ABSTRACT
Background:
Cardiovascular diseases (CVDs) are the leading non-communicable cause of morbidity and mortality worldwide. This study aimed at determining the association of metabolic risk factors with ischemic heart disease (IHD) and heart failure (HF).
Methods:
A cross-sectional study including 104 participants was conducted in three major hospitals between October 2020 and October 2021. All adult patients of either gender, over the age of 35, attending the CVD screening program at the family medicine clinics of the hospitals were included in the study. The physician collected demographic details, history of CVD, diabetes or hypertension, and current medication. Each patient’s body mass index (BMI) was calculated, electrocardiogram (ECG) and blood tests were done. Univariate and multivariate logistic regressions were checked.
Results:
The mean age of the participants was 47.6 (SD = 13.5) years. Diabetes and hypertension had increased odds of IHD by 129 (CI = 6.20 – 2698.42, P = 0.002) and 195 (CI = 13.87 – 2743.11, P < 0.001) times, respectively. Diabetes mellitus (Chi2 = 11.93, P < 0.001) and hypertension (Chi2 = 14.74, P < 0.001) had significant association with HF. Dyslipidemia was significantly associated with IHD (OR = 12.41, CI = 1.15 – 134.12, P = 0.038) and high-grade HF (OR = 14.91 CI = 3.61 – 61.40, P < 0.001).
Conclusion:
Age, dyslipidemia, diabetes, hypertension, and left ventricular hypertrophy have significant association with IHD or HF among the study population.
Keywords: Diabetes, dyslipidemia, heart failure, hypertension, ischemic heart disease, Saudi Arabia
Background
Cardiovascular diseases (CVDs) are the leading non-communicable cause of morbidity and mortality worldwide.[1] In 2020, 19 million people died of CVDs with future estimates that CVDs will contribute to 22.2 million annual deaths by the year 2030.[1,2] CVD is general term which encompasses a wide array of diseases arising within the cardiovascular system where coronary artery disease (CAD) or coronary heart disease (CHD), cerebrovascular disease, peripheral arterial disease (PAD), aortic atherosclerosis, and rheumatic heart disease are the major contributors.[3] In 2015, CAD contributed to 8.9 million deaths worldwide where 7 million people died only in low-income countries and middle-income countries.[4]
A cluster of cardiovascular metabolic risk factors have been reported in the literature including hypertension, diabetes mellitus, obesity, dyslipidemia, and hyperuricemia.[5,6] Hypertension has a long-standing, strong, independent, and linear relationship with CVDs as it is a major risk factor of CAD and the most common cause of heart failure (HF).[7,8] Overall, it has been reported that 33% CVDs are contributed by hypertension.[9] However, this percentage is variable in different studies, and for different types of CVDs.[10] Chronic hypertension leads to vascular stiffness, raised systolic blood pressure and wide pulse pressure, resulting in reduced coronary perfusion, increased oxygen demand and left ventricular hypertrophy (LVH).[11] Diabetes is a global emergency of 21st century and a major risk of CVDs. Diabetes increases CVD mortality as 44% and 52% deaths occur in type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) due to CVDs, respectively.[12] Diabetes causes CVDs via epigenetic, genetic, and cell-signaling defects in various metabolic and inflammatory pathways.[13]
Dyslipidemia is another major risk factor of CVDs. About 87% patients with CVDs suffer from dyslipidemia.[14] Dyslipidemia involves a set of diverse metabolic and immunologic mechanisms which cause narrowing of vessels on account of fatty acids accumulation, endothelial damage, inflammation, smooth cell proliferation, and vascular fibrosis resulting in insufficient blood flow via the affected vessel and ending up with ischemic injury.[15] Similarly, obesity and hyperuricemia lead to increased risk of CVDs. Obesity, especially abdominal obesity, is associated with other cardiovascular risk factors such as hypertension, insulin resistance, raised fibrinogen and C-reactive protein (CRP) leading to increased risk of CAD, stroke, HF and arterial aneurysm.[16] Moreover, the combination of obesity-associated cardiovascular risk factors such as dyslipidemia, type 2 diabetes, and high blood pressure result in a lethal condition known as “metabolic syndrome” which itself is a high risk for CVDs such as congestive HF and atherosclerotic heart disease. The emerging evidence supports that uncontrolled grout contributes to cardiometabolic comorbidities via systemic inflammation, oxidative stress and accelerated atherosclerosis.[17] Hence, early identification and proper prevention of metabolic risk factors may prevent CVDs.
