Abstract
PURPOSE OF REVIEW
Cardiovascular disease (CVD) is the leading cause of mortality in adult women in the United States, yet CVD is underrecognized in women. Disparities in care are further pronounced in women of racial/ethnic minority backgrounds. In this review, we discuss the role of social media (SoMe) as a tool to i) promote women’s cardiovascular (CV) health and ii) address and potentially reduce gaps in care, particularly in general cardiology (targeting atherosclerotic cardiovascular disease), cardio-oncology, and cardio-obstetrics. We also briefly discuss women’s CV health as a common, although not unique, focus of women in cardiology on SoMe.
RECENT FINDINGS
Studies have suggested the utility of social media to help advance subspecialties of cardiology. Leaders within general cardiology, cardio-oncology, and cardio-obstetrics have curated social media strategies to advance their respective fields and call attention to cardiovascular health disparities in female populations and racial/ethnic minorities. In addition to these types of uses, women in cardiology also frequently use SoMe to encourage a career in cardiology and to share experiences, challenges, and resources for support and career advancement as healthcare professionals; men in cardiology and especially those who are allies for sex and racial/ethnic minorities also use SoMe for these means.
SUMMARY
Herein, we highlight the role and myriad applications of social media in the promotion of women’s cardiovascular health. We discuss five primary roles of social media: increasing public awareness, disseminating medical literature in a rapid and accessible fashion, facilitating professional networking, serving as a platform for medical conferences, and empowering patients. These core strategies are discussed through the lens of general cardiology, cardio-oncology, and cardio-obstetrics. We also demonstrate how these applications can be leveraged to increase representation of women in cardiology, also supporting an increased focus on women’s cardiovascular health.
Keywords: Social Media, Women in Cardiology, Disparity, Women’s Cardiovascular Health
INTRODUCTION
Cardiovascular disease (CVD) is the leading cause of death for adult women in the United States.[1] Despite advancements in management, CVD remains underdiagnosed and undertreated in women compared to men, a disparity that is even wider for women of racial minority backgrounds.[1, 2] The reasons behind these disparities are vast, though they are generally attributable to a complex interplay between biological and social factors that are further exacerbated by structural racism, bias regarding women at the patient and provider level, and the under-recognition of emerging sex-specific cardiovascular (CV) risk factors.[3–7] Promoting diversity, equity, and inclusion related to women’s CV health and women in cardiology (WIC) are essential to addressing these disparities.
In an increasingly interconnected world, social media (SoMe) has been utilized to highlight women’s CV health, health disparities, and women in cardiology. SoMe is an umbrella term that encompasses multiple online platforms that allow users to create and share brief content.[8] Many medical specialties, including cardiology, have used SoMe to address lack of awareness and advance benefits of online presence for their specific fields.[9–14] Cardio-oncology and cardio-obstetrics are two such examples.[9, 10, 15]
