Abstract
BACKGROUND
Optimal physical activity is known to reduce cardiovascular, respiratory and endocrine system diseases and, as a consequence, improve quality of life. An important risk factor for reinjuries during normal exercise is the initial connective tissue pathology. The variety of clinical dysplastic manifestations significantly complicate the timely diagnosis of this comorbidity.
AIM
To establish pathognomonic sex-specific dysplasia phenotypes that indicate a particular sensitivity to physical exertion.
METHODS
The study involved 117 participants with recurrent musculoskeletal injuries that occurred during normal exercise. There were 67 women (57.26%) and 50 men (42.74%), which made it possible to compare the presence of the identified signs between sexes. A validated questionnaire was used to screen their connective tissue status.
RESULTS
Ranking the most commonly revealed dysplasia signs depending on their clinical significance made it possible to establish pathognomonic sex-specific phenotypes that indicated a particular susceptibility to injuries. Individualized programs of optimal physical activity are necessary for men with chest deformities, flat-valgus feet, dolichostenomelia, arachnodactylia, hemorrhoids, abdominal muscle diastasis and recurrent hernias. In women, special sensitivity to physical exertion was associated with a combination of signs such as asthenic body, joint hypermobility, overly soft auricles, thin hyperelastic skin, atrophic striae, telangiectasias and varicose veins. Of particular importance were universal signs such as gothic palate, scoliosis, kyphosis, leg deformities, temporomandibular joint crunching, and moderate to high myopia.
CONCLUSION
Participants’ connective tissue condition should be considered when designing optimal physical activity programs. Identifying the established sex-specific dysplasia phenotypes will allow timely optimization of training loads, thus reducing the risk of injury.
Keywords: Injury risk, Physical activity, Connective tissue condition, Sex-specific dysplasia phenotypes, Clinical dysplastic manifestations
Core Tip: Ranking the most commonly revealed dysplasia signs depending on their clinical significance made it possible to establish pathognomonic sex-specific phenotypes that indicate a particular susceptibility to injuries. Individualized programs of optimal physical activity are necessary for men with chest deformities, flat-valgus feet, dolichostenomelia, arachnodactylia, hemorrhoids, abdominal muscle diastasis and recurrent hernias. In women, special sensitivity to physical exertion was associated with a combination of signs such as asthenic body, joint hypermobility, overly soft auricles, thin hyperelastic skin, atrophic striae, telangiectasias and varicose veins. Identifying the established sex-specific dysplasia phenotypes will allow timely optimization of training loads and prescription of therapeutic measures aimed at connective tissue strengthening that will reduce the injury risk during physical activity and improve public health.
INTRODUCTION
Increasing physical activity in the population and promoting a healthy lifestyle are among the priorities of preventive measures in the health-care system[1-4]. Optimal and regular exercise is known to reduce cardiovascular, respiratory and endocrine system diseases and, as a consequence, improve the quality and duration of life[5-7]. A healthy lifestyle and the desire to maintain an optimal body functional state through increased physical activity and sports are becoming an integral part of the modern person’s life, even during the coronavirus disease 2019 pandemic[8-12]. However, physical activity is invariably associated with injury risk, and professional sports are associated with the possible occurrence of musculoskeletal posttraumatic chronic conditions as a result of reinjuries[13-15].
Recently, there has been an increase in the number of cases involving sprains and ruptures of the joint ligament apparatus, dislocations and tendon injuries occurring during normal physical activity[15-19]. An important risk factor for this kind of reinjury is connective tissue pathology, the prevalence of which reaches 85.4% in the population[20-24]. Connective tissue changes caused by impaired synthesis or increased degradation of its components result in its inability to withstand full mechanical load[24,25]. The clinico-morphological manifestations of this pathology are quite variable and exhibit significant differences between sexes[22,23]. In this regard, an individualized approach to connective tissue assessment and optimal physical activity program design, taking into account sex-specific features of the dysplastic signs set, becomes relevant. Therefore, the purpose of this study was to establish pathognomonic sex-specific injury phenotypes for consideration when designing exercise programs that support optimal physical activity in men and women.
