Abstract
Background
People with dementia who are being cared for in long‐term care settings are often not engaged in meaningful activities. We wanted to know whether offering them activities which are tailored to their individual interests and preferences could improve their quality of life and reduce agitation. This review updates our earlier review published in 2018.
Objectives
∙ To assess the effects of personally tailored activities on psychosocial outcomes for people with dementia living in long‐term care facilities.
∙ To describe the components of the interventions.
∙ To describe conditions which enhance the effectiveness of personally tailored activities in this setting.
Search methods
We searched the Cochrane Dementia and Cognitive Improvement Group’s Specialized Register, on 15 June 2022. We also performed additional searches in MEDLINE, Embase, PsycINFO, CINAHL, Web of Science, ClinicalTrials.gov, and the World Health Organization (WHO) ICTRP, to ensure that the search for the review was as up‐to‐date and as comprehensive as possible.
Selection criteria
We included randomised controlled trials (RCTs) and controlled clinical trials offering personally tailored activities. All interventions included an assessment of the participants' present or past preferences for, or interest in, particular activities as a basis for an individual activity plan. Control groups received either usual care or an active control intervention.
Data collection and analysis
Two authors independently selected studies for inclusion, extracted data and assessed the risk of bias of included studies. Our primary efficacy outcomes were agitation and participant quality of life. Where possible, we pooled data across studies using a random effects model.
Main results
We identified three new studies, and therefore included 11 studies with 1071 participants in this review update. The mean age of participants was 78 to 88 years and most had moderate or severe dementia. Ten studies were RCTs (three studies randomised clusters to the study groups, six studies randomised individual participants, and one study randomised matched pairs of participants) and one study was a non‐randomised clinical trial. Five studies included a control group receiving usual care, five studies an active control group (activities which were not personally tailored) and one study included both types of control group. The duration of follow‐up ranged from 10 days to nine months.
In nine studies personally tailored activities were delivered directly to the participants. In one study nursing staff, and in another study family members, were trained to deliver the activities. The selection of activities was based on different theoretical models, but the activities delivered did not vary substantially.
We judged the risk of selection bias to be high in five studies, the risk of performance bias to be high in five studies and the risk of detection bias to be high in four studies.
We found low‐certainty evidence that personally tailored activities may slightly reduce agitation (standardised mean difference −0.26, 95% CI −0.53 to 0.01; I² = 50%; 7 studies, 485 participants). We also found low‐certainty evidence from one study that was not included in the meta‐analysis, indicating that personally tailored activities may make little or no difference to general restlessness, aggression, uncooperative behaviour, very negative and negative verbal behaviour (180 participants). Two studies investigated quality of life by proxy‐rating. We found low‐certainty evidence that personally tailored activities may result in little to no difference in quality of life in comparison with usual care or an active control group (MD ‐0.83, 95% CI ‐3.97 to 2.30; I² = 51%; 2 studies, 177 participants). Self‐rated quality of life was only available for a small number of participants from one study, and there was little or no difference between personally tailored activities and usual care on this outcome (MD 0.26, 95% CI −3.04 to 3.56; 42 participants; low‐certainty evidence). Two studies assessed adverse effects, but no adverse effects were observed.
We are very uncertain about the effects of personally tailored activities on mood and positive affect. For negative affect we found moderate‐certainty evidence that there is probably little to no effect of personally tailored activities compared to usual care or activities which are not personalised (standardised mean difference ‐0.02, 95% CI −0.19 to 0.14; 6 studies, 632 participants). We were not able to undertake meta‐analyses for engagement and sleep‐related outcomes, and we are very uncertain whether personally tailored activities have any effect on these outcomes.
Two studies that investigated the duration of the effects of personally tailored activities indicated that the intervention effects they found persisted only during the period of delivery of the activities.
Authors' conclusions
Offering personally tailored activities to people with dementia in long‐term care may slightly reduce agitation. Personally tailored activities may result in little to no difference in quality of life rated by proxies, but we acknowledge concerns about the validity of proxy ratings of quality of life in severe dementia. Personally tailored activities probably have little or no effect on negative affect, and we are uncertain whether they have any effect on positive affect or mood. There was no evidence that interventions were more likely to be effective if based on one theoretical model rather than another. We included three new studies in this updated review, but two studies were pilot trials and included only a small number of participants. Certainty of evidence was predominately very low or low due to several methodological limitations of and inconsistencies between the included studies. Evidence is still limited, and we remain unable to describe optimal activity programmes. Further research should focus on methods for selecting appropriate and meaningful activities for people in different stages of dementia.
Plain language summary
Personally tailored activities for people with dementia in long‐term care
What are the benefits of activities that are tailored to the interests and preferences of people with dementia living in care homes
What was studied in this review?
People with dementia living in nursing or residential homes often have too little to do. Activities which are available may not be meaningful to them. If a person with dementia has the chance to take part in activities which match his or her personal interests and preferences, this may lead to a better quality of life, may reduce behaviours sometimes described as agitation (such as restlessness or aggression), and may have other positive effects.
What did we want to find out?
We aimed to investigate the effects of offering people with dementia who were living in care homes activities tailored to their personal interests. This review updates our previous review from 2018.
What did we do?
We searched for trials that had offered an activity programme to people with dementia based on their individual interests (an intervention group) and had compared them with other participants who were not offered these activities (a control group).
We found 11 studies including 1071 people with dementia living in care homes. Ten of the studies were randomised controlled trials (RCTs), meaning that it was decided at random whether participants were in the intervention group or the control group. One study was not randomised, which puts it at higher risk of biased results. The people included in the studies had moderate or severe dementia, and almost all had some kind of agitation when the study started. The studies lasted from 10 days to nine months. In all the studies, the people in the intervention groups got an individual activity plan. Most of the activities took place in special sessions run by trained staff, but in two studies the nursing staff or family members were trained to provide the activities during the daily care routine (nursing staff) or during visits (family members). The activities actually offered in the different studies did not vary a lot, but the number of activity sessions per week and the duration of the sessions did vary.
In five studies, the control group got only the usual care delivered in care homes; in five studies, the control group got different activities that were not personally tailored; one study had both types of control group.
What did we find?
The quality of the trials and how well they were reported varied, and this affected our confidence in the results. Offering personally tailored activities to people with dementia living in care homes may slightly improve agitation. In two studies, staff members judged the quality of life of the people with dementia, but offering the activities may result in little to no difference in quality of life. Only two studies mentioned looking for harmful effects; none were reported.
Personally tailored activities may have little or no effect on the negative emotions expressed by the participants. We could not draw any conclusion about effects on the participants' positive emotions, mood, engagement (being involved in what is happening around them) or quality of sleep, because some of the studies did not use the most appropriate methods to carry out their investigations. None of the studies measured effects on the amount of medication participants were given, or effects on carers.
We concluded that offering activity sessions to people with moderate or severe dementia living in care homes may help to manage agitation.
What are the limitations of the evidence?
Our confidence in the results was limited because of the small number of studies and because the studies did not always use the most appropriate methods to carry out their investigations. For example, in some studies it was not clear if they assigned people randomly to the study groups.
How up to date is this evidence?
This review updates our previous review, and the evidence is current to 15 June 2022.
Summary of findings
Summary of findings 1. Personally tailored activities compared to usual care or non‐personalised activities for people with dementia.
| Personally tailored activities compared to usual care or non‐personalised activities for people with dementia | ||||||
| Patient or population: people with dementia Setting: long‐term care facilities Intervention: personally tailored activities Comparison: usual care or non‐personalised activities (active control) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with usual care or non‐personalised activities | Risk with Personally tailored activities | |||||
| Agitation (assessed with different scales, higher scores indicate more agitation); follow‐up: range 10 days to 9 months | ‐ | SMD 0.26 SD lower (0.53 lower to 0.01 higher) | ‐ | 485 (7 RCTs) | ⊕⊕⊝⊝ LOWa,b | |
| Quality of life (self‐rating by the participants; assessed with Quality of Life in Alzheimer’s Disease scale; range 15 to 60; higher scores indicate a higher quality of life); follow‐up: 28 weeks | The mean quality of life score with usual care was 33.00. | The mean quality of life score in the intervention group was on average 0.26 higher (3.04 lower to 3.56 higher). | ‐ | 42 (1 RCT) | ⊕⊕⊝⊝ LOWc | Mean difference adjusted for baseline/demographic characteristics; clinical relevance (by study authors): 3‐point difference; only about one‐third of the participants completed the self‐assessment. |
| Quality of life (proxy‐rating; assessed with Quality of Life in Alzheimer’s Disease scale; range 15 to 60; higher scores indicate a higher quality of life); follow‐up: 8 weeks and 28 weeks | The mean quality of life score (proxy‐rated) was 30.5 with usual care and 36.5 with the active control group. | The mean quality of life score in the intervention group was on average 0.83 lower (3.97 lower to 2.30 higher) | ‐ | 177 (2 RCTs) | ⊕⊕⊝⊝ LOWd,e | Proxy‐rating, clinical relevance (as defined by the authors of one of the studies): 3‐point difference. |
| Adverse events; follow‐up: range 10 days to 4 weeks | Two studies assessed adverse effects, but no adverse effects were reported in either study. | ‐ | 188 (2 RCTs) |
‐ | ||
| Positive affect (assessed with different scales, higher scores indicate a greater display of positive affect); follow‐up: range 10 days to 9 months | ‐ | SMD 0.88 SD higher (0.43 higher to 1.32 higher) | ‐ | 498 (6 RCTs) | ⊕⊝⊝⊝ VERY LOWa,b,f | |
| Negative affect (assessed with different scales, higher scores indicate a greater display of negative affect); follow‐up: range 10 days to 9 months | ‐ | SMD 0.02 SD lower (0.19 lower to 0.14 higher) | ‐ | 632 (6 RCTs) | ⊕⊕⊕⊝ MODERATEb | |
| Mood (assessed with different scales, lower scores indicate improved mood); follow‐up: range 4 weeks to 9 months | ‐ | SMD 0.03 SD lower (0.21 lower to 0.27 higher) | ‐ | 265 (4 RCTs) | ⊕⊝⊝⊝ VERY LOWb,g | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
a Downgraded one level for imprecision: wide confidence interval, crossing the borders of clinical relevance defined by the study authors in one direction. b Downgraded one level for risk of bias: high risk of selection bias, performance bias and detection bias in one study. c Downgraded two levels for imprecision: wide confidence interval, crossing the border of clinical relevance defined by the study authors in both directions. d Downgraded one level for risk of bias: high risk of selection bias and detection bias in some studies. e Downgraded one level for imprecision: wide confidence interval, crossing the border of small effects (SMD) in one direction. f Downgraded one level for inconsistency: substantial heterogeneity. g Downgraded two levels for imprecision: wide confidence interval, crossing the border of small effects (SMD) in both directions.
Background
Description of the condition
Dementia is a syndrome of progressive cognitive and functional decline, threatening the affected person’s capacities to perform activities and to communicate. Worldwide, there were approximately 57.4 million people with dementia in 2019 and the absolute number is expected to rise (GBD 2019 Dementia Forecasting Collaborators 2022). In long‐term care facilities, the estimated prevalence of dementia ranges between 40% and 80% (Helvik 2015; Stewart 2014).
People with dementia often spend their time without being engaged in meaningful activities or being involved with other people (Adlbrecht 2022; Edvardsson 2014; Smith 2018). Although nursing homes regularly offer activities to the residents, these activities tend to be passive, e.g. watching television and listening to music, and are often not perceived as meaningful by people with dementia, or are addressed to residents with better cognitive and functional status (Buettner 2003; Edvardsson 2014; Kristensen 2020). Hence, a lower cognitive function in people with dementia is associated with fewer social interactions and less participation in activities (Dobbs 2005; Edvardsson 2014). To be engaged in meaningful activities provides a sense of connectedness to self, others, and the environment, and helps maintain autonomy and identity in persons with dementia (Han 2016; Phinney 2007). Conversely, understimulation might magnify challenging behaviour, e.g. apathy, boredom, depression, loneliness and agitation (Cohen‐Mansfield 2011; Michelet 2022). People with dementia wish to be involved in activities which meet their interests and which are perceived as meaningful. To be engaged in activities perceived as meaningful is expected to increase peoples' quality of life (Cooney 2009; Edvardsson 2014; Murphy 2007; Phinney 2007; Vernooij‐Dassen 2007).
There is no clear definition of meaningful activities or occupation and therefore meaningfulness is often very broadly defined (Strick 2021). Activities are perceived as meaningful if they have a value for people with dementia and if they are tailored to their individual interests and preferences (Kristensen 2020; Strick 2021). Therefore, we use the term personally tailored activities rather than meaningful activities in this review.
Offering personally tailored activities to people with dementia primarily aims to improve psychosocial outcomes, e.g. agitation or quality of life, rather than to increase cognitive function or to improve particular skills. Since a remarkable sense of self‐identity can persist until late stages of dementia (Kristensen 2020; Mills 1997; Strick 2021), engagement in personally tailored activities could be beneficial for people in all stages of dementia.
Description of the intervention
Interventions offering personally tailored activities for people with dementia living in long‐term care facilities are likely to be complex interventions, comprising different methods of selecting activities tailored to people's interests and preferences, different types of activities, and different modes of delivering the activities (Craig 2008). We focus on interventions aimed at improving psychosocial outcomes (e.g. agitation or quality of life in people with dementia) rather than on interventions exclusively aimed at improving particular skills (e.g. basic activities of daily living, or cognitive function).
All interventions have to include an assessment of interests or preferences of the participants. Interventions can be based on specific models or concepts, e.g. the principles of Montessori or the concept of person‐centred care. The choice of activities offered should be based on the assessment of personal interests or preferences. Activities offered within the interventions include instrumental activities of daily living (e.g. housework, preparing a meal), arts and crafts (e.g. painting, singing), work‐related tasks (e.g. gardening), and recreational activities (e.g. games). The interventions can be delivered in groups or individually; duration and frequency of the sessions can differ. Providers of the interventions we expected to find include different professionals or a multidisciplinary team.
How the intervention might work
Being involved in personally tailored activities may evoke positive emotions, like interest, and reduce agitation. Also, participating in such activities can increase feelings of engagement which can reduce feelings of boredom and loneliness, and increase quality of life (Kristensen 2020; Michelet 2022; Strick 2021). Other expected benefits cover the evocation of autobiographical events (Guétin 2009), the preservation of a person's identity, an increase in the person's occupation and possible maintenance of their relationships (Kristensen 2020). These positive effects may reduce the use of psychotropic medication in people with dementia and may also result in benefits for the caregiver (e.g. increased sense of competence, decreased burden of care).
Why it is important to do this review
There is an increasing need for effective non‐pharmacological interventions to improve psychosocial outcomes in people with dementia in clinical practice. In several dementia guidelines, the use of non‐pharmacological interventions is recommended as a primary approach for behavioural and psychological symptoms (e.g. Fazio 2018; NICE 2018). Interventions offering personally tailored activities could be a promising approach due to their potential effects on agitation, quality of life and the level of engagement of people with dementia. Several studies have evaluated complex interventions offering personally tailored activities to people with dementia in long‐term care facilities. These interventions are complex in nature due to differences in underlying theoretical models, the components of the interventions, the types of activities offered, and the intensity and duration of delivery.
In order to assess the effects of complex interventions properly, a description of the interventions' components is required to ensure comparability and reduce heterogeneity (Guise 2017; Viswanathan 2017). Since the effectiveness of complex interventions is also influenced by implementation fidelity, this information should be incorporated too, e.g. adherence, exposure, quality of delivery, participants’ responsiveness and adherence.
This review updates the original Cochrane Review published in 2018 (Möhler 2018).
Objectives
To assess the effects of personally tailored activities on psychosocial outcomes for people with dementia living in long‐term care facilities.
To describe the components of the interventions.
To describe conditions which enhance the effectiveness of personally tailored activities in this setting.
Methods
Criteria for considering studies for this review
Types of studies
As planned in the published review protocol (Möhler 2012), we included individual or cluster‐randomised controlled trials, controlled clinical trials and controlled before‐after studies.
Types of participants
All people with dementia living in long‐term care facilities, irrespective of the stage of dementia, were eligible.
Types of interventions
All the interventions aimed to improve psychosocial outcomes by offering personally tailored activities to people with dementia in long‐term care. The aims of the interventions did not necessarily include the improvement of a particular skill. The interventions had to comprise two elements.
Assessment of the participants' present or former preferences for particular activities or interests. We accepted both unstructured assessments, e.g. asking for the interests of the person with dementia, or the use of validated tools, e.g. the self‐identity questionnaire (Cohen‐Mansfield 2010), or the NEO Five‐Factor Inventory (NEO‐FFI, Kolanowski 2005). This assessment had to be performed primarily with the person with dementia; however, relatives or health professionals could also be informants, e.g. in later stages of dementia.
An activity plan tailored to the individual participant's present or former preferences. We accepted activities of various kinds: instrumental activities of daily living (e.g. housework, preparing a meal); arts and crafts (e.g. painting, singing); work‐related tasks (e.g. gardening); and recreational activities (e.g. games). The intervention could be delivered by different professionals, e.g. nurses, occupational therapists, social workers or psychologists. The intervention could be delivered either to a group or to individual participants.
We excluded interventions which offered (1) only one specific type of activity (e.g. music or reminiscence), (2) specific care approaches (e.g. person‐centred care) which included the delivery of activities, (3) multi‐component interventions comprising drug treatment and the delivery of activities, and (4) interventions exclusively aimed at improving cognitive function or other particular skills (e.g. communication, basic activities of daily living).
We compared personally tailored activities against other types of psychosocial interventions, placebo interventions (e.g. non‐specific personal attention), usual or optimised usual care.
Types of outcome measures
Primary outcomes
Agitation or challenging behaviour, assessed by e.g. the Cohen‐Mansfield Agitation Inventory (CMAI).
Quality of life, assessed by e.g. Dementia Care Mapping, EuroQol (EQ‐5D).
Adverse effects of the interventions employed (e.g. injuries).
Secondary outcomes
Affect (i.e. expression of emotion), assessed by e.g. Observed Emotion Rating Scale.
Mood, assessed by e.g. Dementia Mood Picture Test.
Level of engagement, assessed by e.g. Observational Measurement of Engagement Assessment, Index of Social Engagement.
Other dementia‐related symptoms such as sleep disturbances, hallucinations or delusions, assessed by e.g. Neuropsychiatric Inventory (NPI).
Use of psychotropic medication.
Effect on the caregivers, e.g. caregivers' distress (assessed by e.g. Neuropsychiatric Inventory Caregiver Distress Scale (NPI‐D)), sense of competence (assessed by e.g. Sense of Competence Questionnaire (SCQ)), quality of life, health status (assessed by e.g. General Health Questionnaire (GHQ‐12)).
Cost.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Dementia and Cognitive Improvement Group's Specialized Register on 15 June 2022 using the following search terms: personally tailored OR individualized OR individualised OR individual OR person‐centred OR meaningful OR personhood OR involvement OR engagement OR engaging OR identity.
The Register is maintained by the Information Specialists of the Cochrane Dementia and Cognitive Improvement Group and contains studies in the areas of dementia prevention, dementia treatment and cognitive enhancement in healthy individuals. The studies are identified from:
monthly searches of a number of major healthcare databases: MEDLINE, Embase, CINAHL (Cumulative Index to Nursing and Allied Health Literature), PsycINFO and LILACS (Latin American and Caribbean Health Science Information database);
monthly searches of a number of trial registers: ISRCTN; UMIN (Japan's Trial Register); the World Health Organization (WHO) portal (which covers ClinicalTrials.gov; ISRCTN; the Chinese Clinical Trials Register; the German Clinical Trials Register; the Iranian Registry of Clinical Trials; and the Netherlands National Trials Register, plus others);
quarterly search of the Cochrane Library’s Central Register of Controlled Trials (CENTRAL);
six‐monthly searches of grey literature source: Web of Science Conference Proceedings.
Details of the search strategies used for the retrieval of reports of trials from the healthcare databases, CENTRAL and conference proceedings can be viewed in the ‘Methods used in reviews’ section within the editorial information about the Dementia and Cognitive Improvement Group.
We also performed additional searches in many of the sources listed above to ensure that the search for the review was as up to date and as comprehensive as possible. The search strategies we used can be seen in Appendix 1.
Searching other resources
We screened reference lists and citations of all potentially eligible publications for additional trials and for additional data (e.g. interventions development, process‐related data).
Data collection and analysis
Selection of studies
Two reviewers (RM, AR in the original review; RM, SC for this update) independently assessed all titles and abstracts obtained from the search for inclusion according to the Criteria for considering studies for this review. We resolved disagreements by discussion or, if necessary, we referred to a third reviewer (GM).
Data extraction and management
Two reviewers (RM, AR in the original review; RM, SC for this update) independently extracted data from all included publications using a standardised form. We checked results for accuracy and, in case of disagreement, called in a third reviewer (GM) to reach consensus.
For each study we extracted the following data: study design, characteristics of participants, baseline data, length of follow‐up, outcome measures, study results, and adverse effects. For each intervention we extracted the following information: method of assessing the individual preferences, types of activities offered, duration and frequency of the intervention's components, information of the implementation fidelity. Additionally, we collected information on the intervention's development (i.e. underlying theoretical considerations, components and delivery) and process‐related data. For cluster‐randomised trials, we also extracted estimates of the intracluster correlation coefficient (ICC) if possible. If necessary, we contacted study authors to obtain missing information.
Assessment of risk of bias in included studies
We followed the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017). We assessed risk of bias in each study for the following criteria: selection bias, performance bias, attrition bias, detection bias, and additional design‐related criteria for cluster‐randomised and non‐randomised trials. Two authors (RM, AR in the original review, and RM, SC for this update) independently assessed methodological quality of studies in order to identify any potential sources of systematic bias. In case of unclear or missing information, we contacted the corresponding author of the trial. We assessed the quality of evidence using the criteria proposed by the GRADE working group (Guyatt 2011).
Measures of treatment effect
For agitation and affect (including mood) we used the standardised mean difference (SMD), which is the absolute mean difference divided by the standard deviation (SD), since the included studies used different rating scales (see also Unit of analysis issues). We used the postintervention means of each scale's total score or subscore (for affect).
