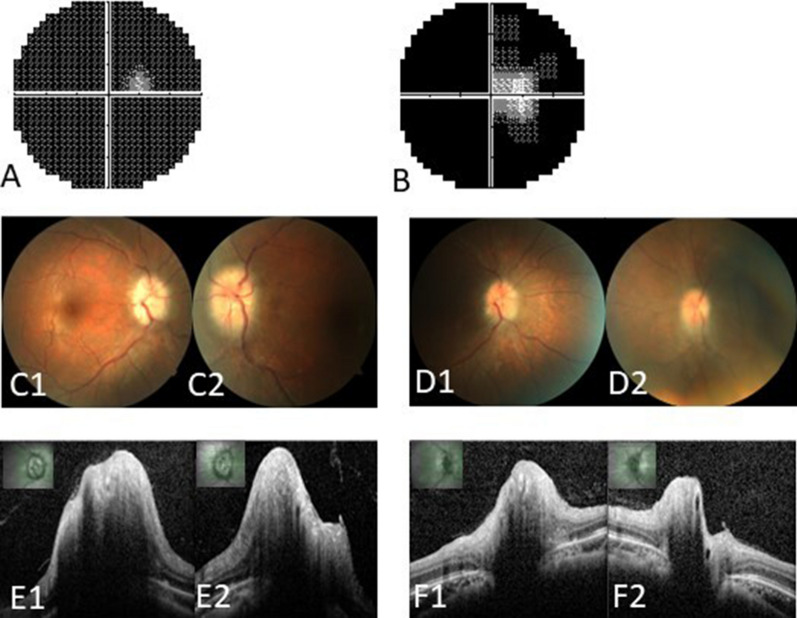
Fig. 1.
The preoperative and postoperative visual findings of a representative case. A 32-year-old female (no. 15) presented with progressive visual loss for 11 months, accompanied by headaches, amaurosis fugax, and tinnitus. She was diagnosed with CVST secondary to thrombocytosis and treated with intravenous heparin and mannitol for 1 month, but her vision loss further progressed. On admission, the BCVA was 20/50 in the right eye and “NLP” in the left, and the right visual field exhibited a tubular aspect (A). Fundus examination revealed papilledema and retinal vein tortuosity in both eyes (C1, C2). Optic disc optic coherence tomography showed bilateral significant papilledema and increased RNFL thickness (E1, E2). Four days after optic nerve sheath fenestration, the BCVA improved to 20/40 in the right and “HM” in the left, and right visual-field defects also improved (B), papilledema noticeably resolved (D1, D2), and bilateral RNFL thickness was decreased (F1, F2). BCVA best-corrected visual acuity, HM hand movement, NLP no light perception, RNFL retinal nerve fiber layer