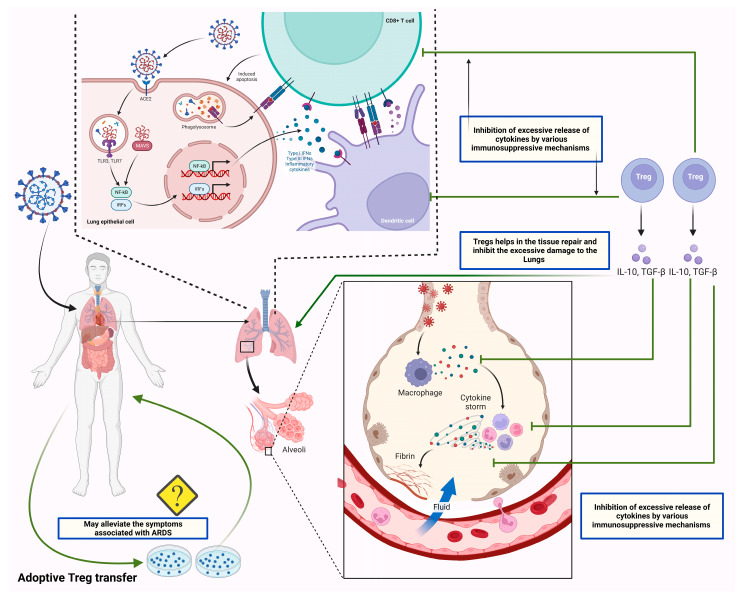
Figure 4.
The figure shows the therapeutic potential of Tregs by suppressing the exaggerated immune response. SARS-CoV-2 infects the lung epithelial cells by entering through ACE2 receptors. SARS-CoV-2 infects lung epithelial cells by using ACE2 receptors. As viral RNA enters the cell, it activates endosomal and cytoplasmic sensors, including TLR3/7 and MAVS. Further, these endosomal and cytoplasmic receptors activate IRFs and NFkB, resulting in the production of inflammatory cytokines such as interferons (IFN). Dendritic cells acquire antigen before migrating to lymphoid organs to activate adaptive immunity. Following the recognition of antigens on antigen-presenting cells (APCs) or infected cells, CD8 T lymphocytes trigger apoptosis. Additionally, the viral antigens present to the T cells through antigen processing. Antigen processing is the process through which APCs, such as dendritic cells and alveolar macrophages, endocytose and kill the SARS-CoV-2 virus. MHC proteins then express antigen fragments on the cell membrane, enabling T lymphocytes to identify them. The overstimulated T cells and APCs in severely infected patients lead to excessive secretion of cytokines/chemokines, which leads to lung damage and ARDS. The balanced concentration of Tregs can suppress the exaggerated immune response through its immunoregulatory and immunosuppressive activities. In this context, recent studies suggested the beneficial effects of the adoptive transfer of Tregs in severely infected patients, which is yet to be approved for its clinical safety.