CVDs and their risk factors are prevalent in Middle East. In Saudi Arabia, 45.7% deaths are attributed to CVDs, anticipating high burden of cardiovascular risk factors in the region.[18] However, a few studies have been conducted to determine the potential metabolic risk factors of CVDs, especially at local level. Therefore, this study was done to determine the association of metabolic risk factors with ischemic heart disease and HF among Saudi population.
Methods
Study designs and aims
This study set out to identify associations between metabolic risk factors and common CVDs particularly, ischemic health disease and HF among patients vising the cardiology outpatient departments in a large tertiary care Saudi Hospital. To this end, we designed a cross-sectional study that was conducted in at King Khalid hospital and Prince Sultan Centre for Healthcare in Al-Kharj City, Prince Sattam bin Abdulaziz University Hospital, and the Al Kharj Military Industries Corporation Hospital in Al-Kharj City in the KSA hospital, Riyadh between October 2020 and October 2020.
Study population
Drawing from the work of Aljefree et al.,[19] Al-Rubeaan et al.[20] and Wilson et al.,[21] we calculated a sample size of 103 to attain 95% confidence and 80% power. All adult patients of either gender, over the age of 18, attending the CVD screening program at the family medicine clinics of the targeted Hospitals in the Kingdom of Saudi Arabia between the dates of October 2020 and October 2021 were included in the study. Patients with acute cardiovascular symptoms who required emergency treatment, those who were unable or unwilling to give informed consent, and patients who did not complete the screening program were excluded from the study.
Data collection
The physician collected basic demographic details – age, gender, nationality, and medical history – history of CVD, diabetes or hypertension, and current medication. The patient’s BMI was calculated using height and weight measurements. Each patient then underwent blood testing for Blood Urea Nitrogen (BUN), urea, creatinine, uric acid, glycated hemoglobin, blood sugars, and a lipid profile. Echocardiogram was done to check for LVH and wall thickness. HF was diagnosed by a cardiologist based on a combination of clinical signs and symptoms, laboratory, and echocardiography findings. Ischemic heart disease (IHD) was diagnosed by a cardiologist based on current or previous diagnostic coronary angiogram results. Patients who screened positive on our tests or who had documented past medical history of CVD were classified as having CVD. Patient electronic medical records data were examined to corroborate their medical history of CVD and their risk factors to minimize the effects of recall bias.
Statistical analysis
Statistical Package for Social Sciences software (SPSS) version 22 was used to run the statistical analyses for this study. Our final dataset contained less than 1% missing data which was negligible. As a part of descriptive analysis, we calculated means and standard deviations for numerical variables and frequency and percentages for categorical data. The potential risk factors were also cross tabulated with IHD and HF.
Univariate logistic regression was used to check the association between each potential risk factor and CVDs. Those variables that were associated with IHD or HF with a strength of evidence P < 0.25 were regarded for inclusion in the multivariable model. Three multivariable logistic regressions were carried out with IHD and HF as the outcomes of interest respectively. Age and sex were “forced-in” variables included in every model owing to their known importance in the pathophysiology of CVD and potential for confounding the association between CVD and other risk factors.
Ethical considerations
We obtained written and informed consent from all study participants before enrollment in the study. The study was conducted following the guidelines set out by the Prince Sattam bin Abdulaziz university ethics committee after obtaining their ethical approval. (Ethical approval number: SCBR-2022/03/18670). All participant identifiers were erased to ensure their confidentiality.
Results
Population characteristics
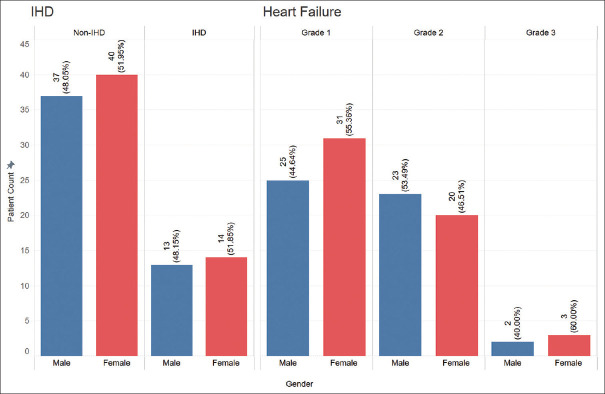
A total of 104 participants were included in our study. They had a mean age of 47.6 (SD = 13.5) years, and 54 (51.9%) were females. Most patients (61.54%) were in the 40 to 64 age group. Overall, 27 (26.0%) and 48 (46.2%) participants had IHD and HF, respectively. The prevalence of CVDs by gender is shown in Figure 1. Sixty-one (58.65%) of the participants were of non-Saudi nationality. Table 1 shows the distribution of other demographic and clinical characteristics of our study population.
