injury) showed that moderate-severe TBI was associated with elevated slow wave sleep (SWS), reduced stage 2, and reduced sleep efficiency [15], and a recent retrospective cohort study in war veterans, with a median follow-up rate of 8.4 years, showed that TBI was associated with insomnia at follow-up when compared with patients without TBI (hazard ratio = 2.07; 95%) [64]. Indeed, insomnia following mild TBI seems to be common and perhaps among the main causes of disability in these patients [65,66], and relevant factors such as female sex, black race, history of psychiatric illness, and intracranial injuries seem to lead towards different insomnia trajectories [67]. Another sleep-related consequence of TBI is increased sleepiness, especially in early stages, and research has highlighted the damage of orexin/hypocretin neurons, whose activation involve wakefulness, as a possible contributor of the association between this association [68]. For example, a study revealed that TBI patients in the acute stage of severe TBI showed increased sleep duration and earlier sleep onset, perhaps suggesting that in the short-term the injured brain enhances sleep need and/or decreases the ability to maintain wakefulness [69]. Importantly, mood disorders (e.g., anxiety and depression), which are also associated with neuroinflammation, have been suggested as potential mediators of this association, and as with many other chronic conditions, it is very difficult to disentangle their role and their respective contribution in sleep–wake disorders following TBI [58,70].
2.4. Inflammation and Neuroinflammation Regulates Sleep
In the healthy brain, experimental studies have shown that inflammatory levels, whether peripheral or within the CNS, affect sleep regulation [71,72]. Cytokines are thought to be among the main effectors linking sleep and inflammation: in fact, IL-1β and TNF-α are sleep regulatory cytokines known to promote longer and deeper sleep. Overexpression of IL-1β and TNF-α following TBI is therefore thought to at least partially contribute to the heightened need for sleep following an injury [73]. Although their effects are smaller, other cytokines and prostaglandins also display sleep regulatory properties [71]. In the daytime, inflammatory levels are associated with fatigue and sleepiness [74]. However, some of these effects seem to be level dependent, where an inverse relation can be observed at higher levels, with high pro-inflammatory cytokines levels being associated with disrupted and fragmented sleep [75]. This observation might partly explain why many chronic inflammatory diseases are associated with sleep disturbances [71]. For instance, in a population with high inflammation and depression, the administration of a TNF blockade significantly improved sleep consolidation [76].
Recent studies show that microglia could play a key mediating role on sleep regulation through their production of sleep regulatory cytokines [77]. Moreover, microglia morphology, phagocytosis activity, and their gene expression were also shown to follow circadian variations [78,79]. Therefore, the normal circadian release of cytokines might contribute to sleep regulation. However, in a study that administered minocycline to attenuate microglial activation in mice that underwent sleep deprivation, a suppression of the normal increase in sleep depth was observed, which did not seem to be mediated by changes in cytokines transcription [80]. These findings suggest that microglial activation play a role in sleep regulation following acute sleep deprivation. Interestingly, animal research has suggested that the duration of post-traumatic sleep is a period that may define vulnerability for a repeated brain injury, which could be more related to glial activation rather than orexin neurons damage [81]. Although it remains unclear as to how exactly neuroinflammation regulates sleep, particularly in clinical populations, current hypotheses include the modulation of synaptic transmission affecting sleep [82,83], and damage to sleep regulatory structures in the brain, such as the thalamus, pituitary, hypothalamus, and brainstem, leading to sleep disturbances and disorders [84]. Alternatively, activated microglia might affect sleep–wake cycles through alterations of hypothalamic neurons that produces hypocretin [77], leading to narcolepsy-like symptoms such as excessive sleepiness, heightened sleep propensity, and disrupted nocturnal sleep. Taken together, current evidence suggest that microglial function regulates sleep, identifying neuroinflammatory processes as potential causes of sleep disturbances in TBI [85]. Furthermore, it seems that the characterization of sleep after TBI is essential to understand better the development of different neuropsychiatric outcomes [86,87].
2.5. Sleep Affects Inflammatory and Neuroinflammatory Processes
Sleep occupies approximately one-third of our lives and plays a central role in maintaining physiological homeostasis. Sleep is also crucial to TBI recovery as it is involved in metabolic and autonomic regulation [72,88,89,90], synaptic plasticity [91,92], memory consolidation [93] and other cognitive functions [94,95], mood regulation [96], as well as glymphatic clearance of metabolites from the brain [97,98]. In addition, sleep is an important regulator of the immune system [71,72]. It comes as no surprise that disturbed sleep has been shown to affect inflammation [71,72,99]. However, the inflammatory response to sleep loss can change depending on the chronicity: acute sleep deprivation results in lower IL-6, IL-1β, and TNF-α levels, whereas prolonged sleep restriction leads to elevated cytokines levels and increased inflammatory gene expression [71]. Sleep disturbances as well as short sleep duration have been associated with elevated inflammatory markers [100]. In patients with insomnia, the presence of short sleep, sleep fragmentation, and reduced slow-wave sleep were associated with higher inflammasome levels [101]. Sleep loss has also been shown to impact neuroinflammation and microglia. In many animal models, acute and chronic sleep loss generally affects microglial morphology, gene expression, activation [78]. After both chronic sleep loss and/or restriction in mice, microglial activation as well as microglial and astrocytic phagocytosis of synaptic components were observed, which may be a response to higher synaptic activity associated with prolonged wakefulness [102]. The authors suggested that sleep loss promotes “housekeeping” of heavily used synapses to downscale them, but these processes might also result in enhanced susceptibility to brain damage. Furthermore, it has been postulated that stress and poor sleep can trigger glial overactivation and a subsequent low-grade neuroinflammatory state, characterized by high levels of IL-1β and TNF-α, which, in turn, increases the excitability of CNS neurons through mechanisms such as long-term potentiation and increased synaptic efficiency [103].
Peripheral inflammation can also lead to neuroinflammation in the context of poor sleep [104,105]. Chronic sleep loss and sleep disorders such as obstructive sleep apnea have been associated with compromised BBB [106,107], and could result in an increased invasion of peripheral immune cells and cytokines into the CNS, thus contributing to neuroinflammation. One study used a 3-day sleep deprivation protocol in rats, and observed that sleep loss was associated with a cascade of pathological mechanisms, including exacerbated cortisol levels suggestive of a hypothalamic–pituitary–adrenal (HPA) response, altered circadian oscillations of clock genes expression, disrupted BBB integrity and microglial activation with elevated pro-inflammatory cytokines levels (IL-6, IL-1β, and TNF-α) [108].
Overall, sleep disturbances may contribute to poor health outcomes partly through detrimental chronic inflammation that can perpetuate tissue damage [84], which could exacerbate TBI-related inflammation and neuronal damage. Taken together, these recent findings highlight the bidirectional relationship between sleep–wake cycles and neuroinflammation. In the context of TBI, we hypothesize that the occurrence of sleep disturbances could be caused in part by neuroinflammatory processes following the trauma, which then, in turn, could synergically promotes neuroinflammatory-related tissue damage.
2.6. Neuroinflammation and Chronic Pain in the Context of Sleep Disturbances and TBI Chronic Pain
A common consequence of both TBI and poor sleep is chronic pain (i.e., pain lasting longer than 6 months). The interaction between sleep and pain problems is complex and likely bidirectional [109], and the most common pain condition after TBI appears in the form of headache, nowadays named persistent headache attributed to traumatic injury to the head [110,111]. The prevalence of persistent post-traumatic headache is as high as 57.8% (95% confidence interval [CI], 55.5–60.2%) across different time points [112]. In addition to headache, the onset of pain after TBI has also been reported in the neck, in the shoulders, or in the upper limbs [113]. In fact, TBI is accompanied by another pain diagnosis in more than 40% of cases [45], and in moderate-to-severe TBI, musculoskeletal complaints (stiffness and aching in joints) are present in 79% of patients assessed, more than 15 years after trauma [114]. While different potential underlying mechanisms have been identified, a possible underlying mechanism to the sleep and pain interaction relates to inflammatory processes (low grade inflammation or neuroinflammation) [71,115,116,117]. Accordingly, a recent study highlighted the role of IL-6 in the development of pathological pain, whose receptors seemed to be elevated in the spinal cord and nerve root ganglia in chronic pain states [118]. In addition, prostaglandins, other cytokines such as IL-1 as well as TNF are considered important pronociceptive factors that could mediate the association between sleep loss and increased pain in the context a chronic pain condition, such as post-traumatic headache. Moreover, it seems that melatonin, an endogenous substance produced in the pineal gland that is mainly associated with sleep–wake circadian regulation, is also linked with suppressing pain and inflammation [119]. Indeed, low melatonin has been postulated as a potential moderator for the association between chronic pain, sleep architecture, and immunometabolic traffic, as it can downregulate inflammatory mediators including prostaglandins and cytokines [119]. A recent review also highlighted the lower levels of melatonin on neuroinflammation and oxidative stress resulting from TBI [120], and a pre-clinical study among severe TBI patients found lower serum melatonin levels in the surviving patients [121]. It has also been shown that individuals with pain and mild TBI may need more time to sleep, and the authors concluded that pain could be associated with more pronounced sleep need in these individuals [122].
Additionally, yet not specifically related to trauma populations, other clinical studies have also found peripheral deficiencies compatible with neuroinflammation in pain syndromes such as fibromyalgia [123], where sleep disturbances are present in most of the cases [103]. Hence, the activation of microglia and astrocytes seems to be critical in the development of most chronic pain conditions [103,124].
3. Neuroinflammation and Other Neuropsychiatric Outcomes in the Context of Sleep Disturbances and TBI
3.1. Mood
TBI, sleep and pain are all major risk factors for mental health disorders such as anxiety or depression [125,126]. Interestingly, these frequent long-term consequences of traumatic injuries share neuroinflammation among key pathophysiological mechanisms [58,127,128,129]. According to a recent systematic review [130], the presence of depressive and/or anxiety symptoms in TBI samples was found to be associated with higher concentrations of serum and CSF, CRP, CSF-derived markers of sVCAM-1, sICAM-1, and sFAS, and IL-10, IL-8, IL-6, and TNF-α. Acute measures of some of these biomarkers predicted the onset of depression at 6 and 12 months post-injury.
Robust animal evidence has linked sleep deprivation to depression and anxiety-like behaviors partly through neuroinflammatory processes [21,108,131,132]. Following sleep deprivation in mice that underwent a TBI, lower corticosterone, enhanced neuroinflammation, exacerbated evidence of neuronal injury, and anxiety-like behaviors were observed as compared to brain-injured mice without sleep deprivation [21].