The ways in which SoMe has been leveraged to impact the cardiovascular health of women have been described.[16–24] The rise of some subspecialities within cardiology with an emphasis on women’s CV health—such as cardio-oncology and cardio-obstetrics—have also resulted in an exponential increase in the utilization of SoMe for the promotion of awareness, education, research, and networking opportunities within these fields.[9, 15, 16, 25, 26] Despite wide use, previous analyses focused on the use of SoMe within these specific subspecialties of cardiology, or as a tool to promote WIC.[9, 10, 12, 15, 25]
In this review, we present known and potential applications of SoMe in promoting CV health, particularly with implications for women as patients and health care professionals. We highlight the use of SoMe for promoting women’s cardiovascular health with respect to atherosclerotic cardiovascular disease (ASCVD), cardio-oncology, and cardio-obstetrics (Table 1). We discuss five major strategies by which SoMe allows for this: raising public awareness, allowing rapid dissemination of medical literature, facilitating professional networking, serving as a platform for medical conferences, and empowering patients (Figure 1). We also demonstrate ways in which SoMe is employed to promote diversity within the cardiology workforce, which has important downstream effects on the advancement of the CV care of women.
Table 1:
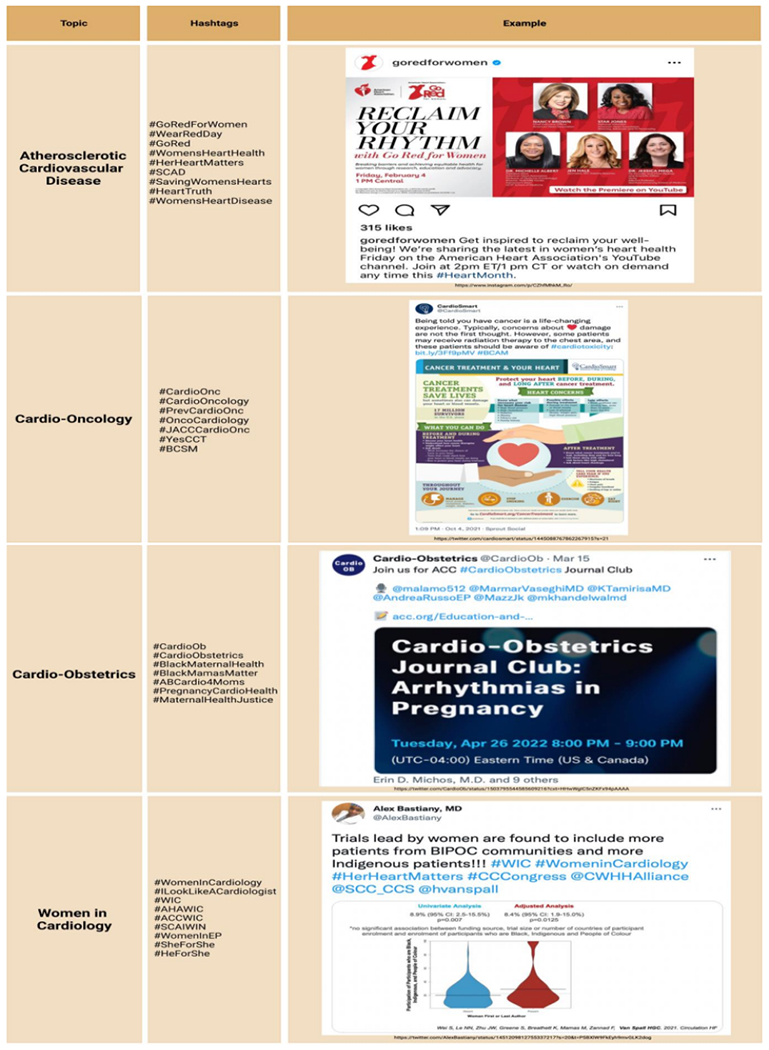
|
Figure 1:
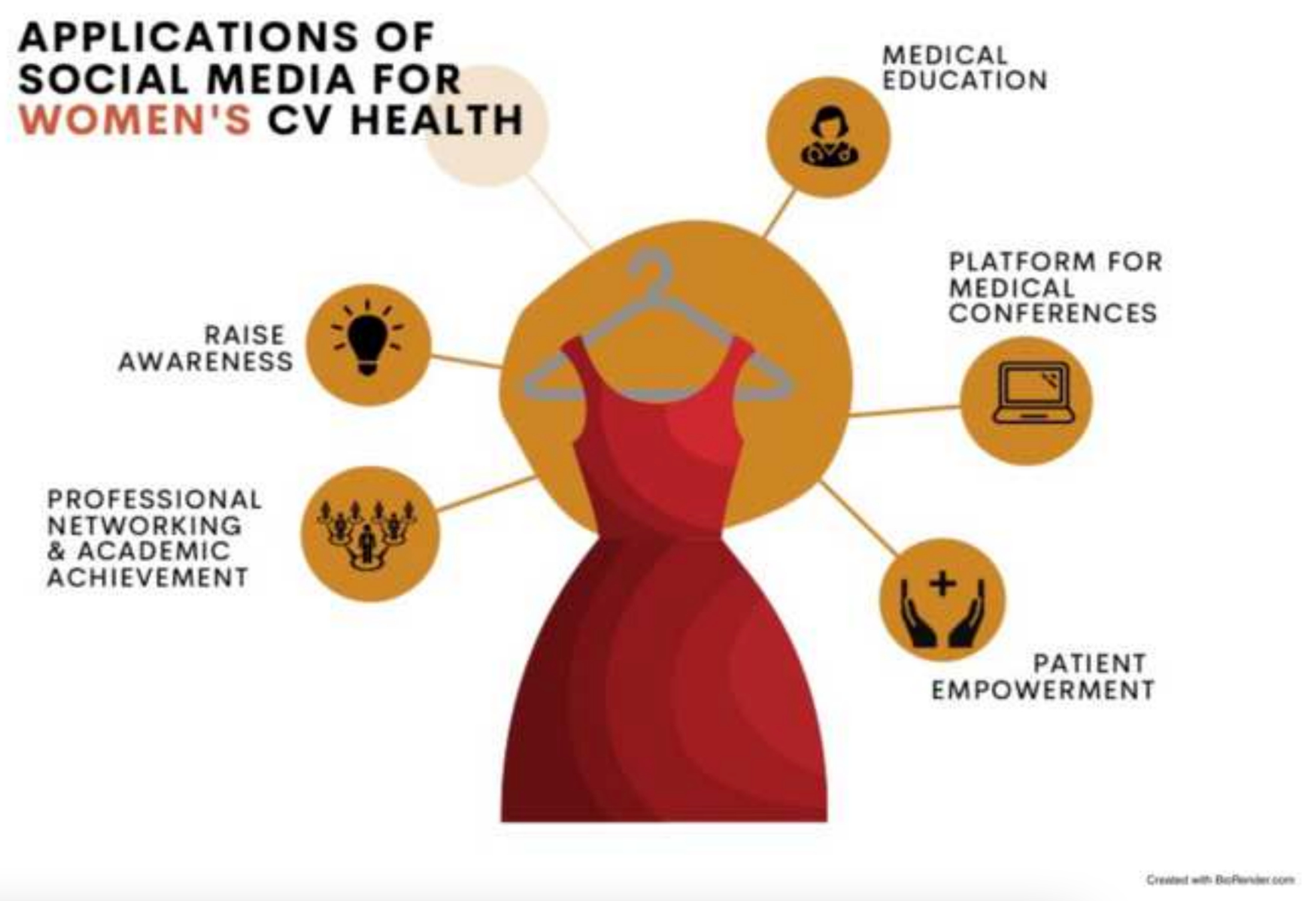
Social media strategies that are commonly used to promote women’s cardiovascular health including raising awareness of women’s cardiovascular health, supporting medical education, and empowering patients. Social media also facilitates professional networking and serves as a virtual platform for medical conferences.
SOCIAL MEDIA TERMS
Understanding ways in which SoMe is leveraged to call attention to women’s CV health and WIC requires understanding of relevant terminology (Figure 2). Commonly used platforms include Twitter, Instagram, YouTube, and Facebook.[8] Twitter (Twitter.com) is a microblogging website where users share up to 280 characters in posts called “tweets.” Tweets often include hashtags, which are keywords preceded by a pound sign (#). Using a hashtag allows for indexing of tweets, thereby simplifying searchability. Although hashtags are used across SoMe platforms, indexing occurs within a single platform. Twitter accounts are public. Users may “follow” other accounts or hashtags, allowing for the creation of curated home pages with updates incorporating new uploads by these users or by others using these hashtags. When users see a tweet, they can choose to passively read it or actively engage. There are three methods of engaging with a tweet: “liking”, commenting, and “retweeting”. To “like” a tweet, the user clicks on a heart icon next to the text, which signals to the author that the tweet has resonated with the reader. Users can also comment on tweets, by publicly sharing related opinions in the form of a brief “reply” message directly under the posted index tweet. “Retweeting” a tweet shows support by sharing the tweet to the user’s own profile. While we focus primarily on Twitter in this review, other social media platforms each have their own primary focus and associated terminologies. Additionally, we describe the role of the Altmetric Attention Score (AAS; Altmetric.com), a numerical score that reflects the internet attention associated with a research article, in promoting women’s CV health or WIC.[11, 27] In these fields, the AAS is usually reflective of the activity and engagement on Twitter.[11, 28]
Figure 2:
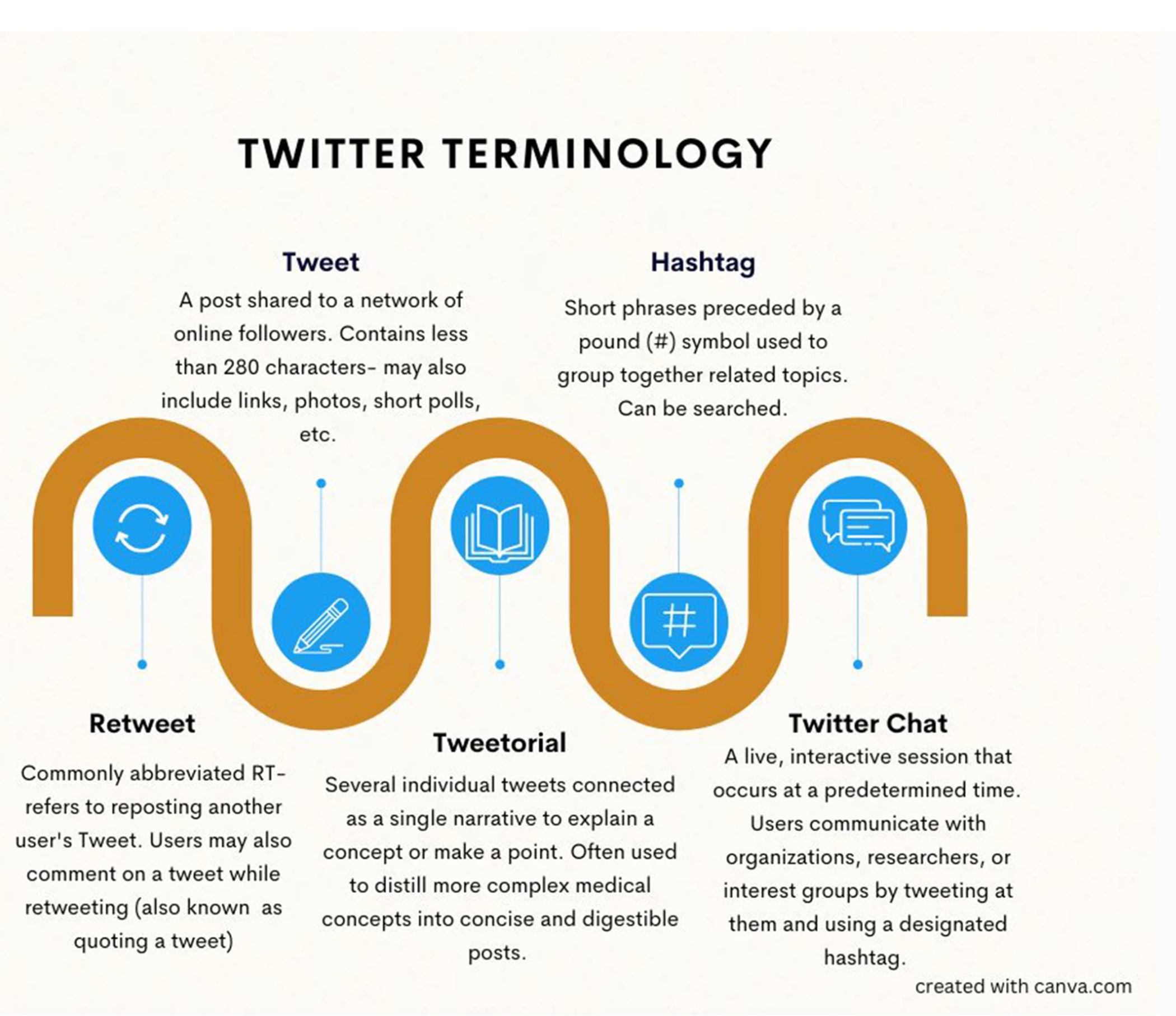
Common Twitter terminology.
