Supplemental Digital Content is Available in the Text.
Recombinant zoster vaccine is efficacious in reducing herpes zoster incidence in at-risk populations and seems to decrease pain duration and need for pain medication in breakthrough herpes zoster cases.
Keywords: Herpes zoster, Pain medication, Efficacy, Adjuvanted recombinant zoster vaccine, Immunosenescence, Immunocompromised
Abstract
Herpes zoster (HZ) and HZ-associated pain greatly affect patients' quality of life, particularly in older and immunocompromised adults, for whom comorbidities and polypharmacy are often reported. Three phase III, randomized, placebo-controlled clinical trials have reported the adjuvanted recombinant zoster vaccine (RZV) as highly efficacious in preventing HZ and reducing pain severity in healthy adults ≥50 years old (Zoster Efficacy Study [ZOE]-50 study, NCT01165177) and ≥70 years old (ZOE-70; NCT01165229) and in immunocompromised adults ≥18 years old undergoing autologous hematopoietic stem cell transplantation (ZOE-HSCT; NCT01610414). Here, we investigated efficacy of RZV in reducing (i) the duration of clinically significant pain (Zoster Brief Pain Inventory pain score ≥3) and (ii) HZ-associated pain medication use and duration of use in participants with confirmed HZ (“breakthrough cases”) from the 3 studies. Recombinant zoster vaccine effectively reduced the duration of clinically significant HZ-associated pain during HZ episodes by 38.5% (P-value: 0.010) in the ZOE-HSCT study. Although a similar trend was observed in the ZOE-50 and ZOE-70 studies, the results were not statistically significant because of the high vaccine efficacy (VE) against HZ resulting in rare breakthrough cases. VE in reducing pain medication use (39.6%; P-value: 0.008) and duration of medication use (49.3%, P-value: 0.040) was reported in the ZOE-70 study; corresponding positive VE estimates were observed in the ZOE-50 and ZOE-HSCT studies but were not statistically significant. Data reported here demonstrate efficacy of RZV in reducing HZ-associated pain duration and pain medication use in breakthrough cases, thereby improving quality of life of those with HZ.
1. Introduction
Herpes zoster (HZ), also known as shingles, is caused by reactivation of the varicella–zoster virus (VZV) and is characterized by a painful dermatomal rash. The pain can be acute or can evolve into postherpetic neuralgia (PHN), a neuropathic pain that usually persists for several months after the rash has resolved.3,12 Other serious complications of HZ include a disseminated rash, encephalitis, HZ ophthalmicus, secondary bacterial infection, and neurological, visceral, and vascular diseases.3,22
Herpes zoster and HZ-associated pain can greatly diminish the patients' quality of life (QoL), interfere with activities of daily living (ADLs), and have a negative impact on the patients' social life and mental health status.23
Older or immunocompromised (IC) adults are at increased risk for developing HZ and HZ-associated complications because of the decrease of VZV-specific T-cell immunity.13,14,16,19,30 Moreover, both in older adults and in IC individuals, HZ rash severity and duration of HZ episodes tend to be increased and disease recurrence is higher.6,10,35
The adjuvanted recombinant zoster vaccine (RZV; Shingrix, GSK) was designed to prevent HZ and HZ-associated complications, including PHN. Recombinant zoster vaccine is a 2-dose subunit vaccine containing recombinant VZV glycoprotein E and the AS01B adjuvant system. Recombinant zoster vaccine is currently approved for administration to adults of all ages who are at increased risk for HZ in the European Union and several other countries worldwide, including Canada, Japan, Australia, and the United States.9,17,20,27,29
Recombinant zoster vaccine was highly efficacious in preventing HZ in older adults in 2 pivotal phase III clinical trials, with an overall vaccine efficacy (VE) of 97.2% in the Zoster Efficacy Study (ZOE)-50 study in adults ≥50 years old (NCT01165177), and an overall VE of 89.8% in the ZOE-70 study involving adults ≥70 years old (NCT01165229).5,25 Based on the pooled data of ZOE-50 and ZOE-70 trials, RZV efficacy in preventing PHN was 91.2% in ≥50 years old and 88.8% in ≥70 years old.5 The efficacy of RZV in preventing HZ in adults ≥18 years old undergoing autologous hematopoietic stem cell transplantation (HSCT) was demonstrated in a separate phase III trial (ZOE-HSCT study; NCT01610414; VE: 68.2%).1 Efficacy was further confirmed in a post hoc analysis of IC patients ≥18 years old presenting hematological malignancies (VE: 87.2%).8
The results from the above studies suggest that RZV can reduce severe HZ-associated pain. Moreover, vaccination tends to shorten duration of clinically significant pain, reduce interference with ADLs, and improve the QoL scores in adults ≥50 years old and HSCT recipients ≥18 years old.6,7
The aim of the current analysis was to determine the efficacy of RZV in reducing the duration of clinically significant HZ-associated pain and assess RZV impact on the use of pain medication in participants with breakthrough disease based on data from the ZOE-50, ZOE-70, and ZOE-HSCT efficacy trials. The populations at risk for HZ in these trials are more likely to have comorbidities and use associated medication. This analysis assessed whether RZV administration to these groups may reduce drug use during HZ breakthrough, a particularly relevant topic in light of the current excess opioid use observed in several countries.15,23,36
2. Methods
The study design, efficacy, and safety results of the ZOE-50, ZOE-70, and ZOE-HSCT studies have been described in detail previously.1,5,25 Study characteristics and inclusion/exclusion criteria of ZOE-50, ZOE-70, and ZOE-HSCT trials are summarized in Supplementary Table S1 and Supplementary Material S2, respectively (available at http://links.lww.com/PAIN/B694). All 3 trials were randomized, observer-blinded, placebo-controlled, phase III studies and were conducted in accordance with the Good Clinical Practice guidelines and the Declaration of Helsinki. All study procedures were approved by the independent ethics committee or institutional review boards at each study site and/or national research committee. All individual participants provided written informed consent before enrollment.
2.1. Outcome measures
In each study, participants with suspected HZ were asked to complete the Zoster Brief Pain Inventory (ZBPI) daily for 28 days after rash onset and then weekly until either the participant had been pain-free for 4 consecutive weeks or 90 days had elapsed since rash onset (whichever happened later); day 0 was defined as the first day of HZ rash.4 The ZBPI questionnaire was previously validated4 and has been extensively used in zoster studies, yielding robust and meaningful results.