Taken together, traumatic injuries seem to interact with sleep disturbances in the installation of persistent trauma-related sequelae affecting mood, potentially through shared neuroinflammatory processes.
3.2. Cognitive Dysfunctions and Neurodegeneration
Neuroinflammation is now recognized as a key pathological mechanism to cognitive aging, neurodegeneration and Alzheimer’s disease [133]. Meta-analyses have concluded that both sleep disturbances and TBI are risk factors for cognitive decline and incident dementia [7,134,135]. There is increasing evidence suggesting that sleep disturbances interact and/or contributes to peripheral inflammation as well as neuroinflammation to predict cognitive dysfunctions and dementia risk. For instance, inflammatory levels have been shown to moderate the association between sleep disturbances and obstructive sleep apnea with dementia risk [136,137]. In animal models, sleep deprivation or fragmentation lead to cognitive dysfunctions and neurodegenerative processes, at least partly through its effect on neuroinflammation (microglial activation, cytokines production, complement activation) [104,132,138,139]. In mice, one group used a 2-month chronic sleep fragmentation protocol, which resulted in the activation of microglia, endosome-autophagosome-lysosome pathway dysfunction, cortical and hippocampal Aβ accumulation, spatial learning and memory impairments, and anxiety-like behaviors [132]. In sleep deprived rats, inhibiting microglial activation mitigated spatial memory impairments, reduced deleterious effects on neurogenesis and gliosis in the hippocampus, and promoted anti-inflammatory cytokines over pro-inflammatory cytokines [139], supporting the causal role of microglial activation in sleep deprivation-induced cognitive dysfunction. Alternatively, sleep disturbances can also directly promote neurodegenerative processes through other mechanisms, such as a lower metabolic clearance of Aβ via the glymphatic system [97]. Interestingly, convincing evidence indicates that neuroinflammation could effectively modulate neurogenesis at different stages, including proliferation, differentiation, migration, survival of newborn neurons, maturation, synaptogenesis, and neuritogenesis among others [140]. Finally, a recent TBI study concluded that post-injury sleep fragmentation engages the dysfunctional post-injury HPA axis, enhances inflammation, and compromises hippocampal function [141]. The latter study suggested that external stressors that disrupt sleep have an integral role in mediating outcome after brain injury. Thus, both systemic inflammation and neuroinflammation can alter adult hippocampal neurogenesis in neurodegenerative disorders. For a more detailed an extensive review in The Dialogue Between Neuroinflammation and Adult Neurogenesis, please see [140].
Following a TBI, accumulating evidence is showing that neuroinflammation contributes to initial neuronal damage and cognitive dysfunction, but also long-term cognitive impairments, neurodegeneration, and risk of developing dementia [8,84,142]. After a single TBI, patients show evidence of white matter degeneration and persistent neuroinflammation up to 18 years post-injury [143]. In a mouse model of TBI, the neuroinflammatory response was found to drive synaptic degeneration and cognitive decline, which was abolished by complement inhibition, suggesting causality [144]. In humans, concomitant tau aggregation and neuroinflammation was observed using neuroimaging in mild TBI patients [41]. Moreover, it has been reported that TBI can also augment the formation of amyloid-b plaques and tau neurofibrillary tangles (NFTs) through inflammation-dependent gene expression and transcription factor activation, which could, in turn, produce sleep disturbances. Importantly, NFTs are another crucial feature of Alzheimer’s disease [84].
Taken together, these findings suggest that the feedback positive loop between TBI, sleep disturbances and neuroinflammation can result in further cognitive dysfunctions and even neurodegeneration.
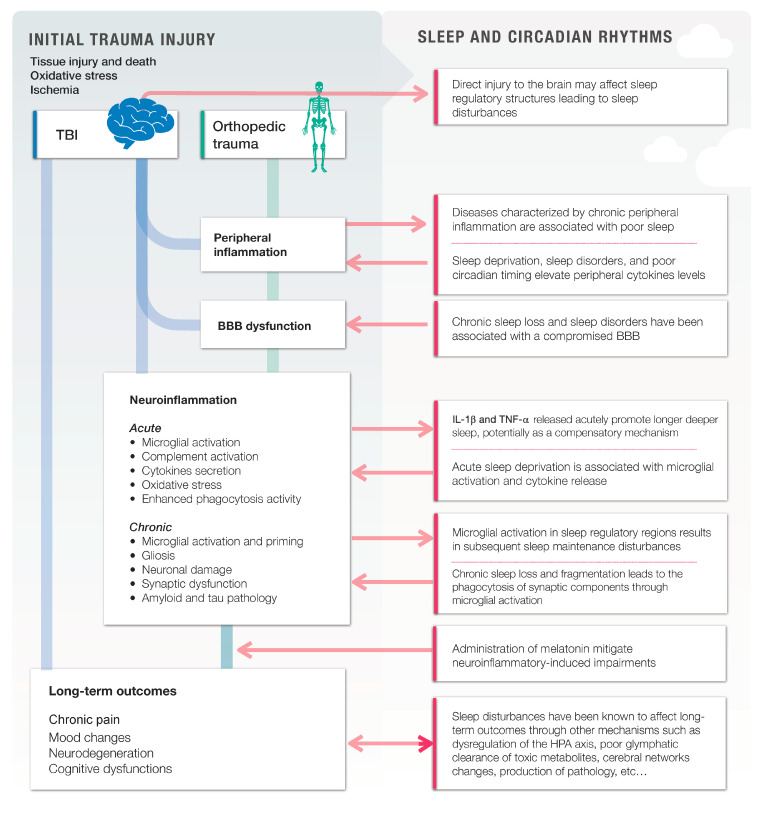
A summary of the abovementioned interactions and mechanisms can be observed in Figure 1.
Figure 1.
The putative role of neuroinflammation in the acquired traumatic injuries and related sleep disturbances. Traumatic brain injuries (TBI) and orthopedic traumas (OT) both lead to a downstream pathophysiological cascade that includes peripheral inflammation, blood–brain barrier (BBB) dysfunction, and neuroinflammation. In turn, chronic neuroinflammation plays a role into the development of poor long-term outcomes. At each step of the way, sleep and sleep disturbances interact bidirectionally with traumatic pathological mechanisms and neuroinflammation. Poorer sleep exacerbates peripheral inflammation, BBB dysfunction, neuroinflammation, and worsen long-term outcomes. On the other hand, the trauma itself, its comorbidities, or neuroinflammation affect sleep regulation, which leads to a positive feedback loop, where neuroinflammation and sleep interact together to affect long-term outcomes following an injury.
4. Future Directions for Clinical Practice: Targeting Neuroinflammation
4.1. Sleep as a Therapeutic Target to Inhibit Neuroinflammation
Many sleep disturbances and disorders are treatable, often using non-pharmaceutical therapeutic strategies, thereby make it an appealing treatment target in order to reduce trauma-related neuroinflammation and improve patients’ lives [115]. Cognitive behavioral therapy (CBT), the gold-standard treatment for insomnia, has proven to be an efficient way of improving sleep quality and restoring inflammatory levels [145,146,147]. CBT has also proven effective in TBI patients and show promise for mitigating patients’ inflammation-related symptoms such as depression, anxiety and pain [148], along with other non-pharmaceutical strategies such as blue light therapy, problem solving treatment, and combined sleep hygiene interventions [149]. Moreover, in addition to sleep, CBT can also be directed towards pain and other associated disorders such as depression and anxiety in a hybrid approach. Hybrid CBT has shown promising results and it can also be carried out online to improve treatment compliance [150,151,152].
Although sleep medications, such as benzodiazepines, hypnotics, and sedating antidepressants, could help treat sleep disturbances, especially in the short term, and thereby have the potential to reduce neuroinflammation and TBI’s related consequences linked to poor sleep [153], this remains to be investigated thoroughly and cautiously. Although still controversial, usage of sleeping pills has been associated with elevated risk of incident dementia [154,155], Moreover, sleeping medications generally perform worse than behavioral techniques such as CBT in treating sleep disturbances in the long term [156].
Nonetheless, a sleep aid with interesting potential is melatonin, as it has been associated with the inhibition of excessive microglial activation [157]. In addition to its endogenous secretion at night promoting adequate sleep–wake cycles, melatonin is also available as a dietary supplement. Among the proposed mechanisms underlying melatonin’s downregulating action on microglial activation is through its role as an antioxidant, therefore reducing ROS [157]. It is also possible that melatonin supplementation could help reduce neuroinflammation through its effect on sleep regulation, although this remains to be confirmed. Interestingly, animal models showed that melatonin administration increased bone fracture healing [158], reduced neuroinflammation and promoted neuroprotection following a TBI [159,160]. In patients that sustained a TBI, a meta-analysis showed that melatonin has a positive effect on pathological findings, neurological status, neurobehavioral outcomes, and cognition [161]. However, it needs to be highlighted that the majority of the included studies were in animal models (i.e., 15 studies in animal models and two in human populations), and that the included human studies were considered to have low quality and were of uncertain significance. Furthermore, a recent randomized clinical trial in a pediatric population with mild TBI (n = 99) showed no significant difference in post-concussive symptoms between the use of melatonin at two different dosages (i.e., 3 and 10 mg) and placebo [162], yet a secondary analysis as per protocol of these data showed some improvements in sleep symptoms with melatonin [163]. Therefore, although there is evidence supporting the use of melatonin treatment after TBI to improve different behavioral and pathological outcomes based on animal models, data remain equivocal in human clinical populations.
4.2. Specifically Targeting Neuroinflammation to Improve Sleep and Trauma-Related Outcomes
Given its relevance and repercussions in different ambits of health, treating neuroinflammation emerges as a critical goal in the management of traumatically injured patients. Whereas peripheral neuroinflammation might be initially targeted with common anti-inflammatory medications, aiming to act on neuroinflammatory processes is much more complex, as some anti-inflammatories can disturb sleep as well, microglia appears as a primary treatment target for novel therapeutics aiming to tackle neuroinflammatory processes, including its selective abolition in animal models [164,165], or being targeted by nanoparticles [166]. Moreover, there are already several inhibitors of TNF-α and IL-1β that are available for clinical use, yet none of them are exempt of potentially serious side effects [167,168]. In addition, the use of psychedelics is receiving again a lot of attention in recent years due to its powerful properties to treat pain and mood disorders, as they have shown potential neuro-restorative effects and anti-neuroinflammatory and pro-immunomodulatory actions [169,170]. Indeed, the effects of some of these compounds is currently being studied in sleep as well [171]. Nonetheless, more development in this line of investigation is needed in the future. For a more detailed summary of pharmacological therapies on TBI, please refer to a recent review of phase 3 clinical trials on this population [172], which highlights key targets for future research.
