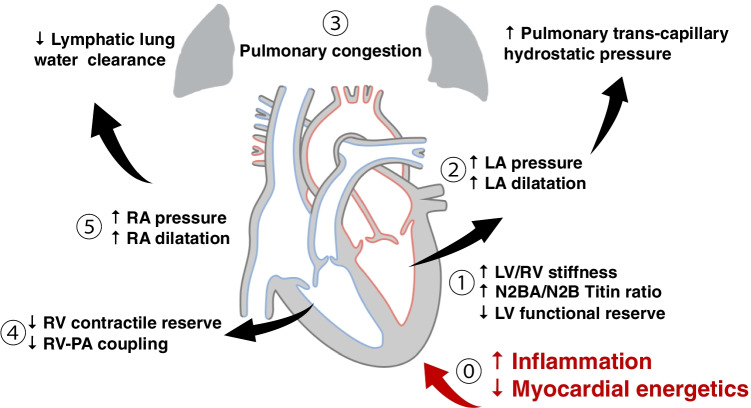
Fig. 3.
A very brief schematic overview of the currently understood pathogenesis of HFpEF. It is important to remember that the HFpEF syndrome is a biventricular process and that the contributions of the right heart are equally important. (1) Increased left ventricular stiffness, and a decreased functional reserve, results in (2) increased left-sided filling pressures with left atrial dilatation and increased left atrial pressure. This leads to increased pulmonary transcapillary hydrostatic pressure, which drives fluid transudation, potentially increasing capillary diameter from the Young-Laplace relation, and resulting in pulmonary congestion (3). Similar maladaptive right heart processes may also occur in parallel. (4) Reduced right ventricular contractile reserve, and reduced coupling of the right ventricle to the pulmonary circulation or RV-PA coupling, results in increased right-sided pressures, with right atrial dilatation and increased right atrial and systemic venous pressures (5). This exacerbates pulmonary congestion by reducing clearance of lung water via pulmonary lymphatics. The underlying pathogenesis of HFpEF is still the subject of ongoing research, but pro-inflammatory changes result in a mechanical increase in the stiffness of the myocardium mediated through alterations in collagen deposition and the biophysics of titin, which occurs concomitantly with metabolic changes leading to an increased oxidative stress on the myocyte