Abstract
Background
Tuberculosis (TB) continues to be a common disease in developing countries, among which middle ear TB is rare. Furthermore, it is relatively difficult to make an early diagnosis and provide follow-up treatment for middle ear TB. So, it is necessary to report this case for reference and further discussion.
Case presentation
We reported 1 case of multidrug-resistant tuberculosis otitis media. TB otitis media is rare in tuberculosis; multidrug-resistant TB otitis media is even more rare. Our paper analyzes the possible causes, imaging, molecular biology, pathology, and clinical manifestations of multidrug-resistant TB otitis media.
Conclusion
PCR and DNA molecular biology techniques are highly recommended for the early diagnosis of multidrug-resistant TB otitis media. Early, effective anti-tuberculosis treatment is the guarantee for further recovery for patients with multidrug-resistant TB otitis media.
Keywords: Multidrug-resistant tuberculosis otitis media, Case report
Abbreviations: TB, Tuberculosis; CT, Computed tomography; MDR, multidrug-resistant; DNA, Deoxyribonucleic Acid; PCR, Polymerase chain reaction
1. Background
Tuberculosis continues to be a common disease in developing countries, and out-of-the-lung tuberculosis accounts for about 15% of TB (tuberculosis). It first affects the lymph nodes, then the pleural cavity, genitourinary tract, bone, and joints, with tuberculosis otitis media being a specific infection of TB branch bacteria in the middle ear mastodon [1], [2]. First reported in 1953, middle ear TB is relatively rare and often prone to delayed diagnosis and treatment [3], [4]. Current studies show that only 0.05–0.9% of chronic otitis media are caused by tuberculosis [5], and primary multidrug-resistant TB is even more rare as a serious challenge to medical practitioners. Although the pathogenesis of middle ear tuberculosis is still being debated, it is widely assumed that TB bacteria primarily infiltrate the middle ear through three routes: (1) other TB stove blood lines spread to the middle ear; (2) tympanic membrane perforation directly planted through the outer ear canal; and (3) airborne TB bacteria spread through the pharynx tube to the middle ear [6]. In our case, the tracheoscopy indicated the main trachea nodules (middle section), while it didn’t show changes in other trachea and bronchial tubes. Pathologic examination indicated that tracheal TB invades from the bronchiole to the segmental bronchi and lobar bronchi. With the TB culture results of ear canal secretions and tracheoscopy lavage solution, we concluded that the transmission of this case may be through tympanic membrane perforation through the outer ear canal directly planted, and tuberculosis is very likely for the middle ear TB transmission of lung secondary infection through the pharynx tube.
2. Case presentation
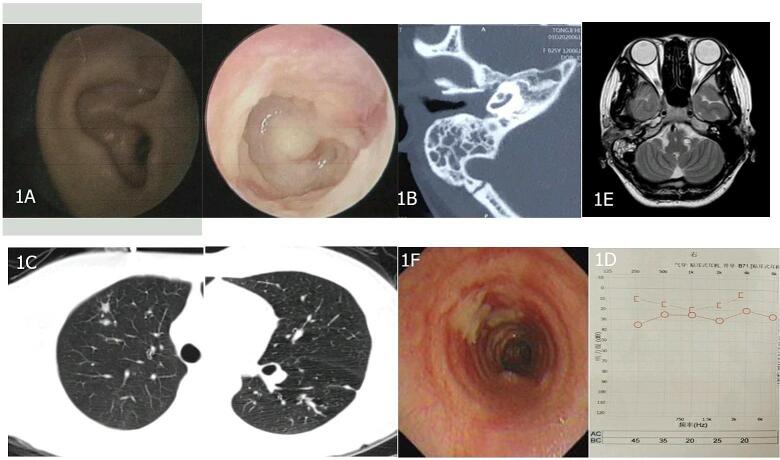
We presented a case of a 25 years old female patient, nurse; right ear fluid with coughing for 6 months. 