An important non-pharmacological treatment option is exercise, given that exercise increases astrocytic activation, more specifically glial fibrillary acidic protein expression in hippocampal astrocytes in the stratum radiatum, a region that contains numerous astrocytes and is relevant for learning and memory [103,173]. Exercise is known to become anti-inflammatory or neuroprotective in several neuroinflammatory diseases. It is possible that exercise also reduces gliosis and glial proliferation [103]. Moreover, via its action on CNS glial cells, regular aerobic exercise has been shown to provide an adaptive advantage against perturbations to homeostasis, such as immunological challenge or ageing in animal models [174]. A systematic review and meta-analysis involving 13 RCTs and 514 participants, revealed that physical activity had positive effects on decreasing TNF-α and CRP (pro-inflammatory), while significantly improving BDNF and IGF-1 (neuroprotective) [175]. Furthermore, exercise is a great option for several sleep disorders including insomnia or sleep apnea [176,177], as it can regular cortisol, release endorphins, and decrease fat among others.
Non-pharmacological integrative approaches including mind/body therapies such as yoga, breathing exercises, meditation, all of them being associated with sleep quality improvement as well, have also been demonstrated to reduce pro-inflammatory cytokines and have proved some positive effects on depression, anxiety, cognition, and pain [178]. Moreover, several plant-based interventions (herbs/spices) currently under investigation [179]. While their non-invasiveness and harmless nature make them appealing as supportive therapy, more research is needed before obtaining any firm conclusion regarding their efficacy.
Other emerging techniques that can be used to target pain and sleep disorders, and specifically neuroinflammation, are non-invasive brain stimulation techniques, such as repetitive transcranial magnetic stimulation (rTMS) [180,181]. In different animal studies, rTMS reduced neuroinflammation by modulating astrocytes and microglia activity, reducing TNF-α, and increasing GABA, which can control excitotoxicity [182,183,184,185]. Additionally, clinical rTMS studies showed increases in serum GABA and BDNF in patients with chronic insomnia [186]. Thus, rTMS could be used not only to manage chronic pain patients but also to reduce their transition to chronicity by tackling the underlying neuroinflammatory mechanisms [115,185], which becomes especially relevant when applied to traumatically injured patients. While other techniques such as transcranial direct current stimulation, transcranial alternating current stimulation or vagal nerve stimulation hold potential in treating neuroinflammation [181,187], research is still lacking.
5. Conclusions
While the innate immune response following a TBI is necessary for recovery, its often prolonged and excessive nature contributes, paradoxically, to worsen outcomes. In that way, TBI leads to a state of peripheral/central neuroinflammation, which can be associated with sleep disturbances. Additionally, TBI and sleep disturbances also exacerbate the neuroinflammatory state, complicating these deleterious interactions even more, and potentially all leading to mood disorders, pain, cognitive deficits and neurodegeneration states. Importantly, finding treatment strategies, such as treating sleep disturbances or using non-invasive brain stimulation to reduce or modulate pro-inflammatory processes, can be useful in order to help TBI patients’ physiological, psychological and cognitive health.
Acknowledgments
We would like to acknowledge Gabrielle Beetz, for her initial contribution to the article and development of the original figure, and specially to the Chaire de recherche de la Fondation Caroline Durand en traumatologie aigue de l’Université de Montréal for their financial support to the project.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was financially supported by the Foundation Caroline Durand Research Chair in Acute Traumatology of Université de Montréal (LDB) and Canada Research Chairs (GL). The first author (AHB) is funded by a Vanier Scholarship. Additionally, another author (LDB) was also supported by Applied Biomedical Research Program, Research Foundation Flanders (Fonds voor Wetenschappelijk Onderzoek Vlaanderen), Belgium (FWO-TBM project no. TBM2021-T000521N-54252, “Towards PREcision MEdicine for Osteoarthritis: Added value of cognitive behavioural therapy for insomnia (the PREMEO trial)”), and by the Strategic Research Program SRP90 (‘Pain Never Sleeps: Unravelling the Sleep-Pain Interaction in Patients with Chronic Pain’) funded by the research council of the Vrije Universiteit Brussel, Brussels, Belgium.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Bramlett H.M., Dietrich W.D. Long-Term Consequences of Traumatic Brain Injury: Current Status of Potential Mechanisms of Injury and Neurological Outcomes. J. Neurotrauma. 2015;32:1834–1848. doi: 10.1089/neu.2014.3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson L., Stewart W., Dams-O’Connor K., Diaz-Arrastia R., Horton L., Menon D.K., Polinder S. The chronic and evolving neurological consequences of traumatic brain injury. Lancet Neurol. 2017;16:813–825. doi: 10.1016/S1474-4422(17)30279-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martins H.A.L., Martins B.B.M., Ribas V.R., Bernardino S.N., de Oliveira D.A., Silva L.C., Sougey E.B., Valenca M.M. Life quality, depression and anxiety symptoms in chronic post-traumatic headache after mild brain injury. Dement. Neuropsychol. 2012;6:53–58. doi: 10.1590/S1980-57642012DN06010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leng Y., Byers A.L., Barnes D.E., Peltz C.B., Li Y., Yaffe K. Traumatic Brain Injury and Incidence Risk of Sleep Disorders in Nearly 200,000 US Veterans. Neurology. 2021;96:e1792–e1799. doi: 10.1212/WNL.0000000000011656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DiSabato D.J., Quan N., Godbout J.P. Neuroinflammation: The devil is in the details. J. Neurochem. 2016;139((Suppl. S2)):136–153. doi: 10.1111/jnc.13607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guzman-Martinez L., Maccioni R.B., Andrade V., Navarrete L.P., Pastor M.G., Ramos-Escobar N. Neuroinflammation as a Common Feature of Neurodegenerative Disorders. Front. Pharmacol. 2019;10:1008. doi: 10.3389/fphar.2019.01008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perry D.C., Sturm V.E., Peterson M.J., Pieper C.F., Bullock T., Boeve B.F., Miller B.L., Guskiewicz K.M., Berger M.S., Kramer J.H., et al. Association of traumatic brain injury with subsequent neurological and psychiatric disease: A meta-analysis. J. Neurosurg. 2016;124:511–526. doi: 10.3171/2015.2.JNS14503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collins-Praino L.E., Corrigan F. Does neuroinflammation drive the relationship between tau hyperphosphorylation and dementia development following traumatic brain injury? Brain Behav. Immun. 2017;60:369–382. doi: 10.1016/j.bbi.2016.09.027. [DOI] [PubMed] [Google Scholar]
- 9.Lyman M., Lloyd D.G., Ji X., Vizcaychipi M.P., Ma D. Neuroinflammation: The role and consequences. Neurosci. Res. 2014;79:1–12. doi: 10.1016/j.neures.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 10.Castriotta R.J., Wilde M.C., Lai J.M., Atanasov S., Masel B.E., Kuna S.T. Prevalence and consequences of sleep disorders in traumatic brain injury. J. Clin. Sleep Med. 2007;3:349–356. doi: 10.5664/jcsm.26855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duclos C., Dumont M., Wiseman-Hakes C., Arbour C., Mongrain V., Gaudreault P.O., Khoury S., Lavigne G., Desautels A., Gosselin N. Sleep and wake disturbances following traumatic brain injury. Pathol. Biol. 2014;62:252–261. doi: 10.1016/j.patbio.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 12.Mollayeva T., D’Souza A., Mollayeva S. Sleep and Psychiatric Disorders in Persons With Mild Traumatic Brain Injury. Curr. Psychiatry Rep. 2017;19:47. doi: 10.1007/s11920-017-0800-z. [DOI] [PubMed] [Google Scholar]
- 13.Ouellet M.C., Beaulieu-Bonneau S., Morin C.M. Insomnia in patients with traumatic brain injury: Frequency, characteristics, and risk factors. J. Head Trauma Rehabil. 2006;21:199–212. doi: 10.1097/00001199-200605000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Mathias J.L., Alvaro P.K. Prevalence of sleep disturbances, disorders, and problems following traumatic brain injury: A meta-analysis. Sleep Med. 2012;13:898–905. doi: 10.1016/j.sleep.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 15.Mantua J., Grillakis A., Mahfouz S.H., Taylor M.R., Brager A.J., Yarnell A.M., Balkin T.J., Capaldi V.F., Simonelli G. A systematic review and meta-analysis of sleep architecture and chronic traumatic brain injury. Sleep Med. Rev. 2018;41:61–77. doi: 10.1016/j.smrv.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Sandsmark D.K., Elliott J.E., Lim M.M. Sleep-Wake Disturbances After Traumatic Brain Injury: Synthesis of Human and Animal Studies. Sleep. 2017;40 doi: 10.1093/sleep/zsx044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang H., Liu Y.J., Ye J.L., Zhao L.H., Li L.L., Hou X.L. Evaluation of sleep disorder in orthopedic trauma patients: A retrospective analysis of 1129 cases. J. Orthop. Surg. Res. 2021;16:344. doi: 10.1186/s13018-021-02487-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen T.Y., Lee S., Buxton O.M. A Greater Extent of Insomnia Symptoms and Physician-Recommended Sleep Medication Use Predict Fall Risk in Community-Dwelling Older Adults. Sleep. 2017;40:zsx142. doi: 10.1093/sleep/zsx142. [DOI] [PubMed] [Google Scholar]