Figure 1.
Prevalence of CVD by genders
Table 1.
Demographic, clinical, and paraclinical characteristics of the study population. Values are expressed as mean (standard deviation) for continuous variables and frequency (percent) for categorical variables
| Variable | Value |
|---|---|
| Age | |
| <25 | 7 (6.73%) |
| 25-39 | 22 (21.15%) |
| 40-64 | 64 (61.54%) |
| ≤65 | 11 (10.58%) |
| Gender | |
| Female | 54 (51.92%) |
| Male | 50 (48.08%) |
| Nationality | |
| Non-Saudi | 61 (58.65%) |
| Saudi | 43 (41.35%) |
| Smoking | |
| No | 100 (96.15%) |
| Yes | 4 (3.85%) |
| Hypertension | |
| Stage 1 | 82 (78.85%) |
| Stage 2 | 19 (18.27%) |
| Stage 3 | 3 (2.88%) |
| Diabetes Mellitus | |
| No | 65 (62.50%) |
| Yes | 39 (37.50%) |
| Dyslipidemia | |
| No | 73 (70.19%) |
| Yes | 31 (29.81%) |
| LVH | |
| 1 | 41 (39.42%) |
| 2 | 58 (55.77%) |
| 3 | 5 (4.81%) |
| Wall Motion Abnormality | |
| 1 | 81 (77.88%) |
| 2 | 23 (22.12%) |
| BMI | 33.91 (7.35) |
| BUN | 4.98 (3.12) |
| Creatinine | 76.11 (50.89) |
| HbA1c | 6.2 (1.83) |
| FBS | 6.56 (2.97) |
| LDL | 2.86 (1.01) |
| HDL | 1.18 (0.20) |
| Cholesterol | 4.65 (0.93) |
| Triglyceride | 1.52 (0.81) |
Risk factors for ischemic heart disease
Age and IHD
There was strong evidence to suggest that the average age of those with IHD was 7 years greater than those without IHD (difference = 6.95 years, P = 0.0087). The age group of 40 to 64 had the greatest number of IHD patients with 21 (77.78%).
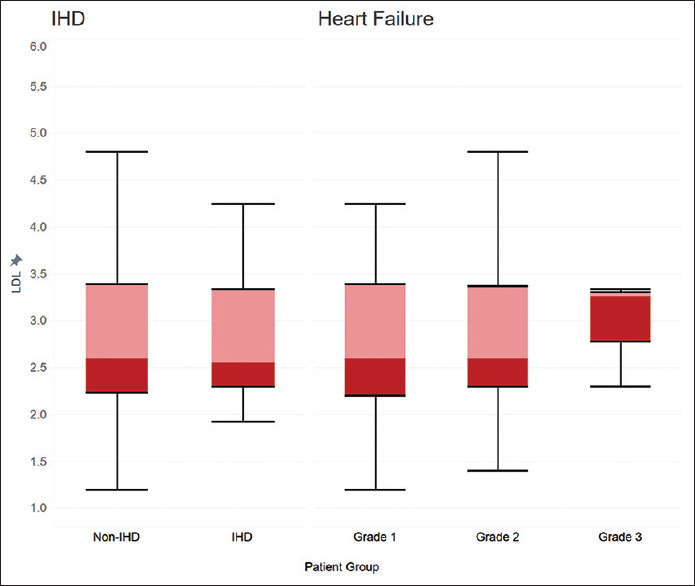
Dyslipidemia and IHD
We found a significant association between dyslipidemia and IHD. (Chi2 = 4.74, P = 0.03, Table 2) The association between dyslipidemia and IHD remained statistically significant ever after adjusting for other risk factors of CVDs (OR = 12.41, CI = 1.15 – 134.12, P = 0.038, Figure 2).
Table 2.