6 months ago, she complained of right ear canal fluid, a transparent, viscous, odorless liquid accompanied by coughing up yellow sputum, with no obvious triggers. Other hospitals repeatedly gave anti-inflammatory treatment with “cephalosporins and quinolones.” Initially, symptoms were controlled, but they gradually returned, accompanied by earache, tinnitus, hearing loss, and ear tightness discomfort. As a result of it, the patient was transformed in our hospital. Here, we presented important examinations of this case. Past history was denial of tuberculosis, hypertension, and other medical histories. Physical examination: visible, water-like secretions in the right outer ear canal. Laboratory examination: hemoglobin-interferon release test (+). Endoscopy: The right tympanic membrane is bloated and has a perforation of the nervous part (Fig. 1A). Ear CT (computed tomography): the soft tissue density shadow can be seen in the outer ear canal, middle ear cavity, sinuses, and mastodon hive on the right side (Fig. 1B). Lung CT: Multiple nodules and nodules in the upper and lower left lobes of the right lung, considering the possibility of TB infection (Fig. 1C). Hearing test: right-ear hearing loss (Fig. 1D). Ear canal secretion examination: anti-acid staining (−), tuberculosis DNA (Deoxyribonucleic Acid) determination 1.0 × 10 × 6 copies/ml. According to the results, we firstly suspected the case as tuberculosis and ear TB. And we gave anti-tuberculosis (isoniazid, rifampicin, pyridine, acetaminophen), liver care treatment, symptoms improved. To confirm our hypothesis, we then performed TB specific examinations. After the detection of high amounts of multidrug-resistant TB-DNA in GeneXpert and the detection of flat-resistant genes, the reverse hybridization test of linear probes of ear canal secretions identified isoniazid and rifampicin drug-resistant genes, and fluoroquinolone-resistant gene mutations tested positive. Alveoli irrigation and lotion examination: antacid staining (−), TB DNA determination 1.0 × 10 × 4 copies/mL, multidrug-resistant (MDR) TB-DNA detection in GeneXpert medium, flat-resistant gene detection. Sputum anti-acid staining (−). Middle ear MRI: right ear with visible long T2 and long T1 signal inequality, granuloma lesions (Fig. 1E). Bronchoscopy examination: the middle section of the trachea pipe wall is filled with blood, swelling, granular nodules, and decay, a medium cheese-like necrosis wall, considering the main bronchial nodules (Fig. 1F). With these results, the patient was finally diagnosed with middle ear TB, tuberculosis, and bronchial nodules, multidrug-resistant TB. We soon performed anti-TB treatment (linezolid, cycloserine, propythioninamide, pyrazinamide, ethambutol, bedaquinoline). The symptoms relieved and the patient showed recovery after 1 months, and we followed treatment. After 10 months, the symptoms and signs were generally relieved, and the imaging and bacteriology examinations showed recovery.
Fig. 1.
Clinical Examination of the case.
3. Discussion and conclusions
Past studies have shown that the typical clinical characteristics of TB otitis media are painless ear leakage, multiple tympanic perforations, middle ear and mastodon granulomas, transsexual hearing loss, surface nerve paralysis, and ineffective treatment with conventional antibiotics [7]. In our report, the first symptom was painless ear leakage, and other symptoms such as external nerve palsy followed. According to the study before, about half of TB otitis media combines tuberculosis, so screening management for lung lesions should be strengthened for patients with TB otitis media [8]. However, some patients with TB otitis media do not develop pulmonary TB, and their symptoms and signs are similar to other chronic purulent otitis media, such as necrotizing otitis media, biliary lipoma, otitis, and its associated mastitis, resulting in diagnostic delays [9].
