Fig. 9.
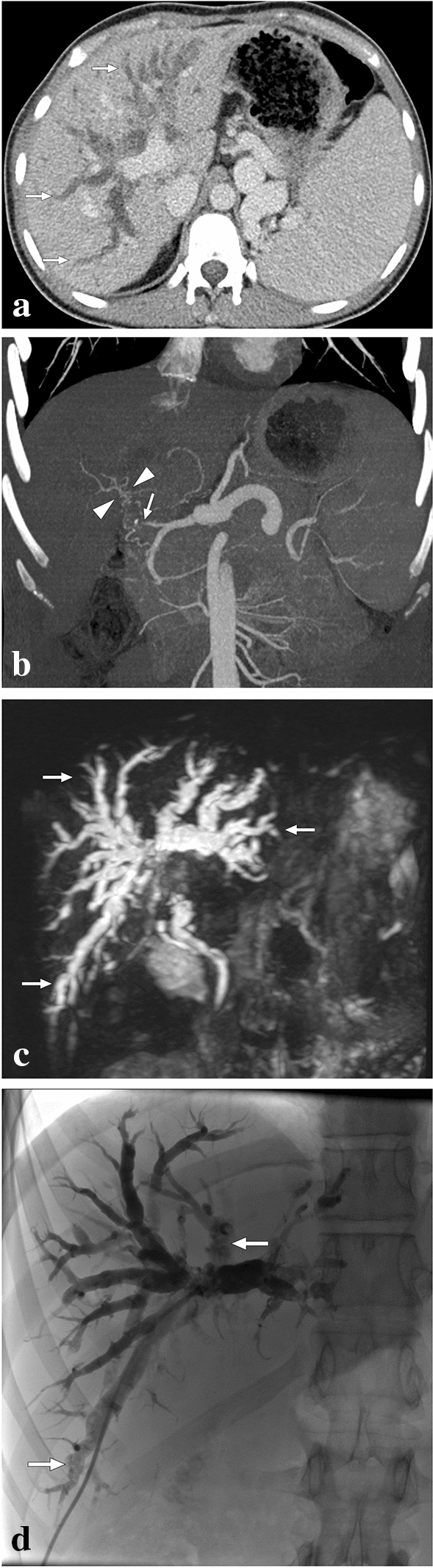
A 20-year-old male who had undergone cadaveric whole liver transplantation due to autoimmune hepatitis presented with new-onset jaundice 10 months after the transplantation. Hepatobiliary US showed diffuse dilatation of intrahepatic bile ducts, and spectral Doppler US revealed a low hepatic arterial resistive index. a Axial plane postcontrast CT image demonstrated extensive intrahepatic bile duct dilation (arrows). Also noted were splenomegaly and enlarged splenic veins. b CT Angiography showed total occlusion of the hepatic artery graft (arrow) with multiple small-sized arterial collaterals (arrowheads) at the level of the hepatic hilus. c 3D-MRCP image better demonstrated the extent of biliary involvement, which may also suggest an obstructive biliary dilatation secondary to a hepatic hilar mass. The constellation of imaging findings suggested ischemic cholangiopathy, and the patient was managed conservatively with repeated biliary drainage interventions. d PTC image 2 years after the transplantation showed biliary sludge and debris formation (arrows) within the dilated intrahepatic bile ducts, and biliary drainage revealed purulent bile content. Despite repeated biliary interventions and appropriate medical treatment, the patient's hepatic functions gradually deteriorated, and a re-transplantation was planned. Unfortunately, the patient expired before the second liver transplantation