Demographic, clinical, and paraclinical characteristics of the IHD versus non-IHD patients. Values are expressed as mean (standard deviation) for continuous variables and frequency (percent) for categorical variables
| Variable | Non-IHD | IHD |
|---|---|---|
| Age | ||
| <25 | 7 (9.09%) | - |
| 25-39 | 19 (24.68%) | 3 (11.11%) |
| 40-64 | 43 (55.84%) | 21 (77.78%) |
| ≤65 | 8 (10.39%) | 3 (11.11%) |
| Gender | ||
| Female | 40 (51.95%) | 14 (51.85%) |
| Male | 37 (48.05%) | 13 (48.15%) |
| Nationality | ||
| Non-Saudi | 48 (62.34%) | 13 (48.15%) |
| Saudi | 29 (37.66%) | 14 (51.85%) |
| Smoking | ||
| No | 76 (98.70%) | 24 (88.895) |
| Yes | 1 (1.30%) | 3 (11.11%) |
| Hypertension | ||
| Stage 1 | 75 (97.40%) | 7 (25.93%) |
| Stage 2 | 1 (1.30%) | 18 (66.67%) |
| Stage 3 | 1 (1.30%) | 2 (7.41%) |
| Diabetes Mellitus | ||
| No | 59 (76.62%) | 6 (22.22%) |
| Yes | 18 (23.38%) | 21 (77.78%) |
| Dyslipidemia | ||
| No | 59 (76.62%) | 14 (51.85%) |
| Yes | 18 (23.38%) | 13 (48.15%) |
| LVH | ||
| 1 | 40 (51.95%) | 1 (3.70%) |
| 2 | 35 (45.45%) | 23 (85.19%) |
| 3 | 2 (2.60%) | 3 (11.11%) |
| Wall Motion Abnormality | ||
| 1 | 76 (98.70%) | 5 (18.52%) |
| 2 | 1 (1.30%) | 22 (81.48%) |
| BMI | 33.75 (7.81) | 34.37 (5.97) |
| BUN | 4.91 (3.44) | 5.23 (1.49) |
| Creatinine | 78.42 (56.69) | 67.50 (14.87) |
| HbA1c | 6.01 (1.66) | 6.90 (2.27) |
| FBS | 6.50 (2.86) | 6.82 (3.42) |
| LDL | 2.88 (1.07) | 2.78 (0.72) |
| HDL | 1.18 (0.21) | 1.16 (0.15) |
| Cholesterol | 4.62 (0.98) | 4.78 (0.69) |
| Triglyceride | 1.56 (0.85) | 1.37 (0.60) |
Figure 2.
Dyslipidemia as a risk factor for CVD
Other risk factors of IHD
A history of diabetes and hypertension were both significantly associated with IHD. In the multivariable logistic regression, having diabetes or hypertension increased the odds of IHD by 129 (CI = 6.20 – 2698.42, P = 0.002) and 195 (CI = 13.87 – 2743.11, P < 0.001) times respectively. We found a statistically significant association between IHD and LVH and wall thickness on echo cardiography [Table 2].
Risk factors for heart failure
Age and heart failure
Among the participants, 56 (53.8%) had grade 1 HF, 43 (41.3%) had grade 2 HF and 5 (4.8%) had grade 3 HF. Those belonging to the age group of 40 to 64 had the most cases of HF [Table 3]. We found that the mean age among those with grade 3 HF was 18 years lower than the mean age among those with grade 1 HF (difference = 18.01, P < 0.001). After controlling for other possible confounders using multiple logistic regression, there was strong evidence to suggest that odds of having grade 2 or 3 HF increased by 1.09 times for each year increase in age. (CI = 1.03 – 1.15, P = 0.002).
Table 3.
