Abstract
Identification and characterisation of novel targets for treatment is a priority in the field of psychiatry. FKBP5 is a gene with decades of evidence suggesting its pathogenic role in a subset of psychiatric patients, with potential to be leveraged as a therapeutic target for these individuals. While it is widely reported that FKBP5/FKBP51 mRNA/protein (FKBP5/1) expression is impacted by psychiatric disease state, risk genotype and age, it is not known in which cell types and sub-anatomical areas of the human brain this occurs. This knowledge is critical to propel FKBP5/1-targeted treatment development. Here, we performed an extensive, large-scale postmortem study (n = 1024) of FKBP5/1, examining neocortical areas (BA9, BA11 and ventral BA24/BA24a) derived from subjects that lived with schizophrenia, major depression or bipolar disorder. With an extensive battery of RNA (bulk RNA sequencing, single-nucleus RNA sequencing, microarray, qPCR, RNAscope) and protein (immunoblot, immunohistochemistry) analysis approaches, we thoroughly investigated the effects of disease state, ageing and genotype on cortical FKBP5/1 expression including in a cell type-specific manner. We identified consistently heightened FKBP5/1 levels in psychopathology and with age, but not genotype, with these effects strongest in schizophrenia. Using single-nucleus RNA sequencing (snRNAseq; BA9 and BA11) and targeted histology (BA9, BA24a), we established that these disease and ageing effects on FKBP5/1 expression were most pronounced in excitatory superficial layer neurons of the neocortex, and this effect appeared to be consistent in both the granular and agranular areas examined. We then found that this increase in FKBP5 levels may impact on synaptic plasticity, as FKBP5 gex levels strongly and inversely correlated with dendritic mushroom spine density and brain-derived neurotrophic factor (BDNF) levels in superficial layer neurons in BA11. These findings pinpoint a novel cellular and molecular mechanism that has potential to open a new avenue of FKBP51 drug development to treat cognitive symptoms in psychiatric disorders.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00401-023-02541-9.
Keywords: FKBP5, FKBP51, Psychosis, Depression, Ageing, Stress, Single cell, Postmortem brain
Introduction
Severe psychiatric disorders—including schizophrenia, major depression and bipolar disorder—present a huge burden for individuals, society and the healthcare system. While there are efficacious treatments, relapse, resistance and chronicity are common, and cognitive symptoms in particular are not adequately treated [28, 58]. A major issue is that the approved use of available drugs and treatments for specific psychiatric diagnoses, and their prescription to specific patients, are currently not based on biological knowledge of the pathological mechanisms that contribute to an individual’s disease presentation. Increased understanding of the molecular underpinnings of psychiatric disease, from the level of genes, to molecular and cell-type contributions, is critical to facilitate mechanism-based diagnoses and to pinpoint the corresponding biological targets for treatment [66]. Despite decades of research, there are very few genes that have been translated from genetic association to a more mechanistic understanding of how this translates on the molecular and cellular levels and ultimately influences disease risk. This is an essential next step to both improve biological classification of psychopathology, and to drive treatment discovery.
FK506 binding protein 51 kDa (FKBP51), encoded by the FKBP5 locus on chromosome 6p21.31, is a gene with strong evidence that it cross-diagnostically contributes to the pathogenesis of psychiatric disorders in a subset of patients. FKBP51 is an allosteric heat shock protein 90 kDa (HSP90) co-chaperone of the glucocorticoid receptor (GR), which is highly responsive to glucocorticoid (cortisol)-mediated stress via 5′ upstream and intronic glucocorticoid-responsive gene-regulatory elements (GRE) [10, 43]. As such, FKBP5/1 is physiologically important for propagating as well as terminating the stress response [76]. Glucocorticoid-induced expression of FKBP5 has been shown to be moderated by both, genetic variation and epigenetic changes at the 5′ upstream and intronic GREs [34, 76]. While FKBP5/1 expression increases over the life course, even in healthy individuals [6, 17, 43, 69, 77], expression that exceeds this neurotypical rise during ageing is likely to be harmful. Our previous studies indicate that amplified FKBP5 expression can be mechanistically caused by a combination of an FKBP5 risk haplotype (tagged by the single-nucleotide polymorphism [SNP] rs1360780 T allele in intron 2) and lasting reduction in DNA methylation in GRE induced by GR binding in the context of early life adversity [34, 36]. In fact, a large number of studies highlight that the combination of this risk haplotype and exposure to early life adversity associates with increased risk for a range of psychiatric disorders, including post-traumatic stress disorder, major depression and also psychosis [43]. This may be mediated by a genetic moderation of effects of exposure to adversity on transdiagnostic intermediate risk factors and symptoms, such as on cognition, self-regulation and activity of limbic brain circuits, thus altering developmental trajectories to risk [19, 21, 26, 70]. This increase in risk is most likely related to a combined, genetic and epigenetic disinhibition of FKBP5 expression [34]. In rodent models, heightened FKBP5/1 expression in the brain has been shown to cause psychiatric-like phenotypes, including impaired stress-coping behaviour, increased anxiety and weakened extinction learning [11, 12, 22]. Also some human postmortem brain studies show a correlation of increased FKBP5 expression with psychiatric disease, including bipolar disorder, autism, schizophrenia and alcohol abuse in different brain regions such as the frontal cortex, the cerebellum and the hippocampus [23, 54, 62, 63]. Interestingly, decreased expression has been observed with post-traumatic stress disorder in the subgenual prefrontal cortex [25].
While there is strong evidence for increased FKBP5/1 expression (via genetic and epigenetic factors) contributing to psychiatric disease risk [76], how these factors coalesce in the human brain, especially in a cell type-specific manner, to raise risk to psychopathology or contribute to specific symptom domains is unknown. Yet, this likely holds an important key to understanding FKBP5/1’s role in pathogenesis, as the brain is where many psychiatric symptoms manifest.
The extensive evidence of heightened FKBP5/1 expression as a risk factor for psychiatric disorders has spurred the development of small-molecule FKBP5 antagonists as novel therapeutics [13, 43]. These agents have a promising profile of effects, with preclinical experiments in rodents showing that FKBP51 antagonists improve stress-coping behaviour and reduce anxiety when given systemically or directly into relevant brain regions such as the amygdala [13, 22]. To further fine-tune development of this drug class, comprehensive characterisation of FKBP5/1 at the molecular level, with cell-type specificity, is urgently needed. Moreover, information on the status of FKBP5/1 directly in the human brain is required, given the brain is where psychotropic medications are most likely to exert their effects and that baseline differences in expression levels could alter the outcomes of a drug’s intended mechanism.
In the most comprehensive study to date, we examined a large collection (total n = 1024) of human postmortem samples from the neocortex (Brodmann areas [BA] 9, 11 and ventral BA24/BA24a) of individuals who lived with schizophrenia, major depression or bipolar disorder compared to matched controls (Table 1). These brain areas are highly implicated in psychiatric disorders, associated with hallmark symptoms of transdiagnostic psychopathology such as executive functioning, emotion and working memory processes [1]. We used bulk and single-cell omics approaches and histological methods to explore the effects of disease state, genotype and age on the cell type- and cortical layer-specific patterns of FKBP5/1 expression; importantly, we provide replication across six independent cohorts and robust validation of our results using multiple methods (e.g. seven different ways to assess FKBP5/1: bulk sequencing, single-nucleus sequencing, exon arrays, qPCR and RNAscope, immunoblot and immunofluorescence staining). Our results provide a new contribution to the field, indicating that the effects of disease state and age converge on the superficial layer LII–III neurons in both the granular and agranular areas of the neocortex we examined, thus pinpointing a clear cellular target for further study and future drug development.
Table 1.
Summary of cohorts, methods, and analyses conducted
| Cohort and brain region | Diagnosis (n) | n | Age range (years) |
Sex (M/F) | Method | Analyses |
|---|---|---|---|---|---|---|
|
Cohort 1, BA9 [64] Lieber Institute for Brain Development, USA |
All controls: lifetime sample, prenatal to adult Case–control: Controls: subset of all control subjects >14 years Schizophrenia Major depression Bipolar disorder |
340 179 121 144 63 |
14weeks-85 14–85 17–96 14–75 21–76 |
228/112 137/42 80/41 87/57 35/28 |
Bulk RNA sequencing |
Lifetime FKBP5 gex (all controls) Case–control differences in FKBP5 gex Case–control differences in FKBP5 gex ageing trajectories |
| SNP genotyping |
Effects of rs1360780 SNP on FKBP5 gex and DNAm Effects of rs1360780 SNP on FKBP5 gex and DNAm ageing trajectories |
|||||
|
Cohort 2, BA9 [59] Victorian Brain Bank at the Florey Institute for Neuroscience and Mental Health, AUS |
Controls Schizophrenia Major depression Bipolar disorder |
62 68 24 15 |
22–80 18–82 19–87 31–79 |
49/13 54/14 12/12 7/8 |
Exon array |
Case–control differences in FKBP5 gex Case–control differences in FKBP5 gex ageing trajectories |
|
Controls Schizophrenia Major depression Bipolar disorder |
20 20 20 16 |
32–80 30–82 27–87 31–79 |
11/9 11/9 11/9 8/8 |
Immunoblot |
Case–control differences in FKBP51 protein Case–control differences in FKBP51 protein ageing trajectories Correlation of FKBP5 gex (exon array) and FKBP51 protein levels in the same subjects |
|
|
Cohort 3, BA9 Neurobiobank at the Ludwig-Maximilians-University, GER |
Controls | 24 | 37–82 | 13/11 | Quantitative PCR | FKBP5 gex ageing trajectory in controls |
| Immunoblot |
FKBP51 protein ageing trajectories in controls Correlation of FKBP5 gex (qPCR) and FKBP51 protein levels in the same subjects |
|||||
| Single-molecular in situ hybridisation (RNAscope) |
Cortical layer specificity of FKBP5 long and short variants Layer-specific ageing trajectories of FKBP5 long and short variants |
|||||
| Immunohistochemistry | FKBP51 protein neuronal staining throughout the BA9 cortical layers | |||||
|
Cohort 4, BA24a Stanley Neuro-pathology Consortium |
Controls Schizophrenia Major Depression Bipolar Disorder |
15 15 15 15 |
29–68 25–62 30–65 25–61 |
9/6 9/6 9/6 9/6 |
Immunoblot |
Case–control differences in FKBP51 protein Case–control differences in FKBP51 protein ageing |
| Immunohistochemistry |
Case–control differences in FKBP51 protein in superficial vs lower layers Case–control differences in FKBP51 protein ageing trajectories |
|||||
|
Cohort 5, BA11 NSW Tissue Resource Centre, AUS |
Controls Schizophrenia |
33 36 |
32–82 26–84 |
20/13 11/25 |
Single-nucleus RNA sequencing |
FKBP5 specificity in distinct cell-type clusters Case–control differences and ageing effects in FKBP5 gex across cell-type clusters |
|
Controls Schizophrenia |
8 11 |
32–73 49–84 |
5/3 9/2 |
Golgi–Cox staining [31] | Correlation of FKBP5 gex with dendritic spine subtypes (mushroom, stubby, filopodia and thin) and BDNF gex in the superficial cortical layer | |
|
Cohort 6, BA9 [51] Douglas–Bell Canada Brain Bank, CA |
Controls Major Depression |
17 17 |
18–87 19–82 |
17/0 17/0 |
Single-nucleus RNA sequencing |
FKBP5 specificity to distinct cell-type clusters Case–control differences and ageing effects in FKBP5 gex across cell-type clusters |
Materials and methods
Human postmortem brain samples
FKBP5 gene expression (gex) and FKBP51 protein expression were examined in the human cortex from 1024 individuals across six postmortem brain cohorts (n = 895 specimens from BA9, n = 69 specimens from BA11, n = 60 specimens from BA24a) (Table 1). Informed consent was given by all donors or their next of kin; extensive details regarding collection, dissection and ethical approvals for each cohort are included in the online resource (Online Resource, Supplementary Tables 1, 2, 3, 4, 5, 6).
