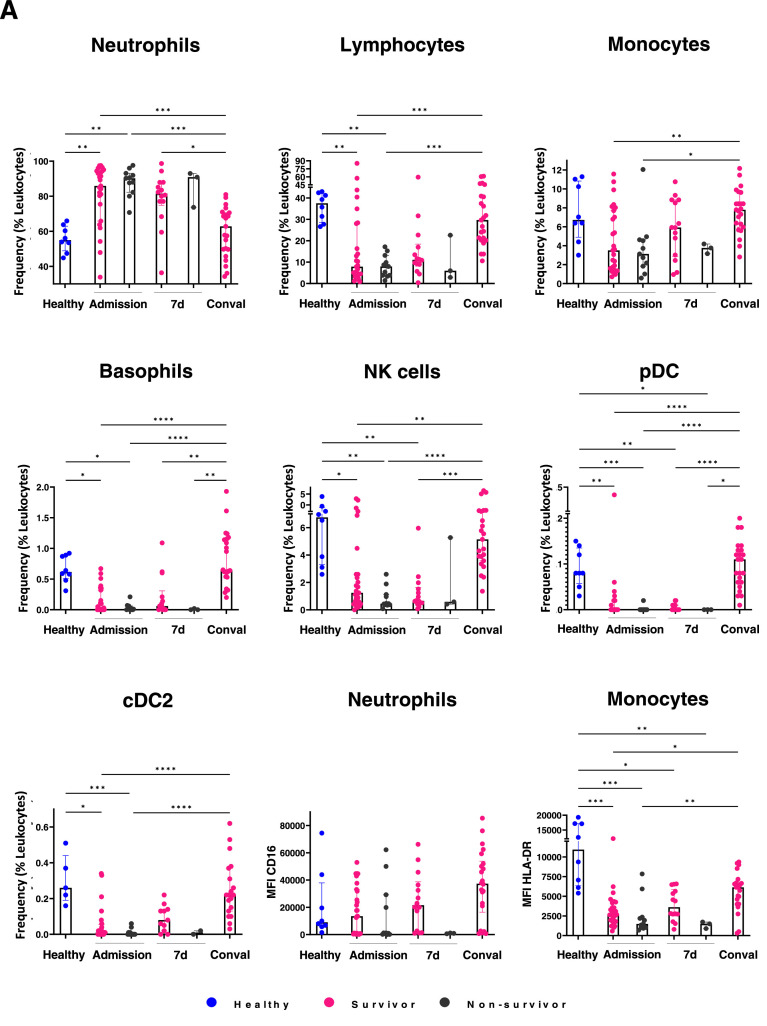
Figure 4.
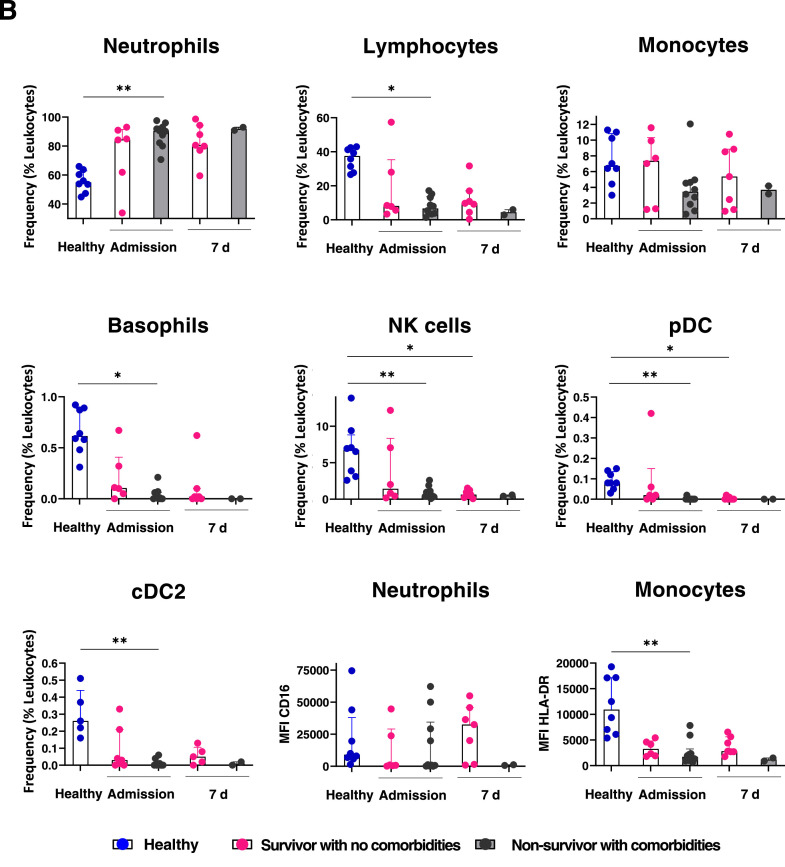
Poor outcome in middle–aged patients is related to myeloid emergency hematopoiesis at the expense of innate immune response effector cells. Immune cell populations were evaluated in middle–aged patients by flow cytometry at admission, 7 days and 4 weeks later. In contrast to survivor patients, significant decrease in lymphocytes, monocytes, NK cells, pDC, CD11c+ DC (cDC2), basophils and functional neutrophils and monocytes is observed in non–survivors. CD16 and HLA–DR expression levels in neutrophils and monocytes, respectively, in poor outcome patients are shown A. Chronic comorbidities contribute to the pathogenic myeloid emergency hematopoiesis along to a defective lymphoid emergency compartment in middle aged COVID–19 patients. Hematological cell frequencies and CD16 and HLA–DR expression levels in neutrophils and monocytes, respectively, in COVID–19 survivors with no comorbidities are compared to their counterpart in non–survivors with comorbidities, at admission and upon 7 days of hospitalization. Healthy donor values are shown as control. Myeloid– and lymphoid– lineage cells related to emergency hematopoiesis are shown in B. MFI, median fluorescence intensity; d, days; Conval, convalescence.