Imaging is very important for the diagnosis of TB otitis media. It shows that the visible soft tissue shadow of the tibia CT fills the whole drum chamber and the mastoid cavity, and there is bone damage absorption. The remaining bone edge is jagged or rat bite-like, and the bone damage is a regeneration reaction with diffuse lesions. Furthermore, dead bone formation is considered to be a typical clinical characteristic of TB otitis media [10]. In our case, CT suggested that soft tissue density shadows were visible in the outer ear canal, middle ear cavity, and celiac cavity, which is consistent with the above description. However, we found no bone damage or dead bone formation. It might be related to the patient's short course of illness and antibiotic control. In addition, chest CT is also important for the early diagnosis of tuberculosis.
Laboratory examinations commonly used for the disease include exosome secretion, anti-acid bacteria smears, culture, polymerase chain reaction (PCR), DNA, etc [8]. Because of the low positive rate of secretion smears and the long incubation time of Mycobacterium tuberculosis, some tests are not conducive to an early diagnosis of the disease [10]. Among them, PCR technology has the advantages of fast and easy automation. According to Cousins et al., PCR has a sensitivity of 98.2% and a specificity of 97.4% [11]. In our case, laboratory examination and the GeneXpert test suggest rifampicin resistance. Further refining the linear probe hybridization test, we found that the patients were resistant to isoniazid, rifampicin, and quinolones, so the final diagnosis of MDR-TB was finally made. Therefore, PCR is particularly important for the diagnosis of extrapulmonary tuberculosis with low-carrying bacteria.
The degree of local lesions and the patient's systemic conditions should be considered when treating TB otitis media. Treatment should include whole body and local anti-tuberculosis drug chemotherapy, surgery, etc., in which anti-tuberculosis treatment is essential, as it is reported that no anti-tuberculosis treatment after surgery may cause recurrence. Early, effective anti-tuberculosis treatment could help avoid invasive surgical intervention. Surgery is only necessary when anti-TB treatment fails or when ear-derived intracranial and intracranial complications occur, and anti-tuberculosis treatment is still required after surgery [13], [14]. For patients with acute open TB combined with TB otitis media, early and effective anti-tuberculosis treatment can prevent the occurrence of corresponding complications. Anti-tuberculosis treatment (isoniazid, rifampicin, pyrazinamide, ethambutol) for 6–12 months is highly recommended [10], [12]. However, if the patient combines chronic purulent tuberculosis otitis media or poor drainage, anti-tuberculosis treatment is ineffective with the formation of dead bones or combined with intracranial and external infections, anti-TB chemotherapy at the same time requires surgical treatment to shorten the course of treatment and improve dry ear rate [4]. In our case, we found the patient is multidrug-resistant (isoniazid, rifampicin, quinolone), and there were no encephalic or extracranial infection, so we used correspond treatment plan which worked well [13], [15].
The reasons for misdiagnosis and mistreatment of multidrug-resistant TB otitis media might be: (1) Multidrug-resistant TB otitis media is clinically rare, and otolaryngologists do not understand the disease enough. (2) The non-specificity of clinical manifestations. (3) The rate of positive anti-acid staining of ear secretions is low; (4) Its pathogenesis is unknown. (5) There is currently no relevant diagnostic guideline or consensus.
In summary, for the examination and treatment of MDR-TB otitis media, we should pay attention to the following matters: (1) After routine treatment, if the patient's otitis media symptoms do not improve or repeat, or if there is a past history of tuberculosis or close contact with TB, multidrug-resistant TB otitis media should be highly suspected. In addition, image inspection and laboratory testing aid in final diagnosis. (2) PCR and DNA molecular biology techniques are important for the early diagnosis of MDR-TB otitis media. (3) Early effective anti-tuberculosis treatment is the guarantee for further recovery for patients with MDR-TB otitis media. However, we also noticed that the disease is only a case; questions such as the incidence rate, transmission routes, pathogenesis of MDR-TB otitis media, and whether surgery should be performed have yet to be further confirmed.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
We would like to thank the technical support provided by Laboratory Department and Respiratory and critical medicine Department of Wuhan Pulmonary Hospital.
