Abstract
Prenatal Exome Sequencing (ES) is increasingly used for prenatal diagnosis because emerging data indicates it has incremental diagnostic benefit in pregnancies with fetal anomalies without identified genetic abnormalities by karyotyping and chromosomal microarray analysis. The aim of this study was to evaluate the medical community’s attitude towards the clinical utility and use of exome sequencing for prenatal diagnosis and to address differences in attitudes and responses by type of practitioner, level of training, and years passed since last full time training. We analyzed the answers of 109 trainees and professionals in the fields of genetic counseling, laboratory science and medicine to an online survey addressing these topics. Multiple choice questions asked participants about their awareness of prenatal ES and what genetic test they would choose to order in certain scenarios. Likert scale questions assessed participants’ opinions of statements asserting when prenatal ES should be used for diagnostic testing. Attitude towards the use of prenatal ES statistically differed (P < 0.05) by type of participant and level of training. Practicing genetic counselors and physicians were more selective in their recommendations for prenatal ES than laboratory scientists. Genetic counseling students and practicing genetic counselors felt similarly about indications for the use of prenatal ES whereas medical students were more liberal in their recommendations for prenatal ES than practicing physicians. This study shows a lack of consensus amongst the medical community regarding the clinical utility and indications for prenatal ES.
Keywords: exome sequencing, prenatal diagnosis, attitudes
Introduction:
Birth defects affect 3% of all newborns. They are the leading cause of infant mortality, contributing to 20% of all infant or perinatal deaths in the United States (Mathews, Macdorman, & Thoma, 2015). Diagnosis of genetic disease in utero may enable better informed delivery planning and perinatal management, and further facilitate opportunities for targeted treatments that have the potential to improve perinatal morbidity and mortality.
Standard prenatal diagnostic technologies focus on detection of aneuploidy and copy number variants primarily by G‐banded karyotyping and chromosomal microarray analysis (CMA), as well as fluorescence in situ hybridization (FISH), and in some locations, quantitative fluorescence polymerase chain reaction-based assays for common aneuploidy detection. When one or more of these diagnostic tests are used, a genetic cause is found for 6.2–80% of fetuses with prenatally diagnosed congenital abnormalities (Best et al., 2018).
For exome sequencing (ES), next generation sequencing technology is used to sequence the coding exons of most genes at high resolution. While the coding regions of DNA only represent 1–2% of the genome, they contain more than 85% of known pathogenic variants (Best et al., 2018). ES is already frequently used for postnatal genetic diagnosis. Fitzgerald et al. demonstrated that ES can identify an underlying genetic etiology in 25–35% of patients with a suspected genetic condition but previously normal genetic testing results (Fitzgerald et al., 2015). The reported use of ES as a prenatal diagnostic method is more limited, with early reporting of prenatal diagnostic rates ranging from 8.5% to 80% (Lord et al., 2019; Yadava & Ashkinadze, 2017). In a retrospective review of 146 fetal exomes, Normand et al. found that prenatal exome sequencing yielded an overall diagnostic rate of 32% (Normand et al., 2018).In a more recent prospective cohort study ES identified diagnostic genetic variants in 10.3% of fetuses with a structural anomaly and normal karyotype or CMA findings (Petrovski et al., 2019). In another prospective cohort study conducted by Lord et al., ES identified a diagnostic genetic variant in 8.5% of structurally abnormal fetuses (excluding abnormalities due to aneuploidy or copy number variants). An additional 3.9% had a genetic variant of unknown significance with potential clinical usefulness (Lord et al., 2019). In a scoping review on the application of exome sequencing for prenatal diagnosis Pratt et al. finds diagnostic yields varying widely from 5% to 57% (Pratt et al., 2020). These studies support that ES has added clinical value when standard prenatal genetic testing does not yield a diagnosis. However, ES has diagnostic limitations. It cannot detect some genetic abnormalities including variants in non-coding regions, trinucleotide repeat expansions, chromosomal rearrangements, aneuploidy, and copy number deletions or additions.
Cost is an important factor in the determination of a diagnostic test’s clinical utility. ES has a speculated cost benefit compared to other diagnostic methods. A cost and value analysis performed by The Association for Molecular Pathology found that use of ES in the diagnosis of children with sensorineural hearing loss and neurodevelopmental disorders of unknown etiology compared to other diagnostic methods (e.g. targeted gene panels) resulted in significant cost savings. For a planned size of one million cases, use of ES in the diagnosis of sensorineural hearing loss saved $0.24 million. For a planned size of one million cases, use of ES in the diagnosis of neurodevelopmental disorders after failure to identify a genetic defect with CMA and fragile X testing saved about $1.33 million (Sabatini et al., 2016). However, large cost-effectiveness studies for prenatal ES have not yet been done.
An important advantage of utilizing ES for in utero diagnosis, when pursued in a “rapid trio” approach (sequencing of the parents along with the fetal sample for rapid integrated result interpretation), is its reported result turnaround time of 3 weeks (Best et al., 2018). Many structural fetal anomalies are first detected between 18 and 22 weeks gestational age during the second trimester fetal anatomy ultrasound. For families who consider termination of pregnancy as a management option based on knowledge from ES results, having a short result turnaround time enables them to do so within the gestational age limitations set by the law where they reside. This decision is highly dependent upon both the nature of the diagnosis and the respective family’s values and expectations.
The medical community’s opinion of this fairly new diagnostic technology is relatively unknown. Focus groups conducted by Quinlan-Jones et al. found that clinical professionals had seven main concerns about the use of prenatal ES in fetuses with structural anomalies including: consent, analysis, interpretation/reinterpretation of results, prenatal issues, uncertainty, secondary findings and information access (Quinlan-Jones et al., 2016). In 2018, Horn and Parker conducted a review of the existing literature on ethical issues in prenatal genomics, including prenatal ES, finding similar themes to those identified by Quinlan-Jones et al. including: valid consent, management and feed‐back of information, responsibilities of health professionals, priority setting and resources and duties towards the future child (Horn & Parker, 2018). In a descriptive study conducted by Harris et al. select cases further illustrated that informed consent and result interpretation are challenges associated with the use of prenatal ES (Harris, Gilmore, Hardisty, Lyerly, & Vora, 2018). Overall, these studies elucidate a clear set of concerns shared by practitioners regarding the use of prenatal ES.
