Abstract
Hypertension is highly prevalent in the United States, and many persons with hypertension do not have controlled blood pressure. Self-measured blood pressure monitoring (SMBP), when combined with clinical support, is an evidence-based strategy for lowering blood pressure and improving control in persons with hypertension. For years, there has been support for widespread implementation of SMBP by national organizations and the federal government, and SMBP was highlighted as a primary intervention in the 2020 Surgeon General’s Call to Action to Control Hypertension, yet optimal SMBP use remains low. There are well-known patient and clinician barriers to optimal SMBP documented in the literature. We explore additional high-level barriers that have been encountered, as broad policy and systems-level changes have been attempted, and offer potential solutions. Collective efforts could modernize data transfer and processing, improve broadband access, expand device coverage and increase affordability, integrate SMBP into routine care and reimbursement practices, and strengthen patient engagement, trust, and access.
Keywords: barriers, blood pressure, cardiovascular disease, health information technology, hypertension, prevention, self-measured blood pressure monitoring
We have a hypertension problem in the United States. It affects all races and ethnicities, age groups, sexes, and presents throughout the country. Using the ACC/AHA 2017 blood pressure guideline defining hypertension as a blood pressure > 130/80 mm Hg, an estimated 47% of US adults (116M) have hypertension, and of those recommended to be on antihypertensive medications and make lifestyle modifications, 74% (68M) do not have controlled blood pressure.1 Uncontrolled blood pressure is a leading cause of heart attack, stroke, heart failure, kidney disease, dementia, and other sequelae. Moreover, hypertensive disorders of pregnancy are increasing in prevalence and raise a woman’s lifetime risk of cardiovascular disease.2–5 Non-Hispanic Black persons develop hypertension at younger ages than non-Hispanic White persons.6 While hypertensive cardiovascular disease mortality rates are increasing for persons aged 35–64 years in the majority of counties in the US, non-Hispanic Black persons carry a disproportionate burden of hypertensive cardiovascular mortality compared to other racial/ethnic groups.7 Additionally, people living in communities with a low socioeconomic status or without insurance are less likely to have controlled hypertension when compared with people with higher socioeconomic status or insurance, respectively.8,9
When combined with clinical support, self-measured blood pressure monitoring (SMBP) is an evidence-based strategy for lowering blood pressure and improving blood pressure control in persons with hypertension.10,11 SMBP, sometimes referred to as home blood pressure monitoring, is the measurement of blood pressure, by an individual with hypertension, outside of the clinical setting, ideally with a clinically validated automatic upper arm device. Optimal SMBP (Figure 1) occurs when a person with hypertension receives training and education on how to select a validated device with an appropriately sized cuff, proper preparation and positioning, frequency of readings and duration of monitoring, and a method for returning patient-generated values. The patient then begins self-measuring their blood pressure at home and transmitting those values, medication side effects, and lifestyle modification information to their clinical team via remote methods. The clinical team receives, processes, and interprets the data and incorporates them into the patient’s care plan by remotely transmitting guidance back to the patient for titration and/or lifestyle modification. This patient–clinician feedback loop continues indefinitely.
Figure 1.
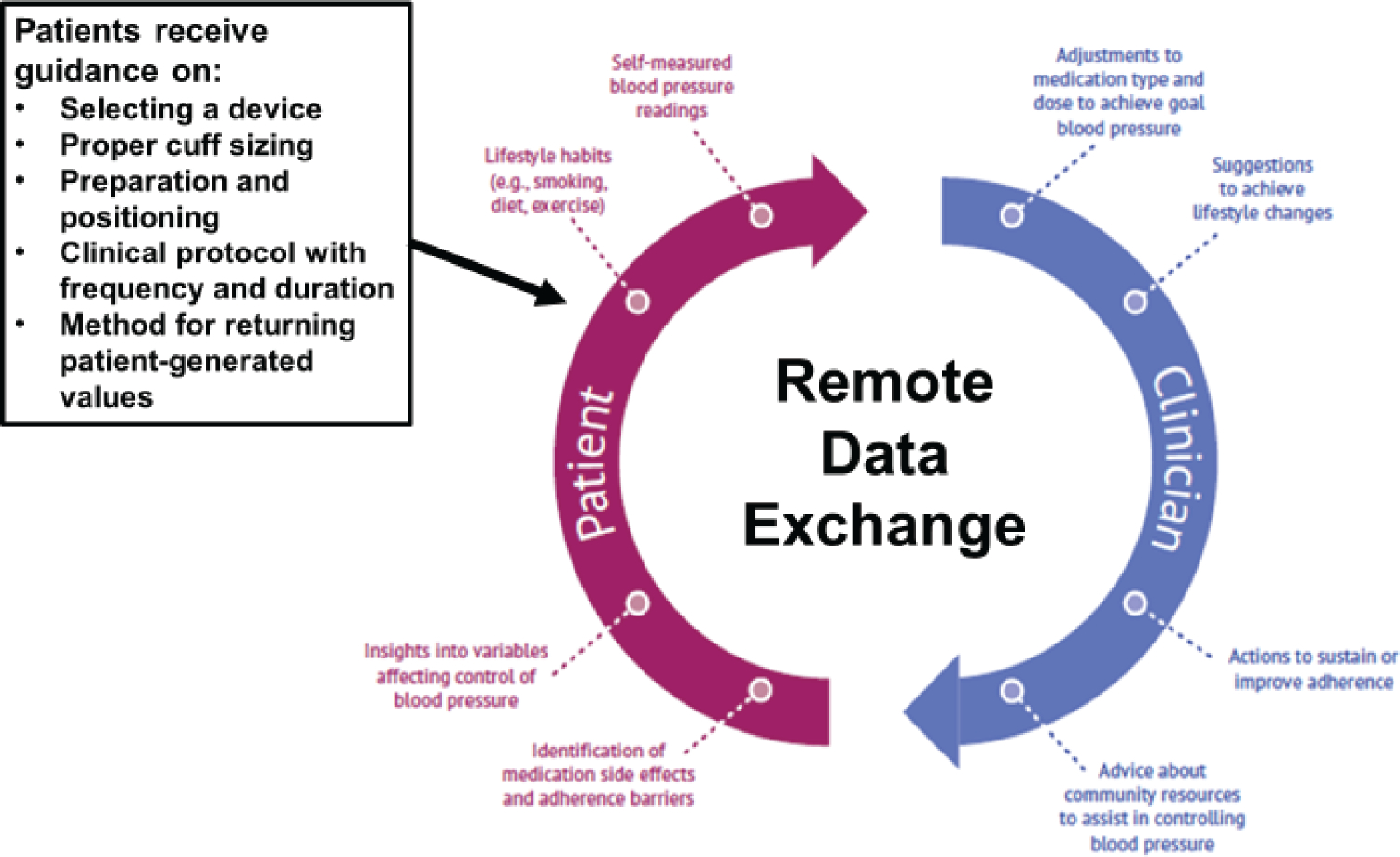
Optimal self-measured blood pressure monitoring (SMBP). Adapted from Centers for Disease Control and Prevention. Self-Measured Blood Pressure Monitoring: Action Steps for Public Health Practitioners. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2013.
SMBP is recommended in numerous US and international clinical guidelines for hypertension management and confirming new hypertension diagnoses.12–16 National health advocacy organizations have published scientific and policy statements on SMBP.17,18 Moreover, Million Hearts, co-led by the Centers for Disease Control and Prevention (CDC) and the Centers for Medicare and Medicaid Services (CMS); the American Medical Association (AMA); Target:BP, a joint effort from AMA and the American Heart Association (AHA); the National Association of Community Health Centers (NACHC); and others have supported the use of SMBP with clinical support for years (Table 1). In 2020, SMBP was highlighted in the Surgeon General’s Call to Action to Control Hypertension as a major strategy for patient engagement to optimize care for hypertension control.19 One immediate result of the Call to Action was the development of the Federal Hypertension Control Leadership Council, comprised of multiple agencies and offices within the US Department of Health and Human Services (HHS), each committed to improving health equity through prevention, detection, and control of hypertension. A major priority of the Federal Hypertension Control Leadership Council is to drive actions that advance the use of SMBP. In 2021, the HHS Office of Minority Health (OMH) and the Health Resources and Services Administration (HRSA) launched the National Hypertension Control Initiative: Addressing Disparities Among Racial and Ethnic Minority Populations. This initiative, in which almost 500 health centers will receive funding and technical assistance to implement optimal SMBP, specifically focuses on patient populations with persistent disparities in hypertension control.20
Table 1.
