Abstract
Cardiac aging is evident by a reduction in function which subsequently contributes to heart failure. The metabolic microenvironment has been identified as a hallmark of malignancy, but recent studies have shed light on its role in cardiovascular diseases (CVDs). Various metabolic pathways in cardiomyocytes and noncardiomyocytes determine cellular senescence in the aging heart. Metabolic alteration is a common process throughout cardiac degeneration. Importantly, the involvement of cellular senescence in cardiac injuries, including heart failure and myocardial ischemia and infarction, has been reported. However, metabolic complexity among human aging hearts hinders the development of strategies that targets metabolic susceptibility. Advances over the past decade have linked cellular senescence and function with their metabolic reprogramming pathway in cardiac aging, including autophagy, oxidative stress, epigenetic modifications, chronic inflammation, and myocyte systolic phenotype regulation. In addition, metabolic status is involved in crucial aspects of myocardial biology, from fibrosis to hypertrophy and chronic inflammation. However, further elucidation of the metabolism involvement in cardiac degeneration is still needed. Thus, deciphering the mechanisms underlying how metabolic reprogramming impacts cardiac aging is thought to contribute to the novel interventions to protect or even restore cardiac function in aging hearts. Here, we summarize emerging concepts about metabolic landscapes of cardiac aging, with specific focuses on why metabolic profile alters during cardiac degeneration and how we could utilize the current knowledge to improve the management of cardiac aging.
Subject terms: Senescence, Cardiology
Introduction
In the past few decades, improved pharmacological and surgical treatments have contributed to increased life expectancy and an aging population in certain industrialized countries.1 In addition, the proportion of the retired population is rapidly increasing; retirees are much more likely to slide into sedentary lifestyles, which further accelerates cardiac aging.2–5 The incidence of age-associated disorders, especially cardiovascular diseases (CVDs), has increased dramatically; in elderly individuals, these age-related disorders correlate with high hospitalization, increased mortality rates, as well as elevated cost.4,5 Even without disease, aging is accompanied with functional decline of multiple organs. It is characterized by unique histological and biochemical features, including oxidative stress, protein misfolding, cell death, and mitochondrial abnormalities.6,7 Similar to other group of organs, the heart function declines gradually with age, which is evident by the reduced pump function and myocardial compliance resulting from increased afterload and insufficient coronary perfusion/oxygenation.8–10 Conventional wisdom suggests that the aging heart manifests increased left ventricular mass, while considerable evidence from autopsies and magnetic resonance imaging demonstrate that cardiac mass tends to be decreased in older adults and remain the same in women in the absence of hypertension.11,12 In line with the reduced performance of other organ systems, the age-related cardiac decline dramatically accelerates after 50 years of age.10
In elderly individuals, the metabolic landscape during cellular senescence can increase the risk of cardiac function dysregulation and cardiac repair dysfunction.13 For example, the stroke volume of the aging heart is mildly increased during moderate aerobic exercise. This is partly due to the strength of the Frank-Starling mechanism (cardiac preload), in which the metabolic demand of the work rate is substantially enhanced.14,15 In addition, a recent study involving metabolic profiling of serum and urine in healthy subjects suggested that aging induces impaired catabolism in glycoproteins, amino acids, and several lipids, among which cumulative metabolites contribute to the cardiac aging process.16 Importantly, accumulated evidence from multiomics exploration has highlighted the complex alterations of metabolic status during aging. In this regard, we review and outline the recent advancements of the mechanisms and therapeutic implications of the metabolic landscape in aging hearts since this information influences the progression of the cardiac dysfunction and lifespan.
Distinct substrate metabolism during cardiac aging
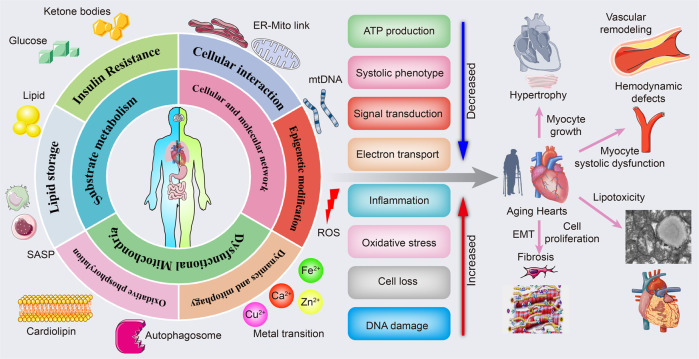
Aging hearts are accompanied by several pathological changes in metabolism (Fig. 1). Below, we outline the major alterations in metabolism and their involvement in developing cardiac aging.
Fig. 1.
The link between cardiac aging and metabolic pathology. Metabolic drivers of cardiac aging. Mitochondrial substrates metabolic disturbance including lipid storage and insulin resistance; dysfunctional mitochondria with impaired oxidative phosphorylation, mitochondria dynamics, and mitophagy; cellular and molecular network. All of which drive reduced ATP production, systolic phenotype, signal transduction, and electron transport, along with increased inflammation, oxidative stress, cell death, and DNA damage. Finally, various pathological alterations, including myocyte growth-induced cardiac hypertrophy, endothelium–mesenchymal transition and cell proliferation-mediated cardiac fibrosis, lipid deposition-induced comparative cardiac lipotoxicity, and insufficient energy-mediated myocyte systolic dysfunction and hemodynamic disorder, contribute to cardiac aging, thus the failing heart. The online resource inside this figure was quoted or modified from Servier Medical Art
Glucose metabolism
Unlike the adult heart, the aging heart experiences proportionally reduced myocardial lipid catabolism. In addition, anaerobic glycolysis, instead of glucose oxidation, gradually dominates the energy source in the aging heart,17 which is in line with pathophysiological changes such as cardiac hypertrophy and impaired contractile function.18 Furthermore, aging is associated with obesity-independent insulin resistance, and involves disrupted mitochondrial structure and dysregulated cellular insulin action.19 Notably, circulating glucose is substantially increased due to the compromised ability of glucose transporters (GLUTs) to transfer glucose during aging, thus causing elevated fasting blood insulin and glucose levels.20 Emerging evidence has shown that culturing cells under hyperglycemia or high insulin conditions accelerates cellular senescent phenotype.21,22 Consistently, age-dependent insulin resistance and glucose intolerance may result in diabetes, CVDs, and stroke and are associated with poor cardiac function during aging.23 Moreover, positron emission tomography imaging of radio-tagged glucose absorption in the aging heart demonstrated insulin resistance and damaged glucose shuttling, as well as the proportional reduction in FA oxidation and lipid accumulation.24,25 In energy provision, glycolysis is unlikely to compensate for impaired glucose oxidation and FA utilization, similar to cardiac ischemia-induced heart failure. Hence, anaerobic glycolysis synergizes with reduced FA utilization, resulting in an irreversible and persistent energy deficit and aberrant cardiac contraction. In addition, the enhanced pentose phosphate pathway impedes glucose utilization in the aging heart.26 Simultaneously, activation of the pentose phosphate pathway may also induce impaired FA oxidation and higher lipofuscin accumulation in cardiomyocytes, leading to cardio-lipotoxicity.27 However, the mechanism behind this remains unclear. Accordingly, the carboxylation of pyruvate to malate without acetyl-CoA production might partly account for the increased glycolytic flux.28,29 The latter is also known as an anaplerotic reaction and partly counteracts impaired pyruvate oxidation even though less energy is produced than that with the unabridged Krebs cycle in mitochondria.30 It seems that anaplerotic reactions partly compensate for insufficient fueling and prevent accumulation of pyruvate in the heart.
Cardiac aging molecular mechanisms are sophisticated, making it impossible to utilize unifying model in deciphering the hyperglycemia-associated cell senescence. Reduction in growth hormone (GH) and insulin-like growth factor (IGF) and increased insulin responsiveness correlate with the prolonged life and an apparent reduction in the aging process.31–33 IGFs, insulin receptors (INSR), and insulin receptor substrate-1 (IRS-1) could regulate insulin resistance as well as contribute to metabolic syndrome (Fig. 5). With regard to cardiac aging, the interaction of insulin-like growth factor-1 (IGF-1) with IGF-1 receptor (IGF-1R) accelerates myocardial pathologies in cardiac aging and longevity in mammals.34 Consistently, forced cardiac expression of the IGF receptor in Drosophila promotes cardiac aging.35 Cardiomyocyte-specific absence of IGF-1R impedes the initiation of senescence-related myocardiopathy. Contradictorily, some studies revealed that endogenous IGF-IR pathway diminishes the age-correlated diastolic dysfunction.36,37 In IGF-1 overexpressing mice, dysregulated diastolic and contractile activity of aging hearts was improved, and cardiac aging was delayed by preservation of cardiac SERCA expression and activity.38,39 Conversely, another study revealed that pharmacological targeting of cardiac IGF-1 pathway could provide a undiscovered strategy for cardiac health and lifespan extension.40 These results emphasize the regulatory function of IGF-1/IGF-1 receptor during aging progression, leading to a difficult discrimination between the cardiac and systemic consequences of IGF-1. To solve this puzzle, plasma IGF-1 deficiency41,42 and controlled inhibition of IGF-1R in cardiomyocytes37 were subsequently investigated; the beneficial effects of forced expression of IGF-1 in heart tissues may be delineated by elevated blood IGF-1 concentration, and IGF-1 promoted the function restoration of the ischemic heart.43 Hence, cardiac and systemic IGF-1 had distinct effects on cardiac aging.
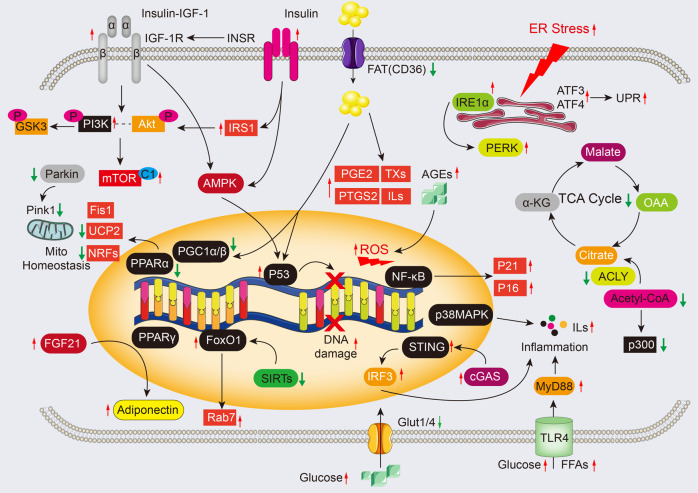
Fig. 5.
Molecular mechanisms and potential signaling for cardiac aging. The insulin/IGF-1 signaling pathway can activate signal transduction through the PI3K/Akt pathway, which in turn phosphorylates multiple targets, regulating the activity of the mTOR complex (mTORC1). IGF-1 also contributes to protein synthesis by activating the PI3K/Akt/mTOR and PI3K/Akt/GSK3β pathways, which can lead to endoplasmic reticulum (ER) stress or protein degradation via the ubiquitin-proteasome system (UPS). In the presence of ER stress, activated IRE1α and PERK can initiate proinflammatory and proapoptotic signaling pathways. Increased NAD+ might contribute to SASP and aging by disturbing AMPK and p53 activation, as well as enhancing p38MAPK and NF-kB activity in senescent cells. During cardiac aging, the maintenance of mitochondrial homeostasis is impaired, which can result in the release of mtDNA and the activation of the cGAS/STING/IRF3 pathway, leading to the production of inflammatory cytokines. The PINK1-Parkin pathway plays a crucial role in maintaining mitochondrial function and dynamics through mitophagy. In addition, ROS can activate the MAPK and PI3K/Akt signaling pathways, as well as increase levels of p53 and p21, which can promote apoptosis and inflammation in chondrocytes. The TLR4-MyD88 pathway can also be activated by circulating FFAs and glucose, leading to the production of proinflammatory factors. The online resource inside this figure was quoted or modified from Servier Medical Art
As the top two abundant glucose transporters in the heart, glucose transporter-1 (GLUT1) localizes in the sarcolemma and regulates cardiac glucose shuttling at basal state, which is dominant in resting cardiomyocytes;44 however, glucose transporter-4 (GLUT4), the primary variant making up about 70% of all glucose transporters, localizes in a particular cellular compartment and shuttles into the plasma membrane upon cardiomyocyte contraction and insulin insult.44 Of note, GLUT4 (also known as SLC2A4) can be impaired during aging, reducing glucose uptake and utilization in cardiomyocytes45 (Fig. 2). Substantial studies have suggested that advanced glucose end products (AGEs) also correlate with cardiomyopathy, especially in the heart of older individuals with diabetes.46–48 AGEs accumulate in the myocardial interstitium, resulting in excessive cross-linking of ECM proteins, which leads to cardiac muscle rigidity and diastolic dysfunction.49–51 Furthermore, AGEs specifically interact with the receptor for advanced glycation end products (RAGE) to activate NF-κB nuclear translocation, which stimulates excessive ROS production and increases the expression of p21 or p16 in the myocardium.52–55 However, how circular AGEs are taken up by cardiomyocytes and removed from cardiomyocytes is poorly understood. More importantly, despite the effectiveness of the short-term intervention targeting of the AGE-RAGE axis,53 chronic AGE inhibition was not considered. More research is therefore needed to fully elucidate circular AGE transportation and the AGEs in people with aging hearts.
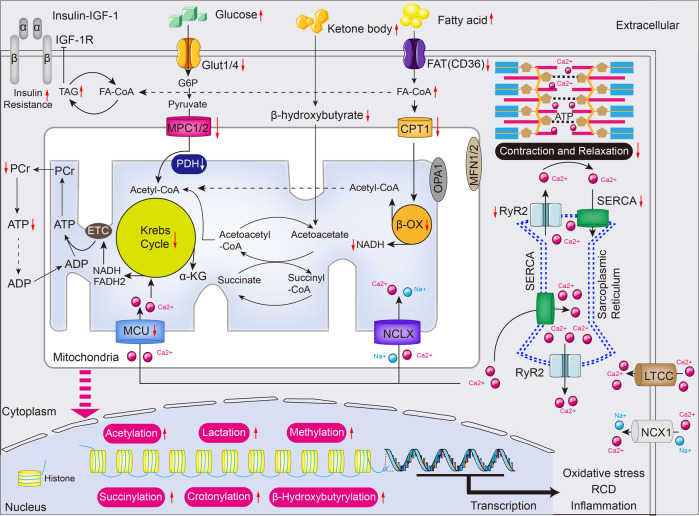
Fig. 2.
Metabolic substates utilization and excitation-contraction coupling in the aged heart. In the aging heart, myocardial lipids catabolism and glucose oxidation are reduced due to insulin resistance, but glycolysis dominates the energy source. Also, the relative contribution of ketone body utilization to ATP production is enhanced. The mismatch between FA oxidation and uptake results in the accumulation of toxic lipid intermediates, leading to impairment of ATP production and formation of high-energy phosphates. Furthermore, several metabolic intermediates interfere with metabolism and course oxidative stress, RCD, and inflammation by post-translational modifications and serving as chromatin-modifying enzymes in cardiac aging. Krebs cycle and excitation-contraction coupling are stimulated by Ca2+ that mainly sources from sarcoplasmic reticulum (SR), while the transport of Ca2+ is disturbed in the aging heart. Red arrows indicate alterations that occur in the aging heart (see text for details). α-KG α-ketoglutarate, ADP adenosine diphosphate, ATP adenosine triphosphate, β-OX fatty acid β-oxidation, CPT1 carnitine O-palmitoyltransferase 1, ETC electron transport chain, FADH2 reduced flavin adenine dinucleotide, FAT fatty acid translocase (also known as CD36), FA-CoA fatty acyl-CoA ester, Glut4 glucose transporter 4 (also known as SLC2A4), G6P glucose-6-phosphate, IGF-1 Insulin-like growth factor 1, LTCC L-type Ca2+ channel, MFN1/2 Mitofusin1/2, MPC1/2 mitochondrial pyruvate carrier1/2, MCU mitochondrial Ca2+ uniporter protein, NADH nicotinamide adenine dinucleotide, NCLX mitochondrial Na+/Ca2+ exchanger protein, NCX1 Na+/Ca2+ exchanger 1, OPA1 dynamin-like guanosine triphosphatase, PCr phosphocreatine, PDH Pyruvate dehydrogenase, RCD regulated cell death, RYR2 ryanodine receptor 2, SERCA sarcoplasmic/endoplasmic reticulum Ca2+ ATPase, TAG triacylglycerol. The online resource inside this figure was quoted or modified from Servier Medical Art
Besides cardiomyocytes, crosstalking between cardiac fibroblasts and cardiomyocytes inhibits glucose metabolism enzyme activity and lactate transporter expression, possibly due to the fibroblast growth factor 21 (FGF21)-adiponectin pathway during aging-related heart failure.56,57 More importantly, defective glucose metabolism in the aging heart is correlated with immune activation in noncardiomyocytes. Notably, elevated insulin promotes T-cell activation during aging, with a subsequent increase in insulin receptor and glycolytic enzymes, both of which are required for adaptive immunity.58,59 In brief, upregulation of the insulin receptor contributes to polyclonal activation of CD4+ and CD8+ T lymphocytes and, subsequently, numerous secretory proinflammatory cytokines, including IFN-γ, TNF, and IL-17.58 Importantly, increased insulin concentrations also impede regulatory T cells (Tregs) in antagonizing inflammation, which serves as the trigger of cardiac aging.60 These data suggest that the T-cell-mediated immune response might be an important trigger for local inflammation in cardiac aging. A prior publication revealed that restored metabolism profiling in myeloid cells counteracts cognitive impairment in the aging central nervous system (CNS), in which aged brain tissues are susceptible to inflammation induced by aging macrophages and microglia.61 Likewise, chronic inflammation in the aging heart is triggered largely by myeloid-derived macrophages, whereas how hyperglycemia impacts cardiac macrophages during aging is not known. Numerous studies have also demonstrated that hyperglycemia stimulates cellular senescence in endothelial cells partly due to reduced arginase 1 (ARG1) expression and nitric oxide synthesis (NOS),62,63 a crucial product for vessel growth and angiogenesis. In addition, elevation of glucose concentrations induced senescence in cardiac fibroblasts (CFs) by promoting telomere shortening,64 which may be caused by the senescence-associated secretory phenotype (SASP)65 of other cell types due to the hyposensitivity of isolated CFs in response to hyperglycemia. Therefore, the involvement of glucose in regulating senescence of various types of cells should be further determined.
Lipid metabolism in the aging heart
Dyslipidemia, including high cholesterol, hypertriglyceridemia, and elevated low-density lipoproteins (LDLs), triggers thrombosis and increases the risk of CVDs.66 Inside the aging heart, dysregulated cardiac function is linked with reduced oxidation of FA. This is indicated by the accumulation of free fatty acids (FFAs) and lipid-laden cells in heart tissues,30,67 consistent with pathological cardiac hypertrophy.18 In contrast, FA delivery into cardiomyocytes is promoted in individuals with advanced aging conditions. Therefore, the imbalance between FA uptake and utilization leads to excess in the intracellular lipids, triggering toxic lipid species (including ceramide and diacylglycerol) and eventually lipotoxicity during cardiac aging.68 Besides aging directly impeding FA oxidation, increased insulin contributes to the inactivation of FA oxidation by restricting the activity of major rate-limiting enzymes in cardiomyocytes.69 Worse of all, the intracellular accumulation of lipids further causes posttranslational modifications of several components that regulate insulin production. Consequently, insulin resistance is accelerated, and cellular senescence is further promoted.70,71 These lines of evidence indicate that abnormal cardiac lipid metabolism promotes cardiac aging (Fig. 2). The mismatch between lipid uptake and oxidation drives cardio-lipotoxicity and partly accounts for insulin resistance during aging.