GENERAL CARDIOLOGY IN WOMEN
Atherosclerotic Cardiovascular Disease
In the United States, there are clear sex and race disparities in the incidence and prevalence of coronary artery disease.[1, 2] Between 2006 and 2016, age-adjusted ASCVD-related death rates amongst non-Hispanic White females was 67.9 per 100,000, compared to that of non-Hispanic Black females at 85.4 per 100,000.[2] Disparities are also seen with regard to the prevention and management of CVD. For example, women are not only less likely than men to be prescribed statins, but when prescribed, they are less likely to be treated with guideline-recommended intensities.[1, 29] Furthermore, women presenting with ST-segment elevation myocardial infarction have been shown to have longer door-to-balloon times compared to men.[30, 31] The disparity in CVD management can be further stratified by race, with Black patients being less likely to receive potentially life-saving interventions including cardiopulmonary resuscitation for out-of-hospital cardiac arrests and invasive coronary angiography for angina.[32]
Lack of awareness of emerging, non-traditional risk factors for CVD is a significant contributor to the presence of these disparities.[5, 6, 33] SoMe has been successfully utilized to narrow this gap by calling attention to CVD in women. In 2002, the National Heart, Lung, and Blood Institute implemented the “The Heart Truth” campaign and the red dress icon.[17] This national campaign has relied heavily upon social marketing to increase awareness of CVD in women and prompt more aggressive risk factor management.[17, 18] Leaders of this campaign used SoMe to promote their message, predominantly through video platforms such as YouTube and personal blogs.[18] The American Heart Association (AHA) similarly has relied upon SoMe since launching the Go Red for Women campaign in 2004, which seeks to increase awareness of women’s CV health.[19] This initiative has close to 70,000 followers on Twitter (@GoRedForWomen).[34] The AHA also designated the first Friday in February as National Wear Red Day, a day dedicated to spreading awareness of women’s CV health.[35] National Wear Red Day has gained substantial traction on SoMe, with participants sharing pictures of themselves and colleagues wearing red and using the hashtag #WearRedDay to support the cause.[36] The campaign resulted in increased relative search volume of the phrases “heart disease (in) women” and “heart attack (in) women” over the 15 years following the launch, suggesting a net positive impact of the GoRedForWomen campaign.[19] A cross-sectional study analyzing trends in CVD awareness in the 10 years after the launch of this campaign demonstrated increasing awareness of CVD among women (56% identifying CVD as the leading cause of death in women compared to 30% in 1997, p<0.001), as well as an increased awareness of non-traditional signs of myocardial infarction (18% in 2012 vs 10% in 1997, p<0.0001).[20] While these findings may not be solely due to the impact of SoMe, it is likely that the campaign’s heavy use of SoMe contributed to the effects seen in this study. More recently in 2019, the AHA National Survey demonstrated a decline in awareness that was most notable in young women and racial minorities, specifically Black and Hispanic women, suggesting that additional work is needed to reach a diverse audience.[21]
In addition to raising awareness, SoMe is well situated to promote women’s CV health because SoMe facilitates rapid dissemination of medical literature and simplifies the sharing of educational content. These facets of SoMe were evident in the Twitter medical community’s response following the release of the AHA’s “Guideline for the Evaluation and Diagnosis of Chest Pain” in November 2021[37] These guidelines were widely discussed on Twitter with a focus on the inclusion of non-traditional presentations of ACS in women.[37, 38] Following their release, Dr. Martha Gulati, the lead author of the guidelines, composed a series of tweets discussing the top 10 messages of these guidelines.[38] As of March 2022, these tweets have had over 1,000 likes and 550 retweets, demonstrating the speed and ease of sharing information via SoMe.[38] Beyond sharing written educational content, SoMe users are often granted access to recordings of lectures, grand rounds, and conferences that would otherwise be limited to those in physical attendance.[12, 39] In this way, the use of SoMe facilitates the spread of educational content not only through written material but also through the promotion of lectures and other presentations.
Spontaneous Coronary Artery Dissection
SoMe is also important in the promotion of women’s CV health through the facilitation of patient empowerment. One compelling example of patients harnessing the power of SoMe comes from the spontaneous coronary artery dissection (SCAD) community. In the early 2000s, geographically disparate women with SCAD connected through SoMe. Together, they advocated for research on what was deemed a rare and poorly studied condition at the time, eventually reaching out to cardiologists at Mayo Clinic to advocate for their cause.[22] This collaboration ultimately led to the use of SoMe to recruit participants for a multinational SCAD registry that resulted in research advancement and a deeper understanding of this disease process.[22–24]
CARDIO-ONCOLOGY IN WOMEN
The role of SoMe in promoting women’s CV health can also be examined through the lens of cardio-oncology, a subspecialty of medicine focused on preventing and managing cardiovascular disease caused by cancer or cancer treatment.[9, 40, 41] Traditional and emerging therapies for many malignancies such as radiation therapy, hematopoietic stem cell transplantation, and immunotherapy can cause CV toxicity.[42] As management continues to progress and life expectancy for women with cancer increases, their CV risk profile is projected to become a larger driver of mortality than cancer recurrence.[43] In 2021, for example, female breast cancer accounted for an estimated 14.8% of all new cancer cases but only 7.2% of all cancer deaths.[44] Several studies have highlighted the impact of breast cancer on CVD risk, revealing that women with a history of breast cancer have a greater risk of death from CVD compared to those without a history of breast cancer.[45–48] A 2021 study also found that 69% of CVD-related mortality among breast cancer survivors was attributed to ischemic heart disease, suggesting ASCVD as a late manifestation of cancer treatment cardiotoxicity due to an interplay between cancer treatments such as aromatase inhibitors and radiation, alongside a high prevalence of CVD risk factors.[47] As with ASCVD in individuals without cancer, racial and ethnic CV disparities in women with cancer are well documented.[42, 49] When compared to White women, Black women are at higher risk cardiotoxicity from cancer treatment.[49, 50] Further, Black women are routinely diagnosed later in the disease course and have more aggressive forms of cancer.[49, 51–53] Together with a young tenure, the multidisciplinary nature of cardio-oncology makes the subspecialty well situated to benefit from SoMe. This potential was recognized by leaders of the field, who have used SoMe to raise awareness of cancer treatment associated cardiotoxicities, target vulnerable patient populations, improve cardiovascular health, and reach across the aisle with our colleagues in oncology for multidisciplinary collaborations.
The use of specific hashtags on SoMe allows for related cardio-oncology content to be organized and easily searchable. #CardioOnc, #CardioOncology, and #PrevCardioOnc are examples of such hashtags.[9] This was seen during the launch of the journal JACC:CardioOncology in September 2019. Individuals involved in the journal used multiple SoMe platforms to aid in the dissemination of the inaugural publications.[54] Because of this, the young journal already has an impact factor greater than 6 less than 3 years since launching the first issue. [54] Indeed, studies suggest that high rates of dissemination on SoMe may associate with subsequent high rates of manuscript download and citation, which drives the impact factor. [11] Beyond increased accessibility, hashtags allow for networking and academic discourse during professional conferences for both those attending in person and those attending virtually.[9] A recent study in JACC: CardioOncology analyzing Twitter utilization trends during national cardiovascular and oncological society meetings demonstrated rapid growth in the use of the platform to disseminate high-quality educational content.[55] In this way, patients and providers alike can not only use SoMe as a tool for academic discourse, education, and networking, but also to promote journals and journal publications, thereby expanding the reach of journals. Doing so allows for faster spread of data and increased visibility of publications that may help with subsequent patient care, research, and education.
The increasing reach of cardio-oncology journals, authors, and healthcare practitioners who use SoMe to promote research pertinent to women’s CVD is reflected in the AAS of such publications. To illustrate, the AHA Scientific Statement on CVD and Breast Cancer, which currently has an AAS of 683. This score ranks the publication in the top 5% of research articles that have been scored by Altimetric, signifying wide dissemination and online engagement.[46, 56] A 2021 review of SoMe for CV journals highlighted several studies demonstrating an association between AAS and the number of CV journal article publication downloads and citations. [11] As engagement increases and AAS rises, SoMe can be leveraged to raise awareness and disseminate new data, ultimately leading to increased knowledge surrounding women’s CV health.
