ABSTRACT
Background:
Given the highly stressful environment surrounding the SARS-CoV-2 pandemic, healthcare workers (HCW) and public safety personnel (PSP) are at an elevated risk for adverse psychological outcomes, including posttraumatic stress disorder (PTSD) and alcohol/substance use problems. As such, the study aimed to identify associations between PTSD severity, related dissociation and emotion dysregulation symptoms, and alcohol/substance use problems among HCWs and PSP.
Methods:
A subset of data (N = 498; HCWs = 299; PSP = 199) was extracted from a larger study examining psychological variables among Canadian HCWs and PSP during the pandemic. Structural equation modelling assessed associations between PTSD symptoms and alcohol/substance use-related problems with dissociation and emotion dysregulation as mediators.
Results:
Among HCWs, dissociation fully mediated the relation between PTSD and alcohol-related problems (indirect effect β = .133, p = .03) and emotion dysregulation partially mediated the relation between PTSD and substance-related problems (indirect effect β = .151, p = .046). In PSP, emotion dysregulation fully mediated the relation between PTSD and alcohol-related problems (indirect effects β = .184, p = .005). For substance-related problems among PSP, neither emotion dysregulation nor dissociation (ps >.05) had any effects.
Conclusion:
To our knowledge, this is the first study examining associations between PTSD severity and alcohol/substance use-related problems via mediating impacts of emotion dysregulation and dissociation among HCWs and PSP during the SARS-CoV-2 pandemic. These findings highlight dissociation and emotion dysregulation as important therapeutic targets for structured interventions aimed at reducing the burden of PTSD and/or SUD among Canadian HCWs or PSP suffering from the adverse mental health impacts of the SARS-CoV-2 pandemic.
KEYWORDS: Trauma, dissociation, emotion dysregulation, alcohol, substance use
HIGHLIGHTS
Among healthcare workers, dissociation mediated relation between posttraumatic stress disorder (PTSD) severity and alcohol-related problems and emotion dysregulation mediated relation between PTSD severity and substance-related problems.
Among public safety personnel, emotion dysregulation mediated relation between PTSD severity and alcohol-related problems. Neither dissociation nor emotion dysregulation mediated relation between PTSD severity and substance-related problems.
Results underscore dissociation and emotion dysregulation as potential key therapeutic targets for intervention for healthcare workers and public safety personnel struggling with PTSD and comorbid alcohol/substance use-related problems.
Abstract
Antecedentes: Dado el ambiente altamente estresante que ha rodeado la pandemia del SARS-CoV-2, los trabajadores de la salud (HCW en su sigla en inglés) y el personal de seguridad pública (PSP en su sigla en inglés) se encuentran con un riesgo más elevado de resultados psicológicos adversos, incluyendo el trastorno de estrés postraumático (TEPT) y problemas de uso de alcohol y substancias (SUD en su sigla en inglés). Como tal, el estudio buscó identificar las asociaciones entre la severidad del TEPT, la disociación asociada y los síntomas de desregulación emocional, y los problemas de uso de alcohol y substancias entre los HCWs y PSP.
Métodos: Se extrajo una muestra de los datos (N = 498; HCWs = 299; PSP = 199) de un estudio mayor examinando las variables psicológicas entre HCWs y PSP canadienses durante la pandemia. El modelamiento de ecuaciones estructurales evaluó las asociaciones entre los síntomas de TEPT y los problemas relacionados con el uso de alcohol y substancias con la disociación y la desregulación emocional como mediadores.
Resultados: Entre HCWs, la disociación medió completamente la relación entre TEPT y los problemas relacionados con el alcohol (efecto indirecto β = .133, p = .03) y la desregulación emocional medió parcialmente la relación entre TEPT y los problemas relacionados con la substancia (efecto indirecto β = .151, p = .046). En los PSP, la desregulación emocional medió completamente la relación entre TEPT y problemas relacionados con el alcohol (efectos indirectos β = .184, p = .005). Para los problemas relacionados al alcohol entre PSP, ni la desregulación emocional ni la disociación (ps >.05) tuvieron algún efecto.
Conclusión: A nuestro conocimiento, este es el primer estudio que examina las asociaciones entre la severidad del TEPT y los problemas relacionados al uso de alcohol y substancias por medio de los impactos mediadores de la desregulación emocional y la disociación entre los HCWs y PSP durante la pandemia del SARS-CoV-2. Estos hallazgos resaltan la disociación y la desregulación emocional como objetivos terapéuticos importantes para intervenciones estructuradas orientadas a reducir la carga del TEPT y/o SUD entre los HCWs o PSP canadienses que se encuentran sufriendo los impactos adversos de la pandemia del SARS-CoV-2 en su salud mental.
PALABRAS CLAVE: Trauma, desregulación emocional, alcohol, uso de substancias
Abstract
背景:鉴于 SARS-CoV-2 疫情周围的高压环境,医护人员 (HCW) 和公共安全人员 (PSP) 出现不良心理后果的风险较高,包括创伤后应激障碍 (PTSD) 和酒精/物质使用问题。 因此,本研究旨在确定 HCW 和 PSP 中 PTSD 严重程度、相关解离和情绪失调症状以及酒精/物质使用问题之间的关联。
方法:从一项较大规模的考查了疫情期间加拿大 HCW 和 PSP 心理变量的研究中提取了一个数据子集(N = 498;HCWs = 299;PSP = 199)。结构方程模型评估了以解离和情绪失调作为中介,PTSD 症状与酒精/物质使用相关问题之间的关联。
结果:在HCW中,解离完全中介了 PTSD 与酒精相关问题之间的关系(间接效应 β = .133,p = .03),情绪失调部分中介了 PTSD 与物质相关问题之间的关系(间接效应 β = .151,p = .046)。 在 PSP 中,情绪失调完全中介了 PTSD 与酒精相关问题之间的关系(间接效应 β = .184,p = .005)。 对于 PSP 中的物质相关问题,情绪失调和解离 (ps >.05) 都没有任何影响。
结论:据我们所知,这是第一项通过在 SARS-CoV-2 疫情期间 HCW 和 PSP 中通过情绪失调和解离的中介影响来检验 PTSD 严重程度与酒精/物质使用相关问题之间关联的研究。 这些发现强调,解离和情绪失调是旨在减轻加拿大HCW或 PSP 遭受 SARS-CoV-2 疫情不良心理健康影响PTSD 和/或 SUD 负担的结构化干预重要治疗靶点。
关键词: 创伤, 解离, 情绪失调, 酒精, 物质使用
1. Introduction
Healthcare Workers (HCWs; e.g. nurses, physicians, personal support workers, and respiratory therapists) and Public Safety Personnel (PSP; e.g. paramedics, firefighters, police officers, and dispatchers) serve in high-stress occupations with elevated risk for trauma exposure (Badger et al., 2008; Carleton et al., 2018a, 2019; Collins & Long, 2003; D’ettorre et al., 2020). Critically, trauma exposure is inextricably linked to the development of posttraumatic stress disorder (PTSD) among these professions (Carleton et al., 2018a, 2018c, 2019; Robles et al., 2021; Saragih et al., 2021). Throughout the SARS-CoV-2 (COVID-19) pandemic, HCWs and PSP have faced an unprecedented risk of developing or further elevating their risk of adverse psychological outcomes such as depression, anxiety, PTSD, and alcohol/substance use (Robles et al., 2021; Saragih et al., 2021; Young et al., 2021). PTSD may develop following exposure to a traumatic event (American Psychological Association, 2013) and is a highly prevalent and functionally debilitating mental health disorder (Norman et al., 2007; Westphal et al., 2011). Within the Diagnostic Statistical Manual for Mental Disorders-5th version (DSM-5), symptoms of PTSD are categorized into four clusters: intrusive thoughts and memories, avoidance behaviours, negative alterations in cognition and mood (NACM), and reactivity (American Psychological Association, 2013). Furthermore, ∼30% of individuals with PTSD meet the criteria for the dissociative subtype which consists of the four symptom clusters with the addition of the depersonalization and derealization symptom clusters (American Psychological Association, 2013).