A small number of quantitative survey studies have been done to explore the attitudes of health professionals towards prenatal ES and related prenatal genetic testing such as CMA. Brew et al. designed a survey to assess the attitudes of members of genetics professional organizations toward the clinical implementation of prenatal ES. The overall response rate of this study was 12%(498/4,313). They found that the majority of respondents believed there would be clinical utility in using prenatal ES for the purposes of diagnosis (89%), pregnancy management (58%), termination decisions (75%), and preparation for childhood-onset conditions that have available treatment (71%), but not for adult-onset conditions with (60%) or without (71%) treatment, or as a standard screening tool (63%). Brew et al. stratified participants by practice setting and found that prenatal practicing participants were significantly more likely to agree in the diagnostic utility of this testing than non-prenatal practicing participants (p = 0.001). Brew et al. further discussed attitudes towards ES in the prenatal setting vs. pediatric and adult settings as well as attitudes towards the return of genetic testing results (Brew et al., 2019). Mikhaelian et al. conducted a survey to characterize the practices and attitudes of North American prenatal genetic counselors regarding CMA. Potential participants were recruited from the National Society of Genetic Counselors and the Canadian Association of Genetic Counselors with an overall response rate of 13% (196/1560). Mikhaelian et al. found that a majority of respondents viewed CMA as useful (73%) and identified three significant predictors for this viewpoint: more prenatal counseling experience, younger age, and previously presenting CMA to a patient. The authors identified three factors that predicted the likelihood of offering CMA to prenatal patients: percentage of time spent in prenatal practice, belief that CMA is useful, and practicing in the USA (versus Canada). Reasons cited for not using CMA included financial concerns, the possibility of ambiguous results, and ethical concerns (Mikhaelian, Veach, Macfarlane, Leroy, & Bower, 2013). Durham et al’s survey aimed at evaluating what prenatal genetic counselor’s practices, attitudes, and barriers are in regard to prenatal CMA reported a similarly favorable attitude towards the use of CMA. Durham et al. surveyed members of the National Society of Genetic Counselors with an approximate response rate of 30% with 95% of respondents having incorporated CMA into clinical practice, 64% believing that the benefits of CMA outweigh the harms, and 52% agreeing that CMA should be offered to all women regardless of indication (Durham et al., 2019).
Emerging data indicates that prenatal exome sequencing has incremental diagnostic benefit in pregnancies with fetal anomalies but no identified genetic abnormalities by karyotyping and chromosomal microarray analysis. ES has the additional benefit of rapid result turnaround time and speculated cost savings. While the medical community’s opinion of this fairly new diagnostic technology is relatively unknown, qualitative studies have made it clear that a shared set of concerns regarding the use of prenatal ES exist. Quantitative surveys assessing health professional attitudes towards prenatal ES are limited in number and do not assess how attitudes differ based on field of training, respondent’s current level of expertise, or years passed since last full time training.
The aim of this study is to investigate a local medical community’s awareness of prenatal ES and their attitude towards its use for prenatal diagnosis. This study further investigates how these attitudes differ based on field of training, respondent’s current level of expertise, and years passed since last full time training.
Methods:
In this IRB approved (H-45618) study we invited 763 trainees and professionals affiliated with Baylor College of Medicine and Baylor College of Medicine’s clinical affiliate institution Texas Children’s Hospital to complete an online survey administered via REDCap. To be included in the study participants must have been adults age 18+ and members of the local medical community identified by having either Baylor College of Medicine or Texas Children’s Hospital email addresses on available listservs. Members of the local medical community include midwives, genetic counseling students, genetic counselors, laboratory scientists, medical students, and practicing physicians – including residents in obstetrics and gynecology or clinical genetics, clinical and diagnostic genetics faculty, and clinical post-doctoral fellows. As described by the inclusion/exclusion criteria, non-members of the local medical community, children under the age of 18, and non-English speakers were excluded from participation in the study. The survey was developed with the help of a practicing genetic counselor and prenatal geneticist with expertise in prenatal ES and clinical prenatal genetics. The survey was developed using themes identified in previous qualitative studies, quantitative studies, and the International Society for Prenatal Diagnosis, the Society for Maternal Fetal Medicine, and the Perinatal Quality Foundation joint position statement on the use of genome-wide sequencing for fetal diagnosis (International Society for Prenatal Diagnosis [ISPD], Society for Maternal and Fetal Medicine [SMFM], & Perinatal Quality Foundation [PQF], 2018). The survey was first piloted to a focus group of seven people comprised of two medical students, one genetic counselor, and four practicing physicians in the fields of clinical genetics, maternal fetal medicine, and reproductive endocrinology and infertility. Participants were asked to draw upon their experience to provide feedback on the preliminary survey questions, as it pertains to question clarity, comprehensive answer choices, and length of time needed for completion of the survey. Their feedback resulted in clarification of survey instructions and modification of question formatting to improve participant understanding. Eligible participants were invited to take the survey via email with a link to the survey. The survey was completed between October 2019 and April 2020.
The survey was composed of demographic questions, Likert scale questions, and multiple-choice questions. A brief definition of exome sequencing was provided. Demographic questions asked participants for their gender identity, profession, and years past since last full-time training. Multiple choice questions were utilized to measure participants’ awareness of prenatal ES and opinion of how prenatal ES should be used for diagnostic testing in conjunction with other diagnostic testing methods. Our team chose to focus on questions concerning the clinical applications of prenatal ES. Data was reported using descriptive statistics.
