Fig. 3.
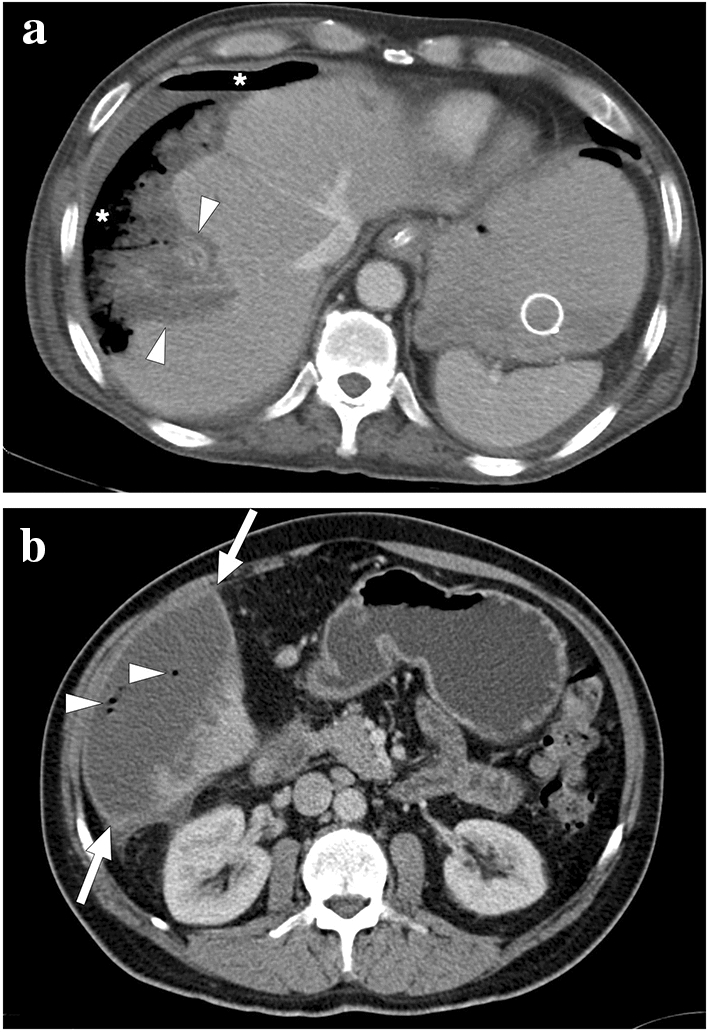
Two different patients with complicated liver infarcts. a A 65-year-old male patient with pancreatic adenocarcinoma underwent a Whipple operation. Three weeks after the operation, the patient presented with severe hematemesis. CT angiography revealed a gastroduodenal artery pseudoaneurysm as the underlying cause of upper gastrointestinal tract bleeding (not shown). An emergent catheter angiography and subsequent percutaneous embolization were performed. Ten days after the embolization, the patient again presented to ER with high fever, hypotension, and severe right upper quadrant pain. Axial plane postcontrast CT image showed necrotic liver parenchyma (arrowheads) with subcapsular and subdiaphragmatic air densities (asterisks). The constellation of imaging findings was found to represent the superinfection of the gangrenous liver segment. Emergent surgery was planned, but the patient expired 3 h after the CT scan. b A 57-year-old male patient underwent catheter angiography embolization of the giant liver hemangioma in segment 6. Twelve days after the embolization, the patient presented to the ER with a high fever, chills, and right upper quadrant pain. An emergent contrast-enhanced abdominal CT showed a large infarcted area in segment 6 (arrows) with air bubbles within this parenchymal segment (arrowheads). The imaging and clinical findings were considered to represent a superinfection of the infarcted parenchyma. Imaging-guided aspiration revealed purulent content and confirmed the diagnosis