Emerging literature during the SARS-CoV-2 pandemic indicates that mental health concerns (including alcohol/substance use) have worsened for HCWs and PSP (Hall, 2020; Mehta et al., 2022; Mongeau-Pérusse et al., 2021; Pestana et al., 2022; Robles et al., 2021; Saragih et al., 2021; Turna et al., 2022; Young et al., 2021), with the number of healthcare visits by HCWs for mental health and substance use problems also increasing throughout (Myran et al., 2022). Based on a recent meta-analysis, the global prevalence rate of PTSD among HCWs during the pandemic is estimated to be 49% (Saragih et al., 2021). In Canada, 25% of intensive care unit HCWs endorsed symptoms consonant with probable PTSD (Mehta et al., 2022). Furthermore, comparing mental health concerns among HCWs in Canada, Brazil, and the USA, Canadian HCWs reported the highest rates of anxiety, depression, and increased alcohol and cannabis use compared to their international counterparts (Turna et al., 2022). In a nationwide cohort study, Canadian HCWs reported increased alcohol consumption compared to pre-pandemic (Mongeau-Pérusse et al., 2021). To our knowledge, no literature has examined prevalence rates of PTSD and alcohol/substance use among Canadian PSP during the pandemic underscoring the need to further study this occupational group. However, pre-pandemic literature indicates 26.7% of Canadian PSP experience at least one mental health disorder during their lifetime and 5.9% of PSP met criteria for hazardous alcohol use (Carleton et al., 2018b) and that it is feasible to expect these rates would increase with the additional stressors of the SARS-CoV-2 pandemic. To date, the majority of literature examining PTSD and alcohol/substance use among HCWs during the pandemic has focused on prevalence rates. While important, prevalence rates do not provide insightful information as to how symptoms of PTSD and alcohol/substance-related problems are associated and impact each other, potentially informing treatment targets for intervention. Accordingly, little is known about the association between PTSD and alcohol/substance-related problems in these groups, as well as about psychological factors (e.g. dissociation, emotional dysregulation) that may mediate this relation, as has been shown in adult treatment-seeking samples (Patel et al., 2022; Weiss et al., 2012).
Critically, there are other factors that may explain the association between PTSD symptoms and alcohol/substance-related problems, providing more nuanced therapeutic targets for intervention. Factors such as dissociation (i.e. a form of psychological escape when physical escape is improbable; 21) and emotion dysregulation (i.e. difficulties in processing and healthily responding to emotional stimuli; Gross & Feldman Barrett, 2011) have been independently linked to PTSD (Spiegel, 2011; Westphal et al., 2017; Wolf et al., 2012) and Substance Use Disorders (SUDs; Garke et al., 2021) pre-pandemic. Dissociation and emotion dysregulation that may be co-occurring with the symptoms of PTSD may drive individuals to use alcohol and non-alcohol substances to cope with their PTSD, as posited by the self-medication hypothesis (Khantzian, 1997). However, limited literature exists examining the role of these factors in explaining the associations between PTSD and SUD, with the focus primarily on clinical samples (Patel et al., 2022; Weiss et al., 2012, 2013). By examining the role of these variables in the relation between PTSD and alcohol/substance-related problems among HCWs and PSP, the results may indicate potentially relevant clinical treatment targets that may be applicable to other adult treatment-seeking samples.
Given higher prevalence rates of PTSD and alcohol/substance use among HCWs and potentially PSP during the pandemic representing a high-risk population likely to develop PTSD and/or SUD (Carmassi et al., 2020), combined with prior literature indicating a high prevalence of comorbid PTSD+SUD in adult treatment-seeking samples (Chilcoat & Menard, 2004; Patel et al., 2021, 2022; Pietrzak et al., 2011), there is a crucial need to identify associations between PTSD and alcohol/substance-related problems among HCWs and PSP and examine mediating factors such as dissociation and emotion dysregulation that may help explain the associations. Accordingly, the purpose of the current study was to identify the global and symptom cluster level associations between PTSD and alcohol/substance use-related problems among samples of Canadian HCWs and PSP with data collected during the height of the pandemic. Furthermore, this study examined the roles of underlying mechanisms (i.e. emotion dysregulation and dissociation) in assessing the associations between PTSD symptoms and alcohol/substance-related problems.
2. Methods
2.1. Participants
Data was drawn from a larger survey-based study assessing psychological and cognitive functioning among HCWs and PSP from various provinces across Canada, most of whom were still actively working (HCWs = 96.%; PSP = 91.5%). Canadian HCWs/PSP were recruited through social media and email advertisements sent from willing healthcare organizations across Canada. Eligibility criteria included: (1) at least 18 years of age, (2) speak and read English, and (3) have provided healthcare or emergency services during the SARS-CoV-2 pandemic in Canada. Participants completed an online battery of self-report assessments during the SARS-CoV-2 pandemic (June 2021 – January 2022) via Research Electronic Data Capture (Harris et al., 2009). Participants provided written informed consent through e-signatures. Upon completion, participants could choose to be entered into a draw for a gift card. This study was approved by Hamilton Integrated Research Ethics Board (#12667). Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
In the present study, 633 HCWs and PSP consented to participate. Of this, one-hundred and thirty-three (n = 133) were removed due to insufficient survey completion (i.e. did not complete demographics and at least one full scale). This yielded a sample of N = 498 participants in the final working data set (two participants removed due to missing demographic data), in which there were HCWs (n = 299) and PSP (n = 199). Missing data were imputed using multiple imputation methods (described briefly in Data Analytic Plan and further in the Supplemental Materials).
2.2. Measures
A subset of measures from the larger study was included in the current study (described below). Demographics included age, biological sex at birth, and education.
2.2.1. Posttraumatic stress disorder severity
PTSD severity in the past month was assessed using the Posttraumatic Stress Disorder Checklist for Diagnostic and Statistical Manual-5 (PCL-5; [Blevins et al., 2015]), a 20-item measure (range: 0–80) comprised of four clusters: Cluster B (Intrusive thoughts and memories; range = 0–20), Cluster C (Avoidance behaviours; range = 0–8), Cluster D (Negative Alterations in Cognition and Mood; range = 0–28), and Cluster E (Alterations in Arousal; range = 0–20). SEM was used to generate a latent factor of PTSD symptoms from the cluster scores (see Supplemental Materials).
2.2.2. Alcohol-Related problems
Alcohol use frequency and alcohol-related problems experienced over the past 12 months were measured using the Alcohol Use Disorders Identification Test (AUDIT), a 10-item self-report screen (range: 0–40) assessing the frequency and severity of alcohol use (Saunders et al., 1993). The AUDIT assesses both consumption of alcohol (three items) and problems related to alcohol consumption (seven items). As such, the AUDIT is referred to as assessing alcohol-related problems rather than consumption. The sum score on the AUDIT was included as an outcome variable in the mediation model.
2.2.3. Substance-related problems
Non-alcohol substance use (i.e. cannabis, illicit substances, prescription medication not used as prescribed, etc.) frequency and substance-related problems experienced over the past 12 months were measured using the Drug Use Disorders Identification Test (DUDIT). It is an 11-item self-report screen (range: 0–44) assessing the frequency and severity of substance use (Berman et al., 2005). Typically, the DUDIT is referred to as assessing substance-related problems rather than consumption. The sum score on the DUDIT was included as an outcome variable in the mediation model.
2.2.4. Emotion dysregulation
The Difficulties in Emotion Regulation Scale (DERS) is a 36-item (range: 36–180) self-report questionnaire assessing six facets of emotion regulation within the past month: (1) non-acceptance of emotional responses, (2) difficulty engaging in goal-directed behaviour, (3) impulse control difficulties, (4) lack of emotional awareness, (5) limited access to emotion regulation strategies, and (6) lack of emotional clarity (Gratz & Roemer, 2004). SEM was used to generate a latent factor of emotion dysregulation from the subscale scores (see Supplemental Materials).