Bulk RNA sequencing (Cohort 1)
Bulk RNA sequencing methods have been previously described [64]. High-throughput sequencing was performed on the final cDNA library using the HiSeq 2000 (Illumina, San Diego, CA, USA), with the Illumina Real Time Analysis module used for image analysis and base-calling and the BCL Converter (CASAVA v1.8.2) to generate FASTQ files with sequencing pair-end 100 bp reads. Splice-read mapper TopHat (v2.0.4) was used to align reads to the human genome reference (UCSC hg19), with known transcripts provided by Ensembl Build GRCh37.67. Mapped reads covering the genomic region of FKBP5 (chr6:35,541,362–35,696,397, GRCh37/hg19) were acquired. Reads covering each exon or unique exon–exon junction level were called using featureCounts (V1.5.0) [40]. Individual raw exon and junction reads were divided by the mapped total reads per subject and log normalised to account for skewedness (log2 fragments per kilobase million [FPKM]). We assessed reads covering a junction common to all FKBP5 transcripts spanning from Exon 5 to Exon 6 (chr6:35,565,191–35,586,872).
SNP genotyping (Cohort 1)
Genomic DNA from postmortem brain Cohort 1 was extracted from 100 mg of pulverised cerebellum tissue with the phenol–chloroform method. SNP genotyping was performed with the HumaHap650Y_V3 or Human 1 M-Duo_V3 BeadChips (Illumina) according to manufacturer’s instruction as previously described [64]. The rs1360780 FKBP5 single-nucleotide polymorphism (SNP) was extracted from the dataset. This SNP has been shown to affect FKBP5 chromatin shape and transcription [36].
Exon arrays (Cohort 2)
This method has been previously described [59]. Briefly, total RNA from Cohort 2 was isolated using TRIzol reagent (Life Technologies, Scoresby, VIC, Australia) and RNeasy mini kits (Qiagen, #74,104, Chadstone Centre, VIC, Australia). RNA quality and quantity were assessed and samples with RINS of 7 or greater were deemed suitable for further analyses with the Affymetrix Human Exon 1.0 ST Array according to the manufacturer’s instructions (Affymetrix, Santa Clara, CA, USA). After hybridisation, chips were scanned and the signals converted into a DAT file for quality control, and CEL and CHP files were generated. Exon array data were used as a replication for the RNAseq gex analyses in Cohort 1 and followed the same statistical methods. For FKBP5 gex measures, we analysed signal from FKBP5 exon 5 (ENSE00000747342.1) which sits adjacent to the FKBP5 exon–exon junction used to assess total FKBP5 gex in Cohort 1.
Quantitative real-time PCR (Cohort 3)
mRNA levels of FKBP5 transcripts in Cohort 3 were measured using qRT-PCR. 40 mg of grey matter was dissected from each tissue block. RNA was extracted and RIN quantified as for RNA sequencing in Cohort 1. cDNA was synthesised from 500 ng of RNA using the Maxima H Minus Reverse Transcriptase system (ThermoFisher Scientific). PCR conditions were set to 94 °C for 5 min, 40 cycles of 94 °C for 30 s, 60 °C for 30 s, 72 °C for 30 s, and 72 °C for 7 min after the last cycle. Primer pairs were designed to amplify the unique junctions for total FKBP5 gex (Online Resource, Supplementary Table 7), using customised TaqMan Gene Expression Assays (Applied Biosystems, Foster City, CA, USA) and the Lightcycler 480 (Roche, Basel, Switzerland). Gex levels of FKBP5 was normalised to geometric means of the constitutively expressed genes β-actin (ACTB) and glyceraldehyde-3-phosphate dehydrogenase (GAPDH). Samples were measured in quadruplicate and averaged.
Single-molecule in situ hybridisation (RNAscope) (Cohort 3)
To quantify the gex and examine cortical localisation of FKBP5 alternative transcripts, single-molecule in situ hybridisation was performed on 16 µm sections from Cohort 3 using the RNAscope V2 kit (Advanced Cell Diagnostics, Newark, CA, USA) according to the manufacturer’s instructions for the RNAscope® Part 1, Fresh Frozen Tissues protocol and the Multiplex Version 2 User Manual Part 2 (ACD). Two hybridisation probes were customised to target either FKBP5 long transcripts (V1-3; 91,000-2041 bp) or FKBP5 short transcript (V4; 1475–2968 bp). Total FKBP5 gex was calculated by summing these probes together. TSA fluorophores for cyanine 3 and cyanine 5 (Perkin Elmer) were used at a concentration of 1:1000. Slides were counterstained with DAPI. Autofluorescence eliminator reagent (Merck Millipore-2160) was applied to reduce autofluorescence and slides were mounted with Aqua-Poly/Mount medium (Polysciences). Consistent regions of interest were identified based on gyri formation, with the anterior most point of each section imaged on a Leica SP8 confocal microscope. 11 z-stack images were taken at 0.5 µm distance of the superficial (LII–III) and deep layers (LIV–VI) based on visual nuclei morphology, density and distance to the cortex edge or white matter. FKBP5 long transcript probes were detected with cyanine 3 at 570 nm, and the short transcript in cyanine 5 at 650 nm. Optimal exposure time and image processing procedures were determined using positive controls (POL2RA for the long transcripts and PPIB for the short transcript), which were undetectable in sections hybridised with the negative control probe DapB. Fiji software [61] was used to merge the 11 z-stacks, adjust thresholds, and automatically quantify the number of nuclei and transcripts for each probe, with one dot representing one transcript. The number of dots was normalised to the number of nuclei, and the average for each subject was calculated.
Immunoblot (Cohort 2, 3 and 4)
Relative protein densities of FKBP51 were determined by immunoblot in Cohort 2, 3 and 4. 10 mg of grey matter from each block was homogenised and protein concentration determined using BCA assays. Samples were loaded in duplicate at a loading concentration of 20 µg of total protein per lane and electrophoresed as previously described [42]. Membranes were then incubated overnight at 4 °C with a validated primary antibody diluted with TBST containing 1% skim milk, followed by washing and secondary antibodies (Online Resource, Supplementary Table 8). Primary antibody specificities were validated in FKBP51 knockout (KO) cells, generated from the SH-SY5Y human neuroblastoma cell line using CRISPR-Cas9 (Online Resource, Supplementary Fig. 1). Enhanced chemiluminescence was applied. The blots were visualised with the BioRad ChemiDoc XRS+ (Cohort 2) or the Amersham 6000 Gel Imager (GE Healthcare, Cohort 3) and quantified with Image Lab Software (BioRad). Membranes were re-probed and normalised to a loading control (Cohort 2: anti-β-actin polyclonal antibody Santa Cruz Biotechnology, Dallas, TX USA #sc-1616, 1:3000; Cohort 3: glyceraldehyde 3-phosphate dehydrogenase Abcam #ab9485, 1:2500). Densitometry values for each sample were normalised to the respective loading control, then to the respective pooled sample to account for gel-to-gel variability. Duplicates were averaged for each sample and the mean of the two primary antibodies taken as the final values.
Immunohistochemistry (Cohort 3 and 4)
To identify and semi-quantify cellular and subcellular localisation of FKBP51 protein, immunohistochemistry was performed in Cohort 3 and 4. A detailed explanation of the staining and quantification methods is included in the Online Resource, Extended Methods. Briefly, fresh frozen sections (14–20 µm) were post-fixed with 4% PFA and antigen retrieval performed using 10 mM citric acid buffer with 0.5% Tween-20 for 10 min. Tissue was permeabilised with 0.3% Triton X-100 in phosphate-buffered saline (PBS) for 5 min and blocked with 10% normal serum and 1% bovine serum albumin, with 0.3 M glycine in PBS at room temperature for 1 h. Sections were incubated with primary antibody solution overnight at 4 °C, and antibodies used are summarised in Online Resource, Supplementary Table 9. Following washing, appropriate secondary antibodies and DAPI were applied. Tissues were counterstained with autofluorescence eliminator reagent (Merck Millipore-2160) and coverslipped with Aqua-Poly/Mount medium. Wide-field microscopy images were acquired on the Leica THUNDER imager (Leica, Germany) and the Leica SP8 confocal microscopes. Images were analysed using ImageJ with the Fiji plugin [61] and QuPath (Version 0.3.2) [2], and cell detection and show detection measurements tools were used to quantify staining. The average intensity of FKBP51 staining per cell type was determined per image for both the FKBP51 detections and the background of the FKBP51 channel, and FKBP51 expression was normalised to the background to account for image-to-image variability. Analysis for Cohort 4 was performed using data acquired on the individual cell level with the data from each cell (e.g. FKBP51 staining intensity) taken as an individual data point and the subject that the cell came from was taken as a covariate [51]. With a dataset of this size (> 6000 cells), normality was assessed with histograms, box plots and qqPlots using ggplot2 in R. Data were log-transformed to achieve normal distribution. On average, data from one of the three acquired images from two subjects had to be excluded from each analysis due to being greater than ± 2 standard deviations from the mean. Analysis was subsequently performed by using parametric tests as per Online Resource, Supplementary Table 10.
Cohort 5 and 6
Single-nuclei RNA sequencing
We performed snRNAseq in Cohort 5 with the 10x Genomics Chromium system (Single Cell 3’ Reagents kit v3.1) with 10,000 nuclei per sample as target recovery. Libraries were pooled equimolarly and treated with Illumina Free Adapter Blocking Reagent before sequencing in two batches on the NovaSeq 6000 System (Illumina). Sequence reads were demultiplexed using the sample index, aligned to a pre-mRNA reference, and UMI were counted after demultiplexing of nuclei barcodes using Cell Ranger v6.0.1. Reads were down-sampled per cell to the 75% quartile of reads per cell (14,786 reads). Count matrices of all individuals were combined and further processed using Scanpy v1.7.1. Nuclei were filtered according to counts, minimum genes expressed and % of mitochondrial genes (counts < 500, genes < 300, Mito% ≥ 15). Genes expressed in < 500 nuclei were removed. Data were normalised and log-transformed using sctransform. Leiden clustering using highly variable genes was applied for clustering. A label transfer algorithm (scarches v0.4.0) was used for an initial cell-type assignment. Cell-type labels from the Allen Brain Atlas (Human M1 10x) were used as a reference. Initial assignments were refined by a manual curation based on marker gene expression [51, 65]. Cells were scaled to 10,000 reads (raw counts), and FKBP5 expression values per single cell were extracted and averaged per subject to obtain a pseudo cell per subject per identified cell type. Excitatory neuron sub-clusters Ex L4-6_2, Exc_L5-6_HTR2C were removed due a high number of zero expressors, which skewed the data and an inability to determine if these were biological or technical dropouts. Exc_7 and Exc_20 were clusters where the cortical layer of origin could not be determined, and they were also removed. We also analysed Cohort 6 10x Genomics Chromium data (v2 chemistry) previously described [51]. Ex 1, Ex 5 and Ex 9 were also removed due a high number of zero expressors. Data were processed with Cellranger and Seurat to identify cell-type clusters. The FindAllMarkers function was used with the bimodal test and logfc.threshold of log(2), with other parameters set to default. FKBP5 expression per single cell was extracted. All cells were scaled to 10,000 reads and then averaged per subject to create a pseudo cell per subject per classified cell type in the dataset.