SoMe use in cardio-oncology also provides an avenue for patient education, empowerment, and advocacy. One such example highlighting the power of SoMe is the hashtag #bcsm, an acronym for “breast cancer social media.” The #bcsm community was created in 2011 when two breast cancer survivors who met on Twitter started a weekly Twitter chat to provide other patients with a virtual community for support and access to evidence-based education.[57, 58] Use of this hashtag has grown overtime, with one study highlighting 19,841 Twitter accounts using the #bcsm hashtag in 2019, which was a 3196% increase from 2011.[57] Further, 80% of respondents to a survey of the #bcsm community reported that participating in scheduled Twitter chats using this hashtag increased their knowledge regarding breast cancer and breast cancer management.[57, 59] Given the effectiveness of this strategy, #bcsm has now been adopted by many healthcare professionals and academic journals, and is often used in conjunction with the #CardioOncology and #CardioOnc hashtags to highlight cardiovascular issues facing breast cancer survivors and share medical literature about CVD in women with breast cancer.
CARDIO-OBSTETRICS
Cardio-obstetrics is another emerging field, in which leaders have utilized SoMe to promote growth and address sex disparities in the intersection of CVD and reproductive health. The field is dedicated to identifying and managing CVD and cardiometabolic risk factors through preconception, pregnancy, and postpartum.[15, 60–64] The recent growth of cardio-obstetrics is especially relevant in the context of rising maternal mortality rates in the United States, with CVD identified as the leading cause during pregnancy and up to one year postpartum.[60, 64–67] Additionally, approximately 20% of pregnant women experience adverse pregnancy outcomes (APOs) such as hypertensive disorders of pregnancy including pre-eclampsia, gestational diabetes, small for gestational age infant, and preterm birth, many of which increase lifetime risk of ASCVD.[60–63] This association is even more pronounced for Black women, who have greater rates of APOs and a three-to-four-fold increased risk of maternal mortality compared to White women (41.7 vs 13.4 deaths per 100,000 live births between 2014 and 2017).[7, 15, 61, 67] This greater risk spans education and income levels, and is largely a result of societal and institutional psychosocial stressors, including structural racism.[7, 68] The role of cardio-obstetrics specialists in managing patients is becoming increasingly important as women continue to choose pregnancy later in life, the rates of cardiometabolic risk factors increase, and women with congenital heart disease and underlying CVD are living to childbearing age.[60]
These well-established associations have led to the development of guideline recommendations to screen for APOs when assessing ASCVD risk in women.[69–72] Despite these guidelines, the relationships between pregnancy and CVD in women remains overlooked among healthcare professionals and the general public. A recent survey administered via Twitter demonstrated that less than 60% of participating clinicians recognized the association between preterm labor and future adverse maternal cardiovascular outcomes.[73] Furthermore, only 34% of cardiologists cited awareness of the related guidelines, compared to 62% of obstetrician/gynecologists who responded.[73] This survey demonstrates the power of SoMe as a means for assessing healthcare provider knowledge and identifying areas to target for public health and medical education campaigns. Notably, the recruitment for this survey was initially suboptimal with e-mail distribution, yet exponentially increased with distribution on Twitter, demonstrating the utility of SoMe for conducting such studies.[73]
Like cardio-oncology, leaders in cardio-obstetrics have used dedicated hashtags to publicize medical literature and raise awareness about the field.[15, 74] Routine use of hashtags such as #CardioObstetrics and #CardioOb has fostered an online community of physicians, facilitating professional networking and collaboration (Figure 3).[15] Many use the hashtag #PregnancyCardioHealth to share new data and trials, and organizations such as the ABC (#ABCardio4Moms and #FacesofBlackMaternalHealth), Black Mamas Matter Alliance (#BlackMamasMatter), and Centers for Disease Control and Prevention (#HearHer) use hashtags to call attention to Black maternal health, while also facilitating women of color creating shared communities.[7, 74–76] These hashtags are also used to highlight related Twitter Chats and virtual journal clubs, using SoMe to encourage networking and promote the spread of information.
Figure 3:
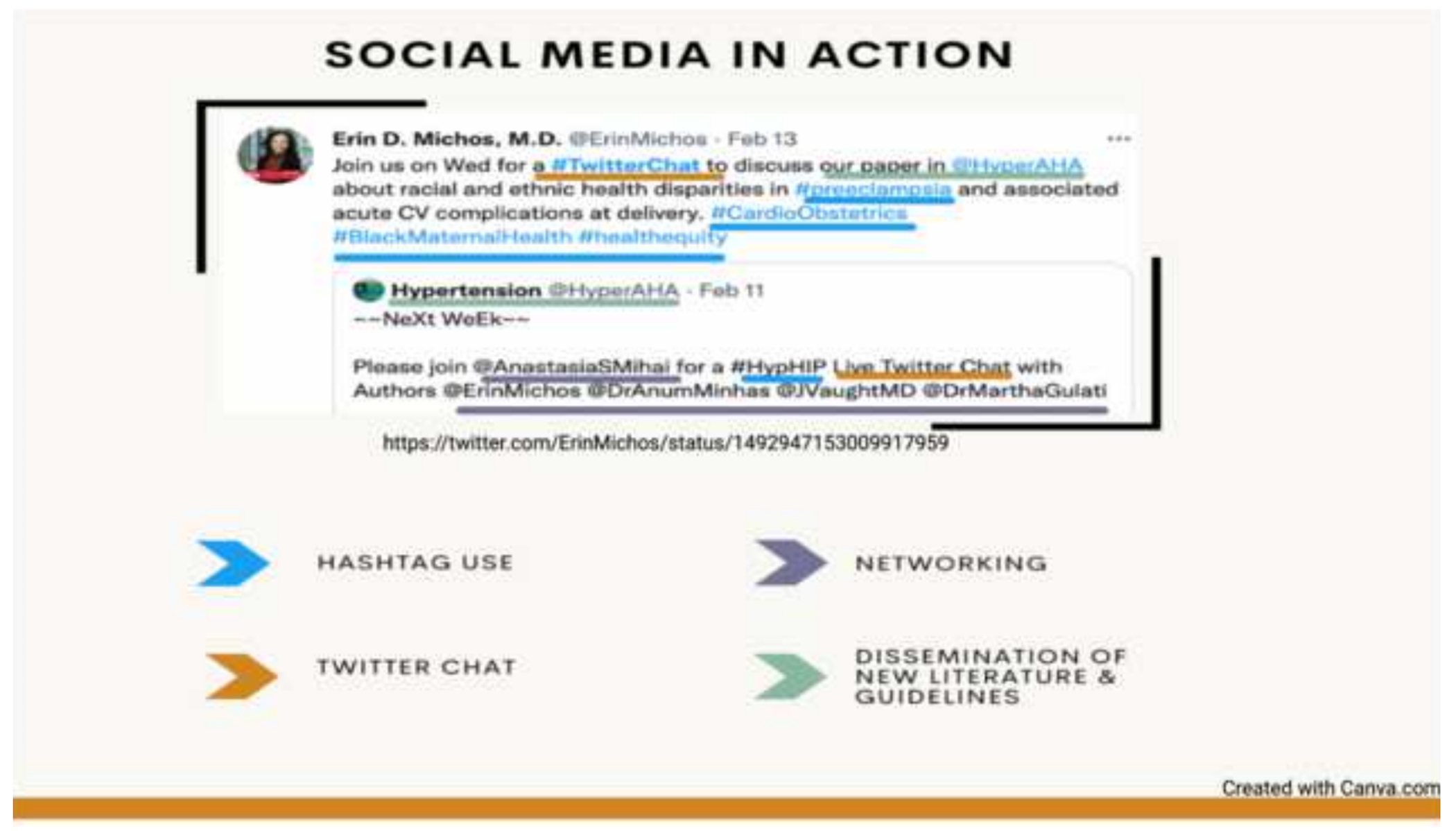
An example of a Tweet that utilizes many of the social media strategies discussed in this review. The author uses Twitter to promote a Twitter Chat as means of networking, disseminates new literature, and employs commonly used hashtags [119, 120].