For continuous data that were not included in a meta‐analysis we calculated the mean difference (MD). If it was not feasible for us to calculate the MD, e.g. in case of substantial baseline imbalances, we presented the study results in narrative form, e.g. as mean values and standard deviation.
None of the trials included in this review reported dichotomous data of interest to this review.
Unit of analysis issues
For all studies, we investigated whether randomisation was performed on individual or group (cluster) level. For cluster‐randomised trials, we extracted information about the ICC, if available. Only one of the included cluster‐randomised trials reported the ICC, with values ranging from 0 to 0.3 (Wenborn 2013). We used the ICC values of the corresponding outcomes (0.19 for agitation and 0.09 for affect) from this study to incorporate the cluster effect in the studies without information on the ICC ‐ Cohen‐Mansfield 2007 and Cohen‐Mansfield 2012 ‐ by recalculating the effective sample size using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017). The numbers of included study participants and clusters in all three studies are comparable.
For cross‐over trials, we checked the risk of a carry‐over effect. In the study by van der Ploeg 2013, we found no evidence for the occurrence of a carry‐over effect; after the intervention sessions, the values of most outcomes returned to the level assessed before the activity sessions started. We used data from the complete study period for both conditions in our analysis since the authors did not report or offer results for the first period. We cannot be sure to have avoided a unit‐of‐analysis error; however, this bias is conservative, being expected to lead to an under‐estimate of the intervention effect (Higgins 2017). The second included cross‐over trial did not perform a washout period, and the authors mentioned that they observed a carry‐over effect (Mbakile‐Mahlanza 2020). Since the authors did not report or offer information about the first period, we did not include this study in the analyses.
One study included four study groups (three different intervention groups and one control group) (Kolanowski 2011). We excluded two intervention groups from the analysis since they did not meet our inclusion criteria (see Description of studies) and we included the two other groups in the analysis (one intervention and the control group).
Dealing with missing data
For all included studies, we extracted the numbers of participants lost to follow‐up, with reasons (see Characteristics of included studies). In case of missing information we contacted the study authors and asked for additional information.
Assessment of heterogeneity
We examined studies for clinical diversity in terms of characteristics of the interventions, participants, and outcomes. We combined data in meta‐analyses only if we considered the studies to be sufficiently clinically homogeneous. To test for statistical heterogeneity, we used the Chi² and I² statistics.
Assessment of reporting biases
In order to minimise the risk of publication bias we performed a comprehensive search, including multiple databases, snowballing techniques and searching trials registers to identify unpublished or ongoing trials. We did not investigate publication bias by means of a graphical funnel plot analysis since we included only a small number of studies. To detect cases of selective reporting in the included studies, we checked trial register information if available.
Data synthesis
We performed meta‐analyses for agitation, quality of life, positive and negative affect and for mood. In all cases, we used a random‐effects model as planned in the protocol since we found clinical diversity of the interventions and statistical heterogeneity (I² > 50%). One study reported different types of (positive and negative) affect (Van Haitsma 2015). To include this study in the meta‐analysis, we combined the different outcomes for positive affect and for negative affect, calculating a combined score for each. To calculate the variance of the combined means, we assumed a positive correlation of 0.5 between the individual outcomes of each category. In the meta‐analysis for mood, the assessment instrument used in one study differed in the direction of the scale (Kolanowski 2011). We recalculated the data of this study using the methods from the Cochrane Handbook for Systematic Reviews of Interventions (we multiplied the mean values by −1 as described in chapter 9.2.3.2) (Higgins 2017).
As in the first published version of this review, we did not perform meta‐analyses for any other outcomes and present the results in a narrative form.
Subgroup analysis and investigation of heterogeneity
Depending on the availability of sufficient data, we conducted subgroup analyses for studies with and without an active control group. In order to include in meta‐analyses one study which included both usual care and active control groups, we split the experimental intervention group using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Chapter 16.5.4) (Higgins 2017).
Sensitivity analysis
We performed a sensitivity analysis to explore the effects of including the study for which we calculated the combined outcome for positive and negative affect (see Data synthesis).
Summary of findings and assessment of the certainty of the evidence
We used the GRADE approach to assess the quality of evidence for the most important outcomes. We assessed the quality of the evidence by judging study limitations, consistency of effect, imprecision, indirectness, and publication bias (Guyatt 2011). To determine imprecision, we defined the borders for minimal important difference as defined by study authors; e.g. in case of quality of life (Wenborn 2013), and for the analyses using the SMDs, we used an effect size of 0.2, which is described as a small effect for SMD in the Cochrane Handbook for Systematic Reviews of Interventions (chapter 12.6.2) (Higgins 2017). We rated quality of evidence as high, moderate, low or very low (Guyatt 2011). We created a summary of findings table for the following outcomes: agitation, quality of life (self‐rating and proxy‐rating), adverse events, positive affect, negative affect, and mood.
Results
Description of studies
Results of the search
The search for this review update identified 6332 unique records (Figure 1). Two authors independently screened titles and abstracts against the inclusion criteria and excluded 6312 citations. We screened 20 publications in full text and included three new studies (Mbakile‐Mahlanza 2020; Travers 2017; Yuen 2019).
1.
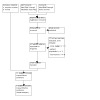
Study flow diagram
In total, we included 11 studies in this review update (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Kolanowski 2011; Mbakile‐Mahlanza 2020; Orsulic‐Jeras 2000; Richards 2005; Travers 2017; van der Ploeg 2013; Van Haitsma 2015; Wenborn 2013; Yuen 2019).
Included studies
Ten of the included studies were randomised controlled trials (RCT) (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Kolanowski 2011; Mbakile‐Mahlanza 2020; Richards 2005; Travers 2017; van der Ploeg 2013; Van Haitsma 2015; Wenborn 2013; Yuen 2019), and one study was a non‐randomised clinical trial (Orsulic‐Jeras 2000). Most of the studies used a parallel group design and randomised clusters (the units of allocation were nursing homes or nursing home wards) to the study groups (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012), individual participants (Kolanowski 2011; Richards 2005; Travers 2017; Van Haitsma 2015; Yuen 2019) or matched pairs of participants (Wenborn 2013). Two studies used a cross‐over design and randomised clusters (Mbakile‐Mahlanza 2020) and individual participants (van der Ploeg 2013) to the study groups. The duration of follow‐up ranged from 10 days (Cohen‐Mansfield 2007) to nine months (Orsulic‐Jeras 2000).
Setting and Participants
Six studies were conducted in the USA (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Kolanowski 2011; Orsulic‐Jeras 2000; Richards 2005; Van Haitsma 2015), three in Australia (Mbakile‐Mahlanza 2020; Travers 2017; van der Ploeg 2013), one in the UK (Wenborn 2013), and one in Hong Kong (Yuen 2019). Most studies recruited the participants from nursing homes and one study recruited from a special care unit (Orsulic‐Jeras 2000).
A total of 1339 participants were recruited, and 1071 participants completed the studies. The number of participants completing the studies ranged from 25 (Orsulic‐Jeras 2000) to 180 (Van Haitsma 2015).
The mean age of participants ranged from 78 to 88 years; this information was not reported in one study (Mbakile‐Mahlanza 2020). The majority of participants were female in most of the studies (63% to 92%), except in one study where the proportion of women was 48% (Richards 2005); no information was available in one study (Mbakile‐Mahlanza 2020).
The studies assessed cognitive function at baseline with different instruments, but almost all of the participants in the included studies had severe dementia. Seven studies used the Mini‐Mental State Examination (MMSE) (range 0 to 30, higher scores indicate more severe cognitive impairment). In most studies the mean MMSE scores were lower than 12 (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Orsulic‐Jeras 2000; Richards 2005; van der Ploeg 2013; Van Haitsma 2015; Wenborn 2013). In one study the scores ranged from 12 to 15 (Kolanowski 2011), and in one study that used the standardised Mini‐Mental State Examination (sMMSE) the mean scores were 19 (intervention group) and 16 (control group), respectively (Travers 2017). Mbakile‐Mahlanza 2020 used the Clinical Dementia Rating Scale (range 6 to 30, higher scores indicate more severe cognitive impairment). The mean value in the group with the intervention period first was approximately 21.9, and the group who received the control period first had a mean score of 26.8. Yuen 2019 assessed cognition with the Global Deterioration Scale, and the participants were in stage 4 and 5 (intervention group 66%, control group 83%, moderate cognitive decline), and in stage 6 and 7 (intervention group 34%, control group 17%, severe cognitive decline).
In five studies, agitation or challenging behaviour at baseline was an inclusion criterion for participants (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Kolanowski 2011; Travers 2017; Yuen 2019); and in one study, physical agitation at baseline was an inclusion criterion (van der Ploeg 2013). In four studies without such an inclusion criterion, all participants showed some form of agitation or challenging behaviour (Mbakile‐Mahlanza 2020; Orsulic‐Jeras 2000; Van Haitsma 2015; Wenborn 2013); one study provided no information about participants' agitation (Richards 2005) (see Characteristics of included studies).
Description of the interventions
Nine of the interventions offered personally tailored activities directly to the participants (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Kolanowski 2011; Orsulic‐Jeras 2000; Richards 2005; Travers 2017; van der Ploeg 2013; Van Haitsma 2015; Yuen 2019). In the study by Mbakile‐Mahlanza 2020, family members who regularly visit the people with dementia in the nursing home were trained to deliver the intervention. In the study by Wenborn 2013, members of the nursing staff were trained to deliver the personally tailored activities to the study participants.
In this section, we describe the included interventions using categories relevant for complex interventions (Hoffmann 2014; Möhler 2015).
Theoretical basis and components of the interventions
Choice of activities in the included studies was based on different theoretical models. The theoretical basis guided the selection of activities which could be offered to the participants, and the methods by which the interventions were individually tailored, i.e. how the activities were chosen for the individual participants. The interventions in Cohen‐Mansfield 2007 and Cohen‐Mansfield 2012 were based on the Treatment Routes for Exploring Agitation (TREA) framework. Kolanowski 2011 used the Need‐Driven Dementia‐Compromised Behavior (NDB) model and tested three different treatment conditions. Four studies used the principles of Montessori (Mbakile‐Mahlanza 2020; Orsulic‐Jeras 2000; van der Ploeg 2013; Yuen 2019). In three studies, the interventions were not based on a specific theoretical framework; however, in all studies the choice of activities followed predefined principles.
The Treatment Routes for Exploring Agitation (TREA) framework
The TREA framework provides a systematic approach for individualising non‐pharmacological interventions to unmet needs of people with dementia and agitation (Cohen‐Mansfield 2000). The TREA framework assumes that different types of agitated behaviours have different aetiologies. To create an individual intervention, the aetiology of the agitated behaviour must be identified. Individual interventions have to be developed based on the remaining abilities of the individual, his/her deficits, e.g. in sensory perception, cognition, and mobility, and personal preferences, e.g. past work, hobbies, important relationships, and sense of identity. With the TREA framework, individual needs and preferences of people with dementia exhibiting agitated behaviours could be assessed by using information from formal or informal caregivers (e.g. nursing staff or family members, respectively), or by observing the person's behaviour and environment. The TREA framework "can be viewed as a decision tree that guides caregivers through the necessary steps for exploring and identifying underlying unmet needs that contribute to agitated behaviours" (Cohen‐Mansfield 2007).
The studies by Cohen‐Mansfield 2007 and Cohen‐Mansfield 2012 used the TREA decision tree protocol to identify all agitated behaviours exhibited by the individual participants and the possible reasons for these behaviours. For each participant, a 4‐hour peak period of agitation was identified at baseline. The intervention was individualised and administered to each participant based on this peak period. Information on the needs and preferences of the participant was identified by providing his or her relatives with a questionnaire to complete, including items concerning the participant's medical history, self‐identity, and social functioning. Based on this assessment, corresponding activities were offered (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012).
Examples of activities offered were: individualised music, family videotapes and pictures, illustrated magazines and large print books, board games and puzzles, plush toys, sorting cards with pictures and words, stress balls, baby dolls, electronic massagers, pain treatment, outdoor trips to the garden of the nursing home, perfume, and Play‐Doh (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012).
Need‐Driven Dementia‐Compromised Behavior model
The NDB model defines behavioural symptoms as an indicator showing unmet needs of people with dementia (Algase 1996). Two aspects are described as potential reasons for behavioural symptoms: background risk factors (neuropathology, cognitive deficits, physical function, and premorbid personality); and proximal precipitating factors (qualities of the physical and social environment, and physiological and psychological need states) (Algase 1996). In this model, personally tailored activities can be seen as proximal factors that meet individual needs, since they aim to enrich the physical and social environment by matching the individual's background factors (Kolanowski 2005).
In the study by Kolanowski 2011, the activities offered based on the NDB model were individually tailored to the participants' cognitive and physical functional level and to their style of interest. Style of interest was defined by the participants' personality traits of extraversion (preferred amount of social stimulation) and openness (individual tolerance for the unfamiliar). Kolanowski 2011 assessed style of interest using form F from the Revised NEO Personality Inventory (NEO‐PI‐R, Costa 1992). For choosing the activities, both the participants' style of interest and the cognitive and physical functional levels were relevant. Kolanowski 2011 tested three treatment conditions based on this framework: (1) activities matched to the participants' (cognitive and physical) functional level, but opposite to their identified style of interest; (2) activities matched to the participants' style of interest, but not their functional level; (3) activities matched to both the participants' functional level and style of interest. Examples of activities offered were: games, puzzles, music (listening or making music), crafts (e.g. making a birdhouse), pet visits, sewing cards, cooking, painting (Kolanowski 2011). In this review, we considered only the activities matched both to the participants' functional level and style of interest to be personally tailored activities.
Principles of Montessori
The principles of Maria Montessori were originally developed to guide child education. This approach put emphasis on task breakdown, guided repetition, progression in difficulty from simple to complex, and the careful matching of demands to levels of competence. Meanwhile, the approach was adapted to be used with people with dementia. Activities offered to people with dementia "are designed to tap procedural memory which is better preserved than verbal memory while minimising language demands and providing external cues to compensate for cognitive deficits" (van der Ploeg 2013).
In the study by van der Ploeg 2013, a maximum of 10 activities were selected based on discussion with families about participants' former interests and hobbies. Mbakile‐Mahlanza 2020 adapted the intervention and offered training for family caregivers regularly visiting the nursing home residents to select 10 activities based on the residents' former interests and current physical abilities and language skills. Orsulic‐Jeras 2000 used the Myers Menorah Park/Montessori Assessment System (MMP/MAS) to individualise the activities. MMP/MAS is a Montessori‐based instrument and provides information on participants' areas of interest.
The intervention investigated by Yuen 2019 (DementiAbility Methods: The Montessori Way (DMMW)) aims to establish a meaningful engagement of people with dementia in individualised activities, roles, and routines in a prepared environment. The intervention comprise five steps.
Participants were invited via presenting the environment prepared for engagement in tailored activities.
Sequences of activities were demonstrated to facilitate participants to perform procedural movements and utilise activity materials.
Activities were tailored based on the participants' needs, interests, abilities, and skills.
The environment was prepared to be meaningful, purposeful, and home‐like, and the materials used were familiar and pleasing to the participant.
The activities were performed and role‐related tasks were accomplished with the participant and the next session was announced.
Examples of activities offered by Orsulic‐Jeras 2000 were: individual Montessori activities (with materials usually taken from the everyday environment e.g. utensils, bowls, flowers, baskets); group Montessori‐based activities (memory bingo); and a structured reading and discussion group. van der Ploeg 2013 offered activities like sorting cards or making puzzles from familiar photographs. Mbakile‐Mahlanza 2020 and Yuen 2019 did not report examples of the activities offered.
Individualised social activity intervention
The intervention by Richards 2005 was based on a conceptual framework which postulated (based on the two‐process model of sleep) that individualised activities can improve the homeostatic sleep drive and strengthen circadian processes; and that this may lead to improved nighttime sleep and decreased daytime sleep (Richards 2005).
The activities were preselected to match various interests as well as cognitive and functional abilities. About 100 different activities were identified by two therapeutic recreation specialists with more than 20 years of collective experience working with nursing home residents with dementia. A list was created comprising the following information for all activities: brief directions for use, which functional limitations preclude their use, and which previous interests of participants are associated with each activity. The activities were also grouped into activities which were appropriate for everyone, and those which were appropriate for participants with mild (MMSE > 15), moderate (MMSE 5 to 15), and severe (MMSE < 5) dementia. The activities offered were selected according to four characteristics of each participant: interests (work and leisure history), cognition and functional status (mobility, hearing, vision, fine motor skills), and napping patterns (time of unscheduled naps). This information was assessed by means of interviews with families, nursing staff, and participants, observation of participants' behaviour, chart review, and by using an Actigraph (for napping patterns).
Examples of the activities offered were: listening to music, petting a toy cat, tossing a ball, writing a letter, playing checkers, making a wreath, preparing and serving a snack (Richards 2005).
Occupational therapy programme
Wenborn 2013 offered an occupational therapy programme. The primary author, an occupational therapist with experience in working with older people with dementia, developed the intervention.
The intervention consisted of two components.
An assessment of the care home's physical environment, including recommendations on how it could be adapted and enhanced to enable the residents to engage in activities.
An education programme for nursing staff that aimed to enhance knowledge, attitudes and skills, based on the principles of experiential learning. The educational component comprised five two‐hour education sessions covering these topics: identify the residents' interests and abilities; choose and offer activities; review and record the outcomes. The care home manager joined the last session to agree an activity action plan for continued implementation of the programme. To ensure the use of the skills and tools in clinical practice, work‐based learning tasks with two residents were conducted between the educational sessions, and one‐to‐one coaching sessions with the primary investigator were held. The activities were personalised to each resident by the use of the Pool Activity Level Checklist (Wenborn 2008).
Individualised Positive Psychosocial Intervention
The study by Van Haitsma 2015 was based on two theoretical models: the Self‐Determination Theory (Deci 2000); and Broaden‐and‐Build Theory (Fredrickson 2001). The Self‐Determination Theory proposes that all people have innate needs for autonomy and competence, which must be fulfilled for psychological well‐being; and the Broaden‐and‐Build Theory focusses on the critical role of positive emotions to improve the person's well‐being. The study is described as being based on the work of Kolanowski 2011, but there were no details about how this study contributed to the design of the intervention or the study.
The Individualised Positive Psychosocial Intervention (IPPI) offered five basic types of activities reflective of the most common preferences.
Physical exercises (e.g. outdoor walk, work with clay).
Music (e.g. singing or listening to a favourite artist).
Reminiscence (e.g. reviewing family photos, writing letters).
Activities of daily living (e.g. manicures, preparing a snack).
Sensory stimulation (e.g. hand massage with lotion, smelling fresh flowers).
From each group, two or more specific activity options were offered (a total of 30 activity options). The activities were selected by researchers and clinicians for each resident based on the Preferences for Everyday Living Inventory‐Nursing Home (PELI‐NH; Van Haitsma 2000). The information was taken directly from the participant or from a family member, activity therapist, or other direct care staff.
BE‐ACTIV
The BE‐ACTIV intervention was originally developed by Meeks 2008 to increase the engagement in activities of nursing home resident with depression. The intervention was based on the integrative behavioural model of depression in older adults. The aim of the intervention is to address reduced positive affect by systematically increasing positive events and activities (Meeks 2008). Travers 2017 adapted the intervention for people with mild to moderate dementia and depression, and to the local and cultural context of Australia.
A Mental Health Therapist offered weekly individual sessions for each participant to identify pleasant activities or events tailored to the participants' abilities and the nursing home environment, and to develop an individual activity plan that aimed to increase the frequency of those events. Furthermore, the events in the previous week were reviewed to identify barriers for being engaged in the planned pleasant events, solve problems and to revise the plan for the next week, if necessary. In addition, two 90‐minutes sessions with information about depression and dementia in nursing home residents was offered to staff members and volunteers of the participating nursing homes. In each nursing home, one staff member was nominated to be actively involved as co‐therapist during the intervention period. This staff member attended the therapist's sessions with the participants in the first, fourth and eighth week, and supported the engagement of the participant in the individually selected pleasant activity or event during the intervention period. If the participants agreed, the co‐therapist also invited the participant's relatives to assist with the implementation of pleasant activities or events, for example with activities outside the nursing home.
The most often selected pleasant activities or events were: reading a book, newspaper or magazine; being pushed around the grounds in a wheelchair or scooter; sitting outside in the sun or fresh air; having a hand massage or manicure; and attending an event in the nursing home.
Feasibility/pilot test
Richards 2005 tested their intervention in a pilot study (Richards 2001). Kolanowski 2011 and Cohen‐Mansfield 2012 used previous studies as a pilot‐test for their interventions (Kolanowski 2005; Cohen‐Mansfield 2007). The intervention by Orsulic‐Jeras 2000 was based on experiences from an earlier project. Mbakile‐Mahlanza 2020 investigated an intervention that was already evaluated by van der Ploeg 2013Travers 2017 conducted a pilot study investigating an adapted version of an intervention that was already evaluated in a different population (people with depression, but no dementia; Meeks 2008). Prior to the Yuen 2019 study, the intervention had been implemented in practice projects in Hong Kong and some case series had been conducted in Canada, but no pilot study was conducted. The remaining four studies did not provide any information on a feasibility or pilot‐test (Cohen‐Mansfield 2007; van der Ploeg 2013; Van Haitsma 2015; Wenborn 2013).
Delivery of the intervention
In most studies, the interventions were delivered directly to the study participants (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Kolanowski 2011; Orsulic‐Jeras 2000; Richards 2005; Travers 2017; van der Ploeg 2013; Van Haitsma 2015; Yuen 2019). In the study by Richards 2005, activities were delivered individually; however, when the same activity was selected for more than one participant at the same time, the activity was offered in groups of up to three participants. The intervention by Orsulic‐Jeras 2000 comprised both individual and group activities (see above: 'Theoretical basis and components of the interventions ‒ Principles of Montessori'). In the study by Wenborn 2013, members of the nursing staff were trained to select, plan and deliver the activities within daily care, and Mbakile‐Mahlanza 2020 trained family members to offer the activities during their visits to the nursing home.