Golgi–Cox staining
Golgi–Cox staining was performed in a subset of Cohort 5 (BA11) as previously described [31] and is described in detail in the Online Resources, Extended Methods. Briefly, fresh frozen tissue blocks (~ 0.5 cm) were stained using the FD Rapid GolgistainTM Kit following the manufacturer’s instructions (FD Neurotechnologies, Columbia, MD, USA). Microscopy was completed using bright-field imaging (DMi8; Leica Microsystems, Wetzlar, Germany). Cortical layers I–VI (LI–VI) were defined according to morphological features [68] and dendritic spines on superficial and deep layer pyramidal neurons were measured using an optical fractionator method to randomly select coordinates within each layer [31]. This was repeated until three to six pyramidal neurons were imaged in the superficial and deep layers. A total of 12,144 dendritic spines were quantified in LII/III of BA11 in Cohort 5 and analysed for correlation with superficial layer FKBP5 gex snRNAseq data.
Statistics
Analyses were performed in R v3.3.1 (https://www.r-project.org). A summary of the statistics implemented has been included in the Online Resource, Supplementary Table 10. All reported P values from lm analyses were calculated from t statistics computed from the log-fold change and its standard error from each multiple regression model. To account for multiple testing, false discovery rate (FDR) correction was computed for all P values obtained comparing different diagnoses (schizophrenia/depression/bipolar vs control) within each statistical test, using an a priori standard FDR cutoff value of 0.05 [4]. To account for the increased chance of type 1 error due to many data points [18], we considered only significant FDR-corrected P values with effect sizes that are likely to have biological significance (correlation R > 0.25 and mean expression differences > 10%).
Results
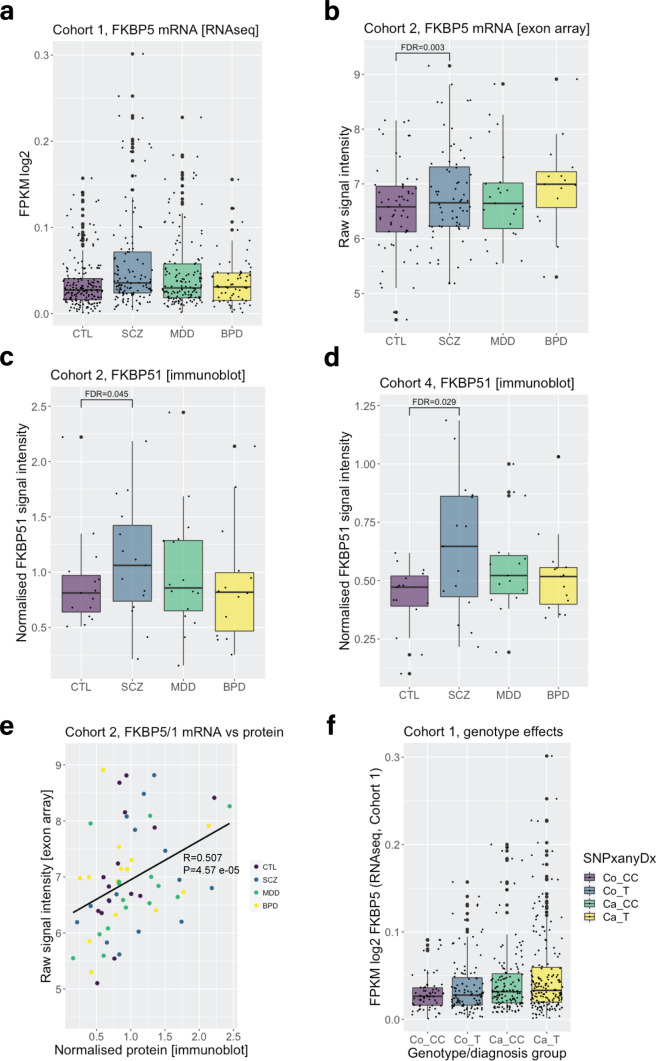
FKBP5 mRNA and FKBP51 protein levels are higher in schizophrenia subjects in the dorsolateral prefrontal cortex (BA9)
To comprehensively understand how the expression patterns of FKBP5 gex and FKBP51 protein are altered in severe psychopathology, we explored the largest sample to date to assess FKBP5 cortical expression differences in cases compared to controls (see Table 1 for explanation of postmortem cohorts and sample sizes). In Cohort 1, we observed a striking + 28.0% mean expression difference in FKBP5 gex in all cases vs controls measured by RNAseq (Cohort 1, n = 507: t = 3.299, P = 0.001043,). Post hoc analysis revealed that this was driven by + 39.8% higher FKBP5 gex in subjects with schizophrenia (t = 3.226, P = 0.001403, FDR = 0.004209) and depression (+ 23.86%; t = 2.478, P = 0.01377, FDR = 0.020655) (Fig. 1a). We replicated this finding in an independent sample (Cohort 2, n = 169, see Table 1) using a different method (exon arrays), and found higher FKBP5 gex in cases vs controls overall (t = 3.325, P = 0.001117), again driven by the schizophrenia subjects (t = 3.348, P = 0.00112, FDR = 0.00336) (Fig. 1b). At the protein level, we found FKBP51 protein was also higher specifically in schizophrenia vs controls (Cohort 2: t = 2.580, P = 0.0149, FDR = 0.04470, + 17.3%, Fig. 1c; Cohort 4: t = 2.685, P = 0.00972, FDR = 0.02916, + 18.3%, Fig. 1d). This was consistent with a strong, positive correlation between FKBP5 gex and FKBP51 protein levels across all subjects in Cohort 2 (R = 0.507, P = 4.57E-05, Fig. 1e). Altogether, these results support that FKBP5 gex and protein levels are increased in psychiatric cases vs controls, with the most pronounced effects seen in schizophrenia subjects.
Fig. 1.
Differences in dorsolateral prefrontal cortex FKBP5/FKBP51 expression in schizophrenia, major depression and bipolar disorder vs controls. a In Cohort 1, linear regression modelling revealed FKBP5 expression was significantly increased in subjects with schizophrenia and major depression compared to controls. Gene expression in Cohort 1 was measured with bulk RNA sequencing assessing reads covering an exon–exon junction between exon 5 and exon 6, common to all FKBP5 alternative transcripts (chr6:35,565,191–35,586,872). b In Cohort 2, linear regression modelling revealed that FKBP5 expression was significantly increased in subjects with schizophrenia compared to controls. Gene expression in Cohort 2 was measured with exon arrays assessing signal intensity from FKBP5 exon 5 (ENSE00000747342.1) which sits adjacent to the FKBP5 exon–exon junction used to assess FKBP5 with RNAseq in Cohort 1. c Linear regression modelling revealed FKBP51 protein expression in Cohort 2 was increased in schizophrenia subjects compared to controls. FKBP51 protein expression was measured with immunoblot, with FKBP51 signal intensity normalised to a loading control and pool to account for sample-to-sample and gel-to-gel variability. d Linear regression modelling revealed FKBP51 protein expression in Cohort 4 was increased in schizophrenia subjects compared to controls. FKBP51 protein expression was measured with immunoblot, with FKBP51 signal intensity normalised to a loading control and pool to account for sample-to-sample and gel-to-gel variability. e FKBP5 mRNA and FKBP51 protein expression in Cohort 2 were significantly and positively correlated (all subjects analysed together irrespective of diagnosis, Spearman’s correlation). f In Cohort 1 (RNAseq), we observed a main effect of case status on FKBP5 mRNA expression (B = 0.01144, t = 2.989, P = 0.0.00295), but there was no additive effect of genotype (B = 0.00144, t = – 0.592, P = 0.55399). Abbreviations: Co, control; Ca, Case; CC, CC homozygotes and T, T carriers. “SNPanyDx” indicates that this was across all cases combined. Abbreviations: BPD bipolar disorder, CTL control, gex gene expression, FDR false discovery rate corrected P values (to account for multiple comparisons), MDD major depressive disorder, SCZ schizophrenia, Cohorts detailed in Table 1
No effect of FKBP5 risk genotype on heightened BA9 FKBP5 mRNA levels
Previous studies have reported that FKBP5 gex is differentially induced by glucocorticoids based on the FKBP5 rs1360780 genotype, with minor allele (T) carriers exhibiting the highest levels of FKBP5 gex after such stimulation [33, 48]. We tested for additive effects of this genotype and case status on FKBP5 gex in Cohort 1 in all cases (combined to improve power) vs controls (T carrier/CC, control n = 108/64, schizophrenia n = 69/45, major depression n = 78/62, bipolar disorder n = 32/28; Online Resource, Supplementary Table 11). We observed a main effect of case status on FKBP5 gex (B = 0.01144, t = 2.989, P = 0.0.00295), but there was no additive effect of genotype (B = 0.00144, t = – 0.592, P = 0.55399; Fig. 1f).
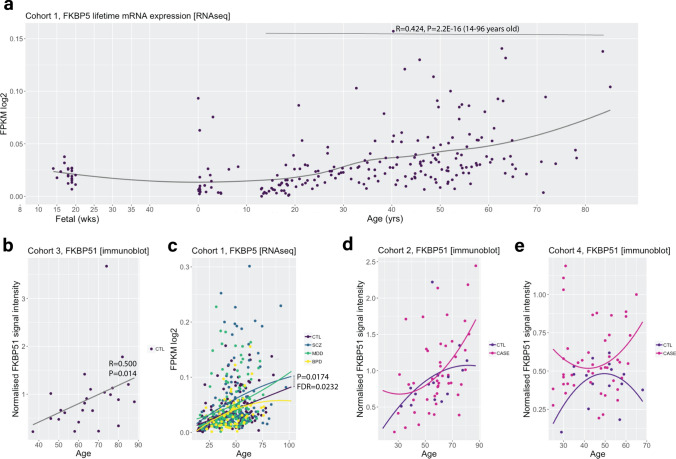
FKBP5 mRNA and bulk FKBP51 protein levels in BA9 increase with age over the human life span
Given age is an important modifier of disease presentation and treatment outcome [46], and reported to impact on FKBP5/1 expression [6, 43, 69], we set out to investigate ageing effects on FKBP5/1 in our cohorts. We firstly characterised the expression pattern of FKBP5 throughout life by analysing a large cohort of BA9 samples from neurotypical controls spanning 14 weeks gestational age to 85 years (Cohort 1; n = 340; Fig. 2a). We found that FKBP5 gex naturally inflected in childhood and adolescence and increased consistently from 14 to 88 years of age (R = 0.424, P = 2.2E-16, Fig. 2a). The strong, positive correlation of gex with age in control adults was also seen in Cohort 2 (Online Resource, Supplementary Fig. 2a; R = 0.61343, P = 1.153E-07) and validated with qPCR using two probes targeting total FKBP5 gex in Cohort 3 (Probe 1, R = 0.460, P = 0.024; Probe 2, R = 0.449, P = 0.028; Online Resource, Supplementary Fig. 2b-c). FKBP51 total protein expression measured with western blot (bulk tissue) was also positively correlated with age in control adults (Cohort 2: R = 0.593, P = 0.022; Cohort 3: R = 0.500, P = 0.014; Fig. 2b). In Cohort 4, FKBP51 and age were not significantly correlated (R = 0.483, P = 0.639; Online Resource, Supplementary Fig. 2d). This is likely because Cohort 4 is younger with only n = 4 subjects over 55 years of age.
Fig. 2.