2.2.5. Dissociative symptomatology
The Multiscale Dissociation Inventory was used to assess dissociative symptoms within the past month (Briere et al., 2005). The MDI is a 30-item self-report questionnaire and measures six different types (range for each subscale: 5–25) of dissociative responses: (1) disengagement, (2) depersonalization, (3) derealization, (4) emotional constriction/numbing, (5) memory disturbance, and (6) identity dissociation. SEM was used to generate a latent factor of dissociative symptoms from the subscale scores (see Supplemental Materials).
2.2.6. Depression, anxiety, and stress
Symptoms of depression, anxiety, and stress over the past week were measured using the DASS-21 (Lovibond & Lovibond, 1995). The scale contains 21 items assessing depressive symptoms (seven items), anxiety symptoms (seven items), and stress symptoms (seven items). Three scores are generated from the scale, one for each category (range for each scale: 0–21). Subscale scores for Depression, Anxiety, and Stress were included as covariates in the mediation model to account for PTSD symptom overlap with depression and anxiety (Gros et al., 2012) and account for occupational stress.
2.2.7. Childhood adversity
The Adverse Childhood Experience Scale (ACES) is a 10-item self-report questionnaire (range: 0–10) used to assess the endorsement of adverse childhood experiences (Merrick et al., 2017). A sum score on the ACES was used as a covariate in the mediation model to account for the impacts of childhood adversity on PTSD severity and substance use (Goodgame Huffman et al., 2022).
2.3. Data analysis plan
Prior to data analysis, missing data (∼40% in HCWs; ∼37% in PSP) were imputed using multiple imputation, a procedure for generating possible values for missing data via a series of regression analyses and an iterative, Bayesian algorithm to generate new estimates for each generated set of imputations (Campion & Rubin, 1989; Enders, 2017). No systematic relationship between missing data was determined; missing data were assumed to be missing at random. Fully condition specification method was used to deal with missing data during imputation. All variables were included in each multiple imputation procedure. Only items that contributed to a total score for each scale were imputed; demographic data, yes/no responses, and other variables were not imputed but were used as predictors of missing values. Five imputed datasets were produced from imputation and pooled into a final imputed dataset. Total scores from the imputed dataset were compared to total scores from the original data set with missing values. No significant differences were found (see Supplemental Tables 1 and 2 for means and standard deviations of non-imputed and imputed datasets for HCWs and PSP).
Table 1.
Sample characteristics for HCWs and PSP.
| HCWs (N = 299) | PSP (N = 199) | t/X2 | p | |
|---|---|---|---|---|
| Demographics | ||||
| Age (%) | ||||
| 20–29 years old | 16.1 | 21.6 | 6.64 | .249 |
| 30–39 years old | 33.1 | 37.7 | ||
| 40–49 years old | 29.1 | 23.6 | ||
| 50–59 years old | 15.7 | 13.6 | ||
| 60–69 years old | 5.4 | 3.5 | ||
| 70–79 years old | 0.7 | 0 | ||
| Sex (% Female) | 91.6% | 39.7% | 154.49 | <.001 |
| Race (%) | ||||
| African/Caribbean | 0.02 | 0 | 6.69 | .010 |
| Caucasian | 86.6 | 94.4 | ||
| East Asian | 0.03 | 0.005 | ||
| Indigenous | 0.02 | 0.03 | ||
| Latin American | 0 | 0.01 | ||
| Pacific Islander | 0 | 0 | ||
| South East Asian | 0.02 | 0.01 | ||
| Other | 0.05 | 0.01 | ||
| Education (%) | ||||
| Completed some college | 2.3 | 10.1 | 119.68 | <.001 |
| Completed college diploma | 18.7 | 50.8 | ||
| Completed some university | 5.7 | 12.1 | ||
| Completed Bachelor's university degree | 45.2 | 24.6 | ||
| Completed Master's/Graduate degree | 21.4 | 1.0 | ||
| Completed Doctoral degree | 5.4 | 0 | ||
| Other | 1.3 | 1.5 | ||
| Childhood Adversity | 3.11 (2.44) | 2.76 (2.42) | 1.614 | .107 |
| Psychiatric Symptoms | ||||
| Depression | 14.45 (9.22) | 13.13 (9.33) | 1.56 | .120 |
| Anxiety | 10.37 (7.30) | 8.33 (7.07) | 3.10 | .002 |
| Stress | 18.73 (7.89) | 16.69 (8.52) | 2.74 | .006 |
| Provisional PTSD Diagnosis (%) | 28.% | 30% | .234 | .629 |
| Global PTSD Severity (PCL-5) | 28.43 (15.27) | 27.20 (17.26) | .819 | .413 |
| Intrusions | 6.94 (4.27) | 6.20 (4.57) | 1.87 | .062 |
| Avoidance | 3.10 (2.15) | 2.72 (2.23) | 1.93 | .055 |
| NACM | 10.27 (6.05) | 9.155 (6.58) | 1.95 | .052 |
| Reactivity | 8.12 (4.48) | 9.13 (5.60) | −2.14 | .033 |
| Substance Use Symptoms | ||||
| Alcohol Related Problems (AUDIT) | 3.92 (3.15) | 6.16 (4.86) | −5.74 | <.001 |
| Substance Related Problems (DUDIT) | 2.26 (3.45) | 2.25 (2.98) | .045 | .964 |
| Cognitive and Emotional Variables | ||||
| Dissociative Symptoms (MDI) | ||||
| Depersonalization | 7.93 (2.86) | 7.74 (3.05) | .721 | .471 |
| Derealization | 7.97 (2.76) | 8.18 (2.99) | −.723 | .470 |
| Memory Disturbance | 8.08 (2.71) | 9.14 (3.64) | −3.49 | <.001 |
| Disengagement | 11.94 (3.26) | 12.05 (4.15) | −.291 | .771 |
| Emotional Constriction | 9.70 (4.02) | 10.53 (4.63) | −2.07 | .040 |
| Identity Dissociation | 5.51 (1.10) | 5.83 (1.55) | −2.49 | .013 |
| Emotion Dysregulation (DERS) | 82.55 (19.69) | 86.61 (20.73) | −2.21 | .027 |
| Non-Acceptance of Emotional Responses | 13.92 (4.99) | 14.85 (5.41) | −1.97 | .049 |
| Difficulty with Goal-Directed Behaviour | 14.09 (4.17) | 13.95 (4.21) | .375 | .708 |
| Impulse Control Difficulties | 10.74 (3.87) | 11.01 (3.84) | −.766 | .444 |
| Lack of Emotional Awareness | 15.72 (4.30) | 17.65 (5.14) | −4.37 | <.001 |
| Limited Access to Emotion Regulation Strategies | 17.28 (6.06) | 17.65 (5.89) | −.683 | .495 |
| Lack of Emotional Clarity | 10.80 (3.29) | 11.51 (3.59) | −2.28 | .023 |
Note. All values reported are means (standard deviations) except for age, sex, race, education, and provisional posttraumatic stress disorder (PTSD) diagnosis where percentages are displayed. For age, sex, race, education, and provisional PTSD diagnosis, Chi-square tests were used to evaluate group differences; all other variables used independent samples t-tests. Depression, Anxiety, and Stress variables are based on subscales of the Depression, Anxiety, Stress Scale-21. Provisional PTSD Diagnosis was based on a cut-off score of 33+ on Posttraumatic Checklist for DSM-5 (PCL-5). Global PTSD Severity is based on the sum score on PCL-5.
Table 2.