Authors’ contributions
CTZ and DRH participated in the conceptualization, design, investigation process, project administration, supervision, formal analysis, validation, and critical revision of the manuscript. CTZ, LXP, YCQ, MCL and OJL participated in the investigation process, data curation, formal analysis, validation and visualization of the work, and writing the original draft. CTZ and DRH participated in the conceptualization and critical revision of the manuscript. All authors read and approved the final manuscript.
Funding
No funding supports this study.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Ethics approval and consent to participate
As a case report, our paper did not require any referral to our institutional clinical ethics committee.
Consent for publication
Written consent for publication of this case report and accompanying images were obtained from the patient.
References
- 1.Corbett E.L., Watt C.J., Walker N., Maher D., Williams B.G., Raviglione M.C., et al. The growing burden of tuberculosis: global trends and interactions with the HIV epidemic. Arch Intern Med. 2003;163(9):1009. doi: 10.1001/archinte.163.9.1009. [DOI] [PubMed] [Google Scholar]
- 2.Fauci AS, Braunwald E, DL K. Harrison's principles of internal medicine. New York: McGraw-Hill; 2005.
- 3.Wallner L.J. Tuberculous otitis media. Laryngoscope. 1953;63:19. doi: 10.1288/00005537-195311000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Vaamonde P., Castro C., Garcia Soto N., Labella T. Tuberculosis otitis media: a signifcant diagnostic challenge. Head Neck Surg. 2004;130:6. doi: 10.1016/j.otohns.2003.12.021. [DOI] [PubMed] [Google Scholar]
- 5.Awan M.S., Salahuddin I. Tuberculous otitis media: two case reports and literature review. Ear Nose Throat J. 2002;81(11):792–794. [PubMed] [Google Scholar]
- 6.Sens P.M., Almeida C.I., Valle L.O., Costa L.H., Angeli M.L. Tuberculosis of the ear, a professional disease? Braz J Otorhinolaryngol. 2008;74(4):621–627. doi: 10.1016/S1808-8694(15)30614-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.S N, M I, K D. Tuberculous otitis media: clinical aspects of 12 cases. Ann Otol Rhinol Laryngol 2003; 12: 4. [DOI] [PubMed]
- 8.Hoca N.T., Ogretensory M. Tuberculous otitis media-a case report. Turkish Res J. 2008;9:3. [Google Scholar]
- 9.Verma R. Tuberculous otomastoiditis: A therapeutic and diagnostic challenge. Indian J Otol. 2017;23(4):260. [Google Scholar]
- 10.Cho Y-S, Lee H-S, Kim S-W, et al. Tuberculous Otitis Media: A Clinical and Radiologic Analysis of 52 Patients. The Laryngoscope 2006: 921-7. [DOI] [PubMed]
- 11.Cousins D.V., Wilton S.D., Francis B.R., Gow B.L. Use of polymerase chain reaction for rapid diagnosis of tuberculosis. J Clin Microbiol. 1992;30(1):255–258. doi: 10.1128/jcm.30.1.255-258.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kahane J., Benjamin T. Tuberculous otitis media. Otol Neurotol. 2009;30:2. doi: 10.1097/MAO.0b013e31818af3c1. [DOI] [PubMed] [Google Scholar]
- 13.Hand J.M., Pankey G.A., Schlossberg D. Tuberculous otomastoiditis. Microbiol Spectr. 2016;4(6) doi: 10.1128/microbiolspec.TNMI7-0020-2016. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization. Companion handbook to the WHO guidelines for the programmatic management of drug-resistant tuberculosis. WHO/HTM/TB/2014.11.Geneva:World Health Organization, 2014. [PubMed]
- 15.World Health Organization . World Health Organization; Geneva: 2018. WHO treatment guidelines for Multidrug and rifampicin-resistant tuberculosis 2018 update Pre-final text. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.