When completing the ZBPI questionnaire, each participant was asked to rate 4 categories of pain [(1) least in the past 24 hours, (2) worst in the past 24 hours, (3) average in the past 24 hours, and (4) right now] on 11-point Likert-type scales (0-10, with 10 signifying the worst imaginable pain). Of these, the worst pain over the past 24 hours category was considered the most reliable indicator of pain.4 For the present analysis, a score rated as 3 or greater on the worst pain in the past 24 hours ZBPI question at any time during the first confirmed HZ episode was considered as clinically significant pain. This score was used to calculate the VE in reducing the duration of HZ-associated pain.
The use of medication against HZ-associated pain during each episode was recorded and used to calculate the VE in reducing the use and duration of HZ-associated pain medication.
In addition, a manual classification of HZ-associated medications used during each episode was performed, based on the World Health Organization's pain relief ladder. The main classes of prescribed drugs were nonopioids (eg, nonsteroidal anti-inflammatory drugs and paracetamol [acetaminophen]), weak opioids (eg, codeine), and strong opioids (eg, morphine and oxycodone).34 All other medications administered to treat an HZ episode, other than the “nonopioids” and “opioids,” were classified into anesthetics, antihistamines, gastro-intestinal medications, antibiotics, and muscle relaxants.
Only HZ cases confirmed by polymerase chain reaction or by the adjudication committee (for equivocal polymerase chain reaction results or unavailable samples) were included in the analyses.5,25
2.2. Statistical analyses
The modified total vaccinated cohort (mTVC) was the primary cohort used for VE evaluations in the studies. The mTVC excluded participants who did not receive the second vaccine dose, for whom the vaccine was not correctly administered or who developed a confirmed case of HZ before 30 days after the second vaccination. Follow-up periods were censored at the first occurrence of a confirmed HZ episode and, for participants of the ZOE-HSCT study, also after relapse of the pre-existing malignant disease. A ZBPI worst pain score of 0 was assumed for participants for whom no ZBPI questionnaires were available.
The assessments of the duration of clinically significant HZ-associated pain and the use and duration of HZ-associated pain medication by participants with a confirmed episode of HZ were secondary objectives of the ZOE-50 and ZOE-70 studies. In the ZOE-HSCT study, duration of clinically significant HZ-associated pain was the secondary objective, while the use and duration of HZ-associated pain medication were tertiary objectives. The use of HZ-associated medication by the type of medication in participants with a confirmed episode of HZ was assessed as post hoc analyses of the ZOE-50, ZOE-70, and ZOE-HSCT studies.
The VE of RZV in reducing the duration of clinically significant pain and the duration of pain medication use for each confirmed case of HZ was assessed by calculating the hazard rate reduction in duration of clinically significant pain and duration of pain medication use (using the Cox-proportional model). The time-to-cessation of clinically significant pain was analyzed using a survival methodology. Confirmed HZ cases without clinically significant pain were considered as nonevent cases with a duration of clinically significant pain (T) of 1. Cases with clinically significant pain were considered as event cases, and their time-to-event was calculated as being the inverse of duration of pain (1/t). These transformations enabled computing of VE in terms of severe worst pain-free period. Duration of clinically significant pain was defined as the last day with clinically significant pain minus the first day with clinically significant pain plus 1. Duration of pain medication use was defined as the sum of nonoverlapping period duration for each pain medication (the last day of each pain medication minus the first day of each pain medication plus 1).
The VE of RZV in reducing the use of pain medication for confirmed cases of HZ was assessed using an asymptotic standardized unconditional binomial test.26 The numbers of HZ-associated pain medications used and the duration of their use were also computed as means (ranges), whereby means were calculated as the arithmetic means and ranges as the differences between the maximum and the minimum values for a given participant group.
3. Results
3.1. Study participants
The ZOE-50, ZOE-70, and ZOE-HSCT studies enrolled 15,411, 13,900, and 1846 participants, most of whom (93.2%-95.8%) were assigned to the mTVC (Supplementary Table S1, available at http://links.lww.com/PAIN/B694). The demographic characteristics of participants with confirmed HZ cases included in the mTVC were described previously for the ZOE-50 study,7 the ZOE-70 study,18 and the ZOE-HSCT study6 and are summarized in Supplementary Table S1, available at http://links.lww.com/PAIN/B694. The number of confirmed HZ cases among participants in the mTVC who received RZV or placebo in each of these studies is presented in Table 1. There were 9 breakthrough cases in the RZV group vs 254 HZ cases in the placebo group in the ZOE-50 study, 23 vs 223 in the ZOE-70 study, and 49 vs 135 in the ZOE-HSCT study.
Table 1.
Reduction in the duration of clinically significant herpes zoster-associated pain in participants with confirmed herpes zoster.
| Study | RZV | Placebo | VE (%) | 95% CI | P | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | n | T (d) | N | n | T (d) | ||||
| ZOE-50 | 9 | 7 | 146 | 254 | 221 | 6705 | 26.9 | (−59.6, 66.5) | 0.432 |
| ZOE-70 | 23 | 18 | 628 | 223 | 198 | 9633 | 28.4 | (−17.7, 56.4) | 0.188 |
| ZOE-HSCT* | 49 | 37 | 892 | 135 | 120 | 6275 | 38.5 | (11.1, 57.5) | 0.010 |
The associated hazard ratio for reduction of the duration of clinically significant HZ-associated pain in the ZOE-HSCT study has been published previously.1
This analysis excluded pain linked to a confirmed HZ case after relapse of the pre-existing malignant disease.
CI, confidence interval; HSCT, hematopoietic stem cell transplantation; HZ, herpes zoster; n, number of participants with at least 1 confirmed HZ episode and at least 1 d of clinically significant HZ-associated pain; N, number of participants with at least 1 confirmed HZ episode; RZV, recombinant zoster vaccine; T, sum of follow-up period (for participants without clinically significant pain, T is 1; for participants with clinically significant pain, T is the duration of clinically significant pain) expressed in d; VE, vaccine efficacy (adjusted by age strata and regions in the ZOE-50 and ZOE-70 studies); ZOE, Zoster Efficacy Study.
3.2. Duration of clinically significant herpes zoster-associated pain
The estimated overall VE in reducing duration of clinically significant HZ-associated pain (ZBPI score ≥3 for worst pain) in participants with a confirmed HZ episode was 26.9% in the ZOE-50 and 28.4% in the ZOE-70 study (Table 1). In the ZOE-HSCT study, the VE in reducing the duration of clinically significant HZ-associated pain was 38.5% (P-value: 0.010).