Although all studies based the selection of activities on an assessment of the participants' present or former preferences, no information was presented in any study about the number of participants who were able to express their individual interests or preferences. Also, no study reported information about the proportion of participants for whom preferences and interests were assessed through the primary caregiver or family members.
There were differences between studies in the number and frequency of sessions delivered, and in the length of the follow‐up period. The frequency of delivering the activity sessions ranged from daily (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Richards 2005) to once per week (Travers 2017). Most studies included a short follow‐up period, from 10 consecutive days (Cohen‐Mansfield 2007) to up to three weeks (Van Haitsma 2015). Two studies had a longer follow‐up period: eight weeks in Travers 2017 and nine months in Orsulic‐Jeras 2000. A detailed overview of the delivery of the interventions is displayed in Table 2 (see also Characteristics of included studies).
1. Delivery of the intervention.
| Reference | Delivered by | Frequency and duration of the sessions | Duration of follow‐up |
| Cohen‐Mansfield 2007 | Research assistant (no further information reported) | Daily; up to 4 h per day (peak period of agitation) | 10 consecutive days |
| Cohen‐Mansfield 2012 | Research assistant (no further information reported) | Daily; up to 4 h per day (peak period of agitation) | 2 weeks |
| Kolanowski 2011 | Research assistant (no further information reported) | 5 days per week; up to 20 minutes twice per day (morning and afternoon) | 4 weeks (3 weeks intervention period plus 1 week postintervention period) |
| Mbakile‐Mahlanza 2020 | Family members (trained by the senior researcher who had experiences with the Montessori approach, 3‐hour group sessions in the nursing home, 30 min to assist the family members filling out the baseline questionnaire, one hour explaining the theoretical basis of Montessori activities in dementia, 90 min for selecting and practising possible activities in small groups) | 2 sessions per week (30 min) in a quiet room with no distractions. Family members interacted with the residents while engaging with the activities. | 2 weeks |
| Orsulic‐Jeras 2000 | Trained volunteer, nursing assistant or activities therapist | At least twice a week; individual activities 10 to 30 min, group activities 25 to 45 min, QAR 30 min to 1 h | 9 months |
| Richards 2005 | Nursing assistant (no further information reported) | Daily; several sessions 15 to 30 min (max 1 to 2 h per day), between 9:00 a.m. and 5:00 p.m. | 21 consecutive days |
| Travers 2017 | Mental Health Therapist (qualified social worker experienced in working with older people with and without cognitive impairment), supported by nominated staff members (co‐therapists) | One session per week (45 min/week) | 8 weeks |
| van der Ploeg 2013 | Activity facilitators (psychologists or higher‐degree psychology students, received regular personal supervision throughout the study) | Twice a week; 30‐min sessions (at times when participants' target behaviour was most frequent) | 4 weeks (2 weeks per condition) |
| Van Haitsma 2015 | Certified nursing assistants (no further information reported) | 3 days per week; 10 min per session (not during mealtimes or shift change) | 3 weeks |
| Wenborn 2013 | Primary investigator (occupational therapist with extensive experience of working with older people with dementia) | Not reported; five 2‐h educational sessions for nursing staff | 28 weeks (16 weeks intervention period plus 12 weeks post‐intervention period) |
| Yuen 2019 | Certified DMMW practitioner (no further information provided) | 3 sessions per week, 45 min. | 2 weeks |
DMMW = DementiAbility Methods: The Montessori Way; QAR = question asking reading group
Five studies used materials guiding the training and the implementation of the interventions (Kolanowski 2011; Travers 2017; van der Ploeg 2013; Van Haitsma 2015; Wenborn 2013): Wenborn 2013 used written manuals or guidelines, and Kolanowski 2011 used a treatment fidelity plan. In the Travers 2017 study, the study coordinator additionally contacted the therapist once per week during the intervention period to improve the treatment fidelity and to address any difficulties that arose.
Information about the implementation process and the implementation fidelity was assessed in five studies (Cohen‐Mansfield 2012; Kolanowski 2011; Travers 2017; Van Haitsma 2015; Wenborn 2013). Cohen‐Mansfield 2012 used a questionnaire to assess information about the implementation process and barriers and facilitators. Kolanowski 2011 used a treatment fidelity plan to ensure the introduction of the intervention as planned. Also, the research assistants paid attention to potential confounding factors (e.g. pain, thirst, poor environmental conditions). Treatment fidelity was checked for 10% of the intervention sessions. Re‐training took place if the intervention was not implemented according to the protocol. Only one deviation from the protocol occurred. Van Haitsma 2015 assessed implementation fidelity during randomly selected sessions. A member of the research team observed compliance with study procedures in both the intervention and active control group. Overall, adherence to protocol was 68%, with higher rates in the intervention group (73%) compared to the active control condition (60%). In the study by Wenborn 2013, the number of staff attending each session was recorded, and feedback regarding the work‐based learning activities was collected from nursing staff and residents. A mean staff attendance of 73% was recorded for the education sessions (range 63 to 86) and a mean uptake of 81% for the individual coaching sessions (range 49 to 100). Reasons for non‐attendance at the sessions included: being off duty (22%); annual leave (20%); on duty but not available (14%); sick leave (12%); study leave (11%); staff personal commitment (11%); and left the care home (9%). No information was collected on the amount of activities delivered to the residents by the nursing staff. Travers 2017 used qualitative interviews with nursing staff or volunteers (n = 14) to collect data about the target group's opinion regarding the feasibility of the intervention, implementation fidelity and the perceived impact on participants’ mood or behaviour.
Characteristics of the control conditions
Six studies offered an active control condition (Kolanowski 2011; Mbakile‐Mahlanza 2020; Travers 2017; van der Ploeg 2013; Van Haitsma 2015; Yuen 2019). The study by Kolanowski 2011 offered activities to the participants that were functionally challenging and opposed to the participant's style of interest (based on the NDM model). In the study by Mbakile‐Mahlanza 2020, family members of the participants received an initial three‐hour group session (30 minutes to complete the baseline questionnaires, 90 minutes of education about dementia, 60 minutes of discussion of the presented materials in small groups). Two active control sessions were conducted each week for two weeks. The family members were asked to read a newspaper with the resident to provide them with some structure. van der Ploeg 2013 used non‐personalised one‐to‐one interactions aimed at engaging the participants in social interaction, e.g. general conversations or conversation based on newspaper stories and pictures. Van Haitsma 2015 offered standardised one‐to‐one social interaction activities (e.g. discussing a magazine). In the study by Travers 2017, a volunteer member of the nursing home staff engaged the participants in the control group in a walking and talking intervention for 30 minutes, based on the participants' walking ability and preferences (sitting and talking was also possible). The volunteers were to have used open‐ended questions and stimuli from the environment to engage the resident in conversation. Yuen 2019 offered six sessions (45 minutes each) with structured social activities. Each session comprised an introduction, the implementation of preset activities (i.e. discussion on newspaper topics and pictures; table games), and a round‐up.
In six studies, the control condition was usual care (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Orsulic‐Jeras 2000; Richards 2005; Van Haitsma 2015; Wenborn 2013). Van Haitsma 2015 offered both an active control group and a usual care control group. In the study by Orsulic‐Jeras 2000, the control group received the usual activities of the centre (individual, small‐group, and large‐group activities, including: bingo, storytelling, trivia, exercise, modified sporting activities, watching movies, discussion groups, musical programmes, sensory stimulation, and activities based on the participants' interests and hobbies; delivered by an activity therapist or nursing assistants). Cohen‐Mansfield 2007 and Cohen‐Mansfield 2012 offered a presentation to the nursing staff about the different forms of agitation, their aetiologies, and possible non‐pharmacological intervention; but this was not counted as active control group. Three studies reported no further information about usual care (Richards 2005; Van Haitsma 2015; Wenborn 2013).
Outcomes and data collection methods
Primary outcomes
Agitation
Eight studies assessed agitation (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Kolanowski 2011; Orsulic‐Jeras 2000; van der Ploeg 2013; Van Haitsma 2015; Wenborn 2013; Yuen 2019).
Cohen‐Mansfield 2007 and Cohen‐Mansfield 2012 used the Agitation Behavior Mapping Instrument (ABMI; Cohen‐Mansfield 1989a). ABMI is a 19‐item instrument to rate agitation in nursing homes by direct observation (a higher score indicates more agitation).
Kolanowski 2011 and Orsulic‐Jeras 2000 used the Cohen‐Mansfield Agitation Inventory (CMAI; Cohen‐Mansfield 1989b), and Yuen 2019 used the Chinese version (CMAI‐C). The CMAI is a proxy‐rating instrument used by nurses to assess agitation and comprises 29 agitated behaviours. Each behaviour is rated on a 7‐point scale (1 = never to 7 = several times an hour). Higher scores indicate greater agitation.
Kolanowski 2011 also used the Passivity in Dementia Scale (PDS), a proxy‐rating instrument with 53 items (range −16 to 40, a higher score indicates less passivity; Colling 2000).
van der Ploeg 2013 selected one specific behaviour for each participant based on the nurses’ rating in a two‐week period before baseline assessment by the CMAI. For each participant, the nurse directly observed whether this specific behaviour occurred within 30 minutes in one‐minute intervals. The observation resulted in an individual behaviour score for each participant ranging from 0 to 30 points per session. The outcome score (mean and SD) was calculated using the observations from all sessions (n = 1.056 observations from all study participants). A higher score indicates a more frequent behaviour.
Van Haitsma 2015 assessed different categories of verbal and nonverbal behaviour by direct observation. Within a 10‐minute "behaviour stream", the onset and cessation of specific behaviours were recorded. Verbal behaviour was categorised as very negative (swearing, screaming, mocking), negative (incoherent, repetitious statements, muttering), positive (coherent conversation, responding to questions), very positive (complimenting, joking) or no verbal behaviour. Nonverbal behaviour was categorised as: psychosocial task (manipulates or gestures towards an object, engages in conversation), restlessness (pacing, fidgeting, disrobing), null behaviour (stares with fixed gaze, eyes unfocused), eyes closed (sits or lies with eyes closed), aggression (hitting, kicking, pushing, scratching, spitting), uncooperative (pulling away, saying “no”, turning head or body away), and positive touch (appropriate touching, hugging, kissing, hand holding). Higher scores indicated a higher frequency of the behaviour.
Wenborn 2013 used the Challenging Behaviour Scale (CBS; Moniz‐Cook 2001) to assess the incidence, frequency and severity of challenging behaviour. The CBS is a 25‐item proxy‐rating instrument used by nurses (higher scores indicate more challenging behaviour).
Quality of life
Quality of life was assessed in two studies (Travers 2017; Wenborn 2013), and both studies used the Quality of Life in Alzheimer’s Disease (QoL‐AD) scale. The instrument comprises 15 items, each rated on a 4‐point scale (1 (poor QoL) to 4 (excellent QoL), range 15 to 60, higher scores indicate a higher quality of life; Logsdon 1999).
Secondary outcomes
Affect
Cohen‐Mansfield 2007 and Cohen‐Mansfield 2012 used Lawton’s Modified Behavior Stream (LMBS; Lawton 1996), covering the following modes of affect: pleasure, interest, anger, anxiety, and sadness. A higher score indicates greater display of the affect.
Four studies used the Philadelphia Geriatric Center Affect Rating Scale (ARS; Lawton 1996), covering the following modes of affect: pleasure, anger, anxiety, sadness, interest, and contentment (Kolanowski 2011; Mbakile‐Mahlanza 2020; Orsulic‐Jeras 2000; van der Ploeg 2013). A higher score indicates greater display of the affect. In the study by Kolanowski 2011, anger and sadness were not used due to the inability to obtain adequate reliability for their measure. Two studies categorised results as positive or negative affect (Cohen‐Mansfield 2012; van der Ploeg 2013); van der Ploeg 2013 used also the category 'neutral affect'. van der Ploeg 2013 calculated outcome scores (mean and SD) based on the observations from all sessions (n = 1.056 observations from all study participants).
Van Haitsma 2015 assessed the duration of different types of affect by direct observation within a 10‐minute "behaviour stream". Positive affect included pleasure (smiling, laughing, singing, nodding) and alertness (eyes following object, intent fixation on object or person, visual scanning, eye contact maintained). Negative affect included sadness (crying, tears, moaning, sighing, mouth turned down at corners), anger (clenched teeth, grimace, pursed lips, eyes narrowed), and anxiety (furrowed brow, motoric restlessness, repeated or agitated motion, hand wringing, leg jiggling). A higher score indicates more frequent occurrence of the specific type of affect.
Wenborn 2013 assessed anxiety using the Rating Anxiety in Dementia scale (RAID; Shankar 1999), with scores of 11 or above indicating clinical anxiety.
Engagement
Three studies measured engagement. Kolanowski 2011 assessed time on task (minutes/seconds; range 0 to 20 minutes), and intensity of participation (ranging from 0 ("dozing") to 3 ("actively engaged"), based on Kovach 1998). Orsulic‐Jeras 2000 used the Myers Research Institute Engagement Scale (MRI‐ES; Judge 2000) (range 0 to 600, higher score indicates more engagement).
Mbakile‐Mahlanza 2020 and van der Ploeg 2013 used the Menorah Park Engagement Scale (MPES) (range 0 to 30, higher values indicate more engagement) (Skrajner 2007). Both scales assessed four types of engagement: constructive engagement (e.g. actively handling objects or talking); passive engagement (e.g. watching or listening); self‐engagement (e.g. fiddling with clothes); and non‐engagement (e.g. a blank stare). van der Ploeg 2013 combined non‐ and self‐engagement into the category 'negative engagement'; and calculated outcome scores (mean and SD) based on the observations from all sessions (n = 1.056 observations from all study participants).
Mood
For this outcome, we included studies that directly assessed mood and studies that assessed depression.
The study by Kolanowski 2011 assessed mood with the Dementia Mood Picture Test (range 0 to 12, higher score indicates more positive mood; Tappen 1995).
Three studies assessed depression. Orsulic‐Jeras 2000 and Wenborn 2013 used the Cornell Scale for Depression (CSD; range 0 to 38; score ≥ 8 indicates depression; Alexopoulos 1988). Travers 2017 used the Geriatric Depression Scale, including 12 items about symptoms of depression suitable for older people with cognitive impairment (range from 0 to 12, a score ≥ 4 indicates probable depression).
Other outcomes (residents)
Richards 2005 assessed the daytime minutes slept, nighttime minutes to sleep onset, minutes slept, minutes awake, sleep efficiency, and the day/night sleep ratio using an Actigraph (motion‐sensing device), as well as the costs of implementing the intervention.
Caregiver outcomes
Mbakile‐Mahlanza 2020 assessed several caregiver outcomes: caregivers' quality of life (assessed by Carer‐QoL, seven‐item questionnaire); carer‐resident's quality of relationship (instrument with a 5‐point Likert scale and the Mutuality Scale of the Family Caregiving Inventory with 15 items); carer’s mastery (assessed by the Pearlin Mastery Scale); and carer’s mood (assessed by the Center for Epidemiological Studies Depression Scale (CES‐D), a 20‐item self‐reported scale of depressive symptoms, including mood, self‐esteem, energy, relationships, sleep and appetite).
Costs
Only one study assessed intervention cost, e.g. costs for staff training, delivery of activities and administration of the intervention (Richards 2005).
None of the included studies performed an economic evaluation.
Duration of the effects
Two studies aimed to assess the duration of the intervention effects. Kolanowski 2011 assessed the effect one week after the intervention period was completed, and van der Ploeg 2013 additionally assessed all outcomes after each session.
Excluded studies
We excluded studies because the intervention or the study design did not meet our inclusion criteria. See Characteristics of excluded studies for the reasons for exclusion of the studies screened in full text.
Risk of bias in included studies
For the original review we contacted corresponding authors of all studies and asked for additional information on methodological details that were not reported in the publications (we sent one reminder to all non‐responding authors). Five authors responded to our request (A Kolanowski, J Cohen‐Mansfield, S Orsulic‐Jeras, E van der Ploeg, K Van Haitsma), and four authors offered additional information; one author did not, for personal reasons.
We also contacted corresponding authors of all newly included studies and for one study we also contacted the senior author (Mbakile‐Mahlanza 2020). We sent one reminder to all authors. None of the contacted authors responded to our request.
The methodological quality of the included studies varied. We judged the risk of bias as unclear in at least two domains in all studies, and seven studies additionally had a high risk of bias in at least one domain (Cohen‐Mansfield 2007; Mbakile‐Mahlanza 2020; Orsulic‐Jeras 2000; Richards 2005; Travers 2017; van der Ploeg 2013; Van Haitsma 2015).
For further information see Characteristics of included studies, Figure 2, and Figure 3.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
The randomisation sequence was adequately generated in six studies (Cohen‐Mansfield 2012; Kolanowski 2011; Travers 2017; van der Ploeg 2013; Van Haitsma 2015; Wenborn 2013). Van Haitsma 2015 used a two‐step randomisation procedure; in the first step the included nursing home units were allocated to deliver one of the two active treatments (intervention or active control); and in the second step, the eligible residents in each ward were allocated to the active treatment or usual care (eligible participants were identified before allocation). In the study by Mbakile‐Mahlanza 2020, baseline imbalances in some criteria occurred, e.g. time the participants lived in the nursing home, dementia severity and physical agitation. These differences might be a result of the small sample size, but we have insufficient information to permit judgement of ‘low risk’ or ‘high risk'. Three studies did not report sufficient information about the method of sequence generation (Cohen‐Mansfield 2007; Richards 2005; Yuen 2019). We considered risk of bias in this domain to be unclear for Richards 2005 and Yuen 2019. In the study by Cohen‐Mansfield 2007 two clusters were not randomly assigned to the study groups, because the facility managers had a strong preference for the intervention group; we judged the risk of bias in this domain to be high.
Allocation to the study groups was adequately concealed in two studies (Kolanowski 2011; Wenborn 2013). Five studies reported insufficient information about allocation concealment (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Mbakile‐Mahlanza 2020; Richards 2005; Yuen 2019) (risk of bias judged to be unclear); and in three studies allocation was not concealed (Travers 2017; van der Ploeg 2013; Van Haitsma 2015) (risk of bias judged to be high).
In the study by Orsulic‐Jeras 2000 group allocation was not performed at random. Participants were allocated to the groups using matching based on the MMSE score, MMP/MAS and the reading subtest of the Wide Range Achievement Test (WRAT3). We considered this study to be at high risk of selection bias.
Blinding
In six studies, blinding of participants and personnel was not possible since the participants in the control group did not receive an intervention (usual care) (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Orsulic‐Jeras 2000; Richards 2005; Van Haitsma 2015; Wenborn 2013). In three of these studies, clusters were allocated to the study groups, and we have insufficient information whether this might have led to a risk of bias (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Wenborn 2013). Three studies allocated individual participants to the study groups and personnel cared for participants in both the intervention and the control group (Orsulic‐Jeras 2000; Richards 2005; Van Haitsma 2015). For these studies we judged risk of performance bias to be high. Of the five studies that offered an active control group, blinding of participants and personnel was adequate in two studies (Kolanowski 2011; Yuen 2019). Two studies reported insufficient information; one of these studies allocated clusters to the study groups, and we have insufficient information to permit judgement of 'low risk' or 'high risk' of bias (Mbakile‐Mahlanza 2020). The other study allocated individual participants to the study groups and personnel cared for participants in both the intervention and the control groups. Although this study offered an active control group, personnel were aware of the study methods, and we judged risk of performance bias to be high (Travers 2017). In one study, personnel not blinded to group allocation delivered both the intervention and the active control activities; we judged the risk of performance bias to be high in this study (van der Ploeg 2013).
Outcome assessors were blinded to group allocation in three studies (Kolanowski 2011; Wenborn 2013; Yuen 2019). In Richards 2005, outcome assessors were not blinded to group allocation, but sleep‐related outcomes were assessed by an objective measure (Actigraphy). We judged risk of detection bias to be low. In two studies, unblinded raters assessed study outcomes (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012). For a subgroup of intervention participants, research assistants performed a blinded assessment based on videotaped activity sessions. There was high agreement between the blinded and unblinded ratings. In the study by Van Haitsma 2015, trained research assistants used a technical device to collect outcome data, but no information about blinding was reported. For these studies, we have insufficient information to permit judgement of ‘low risk’ or ‘high risk'. In four studies unblinded staff collected outcome data, and we judged risk of detection bias to be high (Mbakile‐Mahlanza 2020; Orsulic‐Jeras 2000; Travers 2017; van der Ploeg 2013).
Incomplete outcome data
Attrition rates were low and reasons for attrition were documented in seven studies, so we judged the risk of attrition bias to be low (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Kolanowski 2011; Travers 2017; Van Haitsma 2015; Wenborn 2013; Yuen 2019).
The attrition rate in Richards 2005 was also low, but the study did not report any information about the group allocation of the participants lost to follow‐up. Mbakile‐Mahlanza 2020 reported an attrition rate of 20%, but did not report any information about the study period in which the participants were lost to follow‐up (intervention or control condition first; cross‐over trial), or the reasons for attrition. In the study by van der Ploeg 2013, the attrition rate was more than twice as high as anticipated (anticipated attrition rate 10%; actual attrition rate 23% (13/57)). In the study by Orsulic‐Jeras 2000, only 25 of 44 participants completed the study, but the group allocation of the participants lost to follow‐up was not reported. We considered the risk of attrition bias for these studies to be unclear, since there was no evidence that attrition was due to the intervention.
Selective reporting
Six studies were registered, two studies prospectively (Mbakile‐Mahlanza 2020; Travers 2017), and a study protocol was available for the Mbakile‐Mahlanza 2020 study. However, Mbakile‐Mahlanza 2020 was planned as a cluster‐randomised trial with a waiting‐control group design, but conducted as a cross‐over trial, and the primary endpoint defined in the study register was changed in the final publication. We judged risk of reporting bias to be high. Travers 2017 reported only the primary outcome defined in the study registry, and we judged risk of reporting bias to be unclear. The other studies were registered retrospectively (Cohen‐Mansfield 2012; Kolanowski 2011; van der Ploeg 2013; Wenborn 2013), or not registered (Cohen‐Mansfield 2007; Orsulic‐Jeras 2000; Richards 2005; Van Haitsma 2015; Yuen 2019), and we judged risk of reporting bias to be unclear.