Likert scale questions were utilized to measure participants’ opinions of statements asserting when prenatal ES should be used for diagnostic testing. Participants were asked to rank their opinion from strongly disagree (value=1) to strongly agree (value=5). This variable is reported as mean and standard deviation. We further compared responses to Likert scale questions between types of practitioner and level of training as well as by years passed since last full time training using one-way analysis of variance with Tukey post-hoc analysis for within categories of responders. Statistical analysis was performed using IBM SPSS (version 22, College Station, TX). The survey is available as a supplemental file to this manuscript (Supporting Information).
Results:
Demographic Characteristics
Demographic characteristics of respondents including gender identity, self-identified profession, and years passed since last full-time training are in Table 1. Based on survey responses, we classified respondents as genetic counseling students, practicing genetic counselors, laboratory scientists, medical students, or practicing physicians – including residents in obstetrics and gynecology or clinical genetics, clinical and diagnostic genetics faculty, and clinical post-doctoral fellows. The overall response rate to this survey is 117/763 (15%) and 91/763 (12%) invited participants completed the survey in its entirety. Of the 117 respondents, 26 started but did not complete the demographic information or the remainder of the survey and 18 completed the demographic information but not the remainder of the survey. Respondents were 73.4% female. Approximately half of all respondents were still in full time training (49.5%) and half had completed training (51.5%). Of the half that had completed training, there was an even distribution of years passed since completion.
Table 1: Demographic Characteristics of the Respondents.
Respondents were asked to self-identify their gender, profession, level of training, and years passed since last full-time post graduate training.
| Characteristic | % Responding |
|---|---|
| Gender | |
| Female | 80/109 (73.4%) |
| Male | 27/109 (24.8%) |
| Prefer not to answer | 2/109 (1.8%) |
| Profession | |
| Genetic counselor | 24/109 (22%) |
| ○ Student | 8/24 (33.3%) |
| ○ Practicing genetic counselor | 16/24 (66.7%) |
| PhD scientist | 9/109 (8.3%) |
| ○ Trainee | 1/9 (11.1%) |
| ○ Researcher | 3/9 (33.3%) |
| ○ Lab director | 5/9 (55.6%) |
| Medicine | 76/109 (69.7%) |
| ○ Medical student | 40/76 (52.6%) |
| ○ Intern/Resident | 4/76 (5.3%) |
| ■ OBGYN | 4/4 (100%) |
| ○ Clinical/Post-doctoral fellow | 1/76 (1.3%) |
| ■ REI | 1/1 (100%) |
| ○ Attending | 31/76 (40.8%) |
| ■ OBGYN | 19/31 (61.3%) |
| ■ Genetics | 9/31 (29%) |
| ■ Other | 3/31 (9.7%) |
| Years passed since last full-time training | |
| Still in training | 54/109 (49.5%) |
| 0–5 years | 17/109 (15.6%) |
| 6–10 years | 10/109 (9.2%) |
| 11–15 years | 7/109 (6.4%) |
| 16–20 years | 8/109 (7.3%) |
| 21+ years | 13/109 (11.9%) |
Abbreviations: PhD, Doctor of Philosophy; OBGYN, Obstetrician Gynecologist; REI, Reproductive Endocrinology and Infertility.
Awareness of Prenatal ES
Figure 1 displays the various response rates to each multiple-choice question. Of the 105 respondents, only 4/105 (4%) did not know of exome sequencing (Figure 1a). However, 87/105 (83%) of respondents had not read or were unable to recall published recommendations for clinical prenatal use of ES (Figure 1b). If a participant responded that they had read about or were able to recall published recommendations for clinical prenatal use of ES, they were asked to elaborate on specific recommendations in the form of a free response question (see supporting information). Respondents named various guidelines including publications from the American College of Obstetricians and Gynecologists (ACOG), the American College of Medical Genetics and Genomics (ACMG), the International Society for Prenatal Diagnosis (ISPD), the Society for Maternal Fetal Medicine (SMFM), and the Perinatal Quality Foundation (PQF).
Figure 1: Provider Awareness and Opinions on Prenatal Exome Sequencing.