All direct and indirect paths from parallel mediation model for HCWs.
| Path | β | S.E. | p |
|---|---|---|---|
| PTSD → Alcohol-Related Problems (direct) | .094 | .108 | .38 |
| PTSD → Drug-Related Problems (direct) | −.210 | .105 | .04 |
| PTSD → Dissociation | .680 | .036 | < .00 |
| PTSD → Emotion Dysregulation | .746 | .034 | < .00 |
| Dissociation → Alcohol-Related Problems | .196 | .089 | .03 |
| Dissociation → Drug-Related Problems | .141 | .084 | .09 |
| Emotion Dysregulation → Alcohol-Related Problems | −.022 | .106 | .84 |
| Emotion Dysregulation → Drug-Related Problems | .202 | .100 | .04 |
| PTSD → Dissociation → Alcohol-Related Problems (indirect) | .133 | .061 | .03 |
| PTSD → Dissociation → Drug-Related Problems (indirect) | .096 | .058 | .10 |
| PTSD → Emotion Dysregulation → Alcohol-Related Problems (indirect) | −.016 | .079 | .84 |
| PTSD → Emotion Dysregulation → Drug-Related Problems (indirect) | .151 | .076 | .05 |
Note: β (beta) represents the standardized co-efficient estimate; S.E. represents the standard error of the beta co-efficient estimate.
Descriptive statistics and independent samples t-tests between HCWs and PSP were run in IBM SPSS Statistics Version 27 among the study variables to inform whether group analyses should be conducted. There were significant differences among key variables (see Table 1). As such, separate analyses were conducted for HCWs and PSP. Structural equation modelling was implemented in MPlus Version 8.4 (Muthén & Muthén, 2017) using maximum likelihood estimation to assess the mediating effects of dissociation and emotion dysregulation on the association between PTSD severity and alcohol/substance-related problems. Before modelling, the alcohol-related problems measure (AUDIT sum score), substance-related problems measure (DUDIT sum score), and the identity dissociation subscale from the MDI were square-root transformed based on benchmarks of skewness >2 and kurtosis >7 (Curran et al., 1996). Following established conventions (Schreiber et al., 2006), an excellent-fitting model has a comparative fit index (CFI) and Tucker Lewis Index (TLI) ≥ 0.95, standardized root mean squared residual (SRMR) of ≤ 0.08, and a root mean square error of approximation (RMSEA) ≤ 0.06. Covariates for all models included age, sex, education, depressive symptoms, anxiety symptoms, stress, and childhood adversity.
Parallel mediation models were run for both HCWs and PSP and tested the direct effects of PTSD symptoms on alcohol- and substance-related problems as well as indirect effects via two mediators: dissociation and emotion dysregulation. In addition, a secondary set of models were run to assess the mediating roles of dissociation and emotion dysregulation on specific PTSD symptom clusters (see Supplemental Materials for Data Analytic Plan and Results). Initial models testing the direct effects of PTSD symptoms on alcohol- and substance-related problems without the presence of the mediators can be found in supplemental materials. To ensure multiple imputation did not unduly effect results, parallel mediation models for HCWs and PSP testing the direct and indirect effects of PTSD symptoms on alcohol- and substance-related problems were run using non-imputed data. The main findings are discussed in the results (for complete results see Supplemental Materials).
3. Results
3.1. Descriptive statistics
The final sample consisted of two groups: HCWs (N = 299) and PSP (N = 199). Sample characteristics can be found in Table 1 and group testing results to indicate which variables of interest were different across the two groups.
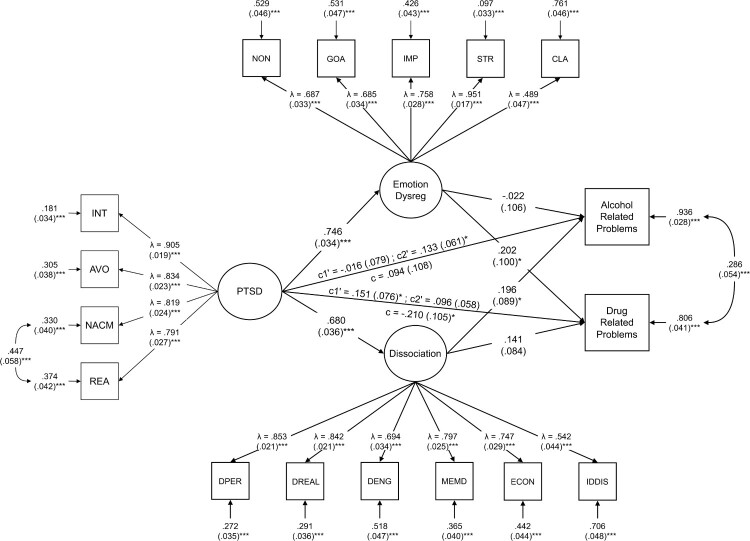
3.2. Healthcare workers
The parallel mediation model assessed the direct and indirect (mediated via dissociation or emotion dysregulation) effects of global PTSD symptoms on alcohol and substance-related problems (see Figure 1 and Table 2). The model accounted for 6.4% of the variance in alcohol-related problems (r2 = .064, p<.05) and 19.4% of the variance in substance-related problems (r2 = .194, p<.0001). Significant covariates in the model included age, education, childhood adversity, depressive, and anxiety symptoms. The direct path from PTSD to alcohol-related problems was significant (β = .212, p<.0001) prior to mediation. After mediation, the direct path was no longer significant (β = .094, p = .383). The indirect path from PTSD to alcohol-related problems was significant via dissociation (indirect effect β = .133, p<.05) whereas the indirect path via emotion dysregulation was not significant (indirect effect β = −.016, p = .835). These results remained consistent among the models run with non-imputed data for HCWs (N = 260). Examining substance-related problems, the direct path from PTSD was not significant prior to the inclusion of mediators (β = .040, p = .492). With the inclusion of mediators, the indirect path via emotion dysregulation was significant (indirect effect β = .151, p<.05), however, the indirect path via dissociation was not significant (indirect effect β = .096, p = .096). Among the models with non-imputed data, the results were non-significant for the indirect effects. However, the magnitude and direction of associations remained the same for emotion dysregulation (indirect effect β = .108, p = .320) and dissociation (indirect effect β = .133, p = .078).
Figure 1.
Parallel mediation model for HCWs. All values are standardized. Standard error for residuals and covariances in parentheses. PTSD = PTSD latent factor, INT = Intrusions, AVO = Avoidance, NACM = Negative Alterations in Cognition and Mood, REA = Reactivity, DPER = Depersonalization, DREAL = Derealization, DENG = Disengagement, MEMD = Memory Disturbance, ECON = Emotional Constriction/Numbing, IDDIS = Identity Dissociation, NON = Non-Acceptance of Emotional Responses, GOA = Difficulty Engaging in Goal-Directed Behaviour, IMP = Impulse Control Difficulties, STR = Lack of Access to Emotion Regulation Strategies, CLA = Lack of Emotional Clarity. Age, sex, education, childhood adversity, depressive symptoms, anxiety symptoms, and stress symptoms were controlled for. Model fit was adequate (c 2(209, N = 299) = 476.46, p < .0001, TLI = .912, CFI = .927, RMSEA = 0.07 [95% CI = .058−.073], SRMR = 0.06). * p < .05; ** p < .01; *** p < .001.