Other potential sources of bias
We rated the two cross‐over trials to be at high risk for other bias. Mbakile‐Mahlanza 2020 did not include a wash‐out period and a carry‐over effects was observed. In van der Ploeg 2013 no paired data were available, only data from the entire study period.
Effects of interventions
See: Table 1
Primary outcomes
Agitation
We performed a meta‐analysis for agitation, including seven studies (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Kolanowski 2011; Orsulic‐Jeras 2000; van der Ploeg 2013; Wenborn 2013; Yuen 2019). One study was not included in the meta‐analysis because the assessed types of behaviours were not comparable with the other studies (Van Haitsma 2015).
We used the SMD, calculated from mean values assessed during or directly after the intervention period or session. For two studies we recalculated the number of participants to incorporate the cluster effect, using an estimate of the ICC (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012 ‒ see Unit of analysis issues). We used a random‐effects model since there was clinical diversity and evidence for moderate heterogeneity (I² = 50%). Higher scores indicate more severe agitation.
We found low‐certainty evidence (downgraded for risk of bias and imprecision) that personally tailored activities may slightly reduce agitation (SMD −0.26, 95% CI −0.53 to 0.01; I² = 50%; 7 studies, 485 participants; Analysis 1.1; Figure 4). We conducted a subgroup analysis comparing the four studies with a usual care control group and the three studies with an active control intervention. There was no statistically significant subgroup effect and no evidence that heterogeneity could be explained by the nature of the comparator intervention (test for subgroup differences P = 0.60, I² = 0%). We observed no other likely explanations for the heterogeneity based on other characteristics of the studies, e.g. population, intervention or outcome measures.
1.1. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 1: Agitation
4.

Forest plot (1.1 Agitation)
In the study by Van Haitsma 2015, the outcomes of general restlessness, aggression, uncooperative behaviour, very negative and negative verbal behaviour seemed to best represent agitation. Higher scores indicate more severe agitation. We found low‐certainty evidence (downgraded for risk of bias and imprecision) that personally tailored activities may slightly improve general restlessness compared to usual care (MD −16.97, 95% CI −18.80 to −15.14; 137 participants; Analysis 1.2), but may make little or no difference in comparison with an active control group (MD 1.22, 95% CI −1.14 to 3.58; 87 participants; Analysis 1.2). Aggression and uncooperative behaviours were rarely observed in all groups; we found low‐certainty evidence (downgraded for risk of bias and imprecision) that personally tailored activities may have little or no effect on aggression and uncooperative behaviours (aggression: personally tailored activities vs usual care MD 0.06, 95% CI 0.05 to 0.07; 137 participants; personally tailored activities vs active control MD −0.06, 95% CI −0.07 to −0.04; 87 participants; uncooperative behaviour: personally tailored activities vs usual care MD 0.01, 95% CI −0.00 to 0.02; 137 participants; personally tailored activities vs active control MD −0.13, 95% CI −0.15 to −0.12; 87 participants; Analysis 1.2). We also found low‐certainty evidence (downgraded for risk of bias and imprecision) that personally tailored activities may slightly increase very negative verbal behaviour in comparison with usual care (MD 7.75, 95% CI 5.51 to 9.99; 137 participants), but may reduce very negative verbal behaviour in comparison with an active control group (MD −29.33, 95% CI −32.22 to −26.44; 87 participants; Analysis 1.2). For negative verbal behaviours, we found low‐certainty evidence (downgraded for risk of bias and imprecision) that personally tailored activities may slightly increase negative verbal behaviour in comparison with usual care (MD 21.68, 95% CI 17.66 to 25.70; 137 participants; Analysis 1.2), and may make little or no difference to negative verbal behaviour in comparison with an active control group (MD 3.07, 95% CI −2.13 to 8.27; 87 participants; Analysis 1.2).
1.2. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 2: Behaviours (van Haitsma 2015)
Quality of life
Two studies investigated the effects of personally tailored activities on quality of life using the same instrument, the QoL‐AD (Nursing Home version) (Travers 2017; Wenborn 2013). In the study by Travers 2017 the trial co‐ordinator assessed quality of life. In Wenborn 2013 study personnel assessed quality of life and a small group of participants, who were able to complete the assessment, rated their quality of life themselves (n = 42 out of n = 139). We used a minimum important difference of three points on the scale used, as defined by Wenborn 2013 (higher scores indicate better quality of life).
For self‐rated quality of life, there was low‐certainty evidence from one study (downgraded two levels for imprecision) indicating little or no difference between personally tailored activities and usual care (MD 0.26, 95% CI −3.04 to 3.56; 42 participants; Wenborn 2013).
For proxy‐rated quality of life, we found low‐certainty evidence (downgraded one level for risk of bias and imprecision) that personally tailored activities may result in little to no difference in quality of life in comparison with usual care or an active control group (MD ‐0.83, 95% CI ‐3.97 to 2.30; I² = 51%; 2 studies, 177 participants; Analysis 1.3; Figure 5). The moderate heterogeneity between the studies may be explained by some differences in the study populations and control groups. Travers 2017 included participants with mild to moderate dementia and depression and had an active control group, while Wenborn 2013 did not select participants with depression and the control group did not receive any intervention (usual care).
1.3. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 3: Quality of life (proxy‐rated)
5.

Forest plot (1.3 Quality of life ‐ proxy‐rate)
Adverse effects
Only two studies assessed adverse effects, and no adverse effects were observed in either study (Cohen‐Mansfield 2012; Kolanowski 2011). No information about adverse effects was reported in the other studies.
Secondary outcomes
Affect
Only one of the newly included studies assessed affect (Mbakile‐Mahlanza 2020), but the results of this cross‐over trial were not included in the analysis since a carry‐over effect occurred and no data of the first period of this trial were available.
We performed meta‐analyses for positive and negative affect (including six studies in each analysis) and mood (including three studies). For positive affect, we used the results from four studies assessing pleasure (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012; Kolanowski 2011; Orsulic‐Jeras 2000), from one study assessing a combination of pleasure and contentment (van der Ploeg 2013), and for one study we calculated a combination of pleasure and alertness (Van Haitsma 2015; see Data synthesis).
For negative affect, we used the following study data: negative affect calculated from anger, anxiety, and sadness (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012), negative affect calculated from anger, sadness, and anxiety/fear (van der Ploeg 2013), anxiety or fear (Kolanowski 2011), and anxiety (Wenborn 2013). From Van Haitsma 2015, we calculated negative affect from sadness, anger, and anxiety (see Data synthesis).
For mood, we combined data on mood from one study (Kolanowski 2011), corrected for the differing direction of the scale (see Data synthesis); and data on depression from two studies (Orsulic‐Jeras 2000; Wenborn 2013). We used the SMD, calculated from mean values assessed during or directly after the intervention period or session. For two studies, we recalculated the number of participants to incorporate the cluster effect, using an estimate of the ICC (Cohen‐Mansfield 2007; Cohen‐Mansfield 2012 ‒ see Unit of analysis issues). We used a random‐effects model since there was clinical diversity and substantial heterogeneity (I² = 84% for positive affect). Higher scores indicate more positive and negative affect, and better mood.
Positive affect
For positive affect, we found very low‐certainty evidence (downgraded one level for risk of bias, inconsistency and imprecision) and we are uncertain whether personally tailored activities increase positive affect in comparison with active control groups or usual care (SMD 0.88, 95% CI 0.43 to 1.32; I² = 80%; 6 studies, 498 participants; Analysis 1.4; Figure 6). The evidence is also very uncertain about the effect of personally tailored activities on positive affect in comparison with active control groups (SMD 0.36, 95% CI 0.09 to 0.63; I² = 0%; 3 studies; 216 participants; Figure 6) or in comparison with usual care (SMD 1.30, 95% CI 0.77 to 1.84; I² = 69%; 4 studies; 282 participants; Figure 6; one study contributed to both subgroup analyses; test for subgroup differences P = 0.002; I² = 89.5%).
1.4. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 4: Positive affect
6.

Forest plot (1.4 Positive affect)
A sensitivity analysis excluding the study for which we derived a combined outcome measure showed an effect similar to the main analysis (SMD 0.76, 95% CI 0.38 to 1.13; I² = 58%; 5 studies; 318 participants; Analysis 1.5).
1.5. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 5: Positive affect ‐ sensitivity analysis excluding recalculated study results
Negative affect
We found moderate‐certainty evidence (downgraded one level for risk of bias) that personally tailored activities probably result in little to no difference in negative affect (SMD ‐0.02, 95% CI −0.19 to 0.14; I² = 0%; 6 studies; 632 participants; Analysis 1.6; Figure 7). The subgroup analyses for the different types of control groups showed similar results (personally tailored activities vs usual care: SMD 0.01, 95% CI −0.19 to 0.22; I² = 0%; 4 studies; 416 participants; personally tailored activities vs active control group: SMD −0.09, 95% CI −0.36 to 0.18; I² = 0%; 3 studies; 216 participants; Figure 7). The sensitivity analysis excluding the study for which we calculated the combined outcome measure also showed similar results (SMD −0.03, 95% CI −0.22 to 0.16; I² = 0%; 5 studies; 452 participants; Analysis 1.7).
1.6. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 6: Negative affect
7.

Forest plot (1.6 Negative affect)
1.7. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 7: Negative affect ‐ sensitivity analysis excluding recalculated study results
Mood
We found very low‐certainty evidence (downgraded one level for risk of bias and two levels for imprecision), and we are very uncertain whether personally tailored activities improve mood (SMD 0.03, 95% CI −0.21 to 0.27; I² = 0%; 4 studies; 265 participants; Analysis 1.8; Figure 8). The results of the subgroups comparing personally tailored activities with usual care and an active control group were comparable (Figure 8).
1.8. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 8: Mood
8.

Forest plot (1.8 Mood)
We performed a sensitivity analysis excluding the study that recruited people with dementia and depression, since the other included studies did not screen the participants for depression. The results were very similar in this sensitivity analysis (SMD 0.02, 95% CI −0.23 to 0.27; I² = 0%; 3 studies; 247 participants; Analysis 1.9).
1.9. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 9: Mood ‐ sensitivity analysis excluding studies with people with depression
Level of engagement
One of the newly included studies assessed engagement (Mbakile‐Mahlanza 2020), but the results of this cross‐over trial were not included in the analysis since a carry‐over effect occurred and no data of the first period of this trial were available. Three studies were included in the analysis, but the studies assessed different types of engagement. The results were not pooled due to the diversity of the outcome measures. We calculated mean differences for the results of two studies (Kolanowski 2011; van der Ploeg 2013), but not for the study by Orsulic‐Jeras 2000, due to pronounced baseline imbalances. Higher scores indicate more engagement. We judged engagement as an indirect (surrogate) outcome, because it is expected that the level of engagement in personally tailored activities might be associated with psychosocial outcomes, but the connection between the level of engagement and psychosocial outcomes is unclear.
Kolanowski 2011 assessed the intensity of participation. We found low‐certainty evidence (downgraded one level each for indirectness and imprecision) that personally tailored activities may make little or no difference to the intensity of participation (MD 0.30, 95% CI 0.16 to 0.44; 63 participants; Analysis 1.10).
1.10. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 10: Intensity of participation
Two studies assessed constructive engagement: one study found an increase of constructive engagement in the intervention group in comparison with an active control group (MD 6.90, 95% CI 3.07 to 10.73; 88 participants; van der Ploeg 2013; Analysis 1.11); and Orsulic‐Jeras 2000 found a decrease of constructive engagement in both groups (intervention group from 172 ± 171 at baseline to 96 ± 64 after six months; control group from 94 ± 79 at baseline to 49 ± 54 after six months; 25 participants). We found very low‐certainty evidence (downgraded one level for risk of bias, indirectness and imprecision) and we are very uncertain whether personally tailored activities improve constructive engagement.
1.11. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 11: Constructive engagement
Two studies assessed passive engagement. van der Ploeg 2013 found a small reduction of passive engagement in comparison with an active control group (MD −1.60, 95% CI −4.99 to 1.79; 88 participants; Analysis 1.12) and Orsulic‐Jeras 2000 found a decrease of passive engagement in the intervention group and nearly no change in the control group offering usual care (intervention group baseline 207 ± 132, after six months 91 ± 66; control group baseline 354 ± 158, after six months 345 ± 188; 25 participants). We found very low‐certainty evidence (downgraded for risk of bias, indirectness and imprecision) and we are very uncertain about the effect of personally tailored activities on passive engagement.
1.12. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 12: Passive engagement
For negative engagement, we found very low‐certainty evidence (downgraded one level for risk of bias, indirectness and imprecision) from one study, and we are very uncertain whether personally tailored activities improve negative engagement in comparison with an active control group (MD −5.50, 95% CI −9.58 to −1.42; 88 participants; van der Ploeg 2013; Analysis 1.13).
1.13. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 13: Negative engagement
Two studies investigated engagement after the sessions ended and all types of engagement returned to the baseline level (Kolanowski 2011; van der Ploeg 2013).
Sleep disturbances
For the sleep‐related outcomes, we found very low‐certainty evidence (downgraded one level for risk of bias, indirectness and imprecision) from one study (Richards 2005).
We are very uncertain whether personally tailored activities improve the amount of daytime sleep (minutes slept: MD −39.16, 95% CI −62.06 to −16.26; 139 participants; Analysis 1.14) or the amount of nighttime sleep (minutes slept: MD 28.81, 95% CI −22.65 to 80.27; 139 participants; Analysis 1.15); there were baseline imbalances between the study groups for nighttime sleep ‐ minutes slept at baseline: intervention group 368.95 ± 158.13; control group 331.37 ± 135.20). We are also uncertain whether personally tailored activities improve the time awake during the night (no MD calculated due to pronounced baseline imbalances, minutes awake: intervention group baseline 266.19 ± 142.02, follow‐up 252.14 ± 138.57; control group baseline 310.44 ± 129.63, follow‐up 304.20 ± 151.31).
1.14. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 14: Daytime minutes slept
1.15. Analysis.

Comparison 1: Personally tailored activities vs usual care or active control, Outcome 15: Nighttime minutes slept
Psychotropic medication
No study offered information on the use of psychotropic medication.
Effects on caregivers
One of the newly included studies assessed caregiver outcomes (Mbakile‐Mahlanza 2020), but the results of this cross‐over trial were not included in the analysis since a carry‐over effect occurred and no data of the first period of this trial were available.
Costs
Only the study by Richards 2005 assessed costs related to staff training, delivery of activities and administration of the intervention. Training costs comprised USD 1200 for teaching the project nursing assistants to conduct the intervention and training the registered nurses in the use of the outcome assessment. Costs for delivery of the activities were about USD 765 and included costs of commercial activities and perishable supplies. The mean cost per activity was estimated at USD 5. Administration costs were about USD 28 (one hour to complete the assessment).
Duration of the effects
Two studies investigated the duration of the intervention effect. In both studies, the values of most outcomes (agitation, positive and negative affect, engagement, and mood) returned to the baseline level. In the study by Kolanowski 2011, this was one week after the intervention period was completed, and in the study by van der Ploeg 2013, this was 30 minutes after the intervention sessions).
No information on the duration of intervention effects was available from the other studies.
Process evaluation
Five studies reported information about implementation fidelity and barriers or facilitators of the implementation process (Cohen‐Mansfield 2012; Kolanowski 2011; Travers 2017; Van Haitsma 2015; Wenborn 2013).
Cohen‐Mansfield 2012 reported that in about 20% of the sessions some participants did not take part in the activities offered, and 84% of the participants did not attend at least one of the sessions. The participants were unwilling or unresponsive (e.g. due to the severity of dementia) or unavailable (e.g. asleep or eating). The participants were more engaged in activities related to food/drink and one‐to‐one socialising activities and less engaged with puzzles, board games, art and craft activities (Cohen‐Mansfield 2012). Kolanowski 2011 calculated the dose of the intervention received by the participants as the product of time on task and intensity of participation per day. The total dose of intervention per participant ranged widely, but the mean dose did not differ significantly between groups. In the study by Van Haitsma 2015, each participant received on average seven intervention sessions (range five to nine). Wenborn 2013 reported information on staff attendance at the training sessions: the participating nurses (n = 52) attended an average of 73% of the education sessions (range 63 to 86) and 81% of the individual coaching sessions (range 49 to 100). No information was reported regarding the amount of activities offered to the residents in the intervention group. In Travers 2017, all participants attended the activity sessions and most participants attended the walking and talking sessions (active control group). As planned, the therapist delivering the intervention had weekly meetings with the project coordinator and the co‐therapists. The time required to plan the activities with the co‐therapists was longer than expected at the beginning of the study (about 20 minutes instead of 10 minutes), but the time decreased during the study period as planning the activities became routine. Members of the nursing staff attended only a small number of the anticipated sessions in weeks one, four and eight (16.7% attendance rate). However, the feasibility of the intervention was judged to be good by most of the co‐therapists and volunteers involved in the delivery of the activities, and they also described positive benefits for the participants based on their personal experience. Barriers to implementation were time restrictions, and some nurses judged the activities planning form to be too complex (Travers 2017).
Discussion
Summary of main results
We included 11 studies in this review update, which evaluated interventions offering personally tailored activity for people with dementia living in long‐term care. In most studies trained staff offered the activities directly to the people with dementia; in two studies nursing staff and family members, respectively, were trained to deliver the activities. The interventions varied in terms of the theoretical basis, the methods used to assess personal interests of the participants, the frequency and duration of the activity sessions and the length of follow‐up; however, the activities delivered seem to be comparable across studies.
Although we included three new studies, our results were similar to those in the first version of this review. Offering personally tailored activities to people with dementia in long‐term care may slightly reduce agitation. There was little information about the duration of effect, but data from two studies indicate that effects might only be detectable in the short or very short term, while the interventions are being delivered. In contrast to the first version of this review, the subgroups offering non‐personalised activities and usual care showed similar negligible effects of personally tailored activities in this review update. One of the newly included studies, which contributed to this analysis, showed a positive effect of personally tailored activities in comparison with an active intervention. Our hypothesis that studies with a usual care control group may find larger intervention effects than studies using an active control group, i.e. non‐personalised activities, was not supported in this analysis. We were unable to explain heterogeneity on the basis of the characteristics of the study populations or interventions.
Two studies investigated quality of life rated by proxy. Low‐certainty evidence from a meta‐analysis of these two studies indicated that personally tailored activities may make little to no difference to proxy‐rated quality of life in comparison with usual care or an active control group. However, these two studies had important differences (e.g. participant characteristics, nature of comparator intervention), and there was statistical heterogeneity in the meta‐analysis; the very small number of studies and the differences between them make this result difficult to interpret. For self‐rated quality of life, low‐certainty evidence indicated little to no difference between personally tailored activities and usual care, but data were only available for a small number of participants from one study. The instrument used to assess quality of life, the QoL‐AD, covers a broad range of aspects, including physical and mental health, living situation, relationship with families and friends, and finances. Although personally tailored activities are expected to have positive effects on some of these aspects, e.g. mood or doing things that the person enjoys, the influence on other aspects seems to be limited, for example financial aspects and living situation. In addition, there is evidence that proxies rated quality of life lower that people with dementia themselves (Burks 2021). Therefore, the results for quality of life should be interpreted with caution.
Only two studies assessed adverse effects, but no adverse effects were observed in these studies.
Personally tailored activities may have little or no effect on negative affect. Due to the very low certainty of the evidence, we are uncertain whether personally tailored activities improve positive affect, mood, engagement or sleep‐related outcomes. We found a relatively large effect size for positive affect, but in studies including an active control group there was only a small effect. Due to these differences and the very low‐certainty evidence, we have very little confidence in this result. Only one study assessed intervention costs, and none of the studies performed an economic evaluation. Two studies investigated the duration of the intervention effects and in both studies effects were only observed during the time the activities were delivered; the majority of outcomes returned to the baseline level after the delivery of the activities ended.
We were not able to investigate conditions which enhance the effectiveness of personally tailored activities in long‐term care, since no information about the context, such as environmental or staff‐related information, was reported. There was no evidence that interventions were more likely to be effective if based on one theoretical model rather than another.
Overall completeness and applicability of evidence
Although all interventions based the selection of activities on the personal interests of the participants, little information was reported about the process of tailoring the activities. Almost all of the participants in the included studies had severe dementia, indicating a substantial decline of memory and severe limitations in activities of daily living. This might have had an influence on the selection of suitable activities, and it seems probable that the activities were also tailored to the cognitive and physical abilities of the participants rather than to their interests only. Only one study described that the participants were more engaged in activities related to one‐to‐one socialising activities or interaction and less engaged with puzzles, board games, art and craft activities (Cohen‐Mansfield 2012). All studies included in this review hypothesised that personally tailored activities are more likely to be meaningful than activities which are not personally tailored, but this aspect was not investigated in the studies. We have insufficient information to explore whether the selection of the activities had an impact on the effects of the interventions and whether the activities offered were judged as meaningful by the participants. The results of this review may not be applicable to residents of long‐term care facilities whose dementia is less severe.
Another aspect that was not addressed in the included studies was the environment and context in which activities were offered. Two of the theoretical frameworks of the interventions comprise environmental aspects: the principles of Montessori (Mbakile‐Mahlanza 2020; Orsulic‐Jeras 2000; van der Ploeg 2013), and the occupational therapy intervention (Wenborn 2013); but no information about environmental aspects or how they were addressed during the delivery of the intervention was reported in the respective studies.
We included three new studies in this review update, but the number of studies contributing to the different outcomes of interest was still small (ranging from two to seven studies). Since almost all of the participants in the included studies had severe dementia, the results of this review may not be applicable to residents of long‐term care facilities whose dementia is less severe. Only two studies investigated quality of life rated by proxy and one of these studies included people with dementia and depression, while the other study did not include an assessment of depressive symptoms. Also, the validity of proxy‐rated quality of life in people with dementia is questioned (Burks 2021). We found clinical heterogeneity of the interventions (e.g. the different theoretical basis, duration and frequency of the activity sessions) and some methodological limitations of the included studies. Therefore, the results of this review must be interpreted with caution.