MATERIALS AND METHODS
Study design and participants
The study, conducted at Sechenov University and European Osteopathic Clinical Center and in accordance with STROBE guidelines, involved 117 participants with recurrent musculoskeletal injuries that occurred during normal physical activity in the absence of a pronounced traumatic factor. Musculoskeletal injuries of varying severity included sprains and ruptures of the joint ligament apparatus, dislocations and tendon tears. All participants, aged 26 to 47 years (average 36.4 ± 6.0 years), underwent a complete clinico-instrumental examination in the period from 2019 to 2022. There were 67 women (57.4%) and 50 men (42.6%), which made it possible to compare the identified dysplasia signs between sexes. Using the statistical package G* (EM) Power (Christian Albrechts-Universität, Olshausenstr, Germany)[26], it was determined that 21 was the minimum sample size required for each group for a statistical power of 85% and alpha criterion of 0.05. The formula and the calculations are shown in Figure 1.
Figure 1.
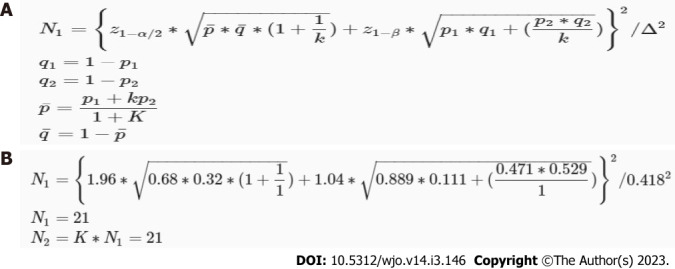
Minimum sample size calculation. A: Formula; B: Calculation process for this study. p1, p2: Proportion (incidence) of groups #1 and #2; Δ = |p2-p1| = absolute difference between two proportions; n1: Sample size for group #1; n2: Sample size for group #2; α: Probability of type I error; β: Probability of type II error; z: Critical Z value for a given α or β; K: Ratio of sample size for group #2 to group #1.
Clinico-instrumental examination
The standard clinico-instrumental therapeutic examination was supplemented with an assessment of anthropometric parameters, such as body height and weight, chest volume, arm span, lower body segment, zygomatic width, face height, and hand and foot length. The facial index (the ratio of the facial height to the zygomatic diameter) was calculated to evaluate the facial skeleton. The Verveck (the ratio of height to the sum of twice the body weight and chest circumference) and Pignet (the difference in height and the sum of body weight and chest circumference) indices were calculated to assess body proportionality. The Varga (the difference between the ratio of body weight to height and age to 100) and Quetelet (the ratio of body weight to squared height) indices were calculated to reveal body weight deficiency. The indices of hand length/height ratios, foot length/height ratios, arm span/height ratios, and upper body/lower body ratios made it possible to diagnose dolichostenomelia features[20,21]. Middle finger length and thumb and wrist tests were used to detect arachnodactyly, and Bayton’s criteria were used to establish joint hypermobility[27-29]. Examinations also included ophthalmic consultation, fibrogastroduodenoscopy, ultrasound, and radiography. The revealed dysplasia signs were registered in a specially developed validated questionnaire[21] based on the Kadurina and Abbakumova[29] scale, in which each sign is assessed from 0 to 4 points.
Ethical considerations
The study complied with the Helsinki Declaration norms and was fully approved by the Local Ethics Committee of the I.M. Sechenov First Moscow State Medical University under protocol No. 08-19 on 05.06.2019. All participants gave informed consent before the study.
Statistical analysis
Comparative analysis and ranking of the revealed signs of dysplasia were carried out using RStudio Desktop (RStudio, Boston, MA, United States). The minimum sample size required for this study was calculated by power analysis. Intergroup qualitative indicators were compared using Pearson’s χ-square test and Fisher’s exact test. Differences were considered to be significant when P < 0.05. The results were counted twice by two independent researchers.
RESULTS
Body proportionality assessment
One of the leading clinico-morphological manifestations of connective tissue pathology is the asthenic body type identified by calculating special indices (Verveck, Pignet, Varga, and Quetelet indices) and characterized by significant longitudinal size predominance and mass deficit. This constitutional type was reliably more common among women with musculoskeletal reinjuries (Figure 2A).