The success of those promoting cardio-obstetrics on SoMe is further reflected in the AAS of many related publications. For example, the Circulation: Cardiovascular Quality and Outcomes publication titled “Working Agenda for Black Mothers” currently has an AAS of 413, placing it in the top 5% of research output scored by Altmetric.[7, 77] Another publication titled “Call to Action: Maternal Health and Saving Mothers: A Policy Statement From the American Heart Association” has a high AAS, highlighting the extent of SoMe reach.[78, 79] As fields such as cardio-oncology and cardio-obstetrics continue to grow, it is likely that engagement with social media will similarly increase. This may ultimately be reflected in the AAS, which serves as a measurable marker of SoMe engagement.
WOMEN IN CARDIOLOGY (WIC)
In addition to sex and racial/ethnic CVD disparities, there are disparities within the cardiology workforce. A 2019 study highlighted this gap, reporting that women comprise only 21.5% of adult general cardiology fellows and less than 15% in procedural subspecialities.[80] The numbers are especially jarring as women make up just under half of Internal Medicine residents.[80] Notably, this disparity is also seen in healthcare system leadership positions and roles on journal editorial boards.[25, 81–83] This gap is further pronounced in cardiologists of minority backgrounds, with more than half of cardiologists in the United States being White, 3% Black, and 4.2% Hispanic or Latino.[84–86]
The lack of diversity in the cardiology workforce has ramifications for women’s CV health.[87, 88] In 2014, authors from the Johns Hopkins Bloomberg School of Public Health described the public health benefits of increased workforce diversity, highlighting a relationship with the inclusion of a more diverse patient population in clinical trials as a means of improving health and health sciences research.[89] This was further supported by an analysis in Nature revealing that female authorship was more likely to result in greater consideration of sex-specific factors in research and clinical guidelines, a necessary step towards improving and promoting women’s CV health.[90] Interestingly, upon reviewing the first authors of the publications referred to throughout our current review, we found that approximately 70% of our references included women as first authors. This may point to a propensity for female authorship of publications related to CV health in women, although additional research is needed to clarify this association.
Of interest, substantially fewer women lead clinical trials and present at major conferences.[91] In addition to disparities in workforce and authorship, analysis of 740 cardiovascular trials revealed that only 38.2% of trial participants were women, with numbers disproportionately lower than disease prevalence in ASCVD.[92] The lack of sex and racial diversity within cardiology likely contributes to women being left out of clinical trials and subsequently cardiology guidelines. Promoting and encouraging women in cardiology is essential to diversifying the workforce, thereby leading to more inclusive clinical trials and the development of more equitable guidelines, ultimately increasing CV care for all women.
SoMe has been used to address these gaps and advocate for a more diverse workforce. Hashtags such as #Ilooklikeacardiologist, #WIC, and #WomenInCardiology are commonly used by cardiologists to call attention to this bipartite gap and facilitate professional networking.[16, 25] Other hashtags such as #ACCWIC, #AHAWIC, #SCAIWIN, and #WomeninEP are also commonly used by subspecialists and members of professional societies.[16] An analysis of six common Twitter hashtags specific to WIC from 2016 to 2019 showed a 706% increase in use, demonstrating robust engagement and advocacy by women driving this change.[16] The widespread reach of messages that include these hashtags was recently demonstrated in a tweet. In the tweet, Dr. Megan Joseph shared her experiences as a pregnant woman in the cardiac catheterization lab and shared a useful resource about radiation safety in an effort to address concerns about occupational radiation exposure that women considering a career in cardiology often express.[93] In her tweet, Dr. Joseph utilized the hashtag #WIC, thereby allowing for a wider reach beyond her individual Twitter following of approximately 500.[94] With sufficient repetition and amplification of messages like this, SoMe can help recruit more women to the field by disseminating information and support for careers of women in cardiology. Of note, there are limitations when using hashtags, particularly acronyms. The hashtag #WIC, for example, is commonly used to refer to resources for low-income women, infants, and children.[95] Use of these hashtags is therefore subject to interpretation, and reliant upon context and audience.
HEALTH EQUITY AND PATIENT EMPOWERMENT ON SOCIAL MEDIA
In addition to facilitating the creation of support groups and advancing research, SoMe also empowers patients by providing them with access to accurate health information from reputable sources, thereby allowing them to initiate and engage in conversations about their health. For example, the Association of Black Cardiologists, Inc. (ABC) routinely uses SoMe to highlight racial/ethnic disparities and encourage Black women and their health care professionals to prioritize their CV health. SoMe is used as a platform for sharing relevant statistics, publicizing webinars and conferences, and highlighting presentations by ABC members.[96–98] Healthcare organizations also leverage SoMe to call attention to women’s CV health and promote public literacy of healthcare conditions. A brief search of the terms “women’s cardiovascular health” on YouTube reveals the extent of this promotion, with multiple large healthcare systems sharing patient-centered videos on different aspects of women’s cardiovascular disease.[99]
ALLYSHIP
While SoMe provides a clear path for promotion of women’s CV health and WIC, women should not be considered responsible for these efforts alone. Achievement of equality requires allyship. This was highlighted in a 2019 publication in The Lancet that presented best practices for the attainment of equality for women in medicine, including allyship.[100] An Editor’s Note in JAMA:Internal Medicine further calls attention to this concept, highlighting the importance of allyship for women in the context of clinical trial leadership.[101] SoMe provides an easily accessible avenue for this. For example, the interests groups HeForShe and White Coats for Black Lives often use hashtags #HeForShe and #wc4bl to publicly signal support, spur conversation, and create change.[7, 102] Other hashtags such as #BlackWomenInMedicine and #WomenInMedicine can be used to support these efforts. Further, by facilitating discussion and networking, SoMe can serve as a launchpad for new ideas. This was seen in the movement away from “manels” (all-male panels), which was first presented on SoMe and has become a national point of discussion.[103] Men can use SoMe to acknowledge the achievements of women and racial minorities, thereby increasingly visibility on a public stage. This can be accomplished through using these hashtags, writing an original Tweet, or liking and/or retweeting a post to show support.
While many already leverage SoMe as a signal of allyship, there remains work to be done. An analysis of the WIC Twitter network showed that women accounted for the majority of the amplification of hashtags in support of WIC.[16] This report also showed that, as the number of women who participated in the amplification of these hashtags increased over the study period, the participation of men concomitantly declined. Men also showed an overall lower level of engagement with WIC hashtags, again highlighting an area for improvement.[16] In addition to expressing allyship on SoMe, there is significant room for improvement in medical curricula to address implicit bias and educate learners on the history of mistreatment that the Black community has experienced from health care as a whole.[7] Such curricular changes should strengthen provider allyship with Black patients, ultimately leading to treatment equality.[7] Each of these ideas requires upstream change, and thereby buy-in from leaders. Allyship is essential to this process. While SoMe has been used to signal support, allies must further leverage SoMe to create systemic change.