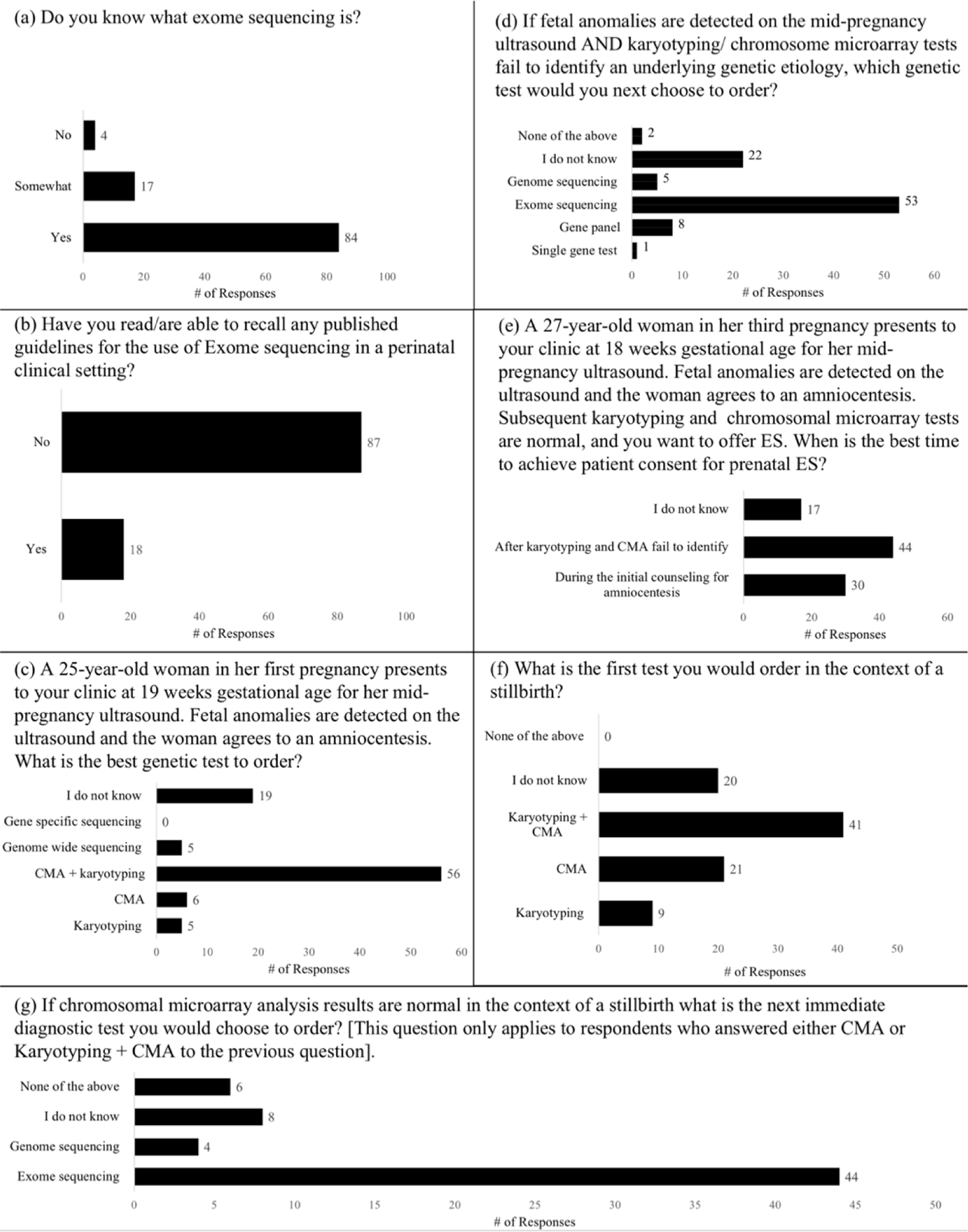
Each panel (a-g) shows a different multiple-choice question, with the corresponding graph of the number of participants who chose a specific response. The Y-axis shows the possible responses and the X-axis shows the number of participants who chose each response. Abbreviations: ES, exome sequencing; CMA, chromosomal microarray analysis.
Preference for Specific Genetic Tests in the Prenatal Setting
When asked which is the best genetic test to order for fetal anomalies detected on ultrasound, 56/91 (62%) answered karyotype CMA (Figure 1c). 53/91 (58%) answered that ES is the next best genetic test to order for fetal anomalies detected on ultrasound following normal karyotype + CMA (Figure 1d). When asked about the best time to obtain consent for prenatal ES, 30/91 (33%) answered that it is during the initial consult for amniocentesis and 44/91 (48%) answered that it is after karyotyping and CMA do not reveal the underlying genetic etiology (Figure 1e). When questioned about testing in the context of a stillbirth, 41/91 (45%) answered that karyotype + CMA is the best genetic test to order (Figure 1f) and 44/62 (71%) answered that ES is the next best genetic test to order normal CMA (+/− Karyotyping) (Figure 1g).
Opinions About When to Use Prenatal ES for Diagnostic Testing
Table 2 shows the averaged response to each Likert scale question per type of practitioner and level of training. There was a significant difference between laboratory scientists and practicing genetic counselors/physicians in their response to statements assessing if prenatal ES should be the first diagnostic genetic test ordered in the context of an abnormal mid-pregnancy ultrasound or a positive combined first screen for trisomy 21. Laboratory scientists were more likely to agree with the use of prenatal ES in these scenarios than practicing genetic counselors or physicians. This trend persisted in response to statements assessing if prenatal ES should be offered to prospective mothers of advanced maternal age (35 years +) or to every prospective mother in her first trimester. Again, laboratory scientists were more likely to agree with the use of prenatal ES in these scenarios than practicing genetic counselors or physicians. Laboratory scientists also responded more favorably than practicing genetic counselors to a statement suggesting everyone should receive ES at birth and a statement suggesting that prenatal ES be offered to every prospective mother in her second trimester.
Table 2: Averaged Scored Response (Mean +/− SD) to Likert Scale Questions by Different Groups of Participants.