The median (mean) duration of clinically significant HZ-associated pain in participants with at least 1 confirmed HZ episode was 11.0 (20.6) days in the RZV group and 15.0 (30.2) days in the placebo group in the ZOE-50 study, 13.5 (34.6) days in the RZV group and 19.0 (48.5) days in the placebo group in the ZOE-70 study, and 14.0 (23.8) days in the RZV group and 24.0 (52.2) days in the placebo group in the ZOE-HSCT study (Table 2). Pain lasted on average between 9.6 (ZOE-50) and 28.4 (ZOE-HSCT) days less in the RZV than the placebo group, but these differences in pain duration were not statistically significant (Table 2, “Placebo-RZV” column). The analysis of pooled data from all 3 studies (ZOE-50, ZOE-70, and ZOE-HSCT), while limited by small sample sizes and heterogeneity of included study groups, consistently showed the trend to an overall shorter duration of pain in the RZV vs placebo group (Table 2).
Table 2.
Mean and median duration of clinically significant herpes zoster-associated pain and difference between the recombinant zoster vaccine and placebo groups.
| Study | RZV | Placebo | Placebo-RZV* | |||||
|---|---|---|---|---|---|---|---|---|
| N | Duration (d) | N | Duration (d) | Difference (d) | P | |||
| Mean (SD) | Median (min, max) | Mean (SD) | Median (min, max) | Mean (SD) | ||||
| ZOE-50 | 7 | 20.6 (26.8) | 11.0 (3.0, 78.0) | 221 | 30.2 (52.0) | 15.0 (1.0, 464.0) | 9.6 | 0.6267 |
| ZOE-70 | 18 | 34.6 (45.5) | 13.5 (1.0, 162.0) | 198 | 48.5 (101.4) | 19.0 (1.0, 834.0) | 13.9 | 0.5653 |
| ZOE-HSCT† | 37 | 23.8 (31.9) | 14.0 (1.0, 178.0) | 120 | 52.2 (127.8) | 24.0 (1.0, 1025.0) | 28.4 | 0.1835 |
| Total (pooled)‡ | 62 | 26.6 (35.7) | 12.5 (1.0, 178.0) | 539 | 41.8 (92.6) | 17.0 (1.0, 1025.0) | 15.2 | 0.1992 |
This column describes calculated difference between the RZV and placebo group.
This analysis excluded pain linked to a confirmed HZ case after relapse of the pre-existing malignant disease.
These results refer to the pooled data of ZOE-50, ZOE-70, and ZOE-HSCT studies, where P values were calculated using the Student two-sample t test.
HSCT, hematopoietic stem cell transplantation; HZ, herpes zoster; max, maximum; min, minimum; N, number of participants with at least 1 confirmed HZ episode with clinically significant HZ-associated pain; RZV, recombinant zoster vaccine; ZOE, Zoster Efficacy Study.
3.3. Pain medication use
In the ZOE-50 study, the use of HZ-associated pain medication was reported for 66.7% of participants in the RZV group and 74.8% of participants in the placebo group during a confirmed HZ episode (Table 3). The overall VE in reducing HZ-associated pain medication use in participants with a confirmed HZ episode was 11.7%. In the ZOE-70 study, 43.5% of participants in the RZV group and 71.8% of participants in the placebo group with a confirmed HZ episode took at least 1 HZ-associated pain medication. The VE for pain medication use was 39.6% (P-value: 0.008). In the ZOE-HSCT study, in participants with a confirmed HZ episode, 65.3% in the RZV group and 69.6% in the placebo group used HZ-associated pain medication. The corresponding VE was 6.2%.
Table 3.
Reduction in the use of herpes zoster-associated pain medication in participants with confirmed herpes zoster.
| Study | RZV | Placebo | VE (%) | 95% CI | P | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | nmed | nmed (mean [range]) | Pain med use (%) | 95% CI | N | n | nmed | nmed (mean [range]) | Pain med use (%) | 95% CI | ||||
| ZOE-50 | 9 | 6 | 13 | 2.2 (3) | 66.7 | (29.9, 92.5) | 254 | 190 | 529 | 2.8 (17) | 74.8 | (69.0, 80.0) | 11.7 | (−19.4, 53.6) | 0.697 |
| ZOE-70 | 23 | 10 | 31 | 3.1 (9) | 43.5 | (23.2, 65.5) | 223 | 160 | 631 | 3.9 (26) | 71.8 | (65.4, 77.6) | 39.6 | (10.8, 64.8) | 0.008 |
| ZOE-HSCT* | 49 | 32 | 65 | 2.0 (9) | 65.3 | (50.4, 78.3) | 135 | 94 | 262 | 2.8 (20) | 69.6 | (61.1, 77.2) | 6.2 | (−15.8, 27.8) | 0.594 |
A ZBPI worst pain score of 0 was assumed for participants who did not complete any ZBPI questionnaires. The number of participants without questionnaires was 1/263 participants in ZOE-50, 2/246 for ZOE-70, and 5/184 for ZOE-HSCT.
This analysis excluded pain medication linked to a confirmed HZ case after relapse of the pre-existing malignant disease.
CI, confidence interval; HSCT, hematopoietic stem cell transplantation; HZ, herpes zoster; med, medication; n, number of participants with at least 1 confirmed HZ episode and at least 1 pain medication (all confirmed HZ episodes considered); N, number of participants with at least 1 confirmed HZ episode; nmed, number of HZ-associated pain medications (all confirmed HZ episodes considered); nmed (mean [range]), mean number and range (minimum subtracted from maximum value for a given participant group) of HZ-associated pain medications per participant; RZV, recombinant zoster vaccine; VE, vaccine efficacy (adjusted by age strata in the ZOE-50 and ZOE-70 studies); ZBPI, Zoster Brief Pain Inventory; ZOE, Zoster Efficacy Study.
3.4. Pain medication duration
The overall VE for reduction in the duration of HZ-associated pain medication was 24.7% (P-value: 0.506) in the ZOE-50 study (Table 4). In the ZOE-70 study, the corresponding VE was 49.3% (P-value: 0.040). In the ZOE-HSCT study, the overall VE in reducing the duration of HZ-associated pain medication was 22.5% (P-value: 0.214).
Table 4.
Reduction in the duration of herpes zoster-associated pain medication use in participants with confirmed herpes zoster.
| Study | RZV | Placebo | VE (%) | 95% CI | P | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | T (d) | Tmean (range) | N | n | T (d) | Tmean (range) | ||||
| ZOE-50 | 9 | 6 | 159 | 26.0 (55) | 254 | 190 | 14,524 | 76.1 (1265) | 24.7 | (−73.7, 67.4) | 0.506 |
| ZOE-70 | 23 | 10 | 1108 | 109.5 (654) | 223 | 160 | 31,949 | 199.3 (4528) | 49.3 | (2.9, 73.5) | 0.040 |
| ZOE-HSCT* | 49 | 32 | 1917 | 59.4 (435) | 135 | 94 | 15,465 | 164.1 (1641) | 22.5 | (−15.9, 48.1) | 0.214 |
This analysis excluded pain medication linked to a confirmed HZ case after relapse of the pre-existing malignant disease.
