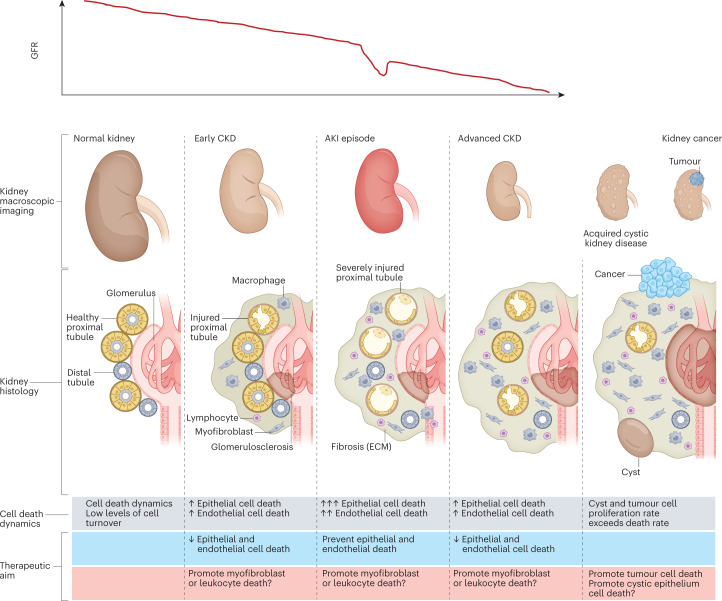
Fig. 1. The natural history of CKD and relationship to cell number and cell death.
The relationship between chronic kidney disease (CKD), acute kidney injury (AKI), acquired kidney cystic disease and kidney cancer can be conceptualized as interrelated processes, characterized by changes in cell number that are driven by the proliferation or death of key cell types. Differences in the dynamics of cell death and turnover represent potential therapeutic targets. AKI is more common in patients with prior CKD and may cause irreversible loss of kidney function or accelerate CKD progression. However, not all episodes of AKI are associated with prior CKD. Of note, AKI is not necessarily characterized by a loss of kidney epithelial cells, but cell death is common in severe episodes of AKI. Acquired kidney cystic disease is usually not clinically relevant although bleeding may occur3. However, acquired kidney cystic disease is a risk factor for renal cell carcinoma7,8. Both acquired kidney cystic disease and kidney cancer are associated with an increase in cell number. In kidney cysts, an excess number of epithelial cells allows cyst growth. Kidney cancer is characterized by an increased number of malignant epithelial cells; the goal of therapy in this context is to kill or extirpate these cells. Renal cell carcinoma may occur in individuals with or without prior CKD. However, CKD is a risk factor for renal cell carcinoma4. Of note, acquired cystic kidney disease renal cell carcinoma is considered a distinct renal neoplasm according to the International Society of Urological Pathology–WHO, and is associated with specific somatic mutations5. ECM, extracellular matrix; GFR, glomerular filtration rate.