Increased cardiac CD36 supports FA transport during aging and sustains enhanced cardiac lipid content.72 Accordingly, aged CD36-depleted mice showed reduced lipid accumulation in heart tissues, and improved ATP production and cardiac dysfunction.73 Conversely, a high-fat diet (HFD) and CD36 overexpression promote FA uptake and higher cardiac lipid content during aging.74 Moreover, peroxisome proliferator-activated receptor-α (PPAR-α) signaling and peroxisome proliferator-activated receptor-γ coactivators (PGC1s) are overtly suppressed in aging-induced cardiac dysfunction,75,76 while aging promotes PPAR-gamma activation,77 all of which dysregulate FA mitochondria shuttling and downregulates its oxidative enzymes in cardiomyocytes.78 In addition, ceramide, a lipid metabolite, has been reported to promote senescence by inducing a reduction in cardiolipin content and mitochondria dysfunction in cardiomyocytes.79 Recently, it has been suggested that enhanced ceramide catabolism restrains cardiac lipotoxicity in type 2 diabetic mice,80 which further supports the adverse cardiac influence of ceramide, but the molecular machinery is less understood. Additional studies indicate that the release of proinflammatory factors of the SASP, sourced from lipid metabolites, was dramatically increased in the aging heart, whereas monounsaturated fatty acids (MUFAs), functioning as a lipid-lowering metabolite, were substantially reduced.81 Moreover, accumulating evidence suggests that exogenous lipids accumulate and are incorporated into triacyclglycerols to form numerous lipid droplets in the aging heart.82 In line with glucose metabolism, lipid metabolism was also verified to modulate T-cell activity in cardiac aging.83 It has been confirmed that macrophage FA oxidation can suppress atherosclerosis,84 but the impacts of macrophage lipid metabolism on cardiac aging are not fully explained. In addition to lipid droplets, fatty acids are also converted to oxylipins, among which increases in proinflammatory prostaglandin E2 (PGE2),85 prostaglandin synthase 2 (PTGS2 or COX-2),86,87 thromboxanes (TXs),88 and leukotrienes (LTs)89 and decreases in anti-inflammatory lipoxin A4,90 resolvins,91 protectins, and maresins are associated with cellular senescence.92 Moreover, the enhancement of cytokines sourced from lipid metabolism recruits and promotes cardiac fibroblast proliferation, thereby inducing wall stiffness and diastolic dysfunction in the aging heart. These data suggest crucial impacts of inflammation and lipid metabolism on cardiac aging, and various aspects regarding lipid metabolism remain mysterious in the context of cardiac aging.
Ketone bodies: a compensatory fuel
Ketone bodies, comprising beta-hydroxybutyrate, acetoacetate, and acetone,93 are derived from FA oxidation and serve as primary body energy sources during fasting and ketogenic diet (KD) in physiological homeostasis.94 In previous studies, ketone body oxidation-related enzymes and intermediates derived from its metabolism were increased in both preclinical models and heart failure patients,95,96 implying that ketone bodies serve as a critical optional energy in heart failure97 (Fig. 2). Given the impaired FA oxidation and glucose utilization in aging, ketone bodies could be an essential substrate that alleviates aging-related cardiac dysfunction and serves as a compensatory fuel. Expectedly, similar to the aging brain that metabolizes 3-beta-hydroxybutyrate (3HB) and acetoacetate (AcAc) ketone bodies,98 increased ketone body flux indeed improves cardiac dysfunction in the aging heart,99 by which the heart compensates for contractile function and manifests cardiac hypertrophy with aging. Besides being the source of energy, it metabolites β-hydroxybutyrate, a histone deacetylases antagonist, induces cell proliferation and inhibits inflammation;100 thus, β-hydroxybutyrate may serve as a blocker of aging-related inflammation. Hence, the ketogenic diet is beneficial for aging-related cardiovascular complications.
The high level of ketone body flux during cardiac aging is necessary to support energy metabolism and increase cardiac metabolic efficiency. In some way, beta-hydroxybutyrate catabolism provides higher ATP production [2.55 vs. 2.33 in ATP production: oxygen consumption ratio (P:O)] than FA palmitate.101 Beta-hydroxybutyrate is regarded as an adjunctive nutritional therapy for aging.102 As a mitochondrial enzyme responsible for the liver-independent ketone body metabolism, cardiac succinyl-CoA-3-oxoacid CoA transferase (SCOT) presents substantially increased activity in aged animals.103 In mice, the absence of SCOT increased vulnerability to ketosis and reduced plasma levels of glucose and lactate.104 In addition, several studies demonstrated the metabolic effects of ketone bodies, which exert antioxidant effects by promoting the proportion of reduced and oxidized glutathione, thus directly counteracting oxidative stress and removing oxygen radicals.105,106 Moreover, increased ketone body flux benefits mitochondrial restoration by causing impaired mitochondria removal through Parkin-mediated mitophagy during cardiac aging.107 Although ketone body flux induces impaired mitochondria removal, the crosstalk between mitophagy and FA oxidation remains exclusive in the context of cardiac aging. Ketogenic diet is reported to decrease midlife mortality and improve memory; simultaneously, the cyclic KD maintained a cardiac phenotype that resemble to young mice in aging mice.108,109 Moreover, a KD inhibited longevity-associated signaling of insulin and mTOR pathway. Notably, it triggered PPAR alpha, a leading factor that governs the transcription of genes for ketogenesis and mitochondrial homeostasis108,109 (Fig. 5). Notably, this study focused only on the short-term impacts of KD, whereas its long-term influences on age-related cardiomyopathy are poorly understood. Moreover, the link between diabetes mellitus (DM) and aging is involved in ketogenesis, which has attracted more attention,110,111 and enhanced cardiac aging in the context of DM makes it intriguing research. In addition, the effects of ketone bodies on cardiac fibroblasts, endothelial cells, and immune cells are not known.
Acetyl-CoA and epigenetic intermediates
Acetyl-coenzyme A (acetyl-CoA) is a crucial cofactor in regulating metabolism. Being the end metabolite of FA oxidation and glycolysis, acetyl-CoA fuels the Krebs cycle and synthesizes ketone bodies. In addition, fluctuations in acetyl-CoA concentration are reported to be involved in alterations in histone modification that loosen or promote their interaction with DNA, therefore regulating gene expression.18,112 Both ATP-citrate lyase (ACLY) and acetyl-CoA synthetase 2 (ACSS2) are responsible for acetyl-CoA synthesis.113,114 The incapability of ACLY results in the reduced nuclear production of citrate-mediated acetyl-CoA, which simultaneously suppresses the acetyl-transferase activity of p300 and results in increased autophagy, which prevents aging outcomes.115 Moreover, shuttling of the pyruvate dehydrogenase complex (PDC) from mitochondria to the nucleus triggers the production of nuclear acetyl-CoA for histone modification and epigenetic regulation,116 which may serve as a trigger for aging progression. In addition, acyl-coenzyme A (CoA)-binding protein (ACBP), or diazepam-binding inhibitor (DBI), which reduces cardiac fibrosis, is a regulatory factor for autophagy,117 supporting the contention that ACBP induces cardioprotection, probably in cardiac aging. In addition, cytoplasmic ACSS2 hinders autophagy from causing aging, inducing AMPK-mediated ACSS2 nuclear translocation, which functions more drastically than cytoplasmic ACSS2 in aging outcomes. Specifically, nuclear ACSS2 accumulation upregulated the transcriptional capacity of HATs, including CREB-binding protein (CBP) and p300/CBP-associated factor (PCAF),118,119 which serve as enhancer elements to stimulate the transcription of cardioprotective genes and facilitate lysosomal biogenesis and autophagy during cardiac aging.112 The distinct location of ACSS2 results in opposite aging outcomes, implying the functional diversity of acetyl-CoA in control of cardiac aging. Consistent with acetyl-CoA, acetate is also regarded as the substrate of ACSS2 to revert the aging phenotype in cultured stem cells.120 Hence, acetyl-CoA governs metabolic hemostasis by operating concurrently as a metabolic product and a secondary messenger during cardiac aging. Several forms of modifications, including methylation, lysine beta-hydroxybutyrylation (Kbhb), and succinylation (Fig. 2), have been found to be involved in CVDs.121 Nevertheless, the impacts of histone modification on cardiac aging and longevity remain to be fully studied. Most recently, other metabolites and associated posttranslational modifications (PTMs), such as malonylation,122,123 lactylation,124,125 crotonylation,126 and glutarylation,127 have been verified in cardiac metabolism. Therefore, studies with emphasis on the influence of metabolite-related modifications on controlling autophagy and transcription, which are important drivers of organismal aging, are needed.
Energy fuel, Ca2+, and myocyte systolic phenotype
In cardiac muscle, excitation-contraction coupling (ECC) directly connects membrane depolarization with contraction, and most energy obtained from OXPHOS in mitochondria is burned off to fuel the incessant myocyte systolic phenotype.128. Cardiac ECC requires enormous amount of cellular energy; the primary energy users are myosin ATPase, the ion exchanger ATPase, and SERCA.129 Of note, energy consumption and Ca2+ transporting rates are associated with post-translational modifications. As an example, both the phosphorylation of SERCA130 and RyR2,131 and the deacetylation of SERCA,132 enhance Ca2+ transporting rate and cardiac contractility. The heart is enriched with metabolic components that serve OXPHOS in mitochondria to fulfill its energy requirements. However, distinguished alterations, i.e., some components are decreased (Cav1.2, Cav1.3, HCN4, and RYR2), while others (NCX and SERCA densities and proteins) are increased in the aging rat heart.133 In addition, ROS-induced SERCA oxidation at Cys674 results in SERCA inactivation and myocyte relaxation impairment in the senescent heart.134 Although the link between Ca2+ and myocyte systolic phenotype has been verified, connections between impaired metabolism, calcium homeostasis, and myocyte systolic phenotype during cardiac aging are poorly understood.
Mitochondrial impairment during cardiac aging
Mitochondrial morphology
As a factory with high energy demands, the heart is very rich in mitochondria, which generate approximately 90% of ATP to maintain pump function in the heart. Depending on the location, cardiac mitochondria are classified into subsarcolemmal mitochondria (SSM) and interfibrillar mitochondria (IFM) that have different activities.135 Specifically, defective IFM results in cardiac aging, and the decrement of IFM is associated with aging-related cardiac dysfunction,136 while that of SSM is unchanged during aging. These data hint a crucial role of IFM in cardiac aging progression. Using transmission electron microscopy (TEM), mitochondrial morphology was evaluated on cardiomyocytes obtained from aging rats. The heart muscle section area analysis revealed that the inner mitochondrial membrane (IMM) per unit volume of mitochondria was dramatically reduced in aging.137 However, in prior studies, no age-related alterations in cristae morphology were observed in heart tissues of aging rats by TEM.138,139 Moreover, impaired IFM renewal and decreased elimination of IFM led to the accumulation of abnormal IFM bearing elevated ROS amount in monocytes, all of which accelerated oxidative stress and the aging phenotype.140,141 In some ways, the species gap of rats and slightly different fixation may have contributed to this distinctive outcome. In addition, several clinical and preclinical studies reported that the aging heart possesses swelling mitochondria characterized by broken inner membrane cristae.135,142 Together, aging impairs mitochondrial integrity with defective IFM in the heart, which may be the earliest alteration in morphology prior to cardiac hypertrophy and fibrosis.
Cardiolipin, a major diphosphatidylglycerol lipid of the IMM,143 is also essential for mitochondrial function. Cardiolipin levels decline substantially in cardiac aging,144 and aging results in decreased membrane fluidity in the inner membrane, which further regulates electron transport. Moreover, aging drives ROS enrichment in cardiolipin, and cardiolipin oxidation by cytochrome c results in age-enhanced oxidative damage to mitochondria.145 Beyond that, cardiolipin may serve as the susceptor to perceive senescence stress and induce signal transduction in mitochondria, while whether cardiolipin participates in lipid metabolism inside mitochondria and the potential mechanism remains unclear. In the future, mitochondrial morphometric analysis during cardiac aging should be conducted in more species, particularly primates.
Mitochondria undergo the processes of biogenesis, dynamics (fusion/fission), and mitophagy. These events not only are crucial for its function but also likely play a role during aging.146 Biogenesis of mitochondria is an elaborated process to regenerate mitochondria from existing ones.147 In addition, mitochondrial biogenesis is affected by aging, and PGC-1α is reported to govern this event and serves as an attractive therapeutic target.148 Specifically, PGC1 stimulates the expression of uncoupling protein 2 (UCP-2) and the nuclear respiratory factors (NRFs), both of which contribute to mitochondrial DNA replication/transcription.148 However, the link between the phenotypes observed with PGC1 enrichment in the nucleus and increased deoxyribonucleoside triphosphate (dNTP) synthesis is unclear. Compared to the neonatal heart, PGC-1α activation in aging cardiomyocytes leads to lower mitochondrial biogenesis, causing reduced specific proliferation within the myocytes.149 In contrast, PGC-1α impedes the senescent phenotype in vascular smooth muscle cells (VSMCs) by restoring mitochondrial biogenesis and p62-mediated mitophagy.150 Of note, reduced length of telomere and mitochondrial defection are common initiators of aging,151 in which PGC-1α/β establishes the connection.152–154 Overexpression of PGC-1α is reported to restore muscle aging by disturbing p53-induced DNA damage and telomere dysfunction.155 Consistently, an emerging study indicated that telomere shortening antagonized PGC-1β-mediated mitochondrial biogenesis and ROS production to induce the aging process.156 Therefore, abnormal PGC-1α/β expression is also involved in the link between reduced length of telomere and mitochondrial defectiveness. However, decreased length of telomere is associated with mitochondrial function and metabolism during early aging via uncertain mechanisms. In addition to PGC-1α, multiple regulators, such as sirtuin, AMPK,157 Nrf2158, and lncRNAs,159 have been suggested to control mitochondrial biogenesis during aging. However, how they impact cardiac aging deserves further investigation.
The aging heart also presents abnormal mitochondrial dynamics with aberrant mitochondrial fission and fusion to regulate cardiac energetic homeostasis under oxidation; both are suggested to mediate the aging process.160 Substantial studies indicate that the promotion of fission or blockade of fusion of mitochondria impedes cellular senescence.161,162 This notion is supported by animal models or isolated cells with proper regulation of mitochondrial fission protein 1 (Fis1) or mitofusin-1 content.163,164 In detail, the skeletal muscle obtained from aging mice shows higher mitofusin-1 and mitofusin-2 and reduced Fis1 content, favoring the notion that fusion supports cardioprotection against oxidation.165 Moreover, cardiac aging is characterized by insulin resistance, accompanied by FA and ROS accumulation in cardiomyocytes, which contributes to the mitochondrial fusion induced by the mismatching between protein-optic-atrophy 1 (OPA1) and dynamin-1-like protein (DRP1).166 OPA1 enables precise control in mitochondrial fusion, mitochondrial DNA preservation, energy exchange, and cristae integrity (Fig. 3a). Conversely, DRP1 serves as a pro-fission protein and controls mitochondrial shape (Fig. 3b).167 As expected, the equation of fission and fusion preserves mitochondrial dynamics and respiration to oppose cellular pathology, such as senescence. Of note, mitochondrial dynamics proteins also serve as the link between ER and mitochondria,168 and the crosstalk of both in cardiac aging requires further exploration. Generally, defective mitochondria are eliminated by mitophagy to prevent oxidative stress during aging, in which there is potential for membrane depolarization to stimulate mitophagy in a Parkin-dependent manner.169 Hence, targeting mitochondrial dynamics and mitophagy (discussed blow) could serve a potential management of age-related cardiac changes.
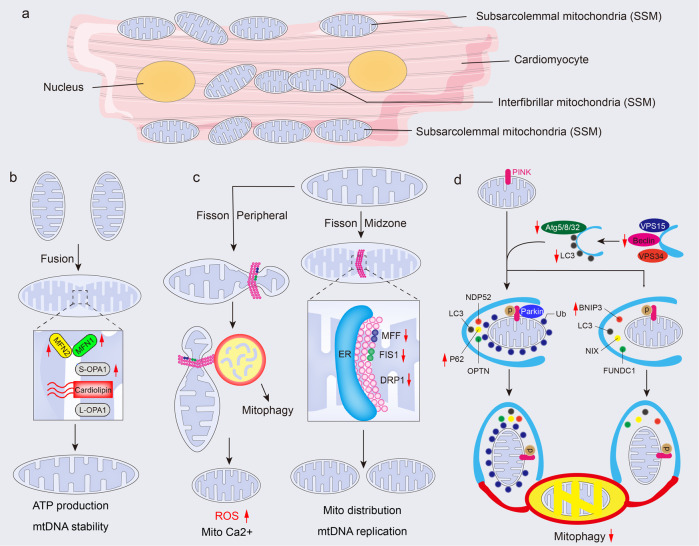
Fig. 3.
Mitochondrial dynamics and mitophagy in the aged heart. a A schematic of a cardiomyocyte to highlight the location of subsarcolemmal (SSM) and interfibrillar mitochondria (IFM). b Mitofusins (MFN1 and MFN2) in the OMM, belongs to proteins of the dynamin-related family of large GTPases, synergizing with OPA1 in the IMM to regulate mitochondria fusion. In the aging heart, long OPA1 (L-OPA1) is cleaved to generate the short form of OPA1 (S-OPA1), and the latter cooperates with cardiolipin to promote the fusion of mitochondria, by which compensates the ATP production and maintains mtDNA stability. c Fission is predominantly orchestrated by the DRP1. DRP1 binds to OMM receptors MFF and mitochondrial FIS1, promoting the midzone fission to course mitochondria distribution with mtDNA replication. Also, DRP1 induces peripheral fission and enables damaged material to be destined for mitophagy. The latter results in higher ROS generation and enhanced mitochondria Ca2+. d As a serine/threonine-protein kinase, PINK1 serves as the sensor that detects impaired mitochondria and leads to the proteolytic cleavage of PINK1 by mitochondrial proteases. Uncleaved PINK1 plays a role in activating parkin through direct phosphorylation of the parkin Ub-like (UBL) domain, as well as phosphorylation of ubiquitin. This, in turn, recruits autophagy receptors such as p62, OPTN, and NDP52, promoting the recruitment of LC3 and subsequent engulfment of damaged mitochondria by autophagosomes. Also, autophagy receptors such as BNIP3, NIX, and FUNDC1 regulate ubiquitin-independent mitophagy by recruiting LC3 and facilitating the engulfment of damaged mitochondria by autophagosomes. Red arrows indicate alterations that occur in the aging heart (see text for details). Atg autophagy-related protein, ATP adenosine triphosphate, BNIP3 bcl-2 19-kDa interacting protein 3, DRP1 dynamin-related protein 1, ER endoplasmic reticulum, FIS1 fission 1 protein, FUNDC1 FUN14 domain containing 1, IMM inner mitochondrial membrane, MFF mitochondrial fission factor, MFN mitofusin, mtDNA mitochondria DNA, NDP52 Nuclear dot protein 52 kDa, OMM outer mitochondrial membrane, OPA1 optic atrophy 1, OPTN optineurin; ROS reactive oxygen species, VPS (also known as PI3KR4) phosphoinositide 3-kinase regulatory subunit 4. The online resource inside this figure was quoted or modified from Servier Medical Art
Mitophagy: an intrinsic scavenger
Mitophagy facilitates the disposal of damaged or excess mitochondria by autophagy specifically targeted to mitochondria. It is a process that specifically targets and degrades whole mitochondria for their removal.170 In contrast, the buildup of impaired mitochondria and presence of cellular dysregulation, inducing aging and age-predisposed cardiac dysfunction,171 can result from defective mitophagy.172 Inactivation of autophagy accelerates the aging-related aggregation of misfolded proteins,173 dysfunctional mitochondria174 and subsequent ROS generation175 in cardiomyocytes, disrupting the cellular environment and promoting the aging-associated cardiac phenotype. Different autophagy-related genes differentially regulate the various stages of autophagy. It has been proposed that Atg5 transgenic mice present boosted autophagic potential in the myocardium, contributing to health benefits such as decreased cardiac fibrosis and increased lifespans when compared with aged-matched control mice.176 Consistently, Becn1F121A/F121A knock-in mice, generated by blocked interaction of Bcl-2 with Beclin1, presented enhanced autophagy and reduced cardiac hypertrophy and interstitial fibrosis.177,178 Conversely, impeding cardiac autophagy contributes to advanced aging of heart accompanied by cardiac hypertrophy and the accumulation of dysfunctional mitochondria.179 Accordingly, increasing evidence indicates that mitophagy is absent during cardiac aging, leading to oxidized and damaged lipofuscin, which serves as a producer of oxygen radicals and further aggravates mitochondrial damage in aged hearts.180 In terms of molecular metabolism, PTEN-induced putative kinase 1 (PINK1)-Parkin-mitofusin2 (Mfn2) labels dysfunctional mitochondria, and autophagosomes are recruited in an LC3-receptor-dependent manner to engulf the targeted mitochondria for removal (Fig. 3c).181 A prior study found that the ablation of Parkin in aging mice led to abnormal mitochondrial accumulation in cardiomyocytes,182 indicating the crucial role of Parkin-mediated mitophagy during cardiac aging. Interestingly, Parkin-deleted mice showed an boosted aging potential and accumulated abnormal mitochondria in the aging heart,182 while forced expression of Parkin in the heart improved mitochondrial health and slowed down aging process in the heart,183 in which the cardioprotective effects of Parkin were dependent on mitochondrial DNA.184 More importantly, long-term Parkin overexpression or high Parkin expression results in cardiac fibrosis,185 but the mechanism is unknown. Notably, emerging findings indicate that mitochondrial autophagy also occurs in a Parkin-independent manner during aging,186 but the exact mechanism behind this phenomenon remains uncertain, thus implying the complexity of mitophagy. In addition to mitochondrial triggers, several proteins have been identified as mitophagy receptors, including FUNDC1, BNIP3, NIX/BNIP3L, Bcl2L13, FKBP8, and prohibitin-2 (PHB2), in governing mitophagy.187–191 However, our knowledge to the fate of these proteins in aging heart is limited, implying the importance of future work. Sirtuins are also involved in autophagy, and they directly regulate metabolic and structural remodeling in cardiac aging. For example, Sirt1 promotes autophagosome genesis and its fusion with lysosome by stimulating FoxO1 deacetylation-dependent transcriptional activation of Rab7 in the heart.192 In addition, an age-induced reduction in NAD+ results in sirtuins suppression and lysosomal dysfunction,193 which further disrupts autophagy-lysosome formation and the accumulation of dysfunctional mitochondria. However, excessive removal of mitochondria, including robust IFM inside the myofibrils, may lead to degradation.194 Understandably, the improper removal of IFM by excessive autophagy reduces IFM content with cardiac aging.195 Multiple mechanisms are used to eliminate damaged mitochondria, including Parkin-independent macroautophagy, mitochondrial proteases,196 ubiquitin proteasome-dependent degradation,197 and mitochondria-derived vesicles.198 Most recently, mitocytosis has been uncovered as a novel way to eliminate aberrant mitochondria and monitor mitochondria quality control,199 which underscores the need for further research since our understanding of aging-related mitocytosis remains unclear. Emerging evidence from multiple studies suggests that aging accelerates mtDNA mutation, which impedes autophagy-related impaired mitochondrial degradation by activating mTOR200 and cGAS-STING signaling.201 Currently, the effects of cardiac aging on these mechanisms have yet to be formally investigated. Although emerging evidence has confirmed the link between aging and autophagy in cardiomyocytes, the effects of autophagy upon endothelial cells, fibroblasts, and macrophages has not been fully recognized. Importantly, the outcome and importance of scrapable mitochondria is almost completely far from clear, and investigation of “the waste” is a promising avenue for future exploration and will without doubt be the subject of cardiac aging studies.