CI, confidence interval; HSCT, hematopoietic stem cell transplantation; HZ, herpes zoster; N, number of participants with at least 1 confirmed HZ episode; n, number of participants with at least 1 confirmed HZ episode and at least 1 d of HZ-associated pain medication use; RZV, recombinant zoster vaccine; T, sum of follow-up period (for participants without pain medication, T is 1; for participants with pain medication, T is the duration of pain medication) expressed in d; Tmean (range), mean and range (minimum subtracted from maximum value for a given participant group) of the duration (in d) of HZ-associated pain medication use; VE, vaccine efficacy (adjusted by age strata and region in the ZOE-50 and ZOE-70 studies); ZOE, Zoster Efficacy Study.
3.5. Herpes zoster-associated medication by type
In each of the studies, adults with a confirmed HZ episode used different classes of HZ-associated medication (Table 5). The most frequently used type of medication in the ZOE-50, ZOE-70, and ZOE-HSCT studies were nonopioids, which were used by 61.2%, 44.3%, and 45.7% of respective participants. Weak opioids were used by 18.6%, 13.0%, and 21.7% of participants, respectively, and strong opioids by 8.0%, 2.0%, and 9.2% of participants.
Table 5.
Herpes zoster-associated medication types in participants with confirmed herpes zoster.
| Medication class | ZOE-50 | ZOE-70 | ZOE-HSCT* | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RZV | Placebo | Total | RZV | Placebo | Total | RZV | Placebo | Total | ||||||||||
| (N = 9) | (N = 254) | (N = 263) | (N = 23) | (N = 223) | (N = 246) | (N = 49) | (N = 135) | (N = 184) | ||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Nonopioids† | 6 | 66.7 | 155 | 61.0 | 161 | 61.2 | 6 | 26.1 | 103 | 46.2 | 109 | 44.3 | 22 | 44.9 | 62 | 45.9 | 84 | 45.7 |
| Weak opioids† | 0 | 0 | 49 | 19.3 | 49 | 18.6 | 2 | 8.7 | 30 | 13.5 | 32 | 13.0 | 6 | 12.2 | 34 | 25.2 | 40 | 21.7 |
| Strong opioids† | 0 | 0 | 21 | 8.3 | 21 | 8.0 | 0 | 0 | 5 | 2.2 | 5 | 2.0 | 5 | 10.2 | 12 | 8.9 | 17 | 9.2 |
| Corticosteroids | 3 | 33.3 | 21 | 8.3 | 24 | 9.1 | 1 | 4.3 | 10 | 4.5 | 11 | 4.5 | 2 | 4.1 | 14 | 10.4 | 16 | 8.7 |
| Antidepressants | 0 | 0 | 17 | 6.7 | 17 | 6.5 | 1 | 4.3 | 18 | 8.1 | 19 | 7.7 | 3 | 6.1 | 13 | 9.6 | 16 | 8.7 |
| Psychiatric medications | 0 | 0 | 29 | 11.4 | 29 | 11.0 | 2 | 8.7 | 25 | 11.2 | 27 | 11.0 | 3 | 6.1 | 29 | 21.5 | 32 | 17.4 |
| Gabapentinoids | 0 | 0 | 32 | 12.6 | 32 | 12.2 | 1 | 4.3 | 17 | 7.6 | 18 | 7.3 | 5 | 10.2 | 16 | 11.9 | 21 | 11.4 |
| Anesthetics | 0 | 0 | 15 | 5.9 | 15 | 5.7 | 0 | 0 | 11 | 4.9 | 11 | 4.5 | 0 | 0 | 7 | 5.2 | 7 | 3.8 |
| Antihistamines | 0 | 0 | 10 | 3.9 | 10 | 3.8 | 1 | 4.3 | 9 | 4.0 | 10 | 4.1 | 1 | 2.0 | 11 | 8.1 | 12 | 6.5 |
| GI medications | 1 | 11.1 | 24 | 9.4 | 25 | 9.5 | 0 | 0 | 6 | 2.7 | 6 | 2.4 | 2 | 4.1 | 2 | 1.5 | 4 | 2.2 |
| Antibiotics | 1 | 11.1 | 37 | 14.6 | 38 | 14.4 | 2 | 8.7 | 32 | 14.3 | 34 | 13.8 | 5 | 10.2 | 14 | 10.4 | 19 | 10.3 |
| Muscle relaxants | 0 | 0 | 1 | 0.4 | 1 | 0.4 | 0 | 0 | 2 | 0.9 | 2 | 0.8 | 0 | 0 | 0 | 0 | 0 | 0 |
| Other medications | 3 | 33.3 | 54 | 21.3 | 57 | 21.7 | 3 | 13.0 | 42 | 18.8 | 45 | 18.3 | 6 | 12.2 | 19 | 14.1 | 25 | 13.6 |
This analysis excluded medication linked to a confirmed HZ case after relapse of the pre-existing malignant disease.
Based on the World Health Organization's pain relief ladder.34
GI, gastro-intestinal; HSCT, hematopoietic stem cell transplantation; HZ, herpes zoster; N, number of participants with at least 1 confirmed HZ episode; n and %, number and percentage of participants with at least 1 confirmed HZ episode taking at least 1 HZ-associated medication of a given type; RZV, recombinant zoster vaccine; ZOE, Zoster Efficacy Study.
4. Discussion
Previous publications of the ZOE-50, ZOE-70, and ZOE-HSCT studies primarily focused on estimating the VE of RZV in preventing HZ, while the present analysis aimed to assess the impact of RZV on the duration of clinically significant pain and on use and duration of pain medication in participants with confirmed breakthrough cases of HZ from these trials. In breakthrough cases in HSCT recipients ≥18 years old, RZV significantly reduced the duration of clinically significant HZ-associated pain. In the ZOE-50 and ZOE-70 studies in older adults, there were corresponding, statistically nonsignificant trends. VE in reducing pain medication use and duration of pain medication use was demonstrated in participants with a confirmed HZ episode in the RZV group compared with the placebo group in the ZOE-70 study. In the ZOE-50 and ZOE-HSCT studies, the corresponding VE estimates were positive, but 95% confidence interval (CI) spanned zero. Although caution must be exerted because the present analysis was not statistically powered, these results suggest that RZV can decrease duration of pain and reduce pain medication use and duration of use in the small proportion of participants with breakthrough cases. The limited numbers of breakthrough cases attest to the previously reported efficacy of RZV in preventing HZ.1,5,25 Although PHN was defined as a categorical variable in the ZOE-70 study, the present analysis approached HZ-associated pain duration as a continuous variable. Previously, the ZOE-70 study reported no evidence for additional efficacy against PHN among RZV recipients with breakthrough HZ.5 However, the present results point to a trend for reduced duration of pain in participants ≥70 years old. These results are complementary. They suggest that RZV may both reduce the incidence of PHN by reducing the risk of HZ and can contribute to decreasing the intensity of all types of pain (acute and PHN) during HZ breakthrough.