Quality of the evidence
As in the first version of this review, the certainty of evidence was predominately very low or low due to several methodological limitations of and inconsistencies between the included studies, and imprecision of the results. Two of the three newly included trials were pilot studies with a small number of participants, and the third study could not be included in the analysis since the required data were not available.
Seven out of the 11 included studies had a high risk of bias in at least one domain. Only two studies had a low risk of selection bias and four studies had a low risk of detection bias. We also found moderate to substantial heterogeneity in the meta‐analyses on agitation and affect. For agitation, heterogeneity was reduced by excluding one study (Cohen‐Mansfield 2012); however, we could not explain this heterogeneity from characteristics of this study. For positive affect we also could not identify the source of heterogeneity.
Generally, investigating the effects of personally tailored activities for people with dementia presents several methodological challenges. One challenge is the theoretical basis for preselecting the activities that could be offered to the participants and the process of choosing the activities for an individual person with dementia. Two models that were used as theoretical basis of the interventions, the Need‐Driven Dementia‐Compromised Behavior (NDB) model (Algase 1996) and Treatment Routes for Exploring Agitation (TREA) framework (Cohen‐Mansfield 2000), assume that agitation is a symptom of unmet needs in people with dementia. Both models postulate that by targeting the identified unmet needs, the specific agitated behaviour could be modified. The principles of Montessori place emphasis on offering activities which best fit the level of competence of people with dementia. The principles focus on task breakdown, guided repetition and progression in difficulty from simple to complex (van der Ploeg 2013). The Individualized Positive Psychosocial Intervention, employed by Van Haitsma 2015, did not focus on specific needs of people with dementia but more general assumptions about a person's needs for autonomy and competence and the importance of positive emotions to improve a person's well‐being. The pragmatic approach used by Travers 2017, which was not developed based on a specific theoretical model, also aimed to systematically increase positive events and activities to improve psychosocial outcomes of people with dementia. This study adapted an intervention developed for people with depression to people with dementia with depressive symptoms. Irrespective of the different theoretical models, the activities offered were very similar. Based on the results of this review, there is no evidence that interventions were more likely to be effective if based on one theoretical model rather than another.
The methods for assessing the participants' interests in order to tailor the activities also differed between studies. No information was available in any study about the number of participants who were able to express their individual interests or preferences. It might be challenging to assess the past or present interests in people with severe dementia. The assessment about interests can also be performed with family members and caregivers, but they might have differing perceptions about the interests and preferences of the participants, and whether activities are perceived as meaningful, than the people with dementia themselves. People with dementia judge activities as personally meaningful if the activities are connected with self (which represents the personal interests and the individual motivation to take part in a specific activity), with others, and with the environment (Han 2016). In addition, people also adapt their interests and preferences to changes of functional and cognitive abilities (Han 2016). Since the included studies did not investigate whether the relatives or primary caregivers were able to give valid information on the participants' interests and preferences, or whether the former interests and preferences changed over time or with progression of cognitive impairment, it remains unclear whether the activities offered were judged as meaningful by the study participants. The active control activities might also be seen as meaningful from the perspective of the study participants, especially the one‐to‐one interactions offered as active control in two studies (van der Ploeg 2013; Van Haitsma 2015), which are likely to meet the need for connectedness of people with dementia (Han 2016).
Another challenge is the characteristics of 'usual care'. There is evidence that people living in nursing homes have only few contacts with others, and that activities offered to them are often not perceived as meaningful (Edvardsson 2014; Harmer 2008; Hill 2010). The usual care offered to the control groups was not well described in several studies and the amount of activity available to the control group may have varied substantially between studies.
It was difficult to distinguish clearly between some of the outcomes addressed in this review, i.e. agitation, engagement and affect. Van Haitsma 2015 categorised several types of behaviour differently from other studies, e.g. "staring with a fixed gaze" was categorised as non‐verbal behaviour in this study while a "blank stare" was categorised as engagement in the studies by Orsulic‐Jeras 2000 and van der Ploeg 2013. We did not include all behaviours assessed by Van Haitsma 2015, but selected behaviours which were most comparable with the concept of agitation assessed in the other studies. The different instruments used to assess agitation or challenging behaviour also warrant consideration. One group of instruments rated the outcome based on direct observation of the participants and another group used proxy rating by the nursing staff. There is some evidence that proxy‐rating instruments assessing quality of life are less valid than instruments based on direct observation, since there might be a stronger influence of personal factors of the proxy‐raters, e.g. personal attitudes (Arons 2013; Gomez‐Gallego 2015; Moyle 2012). For instruments assessing agitation or challenging behaviour, some studies found that the reliability of instruments was moderate to good (Cohen‐Mansfield 2004; van der Linde 2014). In one study (van der Ploeg 2013), a single behaviour was investigated for each participant compared to the wide range of behaviours assessed by the rating scales used in other studies. Irrespective of these differences and uncertainties, the results of the different studies were homogenous, with the exception of one study (Cohen‐Mansfield 2012). Therefore, pooling the results of the different instruments seemed to be feasible, with the caveats mentioned above.
Potential biases in the review process
We followed the method described in the review protocol (Möhler 2012). To reduce the risk of bias in the review process, we followed the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017; Higgins 2021). We conducted a comprehensive search in several sources (databases, trial registers), guided by the Cochrane Dementia and Cognitive Improvement Group's Information Specialist. We also performed backward and forward citation tracking for all included studies. However, due to the small number of studies, we were not able to investigate the risk for publication bias using formal statistical methods. Two reviewers independently conducted study selection, quality appraisal, and data extraction. We also contacted all study authors for missing information.
Agreements and disagreements with other studies or reviews
Two systematic reviews investigating the effects of activities offered to people with dementia in nursing homes have been published, but both reviews included a wide range of non‐pharmacological interventions on psychosocial outcomes (Testad 2014; Travers 2016). Testad 2014 included, among others, interventions offering "pleasant activities with or without social interaction", but the inclusion criteria for both the interventions and the setting differed slightly from this review (e.g. cross‐over trials were excluded and different types of long‐term care settings were included). The review by Travers 2016 investigated, among others, the effects of individualised recreational activities. Both reviews described an improvement of agitation and, in contrast to our analysis, positive effects on pleasure and interest. However, due to the broader scope of both reviews, further studies were included that did not fit with our inclusion criteria. Testad 2014 did not perform meta‐analyses and the narrative synthesis showed small intervention effects. Travers 2016 performed some meta‐analyses including only two studies, and found no or small effects with wide CIs. Neither review rated the certainty of evidence using the GRADE approach (Guyatt 2011); and, therefore, no information about the certainty of the evidence was reported.
Authors' conclusions
Implications for practice.
Offering personally tailored activities to people with dementia in long‐term care may be considered as an intervention to reduce agitation, but the effect might be small and persist only as long as the activities are delivered. However, there is evidence that people with dementia living in nursing homes are often not engaged in activities and, from an ethical perspective, offering activities to people with dementia is necessary. Such activities should be selected based on the functional and cognitive abilities of nursing homes residents, but we can draw no conclusions from the existing body of trial evidence about other specific methods for selecting activities, the types of activity, or the duration and frequency of activities.
Implications for research.
The results indicate that further studies should be conducted to explore the potential benefits of personally tailored activities for improving positive affect and reducing agitation in people with dementia living in long‐term care facilities. But there is some evidence that the effects persists only as long as the activities are delivered.
The theoretical basis on which the activities are chosen seems less important, and the studies did not assess whether the participants judged the offered activities to be meaningful. The concept of 'meaningfulness' — how it could be assessed and how activities could be selected based on the results of such an assessment — needs to be investigated in more detail. Research on this topic seems to be feasible with people in earlier stages of dementia but more challenging in later stages of dementia. Assessing the interests and preferences of people with dementia and tailoring the activities to these interests, preferences and competencies (i.e. stage of dementia and the care dependency of the participants) also needs further investigation. In the context of active components, the effect of direct interaction alone (without offering specific activities) compared to direct interaction while offering specific (meaningful) activities has to be addressed. The role of direct interaction might also differ within the course of dementia, e.g. the activities might be more important in early stages of dementia. Another aspect to be explored is the role of the environment and the context in which activities are offered.
We included several pilot studies or studies with small sample sizes, but sufficiently powered trials are missing. Evaluation studies should be planned that adhere to current methodological standards, especially using a randomised and concealed allocation to the study groups. Adequate blinding is also important, since psychosocial outcomes are generally subjective and often rated by proxies. Therefore, outcome assessment has to be blinded, for example by the use of external blinded research staff. Blinding of nursing staff and participants is possible if clusters are allocated to the study groups or, in case of individual randomisation, if an active control intervention is delivered by research staff without informing the nurses about the group allocation. Therefore, in future studies we recommend comparing personally tailored activities with an active control group, offering direct interaction with participants or activities suitable for people with dementia; or with two control groups — an active control group and a 'usual care' control group. Studies including three groups are time‐ and personnel‐consuming; however, they can add valuable evidence to improve both research and clinical practice. Such studies should also include a process evaluation, which investigates implementation fidelity, barriers to and facilitators of the implementation, and contextual issues. Contextual issues include the willingness of people with dementia to be engaged in the activities, information about the meaningfulness of the activities offered, and details of the activities offered in the active control groups (Grant 2013; Moore 2015; Skivington 2021).
To ensure comprehensive reporting covering the complete research process (development, piloting and evaluation), the corresponding reporting statements should be used, e.g. Criteria for Reporting the Development and Evaluation of Complex Interventions in healthcare: revised guideline (CReDECI 2) for complex interventions (Möhler 2015), the Template for Intervention Description and Replication (TiDieR) criteria for the description of the interventions (Hoffmann 2014), and CONSORT or the corresponding extension, e.g. for randomised pilot and feasibility trials (Eldridge 2016), or cluster‐RCTs (Campbell 2012).
What's new
| Date | Event | Description |
|---|---|---|
| 13 March 2023 | New search has been performed | This review has been extensively updated. New studies included. Conclusions changed. Additional author. |
| 13 March 2023 | New citation required and conclusions have changed | Three new studies were included in this review update. In total, there are 11 studies with 1071 participants. Following the Cochrane Handbook, adverse events are defined as a primary outcome in the review update, rather than secondary outcome as in the first version of this review. |
History
Protocol first published: Issue 4, 2012 Review first published: Issue 2, 2018
Acknowledgements
We thank the Cochrane Dementia and Cognitive Improvement Group, especially Sue Marcus, Jenny McCleery, Anna Noel‐Storr, and Candida Fenton.
We also acknowledge the statistical support of Gerta Rücker (Institute for Medical Biometry and Statistics, Medical Center ‒ University of Freiburg, Faculty of Medicine, University of Freiburg, Germany) to the first version of this review.
We would like to thank peer reviewers Nick Smith and Hanne Kristensen, and consumer reviewer Shibley Rahman, for their comments and feedback.
Appendices
Appendix 1. Sources searched and search strategies
| Source | Search strategy | Hits retrieved |
| 1. CDCIG Register (https://crsweb.cochrane.org/login.html) [most recent search date: 15 June 2022 ] |
#1 "personally tailored" OR individualized OR individualised OR individual OR person‐centred OR meaningful OR personhood #2 involvement OR engagement OR engaging OR identity #3 #1 OR #2 |
May 2012: 149 April 2013: 0 March 2014: 6 January 2015: 1 January 2016: 2 October 2016: 2 June 2017: 3 June 2020: 41 Oct 2021: 43 June 2022: 35 |
| 2. MEDLINE In‐process and other non‐indexed citations and MEDLINE 1946 to present (Ovid SP) [most recent search date: 15 June 2022 ] |
1. exp Dementia/ 2. Delirium/ 3. Wernicke Encephalopathy/ 4. Delirium, Dementia, Amnestic, Cognitive Disorders/ 5. dement*.mp. 6. alzheimer*.mp. 7. (lewy* adj2 bod*).mp. 8. deliri*.mp. 9. (chronic adj2 cerebrovascular).mp. 10. ("organic brain disease" or "organic brain syndrome").mp. 11. ("normal pressure hydrocephalus" and "shunt*").mp. 12. "benign senescent forgetfulness".mp. 13. (cerebr* adj2 deteriorat*).mp. 14. (cerebral* adj2 insufficient*).mp. 15. (pick* adj2 disease).mp. 16. (creutzfeldt or jcd or cjd).mp. 17. huntington*.mp. 18. binswanger*.mp. 19. korsako*.mp. 20. or/1‐19 21. activity.ti,ab. 22. activities.ti,ab. 23. psychosocial.ti,ab. 24. non‐pharmacological.ti,ab. 25. individually‐tailor*.ti,ab. 26. personally‐tailor*.ti,ab. 27. (individual or individuals or individually‐cent*).ti,ab. 28. meaning*.ti,ab. 29. involvement.ti,ab. 30. (engagement or engaging).ti,ab. 31. occupational*.ti,ab. 32. personhood.ti,ab. 33. person‐centred.ti,ab. 34. identity.ti,ab. 35. or/21‐34 36. 20 and 35 37. long‐term care.ti,ab. 38. "care home*".ti,ab. 39. "residential care".ti,ab. 40. "nursing home*".ti,ab. 41. "residential facilit*".ti,ab. 42. Residential Facilities/ 43. Nursing Homes/ 44. "old people* home*".ti,ab. 45. or/37‐44 46. 36 and 45 |
May 2012: 1656 April 2013: 205 March 2014: 177 January 2015: 182 January 2016: 185 October 2016: 367 June 2017: 358 June 2020: 913 Oct 2021: 643 June 2022: 590 |
| 3. Embase 1974 to present (Ovid SP) [most recent search date: 15 June 2022] |
1. exp dementia/ 2. Lewy body/ 3. delirium/ 4. Wernicke encephalopathy/ 5. cognitive defect/ 6. dement*.mp. 7. alzheimer*.mp. 8. (lewy* adj2 bod*).mp. 9. deliri*.mp. 10. (chronic adj2 cerebrovascular).mp. 11. ("organic brain disease" or "organic brain syndrome").mp. 12. "supranuclear palsy".mp. 13. ("normal pressure hydrocephalus" and "shunt*").mp. 14. "benign senescent forgetfulness".mp. 15. (cerebr* adj2 deteriorat*).mp. 16. (cerebral* adj2 insufficient*).mp. 17. (pick* adj2 disease).mp. 18. (creutzfeldt or jcd or cjd).mp. 19. huntington*.mp. 20. binswanger*.mp. 21. korsako*.mp. 22. CADASIL.mp. 23. or/1‐22 24. activity.ti,ab. 25. activities.ti,ab. 26. psychosocial.ti,ab. 27. non‐pharmacological.ti,ab. 28. individually‐tailor*.ti,ab. 29. personally‐tailor*.ti,ab. 30. (individual or individuals or individually‐cent*).ti,ab. 31. meaning*.ti,ab. 32. involvement.ti,ab. 33. (engagement or engaging).ti,ab. 34. occupational*.ti,ab. 35. personhood.ti,ab. 36. person‐centred.ti,ab. 37. identity.ti,ab. 38. or/24‐37 39. 23 and 38 40. long‐term care.ti,ab. 41. "care home*".ti,ab. 42. "residential care".ti,ab. 43. "nursing home*".ti,ab. 44. "residential facilit*".ti,ab. 45. residential home/ 46. nursing home/ 47. "old people* home*".ti,ab. 48. or/40‐47 49. 39 and 48 50. 39 and 48 |
May 2012:2400 April 2013: 382 March 2014: 452 January 2015: 492 January 2016: 463 October 2016: 777 June 2017: 691 June 2020: 1827 Oct 2021: 1116 June 2022: 1026 |
| 4. PsycINFO 1806 to May present (Ovid SP); [most recent search date: 15 June 2022] |
1. exp Dementia/ 2. exp Delirium/ 3. exp Huntingtons Disease/ 4. exp Kluver Bucy Syndrome/ 5. exp Wernickes Syndrome/ 6. exp Cognitive Impairment/ 7. dement*.mp. 8. alzheimer*.mp. 9. (lewy* adj2 bod*).mp. 10. deliri*.mp. 11. (chronic adj2 cerebrovascular).mp. 12. ("organic brain disease" or "organic brain syndrome").mp. 13. "supranuclear palsy".mp. 14. ("normal pressure hydrocephalus" and "shunt*").mp. 15. "benign senescent forgetfulness".mp. 16. (cerebr* adj2 deteriorat*).mp. 17. (cerebral* adj2 insufficient*).mp. 18. (pick* adj2 disease).mp. 19. (creutzfeldt or jcd or cjd).mp. 20. huntington*.mp. 21. binswanger*.mp. 22. korsako*.mp. 23. ("parkinson* disease dementia" or PDD or "parkinson* dementia").mp. 24. or/1‐23 25. activity.ti,ab. 26. activities.ti,ab. 27. psychosocial.ti,ab. 28. non‐pharmacological.ti,ab. 29. individually‐tailor*.ti,ab. 30. personally‐tailor*.ti,ab. 31. (individual or individuals or individually‐cent*).ti,ab. 32. meaning*.ti,ab. 33. involvement.ti,ab. 34. (engagement or engaging).ti,ab. 35. occupational*.ti,ab. 36. personhood.ti,ab. 37. person‐centred.ti,ab. 38. identity.ti,ab. 39. or/25‐38 40. 24 and 39 41. long‐term care.ti,ab. 42. "care home*".ti,ab. 43. "residential care".ti,ab. 44. "nursing home*".ti,ab. 45. "residential facilit*".ti,ab. 46. exp Nursing Homes/ or exp Residential Care Institutions/ 47. "old people* home*".ti,ab. 48. institutionali?ed.ti,ab. 49. or/41‐48 50. 40 and 49 |
May 2012: 1633 April 2012: 191 March 2014: 202 January 2015: 207 January 2016: 228 October 2016: 356 June 2017: 268 June 2020: 610 Oct 2021: 387 June 2022: 316 |
| 5. CINAHL (EBSCOhost) [most recent search date: 15 June 2022] |
S60 S46 AND S59 S59 S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 S58 MH "Random Assignment" S57 MH "Single‐Blind Studies" or MH "Double‐Blind Studies" or MH "Triple‐Blind Studies" S56 MH "Crossover Design" S55 MH "Factorial Design" S54 MH "Placebos" S53 MH "Clinical Trials" S52 TX "multi‐centre study" OR "multi‐center study" OR "multicentre study" OR "multicenter study" OR "multi‐site study" S51 TX crossover OR "cross‐over" S50 AB placebo* S49 TX random* S48 TX trial* S47 TX "latin square" S46 S19 and S34 and S45 S45 S35 or S36 or S37 or S38 or S39 or S40 or S41 or S42 or S43 or S44 S44 TX institutionalised OR institutionalized S43 TX institutional S42 TX "old people* home*" S41 MH "Nursing Homes" S40 MH "Residential Facilities" S39 TX "residential facilit*" S38 TX "nursing home*" S37 TX "residential care" S36 TX "care home*" S35 TX "long‐term care" S34 S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 S33 TX identity S32 TX person‐centred S31 TX personhood S30 TX occupational* S29 TX engagement or engaging S28 TX non‐pharmacological S27 TX psychosocial S26 AB activities S25 AB involvement S24 AB meaningful S23 AB individual OR individuals OR individually‐cent* S22 TX personally‐tailor* S21 TX individually‐tailor* S20 AB activity S19 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 S18 TX korsako* S17 TX binswanger* S16 TX huntington* S15 TX creutzfeldt or jcd or cjd S14 TX pick* N2 disease S13 TX cerebral* N2 insufficient* S12 TX cerebr* N2 deteriorat* S11 TX "benign senescent forgetfulness" S10 TX "normal pressure hydrocephalus" and "shunt*" S9 TX "organic brain disease" or "organic brain syndrome" S8 TX chronic N2 cerebrovascular S7 TX deliri* S6 TX lewy* N2 bod* S5 TX alzheimer* S4 TX dement* S3 MH "Wernicke's Encephalopathy" S2 (MH "Delirium") or (MH "Delirium, Dementia, Amnestic, Cognitive Disorders") S1 MH "Dementia+" |
May 2012: 2367 April 2013: 275 March 2014: 221 January 2015: 158 January 2016: 121 October 2016: 245 June 2017: 274 June 2020: 277 Oct 2021: 129 June 2022: 115 |
| 6. Web of Science and conference proceedings: Clarivate [most recent search date: 15 June 2022] |
TOPIC: (dementia OR alzheimer* OR lewy OR CJD OR JCD OR creutzfeldt OR binswanger OR korsako*) AND TOPIC: (activity OR activities OR psychosocial OR non‐pharmacological OR "individually tailor*" OR "personally tailor*" OR individual OR meaningful* OR occupational OR personhood OR "person cent*" OR identity) AND TOPIC: ("long term care" OR "longterm care" OR "residential care" OR "nursing home*" OR "residential facilit*" OR "old people* home*" OR institutionalised OR institutionalized) AND TOPIC: (randomly OR randomised OR randomized OR "random allocat*" OR RCT OR CCT OR "double blind*" OR "single blind*" OR "double blind*" OR "single blind*" OR trial) | May 2012: 2153 April 2013: 311 March 2014: 104 January 2015: 216 January 2016: 391 October 2016: 773 June 2017: 766 June 2020: 420 Oct 2021: 254 June 2022: 170 |
| 7. LILACS (BIREME) [most recent search date: 15 June 2022] |
dementia OR demencia OR demência OR alzheimer OR alzheimers OR alzheimer’s [Words] and "personally tailored" OR "pessoalmente adaptado" OR "personal a medida" OR individual OR individualised OR individualized OR individualmente OR individualmente OR activity OR activites OR atividades OR "las actividades" OR occupational [Words] | May 2012: 313 April 2013: 21 March 2014: 0 January 2015: 3 January 2016: 52 October 2016: 52 June 2017: 67 June 2020: 201 Oct 2021: 67 June 2022: 46 |
| 8. CENTRAL (CRSO) [most recent search date: 15 June 2022] |
#1 MeSH descriptor Dementia explode all trees #2 MeSH descriptor Delirium, this term only #3 MeSH descriptor Wernicke Encephalopathy, this term only #4 MeSH descriptor Delirium, Dementia, Amnestic, Cognitive Disorders, this term only #5 dement* #6 alzheimer* #7 "lewy* bod*" #8 deliri* #9 "chronic cerebrovascular" #10 "organic brain disease" or "organic brain syndrome" #11 "normal pressure hydrocephalus" and "shunt*" #12 "benign senescent forgetfulness" #13 "cerebr* deteriorat*" #14 "cerebral* insufficient*" #15 "pick* disease" #16 creutzfeldt or jcd or cjd #17 huntington* #18 binswanger* #19 korsako* #20 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19) #21 activity #22 activities #23 psychosocial #24 non‐pharmacological #25 individually‐tailor* #26 personally‐tailor* #27 individual OR individuals OR individually‐cent* #28 meaning* #29 involvement #30 engagement or engaging #31 occupational* #32 personhood #33 person‐centred #34 identity #35 (#22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34) #36 "long‐term care" OT "longterm care" OR "long term care" #37 "care home*" #38 "residential care" #39 "nursing home*" #40 "residential facilit*" #41 MeSH descriptor Residential Facilities explode all trees #42 MeSH descriptor Nursing Homes explode all trees #43 "old people* home*" #44 institutionalised OR institutionalized #45 (#36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44) #46 (#20 AND #35 AND #45) |
May 2012: 280 April 2013: 3 March 2014: 10 January 2015: 18 January 2016: 13 October 2016: 50 June 2017: 17 June 2020: 210 Oct 2021: 46 June 2022: 68 |
| 9. Clinicaltrials.gov (www.clinicaltrials.gov) [most recent search date: 15 June 2022] |
(personally tailored OR individual OR person‐centred OR meaningful OR personhood) | Interventional Studies | dementia OR VCI OR vascular dementia OR VaD OR vascular cognitive impairment OR cadasil OR multi‐infarct OR binswanger | Senior | May 2012: 271 April 2013: 47 March 2014: 88 January 2015: 14 January 2016: 13 October 2016: 58 June 2017: 94 June 2020: 46 Oct 2021: 35 June 2022: 13 |
| 10. ICTRP Search Portal (apps.who.int/trialsearch) [most recent search date: 28 October 2021. Database not available 15 June 2022] |
personally tailored OR individual OR person‐centred OR meaningful OR personhood) | Interventional Studies | dementia OR VCI OR vascular dementia OR VaD OR vascular cognitive impairment OR cadasil OR multi‐infarct OR binswanger | May 2012: 127 April 2013: 12 March 2014: 13 January 2015: 8 January 2016: 16 October 2016: 4 June 2017: 11 June 2020: unavailable Oct 2021: 3 June 2022: 0 |
| TOTAL before de‐duplication | May 2012: 11349 April 2012: 1455 March 2014: 1273 January 2015: 1296 January 2016: 1435 October 2016: 2682 June 2017: 2549 June 2020: 4545 Oct 2021: 2723 June 2022: 2379 |
|
| TOTAL after de‐duplication and first assessment by CDCIG Information Specialists | May 2012: 532 April 2013: 50 March 2014: 52 January 2015: 54 January 2016: 61 October 2016: 105 June 2017: 180 June 2020: 2975 Oct 2021: 1767 June 2022: 1590 |
|
Data and analyses
Comparison 1. Personally tailored activities vs usual care or active control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Agitation | 7 | 485 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.53, 0.01] |
| 1.1.1 Personally tailored activities vs usual care | 4 | 288 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.76, 0.09] |
| 1.1.2 Personally tailored activities vs active control | 3 | 197 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.58, 0.23] |
| 1.2 Behaviours (van Haitsma 2015) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2.1 General restlessness | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2.2 Aggression | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2.3 Uncooperative | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2.4 Very negative verbal | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2.5 Negative verbal | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3 Quality of life (proxy‐rated) | 2 | 177 | Mean Difference (IV, Random, 95% CI) | ‐0.83 [‐3.97, 2.30] |
| 1.4 Positive affect | 6 | 498 | Std. Mean Difference (IV, Random, 95% CI) | 0.88 [0.43, 1.32] |
| 1.4.1 Personally tailored activities vs usual care | 4 | 282 | Std. Mean Difference (IV, Random, 95% CI) | 1.30 [0.77, 1.84] |
| 1.4.2 Personally tailored activities vs active control | 3 | 216 | Std. Mean Difference (IV, Random, 95% CI) | 0.36 [0.09, 0.63] |
| 1.5 Positive affect ‐ sensitivity analysis excluding recalculated study results | 5 | 318 | Std. Mean Difference (IV, Random, 95% CI) | 0.76 [0.38, 1.13] |
| 1.6 Negative affect | 6 | 632 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.19, 0.14] |
| 1.6.1 Personally tailored activities vs usual care | 4 | 416 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.19, 0.22] |
| 1.6.2 Personally tailored activities vs active control | 3 | 216 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.36, 0.18] |
| 1.7 Negative affect ‐ sensitivity analysis excluding recalculated study results | 5 | 452 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.22, 0.16] |
| 1.8 Mood | 4 | 265 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.21, 0.27] |
| 1.8.1 Personally tailored activities vs active control | 2 | 81 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.40, 0.47] |
| 1.8.2 Personally tailored activities vs usual care | 2 | 184 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.26, 0.32] |
| 1.9 Mood ‐ sensitivity analysis excluding studies with people with depression | 3 | 247 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.23, 0.27] |
| 1.9.1 Personally tailored activities vs usual care | 2 | 184 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.26, 0.32] |
| 1.9.2 Personally tailored activities vs active control | 1 | 63 | Std. Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.49, 0.49] |
| 1.10 Intensity of participation | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.11 Constructive engagement | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.12 Passive engagement | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.13 Negative engagement | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.14 Daytime minutes slept | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.15 Nighttime minutes slept | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cohen‐Mansfield 2007.
