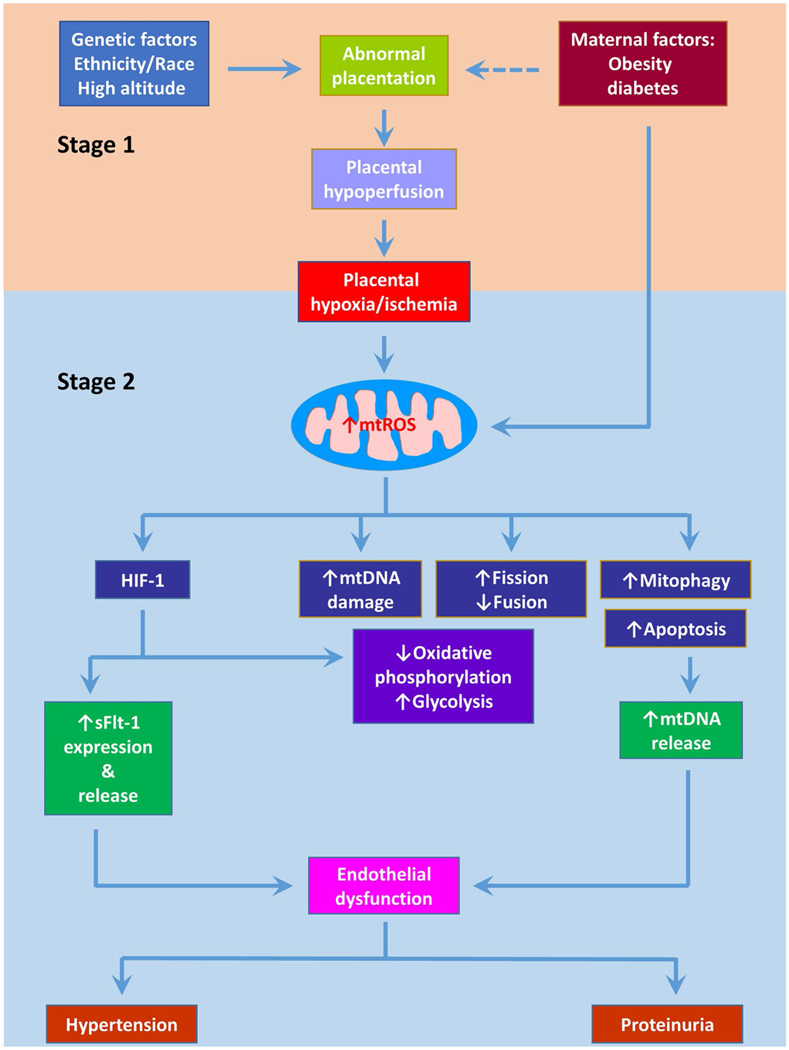
Fig. 1.
Association of mitochondrial dysfunction with preeclampsia. Preeclampsia is proposed to occur in two stages. In the first stage, incomplete spiral artery remodeling causes reduced placental perfusion. In the second stage, the resultant placental hypoxia/ischemia or hypoxia/reoxygenation induces oxidative stress which in turn boosts the release of bioactive factors, leading to endothelial dysfunction and ultimately clinical symptoms such as hypertension and proteinuria. Accumulating evidence suggests mitochondrial dysfunction plays a central role in the pathogenesis of preeclampsia. Placental hypoxia/ischemia-induced mitochondrial reactive oxygen species (mtROS) overproduction apparently is the major player of mitochondrial dysfunction by promoting mtDNA damage and mtDNA release into the circulation, altering mitochondrial dynamics and mitophagy, and increasing apoptosis. mtROS also stabilizes HIF-1 in the placenta which then reprograms metabolism and stimulates sFlt-1 expression and release into the circulation. sFlt-1 and mtDNA along with other bioactive factors initiate systemic inflammation and endothelial dysfunction, engendering preeclamptic phenotype