These results are consistent with the high efficacy of RZV in reducing burden of illness and interference with ADLs reported in all RZV recipients from the ZOE-50 study and the pooled analysis in participants ≥70 years old from the ZOE-50/ZOE-70 studies.7 In these trials, RZV significantly reduced the burden of illness (VE of 98.4% in the ZOE-50 study and 92.1% in the pooled analysis of participants ≥70 years old) and interference with ADL compared with placebo (VE of 99.1% in the ZOE-50 study and 90.3% in the pooled analysis), mostly because of its high VE in preventing HZ.7 The ZOE-HSCT study also reported significant reductions (exceeding 80%) in burden of illness and interference with ADL in confirmed HZ cases of the RZV group vs placebo because of high VE in prevention of HZ as well as attenuation of disease.6
Previously published results from the ZOE-50 and pooled ZOE-50/ZOE-70 studies also demonstrated a tendency for shorter time to resolution of clinically significant pain (ZBPI score ≥3) in RZV-vaccinated participants with a confirmed (breakthrough) HZ episode vs the placebo group,7 supporting the current analysis. Whereas the previous results compared groups for statistical differences by a log-rank test,7 the methodology used here differs in that it calculates VE in reducing duration of clinically significant pain. VE in reducing pain was reported in previous post hoc results from the ZOE-50 and pooled ZOE-50/ZOE-70 studies7; however, the pain metric described was for severe ZBPI pain (defined as ZBPI worst pain score ≥7), thus different from the clinically significant pain metric (ZBPI score ≥3) used in this analysis. Despite the different pain metric used, the previous results are consistent with the results presented here. Different approaches were also used to calculate the number of participants reporting clinically significant pain in this analysis and in previous publications from the ZOE-50, ZOE-70, and ZOE-HSCT studies, namely that participants with a first record of pain were assumed to have pain from the time of rash onset in previous publications, while in the present analysis, pain was only assumed to start on the first day it was reported.1,5,25
The current results are also supported by the ZOE-HSCT results showing a shorter median time to resolution of clinically significant pain in the RZV group than in the placebo group (P-value: 0.048) and significant reductions in mean ZBPI worst pain scores at all times in confirmed HZ cases of the RZV group vs placebo.6 Thus, in addition to preventing a large number of HZ cases, RZV provides incremental benefits in vaccinated participants compared with placebo for shorter duration of clinically significant pain and decreased use and duration of pain medication use associated with breakthrough HZ infection. These results also align with previously published data of the ZOE-50, ZOE-70, and ZOE-HSCT studies regarding the potential of RZV to reduce the risk of PHN5 and other HZ-associated complications in breakthrough cases compared with placebo in older adults and IC patients,1,24 which, in turn, is likely to decrease the need for medication.
Similar pain attenuating effects have previously been reported for other vaccines. In a randomized, placebo-controlled trial in 2005 which enrolled over 38,000 participants (approximately 18,000 of whom were ≥70 years old), a live attenuated zoster vaccine prevented HZ with 51.3% and PHN with 66.5% efficacy.28 The severity of confirmed HZ cases was lower in vaccine than placebo recipients for all analyzed parameters, including the shorter median duration of pain and discomfort (21 days in vaccine vs 24 days in placebo recipients; P-value: 0.03).28 A prospective cohort study reported reduced pain duration and severity after administration of the live attenuated zoster vaccine in participants ≥60 years old.2 Another study by Winston et al.33 in autologous HSCT patients found that a heat-inactivated varicella–zoster vaccine significantly reduced moderate-to-severe HZ-associated pain compared with placebo.
Although antiviral treatment of HZ, if administered early after the onset of an episode, can provide certain relief, most patients will require some form of analgesia to manage HZ-associated pain. Acetaminophen and nonsteroidal anti-inflammatory drugs are commonly prescribed for treatment of mild pain; however, to date, their ability to decrease HZ-associated pain remains to be demonstrated.21 Conversely, opioids and adjuvant analgesics, such as antidepressants and anticonvulsants, were shown to be effective in reducing HZ pain.11,31 However, issues of tolerance, as well as potential misuse and abuse raise concerns regarding the use of these medications, particularly in elderly or IC patients who may present the added complexity of pre-existing comorbidity and polypharmacy.23,36 In the 3 studies presented here, nonopioid and weak opioid painkillers seem to be the most frequently used type of medication (44.3%-61.2% and 13.0%-21.7%, respectively). Although the corticosteroid prednisone was previously shown to be effective in reducing acute pain (but not PHN) when used in combination with antiviral therapy,32 this type of medication was used by only 4.5% to 9.1% of study participants having experienced a confirmed HZ episode. As suggested in the present and associated studies, eligible individuals who received RZV may also have a lower need for pain relief during HZ breakthrough, thereby mitigating risks of overmedication.
To the best of our knowledge, these are the first data investigating the impact of RZV on the use of pain medication in HZ breakthrough disease. Moreover, results presented here, together with data generated in previous studies of RZV, contribute to building a clearer picture of the ability of the vaccine to attenuate burden of disease for the rare RZV recipients experiencing breakthrough cases of HZ.
This analysis presented limitations. The assessments of RZV impact on the duration of clinically significant pain and on the use and duration of pain medication were not primary end points in the ZOE-50, ZOE-70, and ZOE-HSCT studies. Moreover, the evaluation and classification of HZ-associated medication were performed post hoc. Therefore, these studies were not statistically powered to detect any specific differences in these parameters between the RZV and placebo groups, and consequently, it is not possible to draw definitive conclusions regarding results presented here. Owing to the high VE of RZV against HZ, especially in older adults, this analysis was also limited by the low number of cases of confirmed HZ reported by RZV recipients, which prevented meaningful statistical comparison between the RZV and placebo groups for each specific class of medication, including opioids. In addition, the existence of potential confounding factors associated with pain medication use/duration of use (eg, variable availability of given medications and cultural differences) highlights the importance of interpreting results with caution when using reduction in pain medication use/duration of use as a surrogate for pain relief. Finally, participants who did not complete ZBPI questionnaires were assumed to have no pain during this period. Although this could result in an underestimation in the reported duration of pain, the numbers of participants without questionnaires were relatively small in the 3 studies (1/263 participants in ZOE-50, 2/246 in ZOE-70, and 5/184 in ZOE-HSCT).