Figure 2.
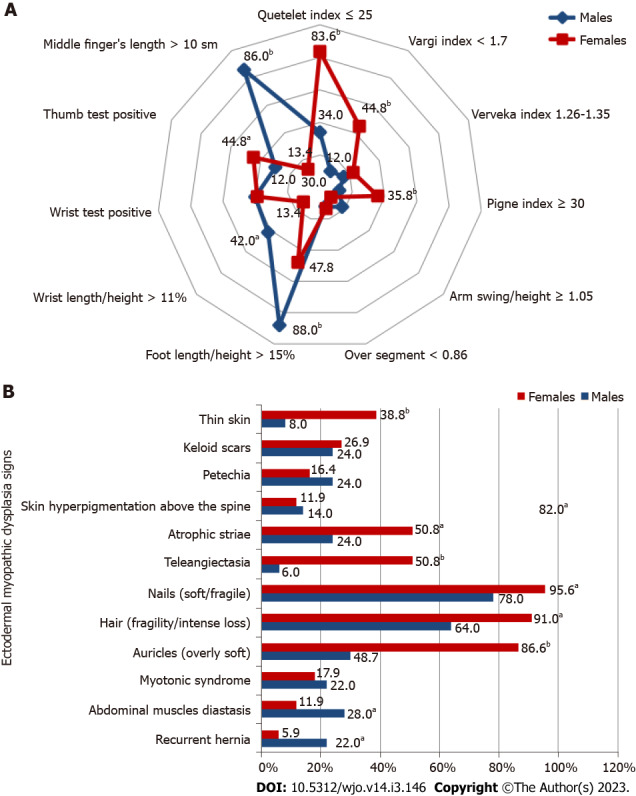
Body proportionality assessment, ectodermal and myopathic sign assessment in persons with musculoskeletal reinjuries. A: Body proportionality assessment; B: Ectodermal and myopathic sign assessment. aP < 0.05, the differences are significant; bP < 0.001, the differences are highly significant.
The data presented in the chart show that men with musculoskeletal disorders were significantly more likely than women to have disproportionately long hands and feet, indicating the presence of dolichostenomelia. Arachnodactyly manifested by long, thin, “spider” fingers was also significantly more common in men in terms of middle finger length. Notably, there was a higher rate of positive thumb tests in women with musculoskeletal reinjuries.
Osteoarticular dysplasia sign assessment
The results of this study are summarized in Figure 3A. Skeletal connective tissue damage in most persons with musculoskeletal reinjuries manifests sex-independent changes such as gothic palate, scoliosis, kyphosis, and X- and O-shaped legs. Spinal pathology, altered leg shapes and, as a consequence, incorrect motor patterns caused pronounced biomechanical disorders and led to shoulder and shoulder blade asymmetry in most subjects regardless of sex. The majority of women, in contrast to men, also had pelvic bone asymmetry. Over half of the participants reported joint crunching during their movements, and half of the patients were affected by TMJ crunching. Compared to that in women, the external phenotype in men with musculoskeletal postexercise disorders was significantly more often formed by chest deformities, first toe macrodactyly, and flat feet in combination with valgus foot placement. Women, in turn, were more likely to have joint hypermobility.
Figure 3.
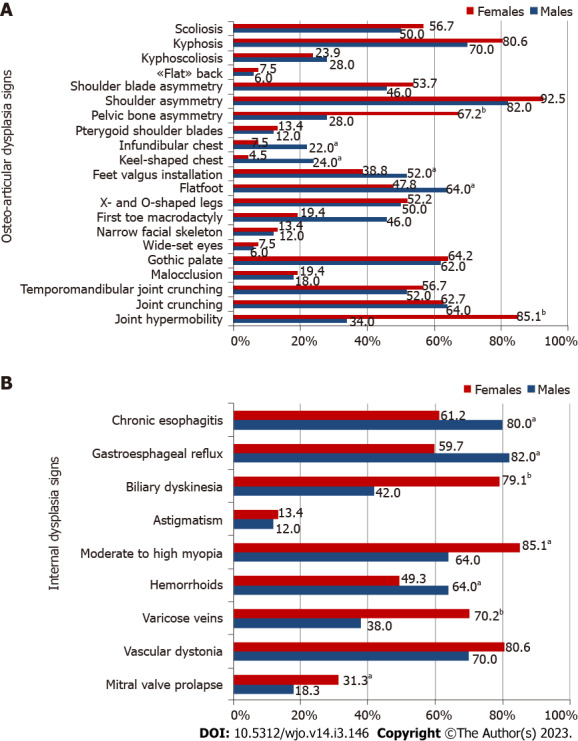
Assessment of osteoarticular dysplasia signs and internal dysplasia signs in persons with musculoskeletal reinjuries. A: Assessment of osteoarticular dysplasia signs; B: Assessment of internal dysplasia signs. aP < 0.05, the differences are significant; bP < 0.001, the differences are highly significant.