POTENTIAL PITFALLS
Although SoMe has a growing and important role in disseminating health information, it also provides a platform for widespread propagation of inaccurate information.[104–106] The dissemination of false information on SoMe takes two forms: “misinformation” can be spread without malicious intent, or “disinformation” can be spread intentionally for personal or financial gain.[105] Regardless of intent, inappropriate use of SoMe threatens population health through multiple mechanisms.[107, 108] These mechanisms can include the promotion of unproven therapies and health behaviors and reliance on poor information in lieu of visiting health professionals and obtaining safe and accurate treatment plans.[107, 108] Health misinformation is especially pervasive regarding cardiovascular health. Dietary and medication advice based on anecdotal and individual experiences are commonplace on SoMe and go unchecked without verification using concrete scientific evidence.[109] Paid promotion of dietary supplements that are not evidence-based is similarly ubiquitous. Non-medical social media personalities with large followings are often paid to promote supplements, relying on misleading claims that are not subject to regulation and lead to financial gain.[110] An additional example that highlights the potential harms of misinformation on SoMe is the dissemination of inaccurate information about statins.[111] There are well-established sex disparities in statin utilization where women are less likely to be prescribed statins than male patients.[29] The dissemination of statin misinformation contributes to poor adherence and may further propagate this disparity.[112, 113] Each of these examples illustrates pitfalls in SoMe that coexist with the benefits. Though the ease of access and rapid dissemination of information on SoMe has the potential to improve overall CV health, this also allows for propagation of false information leading to negative health outcomes.[108]
CONCLUSION
Despite being a leading cause of death for women, CVD remains underrecognized and undertreated in women when compared to men, largely due to a lack of awareness of sex-specific risk enhancers. These disparities in diagnosis and appropriate management are even greater among women of racial minority backgrounds.[1–6] SoMe can narrow this gap by calling attention to women’s CV health, empowering patients, providing an avenue for professional networking and academic advancement, supporting medical education, and serving as a platform of medical conferences. Such examples have been demonstrated in general cardiology, cardio-oncology, and cardio-obstetrics. SoMe is also a powerful tool for recruiting more women and racial/ethnic minorities to choose a career in cardiology and promote allyship among male and overall majority colleagues, both of which will likely impact sex and racial/ethnic disparities in clinical trial design and enrollment, further impacting the CV care of women, especially Black women. In these ways, SoMe provides a unique mechanism for addressing sex and racial/ethnic CV health inequities, with particular implications for women.
Sources of Funding:
This publication was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Numbers UL1TR001436 and KL2TR001438. Its contents do not necessarily represent the official views of the NIH.
Conflicts of Interest:
EHY reports research funding from CSL Behring and Boehringer Ingelheim and Eli and Lilly, and consulting fees from Pfizer. REG has direct stock ownership in Google (Alphabet) and investments in mutual funds that may have positions in social media companies, and is a passive, nonvoting member in an investment company with no knowledge of its investments directly or through mutual funds in social media companies. SAB has direct stock ownership in Google (Alphabet) and investments in mutual funds that may have positions in social media companies. All authors have no additional disclosures.
Footnotes
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
REFERENCES
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Virani SS, Alonso A, Aparicio HJ, et al. : Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation 2021, 143(8):e254–e743. [DOI] [PubMed] [Google Scholar]
- 2.Benjamin EJ, Muntner P, Alonso A, et al. : Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 2019, 139(10):e56–e528. [DOI] [PubMed] [Google Scholar]
- 3.Aggarwal NR, Patel HN, Mehta LS, et al. : Sex differences in ischemic heart disease: advances, obstacles, and next steps. Circulation: Cardiovascular Quality and Outcomes 2018, 11(2):e004437. [DOI] [PubMed] [Google Scholar]
- 4.Stehli J, Duffy SJ, Burgess S, et al. : Sex disparities in myocardial infarction: biology or bias? Heart, Lung and Circulation 2021, 30(1):18–26. [DOI] [PubMed] [Google Scholar]
- 5.Bullock-Palmer RP, Shaw LJ, Gulati M: Emerging misunderstood presentations of cardiovascular disease in young women. Clinical cardiology 2019, 42(4):476–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bairey Merz CN, Andersen H, Sprague E, et al. : Knowledge, attitudes, and beliefs regarding cardiovascular disease in women: the Women’s Heart Alliance. Journal of the American College of Cardiology 2017, 70(2):123–132. [DOI] [PubMed] [Google Scholar]
- 7.Bond RM, Gaither K, Nasser SA, et al. : Working Agenda for Black Mothers: A Position Paper From the Association of Black Cardiologists on Solutions to Improving Black Maternal Health. Circ Cardiovasc Qual Outcomes 2021, 14(2):e007643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Social Media Use in 2021 [https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/]
- 9.Brown SA, Daly RP, Duma N, et al. : Leveraging Social Media for Cardio-Oncology. Curr Treat Options Oncol 2020, 21(10):83. [DOI] [PubMed] [Google Scholar]
- 10.Conley CC, Goyal NG, Brown SA: #CardioOncology: Twitter chat as a mechanism for increasing awareness of heart health for cancer patients. Cardiooncology 2020, 6:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown SA, Campbell C, Fradley M, Volgman AS: Social media for cardiovascular journals: State of the art review. Am Heart J Plus 2021, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parwani P, Choi AD, Lopez-Mattei J, et al. : Understanding Social Media: Opportunities for Cardiovascular Medicine. J Am Coll Cardiol 2019, 73(9):1089–1093. [DOI] [PubMed] [Google Scholar]
- 13.Pemmaraju N: Editorial overview: Emerging importance of social media for real-time communication in the modern medical era. Semin Hematol 2017, 54(4):175–176. [DOI] [PubMed] [Google Scholar]
- 14.Walsh MN: Social Media and Cardiology. J Am Coll Cardiol 2018, 71(9):1044–1047. [DOI] [PubMed] [Google Scholar]
- 15.Davis MB, Walsh MN: Cardio-Obstetrics. Circ Cardiovasc Qual Outcomes 2019, 12(2):e005417. [DOI] [PubMed] [Google Scholar]
- 16.Chandra NV, Hsiao R, Shapiro H, et al. : Women in Cardiology Twitter Network: An Analysis of a Global Professional Virtual Community From 2016 to 2019. J Am Heart Assoc 2021, 10(5):e019321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.About the Heart Truth. In. National Heart Lung and Blood Institute. [Google Scholar]
- 18.Long T, Taubenheim A, Wayman J, Temple S, Ruoff B: “The Heart Truth:” Using the Power of Branding and Social Marketing to Increase Awareness of Heart Disease in Women. Soc Mar Q 2008, 14(3):3–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Suero-Abreu GA, Barajas-Ochoa A, Perez-Peralta A, Rojas E, Berkowitz R: Assessment of the Effect of the Go Red for Women Campaign on Search Engine Queries for Cardiovascular Disease in Women. Cardiology Research 2020, 11(5):348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mosca L, Hammond G, Mochari-Greenberger H, Towfighi A, Albert MA, American Heart Association Cardiovascular Disease and Stroke in Women and Special Populations Committee of the Council on Clinical Cardiology CoEaP, Council on Cardiovascular Nursing, C.uncil on High Bloo: Fifteen-year trends in awareness of heart disease in women: results of a 2012 American Heart Association national survey. Circulation 2013, 127(11):1254–1263, e1251-1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cushman M, Shay CM, Howard VJ, et al. : Ten-Year Differences in Women’s Awareness Related to Coronary Heart Disease: Results of the 2019 American Heart Association National Survey: A Special Report From the American Heart Association. Circulation 2021, 143(7):e239–e248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tweet MS, Gulati R, Aase LA, Hayes SN: Spontaneous coronary artery dissection: a disease-specific, social networking community-initiated study. Mayo Clin Proc 2011, 86(9):845–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hayes SN: Spontaneous coronary artery dissection (SCAD): new insights into this not-so-rare condition. Tex Heart Inst J 2014, 41(3):295–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewey J, El Hajj SC, Hayes SN: Spontaneous Coronary Artery Dissection: New Insights into This Not-So-Rare Condition. Annu Rev Med 2022, 73:339–354. [DOI] [PubMed] [Google Scholar]
- 25.Beygui N, Bahl D, Mansour C, et al. : Social Media as a Tool to Advance Women in Cardiology: Paving the Way for Gender Equality and Diversity. CJC Open 2021, 3(12 Suppl):S130–S136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patel H, Volgman AS: Women in Cardiology: Role of Social Media in Advocacy. Curr Cardiol Rev 2021, 17(2):144–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.What are altmetrics? [https://www.altmetric.com/about-altmetrics/what-are-altmetrics/]
- 28.Parwani P, Martin GP, Mohamed MO, et al. : Relationship of Altmetric Attention Score to Overall Citations and Downloads for Papers Published in JACC. J Am Coll Cardiol 2020, 76(6):757–759. [DOI] [PubMed] [Google Scholar]
- 29.Nanna MG, Wang TY, Xiang Q, et al. : Sex differences in the use of statins in community practice: patient and provider assessment of lipid management registry. Circulation: Cardiovascular Quality and Outcomes 2019, 12(8):e005562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Angeja BG, Gibson CM, Chin R, et al. : Predictors of door-to-balloon delay in primary angioplasty. Am J Cardiol 2002, 89(10):1156–1161. [DOI] [PubMed] [Google Scholar]
- 31.Murphy AC, Yudi MB, Farouque O, et al. : Impact of Gender and Door-to-Balloon Times on Long-Term Mortality in Patients Presenting With ST-Elevation Myocardial Infarction. Am J Cardiol 2019, 124(6):833–841. [DOI] [PubMed] [Google Scholar]
- 32.Huded CP, Johnson M, Kravitz K, et al. : 4-step protocol for disparities in STEMI care and outcomes in women. Journal of the American College of Cardiology 2018, 71(19):2122–2132. [DOI] [PubMed] [Google Scholar]
- 33.O’Kelly AC, Michos ED, Shufelt CL, et al. : Pregnancy and Reproductive Risk Factors for Cardiovascular Disease in Women. Circ Res 2022, 130(4):652–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.GoRedforWomen: GoRedforWomen. In. Twitter.