A plain language summary contextualizing the results and clinical research relevance and impact is presented in Figure 1.
Figure 1.
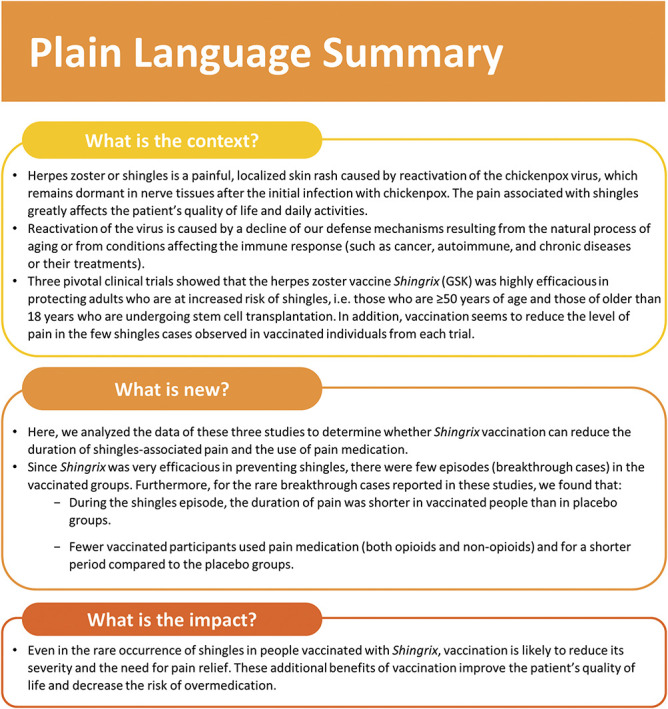
Plain language summary.
5. Conclusions
This analysis, based on data from 3 large clinical efficacy trials, indicates that RZV can be beneficial in attenuating symptoms of breakthrough cases, both in older adults and in HSCT recipients. The results presented here suggest that RZV-vaccinated participants who developed HZ experienced shorter pain duration and required less pain relief than participants who received placebo and developed HZ. Owing to the high efficacy of RZV, the number of breakthrough cases is low; however, for patients experiencing such episodes, particularly those at risk for HZ, RZV has the potential to attenuate severity and duration of the disease, thereby maintaining QoL.
Conflict of interest statement
D.C., A.F.D., J.H.K., M.K., and A.S. were employees of the GSK group of companies at the time the studies were designed, initiated, and/or conducted. A.F.D., M.K., and A.S. are currently employees of the Bill & Melinda Gates Medical Research Institute, PPD, and PATH, respectively. M.A. is an employee of Akka Technologies c/o GSK. D.C., A.F.D., J.H.K., A.S., and M.K. hold or held shares/stock options in GSK group of companies as part of their remuneration. A.L.C. received honorary payment to his institution from GSK group of companies BioCSL/Seqirus and Merck outside the submitted work. R.J. reports personal and consulting fees from GSK group of companies both during the conduct of the study and outside the submitted work and research grant from NIHR. K.M.S. reports grant and/or consulting fees from NIAID-NIH, Roche Genentech, Magenta, Kiadis, GSK group of companies, Jasper, Talaris, and Xenikos; honoraria for lecture from Vanderbilt University, Emory University, EBMT, Washington University in St Louis; lecture support from EBMT, Emory University, Magenta, Washington University in St Louis outside the submitted work. Authors have no other financial and nonfinancial interests to declare.
Appendix A. Supplemental digital content
Supplemental digital content associated with this article can be found online at http://links.lww.com/PAIN/B694.
Supplementary Material
Acknowledgements
The authors would like to thank the study participants, the investigators, and study teams involved in the ZOE-50, ZOE-70, and ZOE-HSCT trials (NCT01165177, NCT01165229, and NCT01610414), which can be found in the appropriate sections of references,1,5,6,7,25 as well as the GSK study staff involved in these trials.
The authors also thank Modis for editorial assistance and publication coordination on behalf of GSK; Marc Pirson, Kristel Vercauteren, and Irena Zurnic provided medical writing support, and Sander Hulsmans coordinated the manuscript development and provided editorial support.
This work was funded by GlaxoSmithKline Biologicals SA. GlaxoSmithKline Biologicals SA was involved in all stages of the studies (ZOE-50/70 and ZOE-HSCT) and analyses, and covered all costs associated with developing and publishing this manuscript.
Information on GSK's data sharing commitments and requesting access to anonymized individual participant data and associated documents can be found at www.clinicalstudydatarequest.com.
Author's contributions: Conceptualization: D.C., R.J., M.K., A.S., and K.M.S.; validation: A.L.C., D.C., A.F.D., R.J., J.H.K., M.K., A.S., and K.M.S.; formal analysis: M.A.; investigation: A.L.C. and K.M.S.; resources: M.A. and K.M.S.; writing (original draft): J.H.K.; visualization: D.C., A.F.D., M.A., J.H.K., M.K., and A.S.; supervision: A.F.D., J.H.K., M.K., and A.S. All authors contributed to the writing (review and editing) of the manuscript and approved the final submission version.
Trademark: Shingrix is a trademark of the GSK group of companies.
Clinical Trial Registration: ClinicalTrials.gov: NCT01165177, NCT01165229, and NCT01610414.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.painjournalonline.com).
Contributor Information
Robert Johnson, Email: rwjbristol@doctors.org.uk.
Martina Kovac, Email: martinamkovac@gmail.com.
Anthony L. Cunningham, Email: tony.cunningham@sydney.edu.au.
Mohamed Amakrane, Email: mohamed.x.amakrane@gsk.com.
Keith M. Sullivan, Email: keith.sullivan@duke.edu.
Alemnew F. Dagnew, Email: fitayehu@yahoo.com.
Desmond Curran, Email: desmond.x.curran@gsk.com.
Anne Schuind, Email: aschuind@yahoo.com.