Electron transport
The transfer of electrons in the electron transport chain (ETC) drives the generation of ATP within cells. It couples with the tricarboxylic acid (TCA) cycle and oxidative phosphorylation (OXPHOS) in mitochondria.202 In the electron transport chain, electrons are transferred along a redox potential gradient from NADH or FADH2 to oxygen, causing hydrogen ions to be transported from the mitochondrial matrix to the inner membrane, and multisubunit enzyme complexes, including complexes I-IV, are involved in this process203 (Fig. 4). In line with the pathological mechanisms underlying congestive heart failure (CHF), cardiac aging disrupts the mitochondrial respiratory of cardiomyocytes by interrupting enzyme function and content of ETC complexes and suppresses the organization of respirasomes (supercomplexes). The function of complex I is to oxidize NADH, resulting in the flow of electrons into coenzyme Q. As mentioned before, aging-related mitochondrial defects is characterized with reduced NAD+ content and NAD:NADH ratio, and an increased NADH content may restrain the enzyme activity of complex I.204 It is demonstrated that restored ability of NAD+ regeneration in complex I can rescue brain degenerative progression and expand the lifespan.205 This is in line with a prior study that suggested that enhanced complex I activity is predicted to not only directly prevent the defects in mitochondria in aging, but also significantly induce NAD+ accumulation in cells, thereby promoting the activation of sirtuins.206 These data strongly support that NAD+ regeneration seems to be the primary mechanism by which mitochondrial complex I acts against degeneration and aging, while the protection of complex I in cardiac aging remains elusive.
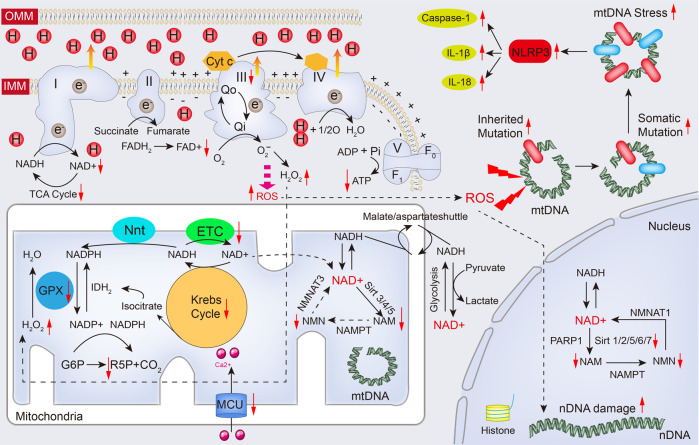
Fig. 4.
Altered NAD(H), ROS and mitochondrial DNA during cardiac aging. The electron transport chain (ETC) is a collection of four enzyme complexes (complexes I-IV) and a large protein complex (complex V) responsible for synthesizing ATP in the mitochondrial inner membrane. It generates ATP from ADP, Pi, and Mg2+ using an electrochemical gradient of protons created by the electron transport chain. As electrons pass down the redox potential gradient from NADH or FADH2 to oxygen, hydrogen ions are actively transported from the matrix to the cytosolic side of the inner membrane by complexes I, III, and IV. Complex I oxidizes NADH, which leads to sequential electron flow to coenzyme Q, complex III, cytochrome c, and ultimately to cytochrome oxidase (complex IV), where oxygen is reduced to water. However, during cardiac aging, the decline in respiration favors the relative reduction of complexes I and III, leading to increased ROS production. This increased ROS contributes to the impairment of the Krebs cycle and reduced ATP production. Furthermore, the cytoplasmic and nuclear NAD+ pools probably equilibrate by diffusion through the nuclear pore. However, the mitochondrial membrane is impermeable to both NAD+ and NADH. Reducing equivalents generated by glycolysis are transferred to the mitochondrial matrix via the malate/aspartate shuttle. In addition, different NAD+-consuming enzymes lead to the generation of nicotinamide, which is recycled via the NAD+ salvage pathway. Different forms of the NMNAT enzyme and sirtuins are localized in different compartments. Of note, a proportion of ROS is involved in reduction reaction by mitochondrial antioxidant system GPX device. While overburden of ROS leads to mtDNA mutation and damage to promote activation of NLRP3 inflammasome. Red arrows indicate alterations that occur in the aging heart (see text for details). ADP adenosine diphosphate, ATP adenosine triphosphate, Cyt c cytochrome c, FAD flavin adenine dinucleotide, FADH2 reduced flavin adenine dinucleotide, F1/Fo F1/Fo ATP synthase, G6P glucose-6-phosphate, GPX glutathione peroxidase, IL-1β interleukin-1β, IL-18 interleukin-18, IDH2 isocitrate dehydrogenase 2, IMM inner mitochondrial membrane, MCU mitochondrial Ca2+ uniporter, mtDNA mitochondria DNA, NADH nicotinamide adenine dinucleotide, NADPH reduced nicotinamide adenine dinucleotide phosphate, NAM nicotinamide, nDNA nuclear DNA, NLRP3 NOD-like receptor family pyrin domain containing 3, NMN nicotinamide mononucleotide, NMNAT1/3 nicotinamide nucleotide adenylyltransferase 1/3, Nnt mitochondrial NAD(P) transhydrogenase, OMM outer mitochondrial membrane, PARP1 poly(ADP-ribose) polymerase, Pi phosphate ion, ROS reactive oxygen species, R5P ribulose 5-phosphate, TCA cycle tricarboxylic acid cycle. The online resource inside this figure was quoted or modified from Servier Medical Art
Defects in the mitochondrial inner membrane environment occur during cardiac aging and contribute to the inactivation of cytochrome oxidase (complex IV), thus restraining the suppressed reaction of oxygen in the ETC.207 Importantly, the content and constitution of cardiolipin in IFM have been found to support the microenvironment of cytochrome oxidase, with subsequent regulation of enzyme activity.203,208 In actuality, aging downregulates the elasticity of the inner membrane and the microenvironment of mitochondria due to severe oxidative damage to membrane phospholipids.209 Similarly, OPA1 was found to bind with complex IV and enhance its activity in mitochondria, thereby contributing to increased longevity in mice.210 Unexpectedly, complex IV-associated Surf-ablating mice presented defective reaction of complex IV, improved insulin response, and boosted genesis of mitochondrial, which thus prolonged the lifespan as well;211 however, the involvement of downregulation in extending lifespan of preclinical models needs to be assessed. The contradictory results of targeting complex IV may be attributed to distinct mechanisms, and the underlying mechanism remains unclear. Notably, how targeting complex IV impacts on cardiac aging also requires more assessment. Besides altered enzyme activity, complex IV net content is reduced with aging and accompanied by enhanced cytotoxicity and endoplasmic reticulum (ER) stress activation,212 both of which trigger mitochondrial ROS production. Composed of cytochrome b/c1 and the iron-sulfur protein, complex III is vulnerable to cellular senescence and functions as the factory of ubiquinol oxidation and electron transfer.213 Similarly, aging significantly counteracts the maximal activity of complex III inside the mitochondrial inner membrane.214 In addition, mutation of the ubiquinol-binding site (Qo) of cytochrome b may result in the aging phenotype of complex III, which could be utilized as novel target for drug development.215 For example, the mutation at Y132 contributes to the decrement in complex III activity,216 and promotes aging-induced oxidative modification inside mitochondria. Along with the rapid development and application of proteomic techniques, multiple omics have uncovered the distinctive mechanism inside complex III during cardiac aging. Likewise, the activity of ATP synthase [also known as complex V] is negatively correlated with aging,217,218 resulting in a substantial decrement in the efficiency of OXPHOS. Moreover, complex V serves as a potential locus of the mitochondrial permeability transition pore (mPTP),219 while defective complex V restrains the formation of mPTP and limits the coupling of OXPHOS to the ETC. Further, Angeli et al. identified mPTP as a pathological pore that contributes to aging by activating the mitochondrial unfolded protein response (UPRmt).217 Thus, the contents and enzyme activity of complexes in the ETC might play different roles in OXPHOS and energy production. However, the mechanism behind this remains unclear, and the influences of complex V on the cardiac aging requires further investigation. Currently, potential approaches for targeting the ECT in cardiac aging remain to be determined, and more research is necessary to translate this information into practical and effective strategies.
NAD+ metabolism and sirtuin
Compared with young hearts, adult and aged hearts have much lower nicotinamide adenine dinucleotide (NAD+) levels and higher NADH levels, with therefore lowered cytosolic NAD+/NADH ratios.220 In addition, sirtuin and poly-ADP-ribose polymerase (PARP) is reduced in aged hearts. Being a critical cofactor for proteins supporting reduction-oxidation (redox) reactions, NAD+ is widely distributed in various cells and transmits electrons from one reaction to another.221 The decrease in mitochondrial function is accompanied by reduced NAD+ amount and the NAD:NADH ratio, both of which compromise the capabilities of NAD+-dependent proteins, including sirtuin and PARP. Notably, NAD+ pools decline during aging,222 and the decrement in NAD+ balance may also be observed in nearly diseases associated with age, including aging hearts.223 NAD+ levels inside cells are very much dictated by the match between de novo synthesis and tryptophan in kynurenine pathway-mediated salvage pathways and consumption by sirtuins and PARP224 (Fig. 4). Notably, PARP has been verified to counteract cell senescence by restraining genotoxic stress,225 while PARP also contributes to proinflammation and the SASP phenotype in senescent cells,226 implying the distinct effects of PARP on senescence initiation and established aging. Blockade of PARP1 antagonizes cell cycle arrest and defective DNA repair by increasing p38MAPK levels in senescent cells.227 More importantly, targeting PARP attenuates aging-associated cardiac and vascular dysfunction by improving mitochondrial function and communication.228,229 Conversely, unlike PARP, sirtuin family proteins (SIRTs) play negative roles in the proinflammatory SASP and senescence response. For example, Sirt 1 is downregulated by autophagy in senescence and aging,230 but Sirt 1 deletion triggers several degenerative alterations in atherosclerosis, neurodegeneration, and cirrhosis by increasing the SASP and cell cycle arrest.231,232 In addition, Sirt 6 might serve as a safeguard against the initiation of aging-related senescent myocyte and cardiac hypertrophy,233–235 particularly exercise-associated protection in the aging heart.236 However, Sirt 6-deficient mice showed premature aging and presented a proinflammatory phenotype.237,238 Both Sirt 1 and Sirt 6 have been found to prevent cardiac aging.239,240 Moreover, Sirt 2 protects against cell senescence and aging by restoring BUBR1, the mitotic checkpoint kinase, and H3K18Ac activation.241,242 Although a previous study confirmed the anti-cardiac hypertrophy effect of Sirt 2,243 whether Sirt 2 regulates cardiac aging is not clear. In line with PARP, elevated NAD+ may present the contrary influences and contribute to the SASP and aging by disturbing AMPK and p53 activation as well as enhancing p38MAPK and NF-kB activity in senescent cells244,245 (Fig. 5). These and many other studies suggest that NAD+ may play different roles at different times in aging. Nicotinamide phosphoribo-syltransferase (Nampt) is the enzyme that catalyzes the initial step in the NAD+ salvage pathway in mammals, which is rate-limiting.246 NAD+ synergizes with sirtuin to regulate protein acetylation and contributes to the improvements in DNA damage and oxidative stress in aging hearts, while downregulated NAD+ with defective Nampt aggravates this cardioprotection.221 Emerging evidence has shown that Nampt is substantially reduced in the ischemic heart, inducing a decrease in NAD+ content, inhibition of autophagic flux, and loss of cardiomyocytes.247 In contrast, increased NAD+ levels through Nampt overexpression led to the induction of autophagy during ischemia and an improvement in cardiac injury in myocardial infarction.193,248 In terms of the mechanism, a decrease in NAD+ levels promote lysosomal dysfunction, increasing the aging heart’s vulnerability to ischemic injury.249 These lines of evidence highlight essential roles for NAD+ in redox maintenance and suggest that replenishing NAD+ with NAD+ precursors, including nicotinamide and nicotinamide riboside, may have broad benefits for both lifespan and quality of health (Fig. 4).
Mitochondrial ROS and mtDNA
Increased ROS emission is an early warning sign for multiple pathological cardiac phenotypes. Mitochondria, especially the quinol oxidation site (Qo center) at complex III, serve as the major site for ROS release,250 in which enhanced ROS production appears before the functional alteration (Fig. 4). Interestingly, the mitochondria-ER interaction sites are also closely associated with the complex III Qo site that generates mitochondria ROS,251 by which ER stress may produce a rise in ROS252 and trigger mitochondrial ROS-indued ROS release.253 In terms of the potential mechanisms, reducing respirasomes decreases the redox hubs that straightly respond to O2 to produce ROS during cardiac aging. In addition, the activity and content of individual ETC complexes are substantially reduced in cardiac aging, directly favoring ROS assembly. Moreover, defective complex III inside the IFM instead of the SSM is a contributor to the elevated ROS assembly in aging hearts; consistent with the enhanced ROS assembly in IFM, markers of oxidative stress are upregulated in these cellular compartments during aging.254,255 Redox metabolism inside mitochondria serves as a crucial signal for cell fate. The combination of metabolite oxidation and oxidant production within mitochondria is crucial for viable cardiomyocytes during cardiac aging. For example, nuclear factor-erythroid 2-related factor 2 (NRF2) serves as a redox-responsive factor and mediates ROS elimination,256 while downregulation of NRF2 is observed in elderly individuals. As expected, reduced ROS production or the oxidized form of glutathione (GSSG) disposition ameliorates cardiac aging,257,258 supporting the concept that ROS derived by mitochondria are harmful to aging hearts. Recently, the correlation between ROS with cardiac aging is reported in some preclinical studies. Ablation of mitochondrial superoxide dismutase (SOD2), a ROS scavenger, leads to the development of senescence and aging.259 SOD3 mutation drives ROS-mediated chronic inflammation and degenerative diseases in aged mice.260 Furthermore, mitochondrial ROS triggers the Jun N-terminal kinase, thereby inducing the secretion of chromatin fragments from cytosol and enhances SASP.261 Several studies have suggested the possible preservative effects of limited assembly of ROS with classic ischemic preconditioning.262 However, the notion of ischemic preconditioning protection does not apply to elderly patients due to excessive ROS content during aging. Generally, it is an open question whether the promoted senescence due to aging is attributed to mitochondrial ROS. Notably, ROS actually serve as key molecules for several cardio-pathological processes, including cardiomyocyte renewal,263 fibroblast proliferation,264,265 differentiation,266,267 immune response268, and cardiomyocyte survival,269 which highlights the complex relationship between ROS and cardiac aging, and requires further investigation.
Due to the absence of protective histones, mtDNA is highly susceptible to oxidative damage.270 In mammalian species, accumulated mtDNA mutations have also been reported to contribute to aging,271 disturbing mitochondrial metabolism and resulting in dysfunctional consequences for targeted organs (Fig. 4). The chance of mutations on mtDNA of aged mice is approximately 1000-fold higher when compared with nuclear genes.272,273 A substantial portion of proteins critical for the genesis and capability of mitochondrial respiratory complexes, particularly complex III inside mitochondria, are determined by mtDNA, in addition, the mtDNA copy number is crucial for mitochondrial function.274 Elevation in oxidative stress contributes to the suppressed mtDNA replication and decrements in mtDNA copy number, causing mitochondrial respiratory chain deficiency and aging-related impairment of metabolism.275 Importantly, increased ROS content drives cardiomyocyte cell cycle arrest through mtDNA damage.276 In addition, defective mtDNA excision repair can lead to the accumulation of point mutations,277 double-strand breaks and, eventually, large deletions, all of which are associated with cardiac aging and dysfunction. For example, a recent study reported that a POLG-mutant mouse carrying a D257A mutation in a key residue of mitochondrial DNA polymerase experienced a loss of mtDNA stability, leading to a significant acceleration of aging processes.278,279 Moreover, increased mtDNA mutation burden contributes to abnormal mitochondrial biogenesis resulting in programmed cell death in cardiomyocytes280,281 (Fig. 4). Recently, studies have revealed that the secretion of mtDNA from the mitochondria, into the cytoplasm, and ultimately into the extracellular milieu accelerates aging and degenerative alteration by enhancing inflammation, innate immune signaling, and programmed cell death in local tissues.282,283 In addition, the extracellular release of mtDNA is emerging as intercellular signaling to mediate cell-to-cell crosstalk in the pathogenesis of CVDs.284 Collectively, both accumulated ROS production and increased mtDNA mutation burden may serve as senescent pioneers before functional alteration in cardiac aging. Of note, the extracellular release of mtDNA needs to be further investigated in future studies.
Therapeutic implications
As outlined above, these results demonstrate the intricate link between metabolism and cardiac aging, therefore prompting us to explore interventions that target metabolism that might serve as an approach for cardiac aging or delay aging progression. Five drugs, including rapamycin, acarbose, nordihydroguaiaretic acid, 17-α-estradiol, and aspirin, have been recognized by the multicenter Intervention Testing Program (ITP) supported by the National Institute for Ageing, as capable of reproducibly increasing lifespan in mice.285 Below, we outlined the possible interventions targeting metabolism in aging hearts and identify future challenges in this field.