- 19.Wickwire E.M., Albrecht J.S., Griffin N.R., Schnyer D.M., Yue J.K., Markowitz A.J., Okonkwo D.O., Valadka A.B., Badjatia N., Manley G.T. Sleep disturbances precede depressive symptomatology following traumatic brain injury. Curr. Neurobiol. 2019;10:49–55. [PMC free article] [PubMed] [Google Scholar]
- 20.Beetz G., Babiloni A.H., Jodoin M., Charlebois-Plante C., Lavigne G.J., De Beaumont L., Rouleau D.M. Relevance of sleep disturbances to orthopedic surgery: A current concepts narrative and practical review. J. Bone Jt. Surg. Am. 2021;103:2045–2056. doi: 10.2106/JBJS.21.00176. [DOI] [PubMed] [Google Scholar]
- 21.Tapp Z.M., Kumar J.E., Witcher K.G., Atluri R.R., Velasquez J.A., O’Neil S.M., Dziabis J.E., Bray C.E., Sheridan J.F., Godbout J.P., et al. Sleep Disruption Exacerbates and Prolongs the Inflammatory Response to Traumatic Brain Injury. J. Neurotrauma. 2020;37:1829–1843. doi: 10.1089/neu.2020.7010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sulhan S., Lyon K.A., Shapiro L.A., Huang J.H. Neuroinflammation and blood-brain barrier disruption following traumatic brain injury: Pathophysiology and potential therapeutic targets. J. Neurosci. Res. 2020;98:19–28. doi: 10.1002/jnr.24331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ellis A., Bennett D.L. Neuroinflammation and the generation of neuropathic pain. Br. J. Anaesth. 2013;111:26–37. doi: 10.1093/bja/aet128. [DOI] [PubMed] [Google Scholar]
- 24.Pape H.C., Marcucio R., Humphrey C., Colnot C., Knobe M., Harvey E.J. Trauma-induced inflammation and fracture healing. J. Orthop. Trauma. 2010;24:522–525. doi: 10.1097/BOT.0b013e3181ed1361. [DOI] [PubMed] [Google Scholar]
- 25.Scholz J., Woolf C.J. The neuropathic pain triad: Neurons, immune cells and glia. Nat. Neurosci. 2007;10:1361–1368. doi: 10.1038/nn1992. [DOI] [PubMed] [Google Scholar]
- 26.Walker A.K., Kavelaars A., Heijnen C.J., Dantzer R. Neuroinflammation and comorbidity of pain and depression. Pharmacol. Rev. 2014;66:80–101. doi: 10.1124/pr.113.008144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Watkins L.R., Milligan E.D., Maier S.F. Glial proinflammatory cytokines mediate exaggerated pain states: Implications for clinical pain. Adv. Exp. Med. Biol. 2003;521:1–21. [PubMed] [Google Scholar]
- 28.Shabab T., Khanabdali R., Moghadamtousi S.Z., Kadir H.A., Mohan G. Neuroinflammation pathways: A general review. Int. J. Neurosci. 2017;127:624–633. doi: 10.1080/00207454.2016.1212854. [DOI] [PubMed] [Google Scholar]
- 29.Colton C.A. Heterogeneity of microglial activation in the innate immune response in the brain. J. Neuroimmune Pharmacol. 2009;4:399–418. doi: 10.1007/s11481-009-9164-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Varatharaj A., Galea I. The blood-brain barrier in systemic inflammation. Brain Behav. Immun. 2017;60:1–12. doi: 10.1016/j.bbi.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 31.Yoshiyama Y., Higuchi M., Zhang B., Huang S.M., Iwata N., Saido T.C., Maeda J., Suhara T., Trojanowski J.Q., Lee V.M. Synapse loss and microglial activation precede tangles in a P301S tauopathy mouse model. Neuron. 2007;53:337–351. doi: 10.1016/j.neuron.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 32.Cunningham C., Campion S., Lunnon K., Murray C.L., Woods J.F., Deacon R.M., Rawlins J.N., Perry V.H. Systemic inflammation induces acute behavioral and cognitive changes and accelerates neurodegenerative disease. Biol. Psychiatry. 2009;65:304–312. doi: 10.1016/j.biopsych.2008.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Witcher K.G., Eiferman D.S., Godbout J.P. Priming the inflammatory pump of the CNS after traumatic brain injury. Trends Neurosci. 2015;38:609–620. doi: 10.1016/j.tins.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Greve M.W., Zink B.J. Pathophysiology of traumatic brain injury. Mt. Sinai J. Med. 2009;76:97–104. doi: 10.1002/msj.20104. [DOI] [PubMed] [Google Scholar]
- 35.Lozano D., Gonzales-Portillo G.S., Acosta S., de la Pena I., Tajiri N., Kaneko Y., Borlongan C.V. Neuroinflammatory responses to traumatic brain injury: Etiology, clinical consequences, and therapeutic opportunities. Neuropsychiatr. Dis. Treat. 2015;11:97–106. doi: 10.2147/NDT.S65815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morganti-Kossmann M.C., Semple B.D., Hellewell S.C., Bye N., Ziebell J.M. The complexity of neuroinflammation consequent to traumatic brain injury: From research evidence to potential treatments. Acta Neuropathol. 2019;137:731–755. doi: 10.1007/s00401-018-1944-6. [DOI] [PubMed] [Google Scholar]
- 37.Wofford K.L., Loane D.J., Cullen D.K. Acute drivers of neuroinflammation in traumatic brain injury. Neural Regen. Res. 2019;14:1481–1489. doi: 10.4103/1673-5374.255958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nimmerjahn A., Kirchhoff F., Helmchen F. Resting microglial cells are highly dynamic surveillants of brain parenchyma in vivo. Science. 2005;308:1314–1318. doi: 10.1126/science.1110647. [DOI] [PubMed] [Google Scholar]
- 39.Gao H.M., Hong J.S. Why neurodegenerative diseases are progressive: Uncontrolled inflammation drives disease progression. Trends Immunol. 2008;29:357–365. doi: 10.1016/j.it.2008.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Acosta S.A., Tajiri N., de la Pena I., Bastawrous M., Sanberg P.R., Kaneko Y., Borlongan C.V. Alpha-synuclein as a pathological link between chronic traumatic brain injury and Parkinson’s disease. J. Cell Physiol. 2015;230:1024–1032. doi: 10.1002/jcp.24830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marklund N., Vedung F., Lubberink M., Tegner Y., Johansson J., Blennow K., Zetterberg H., Fahlstrom M., Haller S., Stenson S., et al. Tau aggregation and increased neuroinflammation in athletes after sports-related concussions and in traumatic brain injury patients - A PET/MR study. Neuroimage Clin. 2021;30:102665. doi: 10.1016/j.nicl.2021.102665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Uryu K., Chen X.H., Martinez D., Browne K.D., Johnson V.E., Graham D.I., Lee V.M., Trojanowski J.Q., Smith D.H. Multiple proteins implicated in neurodegenerative diseases accumulate in axons after brain trauma in humans. Exp. Neurol. 2007;208:185–192. doi: 10.1016/j.expneurol.2007.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tajiri N., Kellogg S.L., Shimizu T., Arendash G.W., Borlongan C.V. Traumatic brain injury precipitates cognitive impairment and extracellular Aβ aggregation in Alzheimer’s disease transgenic mice. PLoS ONE. 2013;8:e78851. doi: 10.1371/journal.pone.0078851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gross T., Schüepp M., Attenberger C., Pargger H., Amsler F. Outcome in polytraumatized patients with and without brain injury. Acta Anaesthesiol. Scand. 2012;56:1163–1174. doi: 10.1111/j.1399-6576.2012.02724.x. [DOI] [PubMed] [Google Scholar]
- 45.Jodoin M., Rouleau D.M., Charlebois-Plante C., Benoit B., Leduc S., Laflamme G.Y., Gosselin N., Larson-Dupuis C., De Beaumont L. Incidence rate of mild traumatic brain injury among patients who have suffered from an isolated limb fracture: Upper limb fracture patients are more at risk. Injury. 2016;47:1835–1840. doi: 10.1016/j.injury.2016.05.036. [DOI] [PubMed] [Google Scholar]
- 46.Rabinowitz A.R., Li X., Levin H.S. Sport and nonsport etiologies of mild traumatic brain injury: Similarities and differences. Annu. Rev. Psychol. 2014;65:301–331. doi: 10.1146/annurev-psych-010213-115103. [DOI] [PubMed] [Google Scholar]
- 47.McDonald S.J., Sun M., Agoston D.V., Shultz S.R. The effect of concomitant peripheral injury on traumatic brain injury pathobiology and outcome. J. Neuroinflammation. 2016;13:90. doi: 10.1186/s12974-016-0555-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Leong B.K., Mazlan M., Abd Rahim R.B., Ganesan D. Concomitant injuries and its influence on functional outcome after traumatic brain injury. Disabil. Rehabil. 2013;35:1546–1551. doi: 10.3109/09638288.2012.748832. [DOI] [PubMed] [Google Scholar]
- 49.Mayer C.L., Huber B.R., Peskind E. Traumatic brain injury, neuroinflammation, and post-traumatic headaches. Headache. 2013;53:1523–1530. doi: 10.1111/head.12173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jung Y.H., Kim H., Jeon S.Y., Kwon J.M., Lee W.J., Kim Y.C., Jang J.H., Choi S.H., Lee J.Y., Kang D.H. Brain Metabolites and Peripheral Biomarkers Associated with Neuroinflammation in Complex Regional Pain Syndrome Using [11C]-(R)-PK11195 Positron Emission Tomography and Magnetic Resonance Spectroscopy: A Pilot Study. Pain Med. 2019;20:504–514. doi: 10.1093/pm/pny111. [DOI] [PubMed] [Google Scholar]
- 51.Prasad Md A., Chakravarthy Md K. Review of complex regional pain syndrome and the role of the neuroimmune axis. Mol. Pain. 2021;17:17448069211006617. doi: 10.1177/17448069211006617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ryan E., Bolger T., Barrett M.J., Blackburn C., Okafor I., McNamara R., Molloy E.J. Paediatric Head Injury and Traumatic Brain Injury. Ir. Med. J. 2020;113:94. [PubMed] [Google Scholar]
- 53.Fraunberger E., Esser M.J. Neuro-Inflammation in Pediatric Traumatic Brain Injury-from Mechanisms to Inflammatory Networks. Brain Sci. 2019;9:319. doi: 10.3390/brainsci9110319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ashwal S., Siebold L., Krueger A.C., Wilson C.G. Post-traumatic Neuroinflammation: Relevance to Pediatrics. Pediatr. Neurol. 2021;122:50–58. doi: 10.1016/j.pediatrneurol.2021.04.010. [DOI] [PubMed] [Google Scholar]