References
- [1].Bastidas A, de la Serna J, El Idrissi M, Oostvogels L, Quittet P, Lopez-Jimenez J, Vural F, Pohlreich D, Zuckerman T, Issa NC, Gaidano G, Lee JJ, Abhyankar S, Solano C, Perez de Oteyza J, Satlin MJ, Schwartz S, Campins M, Rocci A, Vallejo Llamas C, Lee DG, Tan SM, Johnston AM, Grigg A, Boeckh MJ, Campora L, Lopez-Fauqued M, Heineman TC, Stadtmauer EA, Sullivan KM; ZOE-HSCT Study Group. Effect of recombinant zoster vaccine on incidence of herpes zoster after autologous stem cell transplantation: a randomized clinical trial. JAMA 2019;322:123–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Bruxvoort KJ, Liang AS, Harpaz R, Qian L, Sy LS, LaRussa P, Schmid DS, Luo Y, Takhar H, Tseng HF. Patient report of herpes zoster pain: incremental benefits of zoster vaccine live. Vaccine 2019;37:3478–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Centers for Disease Control and Prevention. Shingles (Herpes Zoster): Complications, 2019. Available at: https://www.cdc.gov/shingles/about/complications.html. [Google Scholar]
- [4].Coplan PM, Schmader K, Nikas A, Chan ISF, Choo P, Levin MJ, Johnson G, Bauer M, Williams HM, Kaplan KM, Guess HA, Oxman MN. Development of a measure of the burden of pain due to herpes zoster and postherpetic neuralgia for prevention trials: adaptation of the brief pain inventory. J Pain 2004;5:344–56. [DOI] [PubMed] [Google Scholar]
- [5].Cunningham AL, Lal H, Kovac M, Chlibek R, Hwang SJ, Diez-Domingo J, Godeaux O, Levin MJ, McElhaney JE, Puig-Barbera J, Vanden Abeele C, Vesikari T, Watanabe D, Zahaf T, Ahonen A, Athan E, Barba-Gomez JF, Campora L, de Looze F, Downey HJ, Ghesquiere W, Gorfinkel I, Korhonen T, Leung E, McNeil SA, Oostvogels L, Rombo L, Smetana J, Weckx L, Yeo W, Heineman TC; ZOE Study Group. Efficacy of the herpes zoster subunit vaccine in adults 70 years of age or older. N Engl J Med 2016;375:1019–32. [DOI] [PubMed] [Google Scholar]
- [6].Curran D, Matthews S, Rowley SD, Young JAH, Bastidas A, Anagnostopoulos A, Barista I, Chandrasekar PH, Dickinson M, El Idrissi M, Heras I, Milliken ST, Monserrat Coll J, Navarro Matilla MB, Oostvogels L, Piatkowska-Jakubas B, Quiel D, Sabry W, Schwartz S, Selleslag DLD, Sullivan KM, Theunissen K, Yegin ZA, Yeh SP, Zaja F, Szer J; ZOE-HSCT Study Group. Recombinant zoster vaccine significantly reduces the impact on quality of life caused by herpes zoster in adult autologous hematopoietic stem cell transplant recipients: a randomized placebo-controlled trial (ZOE-HSCT). Biol Blood Marrow Transpl 2019;25:2474–81. [DOI] [PubMed] [Google Scholar]
- [7].Curran D, Oostvogels L, Heineman T, Matthews S, McElhaney J, McNeil S, Diez-Domingo J, Lal H, Andrews C, Athan E, Berglund J, Campora L, de Looze F, Korhonen T, Leung E, Levin M, Volpi A, Johnson RW; ZOE Study Group. Quality of life impact of an adjuvanted recombinant zoster vaccine in adults aged 50 years and older. J Gerontol A Biol Sci Med Sci 2019;74:1231–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Dagnew AF, Ilhan O, Lee WS, Woszczyk D, Kwak JY, Bowcock S, Sohn SK, Rodriguez Macias G, Chiou TJ, Quiel D, Aoun M, Navarro Matilla MB, de la Serna J, Milliken S, Murphy J, McNeil SA, Salaun B, Di Paolo E, Campora L, Lopez-Fauqued M, El Idrissi M, Schuind A, Heineman TC, Van den Steen P, Oostvogels L; ZOE-HSCT study group. Immunogenicity and safety of the adjuvanted recombinant zoster vaccine in adults with haematological malignancies: a phase 3, randomised, clinical trial and post-hoc efficacy analysis. Lancet Infect Dis 2019;19:988–1000. [DOI] [PubMed] [Google Scholar]
- [9].Dooling KL, Guo A, Patel M, Lee GM, Moore K, Belongia EA, Harpaz R. Recommendations of the advisory committee on immunization practices for use of herpes zoster vaccines. MMWR Morb Mortal Wkly Rep 2018;67:103–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Drolet M, Brisson M, Schmader KE, Levin MJ, Johnson R, Oxman MN, Patrick D, Blanchette C, Mansi JA. The impact of herpes zoster and postherpetic neuralgia on health-related quality of life: a prospective study. CMAJ 2010;182:1731–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Dworkin RH, Barbano RL, Tyring SK, Betts RF, McDermott MP, Pennella-Vaughan J, Bennett GJ, Berber E, Gnann JW, Irvine C, Kamp C, Kieburtz K, Max MB, Schmader KE. A randomized, placebo-controlled trial of oxycodone and of gabapentin for acute pain in herpes zoster. PAIN 2009;142:209–17. [DOI] [PubMed] [Google Scholar]
- [12].Dworkin RH, Johnson RW, Breuer J, Gnann JW, Levin MJ, Backonja M, Betts RF, Gershon AA, Haanpaa ML, McKendrick MW, Nurmikko TJ, Oaklander AL, Oxman MN, Pavan-Langston D, Petersen KL, Rowbotham MC, Schmader KE, Stacey BR, Tyring SK, van Wijck AJM, Wallace MS, Wassilew SW, Whitley RJ. Recommendations for the management of herpes zoster. Clin Infect Dis 2007;44(suppl 1):S1–26. [DOI] [PubMed] [Google Scholar]
- [13].Elliott KJ. Other neurological complications of herpes zoster and their management. Ann Neurol 1994;35(suppl):S57–61. [DOI] [PubMed] [Google Scholar]
- [14].Forbes HJ, Bhaskaran K, Thomas SL, Smeeth L, Clayton T, Langan SM. Quantification of risk factors for herpes zoster: population based case-control study. BMJ 2014;348:g2911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Furlan AD, Harvey AM, Chadha R. Warning from Canada: Latin America, South Africa and India may face an opioid epidemic in the coming years. J Glob Health 2020;10:010324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Gnann JW, Jr. Varicella-zoster virus: atypical presentations and unusual complications. J Infect Dis 2002;186(suppl 1):S91–8. [DOI] [PubMed] [Google Scholar]