Effects of age on cortical FKBP5/1 expression levels over the lifetime and in major psychiatric illnesses. a Trajectory of FKBP5 gene expression in control subjects over the life span in BA9, from foetal time points to 88 years of age (Cohort 1, loess fit curve). FKBP5 gene expression increased over the life course in healthy subjects and was positively correlated with age between 14 and 96 years of age (calculated with Spearman’s correlations). b FKBP51 protein expression in BA9 was positively correlated with age in Cohort 3 (calculated with Spearman’s correlations). c FKBP5 ageing trajectory was significantly heightened in schizophrenia subjects vs controls in BA9 (Cohort 1, comparison of nonparametric curves achieved using sm.ancova statistics). d–e FKBP51 protein ageing trajectories were not significant in cases vs controls in Cohort 2 (BA9) or Cohort 4 (B24a). The plots show a comparison of nonparametric curves achieved using sm.ancova statistics. Abbreviations: BPD bipolar disorder, CTL control, MDD major depressive disorder, SCZ schizophrenia, cohorts detailed in Table 1
FKBP5/FKBP51 ageing effects in BA9 are further increased in psychiatric disorders
We then examined the effects of age on FKBP5 gex in cases compared to controls (subjects > 14 years), to determine if having a psychiatric disorder alters the neurotypical increase in FKBP5 gex with age. We initially determined if there was a significant increase in the ageing trajectory by comparing the correlation slopes with sm.ancova. In Cohort 1, FKBP5 gex was more positively correlated with age in schizophrenia subjects vs controls and the ageing trajectory was significantly heightened in the schizophrenia subjects compared to controls (P = 0.0174, FDR = 0.0232; Fig. 2c). To quantify the effect size of the expression difference at older ages, we calculated the mean expression difference in schizophrenia vs control subjects over 50 years, which was + 29.5% higher compared to neurotypical controls over 50 years (t = 2.060, P = 0.02593, FDR = 0.050, Fig. 2c). In Cohort 2, no significant difference in the schizophrenia vs control FKBP5 mRNA ageing trajectory was found (P = 0.056; Online Resource, Supplementary Fig. 2a).
At the protein level in Cohorts 2 and 4, there was not enough statistical power to accurately compare the ageing trajectories in each diagnosis vs neurotypical controls with sm.anova due to too few cases in each diagnosis at older ages. However, given the strong correlation of FKBP5 gex and FKBP51 protein (Fig. 1e), it is likely that the pronounced increase in mRNA with age in schizophrenia also occurs at the protein level. Indeed, the highest FKBP51 protein expression was observed in older cases in both Cohort 2 (Fig. 2d; subjects over 50 years: case protein 0.971 ± 0.464 vs control protein 0.885 ± 0.388, + 9%) and Cohort 4 (Fig. 2e; subjects over 50 years: case protein 0.612 ± 0.201 vs control protein 0.442 ± 0.132, + 27%). These results collectively support that older cases have higher FKBP5 mRNA and likely FKBP51 protein levels compared to neurotypical controls.
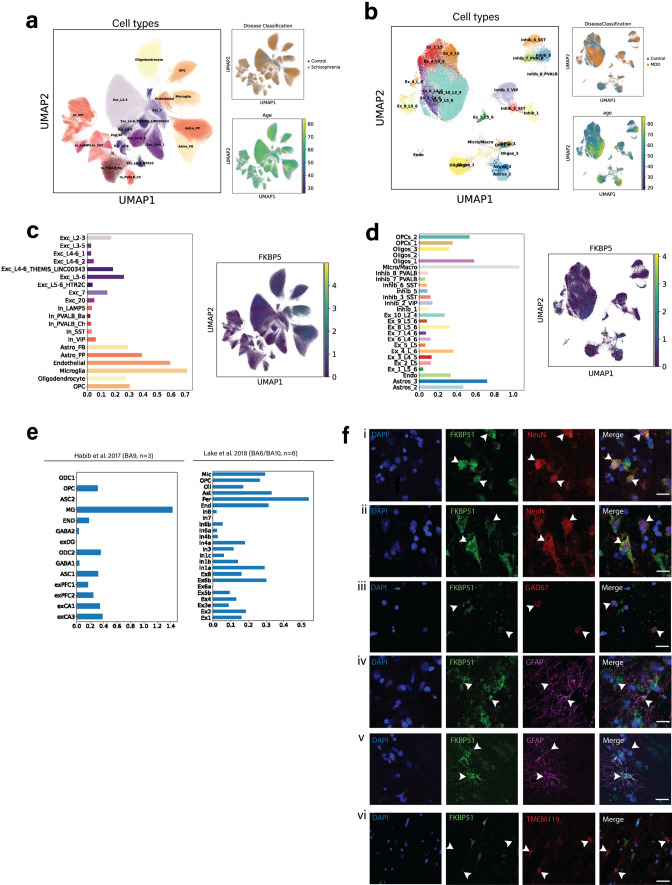
Localisation of FKBP5/FKBP51 expression in multiple areas of the neocortex
To gain deeper insight into the cell-type specificity of heightened FKBP5/1 observed in BA9 and how this may compare to other cortical areas (BA11/24), we assessed FKBP5/1 cell-type distribution and the cortical layer specificity. To date, little is known about the expression patterns of the FKBP5/1 in the human cortex including its cell type and cortical layer distribution. We firstly used single-nucleus RNA sequencing (snRNAseq; Cohort 5 and 6) to examine the levels of FKBP5 gex according to cell type in the granular prefrontal cortex regions BA9 and BA11 (Fig. 3a–d). Among the 20 cell-type clusters in Cohort 5 (BA11, n = 69; Fig. 3a) and 26 delineated cell-type clusters in Cohort 6 (BA9, n = 34; Fig. 3b), FKBP5 gex was most highly expressed in excitatory neurons, microglia and astrocytes (Fig. 3c–d). We also compared our results with other publicly available human prefrontal cortex snRNAseq datasets [20, 38] (Fig. 3e). In BA9 (n = 3) [20], expression was highest in excitatory neurons and microglia. In the adjacent BA6 (agranular)/BA10 (granular) areas (n = 6) [38], the highest levels of FKBP5 were observed in excitatory and inhibitory neurons. High FKBP5 gex in excitatory neurons was thus a consistent finding in both the granular (BA9, 10, 11) and agranular (BA6) regions of the neocortex across the four snRNAseq datasets.
Fig. 3.
Cell-type distribution of FKBP5/FKBP51 expression in the neocortex (BA9, BA10, BA6, BA11). In a Cohort 5 (BA11), and b Cohort 6 (BA9), dimensionality reduction uniform manifold approximation and projection (UMAP) plots depicting total cells across all individuals. The colours indicate the delineated sub-cell type clusters (left of each panel), the distribution of diagnosis across the clusters (top right), and the distribution of age across clusters (bottom right). In c Cohort 5 and d Cohort 6, bar plots show the average FKBP5 gene expression per cell-type cluster, as well as FKBP5 expression across cell clusters. e Bar plots showing the average FKBP5 gene expression per cell type cluster in previously published datasets [20, 38] f Co-localisation of FKBP51 protein expression (green) with nuclear marker DAPI (blue) and (i) NeuN+ neurons (red) in the superficial layer layer; (ii) NeuN+ neurons in the deep layer; (iii) GAD67+ neurons; (iv–v) GFAP+ astrocytes (top showing no colocalization and bottom showing strong colocalization); (vi) TMEM119+ microglia. Scale bar for all images = 20 µm
Immunohistochemistry in BA9 (Cohort 3) confirmed high FKBP51 protein expression in the soma and nucleus of both NeuN+ (Fig. 3f, i–ii) superficial/deep respectively) and GAD67+ (Fig. 3f, iii) cortical neurons. FKBP51 staining intensity was lower and more inconsistent on the glia. For example, GFAP+ astrocytes had highly variable levels of FKBP51 expression, with some cells showing little visually detectable FKBP51 expression (Fig. 3f, iv), and others showing high expression throughout the entire astrocyte (Fig. 3f, v). We also found FKBP51 was localised on some but not all TMEM119+ microglia, albeit with lower expression than in neurons (Fig. 3f, vi).
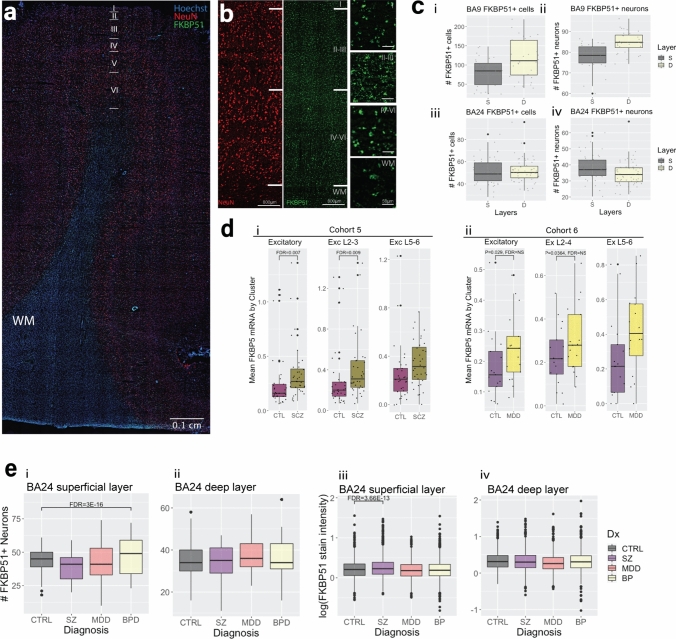
To localise these observations to cortical layers, entire tilescan images of FKBP51 staining were evaluated in both granular (BA9; Cohort 3) and agranular (BA24a, neurotypical controls of Cohort 4) regions of the neocortex (Fig. 4a–b). In BA9 (Cohort 3), FKBP51+ cells (all cell types) were observed both in the superficial layers (LII–III) and the deeper layers (LV–VI; 55% in superficial and 71% in deep, Fig. 4c, i). Additionally, 80% of superficial layer NeuN+ neurons and 84% of deep layer neurons were FKBP51+ in BA9 (Fig. 4c, ii). High levels of FKBP51 expression, but with somewhat different distribution, were also observed in BA24a (Cohort 4), with 91% of cells (all types) in the superficial layer (LII–III) being FKBP51+ and in the deeper layers (LV–VI) 64% were FKBP51+ (Fig. 4c, iii). Additionally, 65% of superficial and 72% of deep layer NeuN+ neurons were FKBP5+ in BA24a (Fig. 4c, iv). This suggests that in both the granular (BA9) and agranular (BA24a) regions of the neocortex studied, FKBP51 is highly expressed on NeuN+ neurons, although the distribution patterns vary in line with the differing cytoarchitecture of these areas [53]. It was not possible to accurately quantify the proportions of FKBP51+ glia due to the inconsistent staining on cell bodies and processes. Overall, snRNAseq and immunohistochemistry both support that the most consistent and intense FKBP5/1 gex/staining was localised on excitatory neurons with slightly varied expression across cortical layers.
Fig. 4.