Assessment of ectodermal and myopathic dysplasia signs
Ectodermal dysplasia signs such as thin hyperelastic skin with a well-visible vessel network, overly soft auricles, atrophic striae, telangiectasias, and nail and hair pathology were more prevalent in women. In addition, abdominal muscle diastasis and recurrent hernia were more typical for men (Figure 2B).
Internal dysplasia sign assessment
The results indicated that most participants with musculoskeletal reinjuries presented vascular dystonia, the incidence of which was shown to have a sex-independent distribution. Mitral valve prolapse, varicose veins and biliary dyskinesia were more common in women, while hemorrhoids, gastroesophageal reflux and chronic esophagitis were often observed in men. A specific sign of connective tissue pathology is moderate to high myopia, which was diagnosed in most men and women with postexercise musculoskeletal disorders, with a significant prevalence in the second subgroup (Figure 3B).
Ranking clinical significance of revealed dysplasia signs
Ranking the most common revealed dysplasia signs depending on their clinical significance made it possible to establish pathognomonic sex-specific phenotypes that indicate a particular susceptibility to injuries. Individual programs of optimal physical activity are necessary for men with chest deformities, flat-valgus feet, dolichostenomelia, arachnodactylia, hemorrhoids, abdominal muscle diastasis and recurrent hernias. In women, special sensitivity to physical exertion was associated with a combination of such signs as asthenic body, joint hypermobility, overly soft auricles, thin hyperelastic skin, atrophic striae, telangiectasias and varicose veins. Of particular importance are universal signs such as gothic palate, scoliosis, kyphosis, leg deformities, temporomandibular joint crunching, and moderate to high myopia (Figure 4).
Figure 4.
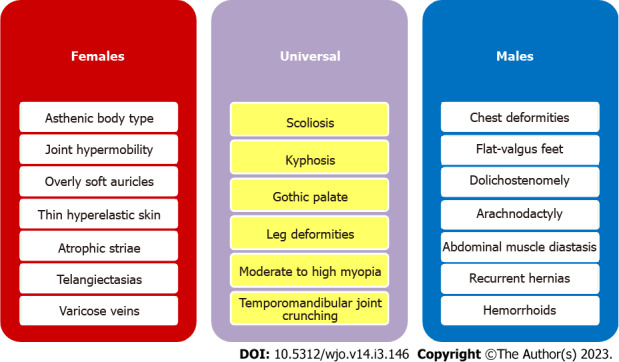
Pathognomonic sex-specific and universal injury predictors.
DISCUSSION
At present, sports medicine is of particular importance in the regular medical-biological support of people engaged in physical exercise and sports[30-33]. The main tasks of sports physicians and physical education specialists are a reasonable choice of sports activities, timely correction of training load, and prevention of injuries and posttraumatic conditions[34-37]. The optimal physical activity program is individually designed for each person and primarily depends on their initial health state. Of particular importance is the detection of connective tissue pathology, which determines the increased sensitivity to mechanical stress, creates injury predisposition and impairs connective tissue recovery in the posttraumatic period, causing further injury recurrence[20,21].