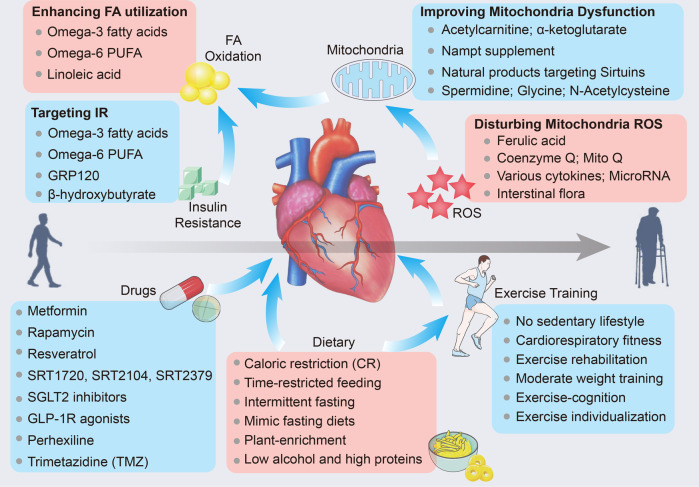
Targeting metabolites and intermediates
Although clear evidence of substantially defective fatty acid (FA) oxidation is emerging as a crucial trigger for metabolic remodeling and dysfunction in cardiac aging, drugs targeting metabolites are not routinely utilized in the clinical field. Since glycolysis requires less oxygen than FA oxidation as a consequence of the same amount of ATP,286,287 blockage of FA utilization may benefit cardiac bioenergetics under normal glucose uptake and utilization conditions. However, insulin resistance antagonizes hepatic glucose output and reduces the glucose uptake in cardiac aging, thereby defying this assumption. In addition, some toxic intermediates of FA oxidation further accelerate the accumulation of lipid droplets in heart tissues during aging and restrain cardiomyocyte survival. Thus, supplementation with FA with highly efficient utilization may benefit the aging heart. Accordingly, omega-3 fatty acids are emerging as a major constituent of the cell membrane used for restriction of age-correlated disease on account of considerable epidemiological evidence, such as the Age-Related Disease Study 2 (AREDS2).288,289 Omega-3 fatty acids reduce triglyceride amounts and bind with enzymes required for the biosynthesis of lipid mediators.290 Likewise, an omega-3 fatty acid diet may counteract cardiac aging.291,292 Moreover, recommendations for the dietary consumption of omega-6 polyunsaturated fatty acids (PUFAs) support CVDs prevention,293 which further suggests that the omega-6 PUFA diet may improve cardiac dysfunction in elderly individuals. Thus, enhancing the FA utilization rate with a linoleic acid (LA) supplement is a possible method for slowing the impairment of cardiac aging (Fig. 5). In addition, selective PPARα agonists (fibrates) decrease myocardial FA supply and uptake by promoting their utilization in extracardiac tissues and impeding lipid disposition in heart tissues.294
In addition, targeting insulin resistance and glucose oxidation may serve as alternative therapeutic strategies to ameliorate metabolic remodeling and improve cardiac efficiency during cardiac aging (Fig. 6). Likewise, omega-3 and omega-6 fatty acids have been reported to reduce inflammation and insulin resistance.295,296 GRP120 is recognized as an omega-3 fatty acid receptor that ameliorates inflammation and optimizes potent insulin sensitization.297 This evidence further favors the hypothesis that omega-3 and omega-6 fatty acid supplements may improve aging hearts. In addition, optimizing glucose oxidation with dichloroacetate stimulates glucose utilization by inhibiting its phosphorylation by promoting pyruvate dehydrogenase (PDH) activity.27 Ketone bodies, especially β-hydroxybutyrate (β-HB), are sourced from FA oxidation and possibly act as an energy origin for heart failure; accordingly, β-HB has the potential to be utilized as ancillary therapy for cardiac aging.102 Moreover, β-HB suppresses mitochondrial dysfunction by disrupting NLPR3 inflammasome formation and antagonizing the proinflammatory SASP in aged mice.298 In addition, both the pan carnitine O-palmitoyl-transferase 1 (CPT1) inhibitor perhexiline299,300 and the acetyl-CoA acyltransferase 2 inhibitor trimetazidine (TMZ)301,302 are metabolic reprogramming modulators that have the ability to partially suppress mitochondrial free FA beta-oxidation partially, enhance glucose oxidation, and promote cardiac energetics (with an increased PCr:ATP ratio). The latter has been further suggested to halt cardiac aging as well as metabolic defects in animal models,303,304 but there is a lack of clinical evidence and a very limited number of patient studies. Most recently, Na+/glucose cotransporter 2 (SGLT2; also known as SLC5A2) inhibitors have been verified to improve cardiac metabolism in type 2 diabetes mellitus,305,306 and SGLT2 inhibitors have been found to delay vascular aging by improving vascular function.307 Further, SGLT2 inhibitors impede the assembly of the more oxygen-efficient substrate β-hydroxybutyrate, a kind of ketone body, in the heart.308 A preclinical study reported that malfunctional SGLT2 in cardiac aging mediates defects in mitochondrial and cardiac contractility.309 Likewise, glucagon-like peptide 1 receptor (GLP-1R) agonists are also ascertained to reverse aging and neurodegeneration at a genetic level.310 However, their role and precise mechanism in cardiac aging remain to be further explored. Moreover, targeting sirtuins such as Sirt1 is significant in slowing cardiovascular aging,311 and recently, sirtuin-activating compounds, including resveratrol, SRT1720, SRT2104, and SRT2379, are also made to trigger the action of sirtuin to mitigate certain age-associated conditions in rodents and nonhuman primates231,312 (Fig. 6). Specifically, various small-scale clinical investigations on the impacts of SRT2104 on cardiovascular and metabolic markers, including those in type 2 diabetes patients, cigarette smokers, and elderly individuals,313 have been completed, with larger trials underway. Notably, the mismatch between FA oxidation and uptake seems to be opposite to insulin resistance and reduced energy fueling during cardiac aging. Cardiovascular aging-induced metabolite utilization seems to have conflicting outcomes, and targeting single metabolic pathways would be more straightforward.
Fig. 6.
Potential therapeutic approach for cardiac aging. Metabolic therapies for the treatment of cardiac aging are aimed to improve insulin resistance, FA oxidation, mitochondria dysfunction, and ROS. Synthetic small molecular drugs targeting insulin resistance, sirtuin activation, and ROS clearance are verified to delay cardiac aging in animal model. Moreover, both dietary advice and exercise training are beneficial for cardiac aging in the elderly. The online resource inside this figure was quoted or modified from Servier Medical Art
Improving mitochondrial dysfunction
As outlined above, enhancing mitophagy, optimizing electron transport, and blocking ROS and mtDNA mutations have emerged as potential strategies to improve mitochondrial dysfunction during aging. Among these, suppression of mitochondrial ROS production has always been a focus, while the past few decades have seen enormous strides to target mitochondrial ROS content. Ferulic acid, a powerful natural antioxidant and scavenger of free radicals, occurs naturally and is well recognized for its beneficial properties; it contributes to lifespan and stress resistance by interrupting ROS accumulation.314 Acetylcarnitine, a tracer of acetyl-CoA, optimizes aging-mediated reduction in OXPHOS, complex III, and complex IV by stimulating the transcription of mtDNA linked to ETC subunits.315 Metformin correlates with an prolonged lifespan in patients by promoting mitochondrial respiration. Accordingly, it was the initial drug assessed for its age-targeting influences in the large clinical study TAME.316–318 Furthermore, a retrospective analysis of patients with diabetes who received metformin showed a prolonged lifespan compared with individuals without DM.319 Importantly, as one of the most crucial antioxidants, coenzyme Q (CoQ) functions as an electron acceptor that obtains electrons from ROS (ROS scavenger) within the mitochondrial respiratory chain.320 It is also an essential cofactor in OXPHOS.321 Levels of CoQ in plasma are substantially reduced in HF patients,322 and CoQ content essentially declines with age.323 According to the Q-SYMBIO trial, continued CoQ10 supplementation to HF patients shows beneficial impacts on HF symptoms, reduces major adverse cardiovascular events (MACEs), and serves as the adjunctive treatment in chronic HF.324,325 Consistently, in several preclinical studies, CoQ has been suggested to improve aging-induced mitochondrial dysfunction by counteracting oxidative stress in the heart.326 Therefore, CoQ supplementation attenuates cardiac fibrosis and aging,327 with favorable clinical applications in CVDs. Subsequently, an optimized Mitoquinol mesylate (MitoQ), the combination of CoQ and lipophilic cation TPP+ is generated, and it is more likely to be absorbed by mitochondria than CoQ.328 Various animal models have verified the beneficial effects of MitoQ upon HF and aging.329,330 However, the evidence of MitoQ application in patients is limited, and consistently the roles of CoQ and MitoQ in cardiac aging need further investigation. Otherwise, various cytokines, miRNAs, and exosomes from the heart or distal organs also determine ROS during cardiac aging, which may be potential strategies (Fig. 6).
In addition to ROS production, suppressing mTOR with rapamycin is found to alleviate the unfavorable effects of cardiac aging and increase lifespan by promoting autophagy.331 In addition, everolimus, an analog of rapamycin has been authorized in clinical utilization as an immunosuppressant in transplanting solid organs, and importantly, healthy older individuals who received a non-immunosuppressive dose of everolimus presented an improved immunological response;332 however, observations mentioned above is limited by concentrating on influences observed 6 weeks after everolimus administration and chronic exposure was not considered. In the following year, a preclinical study revealed that chronic mTOR inhibition prolongs the life of immune-deficient mice by modestly altering gut metagenomes, and some metagenomic impacts correlated with immune outcomes.333 Unfortunately, the mechanism behind this remains unclear and mTOR inhibitor immune effects merit further studies associated with prolonged lifespan. As expected, proper amounts of exercise (discussed blow) can delay cardiac aging by enhancing autophagy and stimulating the phosphorylation of Bcl-2 and its dissociation from Beclin1.334 Enhanced de novo NAD+ synthesis, exogenous Nampt supplementation, or sirtuin targeting may promote NAD metabolism in mitochondria, serving as a potential approach in cardiac aging.335 Most recently, alginate oligosaccharide (AOS) was identified as an effective agent in impeding cardiac aging by improving mitochondrial biogenesis and maintaining mitochondrial integrity in aged mice.336 Similarly, the mitochondrially targeted peptide elamipretide (SS-31) significantly alleviated mitochondrial ROS and protein oxidation in aged hearts by targeting cardiolipin.337 Senolytic drugs that target and eliminate senescent cells present great potential in aging, all of which are involved in natural products and synthesize small molecules338,339 (Fig. 6). Likewise, there is insufficient clinical evidence supporting the use of these strategies in cardiac aging.
Healthy lifestyle for a healthy heart—dietary and exercise interventions
The Western diet is one of the main reasons for the growing obesity epidemic, chronic diseases, and aging. There is strong evidence that eating habits such as dietary restriction, overeating, and the resulting obesity influence both the lifespan and quality of health.340 Caloric restriction (CR) delays cardiac aging by improving mitochondrial bioenergetics by reducing oxidative stress and activating sirtuins.341 Optimal dietary practices that support longevity and health encompass a diet rich in plant-based foods, few processed foods, low alcohol consumption, and high protein consumption.340 Emerging evidence in the nutrition field is presented to promote health and lifespan, such as time-restricted feeding,342 intermittent fasting343, and diets that mimic fasting.344 Most recently, a ketogenic diet with high amount of the ketone body β-hydroxybutyrate is verified to increase lifespan and health.94 Future research should focus on delaying cardiac aging through the dietary strategies and identifying their correlations with precise mechanisms that modulate cardiac aging (Fig. 6).
Maximal aerobic exercise capacity decreases throughout adulthood and accelerates in later years. In addition to optimal diet and drug development, proper exercise is an effective protector for reducing the incidence of age-related disease.345 Overwhelming evidence supports the importance of maintaining high intensity of physical activity, engaging in exercise training, and improving overall cardiorespiratory fitness as effective strategies for treating CVDs.346 Mechanistically, a moderate amount of exercise activates sirtuin-1 and sirtuin-3,347,348 synchronously decreases mitochondrial production of H2O2 with increased MnSOD activity,348 and supports OXPHOS and mitochondrial metabolism, antagonizing fibrosis and proapoptotic signaling in the aging heart.349 Currently, despite the beneficial influences of exercise against aging, the mechanisms and whether this knowledge can be utilized to enhance the hearts of the aging population need further investigation.
Future challenges
What initiates senescence and cardiac aging?
Research advances have linked potential interventions with cardiac aging, whereas the identification of biomarkers for assessing the aging process remain a challenge. Our understanding of the in vivo processes responsible for aging and the induction of senescent cells, particularly in the context of cardiac aging, remains limited. Metabolic warning signs usually occur before cardiac structural alteration and dysfunction, providing a potential approach to detecting metabolic biomarkers during cardiac aging. Although cardiac aging is involved in metabolic disarrangement, DNA damage, telomere attrition, and mitochondrial morphofunctional defects, it has been difficult to determine how they induce senescent cells in the heart. Likewise, the development of multiple omics techniques, including single-cell and spatial omics, seems to provide a spectrum of choices for biomarkers in cardiac aging. Notably, long term and continuous observation in the elderly individuals is required to identify persuasive biomarkers of cardiac aging.
How can cardiac aging progression be delayed?
In addition to targeting metabolites in cardiac aging as described above, the modulation of mtDNA replication and stability can improve mitochondrial metabolism and energy fueling by promoting mtDNA-encoded catalytic subunits of complexes inside mitochondria, which may offer a novel concept for cardiac aging intervention with the tremendous progression of gene editing therapy and CAR T cells.350–352 Furthermore, telomerase activity is typically reduced as an organism age due to increased ROS production in senescent cells. This phenomenon has been implicated in cardiac aging,353 and restoring telomerase activity seems to be a potential approach. Recently, mitochondrial telomerase improves mitochondrial complex I subunit composition, which is responsible for cardioprotection in ischemic cardiomyopathy.354 In line with a previous study, telomerase defects correlate with the deterioration of heart tissue repair.355 Although the link between cardiac pathology and telomerase has been verified over the past decade, there are insufficient clinical data to support its translational value. Importantly, the mechanistic exploration of cardiac aging is relatively superficial in preclinical research, and more therapeutic targets for cardiac aging require further investigation in basic research. Specifically, to accelerate the development of precision medicine for delaying cardiac aging, it is essential to promote greater collaboration among researchers, doctors, patients, and data systems, among other stakeholders.
How can we move from simple organisms to humans?
Although mice are commonly used for research, it is widely acknowledged that essential outcomes observed in mice do not always translate to humans. Although there are many examples of a connection between cardiac aging and the treatment of CVDs, an important consideration is the methodology for testing these interventions and their eventual clinical application in human populations. First, several interventions that are beneficial in a specific genetic scenario may not apply to another.356 That said, the natural genetic variations present in the population may dampen the curative effects of pharmacological intervention, as explained above. Precision medicine has great potential to discover crucial genetic players of aging and to customize strategies to unique genetic variants, because of the large genetic heterogeneity in the human population. Second, despite numerous animal studies suggesting the benefits of nutrition and exercise, some research has challenged the universal applicability of these interventions. Both exercise and dietary restriction have arisen from preclinical studies to present protection against aging in animals,357–359 while it is plausible that individuals who have already optimized their nutrition and exercise habits may not derive significant benefits from further interventions. Subsequently, the same management for aging result in distinct outcomes due to gender differences, even in human investigations. Last, both the intricate nature of biology and the diverse range of biological phenotypes lead to reproducibility problems between different investigators, not only in mouse research but also in other model systems, implying that findings from studies conducted in mice do not always accurately predict outcomes in humans. Thus, more clinical trials are expected to provided more convincing clinical evidence instead of animal experiment in the future.
Conclusions
The aged heart exhibits accumulated ROS and lipids, with concomitant cardiac hypertrophy and diffuse fibrosis, therefore resulting in cardiac remodeling and dysfunction. The rapid increase in our understanding of mitochondrial metabolism that underlies cardiac aging contributes to making recommendations to intervene in aging-related cardiac complications. Importantly, the heart requires continuous energy fueling and relies predominantly on mitochondrial OXPHOS, while defective metabolism and abnormal mitochondria are part of the pathophysiology of cardiac aging prior to heart failure and concomitant clinical symptoms. Cardiac aging initiates shifts in substrate oxidation with impairment of FA oxidation and dysregulated glucose utilization, along with lipid storage and ROS generation in the heart. Improper substrate utilization and increased oxygen radicals are thought to lead to defects to mitochondria, damages to adjacent organelles, and cell death in the elderly heart. Accumulated clues to understanding cardiac aging present a chance to explore novel strategies which could be beneficial to cardiac regenerative diseases, particularly metabolic remodeling, which may serve as an early warning sign in elderly patients. At present, several interventions targeting mitochondria and/or metabolism have already been suggested to delay the development of cardiac aging, including inactivation of ROS with antioxidants, inspiration of mitophagy, Nampt supplementation, and stimulation of sirtuins. In addition, emerging developments in the nutrition field including CR diets, intermittent fasting, and ketogenic diets, have been recently shown to benefit the aged heart. However, before considering the translation of these interventions for the treatment of human patients, future studies should investigate their effects on both lifespan and cardiac aging.
Acknowledgements
The authors receive support from the National Key R&D Program of China (2018YFC1311300); the National Natural Science Foundation of China (No: 82170245, 81860080, and 82070204); The Regional Innovation and Development Joint Fund of National Natural Science Foundation of China (No. U22A20269). All online resource inside figures was quoted and modified from Servier Medical Art (http://smart.servier.com/), licensed under a Creative Common Attribution 3.0 Generic License (https://creativecommons.org/licenses/by/3.0/).
Author contributions
S.X. and Q.T. researched data for the article, discussed its content, wrote the manuscript. S.-C.X. created the figures. All the authors discussed the content of the article and reviewed and/or edited it before submission. All authors have read and approved the article.
Competing interests
The authors declare no competing interests.