Select federal and national actions that promote self-measured blood pressure monitoring
| Timeframe | Event |
|---|---|
|
| |
| June 2008 | “Call to action on use and reimbursement for home blood pressure monitoring. A joint scientific statement from the American Heart Association, the American Society for Hypertension, and the Preventive Cardiology Nurses Association” published |
| January 2012 | AHRQ “Self-Measured Blood Pressure Monitoring: Comparative Effectiveness” report released |
| February 2013 | Million Hearts “Self-Measured Blood Pressure Monitoring: Action Steps for Public Health” released |
| December 2014 | Million Hearts “Self-Measured Blood Pressure Monitoring: Action Steps for Clinicians” released |
| February 2015 | AMA/Johns Hopkins School of Medicine “Self-measured Blood Pressure Monitoring Program: Engaging Patients in Self-measurement” released |
| June 2015 | CDC Community Preventive Services Task Force recommendation on SMBP published; found strong evidence supporting its use with clinical support |
| October 2015 | USPSTF “Hypertension in Adults: Screening” recommendation called for using SMBP to confirm new hypertension diagnoses |
| October 2016 to June 2018 | NACHC/Million Hearts Accelerating SMBP project implemented in 9 health centers |
| November 2016 | Target:BP launched by AMA and AHA |
| November 2017 | “ACC/AHA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults” published; recommended using SMBP for diagnosis and management of hypertension |
| June 2020 | “Self-Measured Blood Pressure Monitoring at Home: A Joint Policy Statement from the American Heart Association and American Medical Association” published |
| October 2020 | Surgeon General’s “Call to Action to Control Hypertension” published; SMBP included as a major strategy for patient engagement in hypertension |
| October 2020 | Federal Hypertension Control Leadership Council convened; named advancing SMBP implementation as a priority |
| January 2021 | HHS OMH/HRSA National Hypertension Control Initiative announced; ~500 health centers to be assisted in using SMBP for hypertension management |
Abbreviations: ACC, American College of Cardiology; AHA, American Heart Association; AHRQ, Agency for Healthcare Research and Quality; AMA, American Medical Association; BP, blood pressure; CDC, Centers for Disease Control and Prevention; HHS, Department of Health and Human Services; HRSA, Health Resources & Services Administration; NACHC, National Association of Community Health Centers; OMH, Office of Minority Health; SMBP, self-measured blood pressure monitoring; USPSTF, United States Preventive Services Task Force.
Despite the national attention and a strong evidence base to support its use, optimal SMBP has yet to be widely implemented. Due to heterogeneity in how SMBP is assessed including how it is defined, how often people engage in it, whether readings are transmitted remotely, and whether patient-generated blood pressure readings are incorporated into care plans, it is challenging to fully quantify the current use of optimal SMBP. Small cohort studies have reported that 40–50% of people with hypertension used SMBP “at home.” 21–23 Two assessments of data from the nationally representative National Health and Nutrition Examination Survey reported 41.9% (2009–2010) and 43.5% (2011–2014) prevalence of SMBP use among persons with self-reported hypertension at least monthly.24,25 A more recent analysis from the 2019 Behavioral Risk Factor Surveillance System reported that 61% of people with self-reported hypertension reported using SMBP, with the majority of them (85.6%) using it “at home” and sharing their readings with a health care professional (>85%).26 However, only 6.9% of people who shared their readings with a health care professional did so via remote methods (e.g., internet or email).
Multiple patient- and clinician-perceived barriers have been documented. For patients, these barriers include out-of-pocket costs for blood pressure devices, measurement burden, and lack of competence with technology.27–30 Clinician-perceived barriers include concerns about time needed to instruct patients on an SMBP monitoring protocol, patient compliance, accuracy of results, and patient affordability of home blood pressure devices.31,32 Here we aim to outline high-level barriers we and our federal/national partners have encountered and offer potential solutions to achieve widespread implementation of SMBP. Many of these barriers are pragmatic challenges that have only been realized as broad policy and systems-level changes have been attempted and may not be widely articulated in the published literature (Table 2).
Table 2.
Challenges and potential solutions to support widespread use of self-measured blood pressure monitoring (SMBP)
| Challenges | Potential solution |
|---|---|
|
| |
| Data ownership, privacy, and security as PGHD flow from patients to non-HIPAA-covered entities to HIPAA covered entities. | • Create policies that make device manufacturers, mHealth app creators, and API developers HIPAA-covered entities |
| Complex, underutilized standards for data exchange for SMBP and other kinds of PGHD | • Develop an implementation strategy to drive standards-based PGHD exchange for SMBP and beyond |
| Broadband accessibility and affordability | • Expand high-speed internet to all areas of the United States at affordable costs |
| Patients may need technical assistance to connect their SMBP device to their home internet, download and use necessary apps, and transmit their blood pressure readings | • Create a technical assistance center by leveraging existing workforce development programs. • Create a network of local assistance by funding libraries and other community-based organizations to deliver assistance |
| Confusion over which SMBP devices to purchase | • Implement policies that drive manufacturers to have their devices undergo independent clinical validation |
| Larger than standard adult BP cuff sizes may be difficult to access | • Collaborate with device manufacturers to ensure large and extra-large cuffs are affordable and readily accessible • Create a universal, one-size fits most, blood pressure cuff |
| SMBP device costs | • Improve coverage at sufficient levels • Encourage value-based insurance design • Support device loaner programs |
| Clinician concerns about lack of reimbursement for SMBP-related services | • Raise awareness of CPT codes 99473 and 99474 • Share the related economic case for SMBP |
| Alleviate physician burden related to SMBP; lack of convenient, patient-trusted sources of training and education for SMBP | • Deploy other members of the care team to provide training, education, and support to patients in SMBP • Develop robust community-based models for training, educating, and supporting patients in SMBP |
Abbreviations: API, application programming interface; BP, blood pressure; CPT, Current Procedural Terminology; HIPAA, Health Insurance Portability and Accountability Act; mHealth, mobile health; PGHD, patient-generated health data; SMBP, self-measured blood pressure monitoring.
SIMPLIFIED, STANDARDS-BASED, AND INTEROPERABLE HEALTH INFORMATION TECHNOLOGY TO SUPPORT REMOTE EXCHANGE OF PATIENT-GENERATED BLOOD PRESSURE READINGS
The current health information technology (IT) landscape for SMBP is complicated (Figure 2). SMBP data can take multiple pathways from patients to their electronic health records (EHRs). Some of the stops along the way may involve customized interfaces that may be costly and burdensome to develop. CDC recently collaborated with the Public Health Informatics Institute (PHII) and representatives from other federal agencies to conduct a national assessment of the health IT and health informatics landscape for SMBP data exchange and make recommendations for streamlining it.33 Those recommendations called out a need to strengthen policies and procedures for SMBP and other types of patient-generated health data (PGHD). Among the issues addressed are data ownership, privacy, and security concerns as PGHD flow from patients to non-HIPAA-covered entities, like device manufacturers, mobile health (mHealth) application creators, and application programming interface (API) developers, to HIPAA-covered clinical entities.
Figure 2.