- 35.National Wear Red Day 2022. In.: National Heart, Lung, and Blood Institute. [Google Scholar]
- 36.#WearRedDay. In. Twitter.
- 37.Gulati M, Levy PD, Mukherjee D, et al. : 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 144(22):e368–e454. [DOI] [PubMed] [Google Scholar]
- 38.In Gulati M.. Twitter; 2021.
- 39.In Ibrahim K. Edited by @KhalilIbrahimMD; 2022.
- 40.Parent S, Pituskin E, Paterson DI: The Cardio-oncology Program: A Multidisciplinary Approach to the Care of Cancer Patients With Cardiovascular Disease. Can J Cardiol 2016, 32(7):847–851. [DOI] [PubMed] [Google Scholar]
- 41.Sadler D, Arnold A, Herrmann J, et al. : Reaching Across the Aisle: Cardio-Oncology Advocacy and Program Building. Curr Oncol Rep 2021, 23(6):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wilcox NS, Rotz SJ, Mullen M, et al. : Sex-Specific Cardiovascular Risks of Cancer and Its Therapies. Circ Res 2022, 130(4):632–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Patnaik JL, Byers T, DiGuiseppi C, Dabelea D, Denberg TD: Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Res 2011, 13(3):R64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cancer Stat Facts: Female Breast Cancer. In. National Cancer Institute Surveillance, Epidemiology, and End Results Program; 2021. [Google Scholar]
- 45.Mehta LS, Watson KE, Barac A, et al. : Cardiovascular Disease and Breast Cancer: Where These Entities Intersect: A Scientific Statement From the American Heart Association. Circulation 2018, 137(8):e30–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mehta LS, Watson KE, Barac A, et al. : Cardiovascular disease and breast cancer: where these entities intersect: a scientific statement from the American Heart Association. Circulation 2018, 137(8):e30–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ramin C, Schaeffer ML, Zheng Z, et al. : All-Cause and Cardiovascular Disease Mortality Among Breast Cancer Survivors in CLUE II, a Long-Standing Community-Based Cohort. J Natl Cancer Inst 2021, 113(2):137–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bradshaw PT, Stevens J, Khankari N, Teitelbaum SL, Neugut AI, Gammon MD: Cardiovascular Disease Mortality Among Breast Cancer Survivors. Epidemiology 2016, 27(1):6–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ohman RE, Yang EH, Abel ML: Inequity in Cardio-Oncology: Identifying Disparities in Cardiotoxicity and Links to Cardiac and Cancer Outcomes. J Am Heart Assoc 2021, 10(24):e023852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Carnethon MR, Pu J, Howard G, et al. : Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association. Circulation 2017, 136(21):e393–e423. [DOI] [PubMed] [Google Scholar]
- 51.Siegel RL, Miller KD, Jemal A: Cancer statistics, 2020. CA Cancer J Clin 2020, 70(1):7–30. [DOI] [PubMed] [Google Scholar]
- 52.Ellis L, Canchola AJ, Spiegel D, Ladabaum U, Haile R, Gomez SL: Racial and Ethnic Disparities in Cancer Survival: The Contribution of Tumor, Sociodemographic, Institutional, and Neighborhood Characteristics. J Clin Oncol 2018, 36(1):25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu AH, Gomez SL, Vigen C, et al. : The California Breast Cancer Survivorship Consortium (CBCSC): prognostic factors associated with racial/ethnic differences in breast cancer survival. Cancer Causes Control 2013, 24(10):1821–1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brown SA, Yang EH, Reza N, et al. : #JACCCardioOnc: Evolution of a Dedicated Social Media Strategy for. JACC CardioOncol 2021, 3(3):461–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jackson SB, Tanoue M, Shahandeh N, et al. : #Cardioonc: Are We Reaching Across the Digital Aisle? JACC CardioOncol 2021, 3(3):457–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Altmetric: Altmetric - Cardiovascular Disease and Breast Cancer: Where These Entities Intersect: A Scientific Statement From the American Heart Association. In. [DOI] [PMC free article] [PubMed]
- 57.Katz MS, Staley AC, Attai DJ: A History of #BCSM and Insights for Patient-Centered Online Interaction and Engagement. J Patient Cent Res Rev 2020, 7(4):304–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.About the #BCSM Community [https://bcsm.org/bcsm-community/]
- 59.Attai DJ, Cowher MS, Al-Hamadani M, Schoger JM, Staley AC, Landercasper J: Twitter Social Media is an Effective Tool for Breast Cancer Patient Education and Support: Patient-Reported Outcomes by Survey. J Med Internet Res 2015, 17(7):e188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sharma G, Lindley K, Grodzinsky A: Cardio-Obstetrics: Developing a Niche in Maternal Cardiovascular Health. J Am Coll Cardiol 2020, 75(11):1355–1359. [DOI] [PubMed] [Google Scholar]
- 61.Parikh NI, Gonzalez JM, Anderson CAM, et al. : Adverse pregnancy outcomes and cardiovascular disease risk: unique opportunities for cardiovascular disease prevention in women: a scientific statement from the American Heart Association. Circulation 2021, 143(18):e902–e916. [DOI] [PubMed] [Google Scholar]
- 62.Hauspurg A, Ying W, Hubel CA, Michos ED, Ouyang P: Adverse pregnancy outcomes and future maternal cardiovascular disease. Clin Cardiol 2018, 41(2):239–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Grandi SM, Filion KB, Yoon S, et al. : Cardiovascular Disease-Related Morbidity and Mortality in Women With a History of Pregnancy Complications. Circulation 2019, 139(8):1069–1079. [DOI] [PubMed] [Google Scholar]
- 64.Mehta LS, Warnes CA, Bradley E, et al. : Cardiovascular Considerations in Caring for Pregnant Patients: A Scientific Statement From the American Heart Association. Circulation 2020, 141(23):e884–e903. [DOI] [PubMed] [Google Scholar]
- 65.Lima FV, Yang J, Xu J, Stergiopoulos K: National Trends and In-Hospital Outcomes in Pregnant Women With Heart Disease in the United States. Am J Cardiol 2017, 119(10):1694–1700. [DOI] [PubMed] [Google Scholar]
- 66.Ouyang P, Sharma G: The Potential for Pregnancy Heart Teams to Reduce Maternal Mortality in Women With Cardiovascular Disease. J Am Coll Cardiol 2020, 76(18):2114–2116. [DOI] [PubMed] [Google Scholar]
- 67.Pregnancy Mortality Surveillance System [https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm]
- 68.Bond RM, Ansong A, Albert MA: Shining a Light on the Superwoman Schema and Maternal Health. Circulation 2022, 145(7):507–509. [DOI] [PubMed] [Google Scholar]
- 69.Visseren FLJ, Mach F, Smulders YM, et al. : 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur J Prev Cardiol 2022, 29(1):5–115. [DOI] [PubMed] [Google Scholar]
- 70.Arnett DK, Blumenthal RS, Albert MA, et al. : 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140(11):e596–e646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bushnell C, McCullough LD, Awad IA, et al. : Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014, 45(5):1545–1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Grundy SM, Stone NJ, Bailey AL, et al. : 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019, 73(24):3168–3209. [DOI] [PubMed] [Google Scholar]
- 73.Wu P, Mamas MA, Gulati M: Health Care Professional’s Knowledge of Pregnancy Complications and Women’s Cardiovascular Health: An International Study Utilizing Social Media. Journal of Women’s Health 2022. [DOI] [PubMed] [Google Scholar]
- 74.Sharma G, Zakaria S, Michos ED, et al. : Improving Cardiovascular Workforce Competencies in Cardio-Obstetrics: Current Challenges and Future Directions. J Am Heart Assoc 2020, 9(12):e015569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.#HearHer. In.