References
- 1.Zeng Y, Hesketh T. The effects of China’s universal two-child policy. Lancet. 2016;388:1930–1938. doi: 10.1016/S0140-6736(16)31405-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mattson MP. Lifelong brain health is a lifelong challenge: from evolutionary principles to empirical evidence. Ageing Res. Rev. 2015;20:37–45. doi: 10.1016/j.arr.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mattson MP, Arumugam TV. Hallmarks of brain aging: adaptive and pathological modification by metabolic states. Cell Metab. 2018;27:1176–1199. doi: 10.1016/j.cmet.2018.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans MA, Sano S, Walsh K. Cardiovascular disease, aging, and clonal hematopoiesis. Annu. Rev. Pathol. 2020;15:419–438. doi: 10.1146/annurev-pathmechdis-012419-032544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lutz W, Sanderson W, Scherbov S. The coming acceleration of global population ageing. Nature. 2008;451:716–719. doi: 10.1038/nature06516. [DOI] [PubMed] [Google Scholar]
- 6.Gorbunova V, et al. The role of retrotransposable elements in ageing and age-associated diseases. Nature. 2021;596:43–53. doi: 10.1038/s41586-021-03542-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Deursen JM. The role of senescent cells in ageing. Nature. 2014;509:439–446. doi: 10.1038/nature13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peverill RE. Changes in left ventricular size, geometry, pump function and left heart pressures during healthy aging. Rev. Cardiovasc. Med. 2021;22:717–729. doi: 10.31083/j.rcm2203079. [DOI] [PubMed] [Google Scholar]
- 9.Spencer KT, et al. Effects of aging on left atrial reservoir, conduit, and booster pump function: a multi-institution acoustic quantification study. Heart. 2001;85:272–277. doi: 10.1136/heart.85.3.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mendonca GV, Pezarat-Correia P, Vaz JR, Silva L, Heffernan KS. Impact of aging on endurance and neuromuscular physical performance: the role of vascular senescence. Sports Med. 2017;47:583–598. doi: 10.1007/s40279-016-0596-8. [DOI] [PubMed] [Google Scholar]
- 11.Scholz DG, Kitzman DW, Hagen PT, Ilstrup DM, Edwards WD. Age-related changes in normal human hearts during the first 10 decades of life. Part I (Growth): a quantitative anatomic study of 200 specimens from subjects from birth to 19 years old. Mayo Clin. Proc. 1988;63:126–136. doi: 10.1016/S0025-6196(12)64945-3. [DOI] [PubMed] [Google Scholar]
- 12.Khouri MG, Maurer MS, El-Khoury Rumbarger L. Assessment of age-related changes in left ventricular structure and function by freehand three-dimensional echocardiography. Am. J. Geriatr. Cardiol. 2005;14:118–125. doi: 10.1111/j.1076-7460.2005.03845.x. [DOI] [PubMed] [Google Scholar]
- 13.Obas V, Vasan RS. The aging heart. Clin. Sci. 2018;132:1367–1382. doi: 10.1042/CS20171156. [DOI] [PubMed] [Google Scholar]
- 14.Piedepalumbo M, Koch WJ, de Lucia C. Metabolomics, heart disease and aging. Aging. 2021;13:6231–6232. doi: 10.18632/aging.202804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Veronica G, Esther RR. Aging, metabolic syndrome and the heart. Aging Dis. 2012;3:269–279. [PMC free article] [PubMed] [Google Scholar]
- 16.Chen L, et al. Comparative blood and urine metabolomics analysis of healthy elderly and young male Singaporeans. J. Proteome Res. 2020;19:3264–3275. doi: 10.1021/acs.jproteome.0c00215. [DOI] [PubMed] [Google Scholar]
- 17.Nyberg M, Jones AM. Matching of O2 utilization and O2 delivery in contracting skeletal muscle in health, aging, and heart failure. Front. Physiol. 2022;13:898395. doi: 10.3389/fphys.2022.898395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bertero E, Maack C. Metabolic remodelling in heart failure. Nat. Rev. Cardiol. 2018;15:457–470. doi: 10.1038/s41569-018-0044-6. [DOI] [PubMed] [Google Scholar]
- 19.Bhashyam S, et al. Aging is associated with myocardial insulin resistance and mitochondrial dysfunction. Am. J. Physiol. Heart Circ. Physiol. 2007;293:H3063–H3071. doi: 10.1152/ajpheart.00163.2007. [DOI] [PubMed] [Google Scholar]
- 20.Acosta O, et al. Increased glucose and placental GLUT-1 in large infants of obese nondiabetic mothers. Am. J. Obstet. Gynecol. 2015;212:e221–e227. doi: 10.1016/j.ajog.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 21.Papachristoforou E, Lambadiari V, Maratou E, Makrilakis K. Association of glycemic indices (hyperglycemia, glucose variability, and hypoglycemia) with oxidative stress and diabetic complications. J. Diabetes Res. 2020;2020:7489795. doi: 10.1155/2020/7489795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao P, et al. Hyperglycaemia-associated macrophage pyroptosis accelerates periodontal inflamm-aging. J. Clin. Periodontol. 2021;48:1379–1392. doi: 10.1111/jcpe.13517. [DOI] [PubMed] [Google Scholar]
- 23.Ghanem SS, et al. Age-dependent insulin resistance in male mice with null deletion of the carcinoembryonic antigen-related cell adhesion molecule 2 gene. Diabetologia. 2017;60:1751–1760. doi: 10.1007/s00125-017-4307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Menasche P, et al. Transplantation of human embryonic stem cell-derived cardiovascular progenitors for severe ischemic left ventricular dysfunction. J. Am. Coll. Cardiol. 2018;71:429–438. doi: 10.1016/j.jacc.2017.11.047. [DOI] [PubMed] [Google Scholar]
- 25.Biegon A, et al. Aromatase imaging with [N-methyl-11C] vorozole PET in healthy men and women. J. Nucl. Med. 2015;56:580–585. doi: 10.2967/jnumed.114.150383. [DOI] [PubMed] [Google Scholar]
- 26.Zhu C, et al. Metabolomics of oxidative stress: Nrf2 independent depletion of NAD or increases of sugar alcohols. Toxicol. Appl. Pharm. 2022;442:115949. doi: 10.1016/j.taap.2022.115949. [DOI] [PubMed] [Google Scholar]
- 27.Kato T, et al. Analysis of metabolic remodeling in compensated left ventricular hypertrophy and heart failure. Circ. Heart Fail. 2010;3:420–430. doi: 10.1161/CIRCHEARTFAILURE.109.888479. [DOI] [PubMed] [Google Scholar]
- 28.Sorokina N, et al. Recruitment of compensatory pathways to sustain oxidative flux with reduced carnitine palmitoyltransferase I activity characterizes inefficiency in energy metabolism in hypertrophied hearts. Circulation. 2007;115:2033–2041. doi: 10.1161/CIRCULATIONAHA.106.668665. [DOI] [PubMed] [Google Scholar]
- 29.Lydell CP, et al. Pyruvate dehydrogenase and the regulation of glucose oxidation in hypertrophied rat hearts. Cardiovasc. Res. 2002;53:841–851. doi: 10.1016/S0008-6363(01)00560-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Doenst T, Nguyen TD, Abel ED. Cardiac metabolism in heart failure: implications beyond ATP production. Circ. Res. 2013;113:709–724. doi: 10.1161/CIRCRESAHA.113.300376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aguiar-Oliveira MH, Bartke A. Growth hormone deficiency: health and longevity. Endocr. Rev. 2019;40:575–601. doi: 10.1210/er.2018-00216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anisimov VN, Bartke A. The key role of growth hormone-insulin-IGF-1 signaling in aging and cancer. Crit. Rev. Oncol. Hematol. 2013;87:201–223. doi: 10.1016/j.critrevonc.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kurauti MA, et al. Insulin and aging. Vitam. Horm. 2021;115:185–219. doi: 10.1016/bs.vh.2020.12.010. [DOI] [PubMed] [Google Scholar]
- 34.Lee WS, Kim J. Insulin-like growth factor-1 signaling in cardiac aging. Biochim. Biophys. Acta Mol. Basis Dis. 2018;1864:1931–1938. doi: 10.1016/j.bbadis.2017.08.029. [DOI] [PubMed] [Google Scholar]
- 35.Wessells RJ, Fitzgerald E, Cypser JR, Tatar M, Bodmer R. Insulin regulation of heart function in aging fruit flies. Nat. Genet. 2004;36:1275–1281. doi: 10.1038/ng1476. [DOI] [PubMed] [Google Scholar]
- 36.Ock S, et al. Deletion of IGF-1 receptors in cardiomyocytes attenuates cardiac aging in male mice. Endocrinology. 2016;157:336–345. doi: 10.1210/en.2015-1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moellendorf S, et al. IGF-IR signaling attenuates the age-related decline of diastolic cardiac function. Am. J. Physiol. Endocrinol. Metab. 2012;303:E213–E222. doi: 10.1152/ajpendo.00538.2011. [DOI] [PubMed] [Google Scholar]
- 38.Torella D, et al. Cardiac stem cell and myocyte aging, heart failure, and insulin-like growth factor-1 overexpression. Circ. Res. 2004;94:514–524. doi: 10.1161/01.RES.0000117306.10142.50. [DOI] [PubMed] [Google Scholar]
- 39.Li Q, et al. Cardiac-specific overexpression of insulin-like growth factor 1 attenuates aging-associated cardiac diastolic contractile dysfunction and protein damage. Am. J. Physiol. Heart Circ. Physiol. 2007;292:H1398–H1403. doi: 10.1152/ajpheart.01036.2006. [DOI] [PubMed] [Google Scholar]
- 40.Abdellatif M, et al. Fine-tuning cardiac insulin-like growth factor 1 receptor signaling to promote health and longevity. Circulation. 2022;145:1853–1866. doi: 10.1161/CIRCULATIONAHA.122.059863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li Q, Ceylan-Isik AF, Li J, Ren J. Deficiency of insulin-like growth factor 1 reduces sensitivity to aging-associated cardiomyocyte dysfunction. Rejuvenation Res. 2008;11:725–733. doi: 10.1089/rej.2008.0717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vasan RS, et al. Serum insulin-like growth factor I and risk for heart failure in elderly individuals without a previous myocardial infarction: the Framingham Heart Study. Ann. Intern. Med. 2003;139:642–648. doi: 10.7326/0003-4819-139-8-200310210-00007. [DOI] [PubMed] [Google Scholar]
- 43.Vinciguerra M, Santini MP, Claycomb WC, Ladurner AG, Rosenthal N. Local IGF-1 isoform protects cardiomyocytes from hypertrophic and oxidative stresses via SirT1 activity. Aging. 2009;2:43–62. doi: 10.18632/aging.100107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Abel ED. Glucose for the aging heart? Circulation. 2007;116:884–887. doi: 10.1161/CIRCULATIONAHA.107.723015. [DOI] [PubMed] [Google Scholar]
- 45.Ozaki N, Sato E, Kurokawa T, Ishibashi S. Early changes in the expression of GLUT4 protein in the heart of senescence-accelerated mouse. Mech. Ageing Dev. 1996;88:149–158. doi: 10.1016/0047-6374(96)01733-2. [DOI] [PubMed] [Google Scholar]
- 46.Van Puyvelde K, Mets T, Njemini R, Beyer I, Bautmans I. Effect of advanced glycation end product intake on inflammation and aging: a systematic review. Nutr. Rev. 2014;72:638–650. doi: 10.1111/nure.12141. [DOI] [PubMed] [Google Scholar]
- 47.Prasad C, Imrhan V, Marotta F, Juma S, Vijayagopal P. Lifestyle and advanced glycation end products (AGEs) burden: its relevance to healthy aging. Aging Dis. 2014;5:212–217. doi: 10.14336/AD.2014.0500212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bodiga VL, Eda SR, Bodiga S. Advanced glycation end products: role in pathology of diabetic cardiomyopathy. Heart Fail Rev. 2014;19:49–63. doi: 10.1007/s10741-013-9374-y. [DOI] [PubMed] [Google Scholar]
- 49.Scavello F, et al. Soluble receptor for advanced glycation end-products regulates age-associated cardiac fibrosis. Int. J. Biol. Sci. 2021;17:2399–2416. doi: 10.7150/ijbs.56379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu J, et al. Glycation end-product cross-link breaker reduces collagen and improves cardiac function in aging diabetic heart. Am. J. Physiol. Heart Circ. Physiol. 2003;285:H2587–H2591. doi: 10.1152/ajpheart.00516.2003. [DOI] [PubMed] [Google Scholar]
- 51.Bakris GL, et al. Advanced glycation end-product cross-link breakers. A novel approach to cardiovascular pathologies related to the aging process. Am. J. Hypertens. 2004;17:23S–30S. doi: 10.1016/j.amjhyper.2004.08.022. [DOI] [PubMed] [Google Scholar]
- 52.Li JS, et al. Mulberry leaves ameliorate diabetes via regulating metabolic profiling and AGEs/RAGE and p38 MAPK/NF-kappaB pathway. J. Ethnopharmacol. 2022;283:114713. doi: 10.1016/j.jep.2021.114713. [DOI] [PubMed] [Google Scholar]
- 53.Moskalev A, Stambler I, Caruso C. Innate and adaptive immunity in aging and longevity: the foundation of resilience. Aging Dis. 2020;11:1363–1373. doi: 10.14336/AD.2020.0603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu J, et al. Receptor for advanced glycation end-products promotes premature senescence of proximal tubular epithelial cells via activation of endoplasmic reticulum stress-dependent p21 signaling. Cell Signal. 2014;26:110–121. doi: 10.1016/j.cellsig.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 55.Liu J, et al. Impact of ER stress-regulated ATF4/p16 signaling on the premature senescence of renal tubular epithelial cells in diabetic nephropathy. Am. J. Physiol. Cell Physiol. 2015;308:C621–C630. doi: 10.1152/ajpcell.00096.2014. [DOI] [PubMed] [Google Scholar]
- 56.Gizak A, McCubrey JA, Rakus D. Cell-to-cell lactate shuttle operates in heart and is important in age-related heart failure. Aging. 2020;12:3388–3406. doi: 10.18632/aging.102818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee SY, et al. Fibroblast growth factor 21 mediates the associations between exercise, aging, and glucose regulation. Med. Sci. Sports Exerc. 2020;52:370–380. doi: 10.1249/MSS.0000000000002150. [DOI] [PubMed] [Google Scholar]
- 58.Fischer HJ, et al. The insulin receptor plays a critical role in T cell function and adaptive immunity. J. Immunol. 2017;198:1910–1920. doi: 10.4049/jimmunol.1601011. [DOI] [PubMed] [Google Scholar]
- 59.Helderman JH. Role of insulin in the intermediary metabolism of the activated thymic-derived lymphocyte. J. Clin. Invest. 1981;67:1636–1642. doi: 10.1172/JCI110199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Han JM, Patterson SJ, Speck M, Ehses JA, Levings MK. Insulin inhibits IL-10-mediated regulatory T cell function: implications for obesity. J. Immunol. 2014;192:623–629. doi: 10.4049/jimmunol.1302181. [DOI] [PubMed] [Google Scholar]
- 61.Minhas PS, et al. Restoring metabolism of myeloid cells reverses cognitive decline in ageing. Nature. 2021;590:122–128. doi: 10.1038/s41586-020-03160-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shosha E, et al. Mechanisms of diabetes-induced endothelial cell senescence: role of arginase 1. Int. J. Mol. Sci. 2018;19:1215. doi: 10.3390/ijms19041215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hayashi T, et al. Endothelial cellular senescence is inhibited by nitric oxide: implications in atherosclerosis associated with menopause and diabetes. Proc. Natl Acad. Sci. USA. 2006;103:17018–17023. doi: 10.1073/pnas.0607873103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Salpea KD, et al. The effect of pro-inflammatory conditioning and/or high glucose on telomere shortening of aging fibroblasts. PLoS ONE. 2013;8:e73756. doi: 10.1371/journal.pone.0073756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mehdizadeh M, Aguilar M, Thorin E, Ferbeyre G, Nattel S. The role of cellular senescence in cardiac disease: basic biology and clinical relevance. Nat. Rev. Cardiol. 2022;19:250–264. doi: 10.1038/s41569-021-00624-2. [DOI] [PubMed] [Google Scholar]
- 66.Atar D, et al. New cardiovascular prevention guidelines: How to optimally manage dyslipidaemia and cardiovascular risk in 2021 in patients needing secondary prevention? Atherosclerosis. 2021;319:51–61. doi: 10.1016/j.atherosclerosis.2020.12.013. [DOI] [PubMed] [Google Scholar]
- 67.Borcherding N, et al. Dietary lipids inhibit mitochondria transfer to macrophages to divert adipocyte-derived mitochondria into the blood. Cell Metab. 2022;34:1499–1513. doi: 10.1016/j.cmet.2022.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Livshits G, Kalinkovich A. Inflammaging as a common ground for the development and maintenance of sarcopenia, obesity, cardiomyopathy and dysbiosis. Ageing Res. Rev. 2019;56:100980. doi: 10.1016/j.arr.2019.100980. [DOI] [PubMed] [Google Scholar]
- 69.Koh JH, et al. TFAM enhances fat oxidation and attenuates high-fat diet-induced insulin resistance in skeletal muscle. Diabetes. 2019;68:1552–1564. doi: 10.2337/db19-0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhang D, et al. Resistance to high-fat diet-induced obesity and insulin resistance in mice with very long-chain acyl-CoA dehydrogenase deficiency. Cell Metab. 2010;11:402–411. doi: 10.1016/j.cmet.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yuan M, et al. Reversal of obesity- and diet-induced insulin resistance with salicylates or targeted disruption of Ikkbeta. Science. 2001;293:1673–1677. doi: 10.1126/science.1061620. [DOI] [PubMed] [Google Scholar]
- 72.Koonen DP, et al. CD36 expression contributes to age-induced cardiomyopathy in mice. Circulation. 2007;116:2139–2147. doi: 10.1161/CIRCULATIONAHA.107.712901. [DOI] [PubMed] [Google Scholar]
- 73.Koonen DP, et al. Alterations in skeletal muscle fatty acid handling predisposes middle-aged mice to diet-induced insulin resistance. Diabetes. 2010;59:1366–1375. doi: 10.2337/db09-1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bergo M, Olivecrona G, Olivecrona T. Regulation of adipose tissue lipoprotein lipase in young and old rats. Int. J. Obes. Relat. Metab. Disord. 1997;21:980–986. doi: 10.1038/sj.ijo.0800506. [DOI] [PubMed] [Google Scholar]
- 75.Barger PM, Brandt JM, Leone TC, Weinheimer CJ, Kelly DP. Deactivation of peroxisome proliferator-activated receptor-alpha during cardiac hypertrophic growth. J. Clin. Invest. 2000;105:1723–1730. doi: 10.1172/JCI9056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lahey R, Wang X, Carley AN, Lewandowski ED. Dietary fat supply to failing hearts determines dynamic lipid signaling for nuclear receptor activation and oxidation of stored triglyceride. Circulation. 2014;130:1790–1799. doi: 10.1161/CIRCULATIONAHA.114.011687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liu L, et al. Diacylglycerol acyl transferase 1 overexpression detoxifies cardiac lipids in PPARgamma transgenic mice. J. Lipid Res. 2012;53:1482–1492. doi: 10.1194/jlr.M024208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sack MN, et al. Fatty acid oxidation enzyme gene expression is downregulated in the failing heart. Circulation. 1996;94:2837–2842. doi: 10.1161/01.CIR.94.11.2837. [DOI] [PubMed] [Google Scholar]
- 79.Babenko NA, Storozhenko GV. Role of ceramide in reduction of the cardiolipin content in the heart during aging. Adv. Gerontol. 2017;30:43–48. [PubMed] [Google Scholar]
- 80.Kim Y, et al. Adiponectin receptor agonist ameliorates cardiac lipotoxicity via enhancing ceramide metabolism in type 2 diabetic mice. Cell Death Dis. 2022;13:282. doi: 10.1038/s41419-022-04726-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wu JH, et al. Genome-wide association study identifies novel loci associated with concentrations of four plasma phospholipid fatty acids in the de novo lipogenesis pathway: results from the Cohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE) consortium. Circ. Cardiovasc. Genet. 2013;6:171–183. doi: 10.1161/CIRCGENETICS.112.964619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Eum JY, et al. Aging-related lipidomic changes in mouse serum, kidney, and heart by nanoflow ultrahigh-performance liquid chromatography-tandem mass spectrometry. J. Chromatogr. A. 2020;1618:460849. doi: 10.1016/j.chroma.2020.460849. [DOI] [PubMed] [Google Scholar]
- 83.Pearce EL, et al. Enhancing CD8 T-cell memory by modulating fatty acid metabolism. Nature. 2009;460:103–107. doi: 10.1038/nature08097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nomura M, et al. Macrophage fatty acid oxidation inhibits atherosclerosis progression. J. Mol. Cell Cardiol. 2019;127:270–276. doi: 10.1016/j.yjmcc.2019.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Muraoka N, et al. Role of cyclooxygenase-2-mediated prostaglandin E2-prostaglandin E receptor 4 signaling in cardiac reprogramming. Nat. Commun. 2019;10:674. doi: 10.1038/s41467-019-08626-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kim JW, et al. Gene expression of cyclooxygenase in the aging heart. J. Gerontol. A Biol. Sci. Med. Sci. 2001;56:B350–B355. doi: 10.1093/gerona/56.8.B350. [DOI] [PubMed] [Google Scholar]
- 87.Han JH, et al. Selective COX-2 inhibitor, NS-398, inhibits the replicative senescence of cultured dermal fibroblasts. Mech. Ageing Dev. 2004;125:359–366. doi: 10.1016/j.mad.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 88.Pastori D, et al. Aging-related decline of glutathione peroxidase 3 and risk of cardiovascular events in patients with atrial fibrillation. J. Am. Heart Assoc. 2016;5:e003682. doi: 10.1161/JAHA.116.003682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Catalano A, Rodilossi S, Caprari P, Coppola V, Procopio A. 5-Lipoxygenase regulates senescence-like growth arrest by promoting ROS-dependent p53 activation. EMBO J. 2005;24:170–179. doi: 10.1038/sj.emboj.7600502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tourki B, et al. Lack of resolution sensor drives age-related cardiometabolic and cardiorenal defects and impedes inflammation-resolution in heart failure. Mol. Metab. 2020;31:138–149. doi: 10.1016/j.molmet.2019.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rymut N, et al. Resolvin D1 promotes efferocytosis in aging by limiting senescent cell-induced MerTK cleavage. FASEB J. 2020;34:597–609. doi: 10.1096/fj.201902126R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Das UN. Bioactive lipids in age-related disorders. Adv. Exp. Med. Biol. 2020;1260:33–83. doi: 10.1007/978-3-030-42667-5_3. [DOI] [PubMed] [Google Scholar]