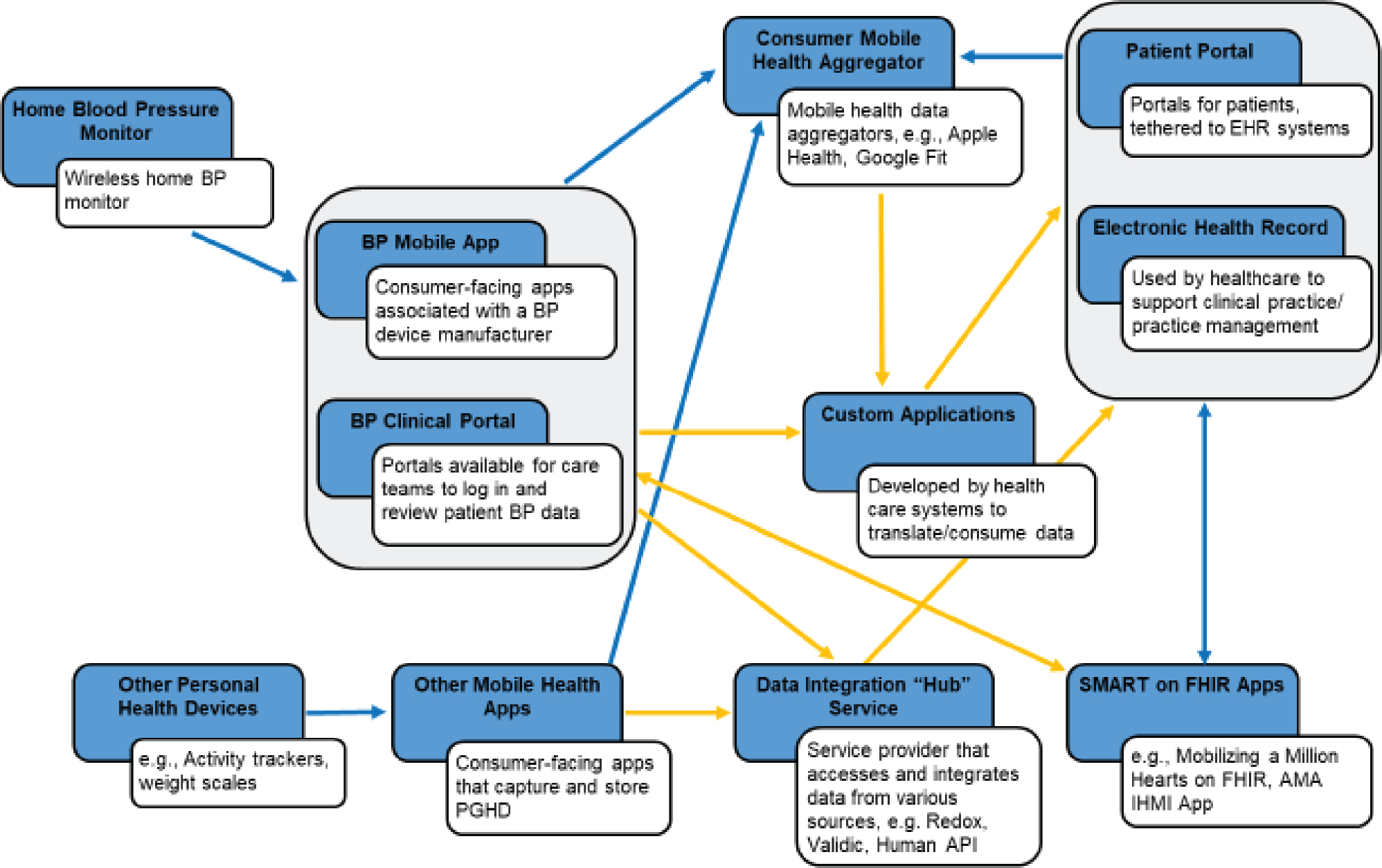
Current health information technology/informatics landscape for self-measured blood pressure monitoring, as of September 2021. Yellow lines are data transmission pathways that could be simplified through standards or other means. Adapted from Public Health Informatics Institute. National Assessment of the Self-Measured Blood Pressure Monitoring (SMBP) Health Information Technology Landscape. September 2021. https://phii.org/SMBP-Health-IT-Landscape.
When clinicians are able to receive patient-generated blood pressure readings, they likely receive a significant amount of data per patient—2 morning readings and 2 nighttime readings each day for 3–7 days for up to 28 readings per monitoring period—and most EHR systems are unable to accept and process these readings into actionable information.34,35 The vital signs section of EHRs should be modified to capture blood pressure value type (e.g., SMBP, office measures, ambulatory blood pressure monitoring, or automated office blood pressures) using structured data fields with dropdown menus, as well as pertinent metadata for each value type (e.g., device type, make, and model). The capability to average blood pressure readings should be a standard functionality as well. By equipping all EHRs with this type of structured data capture, SMBP values could readily be incorporated into clinical decision supports and clinical quality measures, the latter often used in public reporting and incentive programs.
Additionally, there are technical standards and specifications that could enhance and simplify SMBP data exchange with regard to what data elements are being exchanged, in what format, and how. Fast Healthcare Interoperability Resources (FHIR) and Substitutable Medical Applications, Reusable Technologies (SMART), specifically SMART Markers, are 2 relevant standards in this arena.36 Open mHealth is another standard that could advance interoperable, standards-based exchange of PGHD, but there is no current guidance on how best to use these standards to enter PGHD into EHRs. Leadership and better coordination are needed to develop an implementation strategy to drive standards-based PGHD exchange for SMBP and beyond.
READY ACCESS TO HIGH-SPEED BROADBAND
Before patients even begin transmitting data to their clinical team, they need robust access to broadband internet. There are at least 2 major barriers with broadband access: (1) affordability and (2) physical access (i.e., whether high-speed internet is available in a given geography).
The Federal Communications Commission (FCC) and HRSA have spearheaded a variety of efforts to bring affordable internet access to both consumers and clinicians but more can be done.37 Broadband internet access can cost $50–60 per month, with costs varying greatly by delivery type (e.g., Digital Subscriber Line [DSL], cable, or fiber) and internet speed. This includes hidden costs like installation, equipment rental, and data overage fees that currently make broadband cost-prohibitive for many people. Satellite internet is theoretically available in all counties in the US but for those who live in areas where only satellite internet is available, internet access can cost $100 or more per month.38 Rural areas, in general, pay more per megabit per second (Mbps), possibly due to lack of competition or less available infrastructure for sophisticated internet delivery.39 From a lack of competition perspective, 48.3% of US counties have more than half of their population living in areas with fewer than 2 non-satellite broadband providers (Supplementary Figure 1).
Over 40% of US adults with household incomes of <$30k report not having home broadband.39 Using data from the US Census Bureau’s American Community Survey, Figure 3 shows the percent of households that do not purchase a broadband subscription, by county, overlaid with self-reported hypertension prevalence. This map shows 1.3% of counties have >50% of their population with no broadband internet subscription and 22.1% of counties have 30–50% of their population with no broadband internet subscription. These under-resourced areas tend to overlap with areas of high hypertension burden, particularly in the “stroke belt,” where non-Hispanic Black persons comprise ~26% of the population is versus ~10% of the population in the remainder of the US.40 Some households in these counties may have access to the internet through cellular connectivity but almost 1 in 4 adults with household incomes of <$30k do not own smartphones41 and data use limits may be a concern for those who do. While cellular service is generally good through much of the US, there are notable gaps in parts of upstate New York and West Virginia, most of Alaska, and in the western half of the country.42
Figure 3.
