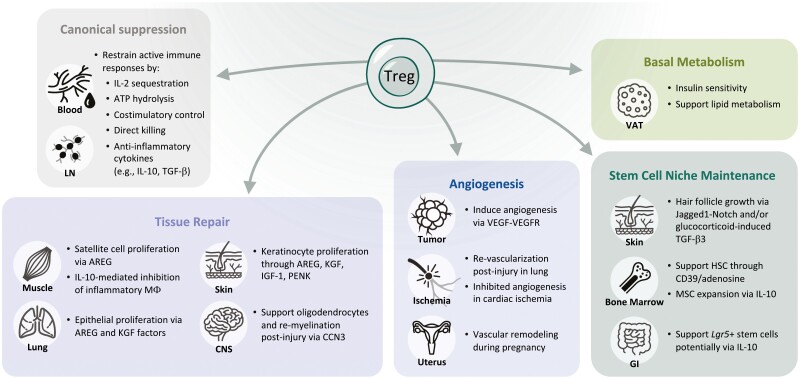
Figure 1:
Diverse functions of Tregs beyond immune suppression. As detailed in the canonical suppression box, Tregs use several mechanisms to dampen proliferation and function of effector T cells and other immune cells. Tregs also have myriad effects on tissue repair, angiogenesis, basal metabolism, and maintenance of the stem cell niche. Roles in tissue repair and mostly been documented in the muscle, lung, skin, and central nervous system (CNS). Treg-secreted AREG, and KGF are critical for inducing proliferation of epithelial cells in the lung and skin and satellite cells in the muscle. In the CNS, Tregs can support oligodendrocytes ability to re-myelinate neurons following injury. Tregs can be pro- or anti-angiogenic depending on the tissue and model. Tregs have been the most well studied and have a clear role in supporting angiogenesis in tumors to enable growth. Their role in ischemia is less clear: Tregs are required for re-vascularization in the lung following injury but appear to inhibit angiogenesis following cardiac ischemia. Tregs also support vascular remodeling that occurs in the uterus during pregnancy. Fat Tregs, specifically those in the visceral adipose tissue (VAT), are the best described tissue Tregs and have clear roles in regulating insulin sensitivity and supporting lipid metabolism. Finally, Tregs support the unique stem cell niches in the skin, bone marrow, and the gut. Through diverse mechanisms, they can directly maintain stem cell quiescence and indirectly affect these cells by restricting expansion of supportive mesenchymal stromal cells. Overall, while some of these findings have been validated in humans, it is important to note that much of the data comes from studies in mice.