- [17].GSK. Shingrix Approved in Europe and Japan for the Prevention of Shingles in Adults Aged 50 and Over, 2018. Available at: https://www.gsk.com/en-gb/media/press-releases/shingrix-approved-in-europe-and-japan-for-the-prevention-of-shingles-in-adults-aged-50-and-over/. [Google Scholar]
- [18].GSK Study Register. GSK Study ID 113077. Study to Evaluate Efficacy, Safety and Immunogenicity of GlaxoSmithKline (GSK) Biologicals' Herpes Zoster (HZ) Vaccine GSK1437173A in Adults Aged 70 Years and Older, 2020. Available at: https://www.gsk-studyregister.com/en/trial-details/?id=113077. [Google Scholar]
- [19].Harpaz R, Ortega-Sanchez IR, Seward JF, Advisory Committee on Immunization Practices (ACIP), Centers for Disease Control and Prevention (CDC). Prevention of herpes zoster: recommendations of the advisory committee on immunization practices (ACIP). MMWR Recomm Rep 2008;57:1–30; quiz CE2-4. [PubMed] [Google Scholar]
- [20].Jayasinghe S, Sheridan S, Macartney K. Herpes zoster vaccination in Australia: what's available and who benefits? Aust Prescr 2020;43:2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Jeon YH. Herpes zoster and postherpetic neuralgia: practical consideration for prevention and treatment. Korean J Pain 2015;28:177–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Johnson RW, Alvarez-Pasquin MJ, Bijl M, Franco E, Gaillat J, Clara JG, Labetoulle M, Michel JP, Naldi L, Sanmarti LS, Weinke T. Herpes zoster epidemiology, management, and disease and economic burden in Europe: a multidisciplinary perspective. Ther Adv Vaccin 2015;3:109–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Johnson RW, Bouhassira D, Kassianos G, Leplege A, Schmader KE, Weinke T. The impact of herpes zoster and post-herpetic neuralgia on quality-of-life. BMC Med 2010;8:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Kovac M, Lal H, Cunningham AL, Levin MJ, Johnson RW, Campora L, Volpi A, Heineman TC; ZOE-50/70 Study Group. Complications of herpes zoster in immunocompetent older adults: incidence in vaccine and placebo groups in two large phase 3 trials. Vaccine 2018;36:1537–41. [DOI] [PubMed] [Google Scholar]
- [25].Lal H, Cunningham AL, Godeaux O, Chlibek R, Diez-Domingo J, Hwang SJ, Levin MJ, McElhaney JE, Poder A, Puig-Barbera J, Vesikari T, Watanabe D, Weckx L, Zahaf T, Heineman TC, Group ZS. Efficacy of an adjuvanted herpes zoster subunit vaccine in older adults. N Engl J Med 2015;372:2087–96. [DOI] [PubMed] [Google Scholar]
- [26].Miettinen O, Nurminen M. Comparative analysis of two rates. Stat Med 1985;4:213–26. [DOI] [PubMed] [Google Scholar]
- [27].Ottawa Public Health. Immunization Update: NACI Recommends RZV (Shingrix®) Vaccine in Persons Aged 50 Years and Older, Ottawa: Ottawa Public Health; 2018. [Google Scholar]
- [28].Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb LD, Arbeit RD, Simberkoff MS, Gershon AA, Davis LE, Weinberg A, Boardman KD, Williams HM, Zhang JH, Peduzzi PN, Beisel CE, Morrison VA, Guatelli JC, Brooks PA, Kauffman CA, Pachucki CT, Neuzil KM, Betts RF, Wright PF, Griffin MR, Brunell P, Soto NE, Marques AR, Keay SK, Goodman RP, Cotton DJ, Gnann JW, Loutit J, Holodniy M, Keitel WA, Crawford GE, Yeh SS, Lobo Z, Toney JF, Greenberg RN, Keller PM, HaRbecke R, Hayward AR, Irwin MR, Kyriakides TC, Chan CY, Chan ISF, Wang WWB, Annunziato PW, Silber JL, Shingles Prevention Study G, Weinberg A. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med 2005;352:2271–84. [DOI] [PubMed] [Google Scholar]
- [29].Robert Koch Institut. Epidemiologisches Bulletin, Robert Koch Institut: 2018. [Google Scholar]
- [30].Sahoo F, Hill JA, Xie H, Leisenring W, Yi J, Goyal S, Kimball LE, Lee I, Seo S, Davis C, Pergam SA, Flowers ME, Liaw KL, Holmberg L, Boeckh M. Herpes zoster in autologous hematopoietic cell transplant recipients in the era of acyclovir or valacyclovir prophylaxis and novel treatment and maintenance therapies. Biol Blood Marrow Transpl 2017;23:505–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Sampathkumar P, Drage LA, Martin DP. Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc 2009;84:274–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Whitley RJ, Weiss H, Gnann JW, Jr, Tyring S, Mertz GJ, Pappas PG, Schleupner CJ, Hayden F, Wolf J, Soong SJ. Acyclovir with and without prednisone for the treatment of herpes zoster. A randomized, placebo-controlled trial. The National Institute of Allergy and Infectious Diseases Collaborative Antiviral Study Group. Ann Intern Med 1996;125:376–83. [DOI] [PubMed] [Google Scholar]
- [33].Winston DJ, Mullane KM, Cornely OA, Boeckh MJ, Brown JW, Pergam SA, Trociukas I, Zak P, Craig MD, Papanicolaou GA, Velez JD, Panse J, Hurtado K, Fernsler DA, Stek JE, Pang L, Su SC, Zhao Y, Chan ISF, Kaplan SS, Parrino J, Lee I, Popmihajlov Z, Annunziato PW, Arvin A. Inactivated varicella zoster vaccine in autologous haemopoietic stem-cell transplant recipients: an international, multicentre, randomised, double-blind, placebo-controlled trial. Lancet 2018;391:2116–27. [DOI] [PubMed] [Google Scholar]
- [34].World Health Organization. WHO's pain relief ladder, 2019. Available at: https://www.who.int/cancer/palliative/painladder/en/. [Google Scholar]
- [35].Yawn BP, Wollan PC, Kurland MJ, St Sauver JL, Saddier P. Herpes zoster recurrences more frequent than previously reported. Mayo Clin Proc 2011;86:88–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Zorzoli E, Pica F, Masetti G, Franco E, Volpi A, Gabutti G. Herpes zoster in frail elderly patients: prevalence, impact, management, and preventive strategies. Aging Clin Exp Res 2018;30:693–702. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental digital content associated with this article can be found online at http://links.lww.com/PAIN/B694.