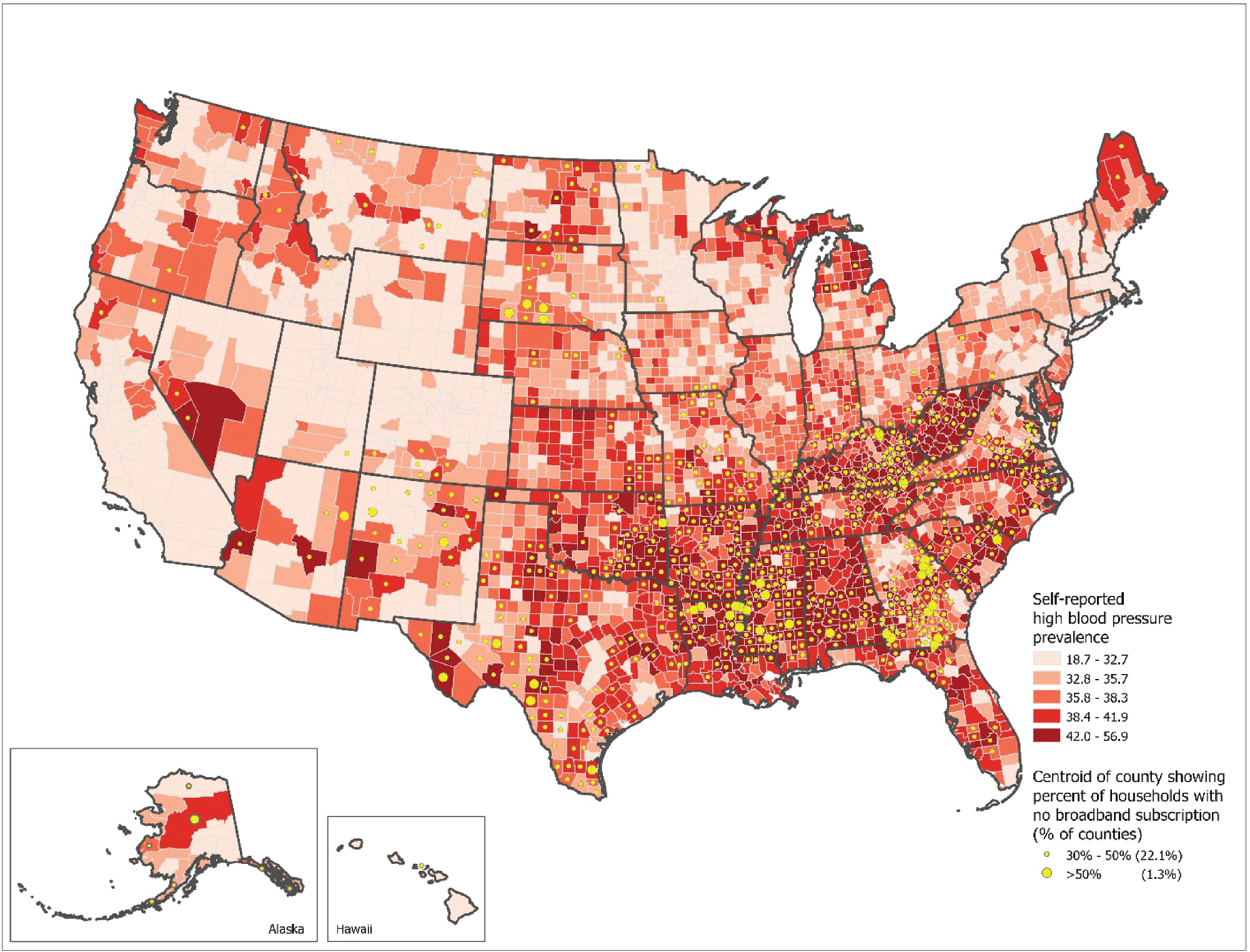
County-level self-reported high blood pressure prevalence among adults aged 18 and oldera and percentage of households with no broadband internet subscription serviceb. aPLACES—Local Data for Better Health (2017). Modeled estimates from Behavioral Risk Factor Surveillance System (BRFSS). https://www.cdc.gov/places. bUS Census American Community Survey 5-year (2015–2019). https://www.census.gov/content/dam/Census/library/publications/2021/acs/acs-49.pdf.
Figure 4 shows physical availability of non-satellite, high-speed broadband access, defined by the FCC as 25/3 Mbps (25 Mbps download speed/3 Mbps upload speed), by county, overlaid with self-reported hypertension prevalence. Many of the counties that have no broadband providers available besides satellite internet also have the highest prevalence of self-reported hypertension. Some have suggested that the broadband gap is even worse when considering the broadband speeds and quality that are actually experienced versus allegedly available.43 Additionally, 25/3 Mbps is considered to be the absolute minimum for “high-speed” internet but many high-level processes or multiple simultaneous users warrant higher speeds (e.g., 100/10 Mbps). Current access to 100/10 Mbps broadband varies greatly across the country (Supplementary Figure 2). Recently, the Biden Administration announced a plan that included $65B to improve broadband infrastructure to 100/20 Mbps, a clear upgrade from the current FCC standard.44 As we as a nation think about improving health equity, committing to widespread, affordable, high-quality broadband access is an integral issue to address, not only for SMBP but for telehealth and PGHD more broadly, particularly for populations like non-Hispanic Black persons or persons from communities of low socioeconomic status who carry a larger burden of uncontrolled blood pressure.
Figure 4.
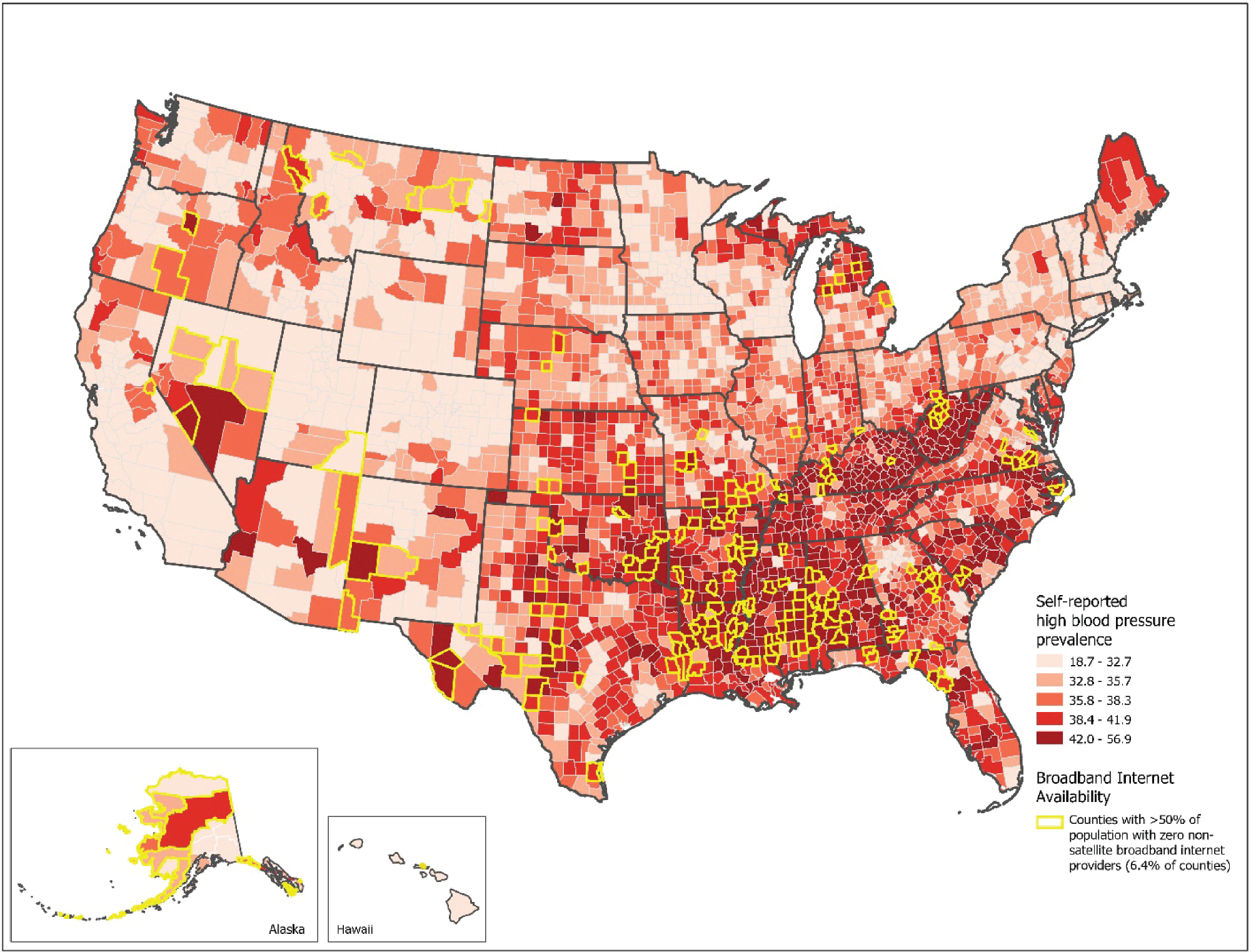
County-level self-reported high blood pressure prevalence among adults aged 18 and oldera and counties with >50% of population with zero nonsatelliteb broadband (25/3 Mbpsc) internet service providersd. aPLACES—Local Data for Better Health (2017). Modeled estimates from Behavioral Risk Factor Surveillance System (BRFSS). https://www.cdc.gov/places. bNonsatellite includes ADSL, cable modem, FTTP, and fixed wireless. c25/3 Mbps = 25 Megabits per second download speed, 3 Megabits per second upload speed. dFCC summary data of fixed broadband coverage by geographic area (2020). https://opendata.fcc.gov/Wireline/Area-Table-June-2020-V1/ktav-pdj7.