- 55.Rizk M., Vu J., Zhang Z. Impact of pediatric traumatic brain injury on hippocampal neurogenesis. Neural Regen. Res. 2021;16:926–933. doi: 10.4103/1673-5374.297057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang Z., Ishrat S., O’Bryan M., Klein B., Saraswati M., Robertson C., Kannan S. Pediatric Traumatic Brain Injury Causes Long-Term Deficits in Adult Hippocampal Neurogenesis and Cognition. J. Neurotrauma. 2020;37:1656–1667. doi: 10.1089/neu.2019.6894. [DOI] [PubMed] [Google Scholar]
- 57.Ware A.L., Yeates K.O., Tang K., Shukla A., Onicas A.I., Guo S., Goodrich-Hunsaker N., Abdeen N., Beauchamp M.H., Beaulieu C., et al. Longitudinal white matter microstructural changes in pediatric mild traumatic brain injury: An A-CAP study. Hum. Brain Mapp. 2022;43:3809–3823. doi: 10.1002/hbm.25885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lavigne G., Khoury S., Chauny J.M., Desautels A. Pain and sleep in post-concussion/mild traumatic brain injury. Pain. 2015;156((Suppl. S1)):S75–S85. doi: 10.1097/j.pain.0000000000000111. [DOI] [PubMed] [Google Scholar]
- 59.Gosselin N., Tellier M. Patients with traumatic brain injury are at high risk of developing chronic sleep-wake disturbances. J. Neurol. Neurosurg. Psychiatry. 2010;81:1297. doi: 10.1136/jnnp.2010.222471. [DOI] [PubMed] [Google Scholar]
- 60.Imbach L.L., Valko P.O., Li T., Maric A., Symeonidou E.R., Stover J.F., Bassetti C.L., Mica L., Werth E., Baumann C.R. Increased sleep need and daytime sleepiness 6 months after traumatic brain injury: A prospective controlled clinical trial. Pt 3Brain. 2015;138:726–735. doi: 10.1093/brain/awu391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Baumann C.R., Werth E., Stocker R., Ludwig S., Bassetti C.L. Sleep-wake disturbances 6 months after traumatic brain injury: A prospective study. Pt 7Brain. 2007;130:1873–1883. doi: 10.1093/brain/awm109. [DOI] [PubMed] [Google Scholar]
- 62.Kempf J., Werth E., Kaiser P.R., Bassetti C.L., Baumann C.R. Sleep-wake disturbances 3 years after traumatic brain injury. J. Neurol. Neurosurg. Psychiatry. 2010;81:1402–1405. doi: 10.1136/jnnp.2009.201913. [DOI] [PubMed] [Google Scholar]
- 63.Saksvik S.B., Karaliute M., Kallestad H., Follestad T., Asarnow R., Vik A., Haberg A.K., Skandsen T., Olsen A. The Prevalence and Stability of Sleep-Wake Disturbance and Fatigue throughout the First Year after Mild Traumatic Brain Injury. J. Neurotrauma. 2020;37:2528–2541. doi: 10.1089/neu.2019.6898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Haynes Z.A., Collen J.F., Poltavskiy E.A., Walker L.E., Janak J., Howard J.T., Werner J.K., Wickwire E.M., Holley A.B., Zarzabal L.A., et al. Risk factors of persistent insomnia among survivors of traumatic injury: A retrospective cohort study. J. Clin. Sleep Med. 2021;17:1831–1840. doi: 10.5664/jcsm.9276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gosselin N., Duclos C. Insomnia following a mild traumatic brain injury: A missing piece to the work disability puzzle? Sleep Med. 2016;20:155–156. doi: 10.1016/j.sleep.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 66.Mollayeva T., Pratt B., Mollayeva S., Shapiro C.M., Cassidy J.D., Colantonio A. The relationship between insomnia and disability in workers with mild traumatic brain injury/concussion: Insomnia and disability in chronic mild traumatic brain injury. Sleep Med. 2016;20:157–166. doi: 10.1016/j.sleep.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 67.Wickwire E.M., Albrecht J.S., Capaldi V.F., II, Jain S.O., Gardner R.C., Werner J.K., Mukherjee P., McKeon A.B., Smith M.T., Giacino J.T., et al. Trajectories of Insomnia in Adults After Traumatic Brain Injury. JAMA Netw. Open. 2022;5:e2145310. doi: 10.1001/jamanetworkopen.2021.45310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Baumann C.R., Bassetti C.L., Valko P.O., Haybaeck J., Keller M., Clark E., Stocker R., Tolnay M., Scammell T.E. Loss of hypocretin (orexin) neurons with traumatic brain injury. Ann. Neurol. 2009;66:555–559. doi: 10.1002/ana.21836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wiseman-Hakes C., Duclos C., Blais H., Dumont M., Bernard F., Desautels A., Menon D.K., Gilbert D., Carrier J., Gosselin N. Sleep in the Acute Phase of Severe Traumatic Brain Injury: A Snapshot of Polysomnography. Neurorehabil. Neural Repair. 2016;30:713–721. doi: 10.1177/1545968315619697. [DOI] [PubMed] [Google Scholar]
- 70.Jahan A.B., Tanev K. Neurobiological Mechanisms Of Depression Following Traumatic Brain Injury. Brain Inj. 2023;37:24–33. doi: 10.1080/02699052.2022.2145362. [DOI] [PubMed] [Google Scholar]
- 71.Besedovsky L., Lange T., Haack M. The Sleep-Immune Crosstalk in Health and Disease. Physiol. Rev. 2019;99:1325–1380. doi: 10.1152/physrev.00010.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Irwin M.R. Sleep and inflammation: Partners in sickness and in health. Nat. Rev. Immunol. 2019;19:702–715. doi: 10.1038/s41577-019-0190-z. [DOI] [PubMed] [Google Scholar]
- 73.Krueger J.M., Majde J.A., Rector D.M. Cytokines in immune function and sleep regulation. Handb. Clin. Neurol. 2011;98:229–240. doi: 10.1016/B978-0-444-52006-7.00015-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lasselin J., Karshikoff B., Axelsson J., Åkerstedt T., Benson S., Engler H., Schedlowski M., Jones M., Lekander M., Andreasson A. Fatigue and sleepiness responses to experimental inflammation and exploratory analysis of the effect of baseline inflammation in healthy humans. Brain Behav. Immun. 2020;83:309–314. doi: 10.1016/j.bbi.2019.10.020. [DOI] [PubMed] [Google Scholar]
- 75.Opp M.R., Obal F., Jr., Krueger J.M. Interleukin 1 alters rat sleep: Temporal and dose-related effects. Pt 2Am. J. Physiol. 1991;260:R52–R58. doi: 10.1152/ajpregu.1991.260.1.R52. [DOI] [PubMed] [Google Scholar]
- 76.Weinberger J.F., Raison C.L., Rye D.B., Montague A.R., Woolwine B.J., Felger J.C., Haroon E., Miller A.H. Inhibition of tumor necrosis factor improves sleep continuity in patients with treatment resistant depression and high inflammation. Brain Behav. Immun. 2015;47:193–200. doi: 10.1016/j.bbi.2014.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nadjar A., Wigren H.M., Tremblay M.E. Roles of Microglial Phagocytosis and Inflammatory Mediators in the Pathophysiology of Sleep Disorders. Front. Cell Neurosci. 2017;11:250. doi: 10.3389/fncel.2017.00250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Deurveilher S., Golovin T., Hall S., Semba K. Microglia dynamics in sleep/wake states and in response to sleep loss. Neurochem. Int. 2021;143:104944. doi: 10.1016/j.neuint.2020.104944. [DOI] [PubMed] [Google Scholar]
- 79.Fonken L.K., Frank M.G., Kitt M.M., Barrientos R.M., Watkins L.R., Maier S.F. Microglia inflammatory responses are controlled by an intrinsic circadian clock. Brain Behav. Immun. 2015;45:171–179. doi: 10.1016/j.bbi.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wisor J.P., Schmidt M.A., Clegern W.C. Evidence for neuroinflammatory and microglial changes in the cerebral response to sleep loss. Sleep. 2011;34:261–272. doi: 10.1093/sleep/34.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rowe R.K., Harrison J.L., Morrison H.W., Subbian V., Murphy S.M., Lifshitz J. Acute Post-Traumatic Sleep May Define Vulnerability to a Second Traumatic Brain Injury in Mice. J. Neurotrauma. 2019;36:1318–1334. doi: 10.1089/neu.2018.5980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Krueger J.M., Clinton J.M., Winters B.D., Zielinski M.R., Taishi P., Jewett K.A., Davis C.J. Involvement of cytokines in slow wave sleep. Prog. Brain Res. 2011;193:39–47. doi: 10.1016/B978-0-444-53839-0.00003-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Krueger J.M., Obal F.J., Fang J., Kubota T., Taishi P. The role of cytokines in physiological sleep regulation. Ann. N. Y. Acad. Sci. 2001;933:211–221. doi: 10.1111/j.1749-6632.2001.tb05826.x. [DOI] [PubMed] [Google Scholar]
- 84.Green T.R.F., Ortiz J.B., Wonnacott S., Williams R.J., Rowe R.K. The Bidirectional Relationship Between Sleep and Inflammation Links Traumatic Brain Injury and Alzheimer’s Disease. Front. Neurosci. 2020;14:894. doi: 10.3389/fnins.2020.00894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rowe R.K., Griesbach G.S. Immune-endocrine interactions in the pathophysiology of sleep-wake disturbances following traumatic brain injury: A narrative review. Brain Res. Bull. 2022;185:117–128. doi: 10.1016/j.brainresbull.2022.04.017. [DOI] [PubMed] [Google Scholar]
- 86.Saber M., Murphy S.M., Cho Y., Lifshitz J., Rowe R.K. Experimental diffuse brain injury and a model of Alzheimer’s disease exhibit disease-specific changes in sleep and incongruous peripheral inflammation. J. Neurosci. Res. 2021;99:1136–1160. doi: 10.1002/jnr.24771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sanchez E., Blais H., Duclos C., Arbour C., Van Der Maren S., El-Khatib H., Baril A.A., Bernard F., Carrier J., Gosselin N. Sleep from acute to chronic traumatic brain injury and cognitive outcomes. Sleep. 2022;45:zsac123. doi: 10.1093/sleep/zsac123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.van Dalfsen J.H., Markus C.R. The influence of sleep on human hypothalamic-pituitary-adrenal (HPA) axis reactivity: A systematic review. Sleep Med. Rev. 2018;39:187–194. doi: 10.1016/j.smrv.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 89.Sauvet F., Drogou C., Bougard C., Arnal P.J., Dispersyn G., Bourrilhon C., Rabat A., Van Beers P., Gomez-Merino D., Faraut B., et al. Vascular response to 1 week of sleep restriction in healthy subjects. A metabolic response? Int. J. Cardiol. 2015;190:246–255. doi: 10.1016/j.ijcard.2015.04.119. [DOI] [PubMed] [Google Scholar]