For the first time, significant sex differences in the prevalence of certain connective dysplasia signs were revealed in persons with musculoskeletal reinjuries. Indeed, while bone and myopathic dysplasia signs were significantly more common in men, the prevalence of skin dysplasia signs and joint hypermobility was noted in women. There is evidence that sex differences in dysplastic phenotypes are largely due to exposure to sex hormones: If testosterone gives greater strength to the connective tissue by stimulating fibroplastic reactions, then estrogen causes its excessive elasticity and extensibility, contributing to the appearance of deformity. This explains the greater percentage of overly soft auricles, thin hyperelastic skin, and atrophic striae in women. Vascular wall failure is manifested by telangiectasias and varicose veins. Overstretching of the most powerful ligaments connecting the lumbar spine and the pelvic bones leads to their inability to firmly fix articular surfaces and form pelvic bone asymmetry, which is more common in women.
The influence of female sex hormones is also responsible for the higher incidence of joint hypermobility in the female population, as confirmed by other studies[25]. Increased amplitude of movement in the carpometacarpal and metacarpophalangeal joints in women causes more frequent positive wrist tests in them. The presence of pathological mobility in the joints naturally leads to the appearance of unnatural movements in most loaded joints during increased physical activity and chronic injury[36].
The pathogenetic mechanism of musculoskeletal reinjury in men with connective tissue dysplasia is more associated with skeletal system involvement in the dysplastic process and pathological motor stereotype formation, leading to degenerative-dystrophic changes in the joints and a tendency toward chronic injuries. Significant changes in the composition of glycosaminoglycans and type I and III collagen of the anterior abdominal wall cause an increase in the proportion of muscle diastasis and recurrent hernias[25].
The obtained data necessitate the development of a differentiated approach to dysplasia sign assessment and connective tissue pathology diagnosis in men and women engaged in physical exercise and sports. At the same time, the current recommendations for identifying dysplastic phenotypes do not take into account the sex of the examined subject[22,37].
One of our study limitations was the relatively small number of participants, which may affect the reliability level of the results. In future studies, we will recruit more subjects. Another limitation is that the study was conducted in one clinical center and among individuals with a large age range. For this reason, this study and its results must be understood as the initial stage of multicenter research for developing measures to prevent sports injuries.
CONCLUSION
The connective tissue condition should be taken into account when attempting to design an optimal physical activity program. It is advisable to develop a differentiated approach to dysplasia sign assessment and connective tissue pathology diagnosis in men and women engaged in physical exercise and sports. Identifying the established sex-specific dysplasia phenotypes will allow timely optimization of training loads and prescription of therapeutic measures aimed at connective tissue strengthening that will reduce injury risk during physical activity and improve public health.
ARTICLE HIGHLIGHTS
Research background
At present, sports medicine is of particular importance in the regular medical-biological support of people engaged in physical exercise and sports. Of particular importance is the detection of connective tissue pathology, which determines the increased sensitivity to mechanical stress, creates injury predisposition and impairs connective tissue recovery in the posttraumatic period, causing further injury recurrence.
Research motivation
This study was created because existing methods often do not take into account differentiated approaches to dysplasia sign assessment and connective tissue pathology diagnosis in men and women and is therefore aimed at filling this gap and creating approaches that complement existing ones.
Research objectives
The purpose of this work was to establish pathognomonic sex-specific injury phenotypes for consideration when designing exercise programs that support optimal physical activity in men and women. The results of the study were conceived as an addition to the existing methods of assessing the risk of further injury recurrence.
Research methods
In our study, we measured 117 participants with recurrent musculoskeletal injuries that occurred during normal physical activity in the absence of a pronounced traumatic factor. Musculoskeletal injuries of varying severity included sprains and ruptures of the joint ligament apparatus, dislocations and tendon tears. Anthropometric parameters and indices indicating the presence of signs of connective tissue dysplasia were studied. An analysis was also performed to identify differences in the presence of signs between sexes. A validated questionnaire was used to screen the connective tissue state.
Research results
In our research, we studied the ranking of the most commonly revealed dysplasia signs depending on their clinical significance, making it possible to establish pathognomonic sex-specific phenotypes that indicate a particular susceptibility to injuries.
Research conclusions
The study results are of particular importance in the context of physical culture and sport safety and emphasize the importance of a differentiated approach of medico- biological support of sports activities in men and women.