ACCESSIBLE TECHNICAL ASSISTANCE TO OVERCOME THE DIGITAL DIVIDE
People with readily available broadband access may need technical assistance to connect their SMBP device to their home internet, download and use necessary applications, and transmit their blood pressure readings. According to a 2021 Pew Research Center survey, 25% of people aged ≥65 years, 14% of people with incomes of less than $30k, and 14% of people with a high school education or less do not use the internet.45 Technical assistance to support SMBP-related technology is not a barrier frequently identified in the hypertension literature though it has been discussed for other health topics.46–48 Ochsner Health, in New Orleans, Louisiana, has an in-house “Ochsner O Bar” to provide training and technical assistance.49 Other health care providers have delivered similar support through home visits by medical informaticists, nurse case managers, or community health workers.33 One potential solution could be a technical assistance center, which could parallel HRSA’s National Health Service Corps’ loan repayment programs for health professionals shortage areas, where workforce is recruited through fiscal incentives. The Office of the National Coordinator for Health Information Technology (ONC) recently announced its Public Health Informatics and Technology Workforce Development Program.50 Perhaps this type of initiative could be leveraged to help span the digital divide in our nation and provide much-needed technical assistance. Another potential solution would be to provide funding opportunities through libraries and other community-based organizations to deliver this kind of assistance. This latter approach could be particularly successful in rural communities.
AMPLE SUPPLY OF VALIDATED BLOOD PRESSURE DEVICES AND APPROPRIATELY SIZED CUFFS
Blood pressure monitoring devices must be cleared for sale in the US by the Food and Drug Administration (FDA). This approval process (i.e., 510(k)) allows device manufacturers to provide validation data on their own devices and allows for ‘substantial equivalence’—where the new device is considered as safe and effective as its predicate model if substantial changes have not been made.51 Both of these factors have led to confusion for clinicians who want to recommend SMBP to their patients but are unsure which device will produce accurate readings. To address this, the AMA partnered with the National Opinion Research Center at the University of Chicago (NORC) to launch the US Blood Pressure Validated Device Listing (VDL™). The VDL lists devices available in the United States that have been validated for clinical accuracy after review by an independent committee of experts and substantial equivalence alone would not qualify for listing.52 As of August 2021, 16 SMBP monitoring devices from 4 manufacturers are listed on the VDL. Moreover, there is a need to have devices validated in specific subpopulations like pregnant women. Clinician and consumer demand and support from national organizations are needed to incentivize device manufacturers to meet these validation standards for their products.
Nationally representative National Health and Nutrition Examination Survey data from 2007 to 2010 show that 52% of men and 38% of women with hypertension require size large or greater blood pressure cuffs.53 Given the increasing rates of obesity in the last decade,54 those estimates are likely even higher today. Furthermore, NACHC worked with 9 health centers to implement SMBP programs for their patients with hypertension. Among participating patients, 50% needed an extra-large blood pressure cuff.55 NACHC created an at-a-glance comparison of devices that were listed on the VDL or in review, as of May 2021, cross-walked with desired device features.56 Only 3 of 16 devices from that crosswalk that were on the VDL at that time are available with an extra-large blood pressure cuff. It is imperative to ensure a ready supply of affordable SMBP devices with appropriate blood pressure cuff sizes to meet the demand. Device manufacturers could use national analyses to guide available cuff sizes. Alternatively, a universal blood pressure cuff could be developed that would fit the vast majority of arms. This has been patented for blood pressure kiosk technology but not yet for home use.57
IMPROVED COVERAGE AND REIMBURSEMENT
Cost-related issues are barriers for patients and clinicians. Devices on the VDL with recommended features cost $50–199 (mean/median $93.42/$90.00). Strikingly, those devices with an extra-large blood pressure cuff available cost $100 or more.56 Many lower-income populations may not be able to afford a recommended device. Insurance coverage is one solution to get devices to those who need them most. Yet, current coverage varies and, when it does exist, it is often insufficient.58 In 2020, Medicare fee-for-service (FFS) Part B began to cover SMBP services, but currently limits coverage of SMBP devices, necessary for the services, to beneficiaries with end stage renal disease. CDC and AMA are collaborating on an assessment of Medicaid coverage for automatic, upper arm SMBP monitoring devices (Healthcare Common Procedure Coding System [HCPCS] code A4670) and separate BP cuffs (HCPCS code A4663). The latter is important if an SMBP device does not come with the correctly sized cuff. The preliminary results (Table 3) show 34 state Medicaid programs provide some level of coverage for automatic upper arm devices and 26 provide coverage for the separate cuffs. However, of the 22 states for which a covered amount could be found, the range for automatic upper arm devices is $8.22 (Arkansas) to $159.44 (New Hampshire) with a mean/median covered amount of $60.50/$54.29, based on the most recent fee schedule data available (CDC/AMA, unpublished data).
Table 3.
Self-measured blood pressure monitoring (SMBP)-related Medicaid coverage and reimbursement, as of July 2021a
| Coverage aspect | States that provide some level of coverage and/or reimbursement |
|---|---|
|
| |
| Automatic BP Device and SMBP Services (HCPCS A4670 and (CPT 99473 and/or 99474)) n = 13 | Delaware, Hawaii, Idaho, Indiana, Michigan, North Carolinab, North Dakota, Ohio, Oregonb, Texas, Virginia, Wisconsin, Wyoming |
| Automatic BP Device Only (HCPCS A4670) n = 21 | Alaska, Arkansas, California, Colorado, Connecticut, DC, Illinois, Iowa, Louisiana, Maine, Maryland, Massachusetts, Minnesota, Missouri, Nebraska, Nevada, New Hampshire, New York, Utah, Vermont, Washington |
| SMBP Services Only (CPT 99473 and/or 99474) n = 8 | Arizona, Floridab, Georgia, Kansas, Kentucky, Montana, New Jersey, New Mexico |
| Separate SMBP Cuff (HCPCS A4663) n = 26 | Alaska, California, Colorado, Connecticut, Delaware, DC, Illinois, Indiana, Kansas, Louisiana, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, New Hampshire, New York, North Dakota, Ohio, Texas, Utah, Virginia, Washington, Wisconsin, Wyoming |
| No SMBP-related coverage or reimbursement n = 8c | Alabama, Oklahoma, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, West Virginia |
Abbreviations: BP, blood pressure; CPT, Current Procedural Terminology, DC, District of Columbia; HCPCS, Healthcare Common Procedure Coding System; SMBP, self-measured blood pressure monitoring.
Results based on the most recent publicly available fee schedule data.
Likely linked to the Public Health Emergency.
Mississippi only provides coverage for separate SMBP cuffs but does not cover the automatic devices or related services.
Another solution that could support additional and sufficient coverage for SMBP devices is expanding the use of value-based insurance design (VBID). VBID, popularized by the University of Michigan Center for VBID, is a strategy that minimizes or eliminates out-of-pocket costs for under-used, high-value services; SMBP monitors are included in those services. In 2020, CMS published a federal register notice with its VBID blueprint that included SMBP monitors as a high-value service that qualified health plans were encouraged to cover with no-cost sharing.59 It should be noted that coverage, when sufficiently available, is only a potential solution for those who have insurance but does not help the uninsured.
