Figure 6.
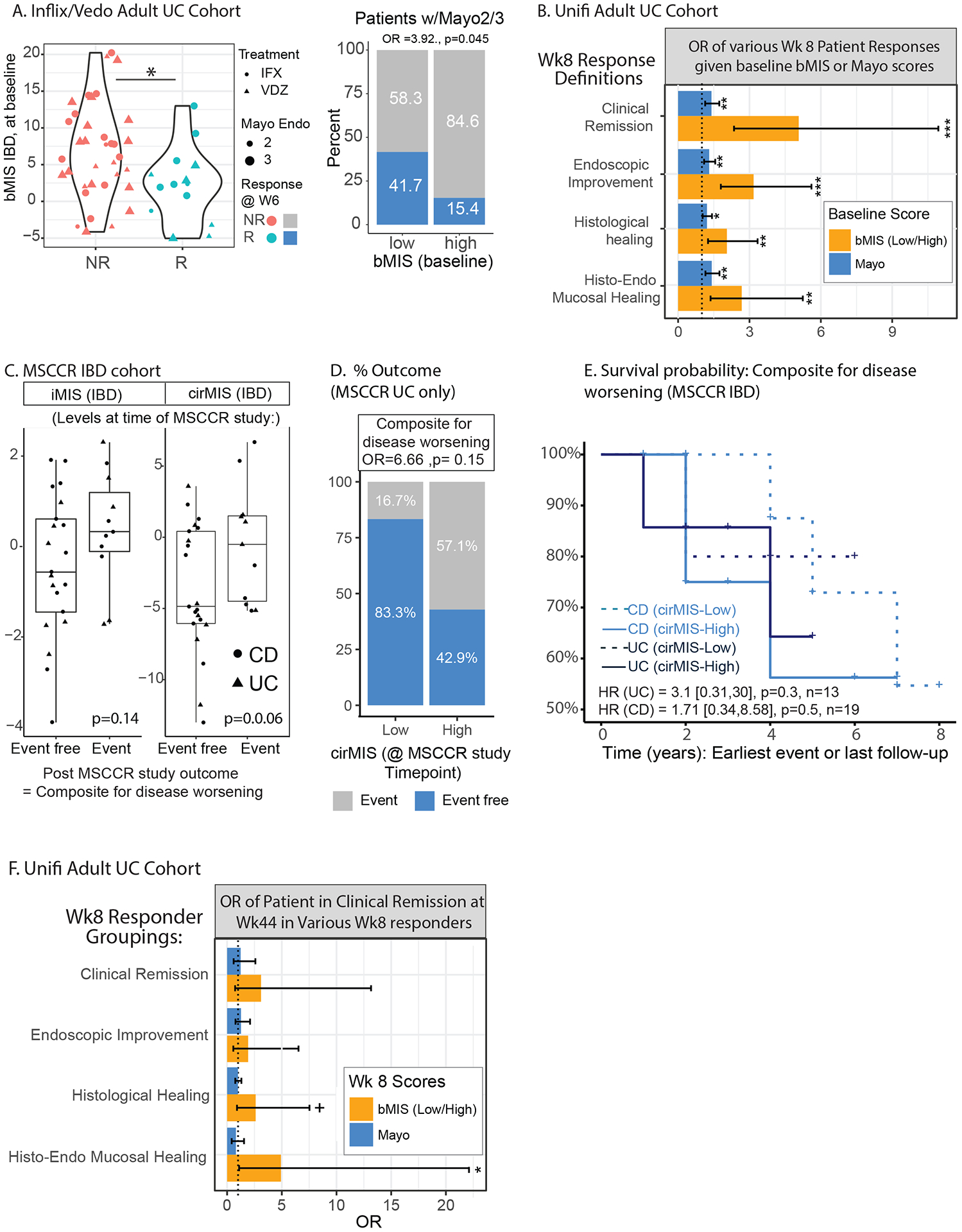
Residual molecular inflammation and clinical outcomes. A. Baseline bMIS_IBD levels in patients from the GEMINI-I/LTS UC and anti-TNF treated patients according to response to therapy (endoscopic mucosal healing (Mayo endoscopic score 0–1) as assessed for VDZ at W6 and for IFX at W4–6) (left panel). The proportion of patients that were considered responders to therapy in the baseline high vs low bMIS group (right panel). B. UNIFI adult UC cohort and the odd’s ratio of having a response, according to various definitions from clinical remission, endoscopic improvement, histological healing and combined histo-endoscopic mucosal healing (see methods) at week 8 of therapy (UST) in baseline high vs low cirMIS group’s (based on median levels) or according to baseline Total Mayo score. An additive model was used. C. A subset of MSCCR patients were identified that were in endoscopic and histological remission at the time of the MSCCR study (called MSCCR endo-histo-remission) see methods). These patients were then categorized as having high or low cirMIS levels based on the tertiles of expression and their post-MSCCR outcomes considered as a composite score to reflect disease worsening were reviewed in their charts. The levels of bMIS_IBD and cirMIS_IBD of the MSCCR endo-histo-remission patient subsets were generally higher in those patients that subsequently had a disease worsening event post-MSCCR study. For the composite score of events reflecting disease worsening, 1 of 6 MSCCR UC patients with low cirMIS had an event while 4 out of 7 patients with a high cirMIS had an event (D). For the CD MSCCR endo-histo-remission patients, the proportion of patients that were event free was the same between high and low cirMIS levels (SF3B). However, Kaplan-Maier survival curves (E) show that patients with higher cirMIS levels, were more likely to have a disease worsening event recorded earlier than compared to the low cirMIS group (in either UC or CD subsets). Specifically, the Cox models reported that for UC patients, the hazard ratio is 3.1 times higher [0.31,30, p=0.3] than the low cirMIS group, and in CD patients, the hazard ratio was 1.71 (0.34,8.58, p=0.5] times higher than the low cirMIS group. (G). UNIFI adult UC cohort and the odd’s ratio of being in response at week 44 (outcome = clinical remission) in patients considered responders at week 8 according to various definitions from clinical remission (n=33), endoscopic improvement (44), histological healing (65) and HEMH (34) (see methods), based on their baseline high vs low cirMIS status, versus their week 8 Total Mayo score. An additive model was used. +: p<0.1; *: p < 0.05; **: p < 0.01; ***: p < 0.001.
