Fig. 8.
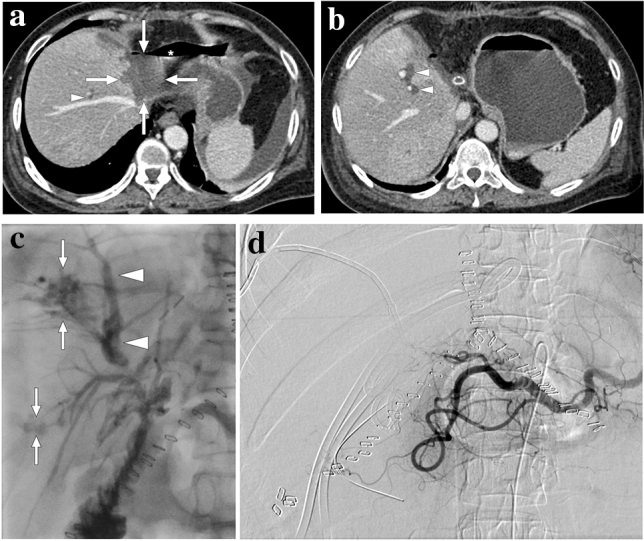
A 55-year-old female patient with a 2-year history of primary sclerosing cholangitis underwent right liver lobe transplantation from a living donor. On day 4 after the transplantation surgery, the abdominopelvic CT exam was within normal limits (not shown). On day 10, bile containing serous fluid leakage was observed through the abdominal incision scar. a and b Axial plane postcontrast abdominal CT images showed a newly developed collection (arrows) containing air–fluid levels (asterisk) along the resection line between the liver and stomach, which was found to represent a biloma. Mild dilatation in the intrahepatic bile ducts was also observed (arrowheads). Subsequent percutaneous transhepatic cholangiography (PTC) demonstrated leakage from the biliary anastomosis site, and percutaneous biliary drainage was subsequently performed. During follow-up, serum bilirubin levels increased progressively despite adequate biliary drainage. c Three months after the transplantation, follow-up PTC revealed dilatation of intrahepatic bile ducts (arrowheads) and leakage of contrast medium into the periportal space (arrows). d To rule out ischemic cholangiopathy, invasive angiography was performed, which revealed the complete occlusion of the hepatic artery. Unfortunately, the patient's clinical condition deteriorated progressively, and the patient expired due to biliary sepsis 2 weeks after the angiography