Until comprehensive coverage is widely available for SMBP devices and to support uninsured patients, some clinicians have implemented SMBP device loaner programs though they are not widespread.60 When developing an SMBP device loaner program, health care settings can consider loan agreements, inventory needs, inventory management procedures, and cleaning and disinfection protocols. NACHC, Target:BP, AMA, and Million Hearts have helpful guidance materials to support SMBP device loaner program efforts.55,61–63
To incentivize widespread implementation of SMBP, adequate clinician reimbursement may be needed for their time to train patients in proper use of a device and to review patient-generated blood pressure values, interpret the data, and use them in care planning. In 2020, 2 new Current Procedural Terminology (CPT) [CPT © Copyright 2021 American Medical Association. All rights reserved. AMA and CPT are registered trademarks of the American Medical Association.] codes were introduced:
99473—an annual reimbursement ($11.52) [According to the 2021 CMS Physician Fee Schedule Look Up. https://www.cms.gov/medicare/physician-fee-schedule/search.] for “self-measured blood pressure using a device validated for clinical accuracy; patient education/training and device calibration.”
99474—a monthly reimbursement ($15.00) [According to the 2021 CMS Physician Fee Schedule Look Up. https://www.cms.gov/medicare/physician-fee-schedule/search.] for “self-measured blood pressure using a device validated for clinical accuracy, separate self-measurements of 2 readings, one minute apart, twice daily over a 30-day period (minimum of 12 readings), collection of data reported by the patient and/or caregiver to the physician or other qualified health care professional, with report of average systolic and diastolic pressures and subsequent communication of a treatment plan to the patient.”
For example, for a clinician with a total patient panel of 2,000 adults, if one assumed half had hypertension and 20% of them were Medicare beneficiaries, reimbursement from the above codes could equate to over $11k per clinician in a given year.64 While these codes offer modest reimbursement, if SMBP for patients with hypertension was systematically conducted in a practice with multiple clinicians, the reimbursement could potentially pay for a full-time staff person to train all patients with hypertension. However, these CPT codes are underutilized. We analyzed monthly claims data for 22.3 million Medicare FFS beneficiaries in 2020 and 19.7 million in 2021, who were aged ≥65 years with at least one month of continuous enrollment in both Part A (hospitalization) and Part B (outpatient care) and had hypertension. We defined hypertension as having a diagnosis code based on ICD-10 code from Part A or Part B claims, or a diagnosis of hypertension based on the Chronic Conditions Warehouse definition used by CMS (Table 4). Among these, only 0.01% had a claim for CPT 99473 both in 2020 and in 2021, while 0.01% in 2020 and <0.01% in 2021 had 1 or more claims for CPT 99474 (CDC, unpublished data). In addition, although CPT 99474 can be billed monthly for each patient using SMBP for ongoing treatment decisions, most patients for whom this code was billed only had one use of the code. These results represent a major opportunity for raising awareness among primary care clinicians and others who care for patients with hypertension. With the deregulation of telehealth during the COVID-19 pandemic and subsequent growth in the number of virtual office visits, these codes could support rapid improvements in hypertension control and provide much-needed data on an important vital sign.
Table 4.
Use of self-measured blood pressure monitoring-related Current Procedural Terminology codesa, January 2020–May 2021
| Year | Total beneficiaries aged 65+, N | Hypertension prevalence, n (%) | CPT 99473 |
CPT 99474 |
|
|---|---|---|---|---|---|
| Training, device setup, and calibration received, n (%) | SMBP for ongoing treatment decisions, total ≥1 session, n (%) | Among beneficiaries with ≥1 use of CPT code, mean number of uses of the code | |||
|
| |||||
| 2020 | 29,958,986 | 22,285,241 (74.4) | 1,815 (0.01) | 1,353 (0.01) | 1.41 |
| 2021 | 27,661,406 | 19,669,335 (71.1) | 1,158 (0.01) | 474 (<0.01) | 1.27 |
Abbreviations: CPT, Current Procedural Terminology; SMBP, self-measured blood pressure monitoring
Analysis assessed the prevalence of use of CPT codes 99473 and 99474 among Medicare fee-for-service (FFS) beneficiaries with hypertension aged 65+ with at least one month of continuous enrollment in Medicare Part A (hospitalization) and Part B (outpatient care), using CMS real-time data. Hypertension prevalence was defined as a diagnosis code based on ICD-10-CM from Part A or Part B claims, or a diagnosis code of hypertension based on the Chronic Conditions Warehouse definition.
CREATIVE SOLUTIONS TO OVERCOME BARRIERS OF TRUST, TIME, AND DISTANCE
When thinking about optimal SMBP implementation, there are tasks that fall under the scopes of practice of physicians and advanced practitioners and tasks that must be completed by patients (Table 5). There are also a number of integral tasks related to training and educating patients that could be done by other members of the care team. Medical assistants and nurses are a ready solution in many health care settings, but smaller practices, in particular, may not have in-house staff who can shoulder the burden of these tasks. Clinical pharmacists, operating through collaborative practice agreements,65 and community health workers can help extend the reach of a practice. For people who have had a cardiovascular event, cardiac or stroke rehabilitation programs, and home health care agencies could include SMBP training and education as part of their standardized curricula and services.
Table 5.
Self-measured blood pressure monitoring (SMBP) tasks by role
| Must be done by a licensed clinician | Can be done by a non-licensed person (e.g., medical assistant, local department of health, community health organization, community health workers) | Must be done by patient |
|---|---|---|
|
| ||
| 1. Diagnose hypertension 2. Prescribe medication(s) 3. Provide SMBP measurement protocol 4. Interpret patient-generated SMBP readings 5. Provide resultant medication titration advice 6. Provide resultant lifestyle modification recommendations |
1. Provide guidance on validated SMBP monitor selection 2. If needed, provide a validated SMBP monitor (free or loaned) 3. Train patients to use a validated SMBP monitor 4. Validate home BP monitor against a more robust machine 5. Train patients to capture and relay SMBP values to the care team, ideally through remote means 6. Provide technical assistance to patients on connecting their SMBP device to their home internet, downloading and using necessary apps, and transmitting their SMBP readings to the care team 7. Reinforce clinician-directed SMBP measurement protocol 8. Share medication adherence strategies 9. Provide lifestyle modification education |
1. Take SMBP readings 2. Take medications as prescribed 3. Make recommended lifestyle modifications 4. Convey SMBP readings to care team 5. Convey side effects, challenges with lifestyle modifications to care team |
Adapted from National Association of Community Health Centers. Self-measured Blood Pressure Monitoring Implementation Guide for Health Care Delivery Organizations. Bethesda, MD: National Association of Community Health Centers; 2018.
One solution outside of the clinical setting could be to use community-based resources. For example, community pharmacists could provide on-site training when SMBP devices are purchased. State or local public health nurses and similar staff could hold classes or office hours for training and technical assistance. Similarly, community-based organizations concerned with health and wellness like the YMCA, senior centers, fire stations, and libraries, as well as gyms and fitness centers, could be venues for SMBP-related training and education. Furthermore, for non-Hispanic Black persons, for whom distrust of the medical system may be an issue, barbershops, salons, or churches could be outlets for SMBP-related training and education, but work is needed to build these types of community-based infrastructure and ensure a connection with clinical care. Using community-based organizations to deliver training and education for patients using SMBP could be a convenient, trusted resource especially in rural areas or when culturally or linguistically tailored information would be helpful. If we are going to reach ~68M adults in the United States for widespread SMBP implementation, the nation needs creative, out-of-the-box solutions to set everyone—clinicians and patients—up for success.