- 90.de Zambotti M., Trinder J., Silvani A., Colrain I.M., Baker F.C. Dynamic coupling between the central and autonomic nervous systems during sleep: A review. Neurosci. Biobehav. Rev. 2018;90:84–103. doi: 10.1016/j.neubiorev.2018.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Frank M.G., Cantera R. Sleep, clocks, and synaptic plasticity. Trends Neurosci. 2014;37:491–501. doi: 10.1016/j.tins.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Tononi G., Cirelli C. Sleep and synaptic homeostasis: A hypothesis. Brain Res. Bull. 2003;62:143–150. doi: 10.1016/j.brainresbull.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 93.Rasch B., Born J. About sleep’s role in memory. Physiol. Rev. 2013;93:681–766. doi: 10.1152/physrev.00032.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kuula L., Pesonen A.K., Heinonen K., Kajantie E., Eriksson J.G., Andersson S., Lano A., Lahti J., Wolke D., Räikkönen K. Naturally occurring circadian rhythm and sleep duration are related to executive functions in early adulthood. J. Sleep Res. 2018;27:113–119. doi: 10.1111/jsr.12581. [DOI] [PubMed] [Google Scholar]
- 95.Hudson A.N., Van Dongen H.P.A., Honn K.A. Sleep deprivation, vigilant attention, and brain function: A review. Neuropsychopharmacology. 2020;45:21–30. doi: 10.1038/s41386-019-0432-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Palagini L., Bastien C.H., Marazziti D., Ellis J.G., Riemann D. The key role of insomnia and sleep loss in the dysregulation of multiple systems involved in mood disorders: A proposed model. J. Sleep Res. 2019;28:e12841. doi: 10.1111/jsr.12841. [DOI] [PubMed] [Google Scholar]
- 97.Xie L., Kang H., Xu Q., Chen M.J., Liao Y., Thiyagarajan M., O’Donnell J., Christensen D.J., Nicholson C., Iliff J.J., et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342:373–377. doi: 10.1126/science.1241224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Fultz N.E., Bonmassar G., Setsompop K., Stickgold R.A., Rosen B.R., Polimeni J.R., Lewis L.D. Coupled electrophysiological, hemodynamic, and cerebrospinal fluid oscillations in human sleep. Science. 2019;366:628–631. doi: 10.1126/science.aax5440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Simpson N., Dinges D.F. Sleep and inflammation. Pt 2Nutr. Rev. 2007;65:S244–S252. doi: 10.1301/nr.2007.dec.S244-S252. [DOI] [PubMed] [Google Scholar]
- 100.Irwin M.R., Olmstead R., Carroll J.E. Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation. Biol. Psychiatry. 2016;80:40–52. doi: 10.1016/j.biopsych.2015.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wang J., Wu X., Liang W., Chen M., Zhao C., Wang X. Objective Short Sleep Duration is Related to the Peripheral Inflammasome Dysregulation in Patients with Chronic Insomnia. Nat. Sci. Sleep. 2020;12:759–766. doi: 10.2147/NSS.S270045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bellesi M., de Vivo L., Chini M., Gilli F., Tononi G., Cirelli C. Sleep Loss Promotes Astrocytic Phagocytosis and Microglial Activation in Mouse Cerebral Cortex. J. Neurosci. 2017;37:5263–5273. doi: 10.1523/JNEUROSCI.3981-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Nijs J., Loggia M.L., Polli A., Moens M., Huysmans E., Goudman L., Meeus M., Vanderweeen L., Ickmans K., Clauw D. Sleep disturbances and severe stress as glial activators: Key targets for treating central sensitization in chronic pain patients? Expert Opin. Ther. Targets. 2017;21:817–826. doi: 10.1080/14728222.2017.1353603. [DOI] [PubMed] [Google Scholar]
- 104.Zhu B., Dong Y., Xu Z., Gompf H.S., Ward S.A., Xue Z., Miao C., Zhang Y., Chamberlin N.L., Xie Z. Sleep disturbance induces neuroinflammation and impairment of learning and memory. Neurobiol. Dis. 2012;48:348–355. doi: 10.1016/j.nbd.2012.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zielinski M.R., Gibbons A.J. Neuroinflammation, Sleep, and Circadian Rhythms. Front. Cell Infect. Microbiol. 2022;12:853096. doi: 10.3389/fcimb.2022.853096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lim D.C., Pack A.I. Obstructive sleep apnea and cognitive impairment: Addressing the blood-brain barrier. Sleep Med. Rev. 2014;18:35–48. doi: 10.1016/j.smrv.2012.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hurtado-Alvarado G., Domínguez-Salazar E., Pavon L., Velázquez-Moctezuma J., Gómez-González B. Blood-Brain Barrier Disruption Induced by Chronic Sleep Loss: Low-Grade Inflammation May Be the Link. J. Immunol. Res. 2016;2016:4576012. doi: 10.1155/2016/4576012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Xing C., Zhou Y., Xu H., Ding M., Zhang Y., Zhang M., Hu M., Huang X., Song L. Sleep disturbance induces depressive behaviors and neuroinflammation by altering the circadian oscillations of clock genes in rats. Neurosci. Res. 2021;171:124–132. doi: 10.1016/j.neures.2021.03.006. [DOI] [PubMed] [Google Scholar]
- 109.Herrero Babiloni A., De Koninck B.P., Beetz G., De Beaumont L., Martel M.O., Lavigne G.J. Sleep and pain: Recent insights, mechanisms, and future directions in the investigation of this relationship. J. Neural Transm. 2020;127:647–660. doi: 10.1007/s00702-019-02067-z. [DOI] [PubMed] [Google Scholar]
- 110.Irvine K.A., Clark J.D. Chronic Pain After Traumatic Brain Injury: Pathophysiology and Pain Mechanisms. Pain Med. 2018;19:1315–1333. doi: 10.1093/pm/pnx153. [DOI] [PubMed] [Google Scholar]
- 111.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1–211. doi: 10.1177/0333102417738202. [DOI] [PubMed] [Google Scholar]
- 112.Nampiaparampil D.E. Prevalence of chronic pain after traumatic brain injury: A systematic review. JAMA. 2008;300:711–719. doi: 10.1001/jama.300.6.711. [DOI] [PubMed] [Google Scholar]
- 113.Khoury S., Benavides R. Pain with traumatic brain injury and psychological disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2018;87 Pt B:224–233. doi: 10.1016/j.pnpbp.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 114.Brown S., Hawker G., Beaton D., Colantonio A. Long-term musculoskeletal complaints after traumatic brain injury. Brain Inj. 2011;25:453–461. doi: 10.3109/02699052.2011.556581. [DOI] [PubMed] [Google Scholar]
- 115.Herrero Babiloni A., Beetz G., Tang N.K.Y., Heinzer R., Nijs J., Martel M.O., Lavigne G.J. Towards the endotyping of the sleep-pain interaction: A topical review on multitarget strategies based on phenotypic vulnerabilities and putative pathways. Pain. 2021;162:1281–1288. doi: 10.1097/j.pain.0000000000002124. [DOI] [PubMed] [Google Scholar]
- 116.Haack M., Simpson N., Sethna N., Kaur S., Mullington J. Sleep deficiency and chronic pain: Potential underlying mechanisms and clinical implications. Neuropsychopharmacology. 2020;45:205–216. doi: 10.1038/s41386-019-0439-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Mullington J.M., Simpson N.S., Meier-Ewert H.K., Haack M. Sleep loss and inflammation. Best Pract. Res. Clin. Endocrinol. Metab. 2010;24:775–784. doi: 10.1016/j.beem.2010.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zhou Y.Q., Liu Z., Liu Z.H., Chen S.P., Li M., Shahveranov A., Ye D.W., Tian Y.K. Interleukin-6: An emerging regulator of pathological pain. J. Neuroinflammation. 2016;13:141. doi: 10.1186/s12974-016-0607-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Chaudhry S.R., Stadlbauer A., Buchfelder M., Kinfe T.M. Melatonin Moderates the Triangle of Chronic Pain, Sleep Architecture and Immunometabolic Traffic. Biomedicines. 2021;9:984. doi: 10.3390/biomedicines9080984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Blum B., Kaushal S., Khan S., Kim J.H., Alvarez Villalba C.L. Melatonin in Traumatic Brain Injury and Cognition. Cureus. 2021;13:e17776. doi: 10.7759/cureus.17776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lorente L., Martin M.M., Ruiz C., Abreu-Gonzalez P., Ramos-Gomez L., Argueso M., Sole-Violan J., Caceres J.J., Jimenez A. Serum melatonin levels in predicting mortality in patients with severe traumatic brain injury. Anaesth. Crit. Care Pain Med. 2021;40:100966. doi: 10.1016/j.accpm.2021.100966. [DOI] [PubMed] [Google Scholar]
- 122.Suzuki Y., Khoury S., El-Khatib H., Chauny J.M., Paquet J., Giguere J.F., Denis R., Gosselin N., Lavigne G.J., Arbour C. Individuals with pain need more sleep in the early stage of mild traumatic brain injury. Sleep Med. 2017;33:36–42. doi: 10.1016/j.sleep.2016.06.033. [DOI] [PubMed] [Google Scholar]
- 123.Uceyler N., Zeller D., Kahn A.K., Kewenig S., Kittel-Schneider S., Schmid A., Casanova-Molla J., Reiners K., Sommer C. Small fibre pathology in patients with fibromyalgia syndrome. Pt 6Brain. 2013;136:1857–1867. doi: 10.1093/brain/awt053. [DOI] [PubMed] [Google Scholar]