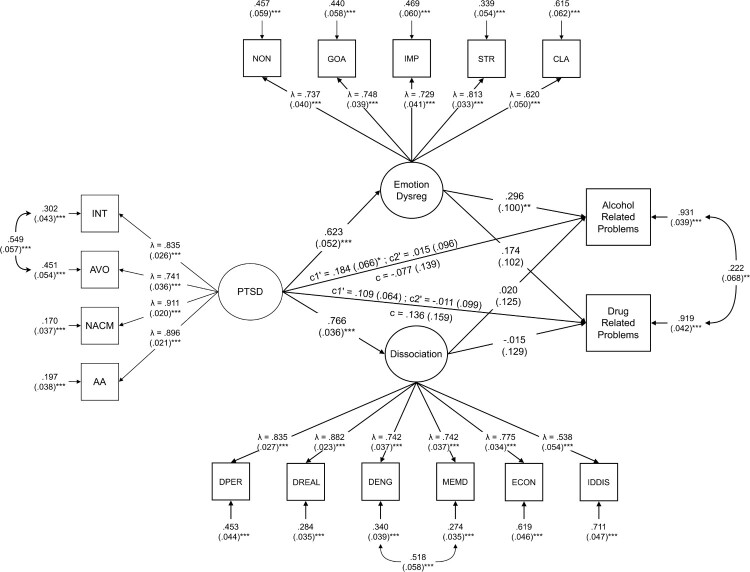
3.3. Public safety personnel
The parallel mediation model assessing the direct and indirect (mediated via dissociation or emotion dysregulation) effects of global PTSD symptoms on alcohol- and substance-related problems (see Figure 2 and Table 3). The model accounted for 6.9% of the variance in alcohol-related problems (r2 = .069, p = .076) and 8.1% of the variance in substance-related problems (r2 = .081, p = .051). Significant covariates in the model included childhood adversity, depressive, anxiety, and stress symptoms. The direct path from PTSD to alcohol-related problems was not significant (β = .129, p = .071) prior to mediation. After mediation, the direct path was still not significant (β = −.077, p = .578). The indirect path from PTSD to alcohol-related problems was not significant via dissociation (indirect effect β = .015, p = .872), whereas the indirect path via emotion dysregulation was significant (indirect effect β = .184, p<.01). These results were relatively consistent with non-imputed data for PSP (N = 141) with dissociation remaining non-significant (indirect effect β = .007, p = .953), whereas, emotion dysregulation was trending (indirect effect β = .229, p = .056). Examining substance-related problems, the direct path from PTSD was not significant prior to the inclusion of mediators (β = .136, p = .396). With the inclusion of mediators, the indirect paths via emotion dysregulation (indirect effect β = .109, p = .091) and dissociation (indirect effect β = −.011, p = .908) were not significant. These results were consistent with the non-imputed data: dissociation (indirect effect β = −.039, p = .761) and emotion dysregulation (indirect effect β = .151, p = .196).
Figure 2.
Parallel mediation model for PSP. All values are standardized. Standard error for residuals and covariances in parentheses. PTSD = PTSD latent factor, INT = Intrusions, AVO = Avoidance, NACM = Negative Alterations in Cognition and Mood, REA = Reactivity, DPER = Depersonalization, DREAL = Derealization, DENG = Disengagement, MEMD = Memory Disturbance, ECON = Emotional Constriction/Numbing, IDDIS = Identity Dissociation, NON = Non-Acceptance of Emotional Responses, GOA = Difficulty Engaging in Goal-Directed Behaviour, IMP = Impulse Control Difficulties, STR = Lack of Access to Emotion Regulation Strategies, CLA = Lack of Emotional Clarity Age, sex, education, childhood adversity, depressive symptoms, anxiety symptoms, and stress symptoms were controlled for. Model fit was adequate (c 2(176, N = 199) = 403.36, p < .0001, TLI = .896, CFI = .913, RMSEA = 0.08 [95% CI = .070−.091], SRMR = 0.07). * p < .05; ** p < .01; *** p < .001.
Table 3.
All direct and indirect paths from parallel mediation model for PSP.
| Path | β | S.E. | p |
|---|---|---|---|
| PTSD → Alcohol-Related Problems (direct) | −.077 | .139 | .58 |
| PTSD → Drug-Related Problems (direct) | .136 | .159 | .39 |
| PTSD → Dissociation | .766 | .036 | < .00 |
| PTSD → Emotion Dysregulation | .623 | .052 | < .00 |
| Dissociation → Alcohol-Related Problems | .020 | .125 | .87 |
| Dissociation → Drug-Related Problems | −.015 | .129 | .91 |
| Emotion Dysregulation → Alcohol-Related Problems | .296 | .100 | .00 |
| Emotion Dysregulation → Drug-Related Problems | .174 | .102 | .09 |
| PTSD → Dissociation → Alcohol-Related Problems (indirect) | .015 | .096 | .87 |
| PTSD → Dissociation → Drug-Related Problems (indirect) | −.011 | .099 | .91 |
| PTSD → Emotion Dysregulation → Alcohol-Related Problems (indirect) | .184 | .066 | .01 |
| PTSD → Emotion Dysregulation → Drug-Related Problems (indirect) | .109 | .064 | .09 |
Note: β (beta) represents the standardized co-efficient estimate; S.E. represents the standard error of the beta co-efficient estimate.
4. Discussion
The current study aimed to identify the associations between PTSD symptoms and alcohol- and substance-related problems among HCWs and PSP during the SARS-CoV-2 pandemic. We found differential associations between PTSD and alcohol- and substance-related problems. Specifically, whereas PTSD symptoms were significantly associated with alcohol-related problems among HCWs, PTSD symptoms were significantly associated with substance-related problems among PSP. Additional examination of putative underlying mechanisms such as dissociation and emotion dysregulation pointed towards the differential mediating roles of these factors in the relation between PTSD and alcohol- and substance-related problems in these two samples. Here, whereas dissociation significantly mediated the relation between PTSD and alcohol-related problems among HCWs, emotion dysregulation mediated the relation between PTSD and substance-related problems in this group. By contrast, among PSP, emotion dysregulation mediated the relation between PTSD and alcohol-related problems; there were no significant mediations for substance-related problems in this group.
The majority of the literature examining PTSD and alcohol/substance use among HCWs and PSP during the SARS-CoV-2 pandemic has focused on prevalence rates and frequency of use. Rates of probable PTSD seen in the current study (25–26%) are similar to rates previously published during the pandemic (Mehta et al., 2022; Saragih et al., 2021). In addition, alcohol- and substance use-related problems among our sample appear consistent with literature where relative increases in alcohol use and related problems are reported during the pandemic (Mongeau-Pérusse et al., 2021; Turna et al., 2022; Young et al., 2021). No literature, to our knowledge, has examined how the symptoms of PTSD or SUD impact one another among HCWs and PSP during the pandemic.
Among current literature examining these associations during the pandemic, one study reported significant associations between PTSD symptoms and alcohol-related problems among a general PSP sample across the United States (Bonumwezi et al., 2022). Given similar low rates of alcohol-related problems and PTSD severity (Bonumwezi et al., 2022), symptom severity may be a potential moderator of the associations between PTSD and alcohol-related problems. Although this hypothesis remains to be examined in follow-up studies, it is notable that Patel et al. (2022) found a contrasting pattern of associations between PTSD and alcohol-related problems in a civilian sample with a high acuity of PTSD and dissociative symptoms as compared to the current PSP sample. In Patel et al. (2021), dissociative symptoms fully mediated the relation between PTSD and alcohol-related problems in this inpatient sample undergoing treatment for PTSD and trauma-related disorders. Further research is needed in PSP samples presenting with high acuity of PTSD and dissociative symptoms to elucidate whether this pattern remains among more functionally impaired PSP.
In terms of examining symptom cluster associations between PTSD and alcohol- and substance-related problems, the majority of the extant literature was published prior to the SARS-CoV-2 pandemic. Similar to current results, significant associations between reactivity symptoms of PTSD and alcohol-related problems were seen among Red Cross workers following the 11 September 2001 attacks (Simons et al., 2005). Among police officers, avoidance symptoms of PTSD were associated with alcohol-related problems (Chopko et al., 2013); however, the current study found no such association (see Supplemental Materials). Critically, the current sample amalgamates multiple PSP occupations, not only police officers. Future research is required to analyze the associations between PTSD and alcohol- and substance-related problems by specific occupation.
Among HCWs, there is no prior literature examining the global and symptom cluster associations between PTSD and substance-related problems prior or during the pandemic with the literature from during the SARS-CoV-2 pandemic focusing on prevalence rate changes. The current results examining the associations between PTSD symptoms and alcohol- and substance-related problems among HCWs add to the relatively limited literature on prevalence rates during the pandemic (Mongeau-Pérusse et al., 2021; Turna et al., 2022; Young et al., 2021). Furthermore, the significant mediating effects of emotion dysregulation and dissociation highlight them as potential treatment targets for structured interventions for HCWs struggling with PTSD and comorbid alcohol/substance-related problems during the pandemic.