Advancing optimal SMBP is a critical opportunity to improve the nation’s blood pressure control. The Surgeon General’s Call to Action to Control Hypertension noted improvements in blood pressure control in all populations will “need broadscale, multisector, culturally sensitive, and diverse interventions”.1 This could be uniquely demonstrated in the expansion of SMBP across the United States. SMBP is evidence based, with accompanying real-world success stories,33,35,49 yet the barriers to use are diverse and significant advancement in uptake will require interventions at multiple points. A collective effort could help modernize data transfer and processing, improve broadband access, expand coverage and increase affordability for SMBP devices and appropriate cuff sizes, integrate SMBP into routine care and reimbursement practices, and strengthen patient engagement, trust, and access. Addressing these areas can help equip and empower individuals, communities, clinicians, and health care organizations across the country to improve blood pressure control and cardiovascular health.
Supplementary Material
ACKNOWLEDGMENTS
We acknowledge Meg Meador, MPH, C-PHI, CPHQ, Director, Clinical Integration and Education at the National Association of Community Health Centers, for her leadership on developing many of the tools referenced in this article. We also acknowledge Andrea S. Kennon, MPH, CHES from ASRT Inc., Division for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention, and Matthew McReynolds, MPH and Iman Ibrahim, MPH Candidate at University of Illinois Chicago, Policy Interns, American Medical Association, for their work on the Medicaid coverage analysis. The findings and conclusions in this report are those of the authors and do not necessarily reflect the official position of the Centers for Disease Control and Prevention.
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
SUPPLEMENTARY MATERIAL
Supplementary data are available at American Journal of Hypertension online.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC). Hypertension Cascade: Hypertension Prevalence, Treatment and Control Estimates Among US Adults Aged 18 Years and Older Applying the Criteria From the American College of Cardiology and American Heart Association’s 2017 Hypertension Guideline—NHANES 2015–2018. US Department of Health and Human Services: Atlanta, GA, 2019. https://millionhearts.hhs.gov/data-reports/hypertension-prevalence.html. Accessed 21 August 2021. [Google Scholar]
- 2.Bornstein E, Eliner Y, Chervenak FA, Grünebaum A. Concerning trends in maternal risk factors in the United States: 1989–2018. EClinicalMedicine. 2020; 29–30:100657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuklina EV, Ayala C, Callaghan WM. Hypertensive disorders and se-vere obstetric morbidity in the United States. Obstet Gynecol 2009; 113:1299–1306. [DOI] [PubMed] [Google Scholar]
- 4.Umesawa M, Kobashi G. Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis. Hypertens Res 2017; 40:213–220. [DOI] [PubMed] [Google Scholar]
- 5.Khosla K, Heimberger S, Nieman KM, Tung A, Shahul S, Staff AC, Rana S. Long-term cardiovascular disease risk in women after hypertensive disorders of pregnancy: recent advances in hypertension. Hypertension. 2021; 78:927–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomas SJ, Booth JN 3rd, Dai C, Li X, Allen N, Calhoun D, Carson AP, Gidding S, Lewis CE, Shikany JM, Shimbo D, Sidney S, Muntner P. Cumulative incidence of hypertension by 55 years of age in Blacks and Whites: the CARDIA Study. J Am Heart Assoc. 2018;7:e007988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaughan A Local Disparities in Hypertensive CVD Mortality. Federal Hypertension Control Leadership Council: Atlanta, GA, 2021. [Google Scholar]
- 8.Shahu A, Herrin J, Dhruva SS, Desai NR, Davis BR, Krumholz HM, Spatz ES. Disparities in socioeconomic context and association with blood pressure control and cardiovascular outcomes in ALLHAT. J Am Heart Assoc 2019; 8:e012277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, Colantonio LD. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA 2020; 324:1190–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med 2013; 159:185–194. [DOI] [PubMed] [Google Scholar]
- 11.Tucker KL, Sheppard JP, Stevens R, Bosworth HB, Bove A, Bray EP, Earle K, George J, Godwin M, Green BB, Hebert P, Hobbs FDR, Kantola I, Kerry SM, Leiva A, Magid DJ, Mant J, Margolis KL, McKinstry B, McLaughlin MA, Omboni S, Ogedegbe O, Parati G, Qamar N, Tabaei BP, Varis J, Verberk WJ, Wakefield BJ, McManus RJ. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS Med 2017; 14:e1002389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published correction appears in Hypertension. 2018;71:e140–144]. Hypertension 2018; 71:e13–e115. [DOI] [PubMed] [Google Scholar]
- 13.Siu AL; U.S. Preventive Services Task Force. Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2015; 163:778–786. [DOI] [PubMed] [Google Scholar]
- 14.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; ESC Scientific Document Group. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 2018; 39:3021–3104. [DOI] [PubMed] [Google Scholar]
- 15.Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, McBrien K, Harris KC, Nakhla M, Cloutier L, Gelfer M, Lamarre-Cliche M, Milot A, Bolli P, Tremblay G, McLean D, Padwal RS, Tran KC, Grover S, Rabkin SW, Moe GW, Howlett JG, Lindsay P, Hill MD, Sharma M, Field T, Wein TH, Shoamanesh A, Dresser GK, Hamet P, Herman RJ, Burgess E, Gryn SE, Grégoire JC, Lewanczuk R, Poirier L, Campbell TS, Feldman RD, Lavoie KL, Tsuyuki RT, Honos G, Prebtani APH, Kline G, Schiffrin EL, Don-Wauchope A, Tobe SW, Gilbert RE, Leiter LA, Jones C, Woo V, Hegele RA, Selby P, Pipe A, McFarlane PA, Oh P, Gupta M, Bacon SL, Kaczorowski J, Trudeau L, Campbell NRC, Hiremath S, Roerecke M, Arcand J, Ruzicka M, Prasad GVR, Vallée M, Edwards C, Sivapalan P, Penner SB, Fournier A, Benoit G, Feber J, Dionne J, Magee LA, Logan AG, Côté AM, Rey E, Firoz T, Kuyper LM, Gabor JY, Townsend RR, Rabi DM, Daskalopoulou SS; Hypertension Canada. Hypertension Canada’s 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol 2018; 34:506–525. [DOI] [PubMed] [Google Scholar]
- 16.Sharman JE, Howes FS, Head GA, McGrath BP, Stowasser M, Schlaich M, Glasziou P, Nelson MR. Home blood pressure monitoring: Australian Expert Consensus Statement. J Hypertens 2015; 33:1721–1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D; American Heart Association; American Society of Hypertension; Preventive Cardiovascular Nurses Association. Call to action on use and reimbursement for home blood pressure monitoring: a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension 2008; 52:10–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shimbo D, Artinian NT, Basile JN, Krakoff LR, Margolis KL, Rakotz MK, Wozniak G; American Heart Association and the American Medical Association. Self-measured blood pressure monitoring at home: a joint policy statement from the american Heart Association and American Medical Association. Circulation 2020; 142:e42–e63. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services. The Surgeon General’s Call to Action to Control Hypertension. U.S. Department of Health and Human Services, Office of the Surgeon General: Washington, DC, 2020. [Google Scholar]
- 20.Health Resources & Services Administration. FY 2021 Supplemental Funding for Hypertension (NHCI-HC). https://bphc.hrsa.gov/program-opportunities/national-hypertension-control-initiative. Accessed 24 August 2021.