Research perspectives
To further develop these findings, it is possible to conduct a larger-scale study with a larger number of participants. Further refinement of the sex-specific dysplasia phenotypes is needed for clarification and, possibly, expansion of these findings. With satisfactorily refined results, it is possible to introduce the proposed methodology into practice for a clinical trial.
Footnotes
Institutional review board statement: The current research study was approved by the Ethics Committee of I.M. Sechenov First Moscow State Medical University (Sechenov University) under protocol No. 08-19 on 05.06.2019.
Informed consent statement: Informed consent was obtained from the participants included in this study.
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: October 17, 2022
First decision: January 3, 2023
Article in press: February 27, 2023
Specialty type: Orthopedics
Country/Territory of origin: Russia
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chaturvedi HTC, India; Rakhshan V, Iran; Shalaby MN, Egypt S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
Contributor Information
Maria V Sankova, Department of Human Anatomy and Histology, I.M. Sechenov First Moscow State Medical University (Sechenov University), Moscow 125009, Russia.
Vladimir N Nikolenko, Department of Human Anatomy and Histology, I.M. Sechenov First Moscow State Medical University (Sechenov University), Moscow 125009, Russia; Department of Normal and Topographic Anatomy, Lomonosov Moscow State University, Moscow 119991, Russia.
Marine V Oganesyan, Department of Human Anatomy and Histology, I.M. Sechenov First Moscow State Medical University (Sechenov University), Moscow 125009, Russia; Department of Normal and Topographic Anatomy, Lomonosov Moscow State University, Moscow 119991, Russia.
Andjela D Vovkogon, Department of Human Anatomy and Histology, I.M. Sechenov First Moscow State Medical University (Sechenov University), Moscow 125009, Russia; European Osteopathic Clinical Center of the Moscow Branch of the “Medical Academy of Osteopathic Education”, Saint Petersburg 199106, Russia.
Aida N Gadzhiakhmedova, Institute of Clinical Medicine, I.M. Sechenov First Moscow State Medical University (Sechenov University), Moscow 119991, Russia.
Tatyana S Zharikova, Department of Human Anatomy and Histology, I.M. Sechenov First Moscow State Medical University (Sechenov University), Moscow 125009, Russia; Department of Normal and Topographic Anatomy, Lomonosov Moscow State University, Moscow 119991, Russia.
Yury O Zharikov, Department of Human Anatomy and Histology, I.M. Sechenov First Moscow State Medical University (Sechenov University), Moscow 125009, Russia. dr_zharikov@mail.ru.
Data sharing statement
No additional data are available.
References
- 1.Dorner TE, Wolner-Strohmeyer G, Katzenbeisser C, Lackinger C, Stein KV. Physical Activity as Part of an Intramural Health Promotion Programme for People with and without Chronic Diseases. A New Tool in Health Care Run by a Public Social Health Insurance. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17207491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stonerock GL, Blumenthal JA. Role of Counseling to Promote Adherence in Healthy Lifestyle Medicine: Strategies to Improve Exercise Adherence and Enhance Physical Activity. Prog Cardiovasc Dis. 2017;59:455–462. doi: 10.1016/j.pcad.2016.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Serra MC, Dondero KR, Larkins D, Burns A, Addison O. Healthy Lifestyle and Cognition: Interaction between Diet and Physical Activity. Curr Nutr Rep. 2020;9:64–74. doi: 10.1007/s13668-020-00306-4. [DOI] [PubMed] [Google Scholar]
- 4.Fletcher GF, Landolfo C, Niebauer J, Ozemek C, Arena R, Lavie CJ. Reprint of: Promoting Physical Activity and Exercise: JACC Health Promotion Series. J Am Coll Cardiol. 2018;72:3053–3070. doi: 10.1016/j.jacc.2018.10.025. [DOI] [PubMed] [Google Scholar]