- 93.Dabek A, Wojtala M, Pirola L, Balcerczyk A. Modulation of cellular biochemistry, epigenetics and metabolomics by ketone bodies. implications of the ketogenic diet in the physiology of the organism and pathological states. Nutrients. 2020;12:788. doi: 10.3390/nu12030788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Puchalska P, Crawford PA. Multi-dimensional roles of ketone bodies in fuel metabolism, signaling, and therapeutics. Cell Metab. 2017;25:262–284. doi: 10.1016/j.cmet.2016.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Aubert G, et al. The failing heart relies on ketone bodies as a fuel. Circulation. 2016;133:698–705. doi: 10.1161/CIRCULATIONAHA.115.017355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bedi KC, Jr., et al. Evidence for intramyocardial disruption of lipid metabolism and increased myocardial ketone utilization in advanced human heart failure. Circulation. 2016;133:706–716. doi: 10.1161/CIRCULATIONAHA.115.017545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Takahara S, Soni S, Maayah ZH, Ferdaoussi M, Dyck JRB. Ketone therapy for heart failure: current evidence for clinical use. Cardiovasc. Res. 2022;118:977–987. doi: 10.1093/cvr/cvab068. [DOI] [PubMed] [Google Scholar]
- 98.Sleiman SF, et al. Exercise promotes the expression of brain derived neurotrophic factor (BDNF) through the action of the ketone body beta-hydroxybutyrate. Elife. 2016;5:e15092. doi: 10.7554/eLife.15092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hyyti OM, Ledee D, Ning XH, Ge M, Portman MA. Aging impairs myocardial fatty acid and ketone oxidation and modifies cardiac functional and metabolic responses to insulin in mice. Am. J. Physiol. Heart Circ. Physiol. 2010;299:H868–H875. doi: 10.1152/ajpheart.00931.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Huang C, et al. The ketone body metabolite beta-hydroxybutyrate induces an antidepression-associated ramification of microglia via HDACs inhibition-triggered Akt-small RhoGTPase activation. Glia. 2018;66:256–278. doi: 10.1002/glia.23241. [DOI] [PubMed] [Google Scholar]
- 101.Cahill GF., Jr. Fuel metabolism in starvation. Annu. Rev. Nutr. 2006;26:1–22. doi: 10.1146/annurev.nutr.26.061505.111258. [DOI] [PubMed] [Google Scholar]
- 102.Wang L, Chen P, Xiao W. beta-hydroxybutyrate as an anti-aging metabolite. Nutrients. 2021;13:3420. doi: 10.3390/nu13103420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cotter DG, Schugar RC, Wentz AE, d’Avignon DA, Crawford PA. Successful adaptation to ketosis by mice with tissue-specific deficiency of ketone body oxidation. Am. J. Physiol. Endocrinol. Metab. 2013;304:E363–E374. doi: 10.1152/ajpendo.00547.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cotter DG, d’Avignon DA, Wentz AE, Weber ML, Crawford PA. Obligate role for ketone body oxidation in neonatal metabolic homeostasis. J. Biol. Chem. 2011;286:6902–6910. doi: 10.1074/jbc.M110.192369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Squires JE, Sun J, Caffrey JL, Yoshishige D, Mallet RT. Acetoacetate augments beta-adrenergic inotropism of stunned myocardium by an antioxidant mechanism. Am. J. Physiol. Heart Circ. Physiol. 2003;284:H1340–H1347. doi: 10.1152/ajpheart.00473.2002. [DOI] [PubMed] [Google Scholar]
- 106.Mallet RT, Sun J. Antioxidant properties of myocardial fuels. Mol. Cell Biochem. 2003;253:103–111. doi: 10.1023/A:1026009519783. [DOI] [PubMed] [Google Scholar]
- 107.Thai PN, et al. Mitochondrial quality control in aging and heart failure: influence of ketone bodies and mitofusin-stabilizing peptides. Front. Physiol. 2019;10:382. doi: 10.3389/fphys.2019.00382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Newman JC, et al. Ketogenic diet reduces midlife mortality and improves memory in aging mice. Cell Metab. 2017;26:547–557 e548. doi: 10.1016/j.cmet.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sedej S. Ketone bodies to the rescue for an aging heart? Cardiovasc. Res. 2018;114:e1–e2. doi: 10.1093/cvr/cvx218. [DOI] [PubMed] [Google Scholar]
- 110.Mishra A, et al. Fasting-mimicking diet prevents high-fat diet effect on cardiometabolic risk and lifespan. Nat. Metab. 2021;3:1342–1356. doi: 10.1038/s42255-021-00469-6. [DOI] [PubMed] [Google Scholar]
- 111.Sakr, H. F., Sirasanagandla, S. R., Das, S., Bima, A. I. & Elsamanoudy, A. Z. Low-carbohydrate ketogenic diet for improvement of glycemic control: mechanism of action of ketosis and beneficial effects. Curr. Diabetes Rev. (2022). [DOI] [PubMed]
- 112.Bradshaw PC. Acetyl-CoA metabolism and histone acetylation in the regulation of aging and lifespan. Antioxidants. 2021;10:572. doi: 10.3390/antiox10040572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Houston R, et al. Acetylation-mediated remodeling of the nucleolus regulates cellular acetyl-CoA responses. PLoS Biol. 2020;18:e3000981. doi: 10.1371/journal.pbio.3000981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mews P, et al. Acetyl-CoA synthetase regulates histone acetylation and hippocampal memory. Nature. 2017;546:381–386. doi: 10.1038/nature22405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Burke AC, Huff MW. ATP-citrate lyase: genetics, molecular biology and therapeutic target for dyslipidemia. Curr. Opin. Lipido. 2017;28:193–200. doi: 10.1097/MOL.0000000000000390. [DOI] [PubMed] [Google Scholar]
- 116.Sutendra G, et al. A nuclear pyruvate dehydrogenase complex is important for the generation of acetyl-CoA and histone acetylation. Cell. 2014;158:84–97. doi: 10.1016/j.cell.2014.04.046. [DOI] [PubMed] [Google Scholar]
- 117.Motino O, et al. ACBP/DBI protein neutralization confers autophagy-dependent organ protection through inhibition of cell loss, inflammation, and fibrosis. Proc. Natl Acad. Sci. USA. 2022;119:e2207344119. doi: 10.1073/pnas.2207344119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Liu X, et al. Acetate production from glucose and coupling to mitochondrial metabolism in mammals. Cell. 2018;175:502–513 e513. doi: 10.1016/j.cell.2018.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Gao X, et al. Acetate functions as an epigenetic metabolite to promote lipid synthesis under hypoxia. Nat. Commun. 2016;7:11960. doi: 10.1038/ncomms11960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhu D, Li X, Tian Y. Mitochondrial-to-nuclear communication in aging: an epigenetic perspective. Trends Biochem. Sci. 2022;47:645–659. doi: 10.1016/j.tibs.2022.03.008. [DOI] [PubMed] [Google Scholar]
- 121.Sabari BR, Zhang D, Allis CD, Zhao Y. Metabolic regulation of gene expression through histone acylations. Nat. Rev. Mol. Cell Biol. 2017;18:90–101. doi: 10.1038/nrm.2016.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zuurbier CJ, et al. Cardiac metabolism as a driver and therapeutic target of myocardial infarction. J. Cell Mol. Med. 2020;24:5937–5954. doi: 10.1111/jcmm.15180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Xu Y, et al. Branched-chain amino acid catabolism promotes thrombosis risk by enhancing tropomodulin-3 propionylation in platelets. Circulation. 2020;142:49–64. doi: 10.1161/CIRCULATIONAHA.119.043581. [DOI] [PubMed] [Google Scholar]
- 124.Wang N, et al. Histone lactylation boosts reparative gene activation post-myocardial infarction. Circ. Res. 2022;131:893–908. doi: 10.1161/CIRCRESAHA.122.320488. [DOI] [PubMed] [Google Scholar]
- 125.Yang K, et al. Lactate promotes macrophage HMGB1 lactylation, acetylation, and exosomal release in polymicrobial sepsis. Cell Death Differ. 2022;29:133–146. doi: 10.1038/s41418-021-00841-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cai W, et al. Modulating lysine crotonylation in cardiomyocytes improves myocardial outcomes. Circ. Res. 2022;131:456–472. doi: 10.1161/CIRCRESAHA.122.321054. [DOI] [PubMed] [Google Scholar]
- 127.Sadhukhan S, et al. Metabolomics-assisted proteomics identifies succinylation and SIRT5 as important regulators of cardiac function. Proc. Natl Acad. Sci. USA. 2016;113:4320–4325. doi: 10.1073/pnas.1519858113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Aronsen JM, Swift F, Sejersted OM. Cardiac sodium transport and excitation-contraction coupling. J. Mol. Cell Cardiol. 2013;61:11–19. doi: 10.1016/j.yjmcc.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 129.Maack C, et al. Treatments targeting inotropy. Eur. Heart J. 2019;40:3626–3644. doi: 10.1093/eurheartj/ehy600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Mattiazzi A, Tardiff JC, Kranias EG. Stress seats a new guest at the table of PLN/SERCA and their partners. Circ. Res. 2021;128:471–473. doi: 10.1161/CIRCRESAHA.121.318742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Campbell HM, et al. Loss of SPEG inhibitory phosphorylation of ryanodine receptor type-2 promotes atrial fibrillation. Circulation. 2020;142:1159–1172. doi: 10.1161/CIRCULATIONAHA.120.045791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gorski PA, et al. Role of SIRT1 in modulating acetylation of the sarco-endoplasmic reticulum Ca(2+)-ATPase in Heart Failure. Circ. Res. 2019;124:e63–e80. doi: 10.1161/CIRCRESAHA.118.313865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Alghamdi AM, Boyett MR, Hancox JC, Zhang H. Cardiac pacemaker dysfunction arising from different studies of ion channel remodeling in the aging rat heart. Front. Physiol. 2020;11:546508. doi: 10.3389/fphys.2020.546508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Qin F, et al. Hydrogen peroxide-mediated SERCA cysteine 674 oxidation contributes to impaired cardiac myocyte relaxation in senescent mouse heart. J. Am. Heart Assoc. 2013;2:e000184. doi: 10.1161/JAHA.113.000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Palmer JW, Tandler B, Hoppel CL. Biochemical properties of subsarcolemmal and interfibrillar mitochondria isolated from rat cardiac muscle. J. Biol. Chem. 1977;252:8731–8739. doi: 10.1016/S0021-9258(19)75283-1. [DOI] [PubMed] [Google Scholar]
- 136.Fannin SW, Lesnefsky EJ, Slabe TJ, Hassan MO, Hoppel CL. Aging selectively decreases oxidative capacity in rat heart interfibrillar mitochondria. Arch. Biochem. Biophys. 1999;372:399–407. doi: 10.1006/abbi.1999.1508. [DOI] [PubMed] [Google Scholar]
- 137.El’darov Ch,M, Vays VB, Vangeli IM, Kolosova NG, Bakeeva LE. Morphometric examination of mitochondrial ultrastructure in aging cardiomyocytes. Biochemistry. 2015;80:604–609. doi: 10.1134/S0006297915050132. [DOI] [PubMed] [Google Scholar]
- 138.Riva A, Tandler B, Loffredo F, Vazquez E, Hoppel C. Structural differences in two biochemically defined populations of cardiac mitochondria. Am. J. Physiol. Heart Circ. Physiol. 2005;289:H868–H872. doi: 10.1152/ajpheart.00866.2004. [DOI] [PubMed] [Google Scholar]
- 139.Riva A, et al. Structure of cristae in cardiac mitochondria of aged rat. Mech. Ageing Dev. 2006;127:917–921. doi: 10.1016/j.mad.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Tanaka-Esposito C, Chen Q, Lesnefsky EJ. Blockade of electron transport before ischemia protects mitochondria and decreases myocardial injury during reperfusion in aged rat hearts. Transl. Res. 2012;160:207–216. doi: 10.1016/j.trsl.2012.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Fernandez-Sanz C, et al. Defective sarcoplasmic reticulum-mitochondria calcium exchange in aged mouse myocardium. Cell Death Dis. 2014;5:e1573. doi: 10.1038/cddis.2014.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Dai DF, Rabinovitch PS. Cardiac aging in mice and humans: the role of mitochondrial oxidative stress. Trends Cardiovasc. Med. 2009;19:213–220. doi: 10.1016/j.tcm.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Chen L, et al. Loss of Sam50 in hepatocytes induces cardiolipin-dependent mitochondrial membrane remodeling to trigger mtDNA release and liver injury. Hepatology. 2022;76:1389–1408. doi: 10.1002/hep.32471. [DOI] [PubMed] [Google Scholar]
- 144.Mejia EM, Cole LK, Hatch GM. Cardiolipin metabolism and the role it plays in heart failure and mitochondrial supercomplex formation. Cardiovasc. Hematol. Disord. Drug Targets. 2014;14:98–106. doi: 10.2174/1871529X14666140505123753. [DOI] [PubMed] [Google Scholar]
- 145.Kagan VE, et al. Cytochrome c acts as a cardiolipin oxygenase required for release of proapoptotic factors. Nat. Chem. Biol. 2005;1:223–232. doi: 10.1038/nchembio727. [DOI] [PubMed] [Google Scholar]
- 146.Picca A, et al. Mitochondrial quality control mechanisms as molecular targets in cardiac ageing. Nat. Rev. Cardiol. 2018;15:543–554. doi: 10.1038/s41569-018-0059-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Popov LD. Mitochondrial biogenesis: an update. J. Cell Mol. Med. 2020;24:4892–4899. doi: 10.1111/jcmm.15194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Wu Z, et al. Mechanisms controlling mitochondrial biogenesis and respiration through the thermogenic coactivator PGC-1. Cell. 1999;98:115–124. doi: 10.1016/S0092-8674(00)80611-X. [DOI] [PubMed] [Google Scholar]
- 149.Russell LK, et al. Cardiac-specific induction of the transcriptional coactivator peroxisome proliferator-activated receptor gamma coactivator-1alpha promotes mitochondrial biogenesis and reversible cardiomyopathy in a developmental stage-dependent manner. Circ. Res. 2004;94:525–533. doi: 10.1161/01.RES.0000117088.36577.EB. [DOI] [PubMed] [Google Scholar]
- 150.Salazar G, et al. SQSTM1/p62 and PPARGC1A/PGC-1alpha at the interface of autophagy and vascular senescence. Autophagy. 2020;16:1092–1110. doi: 10.1080/15548627.2019.1659612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Anderson R, et al. Length-independent telomere damage drives post-mitotic cardiomyocyte senescence. EMBO J. 2019;38:e100492. doi: 10.15252/embj.2018100492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Amano H, et al. Telomere dysfunction induces sirtuin repression that drives telomere-dependent disease. Cell Metab. 2019;29:1274–1290 e1279. doi: 10.1016/j.cmet.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Fang EF, et al. Nuclear DNA damage signalling to mitochondria in ageing. Nat. Rev. Mol. Cell Biol. 2016;17:308–321. doi: 10.1038/nrm.2016.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Zhu Y, Liu X, Ding X, Wang F, Geng X. Telomere and its role in the aging pathways: telomere shortening, cell senescence and mitochondria dysfunction. Biogerontology. 2019;20:1–16. doi: 10.1007/s10522-018-9769-1. [DOI] [PubMed] [Google Scholar]
- 155.Garcia S, et al. Overexpression of PGC-1alpha in aging muscle enhances a subset of young-like molecular patterns. Aging Cell. 2018;17:e12707. doi: 10.1111/acel.12707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Correia-Melo C, et al. Mitochondria are required for pro-ageing features of the senescent phenotype. EMBO J. 2016;35:724–742. doi: 10.15252/embj.201592862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Xin T, Lu C. SirT3 activates AMPK-related mitochondrial biogenesis and ameliorates sepsis-induced myocardial injury. Aging. 2020;12:16224–16237. doi: 10.18632/aging.103644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Huang DD, et al. Nrf2 deficiency exacerbates frailty and sarcopenia by impairing skeletal muscle mitochondrial biogenesis and dynamics in an age-dependent manner. Exp. Gerontol. 2019;119:61–73. doi: 10.1016/j.exger.2019.01.022. [DOI] [PubMed] [Google Scholar]
- 159.Sato M, et al. The lncRNA Caren antagonizes heart failure by inactivating DNA damage response and activating mitochondrial biogenesis. Nat. Commun. 2021;12:2529. doi: 10.1038/s41467-021-22735-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Ma D, et al. Klf5 down-regulation induces vascular senescence through eIF5a depletion and mitochondrial fission. PLoS Biol. 2020;18:e3000808. doi: 10.1371/journal.pbio.3000808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Giacomello M, Pyakurel A, Glytsou C, Scorrano L. The cell biology of mitochondrial membrane dynamics. Nat. Rev. Mol. Cell Biol. 2020;21:204–224. doi: 10.1038/s41580-020-0210-7. [DOI] [PubMed] [Google Scholar]
- 162.Konig T, et al. MIROs and DRP1 drive mitochondrial-derived vesicle biogenesis and promote quality control. Nat. Cell Biol. 2021;23:1271–1286. doi: 10.1038/s41556-021-00798-4. [DOI] [PubMed] [Google Scholar]
- 163.Lee S, et al. Mitochondrial fission and fusion mediators, hFis1 and OPA1, modulate cellular senescence. J. Biol. Chem. 2007;282:22977–22983. doi: 10.1074/jbc.M700679200. [DOI] [PubMed] [Google Scholar]
- 164.Park YY, et al. Loss of MARCH5 mitochondrial E3 ubiquitin ligase induces cellular senescence through dynamin-related protein 1 and mitofusin 1. J. Cell Sci. 2010;123:619–626. doi: 10.1242/jcs.061481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Joseph AM, et al. Dysregulation of mitochondrial quality control processes contribute to sarcopenia in a mouse model of premature aging. PLoS ONE. 2013;8:e69327. doi: 10.1371/journal.pone.0069327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Tsushima K, et al. Mitochondrial reactive oxygen species in lipotoxic hearts induce post-translational modifications of AKAP121, DRP1, and OPA1 that promote mitochondrial fission. Circ. Res. 2018;122:58–73. doi: 10.1161/CIRCRESAHA.117.311307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Pernas L, Scorrano L. Mito-Morphosis: mitochondrial fusion, fission, and cristae remodeling as key mediators of cellular function. Annu. Rev. Physiol. 2016;78:505–531. doi: 10.1146/annurev-physiol-021115-105011. [DOI] [PubMed] [Google Scholar]
- 168.Hirabayashi Y, et al. ER-mitochondria tethering by PDZD8 regulates Ca(2+) dynamics in mammalian neurons. Science. 2017;358:623–630. doi: 10.1126/science.aan6009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Hammerling BC, Gustafsson AB. Mitochondrial quality control in the myocardium: cooperation between protein degradation and mitophagy. J. Mol. Cell Cardiol. 2014;75:122–130. doi: 10.1016/j.yjmcc.2014.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Lou G, et al. Mitophagy and neuroprotection. Trends Mol. Med. 2020;26:8–20. doi: 10.1016/j.molmed.2019.07.002. [DOI] [PubMed] [Google Scholar]
- 171.Kauppila TES, Kauppila JHK, Larsson NG. Mammalian mitochondria and aging: an update. Cell Metab. 2017;25:57–71. doi: 10.1016/j.cmet.2016.09.017. [DOI] [PubMed] [Google Scholar]
- 172.Wu H, et al. Deficiency of mitophagy receptor FUNDC1 impairs mitochondrial quality and aggravates dietary-induced obesity and metabolic syndrome. Autophagy. 2019;15:1882–1898. doi: 10.1080/15548627.2019.1596482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Melentijevic I, et al. C. elegans neurons jettison protein aggregates and mitochondria under neurotoxic stress. Nature. 2017;542:367–371. doi: 10.1038/nature21362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Sun K, Jing X, Guo J, Yao X, Guo F. Mitophagy in degenerative joint diseases. Autophagy. 2021;17:2082–2092. doi: 10.1080/15548627.2020.1822097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Yu B, et al. Mitochondrial phosphatase PGAM5 modulates cellular senescence by regulating mitochondrial dynamics. Nat. Commun. 2020;11:2549. doi: 10.1038/s41467-020-16312-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Pyo JO, et al. Overexpression of Atg5 in mice activates autophagy and extends lifespan. Nat. Commun. 2013;4:2300. doi: 10.1038/ncomms3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Zhong Y, et al. Distinct regulation of autophagic activity by Atg14L and Rubicon associated with Beclin 1-phosphatidylinositol-3-kinase complex. Nat. Cell Biol. 2009;11:468–476. doi: 10.1038/ncb1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Yamamoto S, et al. Autophagy differentially regulates insulin production and insulin sensitivity. Cell Rep. 2018;23:3286–3299. doi: 10.1016/j.celrep.2018.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Lampert MA, et al. BNIP3L/NIX and FUNDC1-mediated mitophagy is required for mitochondrial network remodeling during cardiac progenitor cell differentiation. Autophagy. 2019;15:1182–1198. doi: 10.1080/15548627.2019.1580095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Dai DF, et al. Age-dependent cardiomyopathy in mitochondrial mutator mice is attenuated by overexpression of catalase targeted to mitochondria. Aging Cell. 2010;9:536–544. doi: 10.1111/j.1474-9726.2010.00581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Chen Y, Dorn GW., 2nd PINK1-phosphorylated mitofusin 2 is a Parkin receptor for culling damaged mitochondria. Science. 2013;340:471–475. doi: 10.1126/science.1231031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Kubli DA, Quinsay MN, Gustafsson AB. Parkin deficiency results in accumulation of abnormal mitochondria in aging myocytes. Commun. Integr. Biol. 2013;6:e24511. doi: 10.4161/cib.24511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Hoshino A, et al. Cytosolic p53 inhibits Parkin-mediated mitophagy and promotes mitochondrial dysfunction in the mouse heart. Nat. Commun. 2013;4:2308. doi: 10.1038/ncomms3308. [DOI] [PubMed] [Google Scholar]