| Study characteristics | ||
| Methods |
Study design: cluster‐randomised controlled trial (not registered) Duration of follow‐up: 10 consecutive days Study period: not reported |
|
| Participants |
Country: USA Setting: 12 clusters from 11 suburban nursing home facilities Participants/clusters
Baseline characteristics
|
|
| Interventions |
Intervention: activity programme based on the Treatment Routes for Exploring Agitation (TREA) framework Control: presentation for nursing staff describing the syndromes of agitation, their aetiologies, and possible non‐pharmacologic interventions |
|
| Outcomes |
Primary: agitation (ABMI) Secondary: affect (pleasure, interest, anger, anxiety, sadness) |
|
| Funding | National Institutes of Health; USA | |
| Notes | Cluster effect was not incorporated in the analysis (risk unit‐of‐analysis error) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "To limit contamination of the interventions’ effectiveness, buildings were assigned either control or intervention status (rather than having both within each building). We were unable at times to assign buildings randomly to either intervention or control groups because the administrators of two facilities insisted on making the decision as a condition of participation. Other facilities without such stipulations were randomly assigned to the treatment or control group while balancing the number of facilities in each group." No method of sequence generation was reported. |
| Allocation concealment (selection bias) | Unclear risk | No methods for allocation concealment was reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information about blinding of personnel and participants reported, but blinding seems not possible. The intervention was delivered at cluster level. We have insufficient information to permit judgement of ‘low risk’ or ‘high risk'. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Another measure of reliability examined the possible effect of the nonblindness of the observations. For this measure, 10 study participants were videotaped, and inter‐rater reliability was obtained from a research assistant who was blinded both to the background characteristics of the observed residents and to the raters themselves. The average agreement between observed agitation recorded from videotape and direct observations of agitated behaviors was 95%". We have insufficient information to permit judgement of ‘low risk’ or ‘high risk'. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Participants lost to follow‐up: intervention group: "1 excluded due to illness during intervention", control group: "2 excluded due to hospitalisation after baseline assessment". |
| Selective reporting (reporting bias) | Unclear risk | Not registered, no study protocol available. |
| Other bias | Low risk | ‐ |
Cohen‐Mansfield 2012.
| Study characteristics | ||
| Methods |
Study design: cluster‐randomised controlled trial (NCT00820859, retrospectively registered) Duration of follow‐up: 2 weeks Study period: June 2006 to December 2011 |
|
| Participants |
Country: USA Setting: 11 nursing homes in Rockville, Silver Spring, Takoma Park, Chevy Chase, and Gaithersburg, Maryland, USA. Participants/clusters
Baseline characteristics
|
|
| Interventions |
Intervention: activity programme based on the Treatment Routes for Exploring Agitation (TREA) framework Control: presentation for nursing staff describing the syndromes of agitation, their aetiologies, and possible non‐pharmacologic interventions |
|
| Outcomes |
Primary: agitation (ABMI) Secondary: affect (pleasure, interest, anger, anxiety, sadness) |
|
| Funding | National Institutes of Health (grant 2 R01 AG010l72‐10A2) | |
| Notes | Cluster effect was not incorporated in the analysis (risk unit‐of‐analysis error) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization to intervention or placebo control protocols was performed using random numbers via a ratio of 1.5: 1, with the intent of having more intervention than control participants in order to investigate process issues." |
| Allocation concealment (selection bias) | Unclear risk | No methods for allocation concealment were reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "(...) once treatment started, research assistants were no longer blinded to group assignment." "Study participants were blinded as to their group assignment"; comment: since the control group did not receive an active control intervention, blinding of participants seems not possible. The intervention was delivered at cluster level. We have insufficient information to permit judgement of ‘low risk’ or ‘high risk'. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Research assistants could not be blinded once interventions began." "Another measure of reliability examined the possible effect of the nonblindness of the observations. For this measure, 25 study participants were videotaped, and interrater reliability was obtained from a research assistant blinded both to the background characteristics of the observed residents and to the original ratings. The ICC between videotaped and direct observation in the current study was 0.94 for verbal agitation, 0.93 for physical agitation, and 0.94 for total agitated behaviors." We have insufficient information to permit judgement of ‘low risk’ or ‘high risk'. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Residents not included after cluster randomisation: "Placebo (n = 36), bipolar disorder or schizophrenia diagnosis (n = 3), not agitated (n = 25), age < 60 years (n = 3), death(n = 2), participated in previous TREA study (n = 2), gave consent but could not be included before the data collection phase ended (n = 1). Intervention (n = 62), bipolar disorder or schizophrenia diagnosis (n = 6), not agitated (n = 29), age < 60 years (n = 3), MMSE > 25 (n = 2), no diagnosis of dementia (n = 1), death (n = 13), discharged (n = 6), life expectancy < 3 months (n = 1), gave consent but could not be included before the data collection phase ended (n = 1)" "Did not receive placebo as allocated (n = 4, lost to death), did not receive intervention as allocated (n = 4, lost to death)" |
| Selective reporting (reporting bias) | Unclear risk | Study was registered retrospectively, no study protocol available. |
| Other bias | Low risk | ‐ |
Kolanowski 2011.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial (NCT00388544, retrospectively registered) Duration of follow‐up: 4 weeks (3‐week interventions period + 1‐week post‐intervention period) Study period: August 2005 to November 2008 |
|
| Participants |
Country: USA Setting: 9 community‐based nursing homes in Pennsylvania Participants/clusters
Baseline characteristics
|
|
| Interventions |
Interventions: activity programmes based on the Need‐Driven Dementia‐Compromised Behavior model
Control group: activities opposite to participants' style of interest and challenging for their functional level |
|
| Outcomes | No primary outcome defined.
|
|
| Funding | One author was supported by National Institutes of Health and another author received royalties from the NEO‐PI‐R and the NEOFFI and was supported in part by National Institutes of Health | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The statistician determined participants’ group assignment using a random number generator with random block sizes to ensure equal assignment across the four groups at the completion of the study and approximately equal assignments throughout the study to control for unknown temporal effects." |
| Allocation concealment (selection bias) | Low risk | "Group assignment was concealed until after all screening data were collected. The project director obtained the assignment from a secure central location after verifying that the participant qualified for the study." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Because all participants received some type of activity, it was possible to blind the interventionists, data collectors, video raters, nursing home staff, and participants." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Because all participants received some type of activity, it was possible to blind the interventionists, data collectors, video raters, nursing home staff, and participants." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | After randomisation, in both groups included in this review 1 participant was lost to follow‐up but no participants were excluded from the analysis. |
| Selective reporting (reporting bias) | Unclear risk | Study was registered retrospectively, no study protocol available. |
| Other bias | Low risk | ‐ |
Mbakile‐Mahlanza 2020.
| Study characteristics | ||
| Methods |
Study design: cluster‐randomised cross‐over trial (ACTRN12611000998943) Duration of follow‐up: 6 weeks Study period: not reported |
|
| Participants |
Country: Australia Setting: 9 general and psychogeriatric nursing homes, state of Victoria Participants/clusters
Baseline characteristics
|
|
| Interventions |
Intervention: Montessori‐based activities Control: reading a newspaper |
|
| Outcomes |
Primary:
Secondary:
|
|
| Funding | Alzheimer’s Australia as part of the National Quality Dementia Care Initiative (only reported in the study registration) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Participating nursing homes were randomized to either Montessori condition first (Group A) or control condition first (Group B) sequence, and the group allocation was randomly determined using Excel Random Number Generator." "At each nursing home, a staff member identified potential residents and sought agreement from the family member to be contacted by the research team. When verbal consent was given, a senior researcher contacted the family member to explain the study and answer queries. Those who expressed interest in the study were sent a Participant information and Consent Form package." "Out of the 16 nursing homes visited, a total of 9 facilities consented to participate in the study and a preselection screening was conducted to identify eligible participants." "Due to a small sample size, we were unable to adjust for the group imbalances". We found imbalances between groups for several criteria, e.g. time in the facility, dementia severity and physical agitation, but no information about the level of significance was provided. These differences might be based in the small sample size, and we have insufficient information to permit judgement of ‘low risk’ or ‘high risk'. |
| Allocation concealment (selection bias) | Unclear risk | No information reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "Participants and facility staff were blinded to the hypotheses of the study as well as the condition that the participants were in."
"No blinding was applied to the researchers." The intervention was delivered on cluster level. We have insufficient information to permit judgement of ‘low risk’ or ‘high risk'. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "Another limitation of this study was the absence of researcher blinding, which could potentially introduce bias into the study results during the scoring of resident observations. The nature of Montessori activities (with many materials and other prompts to elicit active participation) makes it virtually impossible to blind researchers to the type of condition that is being scored. Researchers were trained to record affect and engagement consistently across all sessions. Their inter‐rater reliability was excellent." Outcomes were assessed by unblinded researchers. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Drop‐out rate comparable between groups (approx. 20%), but no information about the period in which the participants were lost to follow‐up and no reasons for drop‐out were reported. |
| Selective reporting (reporting bias) | High risk | There are some important differences between the methods planned (described in the study register and study protocol) and the published study:
|
| Other bias | High risk | No wash‐out period included. "We detected carryover effects of the experimental condition on several outcomes for the resident as well as on carers’ mood." |
Orsulic‐Jeras 2000.
| Study characteristics | ||
| Methods |
Study design: controlled clinical trial (not registered) Duration of follow‐up: 9 months Study period: not reported |
|
| Participants |
Country: USA Setting: one dementia special care unit, Menorah Park Center for Senior Living (Orthodox Jewish facility with over 350 long‐term care beds) Participants
Baseline characteristics
|
|
| Interventions |
Intervention: Montessori‐based activities (group or individual activities) Control: usual care (regular activities) |
|
| Outcomes | No primary outcome defined.
|
|
| Funding | Not mentioned | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomised trial; "Thirteen residents were assigned to the treatment condition and 12 to the control condition. Participants were matched across groups according to their scores on the MMSE, along with their performances on the Myers Menorah Park/Montessori Assessment System (MMP/MAS) and the reading subtest of the Wide Range Achievement Test (WRAT3)." |
| Allocation concealment (selection bias) | High risk | Not applicable (not an RCT) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Individual activity sessions "were run by either a trained volunteer, a research assistant, or the activities therapist on the unit." The two types of group activities were run "one day by a volunteer and one day by the activities therapist on the unit" and "led by either a trained volunteer or by the activities therapist on the unit" respectively. The participants in the control group received care and activities as usual and it seems not possible to blind personnel or participants. Since the same nurses cared for participants in both study groups there is a risk of contamination. We judged risk of performance bias to be high. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "Research staff interviewed nursing assistants on the special care unit at pretest and at final posttest for approximately 20 minutes for all measures". Outcome assessors were not blinded to group allocation and assessed subjective outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Forty‐four residents from the dementia SCU were initially recruited. During the course of this 9‐month study, 19 participants dropped out of the study, either because of death (n = 3), transfer to another unit within the facility (n = 12), or excessive absence (n = 4). Thus, 25 participants (23 women and 2 men) completed the study." No information about the group allocation for the participants lost to follow‐up were reported. |
| Selective reporting (reporting bias) | Unclear risk | Not registered, no study protocol available. |
| Other bias | Low risk | ‐ |
Richards 2005.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial (not registered) Duration of follow‐up: 21 consecutive days Study period: not reported |
|
| Participants |
Country: USA Setting: one Department of Veterans Affairs nursing home and six for‐profit community nursing homes, central southeastern United States. Participants
Baseline characteristics
|
|
| Interventions |
Intervention: individualised activity‐programme Control: usual care (including any scheduled activities that the nursing home provided). |
|
| Outcomes | No primary outcome defined.
|
|
| Funding | Veterans Health Administration, National Institute of Nursing Research, National Institutes of Health/National Center for Research Resources to the General Clinical Research Center of the University of Arkansas for Medical Sciences; USA | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Then participants were randomly assigned to one of two groups: ISAI or usual‐care control". No further information reported. |
| Allocation concealment (selection bias) | Unclear risk | No information reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "The project nursing assistants implemented the ISAI and recorded the type, time, and duration of the activities. (...) As part of the ISAI, the project nursing assistants checked on the participants every hour, observed them for napping, wakened them if they were asleep, and provided ISAI. (...) Participants in this [control] group received usual care". Since the same nurses cared for participants in both study groups there is a risk of contamination. We judged risk of performance bias to be high. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The Actigraph (Ambulatory Monitoring, Ardsley, NY), a motion‐sensing device that uses an algorithm to differentiate sleep from wake based on motor activity, measured sleep/wake pattern variables." No information about blinding reported, but the risk of bias was judged to be low since only objective outcomes were assessed via Actigraph. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Of the 147 remaining participants, seven were hospitalized, and one returned home." Comment: no information about the allocated groups of the participants lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Not registered, no study protocol available. |
| Other bias | Low risk | ‐ |
Travers 2017.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial (ACTRN12613000296730) Duration of follow‐up: 8 weeks Study period: not reported |
|
| Participants |
Country: Australia Setting: four nursing homes, southern suburbs of Brisbane, Queensland, 48 to 126 beds. All catered for residents with high and low care needs and all were accredited with the National Accreditation Agency (Aged Care Standards and Accreditation Agency Ltd). The facilities were managed by religious (two), independent not‐for‐profit (one) and private (one) organisations and all facilities employed activities staff and provided a variety of organised activities for residents. Participants
Baseline characteristics
|
|
| Interventions |
Intervention: BE‐ACTIV Control: walking and talking intervention |
|
| Outcomes |
Primary (defined in the trial registration):
Secondary: agitation (CMAI ‐ short form) |
|
| Funding | Funded by the JO & JR Wicking trust | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The Project Coordinator assigned participants a unique study identification number and randomly allocated them to either the BE‐ACTIV or the Walking and Talking intervention using the SPSS randomization function." |
| Allocation concealment (selection bias) | High risk | "The Project Coordinator assigned participants a unique study identification number and randomly allocated them to either the BE‐ACTIV or the Walking and Talking intervention using the SPSS randomization function." Not concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "In the first instance, facility staff (activities staff in particular) and volunteers were invited to attend two 90‐min depression training sessions that were conducted at the commencement of the study in each facility (...) An overview of the project including its rationale and methods was also provided." The therapist and the nursing staff was aware of the group allocation; no information about the blinding of the participants was reported. Since the same nurses cared for participants in both study groups there is a risk of contamination. We judged risk of performance bias to be high. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "The measures of QOL (QOL‐AD‐NH), and depression (GDS‐12R) were re‐administered following completion of the interventions by the Project Coordinator only, who was not blinded regarding participant’s group allocation." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Ten participants were allocated to the BE‐ACTIV intervention and nine to the Walking and Talking intervention. One resident who had been allocated to the Walking and Talking intervention, however, died prior to commencement of the intervention and his data were excluded from all analyses. All remaining participants completed the eight‐week interventions." |
| Selective reporting (reporting bias) | Unclear risk | Only the primary outcomes defined in the trial register were reported. |
| Other bias | Low risk | ‐ |
van der Ploeg 2013.
| Study characteristics | ||
| Methods |
Study design: randomised cross‐over trial (ACTRN12609000564257, retrospectively registered) Duration of follow‐up: 4 weeks (2 weeks per condition, no washout period) Study period: July 2009 to September 2011 |
|
| Participants |
Country: Australia Setting: Nine residential facilities in metropolitan Melbourne, Australia Participants
Baseline characteristics
|
|
| Interventions |
Intervention: personalised Montessori‐based activities Control: non‐personalised activities (active control) |
|
| Outcomes |
Primary: one physically agitated behaviour specific for each participant (based on the CMAI) Secondary
|
|
| Funding | Dementia Collaborative Research Centre (DCRC), Mason Foundation, National Health and Medical Research Council; Australia | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The primary investigator generated the random allocation sequence using Excel Random Number Generator." |
| Allocation concealment (selection bias) | High risk | Group allocation was not concealed (unpublished information from the study author). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "Participants and facility staff were blinded to the hypotheses of the study." "Treatment facilitators reported in supervision meetings that they were sometimes tempted to resort to the Montessori approach when the control activities failed to capture participants’ interest." Staff delivering the intervention were not blinded to group allocation and delivered both the intervention and the active control activities (cross‐over trial). |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "Because of the nature of the activities, it was not possible to blind observers to the Montessori or the control conditions but they were trained to record behavior, affect, and engagement styles consistently across sessions and their inter‐rater reliability was excellent." Outcome assessors were unblinded to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Allocated to Montessori intervention first lost to follow‐up (n = 6): deceased (n = 3), refused intervention (n = 3); Allocated to Montessori intervention second lost to follow‐up (n = 7): deceased (n = 1), refused intervention (n = 1), moved to other facility (n = 1), too busy to schedule sessions (n = 4)." Since the attrition rate was more than twice as high as planned, risk of bias was rated as unclear. |
| Selective reporting (reporting bias) | Unclear risk | Study was retrospectively registered, the study protocol was published after first participants were recruited. |
| Other bias | High risk | No paired data were available (risk of a unit‐of‐analysis bias) and we used the (unpaired) data of the complete study period. |
Van Haitsma 2015.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial (not registered) Duration of follow‐up: 3 weeks Study period: not reported |
|
| Participants |
Country: USA Setting: eight units of a large nonprofit nursing home, Pennsylvania Participants
Baseline characteristics
|
|
| Interventions |
Intervention: Individualized Positive Psychosocial Intervention (IPPI) Active control: standardised 1‐to‐1 activities Control: usual care |
|
| Outcomes | No primary outcome defined.