Lastly, to our knowledge, this is the first study examining the mediating roles of underlying mechanisms (i.e. dissociation and emotion dysregulation) on the relations between PTSD symptoms and alcohol/substance-related problems among HCWs and PSP. Prior literature examining the mediating role of dissociation has focused on adult treatment seeking clinical samples (Patel et al., 2022). Among a sample of individuals seeking treatment for PTSD, dissociation mediated the relation between PTSD symptoms and alcohol-related problems, consistent with current results among HCWs but not PSP. Though, important to note that the two samples between studies differ significantly as the current study was not treatment-seeking and rates of PTSD among this study were ∼28% compared to 100% among the other study, and direct comparisons should be interpreted with caution. As for emotion dysregulation, no studies to date examine emotion dysregulation as a mediator between PTSD symptoms and alcohol-related problems among HCWs or PSP during the pandemic. Pre-pandemic literature suggests emotion dysregulation significantly mediates the relation between PTSD and impulsivity (Weiss et al., 2012) among individuals using substances. Since emotion dysregulation was not a direct mediator between PTSD and SUD, drawing meaningful comparisons is difficult. A narrative review posits that emotion dysregulation may be a transdiagnostic factor underlying PTSD and alcohol/substance-related problems via a combination of low distress tolerance and inability to effectively use goal-directed emotion regulation strategies (Westphal et al., 2017) indicating that the role of emotion dysregulation should be explored further to define its utility as a clinical treatment target.
4.1. Limitations
In the present study, the results should be interpreted in the presence of a few limitations. This study used self-report assessments; while these assessments are widely used and psychometrically validated, they are not diagnostic interviews administered by a licensed clinician. Important to note, the PCL-5 has been validated and shown to be consistent with clinical diagnosis of PTSD among healthcare workers (Cheng et al., 2020) and public safety personnel (Morrison et al., 2021). Second, this study did not assess for Criterion A trauma in conjunction with the PCL-5. However, Criterion A traumas are very common in HCWs and PSP due to the nature of their occupation. In addition, it is common for the PCL-5 to be used with connection to a Criterion A traumatic event during the pandemic (di Tella et al., 2020; Song et al., 2020). Third, due to a lack of Criterion A event assessment, the PTSD symptoms cannot be competely disentangled from burnout symptoms experienced by HCWs and PSP during the pandemic. However, while PTSD and burnout may have similar symptomatology, there are distinct differences in presentation profiles for PTSD and burnout (Restauri & Sheridan, 2020; Tomaszek & Muchacka-Cymerman, 2022). Some symptoms of burnout may coincide (mood, depersonalization [with dissociative subtype PTSD]), however, these symptoms alone are not sufficient for a diagnosis of PTSD, which must also include intrusion symptoms (flashbacks, nightmares), alterations in arousal and reactivity (hypervigilance) and avoidance behaviours, all of which are not criteria for definitional burnout (Restauri & Sheridan, 2020). Further, research has shown that individuals in serving professions who screen positive for PTSD are also much more likely to screen positive for burnout as well, so they seem to be highly comorbid rather than a ‘one or the other’ scenario (Carmassi et al., 2021; Chatzea et al., 2018; Jo et al., 2018; Katsavouni et al., 2016; Li et al., 2021; Mealer et al., 2009). Fourth, data was cross-sectional during a portion of the pandemic, so comparing these results to pre-pandemic results should be done with caution. Another limitation was the use of imputation to account for missing data (∼37–40%), though important to note that imputation has been used for alcohol/substance use measures previously (51). Lastly, within the current study, only underlying mechanisms of dissociation and emotion dysregulation were analyzed concerning PTSD and alcohol/substance-related problems. Other underlying mechanisms, such as impulsivity related to PTSD and substance use should be explored.
5. Conclusion
To our knowledge, this is the first study to analyze the associations between PTSD symptoms and alcohol-/substance-related problems during the SARS-CoV-2 pandemic among HCWs and builds upon the limited literature for PSP. For alcohol-related problems, we found dissociation significantly mediated the relation among HCWs, whereas emotion dysregulation significantly mediated the relation among PSP. For substance-related problems, emotion dysregulation significantly mediated the relation among HCWs; no significant mediation was observed for PSP. Uncovering associations between PTSD symptoms and alcohol/substance-related problems among HCWs and PSP can inform precise treatment targets for individuals of these occupations seeking treatment. Specifically, these results point towards emotion dysregulation and dissociation as potential key therapeutic targets among PSP and HCWs with co-morbid PTSD and alcohol/substance-related problems. Future directions include a longitudinal analysis of these associations following the end of the pandemic and exploring the mediating roles of other factors.
Supplementary Material
Funding Statement
This work was supported by Canadian Institutes of Health Research; The Atlas Institute for Veterans and Families; Homewood Research Institute; Western University.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- American Psychological Association . (2013). Diagnostic and statistical manual of mental disorders. In Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing, Inc. 10.1176/appi.books.9780890425596.dsm04 [DOI] [Google Scholar]
- Badger, K., Royse, D., & Craig, C. (2008). Hospital social workers and indirect trauma exposure: An exploratory study of contributing factors. Health & Social Work, 33(1), 63–71. 10.1093/hsw/33.1.63 [DOI] [PubMed] [Google Scholar]
- Berman, A. H., Bergman, H., Palmstierna, T., & Schlyter, F. (2005). Evaluation of the Drug Use Disorders Identification Test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. European Addiction Research, 11(1), 22–31. 10.1159/000081413 [DOI] [PubMed] [Google Scholar]
- Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Bonumwezi, J. L., Tramutola, D., Lawrence, J., Kobezak, H. M., & Lowe, S. R. (2022). Posttraumatic stress disorder symptoms, work-related trauma exposure, and substance use in first responders. Drug and Alcohol Dependence, 237, 109439. 10.1016/j.drugalcdep.2022.109439 [DOI] [PubMed] [Google Scholar]
- Briere, J., Weathers, F. W., & Runtz, M. (2005). Is dissociation a multidimensional construct? Data from the Multiscale Dissociation Inventory. Journal of Traumatic Stress, 18(3), 221–231. 10.1002/jts.20024 [DOI] [PubMed] [Google Scholar]
- Campion, W. M., & Rubin, D. B. (1989). Multiple imputation for nonresponse in surveys. Journal of Marketing Research, 26(4), 485. 10.2307/3172772 [DOI] [Google Scholar]
- Carleton, N. R., Afifi, T. O., Taillieu, T., Turner, S., Krakauer, R., Anderson, G. S., MacPhee, R. S., Ricciardelli, R., Cramm, H. A., Groll, D., & McCreary, D. R. (2019). Exposures to potentially traumatic events among public safety personnel in Canada. Canadian Journal of Behavioural Science / Revue canadienne des sciences du comportement, 51(1), 37–52. 10.1037/cbs0000115 [DOI] [Google Scholar]