- 184.Woodall BP, et al. Parkin does not prevent accelerated cardiac aging in mitochondrial DNA mutator mice. JCI Insight. 2019;5:e127713. doi: 10.1172/jci.insight.127713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Li SJ, Wu TW, Chien MJ, Mersmann HJ, Chen CY. Involvement of pericardial adipose tissue in cardiac fibrosis of dietary-induced obese minipigs- Role of mitochondrial function. Biochim. Biophys. Acta Mol. Cell Biol. Lipids. 2019;1864:957–965. doi: 10.1016/j.bbalip.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 186.Kageyama Y, et al. Parkin-independent mitophagy requires Drp1 and maintains the integrity of mammalian heart and brain. EMBO J. 2014;33:2798–2813. doi: 10.15252/embj.201488658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Wei Y, Chiang WC, Sumpter R, Jr., Mishra P, Levine B. Prohibitin 2 is an inner mitochondrial membrane mitophagy receptor. Cell. 2017;168:224–238 e210. doi: 10.1016/j.cell.2016.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Bhujabal Z, et al. FKBP8 recruits LC3A to mediate Parkin-independent mitophagy. EMBO Rep. 2017;18:947–961. doi: 10.15252/embr.201643147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Murakawa T, et al. Bcl-2-like protein 13 is a mammalian Atg32 homologue that mediates mitophagy and mitochondrial fragmentation. Nat. Commun. 2015;6:7527. doi: 10.1038/ncomms8527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Chen M, et al. Mitophagy receptor FUNDC1 regulates mitochondrial dynamics and mitophagy. Autophagy. 2016;12:689–702. doi: 10.1080/15548627.2016.1151580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Zhang J, Ney PA. Role of BNIP3 and NIX in cell death, autophagy, and mitophagy. Cell Death Differ. 2009;16:939–946. doi: 10.1038/cdd.2009.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Hariharan N, et al. Deacetylation of FoxO by Sirt1 plays an essential role in mediating starvation-induced autophagy in cardiac myocytes. Circ. Res. 2010;107:1470–1482. doi: 10.1161/CIRCRESAHA.110.227371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Hsu CP, Hariharan N, Alcendor RR, Oka S, Sadoshima J. Nicotinamide phosphoribosyltransferase regulates cell survival through autophagy in cardiomyocytes. Autophagy. 2009;5:1229–1231. doi: 10.4161/auto.5.8.10275. [DOI] [PubMed] [Google Scholar]
- 194.Chen Q, Thompson J, Hu Y, Dean J, Lesnefsky EJ. Inhibition of the ubiquitous calpains protects complex I activity and enables improved mitophagy in the heart following ischemia-reperfusion. Am. J. Physiol. Cell Physiol. 2019;317:C910–C921. doi: 10.1152/ajpcell.00190.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Messerer J, et al. Spermidine supplementation influences mitochondrial number and morphology in the heart of aged mice. J. Anat. 2021;242:91–101. doi: 10.1111/joa.13618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Pickles S, Vigie P, Youle RJ. Mitophagy and quality control mechanisms in mitochondrial maintenance. Curr. Biol. 2018;28:R170–R185. doi: 10.1016/j.cub.2018.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Roverato ND, et al. Parkin is an E3 ligase for the ubiquitin-like modifier FAT10, which inhibits Parkin activation and mitophagy. Cell Rep. 2021;34:108857. doi: 10.1016/j.celrep.2021.108857. [DOI] [PubMed] [Google Scholar]
- 198.Sugiura A, McLelland GL, Fon EA, McBride HM. A new pathway for mitochondrial quality control: mitochondrial-derived vesicles. EMBO J. 2014;33:2142–2156. doi: 10.15252/embj.201488104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Jiao H, et al. Mitocytosis, a migrasome-mediated mitochondrial quality-control process. Cell. 2021;184:2896–2910 e2813. doi: 10.1016/j.cell.2021.04.027. [DOI] [PubMed] [Google Scholar]
- 200.Li-Harms X, et al. Mito-protective autophagy is impaired in erythroid cells of aged mtDNA-mutator mice. Blood. 2015;125:162–174. doi: 10.1182/blood-2014-07-586396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Riley JS, et al. Mitochondrial inner membrane permeabilisation enables mtDNA release during apoptosis. EMBO J. 2018;37:e99238. doi: 10.15252/embj.201899238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Pollyea DA, et al. Venetoclax with azacitidine disrupts energy metabolism and targets leukemia stem cells in patients with acute myeloid leukemia. Nat. Med. 2018;24:1859–1866. doi: 10.1038/s41591-018-0233-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Zhao RZ, Jiang S, Zhang L, Yu ZB. Mitochondrial electron transport chain, ROS generation and uncoupling (Review) Int. J. Mol. Med. 2019;44:3–15. doi: 10.3892/ijmm.2019.4188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Laughlin TG, Bayne AN, Trempe JF, Savage DF, Davies KM. Structure of the complex I-like molecule NDH of oxygenic photosynthesis. Nature. 2019;566:411–414. doi: 10.1038/s41586-019-0921-0. [DOI] [PubMed] [Google Scholar]
- 205.McElroy GS, et al. NAD+ regeneration rescues lifespan, but not ataxia, in a mouse model of brain mitochondrial complex I dysfunction. Cell Metab. 2020;32:301–308 e306. doi: 10.1016/j.cmet.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Hur JH, Stork DA, Walker DW. Complex-I-ty in aging. J. Bioenerg. Biomembr. 2014;46:329–335. doi: 10.1007/s10863-014-9553-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Monette JS, et al. (R)-alpha-Lipoic acid treatment restores ceramide balance in aging rat cardiac mitochondria. Pharm. Res. 2011;63:23–29. doi: 10.1016/j.phrs.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Senoo N, et al. Cardiolipin, conformation, and respiratory complex-dependent oligomerization of the major mitochondrial ADP/ATP carrier in yeast. Sci. Adv. 2020;6:eabb0780. doi: 10.1126/sciadv.abb0780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Zeczycki TN, Whelan J, Hayden WT, Brown DA, Shaikh SR. Increasing levels of cardiolipin differentially influence packing of phospholipids found in the mitochondrial inner membrane. Biochem. Biophys. Res. Commun. 2014;450:366–371. doi: 10.1016/j.bbrc.2014.05.133. [DOI] [PubMed] [Google Scholar]
- 210.Takahashi K, Ohsawa I, Shirasawa T, Takahashi M. Optic atrophy 1 mediates coenzyme Q-responsive regulation of respiratory complex IV activity in brain mitochondria. Exp. Gerontol. 2017;98:217–223. doi: 10.1016/j.exger.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 211.Deepa SS, et al. Improved insulin sensitivity associated with reduced mitochondrial complex IV assembly and activity. FASEB J. 2013;27:1371–1380. doi: 10.1096/fj.12-221879. [DOI] [PubMed] [Google Scholar]
- 212.Zhang Q, et al. The mitochondrial unfolded protein response is mediated cell-non-autonomously by retromer-dependent Wnt signaling. Cell. 2018;174:870–883 e817. doi: 10.1016/j.cell.2018.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Martinez-Reyes I, et al. Mitochondrial ubiquinol oxidation is necessary for tumour growth. Nature. 2020;585:288–292. doi: 10.1038/s41586-020-2475-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Li H, et al. Aging-associated mitochondrial DNA mutations alter oxidative phosphorylation machinery and cause mitochondrial dysfunctions. Biochim. Biophys. Acta Mol. Basis Dis. 2017;1863:2266–2273. doi: 10.1016/j.bbadis.2017.05.022. [DOI] [PubMed] [Google Scholar]
- 215.Zhu J, Egawa T, Yeh SR, Yu L, Yu CA. Simultaneous reduction of iron-sulfur protein and cytochrome b(L) during ubiquinol oxidation in cytochrome bc(1) complex. Proc. Natl Acad. Sci. USA. 2007;104:4864–4869. doi: 10.1073/pnas.0607812104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Bararia D, et al. Cathepsin S alterations induce a tumor-promoting immune microenvironment in follicular lymphoma. Cell Rep. 2020;31:107522. doi: 10.1016/j.celrep.2020.107522. [DOI] [PubMed] [Google Scholar]
- 217.Angeli S, et al. The mitochondrial permeability transition pore activates the mitochondrial unfolded protein response and promotes aging. Elife. 2021;10:e63453. doi: 10.7554/eLife.63453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Gatto C, Grandi M, Solaini G, Baracca A, Giorgio V. The F1Fo-ATPase inhibitor protein IF1 in pathophysiology. Front Physiol. 2022;13:917203. doi: 10.3389/fphys.2022.917203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Giorgio V, et al. Dimers of mitochondrial ATP synthase form the permeability transition pore. Proc. Natl Acad. Sci. USA. 2013;110:5887–5892. doi: 10.1073/pnas.1217823110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Wiley CD, et al. Mitochondrial dysfunction induces senescence with a distinct secretory phenotype. Cell Metab. 2016;23:303–314. doi: 10.1016/j.cmet.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Verdin E. NAD(+) in aging, metabolism, and neurodegeneration. Science. 2015;350:1208–1213. doi: 10.1126/science.aac4854. [DOI] [PubMed] [Google Scholar]
- 222.Katsyuba E, Romani M, Hofer D, Auwerx J. NAD(+) homeostasis in health and disease. Nat. Metab. 2020;2:9–31. doi: 10.1038/s42255-019-0161-5. [DOI] [PubMed] [Google Scholar]
- 223.Abdellatif M, Sedej S, Kroemer G. NAD(+) metabolism in cardiac health, aging, and disease. Circulation. 2021;144:1795–1817. doi: 10.1161/CIRCULATIONAHA.121.056589. [DOI] [PubMed] [Google Scholar]
- 224.Bogan KL, Brenner C. Nicotinic acid, nicotinamide, and nicotinamide riboside: a molecular evaluation of NAD+ precursor vitamins in human nutrition. Annu. Rev. Nutr. 2008;28:115–130. doi: 10.1146/annurev.nutr.28.061807.155443. [DOI] [PubMed] [Google Scholar]
- 225.Fleury H, et al. Exploiting interconnected synthetic lethal interactions between PARP inhibition and cancer cell reversible senescence. Nat. Commun. 2019;10:2556. doi: 10.1038/s41467-019-10460-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Ohanna M, et al. Senescent cells develop a PARP-1 and nuclear factor-{kappa}B-associated secretome (PNAS) Genes Dev. 2011;25:1245–1261. doi: 10.1101/gad.625811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Nassour J, et al. Defective DNA single-strand break repair is responsible for senescence and neoplastic escape of epithelial cells. Nat. Commun. 2016;7:10399. doi: 10.1038/ncomms10399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Radovits T, et al. Single dose treatment with PARP-inhibitor INO-1001 improves aging-associated cardiac and vascular dysfunction. Exp. Gerontol. 2007;42:676–685. doi: 10.1016/j.exger.2007.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Lauritzen KH, et al. Instability in NAD(+) metabolism leads to impaired cardiac mitochondrial function and communication. Elife. 2021;10:e59828. doi: 10.7554/eLife.59828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Xu C, et al. SIRT1 is downregulated by autophagy in senescence and ageing. Nat. Cell Biol. 2020;22:1170–1179. doi: 10.1038/s41556-020-00579-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Bonkowski MS, Sinclair DA. Slowing ageing by design: the rise of NAD(+) and sirtuin-activating compounds. Nat. Rev. Mol. Cell Biol. 2016;17:679–690. doi: 10.1038/nrm.2016.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Covarrubias AJ, Perrone R, Grozio A, Verdin E. NAD(+) metabolism and its roles in cellular processes during ageing. Nat. Rev. Mol. Cell Biol. 2021;22:119–141. doi: 10.1038/s41580-020-00313-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Pillai VB, Samant S, Hund S, Gupta M, Gupta MP. The nuclear sirtuin SIRT6 protects the heart from developing aging-associated myocyte senescence and cardiac hypertrophy. Aging. 2021;13:12334–12358. doi: 10.18632/aging.203027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Li X, et al. SIRT6 protects against myocardial ischemia-reperfusion injury by attenuating aging-related CHMP2B accumulation. J. Cardiovasc. Transl. Res. 2022;15:740–753. doi: 10.1007/s12265-021-10184-y. [DOI] [PubMed] [Google Scholar]
- 235.Ren SC, et al. SIRT6 in vascular diseases, from bench to bedside. Aging Dis. 2022;13:1015–1029. doi: 10.14336/AD.2021.1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Chi C, et al. Exerkine fibronectin type-III domain-containing protein 5/irisin-enriched extracellular vesicles delay vascular ageing by increasing SIRT6 stability. Eur. Heart J. 2022;43:4579–4595. doi: 10.1093/eurheartj/ehac431. [DOI] [PubMed] [Google Scholar]
- 237.Simon M, et al. LINE1 derepression in aged wild-type and SIRT6-deficient mice drives inflammation. Cell Metab. 2019;29:871–885 e875. doi: 10.1016/j.cmet.2019.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.De Cecco M, et al. L1 drives IFN in senescent cells and promotes age-associated inflammation. Nature. 2019;566:73–78. doi: 10.1038/s41586-018-0784-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.D’Onofrio N, Servillo L, Balestrieri ML. SIRT1 and SIRT6 signaling pathways in cardiovascular disease protection. Antioxid. Redox Signal. 2018;28:711–732. doi: 10.1089/ars.2017.7178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Grootaert MOJ, Finigan A, Figg NL, Uryga AK, Bennett MR. SIRT6 protects smooth muscle cells from senescence and reduces atherosclerosis. Circ. Res. 2021;128:474–491. doi: 10.1161/CIRCRESAHA.120.318353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Ma XR, et al. Restoring nuclear entry of Sirtuin 2 in oligodendrocyte progenitor cells promotes remyelination during ageing. Nat. Commun. 2022;13:1225. doi: 10.1038/s41467-022-28844-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Baker DJ, et al. Increased expression of BubR1 protects against aneuploidy and cancer and extends healthy lifespan. Nat. Cell Biol. 2013;15:96–102. doi: 10.1038/ncb2643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Tang X, et al. SIRT2 acts as a cardioprotective deacetylase in pathological cardiac hypertrophy. Circulation. 2017;136:2051–2067. doi: 10.1161/CIRCULATIONAHA.117.028728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Nacarelli T, et al. NAD(+) metabolism governs the proinflammatory senescence-associated secretome. Nat. Cell Biol. 2019;21:397–407. doi: 10.1038/s41556-019-0287-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Wiley CD, Campisi J. From ancient pathways to aging cells-connecting metabolism and cellular senescence. Cell Metab. 2016;23:1013–1021. doi: 10.1016/j.cmet.2016.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Garten A, et al. Physiological and pathophysiological roles of NAMPT and NAD metabolism. Nat. Rev. Endocrinol. 2015;11:535–546. doi: 10.1038/nrendo.2015.117. [DOI] [PubMed] [Google Scholar]
- 247.Hsu CP, Yamamoto T, Oka S, Sadoshima J. The function of nicotinamide phosphoribosyltransferase in the heart. DNA Repair. 2014;23:64–68. doi: 10.1016/j.dnarep.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Hsu CP, Oka S, Shao D, Hariharan N, Sadoshima J. Nicotinamide phosphoribosyltransferase regulates cell survival through NAD+ synthesis in cardiac myocytes. Circ. Res. 2009;105:481–491. doi: 10.1161/CIRCRESAHA.109.203703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Shirakabe A, Ikeda Y, Sciarretta S, Zablocki DK, Sadoshima J. Aging and autophagy in the heart. Circ. Res. 2016;118:1563–1576. doi: 10.1161/CIRCRESAHA.116.307474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Han D, Antunes F, Canali R, Rettori D, Cadenas E. Voltage-dependent anion channels control the release of the superoxide anion from mitochondria to cytosol. J. Biol. Chem. 2003;278:5557–5563. doi: 10.1074/jbc.M210269200. [DOI] [PubMed] [Google Scholar]
- 251.Paillard M, et al. Depressing mitochondria-reticulum interactions protects cardiomyocytes from lethal hypoxia-reoxygenation injury. Circulation. 2013;128:1555–1565. doi: 10.1161/CIRCULATIONAHA.113.001225. [DOI] [PubMed] [Google Scholar]
- 252.Ochoa CD, Wu RF, Terada LS. ROS signaling and ER stress in cardiovascular disease. Mol. Asp. Med. 2018;63:18–29. doi: 10.1016/j.mam.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Zandalinas SI, Mittler R. ROS-induced ROS release in plant and animal cells. Free Radic. Biol. Med. 2018;122:21–27. doi: 10.1016/j.freeradbiomed.2017.11.028. [DOI] [PubMed] [Google Scholar]
- 254.Suh JH, Heath SH, Hagen TM. Two subpopulations of mitochondria in the aging rat heart display heterogenous levels of oxidative stress. Free Radic. Biol. Med. 2003;35:1064–1072. doi: 10.1016/S0891-5849(03)00468-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Gao XH, et al. Aging-dependent changes in rat heart mitochondrial glutaredoxins-Implications for redox regulation. Redox Biol. 2013;1:586–598. doi: 10.1016/j.redox.2013.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Wang L, et al. Oxidative stress in oocyte aging and female reproduction. J. Cell Physiol. 2021;236:7966–7983. doi: 10.1002/jcp.30468. [DOI] [PubMed] [Google Scholar]
- 257.Szlezak D, Hutsch T, Ufnal M, Wrobel M. Heart and kidney H2S production is reduced in hypertensive and older rats. Biochimie. 2022;199:130–138. doi: 10.1016/j.biochi.2022.04.013. [DOI] [PubMed] [Google Scholar]
- 258.Abdel-Rahman EA, et al. Sleep/wake calcium dynamics, respiratory function, and ROS production in cardiac mitochondria. J. Adv. Res. 2021;31:35–47. doi: 10.1016/j.jare.2021.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Velarde MC, Flynn JM, Day NU, Melov S, Campisi J. Mitochondrial oxidative stress caused by Sod2 deficiency promotes cellular senescence and aging phenotypes in the skin. Aging. 2012;4:3–12. doi: 10.18632/aging.100423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Kwon MJ, Lee KY, Lee HW, Kim JH, Kim TY. SOD3 variant, R213G, altered SOD3 function, leading to ROS-mediated inflammation and damage in multiple organs of premature aging mice. Antioxid. Redox Signal. 2015;23:985–999. doi: 10.1089/ars.2014.6035. [DOI] [PubMed] [Google Scholar]
- 261.Vizioli MG, et al. Mitochondria-to-nucleus retrograde signaling drives formation of cytoplasmic chromatin and inflammation in senescence. Genes Dev. 2020;34:428–445. doi: 10.1101/gad.331272.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Crewe C, et al. Extracellular vesicle-based interorgan transport of mitochondria from energetically stressed adipocytes. Cell Metab. 2021;33:1853–1868 e1811. doi: 10.1016/j.cmet.2021.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Yuko AE, et al. LIN28a induced metabolic and redox regulation promotes cardiac cell survival in the heart after ischemic injury. Redox Biol. 2021;47:102162. doi: 10.1016/j.redox.2021.102162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Janbandhu V, et al. Hif-1a suppresses ROS-induced proliferation of cardiac fibroblasts following myocardial infarction. Cell Stem Cell. 2022;29:281–297 e212. doi: 10.1016/j.stem.2021.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Wu J, et al. TNF antagonist sensitizes synovial fibroblasts to ferroptotic cell death in collagen-induced arthritis mouse models. Nat. Commun. 2022;13:676. doi: 10.1038/s41467-021-27948-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Bernard M, et al. Autophagy drives fibroblast senescence through MTORC2 regulation. Autophagy. 2020;16:2004–2016. doi: 10.1080/15548627.2020.1713640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Gong Y, Wang N, Liu N, Dong H. Lipid peroxidation and GPX4 inhibition are common causes for myofibroblast differentiation and ferroptosis. DNA Cell Biol. 2019;38:725–733. doi: 10.1089/dna.2018.4541. [DOI] [PubMed] [Google Scholar]
- 268.Chouchani ET, et al. Ischaemic accumulation of succinate controls reperfusion injury through mitochondrial ROS. Nature. 2014;515:431–435. doi: 10.1038/nature13909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Huang YT, et al. ROS- and HIF1alpha-dependent IGFBP3 upregulation blocks IGF1 survival signaling and thereby mediates high-glucose-induced cardiomyocyte apoptosis. J. Cell Physiol. 2019;234:13557–13570. doi: 10.1002/jcp.28034. [DOI] [PubMed] [Google Scholar]