- 5.Vaughan CA, Ghosh-Dastidar M, Dubowitz T. Attitudes and Barriers to Healthy Diet and Physical Activity: A Latent Profile Analysis. Health Educ Behav. 2018;45:381–393. doi: 10.1177/1090198117722818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keadle SK, Conroy DE, Buman MP, Dunstan DW, Matthews CE. Targeting Reductions in Sitting Time to Increase Physical Activity and Improve Health. Med Sci Sports Exerc. 2017;49:1572–1582. doi: 10.1249/MSS.0000000000001257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thandi MKG, Phinney A, Oliffe JL, Wong S, McKay H, Sims-Gould J, Sahota S. Engaging Older Men in Physical Activity: Implications for Health Promotion Practice. Am J Mens Health. 2018;12:2064–2075. doi: 10.1177/1557988318792158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Filgueira TO, Castoldi A, Santos LER, de Amorim GJ, de Sousa Fernandes MS, Anastácio WLDN, Campos EZ, Santos TM, Souto FO. The Relevance of a Physical Active Lifestyle and Physical Fitness on Immune Defense: Mitigating Disease Burden, With Focus on COVID-19 Consequences. Front Immunol. 2021;12:587146. doi: 10.3389/fimmu.2021.587146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eek F, Larsson C, Wisén A, Ekvall Hansson E. Self-Perceived Changes in Physical Activity and the Relation to Life Satisfaction and Rated Physical Capacity in Swedish Adults during the COVID-19 Pandemic-A Cross Sectional Study. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18020671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dwyer MJ, Pasini M, De Dominicis S, Righi E. Physical activity: Benefits and challenges during the COVID-19 pandemic. Scand J Med Sci Sports. 2020;30:1291–1294. doi: 10.1111/sms.13710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carvalho VO, Gois CO. COVID-19 pandemic and home-based physical activity. J Allergy Clin Immunol Pract. 2020;8:2833–2834. doi: 10.1016/j.jaip.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jimeno-Almazán A, Pallarés JG, Buendía-Romero Á, Martínez-Cava A, Franco-López F, Sánchez-Alcaraz Martínez BJ, Bernal-Morel E, Courel-Ibáñez J. Post-COVID-19 Syndrome and the Potential Benefits of Exercise. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18105329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nauta J, Martin-Diener E, Martin BW, van Mechelen W, Verhagen E. Injury risk during different physical activity behaviours in children: a systematic review with bias assessment. Sports Med. 2015;45:327–336. doi: 10.1007/s40279-014-0289-0. [DOI] [PubMed] [Google Scholar]
- 14.Zwolski C, Quatman-Yates C, Paterno MV. Resistance Training in Youth: Laying the Foundation for Injury Prevention and Physical Literacy. Sports Health. 2017;9:436–443. doi: 10.1177/1941738117704153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wojtys EM. Sports Injury Prevention. Sports Health. 2017;9:106–107. doi: 10.1177/1941738117692555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tarasov AV, Belichenko OI, Smolensky AV. Injuries and diseases of the musculoskeletal system in athletes (literature review) Therapist. 2019;5:4–14. [Google Scholar]
- 17.Plotnikova YA, Erlikh VV. Physiological muscle reactivity in the process of recovery measures after injuries of the musculoskeletal system. [cited 17 August 2022]. Avaliable from: https://www.elibrary.ru/item.asp?edn=icyugh . [Google Scholar]
- 18.Bakulin VS, Gretskaya IB, Bogomolova MM, Bogachev AN. Sportivnyy travmatizm. Profilaktika i reabilitatsiya [Sports injuries. Prevention and rehabilitation] Volgograd. 2013:190. [Google Scholar]
- 19.Wilke J, Groneberg DA. Neurocognitive function and musculoskeletal injury risk in sports:A systematic review. J Sci Med Sport. 2022;25:41–45. doi: 10.1016/j.jsams.2021.07.002. [DOI] [PubMed] [Google Scholar]