- Carleton, N. R., Afifi, T. O., Turner, S., Taillieu, T., Duranceau, S., LeBouthillier, D. M., Sareen, J., Ricciardelli, R., MacPhee, R. S., Groll, D., Hozempa, K., Brunet, A., Weekes, J. R., Griffiths, C. T., Abrams, K. J., Jones, N. A., Beshai, S., Cramm, H. A., Dobson, K. S., … Asmundson, G. J. G. (2018a). Mental disorder symptoms among public safety personnel in Canada. The Canadian Journal of Psychiatry, 63(1), 54–64. 10.1177/0706743717723825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carleton, N. R., Afifi, T. O., Turner, S., Taillieu, T., Duranceau, S., LeBouthillier, D. M., Sareen, J., Ricciardelli, R., MacPhee, R. S., Groll, D., Hozempa, K., Brunet, A., Weekes, J. R., Griffiths, C. T., Abrams, K. J., Jones, N. A., Beshai, S., Cramm, H. A., Dobson, K. S., … Asmundson, G. J. G. (2018b). Mental disorder symptoms among public safety personnel in Canada. The Canadian Journal of Psychiatry, 63(1), 54–64. 10.1177/0706743717723825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carleton, N. R., Afifi, T. O., Turner, S., Taillieu, T., LeBouthillier, D. M., Duranceau, S., Sareen, J., Ricciardelli, R., MacPhee, R. S., Groll, D., Hozempa, K., Brunet, A., Weekes, J. R., Griffiths, C. T., Abrams, K. J., Jones, N. A., Beshai, S., Cramm, H. A., Dobson, K. S., … Asmundson, G. J. G. (2018c). Suicidal ideation, plans, and attempts among public safety personnel in Canada. Canadian Psychology / Psychologie Canadienne, 59(3), 220–231. 10.1037/cap0000136 [DOI] [Google Scholar]
- Carmassi, C., Foghi, C., Dell’Oste, V., Cordone, A., Bertelloni, C. A., Bui, E., & Dell’Osso, L. (2020). PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: What can we expect after the COVID-19 pandemic. Psychiatry Research, 292, 113312. 10.1016/j.psychres.2020.113312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi, C., Malacarne, P., Dell’Oste, V., Bertelloni, C. A., Cordone, A., Foghi, C., & Dell’Osso, L. (2021). Post-traumatic stress disorder, burnout and their impact on global functioning in Italian emergency healthcare workers. Minerva Anestesiologica, 87(5), 556–566. 10.23736/S0375-9393.20.14853-3 [DOI] [PubMed] [Google Scholar]
- Chatzea, V. E., Sifaki-Pistolla, D., Vlachaki, S. A., Melidoniotis, E., & Pistolla, G. (2018). PTSD, burnout and well-being among rescue workers: Seeking to understand the impact of the European refugee crisis on rescuers. Psychiatry Research, 262, 446–451. 10.1016/j.psychres.2017.09.022 [DOI] [PubMed] [Google Scholar]
- Cheng, P., Xu, L. Z., Zheng, W. H., Ng, R. M. K., Zhang, L., Li, L. J., & Li, W. H. (2020). Psychometric property study of the posttraumatic stress disorder checklist for DSM-5 (PCL-5) in Chinese healthcare workers during the outbreak of corona virus disease 2019. Journal of Affective Disorders, 277, 368–374. 10.1016/j.jad.2020.08.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilcoat, H., & Menard, C. (2004). Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders. In Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders. American Psychological Association. 10.1037/10460-000 [DOI] [Google Scholar]
- Chopko, B. A., Palmieri, P. A., & Adams, R. E. (2013). Associations between police stress and alcohol use: implications for practice. Journal of Loss and Trauma, 18(5), 482–497. 10.1080/15325024.2012.719340 [DOI] [Google Scholar]
- Collins, S., & Long, A. (2003). Working with the psychological effects of trauma: Consequences for mental health-care workers - A literature review. Journal of Psychiatric and Mental Health Nursing, 10(4), 417–424. 10.1046/j.1365-2850.2003.00620.x [DOI] [PubMed] [Google Scholar]
- Curran, P. J., West, S. G., & Finch, J. F. (1996). The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods, 1(1), 16–29. 10.1037/1082-989X.1.1.16 [DOI] [Google Scholar]
- D’ettorre, G., Pellicani, V., & Ceccarelli, G. (2020). Post-traumatic stress disorder symptoms in healthcare workers: A ten-year systematic review. Acta Biomedica, 91(12-S), 1–10. 10.23750/abm.v91i12-S.9459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- di Tella, M., Romeo, A., Benfante, A., & Castelli, L. (2020). Mental health of healthcare workers during the COVID-19 pandemic in Italy. Journal of Evaluation in Clinical Practice, 26(6), 1583–1587. 10.1111/jep.13444 [DOI] [PubMed] [Google Scholar]
- Enders, C. K. (2017). Multiple imputation as a flexible tool for missing data handling in clinical research. Behaviour Research and Therapy, 98, 4–18. 10.1016/j.brat.2016.11.008 [DOI] [PubMed] [Google Scholar]
- Garke, M., Isacsson, N. H., Sörman, K., Bjureberg, J., Hellner, C., Gratz, K. L., Berghoff, C. R., Sinha, R., Tull, M. T., & Jayaram-Lindström, N. (2021). Emotion dysregulation across levels of substance use. Psychiatry Research, 296, 113662. 10.1016/j.psychres.2020.113662 [DOI] [PubMed] [Google Scholar]
- Goodgame Huffman, L., Oshri, A., Thompson, J., & Mackillop, J. (2022). Latent typologies of psychiatric symptom comorbidity with substance use: Associations with adverse childhood experiences. Journal of Studies on Alcohol and Drugs, 83(2), 185–194. 10.15288/jsad.2022.83.185 [DOI] [PubMed] [Google Scholar]
- Gratz, K. L., & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Gros, D. F., Price, M., Magruder, K. M., & Frueh, B. C. (2012). Symptom overlap in posttraumatic stress disorder and major depression. Psychiatry Research, 196(2-3), 267–270. 10.1016/j.psychres.2011.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross, J. J., & Feldman Barrett, L. (2011). Emotion generation and emotion regulation: One or two depends on your point of view. Emotion Review, 3(1), 8–16. 10.1177/1754073910380974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall, H. (2020). The effect of the COVID-19 pandemic on healthcare workers’ mental health. Journal of the American Academy of Physician Assistants, 33(7), 45–48. 10.1097/01.JAA.0000669772.78848.8c [DOI] [PubMed] [Google Scholar]
- Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo, I., Lee, S., Sung, G., Kim, M., Lee, S., Park, J., & Lee, K. (2018). Relationship between burnout and PTSD symptoms in firefighters: The moderating effects of a sense of calling to firefighting. International Archives of Occupational and Environmental Health, 91(1), 117–123. 10.1007/s00420-017-1263-6 [DOI] [PubMed] [Google Scholar]
- Katsavouni, F., Bebetsos, E., Malliou, P., & Beneka, A. (2016). The relationship between burnout, PTSD symptoms and injuries in firefighters. Occupational Medicine, 66(1), 32–37. 10.1093/occmed/kqv144 [DOI] [PubMed] [Google Scholar]
- Khantzian, E. (1997). The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4(5), 231–244. 10.3109/10673229709030550 [DOI] [PubMed] [Google Scholar]
- Li, P., Kuang, H., & Tan, H. (2021). The occurrence of post-traumatic stress disorder (PTSD), job burnout and its influencing factors among ICU nurses. American Journal of Translational Research, 13(7), 8302–8308. [PMC free article] [PubMed] [Google Scholar]
- Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- Mealer, M., Burnham, E. L., Goode, C. J., Rothbaum, B., & Moss, M. (2009). The prevalence and impact of post traumatic stress disorder and burnout syndrome in nurses. Depression and Anxiety, 26(12), 1118–1126. 10.1002/da.20631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta, S., Yarnell, C., Shah, S., Dodek, P., Parsons-Leigh, J., Maunder, R., Kayitesi, J., Eta-Ndu, C., Priestap, F., LeBlanc, D., Chen, J., & Honarmand, K. (2022). The impact of the COVID-19 pandemic on intensive care unit workers: A nationwide survey. Canadian Journal of Anesthesia/Journal Canadien d'anesthésie, 69(4), 472–484. 10.1007/s12630-021-02175-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrick, M. T., Ports, K. A., Ford, D. C., Afifi, T. O., Gershoff, E. T., & Grogan-Kaylor, A. (2017). Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse & Neglect, 69, 10–19. 10.1016/j.chiabu.2017.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mongeau-Pérusse, V., Rizkallah, E., Bruneau, J., Chênevert, D., Menvielle, L., & Jutras-Aswad, D. (2021). Changes in alcohol habits among workers during the confinement of COVID-19: Results of a Canadian cross-sectional survey. Substance Abuse: Research and Treatment, 15. 10.1177/11782218211033298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison, K., Su, S., Keck, M., & Beidel, D. C. (2021). Psychometric properties of the PCL-5 in a sample of first responders. Journal of Anxiety Disorders, 77, 102339. 10.1016/j.janxdis.2020.102339 [DOI] [PubMed] [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (2017). Mplus User’s Guide (Eight Edition). Muthén & Muthén. [Google Scholar]