Case–control differences in FKBP5/1 levels in superficial vs deep layer cortical layer excitatory neurons. a Representative tilescan image showing FKBP51 staining in a section of BA9 cortex. b Same image at higher magnification showing the pattern of NeuN neuronal staining (red) and FKBP51 staining (green) across the cortical layers. Layers ~ II–III denote the superficial cortex, layers ~ V–VI denote the deep cortex and WM denotes the white matter. c Box plots showing the number of FKBP51+ cells (left) and neurons (right) in BA9 (i–ii) and in BA24a (iii–iv). S denotes the superficial layer, and D denotes the deep layer. d snRNAseq data from Cohort 5 (i) and Cohort 6 (ii) showing FKBP5 gene expression levels in the excitatory neuron group (total, left), excitatory neurons from cortical layer 2–4 (Exc 2–4, middle) and layer 5–6 (Exc 5–6, right) in control (CTL) vs schizophrenia (SCZ) and major depressive disorder (MDD). FKBP5 expression was significantly higher in schizophrenia, but not depression, vs controls after correcting for multiple comparisons. Data were analysed using linear regression modelling. e Box plots of immunohistochemistry data demonstrating the number of FKBP51+ neurons in (i) the superficial layer and (ii) the deep layer in each psychiatric disorder, as well as the intensity in the superficial (iii) and deep layers in each psychiatric disorder. All differences illustrated with box plots were calculated with linear regression modelling. Abbreviations: CTRL controls, SZ schizophrenia, MDD major depressive disorder, BP bipolar disorder
Cell-type specificity of heightened FKBP5/1 expression in psychopathology
We next assessed case–control differences in FKBP5 gex within our single cell-type snRNAseq clusters. In Cohort 5 (BA11, schizophrenia vs control n = 69), FKBP5 gex was higher in schizophrenia vs controls in all cell-type groups except inhibitory neurons (output of all comparisons in Online Resource, Supplementary Table 12). Given our finding of strong co-localisation of FKBP5/1, specifically on NeuN+ pyramidal neurons, we further examined case–control differences in FKBP5 gex in the excitatory neuron sub-clusters. FKBP5 gex was substantially higher in the excitatory neuron group in schizophrenia (+ 32%, t = 2.969, P = 0.00426, FDR = 0.00746, Fig. 4d, i). Subsequent analysis of FKBP5 gex in the excitatory neuron sub-clusters showed that this increase was specific to the Exc_L2-3 cluster representing LII–III excitatory neurons, with a striking + 37% higher FKBP5 gex in these neurons in schizophrenia vs controls (t = 3.256, P = 0.00186, FDR = 0.0093, Fig. 4d, i). In Cohort 6 (BA9, depression vs control, n = 34), FKBP5 gex expression was + 24.8% higher in depression in the excitatory neuron group, although this did not survive correction for multiple cluster comparisons (t = – 2.327, P = 0.0267, FDR = 0.187; Fig. 4d, ii; Online Resource, Supplementary Table 13 and Supplementary Fig. 3). This increase was again exclusive to the superficial LII–IV excitatory neurons (Ex 10 cluster; + 25%), although the comparison also did not survive multiple correction (t = – 2.190, P = 0.0364, FDR = 0.255; Fig. 4d, ii). There were no other significant depression/control differences between FKBP5 gex in any other cell-type groups, suggesting the heightened FKBP5 gex observed in schizophrenia and possibly to a lesser extent in depression was specific to the superficial layer excitatory neurons.
To extend the superficial layer excitatory neuron finding at the protein level to an agranular neocortical area, we examined Cohort 4 (BA24a) with semi-quantitative immunohistochemistry examining superficial (LII–III) vs deep layer (V–VI) FKBP51+ NeuN+ neurons in cases vs controls. Count and staining intensity data was collected for > 12,000 NeuN+ neurons across all cortical layers. We first examined count data. In the superficial layers, there was no difference in the number of FKBP5+ NeuN+ neurons in schizophrenia or depression, but there was an increase in bipolar disorder vs controls (+ 10% mean difference; t = 10.683, P = 2.00E-16, FDR = 3.00E-16, Fig. 4e, i). There was no difference in the number of FKBP51+ NeuN+ neurons in the deep layers (Fig. 4e, ii). We next examined intensity data. The intensity of FKBP51 staining on superficial NeuN+ neurons was + 11.4% higher in schizophrenia subjects vs controls (t = – 7.408, P < 1.22E-13, FDR < 3.7E-13; Fig. 4e, iii); this increase was not seen in the deep layers (Fig. 4e, iv). In depression, the intensity of FKBP51 expression was – 13.1% lower throughout both the superficial and deep layers (superficial: t = – 9.273, P < 0.001, FDR < 0.001, vs. deep: t = – 4.907, P < 0.001, FDR < 0.001, – 18.30%; Fig. 4e, iii–iv). There was no difference seen in FKBP51 staining intensity in bipolar disorder. These findings suggest that the increase in FKBP5/1 is specific to cortical excitatory neurons of the superficial cortical layers in both granular and agranular areas of the frontal neocortices, with the most pronounced differences observed in schizophrenia subjects.
Age influences FKBP5 and FKBP51 expression in superficial layer excitatory neurons
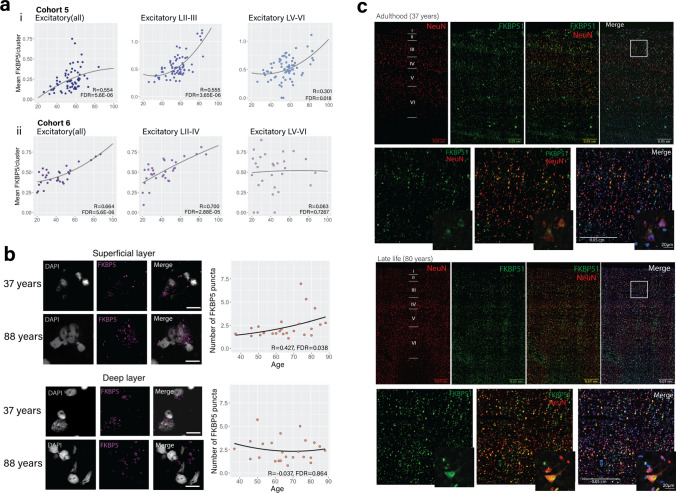
We next checked for ageing effects of FKBP5 gex cell type specifically, by correlating FKBP5 gex and age in all major cell-type clusters (cases and controls combined). In Cohort 5 (BA11), age was correlated with FKBP5 gex in all the major cell-type clusters (Online Resource, Supplementary Table 14). However, the strongest correlation was observed in the excitatory neuron cluster (R = 0.554, P = 8.02e-07, FDR = 5.6E-06), and assessment of the excitatory neuron sub-clusters revealed that the strongest effect was in the superficial layer II-III excitatory neuron cluster (R = 0.555, P = 7.3e-07, FDR = 3.65E-06, Fig. 5a, i). We similarly observed a strong, positive association of FKBP5 gex with ageing in the excitatory neuron cluster in Cohort 6 (BA9; R = 0.664, P = 1.866e-05, FDR = 5.6E-06), and again, assessment of the excitatory neuron sub-clusters revealed that the ageing effect was strongest in, and specific to, the superficial layer 2–4 excitatory neurons (R = 0.700, P = 4.109e-06, FDR = 2.88E-05, Fig. 5a, ii, Online Resource, Supplementary Table 15). RNAscope was used to validate these findings histologically by accurately quantifying the ageing-related changes of FKBP5 transcripts in the superficial vs the deep layers of the BA9 cortex in Cohort 3. Our results also showed a positive correlation of FKBP5 transcript dots and age in the superficial layers of BA9 (R = 0.427, P = 0.018, FDR = 0.038), but not the deep layers (R = – 0.037, P/FDR = 0.864; Fig. 5b). In Cohort 4 (BA24a), we were unable to confirm ageing effects with immunohistochemistry as there were too few subjects at older ages (see Online Resource, Supplementary Table 16). However, in Cohort 3 (BA9), FKBP51 staining intensity was 2.9-fold higher at 88 years compared to 37 years (Fig. 5c). Altogether, these findings consistently show the strong effect of age on FKBP5/1 gene and protein expression is pronounced in superficial layer excitatory neurons across multiple cortical areas.
Fig. 5.
Layer-specific patterns of FKBP51 expression across the neocortex. a snRNAseq data showing FKBP5 gene expression vs age in excitatory neurons (all, left), superficial (LII–III, middle) and deep (LV–VI, left) neuron clusters in (i) Cohort 5 (BA11), and (ii) Cohort 6 (BA9) using Spearman correlations. b RNAscope representative images (left) and results of quantification and analysis with Spearman correlations (right) showing that there was a positive association between FKBP5 gene expression (purple puncta, scale bar = 20 µm) and age in the superficial layers (top) but not the deep layers (bottom). c FKBP51 immunostaining across the BA9 cortex using wide-field microscopy in adulthood (top panel, 37 years old), and later in life (bottom panel, 80 years old). Red represents staining with the neuronal markers NeuN, green represents staining of the FKBP51, and blue represents nuclear staining (Hoechst). The bottom images from each panel are at higher magnification taken from the white rectangle in the top right image. These images demonstrate FKBP51 staining is both high in neurons, and also is more intense (representing higher expression) at older ages
Impacts of elevated FKBP51 expression on dendritic spine architecture
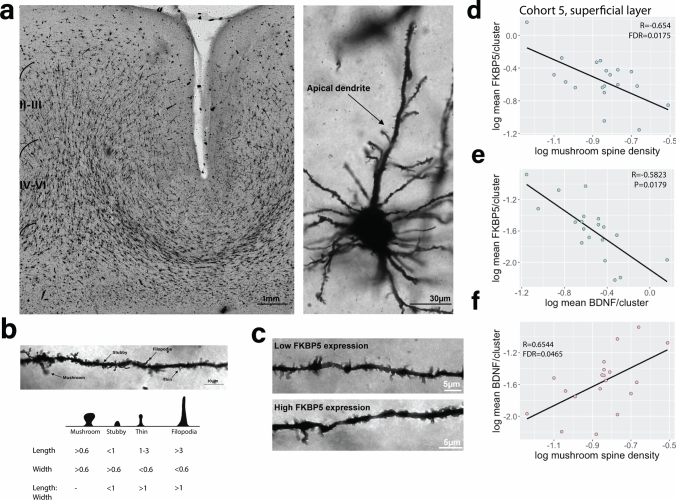
Elevated FKBP5 in the brain has been reported to suppress of glucocorticoid receptor-mediated synaptic plasticity via impacts on dendritic architecture [5, 41, 72]. We therefore determined if the elevated FKBP5 gex levels in BA11 superficial layer neurons in schizophrenia (Cohort 5, snRNAseq gex) correlated with changes in dendritic spine architecture in the same subjects with Golgi–Cox staining and quantification of mushroom, stubby, filopodia and thin dendritic spine subtypes (Fig. 6a–c). While there was a negative correlation of FKBP5 gex levels with dendritic spines (all types), this did not reach statistical significance (R = – 0.4130, P = 0.6858). However, further investigation of individual dendritic spine classes revealed FKBP5 gex levels were strongly inversely correlated with mushroom spine density (R = – 0.6544, P = 0.0044, FDR = 0.01748; Fig. 6d). These data suggest that at least in BA11, the increased levels of FKBP5 gex in superficial layer cortical neurons we consistently observed throughout our study may be related to a decrease in the number of mushroom dendritic spines on superficial layer excitatory cortical neurons.
Fig. 6.
Golgi–Cox staining of dendritic spine subtypes in the orbitofrontal cortex (BA11) and correlation with FKBP5/BDNF gene expression levels analysed with single-nucleus RNA sequencing data derived from the same subjects. a Representative image of a cortical section stained with Golgi-Cox and a stained apical dendrite on a pyramidal neuron. b Classification of different types of dendritic spines: mushroom, stubby, thin and filopodia based on measurements of spine length (base to tip) as well as width (at the widest point) with a photographic example (above) and diagram (below). c Images showing dendritic spine densities in a subject expressing low FKBP5 mRNA levels vs high FKBP5 mRNA levels. Partial correlations accounting for age, PMI and RIN were performed to assess the association between FKBP5 gene expression and d mushroom spine densities and e BDNF gene expression, both showing a strong inverse correlation. f BDNF gene expression and mushroom spine density were strongly positively correlated
Given brain-derived neurotrophic factor (BDNF) is a crucial modulator of dendritic spines [27, 73], and a strong relationship between FKBP5 and BDNF gex levels have been reported [41], we investigated correlations of both FKBP5 gex with BDNF and mushroom spines within the superficial layer neurons in Cohort 5 (BDNF UMAPS: Online Resource, Supplementary Fig. 4). BDNF gex levels were strongly and inversely correlated with FKBP5 gex levels (R = – 0.582288, P = 0.01794; Fig. 6e), as well as being strongly negatively and specifically correlated with mushroom spine density (R = 0.65438, P = 0.01162, FDR = 0.04647; Fig. 6f). These data provide insight into a possible consequence of elevated FKBP5 directly in the human brain, suggesting a strong relationship between FKBP5 and mushroom spine density possibly mediated by BDNF in superficial layer neurons of BA11.