(value 1=strongly disagree; value 5=strongly agree). One-Way ANOVA statistics with Tukey post-hoc analysis for comparison between the groups showed:
| Question | Practicing Genetic Counselors | Genetic Counseling Students | Practicing Physicians | Medical Students | Laboratory Scientists | Degrees of freedom | F-value | p-value | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Everyone should receive ES at birth. | 1.6 ± 0.6 ¶, ⁊ | 1.6 ± 1.2 ¶ | 1.7 ± 0.9 ¶ | 2.8 ± 1.2 †, ‡, § | 2.8 ± 1.1 † | 4 | 7.202 | 0.000 | ||
| 2. prenatal ES should never be used. | 1.1 ± 0.3 | 1.5 ± 0.8 | 1.4 ± 0.7 | 1.5 ± 0.9 | 1.7 ± 1.3 | 4 | 0.929 | 0.451 | ||
| 3. Invasive prenatal testing should be offered to every pregnant woman. | 4.2 ± 1.1 | 4.4 ± 0.7 | 3.6 ± 1.4 | 3.3 ± 1.3 | 3.3 ± 0.9 | 4 | 2.221 | 0.074 | ||
| 4. Prospective parents should be able to request prenatal ES without medical indication. | 2.4 ± 1.1 ¶ | 2.6 ± 1.4 | 2.7 ± 1.5 | 3.6 ± 1.3 † | 3.6 ± 1.2 | 4 | 3.077 | 0.020 | ||
| 5. prenatal ES should be the first diagnostic genetic test ordered in the context of an abnormal mid-pregnancy ultrasound. | 1.6 ± 0.8 ¶, ⁊ | 1.9 ± 1.1 ⁊ | 2.3 ± 1.2 ⁊ | 2.6 ± 0.8 †, ⁊ | 3.9 ± 1.1 †, , §, ¶ | 4 | 8.443 | 0.000 | ||
| 6. prenatal ES should be the genetic test ordered in the context of an abnormal mid-pregnancy ultrasound BUT only after karyotyping + CMA fails to identify an underlying genetic etiology. | 4.0 ± 1.1 | 3.6 ± 1.1 | 4.2 ± 0.8 | 4.1 ± 0.6 | 3.8 ± 1.3 | 4 | 0.806 | 0.525 | ||
| 7. prenatal ES should be the first diagnostic genetic test ordered in the context of a positive combined first screen for trisomy 21. | 1.0 ± 0.0 §, ¶, ⁊ | 1.5 ± 0.8 ¶, ⁊ | 2.3 ± 1.3 †, ¶, ⁊ | 3.2 ± 1.1 †, , § | 3.7 ± 1.1 †, , § | 4 | 15.669 | 0.000 | ||
| 8. prenatal ES should always be used in the context of advanced maternal age (35 years +). | 1.2 ± 0.4 ¶, ⁊ | 1.4 ± 0.6 ¶, ⁊ | 1.9 ± 1.1 ⁊ | 2.6 ± 1.2 | 3.2 ± 1.2 †, , § | 4 | 8.936 | 0.000 | ||
| 9. prenatal ES should be offered to every prospective mother in her first trimester. | 1.6 ± 0.6 ¶, ⁊ | 1.5 ± 0.8 ⁊ | 1.8 ± 0.9 ¶, ⁊ | 2.7 ± 1.6 †, , § | 3.1 ± 1.2 †, , § | 4 | 5.796 | 0.000 | ||
| 10. prenatal ES should be offered to every prospective mother in her second trimester. | 1.6 ± 0.6 ¶, ⁊ | 1.7 ± 0.2 | 1.8 ± 1.0 ¶ | 2.7 ± 1.5 †, § | 3.0 ± 1.1 † | 4 | 4.610 | 0.002 | ||
| 11. ES should be performed on stillbirths. | 2.8 ± 1.2 | 2.1 ± 1.4 | 3.4 ± 1.5 | 3.3 ± 1.3 | 3.8 ± 1.3 | 4 | 2.185 | 0.078 | ||
† = significant difference compared to genetic counselors;
‡ = significant difference compared to genetic counseling students;
§ = significant difference compared to practicing physicians.
¶ = significant difference compared to medical students.
⁊ = significant difference compared to laboratory scientists.
Significant difference is defined as a P value < 0.05. Between groups degrees of freedom, F values, and P values are listed. Abbreviations: ES, exome sequencing; CMA, chromosomal microarray analysis.
Practicing genetic counselors and practicing physicians differed significantly in their response to “prenatal ES should be the first diagnostic genetic test ordered in the context of a positive combined first trimester screen for trisomy 21.” Practicing genetic counselors strongly disagreed that prenatal ES should be the first diagnostic genetic test ordered for a positive combined first screen for trisomy 21, whereas practicing physicians responded more favorably. There was no significant difference between practicing genetic counselor and genetic counseling student responses. There was a significant difference between practicing physician and medical student responses to various statements. For example, medical students felt significantly more favorably about everyone receiving ES at birth, prenatal ES being the first diagnostic genetic test ordered in the context of a positive combined first screen for trisomy 21, and prenatal ES being offered to every prospective mother in either her first or second trimester. In all scenarios, practicing physicians were more selective than medical students in their recommendations for prenatal ES.
Table 3 shows the averaged response to each Likert scale question per years passed since last full time training. There was no statistically significant difference between the responses for each question and years passed since last full time training.
Table 3: Averaged Scored Response (Mean +/− SD) to Likert Scale Questions by Years Passed Since Last Full Time Training.
(value 1=strongly disagree; value 5=strongly agree). One-Way ANOVA statistics with Tukey post-hoc analysis for comparison between the groups showed no significant difference between the responses for each question and years passed since last full time training . Significant difference is defined as a P value < 0.05. Between groups degrees of freedom, F values, and P values are listed. Abbreviations: ES, exome sequencing; CMA, chromosomal microarray analysis.