- 20.Nikolenko V, Oganesyan M, Vovkogon A, Sankova M, Rizaeva N. Morphological markers of structural and functional disorders of the musculoskeletal system arising after physical activity. Hum Sport Med. 2019;19:103–111. [Google Scholar]
- 21.Nikolenko VN, Oganesyan MV, Vovkogon AD, Cao Y, Churganova AA, Zolotareva MA, Achkasov EE, Sankova MV, Rizaeva NA, Sinelnikov MY. Morphological signs of connective tissue dysplasia as predictors of frequent post-exercise musculoskeletal disorders. BMC Musculoskelet Disord. 2020;21:660. doi: 10.1186/s12891-020-03698-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martynov AI, Nechaeva GI. Guidelines of the Russian scientific medical society of internal medicine on the diagnosis, treatment and rehabilitation of patients with the connective tissue dysplasia (first edition) Med News North Cauc. 2018;13 [Google Scholar]
- 23.Akimova A, Mironov V, Gagiev V, Tarasova E, Palabugina P, Khusainova D, Talankina A. Features of the clinic and autonomic regulation of sinus rhythm of the heart in individuals with undifferentiated connective tissue dysplasia. Bull Ural Med Acad Sci. 2017;14:315–324. [Google Scholar]
- 24.Arseni L, Lombardi A, Orioli D. From Structure to Phenotype: Impact of Collagen Alterations on Human Health. Int J Mol Sci. 2018;19 doi: 10.3390/ijms19051407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sankova MV, Nikolenko VN, Oganesyan MV, Vovkogon AD, Chirkova EL, Sinelnikov MY. Age Pathognomonic Indicators of Injury Predisposition as a Basis for Public Health Preservation during Physical Activity. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18041989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 27.Castori M, Hakim A. Contemporary approach to joint hypermobility and related disorders. Curr Opin Pediatr. 2017;29:640–649. doi: 10.1097/MOP.0000000000000541. [DOI] [PubMed] [Google Scholar]
- 28.Kumar B, Lenert P. Joint Hypermobility Syndrome: Recognizing a Commonly Overlooked Cause of Chronic Pain. Am J Med. 2017;130:640–647. doi: 10.1016/j.amjmed.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 29.Kadurina T, Abbakumova L. Assessment of the severity of undifferentiated connective tissue dysplasia in children. Med Bull North Caucasus. 2008;2:15–20. [Google Scholar]
- 30.Kiselev OA, Iurchenko NI. Enhancement of state support mechanisms for sports in the Russian Federation. Ars Administrandi. 2020;1:25–43. [Google Scholar]
- 31.Pujalte GGA, Maynard JR. The increasing importance of sports science and medicine. J Int Med Res. 2020;48:300060519827694. doi: 10.1177/0300060519827694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frank RM, Bradsell H, Thompson SR. What’s new in sports medicine. J Bone Joint Surg Am. 2021;103:653–659. doi: 10.2106/JBJS.21.00152. [DOI] [PubMed] [Google Scholar]
- 33.Chang TJ. Sports Medicine. Clin Podiatr Med Surg. 2023;40:xiii–xxiv. doi: 10.1016/j.cpm.2022.10.001. [DOI] [PubMed] [Google Scholar]
- 34.Neunhaeuserer D, Niebauer J, Degano G, Baioccato V, Borjesson M, Casasco M, Bachl N, Christodoulou N, Steinacker JM, Papadopoulou T, Pigozzi F, Ermolao A. Sports and exercise medicine in Europe and the advances in the last decade. Br J Sports Med. 2021;55:1122–1124. doi: 10.1136/bjsports-2021-103983. [DOI] [PubMed] [Google Scholar]
- 35.Kweon CY, Hagen MS, Gee AO. What's New in Sports Medicine. J Bone Joint Surg Am. 2020;102:636–643. doi: 10.2106/JBJS.20.00014. [DOI] [PubMed] [Google Scholar]
- 36.Vorotnikov AA, Tsymbal AN, Next AA, Saneeva GA. Pathology of the musculoskeletal system in connective tissue dysplasia syndrome. Med Bull North Cauc. 2012;3:96–100. [Google Scholar]
- 37.Zemtsovskyi EV, Malev EG, Reeva SV, Luneva EB, Parfenova NN, Lobanov MYu, Belyaeva EL, Vyutrikh EV, Timofeev EV, Belousova TI, Bergmane OA, Zaripov BI, Korshunova AL, Pankova IA. Diagnostics of inherited connective tissue disorders: achievements and future directions. Russian J Cardiol. 2013;102:38–43. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No additional data are available.