- 270.Steenman M, Lande G. Cardiac aging and heart disease in humans. Biophys. Rev. 2017;9:131–137. doi: 10.1007/s12551-017-0255-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Kujoth GC, et al. Mitochondrial DNA mutations, oxidative stress, and apoptosis in mammalian aging. Science. 2005;309:481–484. doi: 10.1126/science.1112125. [DOI] [PubMed] [Google Scholar]
- 272.Khaidakov M, Heflich RH, Manjanatha MG, Myers MB, Aidoo A. Accumulation of point mutations in mitochondrial DNA of aging mice. Mutat. Res. 2003;526:1–7. doi: 10.1016/S0027-5107(03)00010-1. [DOI] [PubMed] [Google Scholar]
- 273.Sithara T, Drosatos K. Metabolic complications in cardiac aging. Front Physiol. 2021;12:669497. doi: 10.3389/fphys.2021.669497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Weinberg SE, et al. Mitochondrial complex III is essential for suppressive function of regulatory T cells. Nature. 2019;565:495–499. doi: 10.1038/s41586-018-0846-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Shu L, et al. ATAD3B is a mitophagy receptor mediating clearance of oxidative stress-induced damaged mitochondrial DNA. EMBO J. 2021;40:e106283. doi: 10.15252/embj.2020106283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Puente BN, et al. The oxygen-rich postnatal environment induces cardiomyocyte cell-cycle arrest through DNA damage response. Cell. 2014;157:565–579. doi: 10.1016/j.cell.2014.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Trifunovic A, et al. Premature ageing in mice expressing defective mitochondrial DNA polymerase. Nature. 2004;429:417–423. doi: 10.1038/nature02517. [DOI] [PubMed] [Google Scholar]
- 278.Maclaine KD, Stebbings KA, Llano DA, Rhodes JS. Voluntary wheel running has no impact on brain and liver mitochondrial DNA copy number or mutation measures in the PolG mouse model of aging. PLoS ONE. 2020;15:e0226860. doi: 10.1371/journal.pone.0226860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Gorr MW, et al. Molecular signature of cardiac remodeling associated with Polymerase Gamma mutation. Life Sci. 2022;298:120469. doi: 10.1016/j.lfs.2022.120469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Edgar D, et al. Random point mutations with major effects on protein-coding genes are the driving force behind premature aging in mtDNA mutator mice. Cell Metab. 2009;10:131–138. doi: 10.1016/j.cmet.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 281.Nekhaeva E, et al. Clonally expanded mtDNA point mutations are abundant in individual cells of human tissues. Proc. Natl Acad. Sci. USA. 2002;99:5521–5526. doi: 10.1073/pnas.072670199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Kim J, et al. VDAC oligomers form mitochondrial pores to release mtDNA fragments and promote lupus-like disease. Science. 2019;366:1531–1536. doi: 10.1126/science.aav4011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Jauhari A, et al. Melatonin inhibits cytosolic mitochondrial DNA-induced neuroinflammatory signaling in accelerated aging and neurodegeneration. J. Clin. Invest. 2020;130:3124–3136. doi: 10.1172/JCI135026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Xu Y, et al. Extracellular mitochondrial components and effects on cardiovascular disease. DNA Cell Biol. 2021;40:1131–1143. doi: 10.1089/dna.2021.0087. [DOI] [PubMed] [Google Scholar]
- 285.Nadon NL, Strong R, Miller RA, Harrison DE. NIA interventions testing program: investigating putative aging intervention agents in a genetically heterogeneous mouse model. EBioMedicine. 2017;21:3–4. doi: 10.1016/j.ebiom.2016.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Weisel FJ, et al. Germinal center B cells selectively oxidize fatty acids for energy while conducting minimal glycolysis. Nat. Immunol. 2020;21:331–342. doi: 10.1038/s41590-020-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Tardo-Dino PE, et al. The effect of a physiological increase in temperature on mitochondrial fatty acid oxidation in rat myofibers. J. Appl Physiol. 2019;127:312–319. doi: 10.1152/japplphysiol.00652.2018. [DOI] [PubMed] [Google Scholar]
- 288.Chew EY, et al. Effect of omega-3 fatty acids, lutein/zeaxanthin, or other nutrient supplementation on cognitive function: the AREDS2 randomized clinical trial. JAMA. 2015;314:791–801. doi: 10.1001/jama.2015.9677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Age-Related Eye Disease Study 2 Research, G. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA. 2013;309:2005–2015. doi: 10.1001/jama.2013.4997. [DOI] [PubMed] [Google Scholar]
- 290.Back M. Omega-3 fatty acids in atherosclerosis and coronary artery disease. Future Sci. OA. 2017;3:FSO236. doi: 10.4155/fsoa-2017-0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Satizabal CL, et al. Association of red blood cell omega-3 fatty acids with MRI markers and cognitive function in midlife: the framingham heart study. Neurology. 2022;99:e2572–82. doi: 10.1212/WNL.0000000000201296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Saeedi Saravi SS, et al. Lifelong dietary omega-3 fatty acid suppresses thrombotic potential through gut microbiota alteration in aged mice. iScience. 2021;24:102897. doi: 10.1016/j.isci.2021.102897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Marklund M, et al. Biomarkers of dietary omega-6 fatty acids and incident cardiovascular disease and mortality. Circulation. 2019;139:2422–2436. doi: 10.1161/CIRCULATIONAHA.118.038908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Cook WS, Yeldandi AV, Rao MS, Hashimoto T, Reddy JK. Less extrahepatic induction of fatty acid beta-oxidation enzymes by PPAR alpha. Biochem. Biophys. Res. Commun. 2000;278:250–257. doi: 10.1006/bbrc.2000.3739. [DOI] [PubMed] [Google Scholar]
- 295.Tortosa-Caparros E, Navas-Carrillo D, Marin F, Orenes-Pinero E. Anti-inflammatory effects of omega 3 and omega 6 polyunsaturated fatty acids in cardiovascular disease and metabolic syndrome. Crit. Rev. Food Sci. Nutr. 2017;57:3421–3429. doi: 10.1080/10408398.2015.1126549. [DOI] [PubMed] [Google Scholar]
- 296.Brown TJ, et al. Omega-3, omega-6, and total dietary polyunsaturated fat for prevention and treatment of type 2 diabetes mellitus: systematic review and meta-analysis of randomised controlled trials. BMJ. 2019;366:l4697. doi: 10.1136/bmj.l4697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Oh DY, et al. GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell. 2010;142:687–698. doi: 10.1016/j.cell.2010.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Deng Y, et al. Targeting mitochondria-inflammation circuit by beta-hydroxybutyrate mitigates HFpEF. Circ. Res. 2021;128:232–245. doi: 10.1161/CIRCRESAHA.120.317933. [DOI] [PubMed] [Google Scholar]
- 299.Chong CR, Sallustio B, Horowitz JD. Drugs that affect cardiac metabolism: focus on perhexiline. Cardiovasc Drugs Ther. 2016;30:399–405. doi: 10.1007/s10557-016-6664-3. [DOI] [PubMed] [Google Scholar]
- 300.Davogustto G, Taegtmeyer H. Perhexiline, cardiac energetics, and heart failure: lessons from the first law of thermodynamics. JACC Heart Fail. 2015;3:659–660. doi: 10.1016/j.jchf.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 301.Xie H, Xu G, Aa J, Gu S, Gao Y. Modulation of perturbed cardiac metabolism in rats under high-altitude hypoxia by combination treatment with L-carnitine and trimetazidine. Front. Physiol. 2021;12:671161. doi: 10.3389/fphys.2021.671161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Ferrari R, et al. Efficacy and safety of trimetazidine after percutaneous coronary intervention (ATPCI): a randomised, double-blind, placebo-controlled trial. Lancet. 2020;396:830–838. doi: 10.1016/S0140-6736(20)31790-6. [DOI] [PubMed] [Google Scholar]
- 303.Zhang X, et al. Trimetazidine and lcarnitine prevent heart aging and cardiac metabolic impairment in rats via regulating cardiac metabolic substrates. Exp. Gerontol. 2019;119:120–127. doi: 10.1016/j.exger.2018.12.019. [DOI] [PubMed] [Google Scholar]
- 304.Lin JQ, Wang JX, Yu S, Fu SH, Zhang YJ. Newly discovered molecules associated with trimetazidine on improvement of skeletal muscle function in aging: evidence from myoblasts and mice. Exp. Gerontol. 2022;161:111733. doi: 10.1016/j.exger.2022.111733. [DOI] [PubMed] [Google Scholar]
- 305.Rieg T, Vallon V. Development of SGLT1 and SGLT2 inhibitors. Diabetologia. 2018;61:2079–2086. doi: 10.1007/s00125-018-4654-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Zelniker TA, Braunwald E. Mechanisms of cardiorenal effects of sodium-glucose cotransporter 2 inhibitors: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2020;75:422–434. doi: 10.1016/j.jacc.2019.11.031. [DOI] [PubMed] [Google Scholar]
- 307.Liu L, Ni YQ, Zhan JK, Liu YS. The role of SGLT2 inhibitors in vascular aging. Aging Dis. 2021;12:1323–1336. doi: 10.14336/AD.2020.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Mudaliar S, Alloju S, Henry RR. Can a shift in fuel energetics explain the beneficial cardiorenal outcomes in the EMPA-REG OUTCOME study? A unifying hypothesis. Diabetes Care. 2016;39:1115–1122. doi: 10.2337/dc16-0542. [DOI] [PubMed] [Google Scholar]
- 309.Olgar Y, et al. Ageing-associated increase in SGLT2 disrupts mitochondrial/sarcoplasmic reticulum Ca(2+) homeostasis and promotes cardiac dysfunction. J. Cell Mol. Med. 2020;24:8567–8578. doi: 10.1111/jcmm.15483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Li Z, et al. Systemic GLP-1R agonist treatment reverses mouse glial and neurovascular cell transcriptomic aging signatures in a genome-wide manner. Commun. Biol. 2021;4:656. doi: 10.1038/s42003-021-02208-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Mengozzi A, et al. Targeting SIRT1 rescues age- and obesity-induced microvascular dysfunction in ex vivo human vessels. Circ. Res. 2022;131:476–491. doi: 10.1161/CIRCRESAHA.122.320888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Mercken EM, et al. SRT2104 extends survival of male mice on a standard diet and preserves bone and muscle mass. Aging Cell. 2014;13:787–796. doi: 10.1111/acel.12220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Kane AE, Sinclair DA. Sirtuins and NAD(+) in the development and treatment of metabolic and cardiovascular diseases. Circ. Res. 2018;123:868–885. doi: 10.1161/CIRCRESAHA.118.312498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Li H, et al. Ferulic acid supplementation increases lifespan and stress resistance via insulin/IGF-1 signaling pathway in C. elegans. Int. J. Mol. Sci. 2021;22:4279. doi: 10.3390/ijms22084279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Kerner J, et al. Acetyl-L-carnitine increases mitochondrial protein acetylation in the aged rat heart. Mech. Ageing Dev. 2015;145:39–50. doi: 10.1016/j.mad.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Kulkarni AS, Gubbi S, Barzilai N. Benefits of metformin in attenuating the hallmarks of aging. Cell Metab. 2020;32:15–30. doi: 10.1016/j.cmet.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Barzilai N, Crandall JP, Kritchevsky SB, Espeland MA. Metformin as a tool to target aging. Cell Metab. 2016;23:1060–1065. doi: 10.1016/j.cmet.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Justice JN, et al. A framework for selection of blood-based biomarkers for geroscience-guided clinical trials: report from the TAME Biomarkers Workgroup. Geroscience. 2018;40:419–436. doi: 10.1007/s11357-018-0042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Bannister CA, et al. Can people with type 2 diabetes live longer than those without? A comparison of mortality in people initiated with metformin or sulphonylurea monotherapy and matched, non-diabetic controls. Diabetes Obes. Metab. 2014;16:1165–1173. doi: 10.1111/dom.12354. [DOI] [PubMed] [Google Scholar]
- 320.Liparulo I, et al. Coenzyme Q biosynthesis inhibition induces HIF-1alpha stabilization and metabolic switch toward glycolysis. FEBS J. 2021;288:1956–1974. doi: 10.1111/febs.15561. [DOI] [PubMed] [Google Scholar]
- 321.Raizner AE, Quinones MA. Coenzyme Q10 for patients with cardiovascular disease: JACC focus seminar. J. Am. Coll. Cardiol. 2021;77:609–619. doi: 10.1016/j.jacc.2020.12.009. [DOI] [PubMed] [Google Scholar]
- 322.Folkers K, Wolaniuk J, Simonsen R, Morishita M, Vadhanavikit S. Biochemical rationale and the cardiac response of patients with muscle disease to therapy with coenzyme Q10. Proc. Natl Acad. Sci. USA. 1985;82:4513–4516. doi: 10.1073/pnas.82.13.4513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Lass A, Kwong L, Sohal RS. Mitochondrial coenzyme Q content and aging. Biofactors. 1999;9:199–205. doi: 10.1002/biof.5520090215. [DOI] [PubMed] [Google Scholar]
- 324.Mortensen SA, et al. The effect of coenzyme Q10 on morbidity and mortality in chronic heart failure: results from Q-SYMBIO: a randomized double-blind trial. JACC Heart Fail. 2014;2:641–649. doi: 10.1016/j.jchf.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 325.Sharma A, Fonarow GC, Butler J, Ezekowitz JA, Felker GM. Coenzyme Q10 and heart failure: a state-of-the-art review. Circ. Heart Fail. 2016;9:e002639. doi: 10.1161/CIRCHEARTFAILURE.115.002639. [DOI] [PubMed] [Google Scholar]
- 326.Ochoa JJ, Quiles JL, Huertas JR, Mataix J. Coenzyme Q10 protects from aging-related oxidative stress and improves mitochondrial function in heart of rats fed a polyunsaturated fatty acid (PUFA)-rich diet. J. Gerontol. A Biol. Sci. Med. Sci. 2005;60:970–975. doi: 10.1093/gerona/60.8.970. [DOI] [PubMed] [Google Scholar]
- 327.Hargreaves IP, Mantle D. Coenzyme Q10 supplementation in fibrosis and aging. Adv. Exp. Med. Biol. 2019;1178:103–112. doi: 10.1007/978-3-030-25650-0_6. [DOI] [PubMed] [Google Scholar]
- 328.Smith RA, Hartley RC, Cocheme HM, Murphy MP. Mitochondrial pharmacology. Trends Pharm. Sci. 2012;33:341–352. doi: 10.1016/j.tips.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 329.Goh KY, et al. Mitoquinone ameliorates pressure overload-induced cardiac fibrosis and left ventricular dysfunction in mice. Redox Biol. 2019;21:101100. doi: 10.1016/j.redox.2019.101100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Pak O, et al. Impact of the mitochondria-targeted antioxidant MitoQ on hypoxia-induced pulmonary hypertension. Eur. Respir. J. 2018;51:1701656. doi: 10.1183/13993003.01024-2017. [DOI] [PubMed] [Google Scholar]
- 331.Harrison DE, et al. Rapamycin fed late in life extends lifespan in genetically heterogeneous mice. Nature. 2009;460:392–395. doi: 10.1038/nature08221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Mannick JB, et al. mTOR inhibition improves immune function in the elderly. Sci. Transl. Med. 2014;6:268ra179. doi: 10.1126/scitranslmed.3009892. [DOI] [PubMed] [Google Scholar]
- 333.Hurez V, et al. Chronic mTOR inhibition in mice with rapamycin alters T, B, myeloid, and innate lymphoid cells and gut flora and prolongs life of immune-deficient mice. Aging Cell. 2015;14:945–956. doi: 10.1111/acel.12380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.He C, et al. Exercise-induced BCL2-regulated autophagy is required for muscle glucose homeostasis. Nature. 2012;481:511–515. doi: 10.1038/nature10758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Finkel T, Deng CX, Mostoslavsky R. Recent progress in the biology and physiology of sirtuins. Nature. 2009;460:587–591. doi: 10.1038/nature08197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Feng W, et al. Alginate oligosaccharide alleviates D-galactose-induced cardiac ageing via regulating myocardial mitochondria function and integrity in mice. J. Cell Mol. Med. 2021;25:7157–7168. doi: 10.1111/jcmm.16746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Chiao YA, et al. Late-life restoration of mitochondrial function reverses cardiac dysfunction in old mice. Elife. 2020;9:e55513. doi: 10.7554/eLife.55513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Xu M, et al. Senolytics improve physical function and increase lifespan in old age. Nat. Med. 2018;24:1246–1256. doi: 10.1038/s41591-018-0092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Chang J, et al. Clearance of senescent cells by ABT263 rejuvenates aged hematopoietic stem cells in mice. Nat. Med. 2016;22:78–83. doi: 10.1038/nm.4010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Campisi J, et al. From discoveries in ageing research to therapeutics for healthy ageing. Nature. 2019;571:183–192. doi: 10.1038/s41586-019-1365-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Shinmura K. Effects of caloric restriction on cardiac oxidative stress and mitochondrial bioenergetics: potential role of cardiac sirtuins. Oxid. Med. Cell Longev. 2013;2013:528935. doi: 10.1155/2013/528935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Hatori M, et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 2012;15:848–860. doi: 10.1016/j.cmet.2012.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Longo VD, Mattson MP. Fasting: molecular mechanisms and clinical applications. Cell Metab. 2014;19:181–192. doi: 10.1016/j.cmet.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Brandhorst S, et al. A periodic diet that mimics fasting promotes multi-system regeneration, enhanced cognitive performance, and healthspan. Cell Metab. 2015;22:86–99. doi: 10.1016/j.cmet.2015.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Duggal NA, Pollock RD, Lazarus NR, Harridge S, Lord JM. Major features of immunesenescence, including reduced thymic output, are ameliorated by high levels of physical activity in adulthood. Aging Cell. 2018;17:e12750. doi: 10.1111/acel.12750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Parry-Williams G, Sharma S. The effects of endurance exercise on the heart: panacea or poison? Nat. Rev. Cardiol. 2020;17:402–412. doi: 10.1038/s41569-020-0354-3. [DOI] [PubMed] [Google Scholar]
- 347.Pacifici F, et al. Proposed tandem effect of physical activity and sirtuin 1 and 3 activation in regulating glucose homeostasis. Int. J. Mol. Sci. 2019;20:4748. doi: 10.3390/ijms20194748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Munoz A, et al. Physical exercise improves aging-related changes in angiotensin, IGF-1, SIRT1, SIRT3, and VEGF in the substantia nigra. J. Gerontol. A Biol. Sci. Med. Sci. 2018;73:1594–1601. doi: 10.1093/gerona/gly072. [DOI] [PubMed] [Google Scholar]
- 349.Kwak HB, et al. MnSOD overexpression reduces fibrosis and pro-apoptotic signaling in the aging mouse heart. J. Gerontol. A Biol. Sci. Med. Sci. 2015;70:533–544. doi: 10.1093/gerona/glu090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Kim S, et al. Enhancement of gene editing and base editing with therapeutic ribonucleoproteins through in vivo delivery based on absorptive silica nanoconstruct. Adv. Healthc. Mater. 2022;12:e2201825. doi: 10.1002/adhm.202201825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Rurik JG, et al. CAR T cells produced in vivo to treat cardiac injury. Science. 2022;375:91–96. doi: 10.1126/science.abm0594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Villanueva MT. Repairing cardiac injury with transient CAR-T cells. Nat. Rev. Drug Disco. 2022;21:179. doi: 10.1038/d41573-022-00024-2. [DOI] [PubMed] [Google Scholar]
- 353.Martinez P, Blasco MA. Heart-breaking telomeres. Circ. Res. 2018;123:787–802. doi: 10.1161/CIRCRESAHA.118.312202. [DOI] [PubMed] [Google Scholar]
- 354.Ale-Agha N, et al. Mitochondrial telomerase reverse transcriptase protects from myocardial ischemia/reperfusion injury by improving complex I composition and function. Circulation. 2021;144:1876–1890. doi: 10.1161/CIRCULATIONAHA.120.051923. [DOI] [PubMed] [Google Scholar]
- 355.Madonna R, De Caterina R, Willerson JT, Geng YJ. Biologic function and clinical potential of telomerase and associated proteins in cardiovascular tissue repair and regeneration. Eur. Heart J. 2011;32:1190–1196. doi: 10.1093/eurheartj/ehq450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Liao CY, Rikke BA, Johnson TE, Diaz V, Nelson JF. Genetic variation in the murine lifespan response to dietary restriction: from life extension to life shortening. Aging Cell. 2010;9:92–95. doi: 10.1111/j.1474-9726.2009.00533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Harper JM, Leathers CW, Austad SN. Does caloric restriction extend life in wild mice? Aging Cell. 2006;5:441–449. doi: 10.1111/j.1474-9726.2006.00236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Mattison JA, et al. Impact of caloric restriction on health and survival in rhesus monkeys from the NIA study. Nature. 2012;489:318–321. doi: 10.1038/nature11432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Munoz, V. R. et al. Short-term physical exercise controls age-related hyperinsulinemia and improves hepatic metabolism in aged rodents. J. Endocrinol. Invest. (2022). [DOI] [PubMed]