| Question | Still in training | 0–5 years | 6–10 years | 11–15 years | 16–20 years | 21+ years | Degrees of freedom | F-value | p-value |
|---|---|---|---|---|---|---|---|---|---|
| 1. Everyone should receive ES at birth | 2.5 ± 1.3 | 1.5 ± 0.7 | 2.2 ± 0.8 | 1.9 ± 0.9 | 1.6 ± 0.7 | 2.2 ± 1.3 | 5 | 2.06 | 0.08 |
| 2. prenatal ES should never be used | 1.7 ± 1.1 | 1.4 ± 0.8 | 1.1 ± 0.3 | 1.3 ± 0.5 | 1.5 ± 0.8 | 1.1 ± 0.3 | 5 | 1.53 | 0.19 |
| 3. Invasive prenatal testing should be offered to every pregnant woman | 3.6 ± 1.2 | 3.9 ± 1.3 | 3.7 ± 1.7 | 3.4 ± 1.3 | 3.9 ± 1.0 | 3.8 ± 1.1 | 5 | 0.31 | 0.91 |
| 4. Prospective parents should be able to request prenatal ES without medical indication | 3.2 ± 1.3 | 2.2 ± 1.3 | 3.3 ± 1.4 | 3.1 ± 1.3 | 2.9 ± 1.5 | 2.6 ± 1.6 | 5 | 1.58 | 0.18 |
| 5. prenatal ES should be the first diagnostic genetic test ordered in the context of an abnormal mid-pregnancy ultrasound | 2.5 ± 1.0 | 1.9 ± 1.0 | 2.7 ± 1.7 | 2.3 ± 1.0 | 2.5 ± 1.1 | 2.6 ± 1.6 | 5 | 0.83 | 0.53 |
| 6. prenatal ES should be the genetic test ordered in the context of an abnormal mid-pregnancy ultrasound BUT only after karyotyping + CMA fails to identify an underlying genetic etiology | 3.9 ± 0.9 | 3.6 ± 1.2 | 4.1 ± 0.8 | 4.4 ± 0.8 | 4.1 ± 0.4 | 4.4 ± 0.7 | 5 | 1.55 | 0.18 |
| 7. prenatal ES should be the first diagnostic genetic test ordered in the context of a positive combined first screen for trisomy 21 | 2.8 ± 1.3 | 1.7 ± 1.2 | 2.6 ± 1.4 | 2.0 ± 1.1 | 1.6 ± 1.1 | 2.5 ± 1.6 | 5 | 2.11 | 0.07 |
| 8. prenatal ES should always be used in the context of advanced maternal age (35 years +). | 2.3 ± 1.2 | 1.4 ± 0.5 | 2.6 ± 1.5 | 1.6 ± 1.0 | 1.6 ± 1.2 | 2.1 ± 1.2 | 5 | 2.17 | 0.07 |
| 9. prenatal ES should be offered to every prospective mother, irrespective of risk, in her first trimester | 2.3 ± 1.4 | 1.4 ± 0.5 | 2.1 ± 1.3 | 2.1 ± 1.2 | 2.1 ± 1.0 | 2.3 ± 1.2 | 5 | 1.26 | 0.29 |
| 10. prenatal ES should be offered to every prospective mother, irrespective of risk, in her second trimester | 2.4 ± 1.4 | 1.6 ± 0.9 | 2.0 ± 1.3 | 2.1 ± 1.2 | 2.1 ± 1.0 | 2.3 ± 1.1 | 5 | 0.98 | 0.43 |
| 11. ES should be performed on all stillbirths | 3.0 ± 1.3 | 3.5 ± 1.6 | 3.1 ± 1.3 | 3.7 ± 1.0 | 3.4 ± 1.3 | 3.0 ± 1.7 | 5 | 0.54 | 0.75 |
Discussion:
This survey indicates a lack of consensus amongst healthcare professionals at a single academic medical center regarding the indications for and clinical utility of prenatal ES. Laboratory scientists felt more favorable about the use of prenatal ES than practicing genetic counselors or physicians. In addition, practicing genetic counselors and genetic counseling students felt similarly about when to use prenatal ES, but medical students and practicing physicians differed significantly in their attitude towards prenatal ES. Practicing physicians were more selective with their recommendations for the use of prenatal ES than medical students. We also found a difference of opinion about the best timing for obtaining patient consent for prenatal ES and about the diagnostic utility of prenatal ES in the context of a stillbirth.
Various studies have demonstrated that both ethical and practical concerns on topics like consent and data interpretation exist amongst practitioners regarding the use of prenatal ES (Harris et al., 2018; Horn & Parker, 2018; Quinlan-Jones et al., 2016). These concerns may explain why practitioners who are more intimately familiar with the clinical application of prenatal ES, such as practicing genetic counselors and physicians in clinical genetics or obstetrics and gynecology, are more selective with their recommendations for prenatal ES than laboratory scientists. Laboratory scientists may perceive a difference in the utility of prenatal ES for research compared to its use in clinical practice. Considering that obtaining consent for prenatal ES is a frequently cited concern, this survey’s findings on this topic are of particular interest. When all practitioners were surveyed on the best time to obtain consent for prenatal ES, 33% answered that it is during the initial genetic consult when diagnostic testing is offered and 48% answered that it is after results of karyotyping and CMA (the standard prenatal genetic tests offered on amniotic fluid or other prenatal samples) are non-diagnostic. In contrast to all practitioners, 71% of the practicing genetic counselors and students surveyed answered that the best time to obtain consent for prenatal ES it is after the results of karyotyping and CMA are non-diagnostic and 25% answered that it is during the initial genetic consult when diagnostic testing is offered. This data reflects that there is no published standard procedure for when to counsel on and obtain consent for prenatal ES. The significant difference in attitude between medical students and practicing physicians towards the use of prenatal ES, with practicing physicians being more selective in their recommendations, highlights the importance of genetics education in the preclinical years of medical school. Practicing physicians may have a better understanding of the ethical and practical concerns associated with prenatal ES highlighted in the introduction.
This study targeted a broad array of health practitioners, including genetic counseling students, practicing genetic counselors, laboratory scientists, medical students, practicing physicians, including residents in obstetrics and gynecology or clinical genetics, clinical and diagnostic genetics faculty, and clinical postdoctoral fellows. While it is unknown what proportion of the study participants are likely to be conducting/offering/discussing prenatal tests now or in the future, we feel that it is important for all practitioners to have a basic understanding of the clinical indications for exome sequencing as the use of this relatively new diagnostic technology becomes more mainstream. At the time the survey was administered the ISPD, SMFM, and PQF had released a joint position statement on the use of genome-wide sequencing for fetal diagnosis. This statement recommends use of prenatal ES either concurrently with standard diagnostic testing or after standard diagnostic testing proves uninformative. The ISPD, SMFM, and PQF do not recommend the routine use of prenatal ES as a sole primary diagnostic test (ISPD, SMFM, & PQF, 2018). More recently the ACMG released a points to consider document regarding the use of fetal ES for prenatal diagnosis that states ES may be considered when a diagnosis cannot be obtained using routine prenatal methods in a fetus with one or more significant anomalies (Monaghan, Leach, Pekarek, Prasad, & Rose, 2020). Over 80% of respondents had not read or were unable to recall published recommendations for clinical prenatal use of ES. This may reflect suboptimal dissemination of said guidelines. Alternatively, more general health practitioners may have limited interest in the use of prenatal ES, which is reflected in the low overall survey response rate of 15%. We speculate that this somewhat low response rate is in itself an indicator of invited participant’s level of discomfort with or limited awareness of prenatal ES, but this conjecture requires further investigation. A concerted effort should be made within the medical community to raise interest for prenatal ES.