Demographic, clinical, and paraclinical characteristics of the patients with different grades of HF. Values are expressed as mean (standard deviation) for continuous variables and frequency (percent) for categorical variables
| Variable | Grade 1 | Grade 2 | Grade 3 |
|---|---|---|---|
| Age | |||
| <25 | 7 (12.50%) | - | - |
| 25-39 | 18 (32.14%) | 4 (9.30%) | - |
| 40-64 | 28 (50.00%) | 33 (76.74%) | 3 (60.00%) |
| ≤65 | 3 (5.36%) | 6 (13.95%) | 2 (40.00%) |
| Gender | |||
| Female | 31 (55.36%) | 20 (46.51%) | 3 (60.00%) |
| Male | 25 (44.64%) | 23 (53.49%) | 2 (40.00%) |
| Nationality | |||
| Non-Saudi | 35 (62.50%) | 24 (55.81%) | 2 (40.00%) |
| Saudi | 21 (37.50%) | 19 (44.19%) | 3 (60.00%) |
| Smoking | |||
| No | 54 (96.43%) | 42 (97.67%) | 4 (80.00%) |
| Yes | 2 (3.57%) | 1 (2.33%) | 1 (20.00%) |
| Hypertension | |||
| Stage 1 | 52 (92.86%) | 29 (67.44%) | 1 (20.00%) |
| Stage 2 | 4 (7.14%) | 11 (25.58%) | 4 (80.00%) |
| Stage 3 | - | 3 (6.98%) | - |
| Diabetes Mellitus | |||
| No | 44 (78.57%) | 18 (41.86%) | 3 (60.00%) |
| Yes | 12 (21.435) | 25 (58.14%) | 2 (40.00%) |
| Dyslipidemia | |||
| No | 50 (89.29%) | 22 (51.16%) | 1 (20.00%) |
| Yes | 6 (10.71%) | 21 (48.84%) | 4 (80.00%) |
| LVH | |||
| 1 | 36 (80.36%) | 5 (11.63%) | - |
| 2 | 20 (35.71%) | 34 (79.07%) | 4 (80.00%) |
| 3 | - | 4 (9.30%) | 1 (20.00%) |
| Wall Motion Abnormality | |||
| 1 | 56 (100.00%) | 25 (58.14%) | - |
| 2 | - | 18 (41.86%) | 5 (100.00%) |
| BMI | 33.64 (8.44) | 34.07 (5.89) | 35.60 (6.58) |
| BUN | 4.60 (3.31) | 5.39 (2.95) | 5.89 (1.92) |
| Creatinine | 74.96 (49.39) | 78.08 (55.30) | 70.00 (14.73) |
| HbA1c | 6.13 (1.98) | 6.28 (1.72) | 6.33 (0.58) |
| FBS | 6.84 (3.56) | 6.34 (2.12) | 5.07 (0.12) |
| LDL | 2.81 (1.11) | 2.91 (0.91) | 2.97 (0.58) |
| HDL | 1.19 (0.22) | 1.18 (0.17) | 1.03 (0.18) |
| Cholesterol | 4.67 (0.94) | 4.61 (0.95) | 4.86 (0.46) |
| Triglyceride | 1.52 (0.84) | 1.51 (0.78) | 1.69 (0.88) |
Diabetes and hypertension as risk factors for heart failure
There was a statistically significant association between HF and diabetes mellitus. [Figure 3] Those with diabetes had five times the odds of having high grade HF compared to those without diabetes after controlling for other risk factors. (OR = 5.07, CI = 1.48 – 17.46, P = 0.01) Similarly, there was a significant association between HF and hypertension (Chi2 = 14.74, P < 0.001). However, after controlling for other possible risk factors, this association was not statistically significant.
Figure 3.

Diabetes mellitus as a risk factor for CVDs
Dyslipidemia and heart failure
History of dyslipidemia was significantly associated with HF (Chi2 = 19.21, P < 0.001, Figure 2). In our multiple regression model, those with dyslipidemia had 15 times the odds of high-grade HF compared to those with a normal lipid profile (OR = 14.91 CI = 3.61 – 61.40, P < 0.001).
Discussion
This cross-sectional study was conducted to identify the metabolic risk factors of common CVDs in Saudi Arabia. The study revealed significant association of age, dyslipidemia, diabetes, hypertension, and LVH with IHD or HF. However, nationality, gender, smoking, BMI, creatinine, and BUN had no significant association with IHD or HF. The present study identified that the patients with IHD had 7 years higher mean age than those without IHD. Similarly, the patients with grade 3 HF had 18 years lesser average age than those without HF. In addition, the patients having dyslipidemia showed 15 times higher risk for HF as compared to that experienced by the patients without dyslipidemia.
Age and cardiovascular disease
Our study found a strong association between increasing age and risk of CVDs. The link between advancing age and CVD may be attributed to the accumulation of multiple risk factors such as hypertension, diabetes, dyslipidemia, renal impairment, and smoking.[22] In the elderly, a cluster of factors including oxidative stress, genetic stability, inflammation and endothelial homeostasis are play a pivotal role in vascular aging resulting in IHD.[23] Similarly, prevalence of HF increases with advancing age. Bosch et al.[24] retrospectively analyzed the electronic records of 56,320 adult patients from 11 general practices and reported 0.04% and 20.9% among patients aged <44 years and ≥85 years, respectively. This highlights the need for screening for risk factors and CVDs among older age groups.