|
|
| Funding | Alzheimer’s Association Tacrine Fund (Pilot Research Grant TRG‐95‐006) and the Pennsylvania Department of Health (4100054858) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Drawing sealed ward‐numbers (unpublished information). |
| Allocation concealment (selection bias) | High risk | No information reported, group allocation was not concealed (unpublished information from the study author). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "Having each unit provide only one of the two experimental conditions mitigated the possibility of cross‐contamination because staff members were blinded to the condition of their unit." On each unit, one group of residents received one type of activity programme (intervention or active control) and another group of participants received usual care; blinding of personnel refers only to the type of activity programme (intervention or active control). Since nursing staff was aware whether a participant received an activity programme or usual care there is a risk of contamination. We judged risk of performance bias to be high. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Before data collection began, RA training included studying the coding manual, observing senior researchers code resident behavior, discussing coding decisions, and practicing coding with a mentor. Within 2 months, all trainees showed adequate reliability (75% agreement or better) and could code interventions independently. Each week, the research team analysed reliability." Outcomes were assessed by trained research assistants using a technical device (event recorder). No information about blinding was reported. We have insufficient information to permit judgement of ‘low risk’ or ‘high risk'. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Participants lost to follow‐up: n = 15; intervention group: n = 5 (n = 3 refused, n = 1 died, n = 1 hospitalised), active control group: n = 6 (n = 1 refused, n = 0 died, n = 5 hospitalised), usual care group: n = 4 (n = 2 refused, n = 1 died, n = 1 hospitalised). |
| Selective reporting (reporting bias) | Unclear risk | Not registered, no study protocol available. |
| Other bias | Low risk | ‐ |
Wenborn 2013.
| Study characteristics | ||
| Methods |
Study design: cluster‐randomised controlled trial (ISRCTN67952488, retrospectively registered) Duration of follow‐up: 28 weeks (16 weeks delivery of the intervention, 12 weeks post‐intervention follow‐up) Study period: not reported |
|
| Participants |
Country: UK Setting: care homes across London Participants/clusters
Baseline characteristics
|
|
| Interventions |
Intervention: staff training designed to enable care home staff to provide personalised activities Control: usual care |
|
| Outcomes |
Primary: Quality of Life (QoL‐AD, self‐ and caregiver‐rating) Secondary: challenging behaviour (CBS), depression (CSD), anxiety (RAID), number and type of medication |
|
| Funding | North East London Mental Health NHS Trust ‒ Occupational Therapy service; UK | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Care homes were recruited as matched pairs (matched according to provider: statutory, private or voluntary organisation and size). In each pair, 1 care home was allocated to the intervention group and the other to the control group using a computer random number generator (published and unpublished information). |
| Allocation concealment (selection bias) | Low risk | Allocation was performed by a remote randomisation service (unpublished information). |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information reported. The nursing staff was trained to deliver the intervention; therefore blinding seems not possible, but the intervention was delivered at the cluster level. We have insufficient information to permit judgement of ‘low risk’ or ‘high risk'. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes were assessed by the primary investigator "at baseline and by blinded assessors at follow‐up." Baseline assessment was conducted before the clusters were randomised. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Participants lost to follow‐up: n = 51; intervention group n = 25 (n = 17 died, n = 7 admitted to hospital, n = 1 moved), control group n = 26 (n = 23 died, n = 1 admitted to hospital, n = 2 moved). |
| Selective reporting (reporting bias) | Unclear risk | Study was retrospectively registered, no study protocol available. |
| Other bias | Low risk | ‐ |
Yuen 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial (not registered) Duration of follow‐up: 2 weeks Study period: not reported |
|
| Participants |
Country: Hong Kong, New Territories West region Setting: one long‐term care home Participants
Baseline characteristics
|
|
| Interventions |
Intervention: DementiAbility Methods: The Montessori Way Control: structured social activities |
|
| Outcomes | Agitation (CMAI, Chinese version) | |
| Funding | No information reported | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After screening, 46 demented residents with moderate to severe cognitive decline were randomly allocated into the DMMW intervention (DMMW; n = 23) group and the structured social activities (Structured social activities as control [SC]; n = 23) control group." Method of sequence generation not reported. |
| Allocation concealment (selection bias) | Unclear risk | No information reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "The structure and format of the intervention and control groups were designed to parallel each other in terms of their duration (ie, 45 minutes per session) and frequency of sessions (ie, three times per week) and group size. The intervention group was administered by certified DMMW practitioner while the control group was administered by noncertified professional who had same years of allied health experience in dementia care." Participants of both study groups received any intervention and we judged risk of performance bias to be low. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The assessment on participants was conducted by trained raters, including personal care worker and nurse who were blind to group assignment of the participants." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "There was full attendance and no attribution during the study period." |
| Selective reporting (reporting bias) | Unclear risk | Not registered, no study protocol available. |
| Other bias | Low risk | ‐ |
ABMI = Agitation Behavior Mapping Instrument; ADL = Activities of daily living; ARS = Philadelphia Geriatric Center Affect Rating Scale; CAPE‐BRS = Clifton Assessment Procedures for the Elderly – Behaviour Rating Scale; CBS = Challenging Behaviour Scale; CDR = Clinical Dementia Rating Scale; CMAI = Cohen‐Mansfield Agitation Inventory; CSD = Cornell Scale for Depression; DMMW = DementiAbility Methods: The Montessori Way; DSM = Diagnostic and Statistical Manual of Mental Disorders; GDS‐12R = Geriatric Depression Scale; MDS = Minimum Data Set; MMSE = mini mental state examination; MPES = Menorah Park Engagement Scale; MRI‐ES = Myers Research Institute Engagement Scale; PDS = Passivity in Dementia Scale; QoL‐AD = Quality of Life ‐ Alzheimer's Disease; RAID = Rating Anxiety in Dementia scale; SD: standard deviation; sMMSE = standardized Mini‐Mental State Examination score; TREA = Treatment Routes for Exploring Agitation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACTRN12618001505291 | Ineligible intervention |
| Beck 2002 | Ineligible intervention |
| Chan 2021 | Ineligible population |
| Chaudhry 2020 | Ineligible study design |
| Cohen‐Mansfield 2006 | Ineligible setting (participants recruited from both long‐term care facilities and day centres, no data on the different settings available) |
| Davison 2016 | Ineligible intervention |
| Diehl 2020 | Ineligible intervention |
| DiNapoli 2016 | Ineligible setting (geriatric psychiatry) |
| Eloniemi‐Sulkava 2019 | Ineligible intervention |
| Farina 2006 | Ineligible setting (day care centre) |
| Farina 2009 | Ineligible setting (day care centre) |
| Gaspar 2020 | Ineligible study design |
| Gerber 1991 | Ineligible setting (psychiatric hospital) |
| Hong 2011 | Ineligible intervention |
| Hopman‐Rock 1999 | Ineligible intervention |
| Hsu 2015 | Ineligible intervention |
| Kolanowski 2005 | Ineligible study design |
| Koskela 2017 | Ineligible intervention |
| Kovach 2004 | Ineligible intervention |
| Lin 2009 | Ineligible intervention |
| Livingston 2019 | Ineligible intervention |
| Luttenberger 2012 | Ineligible intervention |
| Mansbach 2017 | Ineligible intervention |
| Meeks 2008 | Ineligible population |
| Morley 2014 | Ineligible study design |
| Mowrey 2013 | Ineligible study design |
| NCT04515875 | Ineligible population |
| O'Sullivan 2021 | Ineligible intervention |
| O'Sullivan 2022 | Ineligible intervention |
| Patel 2016 | Ineligible study design |
| Pieper 2016 | Ineligible intervention |
| Politis 2004 | Ineligible intervention |
| Rapp 2013 | Ineligible intervention |
| Sackley 2009 | Ineligible intervention |
| Sánchez 2016 | Ineligible intervention |
| Schneider 2003 | Ineligible study design |
| Smith 2019 | Ineligible study design |
| Sung 2010 | Ineligible intervention |
| Treusch 2015 | Ineligible intervention |
| Vink 2014 | Ineligible intervention |
| Wilkinson 2018 | Ineligible intervention |
| Wilks 2019 | Ineligible study design |
Differences between protocol and review
In the protocol, adverse events were planned as secondary outcomes. Due to changes in the Cochrane Handbook, adverse events are a primary outcome in the review update.
Contributions of authors
RM and GM initially planned the study. RM, AR, HR and GM wrote the study protocol.
In the first version of this review (Möhler 2018), RM, AR and HR selected studies, conducted the critical appraisal and extracted data. RM, AR and GM interpreted the study data. RM contacted the study authors and wrote the drafts of the review. All authors contributed to all drafts of the review.
In this update, RM and SC selected studies, conducted the critical appraisal and extracted data. RM, SC, and GM interpreted the study data. RM contacted the study authors and wrote the drafts of the review. All authors contributed to all drafts of the review.
Sources of support
Internal sources
No sources of support provided
External sources
-
Ministry of Education and Research, Germany
The preparation of the first version of this review was supported by the German Ministry of Education and Research (Grant number 01 KG 1022)
-
NIHR, UK
This review update was supported by the National Institute for Health and Care Research (NIHR), via Cochrane Infrastructure funding to the Cochrane Dementia and Cognitive Improvement group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service or the Department of Health.
Declarations of interest
RM: none known.
SC: none known.
AR: none known.
HR: none known.
GM: none known.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Cohen‐Mansfield 2007 {published data only}
- Cohen-Mansfield J, Libin A, Marx MS. Nonpharmacological treatment of agitation: a controlled trial of systematic individualized intervention. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2007;62(8):908-16. [DOI] [PubMed] [Google Scholar]
Cohen‐Mansfield 2012 {published data only}
- Cohen-Mansfield J, Thein K, Marx MS, Dakheel-Ali M, Freedman L. Efficacy of nonpharmacologic interventions for agitation in advanced dementia: a randomized, placebo-controlled trial. Journal of Clinical Psychiatry 2012;73(9):1255-61. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Thein K, Marx MS, Dakheel-Ali M. What are the barriers to performing nonpharmacological interventions for behavioral symptoms in the nursing home? Journal of the American Medical Directors Association 2012;13(4):400-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00820859. Treatment Routes for Exploring Agitation (TREA). www.clinicaltrials.gov/ct2/show/NCT00820859 (first received 12 January 2009).
Kolanowski 2011 {published and unpublished data}
- Kolanowski A, Litaker M, Buettner L, Moeller J, Costa PT Jr. A randomized clinical trial of theory-based activities for the behavioral symptoms of dementia in nursing home residents. Journal of the American Geriatrics Society 2011;59(6):1032-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00388544. Enhancing Quality of Life for Nursing Home Residents. www.clinicaltrials.gov/ct2/show/NCT00388544 (first received 17 October 2006).
Mbakile‐Mahlanza 2020 {published data only}
- ACTRN12611000998943. A cluster-randomised controlled trial of family-mediated personalised activities for nursing home residents with dementia. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12611000998943 (first received 19 September 2011).
- Mbakile-Mahlanza L, Van der Ploeg ES, Busija L, Camp C, Walker H, O'Connor DW. A cluster-randomized crossover trial of Montessori activities delivered by family carers to nursing home residents with behavioral and psychological symptoms of dementia. International Psychogeriatrics 2020;32(3):347-58. [DOI] [PubMed] [Google Scholar]
- Ploeg ES, Camp CJ, Eppingstall B, Runci SJ, O'Connor DW. The study protocol of a cluster-randomised controlled trial of family-mediated personalised activities for nursing home residents with dementia. BMC Geriatrics 2012;12:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Orsulic‐Jeras 2000 {published data only}
- Orsulic-Jeras S, Schneider NM, Camp CJ. Montessori-based activities for long-term care residents with dementia. Topics in Geriatric Rehabilitation 2000;16(1):78-91. [DOI] [PubMed] [Google Scholar]
Richards 2005 {published data only}
- Richards KC, Beck C, O'Sullivan PS, Shue VM. Effect of individualized social activity on sleep in nursing rome residents with dementia. Journal of the American Geriatrics Society 2005;53(9):1510-7. [DOI] [PubMed] [Google Scholar]
Travers 2017 {published data only}
- ACTRN12613000296730. Having more fun: Increasing enjoyable activities to improve mood in nursing home residents with Alzheimer’s disease: A pilot study. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12613000296730 (first received 11 March 2013).
- Travers C. Increasing enjoyable activities to treat depression in nursing home residents with dementia: a pilot study. Dementia 2017;16(2):204-18. [DOI] [PubMed] [Google Scholar]
van der Ploeg 2013 {published and unpublished data}
- ACTRN12609000564257. Personalised, one-to-one interaction using Montessori-type activities as a treatment of challenging behaviours in people with dementia: a pilot controlled trial. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12609000564257 (first received 9 July 2009).
- Ploeg ES, Eppingstall B, Camp CJ, Runci SJ, Taffe J, O'Connor DW. A randomized crossover trial to study the effect of personalized, one-to-one interaction using Montessori-based activities on agitation, affect, and engagement in nursing home residents with Dementia. International Psychogeriatrics 2013;25(4):565-75. [DOI] [PubMed] [Google Scholar]
- Ploeg ES, O'Connor DW. Evaluation of personalised, one-to-one interaction using Montessori-type activities as a treatment of challenging behaviours in people with dementia: the study protocol of a crossover trial. BMC Geriatrics 2010;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Haitsma 2015 {published data only}
- Van Haitsma KS, Curyto K, Abbott KM, Towsley GL, Spector A, Kleban M. A randomized controlled trial for an individualized positive psychosocial intervention for the affective and behavioral symptoms of dementia in nursing home residents. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 2015;70(1):35-45. [DOI] [PubMed] [Google Scholar]
Wenborn 2013 {published data only}
- ISRCTN67952488. Does occupational therapy intervention improve the quality of life for older people with dementia in a care home setting? www.isrctn.com/ISRCTN67952488?q=ISRCTN67952488 (first received 6 October 2006).
- Wenborn J, Challis D, Head J, Miranda-Castillo C, Popham C, Thakur R, et al. Providing activity for people with dementia in care homes: A cluster randomised controlled trial. International Journal of Geriatric Psychiatry 2013;28(12):1296-304. [DOI] [PubMed] [Google Scholar]
Yuen 2019 {published data only}
- Yuen I, Kwok T. Effectiveness of DementiAbility methods: the Montessori way on agitation in long-term care home residents with dementia in Hong Kong. International Journal of Geriatric Psychiatry 2019;34(9):1352-8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
ACTRN12618001505291 {published data only}
- iPads for people with dementia in residential care: a feasibility pilot randomized controlled trial. www.anzctr.org.au/ACTRN12618001505291.aspx.
Beck 2002 {published data only}
- Beck CK, Vogelpohl TS, Rasin JH, Uriri JT, O'Sullivan P, Walls R, et al. Effects of behavioral interventions on disruptive behavior and affect in demented nursing home residents. Nursing Research 2002;51(4):219-28. [DOI] [PubMed] [Google Scholar]
Chan 2021 {published data only}
- Chan HY, Yau YM, Li SF, Kwong KS, Chong YY, Lee IF, et al. Effects of a culturally adapted group based Montessori based activities on engagement and affect in Chinese older people with dementia: a randomized controlled trial. BMC Geriatrics 2021;21(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chaudhry 2020 {published data only}
- Chaudhry N, Tofique S, Husain N, Couture D, Glasgow P, Husain M, et al. Montessori intervention for individuals with dementia: feasibility study of a culturally adapted psychosocial intervention in Pakistan (MIRACLE). BJPsych Open 2020;6(4):e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen‐Mansfield 2006 {published data only}
- Cohen-Mansfield J, Parpura-Gill A, Golander H. Utilization of self-identity roles for designing interventions for persons with dementia. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 2006;61(4):P202-12. [DOI] [PubMed] [Google Scholar]
Davison 2016 {published data only}
- Davison TE, Nayer K, Coxon S, Bono A, Eppingstall B, Jeon Y-H, et al. A personalized multimedia device to treat agitated behavior and improve mood in people with dementia: a pilot study. Geriatric Nursing 2016;37(1):25-39. [DOI] [PubMed] [Google Scholar]
Diehl 2020 {published data only}
- Diehl K, Kratzer A, Graessel E. The MAKS-s study: multicomponent non-pharmacological intervention for people with severe dementia in inpatient care - study protocol of a randomised controlled trial. BMC Geriatrics 2020;20(1):405. [DOI] [PMC free article] [PubMed] [Google Scholar]
DiNapoli 2016 {published data only}
- DiNapoli EA, Scogin F, Bryant AN, Sebastian S, Mundy MJ. Effect of individualized social activities on quality of life among older adults with mild to moderate cognitive impairment in a geriatric psychiatry facility. Aging & Mental Health 2016;20(3):262-70. [DOI] [PubMed] [Google Scholar]
Eloniemi‐Sulkava 2019 {published data only}
- Eloniemi-Sulkava U, Pesonen T, Savikko N, Koskinen J, Sulkava R, Woods B. Changing Minds in care of people with dementia in Finland. Randomised controlled trial [2019]. International Psychogeriatrics 2019;31(Supplement 1):52. [Google Scholar]
Farina 2006 {published data only}
- Farina E, Mantovani F, Fioravanti R, Pignatti R, Chiavari L, Imbornone E, et al. Evaluating two group programmes of cognitive training in mild-to-moderate AD: is there any difference between a 'global' stimulation and a 'cognitive-specific' one? Aging and Mental Health 2006;10(3):211-8. [DOI] [PubMed] [Google Scholar]
Farina 2009 {published data only}
- Farina E, Villanelli F. Conducting an Intervention Program Mediated by Recreational Activities and Socialization in Groups for Clients with Alzheimer's Disease. In: Söderback I, editors(s). International Handbook of Occupational Therapy Interventions. Springer, 2009:423-9. [Google Scholar]
Gaspar 2020 {published data only}
- Gaspar PM, Westberg K. Evaluation of the Montessori-Inspired Lifestyle R as the Foundation of Care in Assisted Living Memory Care. Journal of Gerontological Nursing 2020;46(5):40-6. [DOI] [PubMed] [Google Scholar]
Gerber 1991 {published data only}
- Gerber GJ, Prince PN, Snider HG, Atchison K, Dubois L, Kilgour JA. Group activity and cognitive improvement among patients with Alzheimer's disease. Hospital and Community Psychiatry 1991;42(8):843-5. [DOI] [PubMed] [Google Scholar]
Hong 2011 {published data only}
- Hong GR. [Effects of multisensory stimulation using familiarity: persons with dementia in long-term care facility in Korea]. Journal of Korean Academy of Nursing 2011;41(4):528-38. [DOI] [PubMed] [Google Scholar]
Hopman‐Rock 1999 {published data only}
- Hopman-Rock M, Staats PG, Tak EC, Dröes RM. The effects of a psychomotor activation programme for use in groups of cognitively impaired people in homes for the elderly. International Journal of Geriatric Psychiatry 1999;14(8):633-42. [DOI] [PubMed] [Google Scholar]
Hsu 2015 {published data only}
- Hsu MH, Flowerdew R, Parker M, Fachner J, Odell-Miller H. Individual music therapy for managing neuropsychiatric symptoms for people with dementia and their carers: a cluster randomised controlled feasibility study. BMC Geriatrics 2015;15:84. [DOI] [PMC free article] [PubMed]
Kolanowski 2005 {published and unpublished data}
- Kolanowski AM, Litaker M, Buettner L. Efficacy of theory-based activities for behavioral symptoms of dementia. Nursing Research 2005;54(4):219-28. [DOI] [PubMed] [Google Scholar]
Koskela 2017 {published data only}
- Koskela SA, Jones F, Clarke N, Anderson L, Kennedy B, Grant R, et al. Active Residents in Care Homes (ARCH): study protocol to investigate the implementation and outcomes of a whole-systems activity programme in residential care homes for older people. Physiotherapy 2017;103(1):113-20. [DOI] [PubMed] [Google Scholar]
- Smith R, Wood J, Jones F, Anderson L, Hurley M. Active residents in care homes: A holistic approach to promoting and encouraging meaningful activity for residents living in care homes: Innovative Practice. Dementia (London) 2019;18(5):1942-47. [DOI] [PubMed] [Google Scholar]
Kovach 2004 {published data only}
- Kovach CR, Taneli Y, Dohearty P, Schlidt AM, Cashin S, Silva-Smith AL. Effect of the BACE intervention on agitation of people with dementia. Gerontologist 2004;44(6):797-806. [DOI] [PubMed] [Google Scholar]
Lin 2009 {published data only}
- Lin LC, Yang MH, Kao CC, Wu SC, Tang SH, Lin JG. Using acupressure and Montessori-based activities to decrease agitation for residents with dementia: a cross-over trial. Journal of the American Geriatrics Society 2009;57(6):1022-9. [DOI] [PubMed] [Google Scholar]
Livingston 2019 {published data only}
- Livingston G, Barber J, Marston L, Stringer A, Panca M, Hunter R, et al. Clinical and cost-effectiveness of the Managing Agitation and Raising Quality of Life (MARQUE) intervention for agitation in people with dementia in care homes: a single-blind, cluster-randomised controlled trial. Lancet Psychiatry 2019;6(4):293-304. [DOI] [PubMed] [Google Scholar]
Luttenberger 2012 {published data only}
- Luttenberger K, Donath C, Uter W, Graessel E. Effects of multimodal nondrug therapy on dementia symptoms and need for care in nursing home residents with degenerative dementia: a randomized-controlled study with 6-month follow-up. Journal of the American Geriatrics Society 2012;60(5):830-40. [DOI] [PubMed] [Google Scholar]
Mansbach 2017 {published data only}
- Mansbach WE, Mace RA, Clark KM, Firth IM. Meaningful activity for long-term care residents with dementia: a comparison of activities and raters. Gerontologist 2017;57(1):461-8. [DOI] [PubMed] [Google Scholar]
Meeks 2008 {published data only}
- Meeks S, Looney SW, Van Haitsma K, Teri L. BE-ACTIV: A staff-assisted behavioral intervention for depression in nursing homes. Gerontologist 2008;48(1):105-14. [DOI] [PubMed] [Google Scholar]
Morley 2014 {published data only}
- Morley JE, Philpot CD, Gill D, Berg-Weger M. Meaningful activities in the nursing home. Journal of the American Medical Directors Association 2014;15(2):79-81. [DOI] [PubMed] [Google Scholar]
Mowrey 2013 {published data only}
- Mowrey C, Parikh PJ, Bharwani G, Bharwani M. Application of behavior-based ergonomics therapies to improve quality of life and reduce medication usage for Alzheimer's/dementia residents. American Journal of Alzheimer's Disease and Other Dementias 2013;28(1):35-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT04515875 {published data only}
- PREMA Intervention for Adults With Mild Cognitive Impairment and Their Caregivers (PREMA). www.clinicaltrials.gov/ct2/show/NCT04515875.