- 124.Ji R.R., Xu Z.Z., Gao Y.J. Emerging targets in neuroinflammation-driven chronic pain. Nat. Rev. Drug Discov. 2014;13:533–548. doi: 10.1038/nrd4334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hammond F.M., Corrigan J.D., Ketchum J.M., Malec J.F., Dams-O’Connor K., Hart T., Novack T.A., Bogner J., Dahdah M.N., Whiteneck G.G. Prevalence of Medical and Psychiatric Comorbidities Following Traumatic Brain Injury. J. Head Trauma Rehabil. 2019;34:E1–E10. doi: 10.1097/HTR.0000000000000465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Clay F.J., Watson W.L., Newstead S.V., McClure R.J. A systematic review of early prognostic factors for persisting pain following acute orthopedic trauma. Pain Res. Manag. 2012;17:35–44. doi: 10.1155/2012/935194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Campos A.C.P., Antunes G.F., Matsumoto M., Pagano R.L., Martinez R.C.R. Neuroinflammation, Pain and Depression: An Overview of the Main Findings. Front. Psychol. 2020;11:1825. doi: 10.3389/fpsyg.2020.01825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhang L., Zhang J., You Z. Switching of the Microglial Activation Phenotype Is a Possible Treatment for Depression Disorder. Front. Cell Neurosci. 2018;12:306. doi: 10.3389/fncel.2018.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Manchanda S., Singh H., Kaur T., Kaur G. Low-grade neuroinflammation due to chronic sleep deprivation results in anxiety and learning and memory impairments. Mol. Cell. Biochem. 2018;449:63–72. doi: 10.1007/s11010-018-3343-7. [DOI] [PubMed] [Google Scholar]
- 130.Feiger J.A., Snyder R.L., Walsh M.J., Cissne M., Cwiek A., Al-Momani S.I., Chiou K.S. The Role of Neuroinflammation in Neuropsychiatric Disorders Following Traumatic Brain Injury: A Systematic Review. J. Head Trauma Rehabil. 2022;37:E370–E382. doi: 10.1097/HTR.0000000000000754. [DOI] [PubMed] [Google Scholar]
- 131.Wadhwa M., Chauhan G., Roy K., Sahu S., Deep S., Jain V., Kishore K., Ray K., Thakur L., Panjwani U. Caffeine and Modafinil Ameliorate the Neuroinflammation and Anxious Behavior in Rats during Sleep Deprivation by Inhibiting the Microglia Activation. Front. Cell Neurosci. 2018;12:49. doi: 10.3389/fncel.2018.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Xie Y., Ba L., Wang M., Deng S.Y., Chen S.M., Huang L.F., Zhang M., Wang W., Ding F.F. Chronic sleep fragmentation shares similar pathogenesis with neurodegenerative diseases: Endosome-autophagosome-lysosome pathway dysfunction and microglia-mediated neuroinflammation. CNS Neurosci. Ther. 2020;26:215–227. doi: 10.1111/cns.13218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gray S.C., Kinghorn K.J., Woodling N.S. Shifting equilibriums in Alzheimer’s disease: The complex roles of microglia in neuroinflammation, neuronal survival and neurogenesis. Neural Regen. Res. 2020;15:1208–1219. doi: 10.4103/1673-5374.272571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bubu O.M., Brannick M., Mortimer J., Umasabor-Bubu O., Sebastião Y.V., Wen Y., Schwartz S., Borenstein A.R., Wu Y., Morgan D., et al. Sleep, Cognitive impairment, and Alzheimer’s disease: A Systematic Review and Meta-Analysis. Sleep. 2017;40:zsw032. doi: 10.1093/sleep/zsw032. [DOI] [PubMed] [Google Scholar]
- 135.Snowden T.M., Hinde A.K., Reid H.M.O., Christie B.R. Does Mild Traumatic Brain Injury Increase the Risk for Dementia? A Systematic Review and Meta-Analysis. J. Alzheimers Dis. 2020;78:757–775. doi: 10.3233/JAD-200662. [DOI] [PubMed] [Google Scholar]
- 136.Baril A.A., Beiser A.S., Redline S., McGrath E.R., Aparicio H.J., Gottlieb D.J., Seshadri S., Pase M.P., Himali J.J. Systemic inflammation as a moderator between sleep and incident dementia. Sleep. 2021;44:zsaa164. doi: 10.1093/sleep/zsaa164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Baril A.A., Beiser A.S., Redline S., McGrath E.R., Gottlieb D.J., Aparicio H., Seshadri S., Himali J.J., Pase M.P. Interleukin-6 Interacts with Sleep Apnea Severity when Predicting Incident Alzheimer’s Disease Dementia. J. Alzheimers Dis. 2021;79:1451–1457. doi: 10.3233/JAD-200545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Wadhwa M., Prabhakar A., Anand J.P., Ray K., Prasad D., Kumar B., Panjwani U. Complement activation sustains neuroinflammation and deteriorates adult neurogenesis and spatial memory impairment in rat hippocampus following sleep deprivation. Brain Behav. Immun. 2019;82:129–144. doi: 10.1016/j.bbi.2019.08.004. [DOI] [PubMed] [Google Scholar]
- 139.Wadhwa M., Prabhakar A., Ray K., Roy K., Kumari P., Jha P.K., Kishore K., Kumar S., Panjwani U. Inhibiting the microglia activation improves the spatial memory and adult neurogenesis in rat hippocampus during 48 h of sleep deprivation. J. Neuroinflammation. 2017;14:222. doi: 10.1186/s12974-017-0998-z. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 140.Amanollahi M., Jameie M., Heidari A., Rezaei N. The Dialogue Between Neuroinflammation and Adult Neurogenesis: Mechanisms Involved and Alterations in Neurological Diseases. Mol. Neurobiol. 2022;60:923–959. doi: 10.1007/s12035-022-03102-z. [DOI] [PubMed] [Google Scholar]
- 141.Tapp Z.M., Cornelius S., Oberster A., Kumar J.E., Atluri R., Witcher K.G., Oliver B., Bray C., Velasquez J., Zhao F., et al. Sleep fragmentation engages stress-responsive circuitry, enhances inflammation and compromises hippocampal function following traumatic brain injury. Exp. Neurol. 2022;353:114058. doi: 10.1016/j.expneurol.2022.114058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Faden A.I., Wu J., Stoica B.A., Loane D.J. Progressive inflammation-mediated neurodegeneration after traumatic brain or spinal cord injury. Br. J. Pharmacol. 2016;173:681–691. doi: 10.1111/bph.13179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Johnson V.E., Stewart J.E., Begbie F.D., Trojanowski J.Q., Smith D.H., Stewart W. Inflammation and white matter degeneration persist for years after a single traumatic brain injury. Pt 1Brain. 2013;136:28–42. doi: 10.1093/brain/aws322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Alawieh A., Chalhoub R.M., Mallah K., Langley E.F., York M., Broome H., Couch C., Adkins D., Tomlinson S. Complement Drives Synaptic Degeneration and Progressive Cognitive Decline in the Chronic Phase after Traumatic Brain Injury. J. Neurosci. 2021;41:1830–1843. doi: 10.1523/JNEUROSCI.1734-20.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Irwin M.R., Olmstead R., Breen E.C., Witarama T., Carrillo C., Sadeghi N., Arevalo J.M., Ma J., Nicassio P., Ganz P.A., et al. Tai chi, cellular inflammation, and transcriptome dynamics in breast cancer survivors with insomnia: A randomized controlled trial. J. Natl. Cancer Inst. Monogr. 2014;2014:295–301. doi: 10.1093/jncimonographs/lgu028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Heffner K.L., France C.R., Ashrafioun L., Quiñones M., Walsh P., Maloney M.D., Giordano B.D., Pigeon W.R. Clinical Pain-related Outcomes and Inflammatory Cytokine Response to Pain Following Insomnia Improvement in Adults With Knee Osteoarthritis. Clin. J. Pain. 2018;34:1133–1140. doi: 10.1097/AJP.0000000000000644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Chen H.Y., Cheng I.C., Pan Y.J., Chiu Y.L., Hsu S.P., Pai M.F., Yang J.Y., Peng Y.S., Tsai T.J., Wu K.D. Cognitive-behavioral therapy for sleep disturbance decreases inflammatory cytokines and oxidative stress in hemodialysis patients. Kidney Int. 2011;80:415–422. doi: 10.1038/ki.2011.151. [DOI] [PubMed] [Google Scholar]
- 148.Nguyen S., McKay A., Wong D., Rajaratnam S.M., Spitz G., Williams G., Mansfield D., Ponsford J.L. Cognitive Behavior Therapy to Treat Sleep Disturbance and Fatigue After Traumatic Brain Injury: A Pilot Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2017;98:1508–1517.e2. doi: 10.1016/j.apmr.2017.02.031. [DOI] [PubMed] [Google Scholar]
- 149.Bogdanov S., Naismith S., Lah S. Sleep outcomes following sleep-hygiene-related interventions for individuals with traumatic brain injury: A systematic review. Brain Inj. 2017;31:422–433. doi: 10.1080/02699052.2017.1282042. [DOI] [PubMed] [Google Scholar]
- 150.Tang N.K.Y., Moore C., Parsons H., Sandhu H.K., Patel S., Ellard D.R., Nichols V.P., Madan J., Collard V.E.J., Sharma U., et al. Implementing a hybrid cognitive-behavioural therapy for pain-related insomnia in primary care: Lessons learnt from a mixed-methods feasibility study. BMJ Open. 2020;10:e034764. doi: 10.1136/bmjopen-2019-034764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Tang N.K.Y. Cognitive behavioural therapy in pain and psychological disorders: Towards a hybrid future. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2018;87 Pt B:281–289. doi: 10.1016/j.pnpbp.2017.02.023. [DOI] [PubMed] [Google Scholar]
- 152.Finan P.H., Buenaver L.F., Coryell V.T., Smith M.T. Cognitive-Behavioral Therapy for Comorbid Insomnia and Chronic Pain. Sleep Med. Clin. 2014;9:261–274. doi: 10.1016/j.jsmc.2014.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Herrero Babiloni A., Beetz G., Bruneau A., Martel M.O., Cistulli P.A., Nixdorf D.R., Conway J.M., Lavigne G.J. Multitargeting the sleep-pain interaction with pharmacological approaches: A narrative review with suggestions on new avenues of investigation. Sleep Med. Rev. 2021;59:101459. doi: 10.1016/j.smrv.2021.101459. [DOI] [PubMed] [Google Scholar]
- 154.Chen P.L., Lee W.J., Sun W.Z., Oyang Y.J., Fuh J.L. Risk of dementia in patients with insomnia and long-term use of hypnotics: A population-based retrospective cohort study. PLoS ONE. 2012;7:e49113. doi: 10.1371/journal.pone.0049113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Desmidt T., Delrieu J., Lebouvier T., Robert G., David R., Balageas A.C., Surget A., Belzung C., Arlicot N., Ribeiro M.J., et al. Benzodiazepine use and brain amyloid load in nondemented older individuals: A florbetapir PET study in the Multidomain Alzheimer Preventive Trial cohort. Neurobiol. Aging. 2019;84:61–69. doi: 10.1016/j.neurobiolaging.2019.08.008. [DOI] [PubMed] [Google Scholar]