Diabetes, hypertension, and dyslipidemia as risk factors of cardiovascular disease
Dyslipidemia, diabetes, hypertension, and LVH were found to be major risk factors of IHD and HF in our study. Several other previously published studies have found similar results. Mahalle et al.[25] studied 300 angiography-confirmed CAD patients to determine lipid abnormalities and their association with CAD. They reported 41.3% atherogenic dyslipidemia in the patients with CAD. Hence, dyslipidemia is an independent major risk factor of CAD. In combination with other comorbidities such and diabetes and hypertension, dyslipidemia results in worse outcome. Lee et al.[26] studied the relationship of high triglyceride (TG) levels and low HDL cholesterol (HDL-C) with glycemic control in terms of CHD. They reported the patients with high TG and low HDL levels had 1.32-fold greater hazard ratios for CHD than those with normal ranges of TG and HDL. Moreover, they reported 1.54- and 2.13-fold greater hazard ratios for CHD and stroke among diabetic patients with high TG and low HDL as compared to non-diabetic patients, respectively. Ariyanti and Besral conducted a case-control study to determine association of dyslipidemia and hypertension with CHD. They reported that hypertensive patients with dyslipidemia had 18 times greater risk of CHD than those without dyslipidemia.[27] Evidence from our study taken together with that from other similar studies point toward the need for screening for and treating these risk factors and among those who have these risk factors, having a high degree of suspicion for the development of CVD.
Strengths and Limitations
The advantage of this study is that the study has put forth the association of different metabolic risk factors of IHD and HF among people living in Saudi Arabia which may provoke the authorities to establish proper policies to reduce these risk factors of CVD. The study is limited in terms of small sample size and a single healthcare centered study which does not allow its result to be generalized.
Conclusion
In conclusion, age, dyslipidemia, diabetes, hypertension, and LVH significantly increased the risk of IHD or HF among study population. Our results suggest that meticulous screening and management of these risk factors among eligible Saudi population can go a long way in preventing serious cardiovascular morbidity and mortality. Additionally, those with confirmed risk factors should be regarded with a high degree of suspicion for development of a CVD. We recommend further studies in this field to improve generalizability to the Saudi Population.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
This publication was supported by the Deanship of Scientific Research at Prince Sattam bin Abdulaziz University, Al-Kharj, Saudi Arabia.
References
- 1.Ruan Y, Guo Y, Zheng Y, Huang Z, Sun S, Kowal P, et al. Cardiovascular disease (CVD) and associated risk factors among older adults in six low-and middle-income countries: Results from SAGE Wave 1. BMC Public Health. 2018;18:1–3. doi: 10.1186/s12889-018-5653-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart disease and stroke statistics—2022 update: A report from the American Heart Association. Circulation. 2022;145:e153–639. doi: 10.1161/CIR.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 3.Stewart J. Primary prevention of cardiovascular disease: A review of contemporary guidance and literature. JRSM Cardiovasc Dis. 2017;6:2048004016687211. doi: 10.1177/2048004016687211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ralapanawa U, Sivakanesan R. Epidemiology and the magnitude of coronary artery disease and acute coronary syndrome: A narrative review. J Epidemiol Glob Health. 2021;11:169–77. doi: 10.2991/jegh.k.201217.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet. 2020;395:795–808. doi: 10.1016/S0140-6736(19)32008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Borghi C, Piani F. Uric acid and risk of cardiovascular disease: A question of start and finish. Hypertension. 2021;78:1219–21. doi: 10.1161/HYPERTENSIONAHA.121.17631. [DOI] [PubMed] [Google Scholar]
- 7.Fakhri M, Sarokhani D, Ghiasi B, Dehkordi AH. Prevalence of hypertension in cardiovascular disease in Iran: Systematic review and meta-analysis. Int J Prev Med. 2020;11:56. doi: 10.4103/ijpvm.IJPVM_351_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–37. doi: 10.1038/s41581-019-0244-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ruiz-Hernandez A, Tellez-Plaza M, Dominguez-Lucas A, Pichler G, Martin-Escudero JC, Martinez-Garcia F, et al. Population attributable risk for cardiovascular disease associated with hypertension. Results from the Hortega follow-up study. J Hypertens. 2018;36:e27. [Google Scholar]
- 10.Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020;75:285–92. doi: 10.1161/HYPERTENSIONAHA.119.14240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Humrahian SM. Pathophysiology of hypertension. May 18, 2017. Available from: https://emedicine.medscape.com/article/1937383-overview .