- 76.We Are the Faces of Black Maternal Health [https://wearethefaces.abcardio.org/]
- 77.Altmetric: Altmetric - Working Agenda for Black Mothers. In.
- 78.Mehta LS, Sharma G, Creanga AA, et al. : Call to Action: Maternal Health and Saving Mothers: A Policy Statement From the American Heart Association. Circulation 2021, 144(15):e251–e269. [DOI] [PubMed] [Google Scholar]
- 79.Altmetric - Call to Action: Maternal Health and Saving Mothers: A Policy Statement From the American Heart Association [https://ahajournals.altmetric.com/details/113075681] [DOI] [PubMed]
- 80.Mehta LS, Fisher K, Rzeszut AK, et al. : Current Demographic Status of Cardiologists in the United States. JAMA Cardiol 2019, 4(10):1029–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Balasubramanian S, Saberi S, Yu S, Duvernoy CS, Day SM, Agarwal PP: Women Representation Among Cardiology Journal Editorial Boards. Circulation 2020, 141(7):603–605. [DOI] [PubMed] [Google Scholar]
- 82.Khan MS, Usman MS, Siddiqi TJ, et al. : Women in Leadership Positions in Academic Cardiology: A Study of Program Directors and Division Chiefs. J Womens Health (Larchmt) 2019, 28(2):225–232. [DOI] [PubMed] [Google Scholar]
- 83.Blumenthal DM, Olenski AR, Yeh RW, et al. : Sex Differences in Faculty Rank Among Academic Cardiologists in the United States. Circulation 2017, 135(6):506–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Keir M, McFadden C, Ruzycki S, et al. : Lack of Equity in the Cardiology Physician Workforce: A Narrative Review and Analysis of the Literature. CJC Open 2021, 3(12 Suppl):S180–S186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Johnson AE, Talabi MB, Bonifacino E, et al. : Racial Diversity Among American Cardiologists: Implications for the Past, Present, and Future. Circulation 2021, 143(24):2395–2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Auseon AJ, Kolibash AJ, Capers Q: Successful efforts to increase diversity in a cardiology fellowship training program. J Grad Med Educ 2013, 5(3):481–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Capers Q, Johnson A, Berlacher K, Douglas PS: The Urgent and Ongoing Need for Diversity, Inclusion, and Equity in the Cardiology Workforce in the United States. J Am Heart Assoc 2021, 10(6):e018893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gomez LE, Bernet P: Diversity improves performance and outcomes. J Natl Med Assoc 2019, 111(4):383–392. [DOI] [PubMed] [Google Scholar]
- 89.LaVeist TA, Pierre G: Integrating the 3Ds--social determinants, health disparities, and health-care workforce diversity. Public Health Rep 2014, 129 Suppl 2:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nielsen MW, Andersen JP, Schiebinger L, Schneider JW: One and a half million medical papers reveal a link between author gender and attention to gender and sex analysis. Nat Hum Behav 2017, 1(11):791–796. [DOI] [PubMed] [Google Scholar]
- 91.Walsh MN: Gender Diversity in Cardiovascular Clinical Trial Research Begins at the Top. J Am Coll Cardiol 2022, 79(9):929–932. [DOI] [PubMed] [Google Scholar]
- 92.Jin X, Chandramouli C, Allocco B, Gong E, Lam CSP, Yan LL: Women’s Participation in Cardiovascular Clinical Trials From 2010 to 2017. Circulation 2020, 141(7):540–548. [DOI] [PubMed] [Google Scholar]
- 93.Sarma AA, Nkonde-Price C, Gulati M, et al. : Cardiovascular Medicine and Society: The Pregnant Cardiologist. J Am Coll Cardiol 2017, 69(1):92–101. [DOI] [PubMed] [Google Scholar]
- 94.Joseph MS. In. Edited by @mshetts1; 2021.
- 95.Association NW. In. Edited by @NatWICAssoc.
- 96.Cardiologists AoB. In. Edited by @ABCardio1.
- 97.Association of Black Cardiologists [https://abcardio.org]
- 98.Cardiologists AoB. In. Edited by @ABCardio1; 2022. [Google Scholar]
- 99. .In. YouTube.
- 100.Coe IR, Wiley R, Bekker LG: Organisational best practices towards gender equality in science and medicine. Lancet 2019, 393(10171):587–593. [DOI] [PubMed] [Google Scholar]
- 101.Wang TY, DesJardin JT: Time to End “Manels” in Clinical Trial Leadership. JAMA Intern Med 2020, 180(10):1383–1384. [DOI] [PubMed] [Google Scholar]
- 102.HeForShe. In. Edited by @HeForShe.
- 103.Else H: How to banish manels and manferences from scientific meetings. Nature 2019, 573(7773):184–186. [DOI] [PubMed] [Google Scholar]
- 104.Suarez-Lledo V, Alvarez-Galvez J: Prevalence of Health Misinformation on Social Media: Systematic Review. J Med Internet Res 2021, 23(1):e17187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Patrick M, Venkatesh RD, Stukus DR: Social media and its impact on health care. Ann Allergy Asthma Immunol 2022, 128(2):139–145. [DOI] [PubMed] [Google Scholar]
- 106.Wang Y, McKee M, Torbica A, Stuckler D: Systematic Literature Review on the Spread of Health-related Misinformation on Social Media. Soc Sci Med 2019, 240:112552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, Hoving C: A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res 2013, 15(4):e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Koenderman L, Montecucco F, Nathoe H: Science and the social media: Time for a reset. Eur J Clin Invest 2021, 51(8):e13643. [DOI] [PubMed] [Google Scholar]
- 109.D’Souza MS, Dong TA, Ragazzo G, et al. : From Fad to Fact: Evaluating the Impact of Emerging Diets on the Prevention of Cardiovascular Disease. Am J Med 2020, 133(10):1126–1134. [DOI] [PubMed] [Google Scholar]
- 110.Klein JJ, Schweikart SJ: Does Regulating Dietary Supplements as Food in a World of Social Media Influencers Promote Public Safety? AMA J Ethics 2022, 24(5):E396–401. [DOI] [PubMed] [Google Scholar]
- 111.Golder S, O’Connor K, Hennessy S, Gross R, Gonzalez-Hernandez G: Assessment of Beliefs and Attitudes About Statins Posted on Twitter: A Qualitative Study. JAMA Netw Open 2020, 3(6):e208953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hill JA, al e: Medical Misinformation: Vet the Message! J Am Heart Assoc 2019, 8(3):e011838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Nelson AJ, Puri R, Nissen SE: Statins in a Distorted Mirror of Media. Curr Atheroscler Rep 2020, 22(8):37. [DOI] [PubMed] [Google Scholar]
- 114.@CardioSmart. In.; 2021.
- 115.Alex Bastiany M In. Edited by @AlexBastiany; 2021.
- 116.Cardio-Obstetrics. In. Edited by @CardioOb; 2022.
- 117.Women GRf. In. Edited by goredforwomen; 2022.
- 118.Wei S, Le N, Zhu JW, et al. : Factors Associated With Racial and Ethnic Diversity Among Heart Failure Trial Participants: A Systematic Bibliometric Review. Circ Heart Fail 2022, 15(3):e008685. [DOI] [PubMed] [Google Scholar]
- 119.Minhas AS, Ogunwole SM, Vaught AJ, et al. : Racial Disparities in Cardiovascular Complications With Pregnancy-Induced Hypertension in the United States. Hypertension 2021, 78(2):480–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Erin D Michos MD. In. Edited by @ErinMichos; 2022.