This study adds to the established knowledge base about health professional attitudes towards prenatal ES. Brew et al.surveyed genetic professionals and found that the majority of respondents believed there would be clinical utility in using prenatal ES to help diagnose a fetus with ultrasound abnormalities (Brew et al. 2019). Our survey further explores if prenatal ES should be the first diagnostic test ordered in the context of an abnormal ultrasound or a second line test ordered only after karyotyping and CMA fail to identify an underlying genetic etiology. With the exception of laboratory scientists, all groups of participants responded more favorably to the second scenario. Furthermore, while Brew et al.’s analysis finds that participants working in prenatal care were significantly more likely to agree on the diagnostic utility of prenatal ES than non-prenatal provider participants, they do not directly compare the opinions between these two groups (Brew et al. 2019). Our survey compared attitudes towards the use of prenatal ES for diagnostic testing by type of participant, level of training, and years passed since last full time training. We further asked participants what genetic test they would choose to order in common clinical scenarios in order to assess how prenatal ES should be used for diagnostic testing in conjunction with other diagnostic testing methods. A majority of respondents agreed that karyotype + CMA is the best genetic test to order for fetal anomalies detected on ultrasound. If karyotyping and CMA do not reveal the underlying genetic etiology a majority of respondents agreed that ES is the next best genetic test to order.
Study Limitations
The largest limitation of this study is the aforementioned low overall response rate of 15% and completed survey response rate of 12%. However, this response is comparable to other published surveys on the topic of exome sequencing. Gore et al.’s survey investigating challenges to informed consent for exome sequencing had a response rate of 9.3% (Gore, Bridges, Cohen, & Biesecker, 2019). Niguidula et al. and Mazzola et al.’s surveys on the topic of exome sequencing had response rates of 2.2% and 12.6% respectively (Mazzola, O’Connor, & Yashar, 2019; Niguidula et al., 2018). Further limitations of this survey include the potential for responder bias inherent in survey-based studies as well as a lack of result generalizability. This survey was limited to practitioners affiliated with two institutions in Houston, TX, Baylor College of Medicine and Texas Children’s Hospital. Therefore, the opinions expressed by these practitioners may not be generalizable to practitioners located in other regions of the United States or internationally. Another limitation of this study may be limited participant background knowledge on the use of prenatal ES. While the beginning of the survey included a brief definition of ES it did not elaborate on the use of ES in the prenatal setting.
Conclusion:
This study indicates a lack of consensus amongst the medical and diagnostic lab community regarding the clinical utility and appropriate use of prenatal ES. Attitudes towards the use of prenatal ES statistically differed by type of participant and level of training. Overall, practicing genetic counselors and physicians were more selective in their recommendations for prenatal ES than laboratory scientists, and practicing physicians were more selective in their recommendations for prenatal ES than medical students. This study demonstrates the need for increased education on prenatal ES for the medical community and the need to better disseminate pre-existing guidelines on the use of prenatal ES. The multiple-choice questions illuminated differences of opinion in how to use prenatal ES, when to use prenatal ES, when to obtain consent for prenatal ES, and what guidelines to reference for prenatal ES use. Although our study was relatively small with a low response rate, the questions posed address some of the topics that health policy makers may consider. Our findings highlight the need for more data in this area. Future areas of analysis may include stratifying practitioner attitudes based on MD specialties or location of practice.
Supplementary Material
What is known about this topic:
Exome sequencing has incremental diagnostic benefit in pregnancies with fetal anomalies without identified genetic abnormalities by karyotyping and chromosomal microarray analysis.
What this paper adds to this topic:
This study adds perspective on an academic medical center’s healthcare providers’ awareness of prenatal exome sequencing and their attitudes towards its use for prenatal diagnosis. This study further investigates how these attitudes differ based on field of training, respondent’s current level of expertise, and years passed since last full-time training.
Acknowledgements:
Dr. Van den Veyver receives support from the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health for prenatal genome-wide sequencing research under award R01HD055651 and receives support under Award Number P50HD103555 for use of the administrative core. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The research presented in the paper was conducted while the first author, Kylie Johnson, was in training.
Footnotes
Conflict of interest statement: Dr. Ignatia Van den Veyver is a Scientific Advisory Board member for Baylor Genetics Laboratories without financial compensation. Dr. Ignatia Van den Veyver performs NIH-funded research on fetal genome-wide sequencing, with reagent support from Illumina but no financial support or compensation. Author Kylie Johnson, Author Hadi Erfani, Author Mohamad Ali Maktabi and Author Salma Nassef declare that they have no conflict of interest.
Informed consent: This study was approved by and conducted according to the ethical standards of the Baylor College of Medicine institutional review board. All applicable international, national, and/or institutional guidelines were followed. This study was approved by the IRB after expedited review and was granted an informed consent waiver (H-45618).