Discussion
With a strong body of evidence from human peripheral blood and preclinical animal studies spurring the development of FKBP51-targeting drugs for psychiatric disorders, it has long been crucial to close the gap on how FKBP51 is cell type-specifically affected directly in the human brain [43]. In this large-scale postmortem study, we showed that cortical FKBP5/FKBP51 mRNA/protein (FKBP5/1) expression levels are consistently increased in psychopathology and exacerbated with age across multiple areas of the neocortex—the dorsolateral prefrontal cortex, the orbitofrontal cortex, and the ventral anterior cingulate cortex—with strikingly higher gene and protein expression levels in individuals with schizophrenia, and depression to a lesser extent. We then traced these effects to the cell-type level to show that they were consistently more pronounced in superficial layer excitatory neurons relative to other cell types across these brain areas, and highly associated with dendritic spine morphology at least in the orbitofrontal cortex. Specifically, we showed that higher levels of FKBP51 inversely correlate with reduced BDNF levels and decreased density of mature dendritic spines on these neurons. These findings might have important implications for the dysregulation of cortical circuitry in individuals with schizophrenia and possibly depression, especially those that are older in age. This opens the door for a novel strategy of therapeutic treatment development.
Cognitive deficits are among the most debilitating and difficult to treat symptoms in psychiatric disorders, particularly schizophrenia, and commonly associated with worse prognosis [47]. Deficits in executive functioning and working memory (dorsolateral prefrontal cortex), motivational, emotional and social behaviour (orbitofrontal cortex) and emotion and pain regulation (anterior cingulate cortex) are all reported in psychopathology and, respectively, largely attributable to the areas examined in this study. These regions are part of the neocortex and organised into layers which vary in their cellular composition and connections, both within each of these areas themselves, and their connections to other brain regions [14, 53]. The dorsolateral prefrontal and orbitofrontal cortices are part of the granular neocortex. In these areas, the superficial layer (LI–III) comprises the upper third of the entire cortex thickness and predominately consists of cortico-cortical connections, whereby superficial layer excitatory neuron subtypes project to other cortical regions and release glutamate on target neurons [9], with dendrites being the functional contacts between them [58]. The anterior cingulate cortex is part of the agranular cortex, which lacks a granular layer (Layer IV). In this area, the superficial layers (LII–III) comprise the upper half of the entire cortex thickness, and the two layers are not well differentiated [53]. The projections of the cells within this area of the cortex are not well characterised in humans, although Layer LII neurons are hypothesised to act as a communication hub to the deeper layers, and in rhesus monkeys, Layer LIII contains projections to other cortical areas including the dorsolateral prefrontal cortex and orbitofrontal cortex [53, 67]. Thus, the alterations to FKBP5/1 we observed in these areas may have widespread consequences for local and inter-region circuitry.
In schizophrenia, differences in the morphology of Layer III neurons in the orbitofrontal cortex [15] and dorsolateral prefrontal cortex are a consistent finding [39], particularly reduced dendritic spine densities on these neurons [24, 50, 55]. Decreased thickness of the cortical laminae and smaller pyramidal neuron size have also been reported in the anterior cingulate cortex (specifically BA24) of schizophrenia subjects [8]. Our finding that heightened FKBP5 in superficial layer neurons in the orbitofrontal cortex is coupled with lower mushroom spine density suggests that there are consequences for circuitry, as the necks of mushroom spines play a crucial role in regulating calcium signalling and the incoming excitatory signal through the synapse, particularly via α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors [37]. This is interesting given that in transgenic mice overexpressing the human FKBP5, FKBP51 exerts effects on chaperone-mediated recycling of AMPA receptors, with high FKBP5 accelerating the rate of AMPA recycling and thus altering AMPA receptor trafficking [7]. Mushroom spines are also the most mature form of dendritic spine, and a reduction in this spine type suggests there are more chronic changes in dendritic spine architecture that may impact on long-term potentiation [1]. In support, knockout of Fkbp5 in mice has been shown to decrease long-term potentiation and increase presynaptic GABA release [57], and transgenic mice overexpressing human FKBP51 display impaired long-term depression as well as spatial reversal learning and memory [7].
Our finding that FKBP5 expression in the orbitofrontal cortex is strongly inversely correlated not only with mushroom spine density, but also the crucial spine modulator BDNF, suggests heightened FKBP5 leads to dysfunctional downstream signalling that may impact synaptic plasticity via BDNF, at least in this brain region [73]. This is consistent with the repeatedly described role of FKBP51 as a molecular hub for many downstream pathways including BDNF [76]. For example, we have previously shown that glucocorticoid-induced FKBP5 expression increases the production of the mature and active form of BDNF via epigenetic mechanisms and enhanced secretion of matrix metalloproteinase 9 (MMP9), which was positively coupled to dendritic spine density [16, 41]. The inverse correlation between FKBP5 and BDNF in the current study is likely related to the direct effects of FKBP51 on DNMT1, leading to increased methylation of the BDNF locus and thus decreased expression [11]. Heightened FKBP5 levels are intertwined with a dysregulated stress response and maladaptive cortisol levels over time [75], with the latter being a common finding in psychopathology [44]. FKBP51 can also be increased via lasting epigenetic disinhibition following exposure to early life adversity, a major common risk factor for psychiatric disease [33, 43]. Elevated glucocorticoid concentrations have been independently shown to cause both increased expression of FKBP5 [48], as well as atrophy and attrition of dendritic spines [30, 45]. Our group and others have also reported that FKBP5 levels in the postmortem orbitofrontal cortex are inversely correlated with dendritic mushroom spine density in mixed psychiatric cases with a history of severely stressful life events [31] and in post-traumatic stress disorder [72]. It should be noted that our dendritic spine data were acquired from the orbitofrontal cortex, which may not be necessarily generalisable to the dorsolateral prefrontal cortex. However interestingly, both excitatory and inhibitory superficial layer neurons in the dorsolateral prefrontal cortex were recently reported to be vulnerable to the effects of psychopathology in schizophrenia, indicating a core network impairment in this sub-region that may originate from gene × environment interactions during development [3]. Our study may indicate that FKBP5 is a contributor in this process given FKBP5 is governed by gene × environment interactions, and its expression is increased via epigenetic mechanisms in the presence of early life adversity [43]. Further study of this hypothesis, specifically in the dorsolateral prefrontal cortex, will be important.
Until now, FKBP5/1 cell-type distribution and expression patterns in the human brain have been largely unknown. We show that FKBP51 is highly and consistently expressed across virtually all cell types in the studied neocortical areas, consistent with the expression of glucocorticoid receptors which are reportedly ubiquitously expressed [52]. We showed that the most pronounced and consistent expression of FKBP5/1 is in excitatory neurons in both the superficial and deep cortical layers across multiple prefrontal cortical areas including BA9, 11, 10, 24, and 6. While FKBP5 snRNAseq expression appeared to be high on microglia and astrocytes, FKBP51 immunostaining in these cells was more inconsistent, with very high staining intensity noted on some cells and undetectable staining on others. Of note, in our snRNAseq experiments, more microglia (and nuclei in total) were captured from cases compared to controls (480 vs 372 respectively [51]), which could contribute to the increased FKBP5 gex observed overall given microglia appear to be high expressors of FKBP5 mRNA. It is also possible that microglia-associated FKBP5 expression may be reflective of increased microglia numbers, which is suggested to occur in psychiatric disorders [30]. Regarding neuronal expression, it should be noted that superficial layer excitatory neurons are functionally diverse with differing projections in cortical circuitry, with these connections also varying according to the cortical area and granularity [49, 74]. Our study did not specifically differentiate between these subtypes. Our immunostaining images from both the dorsolateral prefrontal and anterior cingulate cortices suggested that in these two regions, FKBP51 staining intensity on NeuN+ neurons did not vary according to NeuN+ cell morphology; however, we acknowledge that 20–35% of superficial layer NeuN+ neurons did not express FKBP51. We hypothesise that the lack of expression on certain neurons is more likely to be state dependent, rather than sub-class dependent, given there was no notable sublaminar distribution of FKBP51 in these cortical areas, and FKBP5/1 expression may rapidly fluctuate in response to stress [60].
While it is a strength of this study that our findings were relatively consistent across six independent cohorts spanning three neocortical areas and using seven different experimental approaches, it should be noted that the cytoarchitecture of the dorsolateral prefrontal cortex, orbitofrontal cortex and anterior cingulate cortex are not directly comparable [9]. The distribution and densities of the pyramidal cell populations in these regions varies, as well as their function and connectivity [9]. Each of these neocortical areas also possesses subfields and gradients of granularity rostral to caudal, and medial to lateral [29]. The comparability and reliability of these results, and their comparison across independent cohorts with different sampling procedures, should thus be considered in this context and the results from one subfield are not necessarily generalisable across the entire neocortex. In future, studies will also be required to characterise FKBP5/1 expression beyond areas related to frontal lobe dysfunction. Other key regions also involved in processing the stress response such as the hippocampus, amygdala, hypothalamus and cerebellum are comparatively understudied.
Previous gene × environment studies investigating the effects of the FKBP5 risk haplotype on the development of psychiatric disorders have reported a cross-diagnostic effect that is not specific to one disorder, but can raise risk to many psychopathologies [43]. Carriers of the FKBP5 risk haplotype are at an increased risk of developing a psychiatric disorder, but only if exposed to early life adversity [34, 35]. In our study, we found there was no additive effect of the risk haplotype on FKBP5 expression. However it is important to note that we did not have childhood adversity information for our subjects, although childhood adversity is a common occurrence in individuals with psychiatric disorders [32]. Exposure to childhood adversity is a key component of the genetic and especially epigenetic mechanism that causes disinhibition of FKBP5 transcription and heightened levels of FKBP5 [34]. Decreases in DNA methylation in functional FKBP5 enhancers are observed following exposure to early adversity or exposure to glucocorticoids and accentuated in FKBP5 risk haplotype carriers [36, 56, 71]. Importantly, also in the human cortex, decreases in DNA methylation were seen in the same enhancers with increasing age [6]. This suggests that enhanced FKBP5 expression may be differentially driven by different combinations of environmental and genetic risk factors and in relation to age, so it is likely that not all patients are affected by higher FKBP5 expression. Indeed, our data shows a spread of FKBP5/1 expression (Figs. 1, 2) suggesting that for at least a subset of schizophrenia subjects, particularly those that are older, FKBP51 antagonism may present as an efficacious treatment approach with potential to ameliorate cognitive deficits via effects on dendritic spines as previously shown in cell cultures [41]. So far, data on reliable peripheral or other biomarkers for increased brain FKBP5 are missing. Curation of large postmortem cohorts with information regarding environmental exposures, cognitive function measures (from when the subjects were alive) and matching peripheral blood samples would all be helpful for clinical translation. As pharmacological targeting of FKBP51 has become more specific [13], another compelling way to study FKBP51 (and its link to cognitive function) could be made possible with the development of positron-emission topography imaging ligands targeting FKBP51, enabling its study in the brain of living people.