- Myran, D. T., Cantor, N., Rhodes, E., Pugliese, M., Hensel, J., Taljaard, M., Talarico, R., Garg, A. X., McArthur, E., Liu, C. W., Jeyakumar, N., Simon, C., McFadden, T., Gerin-Lajoie, C., Sood, M. M., & Tanuseputro, P. (2022). Physician health care visits for mental health and substance use during the COVID-19 pandemic in Ontario, Canada. JAMA Network Open, 5(1), e2143160–e2143160. 10.1001/jamanetworkopen.2021.43160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman, S. B., Stein, M. B., & Davidson, J. R. (2007). Profiling posttraumatic functional impairment. Journal of Nervous & Mental Disease, 195(1), 48–53. 10.1097/01.nmd.0000252135.25114.02 [DOI] [PubMed] [Google Scholar]
- Patel, H., Holshausen, K., Oshri, A., Andrews, K., Penta, S., Raymond, H., McKinnon, M., Brasch, J., MacKillop, J., & Amlung, M. (2021). Posttraumatic stress disorder symptomatology and substance use in an outpatient concurrent disorders sample. The Canadian Journal of Psychiatry, 66(9), 788–797. 10.1177/07067437211011851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel, H., O’Connor, C., Andrews, K., Amlung, M., Lanius, R., & McKinnon, M. C. (2022). Dissociative symptomatology mediates the relation between posttraumatic stress disorder severity and alcohol-related problems. Alcoholism: Clinical and Experimental Research, 46(2), 289–299. 10.1111/acer.14764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pestana, D. V. S., Raglione, D., Junior, L. D., Liberatti, C. S. P., Braga, E. C., Ezequiel, V. A. L., Alves, A. S., Mauro, J. G., Dias, J. O. A., Moreira, P. T. F., Madureira, B. D. B., Paiva, L. P., de Lucena, B. M. N., Junior, J. M. S., & Malbouisson, L. M. S. (2022). Stress and substance abuse among workers during the COVID-19 pandemic in an intensive care unit: A cross-sectional study. PLoS One, 17(2), e0263892. 10.1371/journal.pone.0263892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2011). Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders, 25(3), 456–465. 10.1016/j.janxdis.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Restauri, N., & Sheridan, A. D. (2020). Burnout and posttraumatic stress disorder in the coronavirus disease 2019 (COVID-19) pandemic: Intersection, impact, and interventions. Journal of the American College of Radiology, 17(7), 921–926. 10.1016/j.jacr.2020.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles, R., Rodríguez, E., Vega-Ramírez, H., Álvarez-Icaza, D., Madrigal, E., Durand, S., Morales-Chainé, S., Astudillo, C., Real-Ramírez, J., Medina-Mora, M. E., Becerra, C., Escamilla, R., Alcocer-Castillejos, N., Ascencio, L., Díaz, D., González, H., Barrón-Velázquez, E., Fresán, A., Rodríguez-Bores, L., … Reyes-Terán, G. (2021). Mental health problems among healthcare workers involved with the COVID-19 outbreak. Brazilian Journal of Psychiatry, 43(5), 494–503. 10.1590/1516-4446-2020-1346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saragih, I. D., Tonapa, S. I., Saragih, I. S., Advani, S., Batubara, S. O., Suarilah, I., & Lin, C. J. (2021). Global prevalence of mental health problems among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. International Journal of Nursing Studies, 121, 104002. 10.1016/j.ijnurstu.2021.104002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders, J., Aasland, O., Babor, T., De La Fuente, J., & Grant, M. (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88(791), 791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Schreiber, J. B., Stage, F. K., King, J., Nora, A., & Barlow, E. A. (2006). Reporting structural equation modeling and confirmatory factor analysis results: A review. The Journal of Educational Research, 99(6), 323–338. 10.3200/JOER.99.6.323-338 [DOI] [Google Scholar]
- Simons, J. S., Gaher, R. M., Jacobs, G. A., Meyer, D., & Johnson-Jimenez, E. (2005). Associations between alcohol use and PTSD symptoms among American red cross disaster relief workers responding to the 9/11/2001 attacks. The American Journal of Drug and Alcohol Abuse, 31(2), 285–304. 10.1081/ADA-47937 [DOI] [PubMed] [Google Scholar]
- Song, X., Fu, W., Liu, X., Luo, Z., Wang, R., Zhou, N., Yan, S., & Lv, C. (2020). Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain, Behavior, and Immunity, 88, 60–65. 10.1016/j.bbi.2020.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel, D. (2011). Divided consciousness: Dissociation in DSM-5. Depression and Anxiety, 29(8), 667–670. 10.1002/da.21984 [DOI] [PubMed] [Google Scholar]
- Tomaszek, K., & Muchacka-Cymerman, A. (2022). Student burnout and PTSD symptoms: The role of existential anxiety and academic fears on students during the COVID-19 pandemic. Depression Research and Treatment, 2022, 1–9. 10.1155/2022/6979310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turna, J., Patterson, B., Goldman Bergmann, C., Lamberti, N., Rahat, M., Dwyer, H., Francisco, A. P., Vismara, M., Dell’Osso, B., Sideris, B., & Van Ameringen, M. (2022). Mental health during the first wave of COVID-19 in Canada, the USA, Brazil and Italy. International Journal of Psychiatry in Clinical Practice, 26(2), 148–156. 10.1080/13651501.2021.1956544 [DOI] [PubMed] [Google Scholar]
- Weiss, N. H., Tull, M. T., Lavender, J., & Gratz, K. L. (2013). Role of emotion dysregulation in the relationship between childhood abuse and probable PTSD in a sample of substance abusers. Child Abuse & Neglect, 37(11), 944–954. 10.1016/j.chiabu.2013.03.014 [DOI] [PubMed] [Google Scholar]
- Weiss, N. H., Tull, M. T., Viana, A. G., Anestis, M. D., & Gratz, K. L. (2012). Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders, 26(3), 453–458. 10.1016/j.janxdis.2012.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westphal, M., Aldao, A., & Jackson, C. (2017). Emotion dysregulation in comorbid posttraumatic stress disorder and substance use disorders: A narrative review. Military Psychology, 29(3), 216–233. 10.1037/mil0000157 [DOI] [Google Scholar]
- Westphal, M., Olfson, M., Gameroff, M. J., Wickramaratne, P., Pilowsky, D. J., Neugebauer, R., Lantigua, R., Shea, S., & Neria, Y. (2011). Functional impairment in adults with past posttraumatic stress disorder: Findings from primary care. Depression and Anxiety, 28(8), 686–695. 10.1002/da.20842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf, E. J., Miller, M. W., Reardon, A. F., Ryabchenko, K. A., Castillo, D., & Freund, R. (2012). A latent class analysis of dissociation and posttraumatic stress disorder: Evidence for a dissociative subtype. Archives of General Psychiatry, 69(7), 698–705. 10.1001/archgenpsychiatry.2011.1574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young, K. P., Kolcz, D. L., O’Sullivan, D. M., Ferrand, J., Fried, J., & Robinson, K. (2021). Health care workers’ mental health and quality of life during COVID-19: Results from a mid-pandemic, national survey. Psychiatric Services, 72(2), 122–128. 10.1176/appi.ps.202000424 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.