- 156.Morin C.M., Vallières A., Guay B., Ivers H., Savard J., Mérette C., Bastien C., Baillargeon L. Cognitive behavioral therapy, singly and combined with medication, for persistent insomnia: A randomized controlled trial. JAMA. 2009;301:2005–2015. doi: 10.1001/jama.2009.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Gao J., Su G., Liu J., Zhang J., Zhou J., Liu X., Tian Y., Zhang Z. Mechanisms of Inhibition of Excessive Microglial Activation by Melatonin. J. Mol. Neurosci. 2020;70:1229–1236. doi: 10.1007/s12031-020-01531-w. [DOI] [PubMed] [Google Scholar]
- 158.Kose D., Kose A., Halici Z., Gurbuz M.A., Aydin A., Ugan R.A., Karaman A., Toktay E. Do peripheral melatonin agonists improve bone fracture healing? The effects of agomelatine and ramelteon on experimental bone fracture. Eur. J. Pharmacol. 2020;887:173577. doi: 10.1016/j.ejphar.2020.173577. [DOI] [PubMed] [Google Scholar]
- 159.Lin C., Chao H., Li Z., Xu X., Liu Y., Hou L., Liu N., Ji J. Melatonin attenuates traumatic brain injury-induced inflammation: A possible role for mitophagy. J. Pineal Res. 2016;61:177–186. doi: 10.1111/jpi.12337. [DOI] [PubMed] [Google Scholar]
- 160.Babaee A., Eftekhar-Vaghefi S.H., Asadi-Shekaari M., Shahrokhi N., Soltani S.D., Malekpour-Afshar R., Basiri M. Melatonin treatment reduces astrogliosis and apoptosis in rats with traumatic brain injury. Iran J. Basic Med. Sci. 2015;18:867–872. [PMC free article] [PubMed] [Google Scholar]
- 161.Barlow K.M., Esser M.J., Veidt M., Boyd R. Melatonin as a Treatment after Traumatic Brain Injury: A Systematic Review and Meta-Analysis of the Pre-Clinical and Clinical Literature. J. Neurotrauma. 2019;36:523–537. doi: 10.1089/neu.2018.5752. [DOI] [PubMed] [Google Scholar]
- 162.Barlow K.M., Brooks B.L., Esser M.J., Kirton A., Mikrogianakis A., Zemek R.L., MacMaster F.P., Nettel-Aguirre A., Yeates K.O., Kirk V., et al. Efficacy of Melatonin in Children With Postconcussive Symptoms: A Randomized Clinical Trial. Pediatrics. 2020;145:2812. doi: 10.1542/peds.2019-2812. [DOI] [PubMed] [Google Scholar]
- 163.Barlow K.M., Kirk V., Brooks B., Esser M.J., Yeates K.O., Zemek R., Kirton A., Mikrogianakis A., MacMaster F., Nettel-Aguirre A., et al. Efficacy of Melatonin for Sleep Disturbance in Children with Persistent Post-Concussion Symptoms: Secondary Analysis of a Randomized Controlled Trial. J. Neurotrauma. 2021;38:950–959. doi: 10.1089/neu.2020.7154. [DOI] [PubMed] [Google Scholar]
- 164.Witcher K.G., Bray C.E., Dziabis J.E., McKim D.B., Benner B.N., Rowe R.K., Kokiko-Cochran O.N., Popovich P.G., Lifshitz J., Eiferman D.S., et al. Traumatic brain injury-induced neuronal damage in the somatosensory cortex causes formation of rod-shaped microglia that promote astrogliosis and persistent neuroinflammation. Glia. 2018;66:2719–2736. doi: 10.1002/glia.23523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Spangenberg E., Severson P.L., Hohsfield L.A., Crapser J., Zhang J., Burton E.A., Zhang Y., Spevak W., Lin J., Phan N.Y., et al. Sustained microglial depletion with CSF1R inhibitor impairs parenchymal plaque development in an Alzheimer’s disease model. Nat. Commun. 2019;10:3758. doi: 10.1038/s41467-019-11674-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Cerqueira S.R., Ayad N.G., Lee J.K. Neuroinflammation Treatment via Targeted Delivery of Nanoparticles. Front. Cell Neurosci. 2020;14:576037. doi: 10.3389/fncel.2020.576037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Rahimifard M., Maqbool F., Moeini-Nodeh S., Niaz K., Abdollahi M., Braidy N., Nabavi S.M., Nabavi S.F. Targeting the TLR4 signaling pathway by polyphenols: A novel therapeutic strategy for neuroinflammation. Ageing Res. Rev. 2017;36:11–19. doi: 10.1016/j.arr.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 168.Song L., Pei L., Yao S., Wu Y., Shang Y. NLRP3 Inflammasome in Neurological Diseases, from Functions to Therapies. Front. Cell Neurosci. 2017;11:63. doi: 10.3389/fncel.2017.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Elman I., Pustilnik A., Borsook D. Beating pain with psychedelics: Matter over mind? Neurosci. Biobehav. Rev. 2022;134:104482. doi: 10.1016/j.neubiorev.2021.12.005. [DOI] [PubMed] [Google Scholar]
- 170.Calder A.E., Hasler G. Towards an understanding of psychedelic-induced neuroplasticity. Neuropsychopharmacology. 2023;48:104–112. doi: 10.1038/s41386-022-01389-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Thomas C.W., Blanco-Duque C., Breant B.J., Goodwin G.M., Sharp T., Bannerman D.M., Vyazovskiy V.V. Psilocin acutely alters sleep-wake architecture and cortical brain activity in laboratory mice. Transl. Psychiatry. 2022;12:77. doi: 10.1038/s41398-022-01846-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Hiskens M.I. Targets of Neuroprotection and Review of Pharmacological Interventions in Traumatic Brain Injury. J. Pharmacol. Exp. Ther. 2022;382:149–166. doi: 10.1124/jpet.121.001023. [DOI] [PubMed] [Google Scholar]
- 173.Saur L., Baptista P.P., de Senna P.N., Paim M.F., do Nascimento P., Ilha J., Bagatini P.B., Achaval M., Xavier L.L. Physical exercise increases GFAP expression and induces morphological changes in hippocampal astrocytes. Brain Struct. Funct. 2014;219:293–302. doi: 10.1007/s00429-012-0500-8. [DOI] [PubMed] [Google Scholar]
- 174.Barad Z., Augusto J., Kelly A.M. Exercise-induced modulation of neuroinflammation in ageing. J. Physiol. 2022 doi: 10.1113/JP282894. in press . [DOI] [PubMed] [Google Scholar]
- 175.Ma C., Lin M., Gao J., Xu S., Huang L., Zhu J., Huang J., Tao J., Chen L. The impact of physical activity on blood inflammatory cytokines and neuroprotective factors in individuals with mild cognitive impairment: A systematic review and meta-analysis of randomized-controlled trials. Aging Clin. Exp. Res. 2022;34:1471–1484. doi: 10.1007/s40520-021-02069-6. [DOI] [PubMed] [Google Scholar]
- 176.De Nys L., Anderson K., Ofosu E.F., Ryde G.C., Connelly J., Whittaker A.C. The effects of physical activity on cortisol and sleep: A systematic review and meta-analysis. Psychoneuroendocrinology. 2022;143:105843. doi: 10.1016/j.psyneuen.2022.105843. [DOI] [PubMed] [Google Scholar]
- 177.Memon A.R., Gupta C.C., Crowther M.E., Ferguson S.A., Tuckwell G.A., Vincent G.E. Sleep and physical activity in university students: A systematic review and meta-analysis. Sleep Med. Rev. 2021;58:101482. doi: 10.1016/j.smrv.2021.101482. [DOI] [PubMed] [Google Scholar]
- 178.Lurie D.I. An Integrative Approach to Neuroinflammation in Psychiatric disorders and Neuropathic Pain. J. Exp. Neurosci. 2018;12:1179069518793639. doi: 10.1177/1179069518793639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Jacquens A., Needham E.J., Zanier E.R., Degos V., Gressens P., Menon D. Neuro-Inflammation Modulation and Post-Traumatic Brain Injury Lesions: From Bench to Bed-Side. Int. J. Mol. Sci. 2022;23:11193. doi: 10.3390/ijms231911193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Lefaucheur J.P., Aleman A., Baeken C., Benninger D.H., Brunelin J., Di Lazzaro V., Filipovic S.R., Grefkes C., Hasan A., Hummel F.C., et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS): An update (2014-2018) Clin. Neurophysiol. 2020;131:474–528. doi: 10.1016/j.clinph.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 181.Herrero Babiloni A., Bellemare A., Beetz G., Vinet S.A., Martel M.O., Lavigne G.J., De Beaumont L. The effects of non-invasive brain stimulation on sleep disturbances among different neurological and neuropsychiatric conditions: A systematic review. Sleep Med. Rev. 2021;55:101381. doi: 10.1016/j.smrv.2020.101381. [DOI] [PubMed] [Google Scholar]
- 182.Ljubisavljevic M.R., Javid A., Oommen J., Parekh K., Nagelkerke N., Shehab S., Adrian T.E. The Effects of Different Repetitive Transcranial Magnetic Stimulation (rTMS) Protocols on Cortical Gene Expression in a Rat Model of Cerebral Ischemic-Reperfusion Injury. PLoS ONE. 2015;10:e0139892. doi: 10.1371/journal.pone.0139892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Sasso V., Bisicchia E., Latini L., Ghiglieri V., Cacace F., Carola V., Molinari M., Viscomi M.T. Repetitive transcranial magnetic stimulation reduces remote apoptotic cell death and inflammation after focal brain injury. J. Neuroinflammation. 2016;13:150. doi: 10.1186/s12974-016-0616-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Crowley T., Cryan J.F., Downer E.J., O’Leary O.F. Inhibiting neuroinflammation: The role and therapeutic potential of GABA in neuro-immune interactions. Brain Behav. Immun. 2016;54:260–277. doi: 10.1016/j.bbi.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 185.Jodoin M., Rouleau D., Larson-Dupuis C., Gosselin N., De Beaumont L. The clinical utility of repetitive transcranial magnetic stimulation in reducing the risks of transitioning from acute to chronic pain in traumatically injured patients. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2017;87:322–331. doi: 10.1016/j.pnpbp.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 186.Feng J., Zhang Q., Zhang C., Wen Z., Zhou X. The Effect of sequential bilateral low-frequency rTMS over dorsolateral prefrontal cortex on serum level of BDNF and GABA in patients with primary insomnia. Brain Behav. 2019;9:e01206. doi: 10.1002/brb3.1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Regner G.G., Torres I.L.S., de Oliveira C., Pfluger P., da Silva L.S., Scarabelot V.L., Stroher R., de Souza A., Fregni F., Pereira P. Transcranial direct current stimulation (tDCS) affects neuroinflammation parameters and behavioral seizure activity in pentylenetetrazole-induced kindling in rats. Neurosci. Lett. 2020;735:135162. doi: 10.1016/j.neulet.2020.135162. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.