This study addresses a crucial knowledge gap regarding the cell-type specificity of FKBP51 alterations across the human neocortex and pinpoints a functional pathway of high relevance to treatment development. Our findings support that FKBP51 antagonists may be most suitable for older individuals with schizophrenia, and possibly depression. Future studies would need to clarify if this is only in a subset of patients that carry the FKBP5 risk genotype and have been exposed to childhood adversity. This work opens the door for new targeted development of novel drugs that target cortical FKBP51, such as SAFiT2 [41], with the potential to treat cognitive deficits, which are the most debilitating but untreated symptoms of psychiatric disorders, via BDNF-mediated synaptic plasticity.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the families from the USA, Canada, Germany and Australia who donated brain tissues to this research. We specifically thank the Lieber and Maltz families for their contributions towards the Lieber Institute brain collection. The Douglas-Bell Canada Brain Bank is funded by the Réseau Québécois sur le suicide, le troubles de l’humeur et les troubles associés (FRQS) as well as by Healthy Brains for Healthy Lives (CFREF) and Brain Canada grants to Dr Mechawar and Dr Turecki. The Victorian Brain Bank tissue collection was supported by the National Health and Medical Research Council (NHMRC; Australia; grant number 566967) and the Cooperative Research Centre (CRC) for Mental Health and the Operational Infrastructure Support from the Victorian State Government. We would additionally like to thank Geoff Pavey for his efforts in curating the Australian Victorian Brain Bank and Madhara Udawela for supervising preparation of brain tissues in Cohort 2. Tissues received from the New South Wales Brain Tissue Resource Centre at the University of Sydney were supported by the University of Sydney. Research reported in this publication was supported by the National Institute of Alcohol Abuse and Alcoholism of the National Institutes of Health under Award Number NIAAA012725-15. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Author contributions
N.MA. and E.B.B. conceived, designed and managed the work, performed all analyses and drafted the manuscript. J.A., D.C., M.M., A.S.F., T.H, R.T. and A.E.J. were all involved in conceptualising and assisting with the statistical analyses. J.A., D.C., T.H. and C.C. were also involved in substantively drafting and revising the work. S.M., D.K., R.B., K.Z.E., A.R.C., N.C.G. and K.H. performed immunoblot and histological analyses and assisted with interpretation of this data. V.M., N.S.M., K.W., G.R., C.N., M.G. and N.G. were involved in the preparation of omics data for statistical analyses. M.Z., E.S., T.A., P.F., J.E.K., D.R.W., N.Me., A.S., B.D., G.T. and T.M.H. were all involved in collection, dissection and curation of the brain samples used in this study, as well as managing the experiments and sharing the resulting datasets. All authors were involved in the acquisition, analysis and interpretation of the data, and approved the final version of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. Dr Matosin was supported by a Project Grant (#PG2020645) and Al & Val Rosenstrauss Fellowship from the Rebecca L. Cooper Medical Research Foundation, as well as an Australian National Health and Medical Research Council (NHMRC) Early Career Fellowship (APP1105445), Alexander von Humboldt Foundation Research Fellowship and International Brain Research Organisation (IBRO) Research Fellowship. Dr Matosin (#26486), Dr Arloth (#28063) and Dr Gassen (#25348) were all supported with NARSAD Young Investigator Grants. Dr Mechawar and Dr Turecki were supported by grants from The Canadian Institutes of Health Research, Healthy Brains, Healthy Lives McGill grant scheme and ERA-NET NEURON (Network of European Funding for Neuroscience Research). This work was supported by the Hope for Depression Research Foundation.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
Dr Binder is a co-inventor of the following patent applications: FKBP5: a novel target for antidepressant therapy. European Patent # EP1687443 B1: Polymorphisms in ABCB1 associated with a lack of clinical response to medicaments. United States Patent # 8030033; Means and methods for diagnosing predisposition for treatment emergent suicidal ideation (TESI). European application number: 08016477.5, international application number: PCT/EP2009/061575. Dr Falkai has been an honorary speaker for AstraZeneca, Bristol Myers Squibb, Eli Lilly, Essex, GE Healthcare, GlaxoSmithKline, Janssen Cilag, Lundbeck, Otsuka, Pfizer, Servier and Takeda. During the past 5 years, but not presently, Dr Falkai has been a member of the advisory boards of Janssen-Cilag, AstraZeneca, Eli Lilly and Lundbeck. Dr Schmitt has been an honorary speaker for TAD Pharma and Roche and has been a member of advisory boards for Roche. The remaining authors declare no competing interests or conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Natalie Matosin, Email: nmatosin@uow.edu.au.
Elisabeth B. Binder, Email: binder@psych.mpg.de
References
- 1.Arnsten AFT. Stress signalling pathways that impair prefrontal cortex structure and function. Nat Rev Neurosci. 2009;10:410–422. doi: 10.1038/nrn2648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bankhead P, Loughrey MB, Fernandez JA, Dombrowski Y, McArt DG, Dunne PD, et al. QuPath: Open source software for digital pathology image analysis. Sci Rep. 2017;7:16878. doi: 10.1038/s41598-017-17204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Batiuk MY, Tyler T, Dragicevic K, Mei S, Rydbirk R, Petukhov V, et al. Upper cortical layer-driven network impairment in schizophrenia. Sci Adv. 2022 doi: 10.1126/sciadv.abn8367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Roy Stat Soc Ser B (Methodol) 1995;57:289–300. [Google Scholar]
- 5.Bennett MR, Lagopoulos J. Stress and trauma: BDNF control of dendritic-spine formation and regression. Prog Neurobiol. 2014;112:80–99. doi: 10.1016/j.pneurobio.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Blair LJ, Nordhues BA, Hill SE, Scaglione KM, O'Leary JC, 3rd, Fontaine SN, et al. Accelerated neurodegeneration through chaperone-mediated oligomerization of tau. J Clin Investig. 2013;123:4158–4169. doi: 10.1172/jci69003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blair LJ, Criado-Marrero M, Zheng D, Wang X, Kamath S, Nordhues BA, et al. The disease-associated chaperone FKBP51 impairs cognitive function by accelerating AMPA receptor recycling. eNeuro. 2019 doi: 10.1523/ENEURO.0242-18.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bouras C, Kovari E, Hof PR, Riederer BM, Giannakopoulos P. Anterior cingulate cortex pathology in schizophrenia and bipolar disorder. Acta Neuropathol. 2001;102:373–379. doi: 10.1007/s004010100392. [DOI] [PubMed] [Google Scholar]
- 9.Brodmann K (2006) Brodmann's Localisation in the Cerebral Cortex. Springer Nature, City
- 10.Criado-Marrero M, Rein T, Binder EB, Porter JT, Koren J, 3rd, Blair LJ. Hsp90 and FKBP51: complex regulators of psychiatric diseases. Philos Trans R Soc Lond B Biol Sci. 2018 doi: 10.1098/rstb.2016.0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Criado-Marrero M, Smith TM, Gould LA, Kim S, Penny HJ, Sun Z, et al. FKBP5 and early life stress affect the hippocampus by an age-dependent mechanism. Brain Behav Immun Health. 2020;9:100143. doi: 10.1016/j.bbih.2020.100143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Engelhardt C, Tang F, Elkhateib R, Bordes J, Brix LM, van Doeselaar L, et al. FKBP51 in the oval bed nucleus of the stria terminalis regulates anxiety-like behavior. eNeuro. 2021 doi: 10.1523/ENEURO.0425-21.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gaali S, Kirschner A, Cuboni S, Hartmann J, Kozany C, Balsevich G, et al. Selective inhibitors of the FK506-binding protein 51 by induced fit. Nat Chem Biol. 2015;11:33–37. doi: 10.1038/nchembio.1699. [DOI] [PubMed] [Google Scholar]
- 14.Garey LJ (1999) Brodmann's' localisation in the cerebral cortex'. World Scientific, City
- 15.Garey LJ, Ong WY, Patel TS, Kanani M, Davis A, Mortimer AM, et al. Reduced dendritic spine density on cerebral cortical pyramidal neurons in schizophrenia. J Neurol Neurosurg Psychiatry. 1998;65:446–453. doi: 10.1136/jnnp.65.4.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gassen NC, Fries GR, Zannas AS, Hartmann J, Zschocke J, Hafner K, et al. Chaperoning epigenetics: FKBP51 decreases the activity of DNMT1 and mediates epigenetic effects of the antidepressant paroxetine. Sci Signal. 2015 doi: 10.1126/scisignal.aac7695. [DOI] [PubMed] [Google Scholar]
- 17.Gassen NC, Chrousos GP, Binder EB, Zannas AS. Life stress, glucocorticoid signaling, and the aging epigenome: Implications for aging-related diseases. Neurosci Biobehav Rev. 2016 doi: 10.1016/j.neubiorev.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 18.Gómez-de-Mariscal E, Guerrero V, Sneider A, Jayatilaka H, Phillip JM, Wirtz D, et al. Use of the p-values as a size-dependent function to address practical differences when analyzing large datasets. Sci Rep. 2021;11:20942. doi: 10.1038/s41598-021-00199-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Green MJ, Raudino A, Cairns MJ, Wu J, Tooney PA, Scott RJ, et al. Do common genotypes of FK506 binding protein 5 (FKBP5) moderate the effects of childhood maltreatment on cognition in schizophrenia and healthy controls? J Psychiatr Res. 2015;70:9–17. doi: 10.1016/j.jpsychires.2015.07.019. [DOI] [PubMed] [Google Scholar]
- 20.Habib N, Avraham-Davidi I, Basu A, Burks T, Shekhar K, Hofree M, et al. Massively parallel single-nucleus RNA-seq with DroNc-seq. Nat Methods. 2017;14:955–958. doi: 10.1038/nmeth.4407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Halldorsdottir T, Kurtoic D, Muller-Myhsok B, Binder EB, Blair C. Neurobiology of self-regulation: longitudinal influence of FKBP5 and intimate partner violence on emotional and cognitive development in childhood. Am J Psychiatry. 2019;176:626–634. doi: 10.1176/appi.ajp.2019.18091018. [DOI] [PubMed] [Google Scholar]
- 22.Hartmann J, Wagner KV, Gaali S, Kirschner A, Kozany C, Rühter G, et al. Pharmacological inhibition of the psychiatric risk factor FKBP51 has anxiolytic properties. Doi. 2015 doi: 10.1523/JNEUROSCI.4024-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hertzberg L, Zohar AH, Yitzhaky A. Gene expression meta-analysis of cerebellum samples supports the FKBP5 gene-environment interaction model for schizophrenia. Life (Basel) 2021 doi: 10.3390/life11030190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hill JJ, Hashimoto T, Lewis DA. Molecular mechanisms contributing to dendritic spine alterations in the prefrontal cortex of subjects with schizophrenia. Mol Psychiatry. 2006;11:557–566. doi: 10.1038/sj.mp.4001792. [DOI] [PubMed] [Google Scholar]
- 25.Holmes SE, Girgenti MJ, Davis MT, Pietrzak RH, DellaGioia N, Nabulsi N, et al. Altered metabotropic glutamate receptor 5 markers in PTSD: In vivo and postmortem evidence. Proc Natl Acad Sci USA. 2017 doi: 10.1073/pnas.1701749114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holz NE, Buchmann AF, Boecker R, Blomeyer D, Baumeister S, Wolf I, et al. Role of FKBP5 in emotion processing: results on amygdala activity, connectivity and volume. Brain Str Funct. 2015;220:1355–1368. doi: 10.1007/s00429-014-0729-5. [DOI] [PubMed] [Google Scholar]
- 27.Horch HW, Kruttgen A, Portbury SD, Katz LC. Destabilization of cortical dendrites and spines by BDNF. Neuron. 1999;23:353–364. doi: 10.1016/s0896-6273(00)80785-0. [DOI] [PubMed] [Google Scholar]