Animal studies: No non-human animal studies were carried out by the authors for this article.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Best S, Wou K, Vora N, Van der Veyver IB, Wapner R, & Chitty LS (2018). Promises, pitfalls and practicalities of prenatal whole exome sequencing. Prenatal Diagnosis, 38(1), 10–19. 10.1002/pd.5102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brew CE, Castro BA, Pan V, Hart A, Blumberg B, & Wicklund C (2019). Genetics professionals’ attitudes toward prenatal exome sequencing. Journal of Genetic Counseling, 28(2), 229–239. 10.1002/jgc4.1112 [DOI] [PubMed] [Google Scholar]
- Durham L, Papanna R, Stevens B, Noblin S, Rodriguez-Buritica D, Hashmi SS, & Krstic N (2019). The utilization of prenatal microarray: A survey of current genetic counseling practices and barriers. Prenatal Diagnosis, 39(5), 351–360. 10.1002/pd.5435 [DOI] [PubMed] [Google Scholar]
- Fitzgerald TW, Gerety SS, Jones WD, Van Kogelenberg M, King DA, McRae J, … Hurles ME (2015). Large-scale discovery of novel genetic causes of developmental disorders. Nature, 519, 223–228. 10.1038/nature14135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gore RH, Bridges JFP, Cohen JS, & Biesecker BB (2019). Challenges to informed consent for exome sequencing: A best–worst scaling experiment. Journal of Genetic Counseling, 28(6), 1189–1197. 10.1002/jgc4.1171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris S, Gilmore K, Hardisty E, Lyerly AD, & Vora NL (2018). Ethical and counseling challenges in prenatal exome sequencing. Prenatal Diagnosis, 38(12), 897–903. 10.1002/pd.5353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn R, & Parker M (2018). Opening Pandora’s box?: ethical issues in prenatal whole genome and exome sequencing. Prenatal Diagnosis, 38(1), 20–25. 10.1002/pd.5114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Society for Prenatal Diagnosis, Society for Maternal and Fetal Medicine, & Perinatal Quality Foundation (2018). Joint Position Statement from the International Society for Prenatal Diagnosis (ISPD), the Society for Maternal Fetal Medicine (SMFM), and the Perinatal Quality Foundation (PQF) on the use of genome-wide sequencing for fetal diagnosis. Prenatal Diagnosis, 38(1), 6–9. 10.1002/pd.5195 [DOI] [PubMed] [Google Scholar]
- Lord J, McMullan DJ, Eberhardt RY, Rinck G, Hamilton SJ, Quinlan-Jones E, … Wilson E (2019). Prenatal exome sequencing analysis in fetal structural anomalies detected by ultrasonography (PAGE): a cohort study. The Lancet, 393(10173), 747–757. 10.1016/S0140-6736(18)31940-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews TJ, Macdorman MF, & Thoma ME (2015). Infant mortality statistics from the 2013 period linked birth/infant death data set. National Vital Statistics Reports, 64(9), 1–30. [PubMed] [Google Scholar]
- Mazzola SE, O’Connor B, & Yashar BM (2019). Primary care physicians’ understanding and utilization of pediatric exome sequencing results. Journal of Genetic Counseling, 28(6), 1130–1138. 10.1002/jgc4.1163 [DOI] [PubMed] [Google Scholar]
- Mikhaelian M, Veach PM, Macfarlane I, Leroy BS, & Bower M (2013). Prenatal chromosomal microarray analysis: A survey of prenatal genetic counselors’ experiences and attitudes. Prenatal Diagnosis, 33(4), 371–377. 10.1002/pd.4071 [DOI] [PubMed] [Google Scholar]
- Monaghan KG, Leach NT, Pekarek D, Prasad P, & Rose NC (2020). The use of fetal exome sequencing in prenatal diagnosis: a points to consider document of the American College of Medical Genetics and Genomics (ACMG). Genetics in Medicine, 22(4), 675–680. 10.1038/s41436-019-0731-7 [DOI] [PubMed] [Google Scholar]
- Niguidula N, Alamillo C, Shahmirzadi Mowlavi L, Powis Z, Cohen JS, & Farwell Hagman KD (2018). Clinical whole-exome sequencing results impact medical management. Molecular Genetics and Genomic Medicine, 6(6), 1068–1078. 10.1002/mgg3.484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Normand EA, Braxton A, Nassef S, Ward PA, Vetrini F, He W, … Yang Y (2018). Clinical exome sequencing for fetuses with ultrasound abnormalities and a suspected Mendelian disorder. Genome Medicine, 10(74). 10.1186/s13073-018-0582-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrovski S, Aggarwal V, Giordano JL, Stosic M, Wou K, Bier L, … Wapner RJ (2019). Whole-exome sequencing in the evaluation of fetal structural anomalies: a prospective cohort study. The Lancet, 393(10173), 758–767. 10.1016/S0140-6736(18)32042-7 [DOI] [PubMed] [Google Scholar]
- Pratt M, Garritty C, Thuku M, Esmaeilisaraji L, Hamel C, Hartley T, … Armour CM (2020). Application of exome sequencing for prenatal diagnosis: a rapid scoping review. Genetics in Medicine, 22(12), 1925–1934. 10.1038/s41436-020-0918-y [DOI] [PubMed] [Google Scholar]
- Quinlan-Jones E, Kilby MD, Greenfield S, Parker M, McMullan D, Hurles ME, & Hillman SC (2016). Prenatal whole exome sequencing: the views of clinicians, scientists, genetic counsellors and patient representatives. Prenatal Diagnosis, 36(10), 935–941. 10.1002/pd.4916 [DOI] [PubMed] [Google Scholar]
- Sabatini LM, Mathews C, Ptak D, Doshi S, Tynan K, Hegde MR, … Bossler AD (2016). Genomic Sequencing Procedure Microcosting Analysis and Health Economic Cost-Impact Analysis: A Report of the Association for Molecular Pathology. Journal of Molecular Diagnostics, 18(3), 319–328. 10.1016/j.jmoldx.2015.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadava SM, & Ashkinadze E (2017). 125: Whole exome sequencing (WES) in prenatal diagnosis for carefully selected cases. 61 American Journal of Obstetrics and Gynecology, 216(1), 87–88. 10.1016/j.ajog.2016.11.029 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