O'Sullivan 2021 {published data only}
- O'Sullivan JL, Lech S, Gellert P, Grittner U, Voigt-Antons JN, Möller S, et al. A tablet-based intervention for activating nursing home residents with dementia: results from a cluster-randomized controlled trial. International Psychogeriatrics 2022;34(2):129-41. [DOI] [PubMed] [Google Scholar]
O'Sullivan 2022 {published data only}
- O'Sullivan JL, Lech S, Gellert P, Grittner U, Voigt-Antons JN, Möller S, et al. A tablet-based intervention for activating nursing home residents with dementia: results from a cluster-randomized controlled trial. 2022 International Psychogeriatrics;34(2):129-41. [DOI] [PubMed] [Google Scholar]
Patel 2016 {published data only}
- Patel P, Porter T, Smith J, Mirk A. Montessori based activities in veterans with severe dementia: engagement, affect, and behavior. Journal of the American Geriatrics Society 2016;64(Supplement S1):S66-7. [Google Scholar]
Pieper 2016 {published data only}
- Pieper MJ, Francke AL, Steen JT, Scherder EJ, Twisk JW, Kovach CR, Achterberg WP. Effects of a stepwise multidisciplinary intervention for challenging behavior in advanced dementia: a cluster randomized controlled trial. Journal of the American Geriatrics Society 2016;64(2):261-9. [DOI] [PubMed] [Google Scholar]
Politis 2004 {published data only}
- Politis AM, Vozzella S, Mayer LS, Onyike CU, Baker AS, Lyketsos CG. A randomized, controlled, clinical trial of activity therapy for apathy in patients with dementia residing in long-term care. International Journal of Geriatric Psychiatry 2004;19(11):1087-94. [DOI] [PubMed] [Google Scholar]
Rapp 2013 {published data only}
- Rapp MA, Mell T, Majic T, Treusch Y, Nordheim J, Niemann-Mirmehdi M, et al. Agitation in nursing home residents with dementia (VIDEANT Trial): effects of a cluster-randomized, controlled, guideline implementation trial. Journal of the American Medical Directors Association 2013;14(9):690-5. [DOI] [PubMed] [Google Scholar]
Sackley 2009 {published data only}
- Sackley CM, Van Den Berg ME, Lett K, Patel S, Hollands K, Wright CC, et al. Effects of a physiotherapy and occupational therapy intervention on mobility and activity in care home residents: A cluster randomised controlled trial. BMJ 2009;339(7722):670-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sánchez 2016 {published data only}
- Sánchez A, Marante-Moar MP, Sarabia C, Labra C, Lorenzo T, Maseda A, et al. Multisensory stimulation as an intervention strategy for elderly patients with severe dementia: a pilot randomized controlled trial. American Journal of Alzheimer's Disease and Other Dementias 2016;31(4):341-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schneider 2003 {published data only}
- Schneider NM, Camp CJ. Use of Montessori-based activities by visitors of nursing home residents with dementia. Clinical Gerontologist 2003;26(1-2):71-84. [Google Scholar]
Smith 2019 {published data only}
- Smith R, Wood J, Jones F, Anderson L, Hurley M. Active residents in care homes: a holistic approach to promoting and encouraging meaningful activity for residents living in care homes: innovative Practice. Dementia 2019;18(5):1942-47. [DOI] [PubMed] [Google Scholar]
Sung 2010 {published data only}
- Sung HC, Chang AM, Lee WL. A preferred music listening intervention to reduce anxiety in older adults with dementia in nursing homes. Journal of Clinical Nursing 2010;19(7-8):1056-64. [DOI] [PubMed] [Google Scholar]
Treusch 2015 {published data only}
- Treusch Y, Majic T, Page J, Gutzmann H, Heinz A, Rapp MA. Apathy in nursing home residents with dementia: results from a cluster-randomized controlled trial. European Psychiatry 2015;30(2):251-7. [DOI] [PubMed] [Google Scholar]
Vink 2014 {published data only}
- Vink AC, Zuidersma M, Boersma F, Jonge P, Zuidema SU, Slaets JP. Effect of music therapy versus recreational activities on neuropsychiatric symptoms in elderly adults with dementia: an exploratory randomized controlled trial. Journal of the American Geriatrics Society 2014;62(2):392-3. [DOI] [PubMed] [Google Scholar]
Wilkinson 2018 {published data only}
- Wilkinson A, Chignell M, Kanik M, O'Neill J. Designing for dementia: the impact of interactive ambient technology on well-being in long-term care homes. Alzheimer's & Dementia 2018;14(7 Supplement):P636. [Google Scholar]
Wilks 2019 {published data only}
- Wilks SE, Boyd PA, Bates SM, Cain DS, Geiger JR. Montessori-based activities among persons with late-stage dementia: evaluation of mental and behavioral health outcomes. Dementia (London) 2019;18(4):1373-92. [DOI] [PubMed] [Google Scholar]
Additional references
Adlbrecht 2022
- Adlbrecht L, Nemeth T, Frommlet F, Bartholomeyczik S, Mayer H. Engagement in purposeful activities and social interactions amongst persons with dementia in special care units compared to traditional nursing homes: An observational study. Scandinavian Journal of Caring Science 2022;36(3):650-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alexopoulos 1988
- Alexopoulos GS, Abrams RC, Young RC, Shamoian CA. Cornell Scale for depression in dementia. Biological Psychiatry 1988;23(3):271-84. [DOI] [PubMed] [Google Scholar]
Algase 1996
- Algase DL, Beck C, Kolanowski A, Whall A, Berent SK, Richards K, et al. Need-driven dementia-compromised behavior: an alternative view of disruptive behavior. American Journal of Alzheimer's Disease and Other Dementias 1996;11(6):10–9. [Google Scholar]
American Psychiatric Association 1994
- American Psychiatric Association. Diagnosis and statistical manual of mental disorders (4th edition). Washington (DC): American Psychiatric Association, 1994. [Google Scholar]
Arons 2013
- Arons AM, Krabbe PF, Schölzel-Dorenbos CJ, Wilt GJ, Rikkert MG. Quality of life in dementia: a study on proxy bias. BMC Medical Research Methodology 2013;13:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buettner 2003
- Buettner LL, Fitzsimmons S. Activity calendars for older adults with dementia: what you see is not what you get. American Journal of Alzheimer's Disease and other Dementias 2003;18(4):215-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burks 2021
- Burks HB, des Bordes JK, Chadha R, Holmes HM, Rianon NJ. Quality of life assessment in older adults with dementia: a systematic review. Dementia and Geriatric Cognitive Disorders 2021;50(2):103-10. [DOI] [PubMed] [Google Scholar]
Campbell 2012
- Campbell MK, Piaggio G, Elbourne DR, Altman DG, CONSORT Group. Consort 2010 statement: extension to cluster randomised trials. BMJ 2012;345:e5661. [DOI] [PubMed] [Google Scholar]
Cohen‐Mansfield 1989a
- Cohen-Mansfield J, Werner P, Marx MS. An observational study of agitation in agitated nursing home residents. International Psychogeriatrics 1989;1(2):153-65. [DOI] [PubMed] [Google Scholar]
Cohen‐Mansfield 1989b
- Cohen-Mansfield J, Marx M, Rosenthal S. A description of agitation in a nursing home. Journal of Gerontology 1989;44(3):M77–M84. [DOI] [PubMed] [Google Scholar]
Cohen‐Mansfield 2000
- Cohen-Mansfield J. Theoretical frameworks for behavioral problems in dementia. Alzheimer's Care Today 2000;1(4):8-21. [Google Scholar]
Cohen‐Mansfield 2004
- Cohen-Mansfield J, Libin A. Assessment of agitation in elderly patients with dementia: correlations between informant rating and direct observation. International Journal of Geriatric Psychiatry 2004;19(9):881-91. [DOI] [PubMed] [Google Scholar]
Cohen‐Mansfield 2010
- Cohen-Mansfield J, Marx MS, Thein K, Dakheel-Ali M. The impact of past and present preferences on stimulus engagement in nursing home residents with dementia. Aging & Mental Health 2010;14(1):67-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen‐Mansfield 2011
- Cohen-Mansfield J, Marx MS, Freedman LS, Murad H, Regier NG, Thein K, et al. The comprehensive process model of engagement. American Journal of Geriatric Psychiatry 2011;19(10):859-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Colling 2000
- Colling KB. A taxonomy of passive behaviors in people with Alzheimer's disease. Journal of Nursing Scholarship 2000;32(3):239-44. [DOI] [PubMed] [Google Scholar]
Cooney 2009
- Cooney A, Murphy K, O'Shea E. Resident perspectives of the determinants of quality of life in residential care in Ireland. Journal of Advanced Nursing 2009;65(5):1029-38. [DOI] [PubMed] [Google Scholar]
Costa 1992
- Costa P, McCrae R. Revised NEO personality inventory and NEO five-factor inventory: professional manual. Odessa: Psychological Assessment Resources, 1992. [Google Scholar]
Craig 2008
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deci 2000
- Deci EL, Ryan RM. The "what" and "why" of goal pursuits: Human needs and the self-determination of behavior. Psychological Inquiry 2000;11(4):227-68. [Google Scholar]
Dobbs 2005
- Dobbs D, Munn J, Zimmerman S, Boustani M, Williams CS, Sloane PD, et al. Characteristics associated with lower activity involvement in long-term care residents with dementia. Gerontologist 2005;1(Suppl 1):81-6. [DOI] [PubMed] [Google Scholar]
Edvardsson 2014
- Edvardsson D, Petersson L, Sjogren K, Lindkvist M, Sandman P-O. Everyday activities for people with dementia in residential aged care: associations with person-centredness and quality of life. International Journal of Older People Nursing 2014;9(4):269-76. [DOI] [PubMed] [Google Scholar]
Eldridge 2016
- Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Pilot and Feasibility Studies 2016;2:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fazio 2018
- Fazio S, Pace D, Maslow K, Zimmerman S, Kallmyer B. Alzheimer's Association dementia care practice recommendations. Gerontologist 2018;58(suppl 1):S1-S9. [DOI] [PubMed] [Google Scholar]
Fredrickson 2001
- Fredrickson BL. The role of positive emotions in positive psychology. The broaden-and-build theory of positive emotions. American Psychologist 2001;56(3):218-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
GBD 2019 Dementia Forecasting Collaborators 2022
- GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022;7(2):e105-e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gomez‐Gallego 2015
- Gomez-Gallego M, Gomez-Garcia J, Ato-Lozano E. Addressing the bias problem in the assessment of the quality of life of patients with dementia: determinants of the accuracy and precision of the proxy ratings. Journal of Nutrition, Health & Aging 2015;19(3):365-72. [DOI] [PubMed] [Google Scholar]
Grant 2013
- Grant A, Treweek S, Dreischulte T, Foy R, Guthrie B. Process evaluations for cluster-randomised trials of complex interventions: a proposed framework for design and reporting. Trials 2013;14:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guétin 2009
- Guétin S, Portet F, Picot MC, Pommié C, Messaoudi M, Djabelkir L, et al. Effect of music therapy on anxiety and depression in patients with Alzheimer's type dementia: randomised, controlled study. Dementia and Geriatric Cognitive Disorders 2009;28(1):36-46. [DOI] [PubMed] [Google Scholar]
Guise 2017
- Guise JM, Chang C, Butler M, Viswanathan M, Tugwell P. AHRQ series on complex intervention systematic reviews-paper 1: an introduction to a series of articles that provide guidance and tools for reviews of complex interventions. Journal of Clinical Epidemiology 2017;90:6-10. [DOI] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383-94. [DOI] [PubMed] [Google Scholar]
Han 2016
- Han A, Radel J, McDowd JM, Sabata D. Perspectives of people with dementia about meaningful activities: a synthesis. American Journal of Alzheimer's Disease and Other Dementias 2016;31(2):115-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harmer 2008
- Harmer BJ, Orrell M. What is meaningful activity for people with dementia living in care homes? A comparison of the views of older people with dementia, staff and family carers. Aging & Mental Health 2008;12(5):548-58. [DOI] [PubMed] [Google Scholar]
Helvik 2015
- Helvik AS, Engedal K, Benth JŠ, Selbæk G. Prevalence and severity of dementia in nursing home residents. Dementia and Geriatric Cognitive Disorders 2015;40(3-4):166-77. [DOI] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017). The Cochrane Collaboration, 2017. Available from www.training.cochrane.org/handbook.
Higgins 2021
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook. [DOI] [PMC free article] [PubMed]
Hill 2010
- Hill NL, Kolanowski A, Kürüm E. Agreeableness and activity engagement in nursing home residents with dementia. Journal of Gerontological Nursing 2010;36(9):45-52. [DOI] [PubMed] [Google Scholar]
Hoffmann 2014
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. [DOI] [PubMed] [Google Scholar]
Judge 2000
- Judge KS, Camp CJ, Orsulic-Jeras S. Use of montessori-based activities for clients with dementia in adult daycare: effects on engagement. American Journal of Alzheimer's Disease and Other Dementias 2000;15(1):42-6. [Google Scholar]
Kovach 1998
- Kovach CR, Magliocco JS. Late-stage dementia and participation in therapeutic activities. Applied Nursing Research 1998;11(4):167-73. [DOI] [PubMed] [Google Scholar]
Kristensen 2020
- Kristensen H, Peoples H. Experiences related to quality of life in people with dementia living in institutional settings–a meta-aggregation. British Journal of Occupational Therapy 2020;83(3):145-61. [Google Scholar]
Lawton 1996
- Lawton MP, Van Haitsma K, Klapper J. Observed affect in nursing home residents with Alzheimer's disease. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 1996;51(1):P3-14. [DOI] [PubMed] [Google Scholar]
Logsdon 1999
- Logsdon RG, Gibbons LE, McCurry SM, Teri L. Quality of life in Alzheimer’s disease: patient and caregiver reports. Journal of Mental Health and Aging 1999;5(1):21-32. [Google Scholar]
Michelet 2022
- Michelet M, Selbaek G, Strand BH, Lund A, Engedal K, Bieber A et al. Associations between unmet needs for daytime activities and company and scores on the Neuropsychiatric Inventory-Questionnaire in people with dementia: a longitudinal study. Aging & Mental Health 2022;26(4):725-34. [DOI] [PubMed] [Google Scholar]
Mills 1997
- Mills MA. Narrative identity and dementia: a study of emotion and narrative in older people with dementia. Ageing and Society 1997;17(6):673-98. [Google Scholar]
Möhler 2015
- Möhler R, Köpke S, Meyer G. Criteria for Reporting the Development and Evaluation of Complex Interventions in healthcare: revised guideline (CReDECI 2). Trials 2015;16(1):204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moniz‐Cook 2001
- Moniz-Cook E, Woods R, Gardiner E, Silver M, Agar S. The Challenging Behaviour Scale (CBS): development of a scale for staff caring for older people in residential and nursing homes. British Journal of Clinical Psychology 2001;40(Pt 3):309-22. [DOI] [PubMed] [Google Scholar]
Moore 2015
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350:h1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moyle 2012
- Moyle W, Murfield JE, Griffiths SG, Venturato L. Assessing quality of life of older people with dementia: a comparison of quantitative self-report and proxy accounts. Journal of Advanced Nursing 2012;68(10):2237-46. [DOI] [PubMed] [Google Scholar]
Murphy 2007
- Murphy K, Shea EO, Cooney A. Quality of life for older people living in long-stay settings in Ireland. Journal of Clinical Nursing 2007;16(11):2167-77. [DOI] [PubMed] [Google Scholar]
NICE 2018
- National Institute for Health and Care Excellence. Dementia: assessment, management and support for people living with dementia and their carers. NICE Clinical Guidelines; 2018. Available at www.nice.org.uk/guidance/ng97. [PubMed]
Phinney 2007
- Phinney A, Chaudhury H, O'Connor DL. Doing as much as I can do: the meaning of activity for people with dementia. Aging & Mental Health 2007;11(4):384-93. [DOI] [PubMed] [Google Scholar]
Richards 2001
- Richards KC, Sullivan SC, Phillips RL, Beck CK, Overton-McCoy AL. The effect of individualized activities on the sleep of nursing home residents who are cognitively impaired: a pilot study. Journal of Gerontological Nursing 2001;27(9):30-7. [DOI] [PubMed] [Google Scholar]
Shankar 1999
- Shankar KK, Walker M, Frost D, Orrell M. The development of a valid and reliable scale for rating anxiety in dementia (RAID). Aging & Mental Health 1999;3(1):39-49. [Google Scholar]
Skivington 2021
- Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ 2021;374:n2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
Skrajner 2007
- Skrajner MJ, Camp CJ. Resident-Assisted Montessori Programming (RAMP): use of a small group reading activity run by persons with dementia in adult day health care and long-term care settings. American Journal of Alzheimer's Disease and Other Dementias 2007;22(1):27-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2018
- Smith N, Towers A, Palmer S, Beecham J, Welch E. Being occupied: supporting ‘meaningful activity’in care homes for older people in England. Ageing & Society 2018;38(11):2218-40. [Google Scholar]
Stewart 2014
- Stewart R, Hotopf M, Dewey M, Ballard C, Bisla J, Calem M, et al. Current prevalence of dementia, depression and behavioural problems in the older adult care home sector: the South East London Care Home Survey. Age and Ageing 2014;43(4):562-7. [DOI] [PubMed] [Google Scholar]
Strick 2021
- Strick K, Abbott R, Thompson Coon J, Garside R. Meta-ethnography of the purpose of meaningful occupation for people living with dementia. International Journal of Older People Nursing 2021;16(5):e12391. [DOI] [PubMed] [Google Scholar]
Tappen 1995
- Tappen RM, Barry C. Assessment of affect in advanced Alzheimer's disease: the Dementia Mood Picture Test. Journal of Gerontological Nursing 1995;21(3):44-6. [DOI] [PubMed] [Google Scholar]
Testad 2014
- Testad I, Corbett A, Aarsland D, Lexow KO, Fossey J, Woods B, et al. The value of personalized psychosocial interventions to address behavioral and psychological symptoms in people with dementia living in care home settings: a systematic review. International Psychogeriatrics 2014;26(7):1083-98. [DOI] [PubMed] [Google Scholar]
Travers 2016
- Travers C, Brooks D, Hines S, O'Reilly M, McMaster M, He W, et al. Effectiveness of meaningful occupation interventions for people living with dementia in residential aged care: a systematic review. JBI Database of Systematic Reviews and Implementation Reports 2016;14(12):163-225. [DOI] [PubMed] [Google Scholar]
van der Linde 2014
- Linde RM, Stephan BC, Dening T, Brayne C. Instruments to measure behavioural and psychological symptoms of dementia. International Journal of Methods in Psychiatric Research 2014;23(1):69-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Haitsma 2000
- Van Haitsma K. The assessment and integration of preferences into care practices for persons with dementia residing in the nursing home. In: Rubinstein R, Moss M, Kleban M, editors(s). The many dimensions of aging. New York: Springer, 2000. [Google Scholar]
Vernooij‐Dassen 2007
- Vernooij-Dassen M. Meaningful activities for people with dementia. Aging & Mental Health 2007;11(4):359-60. [DOI] [PubMed] [Google Scholar]
Viswanathan 2017
- Viswanathan M, McPheeters ML, Murad MH, Butler ME, Devine EEB, Dyson MP et al. AHRQ series on complex intervention systematic reviews-paper 4: selecting analytic approaches. Journal of Clinical Epidemiology 2017;90:28-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wenborn 2008
- Wenborn J, Challis D, Pool J, Burgess J, Elliott N, Orrell M. Assessing the validity and reliability of the Pool Activity Level (PAL) Checklist for use with older people with dementia. Aging & Mental Health 2008;12(2):202-11. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Möhler 2012
- Möhler R, Renom A, Renom H, Meyer G. Personally-tailored activities for improving psychosocialoutcomes for people with dementia in long-term care. Cochrane Database of Systematic Reviews 2012, Issue 4. Art. No: CD009812. [DOI: 10.1002/14651858.CD009812] [DOI] [PMC free article] [PubMed] [Google Scholar]
Möhler 2018
- Möhler R, Renom A, Renom H, Meyer G. Personally tailored activities for improving psychosocial outcomes for people with dementia in long-term care. Cochrane Database of Systematic Reviews 2018, Issue 2. Art. No: CD009812. [DOI: 10.1002/14651858.CD009812.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