- 28.Howes OD, Thase ME, Pillinger T. Treatment resistance in psychiatry: state of the art and new directions. Mol Psychiatry. 2022;27:58–72. doi: 10.1038/s41380-021-01200-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huntenburg JM, Bazin PL, Margulies DS. Large-scale gradients in human cortical organization. Trends Cogn Sci. 2018;22:21–31. doi: 10.1016/j.tics.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 30.Kaul D, Schwab S, Mechawar N, Matosin N (2021) How stress physically re-shapes the brain: impact on brain cell shapes, numbers and connections in psychiatric disorders. Neurosci Biobehav Rev 10.1016/j.neubiorev.2021.01.025 [DOI] [PubMed]
- 31.Kaul D, Smith CC, Stevens J, Fröhlich AS, Binder EB, Mechawar N, et al. Severe childhood and adulthood stress associates with neocortical layer-specific reductions of mature spines in psychiatric disorders. Neurobiol Stress. 2020;13:100270. doi: 10.1016/j.ynstr.2020.100270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry. 2010;197:378–385. doi: 10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klengel T, Binder EB. Allele-specific epigenetic modification: a molecular mechanism for gene-environment interactions in stress-related psychiatric disorders? Epigenomics. 2013;5:109–112. doi: 10.2217/epi.13.11. [DOI] [PubMed] [Google Scholar]
- 34.Klengel T, Binder EB. FKBP5 allele-specific epigenetic modification in gene by environment interaction. Neuropsychopharmacology. 2015;40:244–246. doi: 10.1038/npp.2014.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klengel T, Binder EB. Epigenetics of stress-related psychiatric disorders and gene x environment interactions. Neuron. 2015;86:1343–1357. doi: 10.1016/j.neuron.2015.05.036. [DOI] [PubMed] [Google Scholar]
- 36.Klengel T, Mehta D, Anacker C, Rex-Haffner M, Pruessner JC, Pariante CM, et al. Allele-specific FKBP5 DNA demethylation mediates gene-childhood trauma interactions. Nat Neurosci. 2013;16:33–41. doi: 10.1038/nn.3275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kusters R, Kapitein LC, Hoogenraad CC, Storm C. Shape-induced asymmetric diffusion in dendritic spines allows efficient synaptic AMPA receptor trapping. Biophys J. 2013;105:2743–2750. doi: 10.1016/j.bpj.2013.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lake BB, Chen S, Sos BC, Fan J, Kaeser GE, Yung YC, et al. Integrative single-cell analysis of transcriptional and epigenetic states in the human adult brain. Nat Biotechnol. 2018;36:70–80. doi: 10.1038/nbt.4038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lewis DA, Gonzalez-Burgos G. Intrinsic excitatory connections in the prefrontal cortex and the pathophysiology of schizophrenia. Brain Res Bull. 2000;52:309–317. doi: 10.1016/s0361-9230(99)00243-9. [DOI] [PubMed] [Google Scholar]
- 40.Liao Y, Smyth GK, Shi W. featureCounts: an efficient general purpose program for assigning sequence reads to genomic features. Bioinformatics. 2013;30:923–930. doi: 10.1093/bioinformatics/btt656. [DOI] [PubMed] [Google Scholar]
- 41.Martinelli S, Anderzhanova EA, Bajaj T, Wiechmann S, Dethloff F, Weckmann K, et al. Stress-primed secretory autophagy promotes extracellular BDNF maturation by enhancing MMP9 secretion. Nat Commun. 2021;12:4643. doi: 10.1038/s41467-021-24810-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matosin N, Fernandez-Enright F, Fung SJ, Lum JS, Engel M, Andrews JL, et al. Alterations of mGluR5 and its endogenous regulators Norbin, Tamalin and Preso1 in schizophrenia: towards a model of mGluR5 dysregulation. Acta Neuropathol. 2015;130:119–129. doi: 10.1007/s00401-015-1411-6. [DOI] [PubMed] [Google Scholar]
- 43.Matosin N, Halldorsdottir T, Binder EB. Understanding the molecular mechanisms underpinning gene by environment interactions in psychiatric disorders: The FKBP5 model. Biol Psychiatry. 2018;83:821–830. doi: 10.1016/j.biopsych.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 44.McEwen BS, Akil H. Revisiting the stress concept: implications for affective disorders. J Neurosci. 2020;40:12–21. doi: 10.1523/JNEUROSCI.0733-19.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McEwen BS, Sapolsky RM. Stress and cognitive function. Curr Opin Neurobiol. 1995;5:205–216. doi: 10.1016/0959-4388(95)80028-x. [DOI] [PubMed] [Google Scholar]
- 46.McMahon FJ. Prediction of treatment outcomes in psychiatry–where do we stand ? Dialogues Clin Neurosci. 2014;16:455–464. doi: 10.31887/DCNS.2014.16.4/fmcmahon. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McTeague LM, Goodkind MS, Etkin A. Transdiagnostic impairment of cognitive control in mental illness. J Psychiatr Res. 2016;83:37–46. doi: 10.1016/j.jpsychires.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Menke A, Klengel T, Rubel J, Brückl T, Pfister H, Lucae S, et al. Genetic variation in FKBP5 associated with the extent of stress hormone dysregulation in major depression. Genes Brain Behav. 2013;12:289–296. doi: 10.1111/gbb.12026. [DOI] [PubMed] [Google Scholar]
- 49.Moradi Chameh H, Rich S, Wang L, Chen FD, Zhang L, Carlen PL, et al. Diversity amongst human cortical pyramidal neurons revealed via their sag currents and frequency preferences. Nat Commun. 2021;12:2497. doi: 10.1038/s41467-021-22741-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moyer CE, Shelton MA, Sweet RA. Dendritic spine alterations in schizophrenia. Neurosci Lett. 2015;601:46–53. doi: 10.1016/j.neulet.2014.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nagy C, Maitra M, Tanti A, Suderman M, Théroux J-F, Davoli MA, et al. Single-nucleus transcriptomics of the prefrontal cortex in major depressive disorder implicates oligodendrocyte precursor cells and excitatory neurons. Nat Neurosci. 2020;23:771–781. doi: 10.1038/s41593-020-0621-y. [DOI] [PubMed] [Google Scholar]
- 52.Nicolaides NC, Galata Z, Kino T, Chrousos GP, Charmandari E. The human glucocorticoid receptor: molecular basis of biologic function. Steroids. 2010;75:1–12. doi: 10.1016/j.steroids.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Palomero-Gallagher N, Mohlberg H, Zilles K, Vogt B. Cytology and receptor architecture of human anterior cingulate cortex. J Comp Neurol. 2008;508:906–926. doi: 10.1002/cne.21684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Patel N, Crider A, Pandya CD, Ahmed AO, Pillai A. Altered mRNA levels of glucocorticoid receptor, mineralocorticoid receptor, and co-chaperones (FKBP5 and PTGES3) in the middle frontal gyrus of autism spectrum disorder subjects. Mol Neurobiol. 2016;53:2090–2099. doi: 10.1007/s12035-015-9178-2. [DOI] [PubMed] [Google Scholar]
- 55.Penzes P, Cahill ME, Jones KA, VanLeeuwen J-E, Woolfrey KM. Dendritic spine pathology in neuropsychiatric disorders. Nat Neurosci. 2011;14:285–293. doi: 10.1038/nn.2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Provençal N, Arloth J, Cattaneo A, Anacker C, Cattane N, Wiechmann T, et al. Glucocorticoid exposure during hippocampal neurogenesis primes future stress response by inducing changes in DNA methylation. Proc Natl Acad Sci U S A. 2020;117:23280–23285. doi: 10.1073/pnas.1820842116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Qiu B, Xu Y, Wang J, Liu M, Dou L, Deng R, et al. Loss of FKBP5 affects neuron synaptic plasticity: an electrophysiology insight. Neuroscience. 2019;402:23–36. doi: 10.1016/j.neuroscience.2019.01.021. [DOI] [PubMed] [Google Scholar]
- 58.Roland PE, Hilgetag CC, Deco G. Cortico-cortical communication dynamics. Front Syst Neurosci. 2014;8:19. doi: 10.3389/fnsys.2014.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Scarr E, Udawela M, Thomas EA, Dean B. Changed gene expression in subjects with schizophrenia and low cortical muscarinic M1 receptors predicts disrupted upstream pathways interacting with that receptor. Mol Psychiatry. 2018;23:295–303. doi: 10.1038/mp.2016.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Scharf SH, Liebl C, Binder EB, Schmidt MV, Müller MB (2011) Expression and regulation of the Fkbp5 gene in the adult mouse brain. PLoS One, City [DOI] [PMC free article] [PubMed]
- 61.Schindelin J, Arganda-Carreras I, Frise E, Kaynig V, Longair M, Pietzsch T, et al. Fiji: an open-source platform for biological-image analysis. Nat Methods. 2012;9:676–682. doi: 10.1038/nmeth.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Seifuddin F, Pirooznia M, Judy JT, Goes FS, Potash JB, Zandi PP. Systematic review of genome-wide gene expression studies of bipolar disorder. BMC Psychiatry. 2013;13:213–213. doi: 10.1186/1471-244X-13-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sinclair D, Fillman SG, Webster MJ, Weickert CS. Dysregulation of glucocorticoid receptor co-factors FKBP5, BAG1 and PTGES3 in prefrontal cortex in psychotic illness. Sci Rep. 2013 doi: 10.1038/srep03539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tao R, Davis KN, Li C, Shin JH, Gao Y, Jaffe AE, et al. GAD1 alternative transcripts and DNA methylation in human prefrontal cortex and hippocampus in brain development, schizophrenia. Mol Psychiatry. 2017 doi: 10.1038/mp.2017.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Velmeshev D, Schirmer L, Jung D, Haeussler M, Perez Y, Mayer S, et al. Single-cell genomics identifies cell type-specific molecular changes in autism. Science. 2019;364:685–689. doi: 10.1126/science.aav8130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Visscher PM, Wray NR, Zhang Q, Sklar P, McCarthy MI, Brown MA, et al. 10 years of GWAS discovery: biology, function, and translation. Am J Hum Genet. 2017;101:5–22. doi: 10.1016/j.ajhg.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vogt BA, Pandya DN. Cingulate cortex of the rhesus monkey: II. Cortical afferents J Comp Neurol. 1987;262:271–289. doi: 10.1002/cne.902620208. [DOI] [PubMed] [Google Scholar]
- 68.von Economo CF, Koskinas GN, Triarhou LC (2008) Atlas of cytoarchitectonics of the adult human cerebral cortex. Karger Basel, City
- 69.Weickert CS, Webster MJ, Boerrigter D, Sinclair D (2015) FKBP5 mRNA Increases after adolescence in human DLPFC. Biol Psychiatry [DOI] [PubMed]
- 70.Wesarg C, Veer IM, Oei NYL, Daedelow LS, Lett TA, Banaschewski T, et al. The interaction of child abuse and rs1360780 of the FKBP5 gene is associated with amygdala resting-state functional connectivity in young adults. Hum Brain Mapp. 2021;42:3269–3281. doi: 10.1002/hbm.25433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wiechmann T, Röh S, Sauer S, Czamara D, Arloth J, Ködel M, et al. Identification of dynamic glucocorticoid-induced methylation changes at the FKBP5 locus. Clin Epigenetics. 2019;11:83. doi: 10.1186/s13148-019-0682-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Young KA, Thompson PM, Cruz DA, Williamson DE, Selemon LD. BA11 FKBP5 expression levels correlate with dendritic spine density in postmortem PTSD and controls. Neurobiol stress. 2015;2:67–72. doi: 10.1016/j.ynstr.2015.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zagrebelsky M, Tacke C, Korte M. BDNF signaling during the lifetime of dendritic spines. Cell Tissue Res. 2020;382:185–199. doi: 10.1007/s00441-020-03226-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zaitsev AV, Povysheva NV, Gonzalez-Burgos G, Lewis DA. Electrophysiological classes of layer 2/3 pyramidal cells in monkey prefrontal cortex. J Neurophysiol. 2012;108:595–609. doi: 10.1152/jn.00859.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zannas AS, Binder EB. Gene-environment interactions at the FKBP5 locus: sensitive periods, mechanisms and pleiotropism. Genes Brain Behav. 2014;13:25–37. doi: 10.1111/gbb.12104. [DOI] [PubMed] [Google Scholar]
- 76.Zannas AS, Wiechmann T, Gassen NC, Binder EB. Gene–Stress–Epigenetic Regulation of FKBP5: Clinical and Translational Implications. Neuropsychopharmacology. 2016;41:261–274. doi: 10.1038/npp.2015.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zannas AS, Jia M, Hafner K, Baumert J, Wiechmann T, Pape JC, et al. Epigenetic upregulation of FKBP5 by aging and stress contributes to NF-kappaB-driven inflammation and cardiovascular risk. Proc Natl Acad Sci U S A. 2019;116:11370–11379. doi: 10.1073/pnas.1816847116. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.