- 12.Fan W. Epidemiology in diabetes mellitus and cardiovascular disease. Cardiovasc Endocrinol. 2017;6:8–16. doi: 10.1097/XCE.0000000000000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rodriguez-Araujo G, Nakagami H. Pathophysiology of cardiovascular disease in diabetes mellitus. Cardiovasc Endocrinol Metab. 2018;7:4–9. doi: 10.1097/XCE.0000000000000141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hedayatnia M, Asadi Z, Zare-Feyzabadi R, Yaghooti-Khorasani M, Ghazizadeh H, Ghaffarian-Zirak R, et al. Dyslipidemia and cardiovascular disease risk among the MASHAD study population. Lipids Health Dis. 2020;19:42. doi: 10.1186/s12944-020-01204-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wengrofsky P, Lee J, Makaryus AN. Dyslipidemia and its role in the pathogenesis of atherosclerotic cardiovascular disease: Implications for evaluation and targets for treatment of dyslipidemia based on recent guidelines. Dyslipidemia. IntechOpen. 2019 [Google Scholar]
- 16.Akil L, Ahmad HA. Relationships between obesity and cardiovascular diseases in four southern states and Colorado. J Health Care Poor Underserved. 2011;22(4 Suppl):61–72. doi: 10.1353/hpu.2011.0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Altowaijri A, Alshehri N, Balkhi B, Alghamdi A. PCV50 economic burden of major cardiovascular diseases and ischemic stroke in Saudi Arabia: A cost of illness study. Value Health. 2020;23:S495–6. [Google Scholar]
- 18.Shahin L, Patel KM, Heydari MK, Kesselman MM. Hyperuricemia and cardiovascular risk. Cureus. 2021;13:e14855. doi: 10.7759/cureus.14855. doi: 10.7759/cureus.14855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aljefree N, Ahmed F. Prevalence of cardiovascular disease and associated risk factors among adult population in the Gulf region: A systematic review. Adv Public Health 2015. 2015:18. [Google Scholar]
- 20.Al-Rubeaan K, Bawazeer N, Al Farsi Y, Youssef AM, Al-Yahya AA, AlQumaidi H, et al. Prevalence of metabolic syndrome in Saudi Arabia-A cross sectional study. BMC Endocr Disord. 2018;18:1–9. doi: 10.1186/s12902-018-0244-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilson PW, D’Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112:3066–72. doi: 10.1161/CIRCULATIONAHA.105.539528. [DOI] [PubMed] [Google Scholar]
- 22.Madhavan MV, Gersh BJ, Alexander KP, Granger CB, Stone GW. Coronary artery disease in patients ≥80 years of age. J Am Coll Cardiol. 2018;71:2015–40. doi: 10.1016/j.jacc.2017.12.068. [DOI] [PubMed] [Google Scholar]
- 23.Kibel A, Lukinac AM, Dambic V, Juric I, Selthofer-Relatic K. Oxidative stress in ischemic heart disease. Oxid Med Cell Longev 2020. 2020 doi: 10.1155/2020/6627144. 6627144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bosch L, Assmann P, de Grauw WJ, Schalk BW, Biermans MC. Heart failure in primary care: Prevalence related to age and comorbidity. Prim Health Care Res Dev. 2019;20:e79. doi: 10.1017/S1463423618000889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mahalle N, Garg MK, Naik SS, Kulkarni MV. Study of pattern of dyslipidemia and its correlation with cardiovascular risk factors in patients with proven coronary artery disease. Indian J Endocrinol Metab. 2014;18:48–55. doi: 10.4103/2230-8210.126532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee JS, Chang PY, Zhang Y, Kizer JR, Best LG, Howard BV. Triglyceride and HDL-C dyslipidemia and risks of coronary heart disease and ischemic stroke by glycemic dysregulation status: The strong heart study. Diabetes Care. 2017;40:529–37. doi: 10.2337/dc16-1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ariyanti R, Besral B. Dyslipidemia associated with hypertension increases the risks for coronary heart disease: A case-control study in Harapan Kita Hospital, National Cardiovascular Center, Jakarta. J Lipids 2019. 2019 doi: 10.1155/2019/2517013. 2517013. [DOI] [PMC free article] [PubMed] [Google Scholar]