- 21.Breaux-Shropshire TL, Brown KC, Pryor ER, Maples EH. Prevalence of blood pressure self-monitoring, medication adherence, self-efficacy, stage of change, and blood pressure control among municipal workers with hypertension. Workplace Health Saf 2012; 60:265–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poon IO, Etti N, Lal LS. Does the use of home blood pressure monitoring vary by race, education, and income? Ethn Dis 2010; 20:2–6. [PubMed] [Google Scholar]
- 23.Viera AJ, Cohen LW, Mitchell CM, Sloane PD. Use of home blood pressure monitoring by hypertensive patients in primary care: survey of a practice-based research network cohort. J Clin Hypertens (Greenwich) 2008; 10:280–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ostchega Y, Berman L, Hughes JP, Chen TC, Chiappa MM. Home blood pressure monitoring and hypertension status among US adults: the National Health and Nutrition Examination Survey (NHANES), 2009–2010. Am J Hypertens 2013; 26:1086–1092. [DOI] [PubMed] [Google Scholar]
- 25.Ostchega Y, Zhang G, Kit BK, Nwankwo T. Factors associated with home blood pressure monitoring among US adults: National Health and Nutrition Examination Survey, 2011–2014. Am J Hypertens 2017; 30:1126–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fang J, Luncheon C, Wall HK, Wozniak G, Loustalot F. Self-measured blood pressure monitoring among adults with self-reported hypertension in 20 US states and the District of Columbia, 2019. Am J Hypertens 2021; 34:1148–1153. [DOI] [PubMed] [Google Scholar]
- 27.Carter EJ, Moise N, Alcántara C, Sullivan AM, Kronish IM. Patient barriers and facilitators to ambulatory and home blood pressure monitoring: a qualitative study. Am J Hypertens 2018; 31:919–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grant S, Hodgkinson JA, Milner SL, Martin U, Tompson A, Hobbs FR, Mant J, McManus RJ, Greenfield SM. Patients’ and clinicians’ views on the optimum schedules for self-monitoring of blood pressure: a qualitative focus group and interview study. Br J Gen Pract 2016; 66:e819–e830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huff LS, Zittleman L, DeAlleaume L, Bernstein J, Chavez R, Sutte C, LeBlanc WG, Parnes B. What keeps patients from adhering to a home blood pressure program? J Am Board Fam Med 2011; 24:370–379. [DOI] [PubMed] [Google Scholar]
- 30.Wood PW, Boulanger P, Padwal RS. Home Blood pressure telemonitoring: rationale for use, required elements, and barriers to implementation in Canada. Can J Cardiol 2017; 33:619–625. [DOI] [PubMed] [Google Scholar]
- 31.Kronish IM, Kent S, Moise N, Shimbo D, Safford MM, Kynerd RE, O’Beirne R, Sullivan A, Muntner P. Barriers to conducting ambulatory and home blood pressure monitoring during hypertension screening in the United States. J Am Soc Hypertens 2017; 11:573–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Robins LS, Jackson JE, Green BB, Korngiebel D, Force RW, Baldwin LM. Barriers and facilitators to evidence-based blood pressure control in community practice. J Am Board Fam Med 2013; 26:539–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Public Health Informatics Institute. Self-Measured Blood Pressure Monitoring (SMBP): Key Findings from a National Health Information Technology Landscape Analysis. September 2021. https://phii.org/SMBP-Health-IT-Landscape. Accessed 15 September 2021. [Google Scholar]
- 34.Muldoon MF, Kronish IM, Shimbo D. Of Signal and noise: overcoming challenges in blood pressure measurement to optimize hypertension care. Circ Cardiovasc Qual Outcomes 2018; 11:e004543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meador M, Hannan J, Roy D, Whelihan K, Sasu N, Hodge H, Lewis JH. Accelerating Use Of self-measured blood pressure monitoring (SMBP) Through clinical-community care models. J Community Health 2021; 46:127–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sayeed R, Gottlieb D, Mandl KD. SMART Markers: collecting patient-generated health data as a standardized property of health information technology. NPJ Digit Med 2020; 3:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Congressional Research Service. Federal Universal Service Fund and Other Selected Federal Broadband Programs: A Primer. 2021. https://crsreports.congress.gov/product/pdf/IF/IF11748. Accessed 11 August 2021.
- 38.Anders D What Is the Average Internet Bill? 2021. https://www.allconnect.com/blog/cost-of-high-speed-internet. Accessed 11 August 2021.
- 39.BroadbandSearch. The Cost of the Internet by State in the USA. 2021. https://www.broadbandsearch.net/blog/internet-cost-by-state. Accessed 11 August 2021.
- 40.Howard G, Howard VJ. Twenty years of progress toward understanding the stroke belt. Stroke 2020; 51:742–750. [DOI] [PubMed] [Google Scholar]
- 41.Anderson M, Kumar M. Digital Divide Persists Even as Lower-Income Americans Make Gains in Tech Adoption. Pew Research Center. 2019. https://www.pewresearch.org/fact-tank/2019/05/07/digital-divide-persists-even-as-lower-income-americans-make-gains-in-tech-adoption/. Accessed 11 August 2021.
- 42.Federal Communication Commission. 4G LTE Coverage as of May 15, 2021 (AT&T Mobility, T-Mobile, UScellular, Verizon). 2021. https://www.arcgis.com/apps/webappviewer/index.html?id=6c1b2e73d9d749cdb7bc88a0d1bdd25b. Accessed 24 August 2021.
- 43.Brandom R, Joel W. This is a Map of America’s Broadband Problem—A County-by-County Look at the Broadband Gap. The Verge. 2021. https://www.theverge.com/22418074/broadband-gap-america-map-county-microsoft-data. Accessed 24 August 2021.
- 44.Congress.gov. H.R.3684—117th Congress (2021–2022): Infrastructure Investment and Jobs Act. 2021. https://www.congress.gov/bill/117th-congress/house-bill/3684. Accessed 24 August 2021.
- 45.Pew Research Center, 7% of Americans Don’t Use the Internet. Who Are They? April 2, 2021, Survey Conducted January 25–February 8, 2021. https://www.pewresearch.org/fact-tank/2021/04/02/7-of-americans-dont-use-the-internet-who-are-they/. Accessed 31 August 2021.
- 46.Saeed SA, Masters RM. Disparities in Health care and the digital divide. Curr Psychiatry Rep 2021; 23:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ng BP, Park C. Accessibility of telehealth services during the COVID-19 pandemic: a cross-sectional survey of Medicare beneficiaries. Prev Chronic Dis 2021; 18:E65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim EH, Stolyar A, Lober WB, Herbaugh AL, Shinstrom SE, Zierler BK, Soh CB, Kim Y. Challenges to using an electronic personal health record by a low-income elderly population. J Med Internet Res 2009; 11:e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Milani RV, Wilt JK, Milani AR, Bober RM, Malamud E, Entwisle J, Lavie CJ. Digital management of hypertension improves systolic blood pressure variability. Am J Med 2020; 133:e355–e359. [DOI] [PubMed] [Google Scholar]
- 50.HealthIT.gov. ONC Funding Opportunities—Public Health Informatics & Technology (PHIT) Workforce Development Program. https://www.healthit.gov/topic/onc-funding-opportunities/public-health-informatics-technology-phit-workforce-development. Accessed 20 August 2021.
- 51.U.S. Food & Drug Administration. Premarket Notification 510(k). https://www.fda.gov/medical-devices/premarket-submissions/premarket-notification-510k. Accessed 25 August 2021.
- 52.American Medical Association. Validated Device Listing (VDL) Criteria. 2021. https://www.validatebp.org/wp-content/uploads/2021/06/VDLCriteria-Document_Blood-Pressure_AMA_Rev1-2021.pdf. Accessed 11 August 2021.
- 53.Ostchega Y, Hughes JP, Zhang G, Nwankwo T, Chiappa MM. Mean mid-arm circumference and blood pressure cuff sizes for U.S. adults: National Health and Nutrition Examination Survey, 1999–2010. Blood Press Monit 2013; 18:138–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ogden CL, Fryar CD, Martin CB, Freedman DS, Carroll MD, Gu Q, Hales CM. Trends in Obesity Prevalence by Race and Hispanic Origin-1999–2000 to 2017–2018. JAMA 2020; 324:1208–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.National Association of Community Health Centers. Self-Measured Blood Pressure Monitoring (SMBP) Implementation Toolkit. December 2020. https://www.nachc.org/wp-content/uploads/2020/12/SMBP-Toolkit_FINAL.pdf. Accessed 20 August 2021.
- 56.National Association of Community Health Centers. Choosing a Home Blood Pressure Monitor for Your Practice: At-a-Glance Comparison. 2021. https://www.nachc.org/wp-content/uploads/2021/05/Choosing-a-Home-BP-Monitor_At-a-Glance-Comparison.pdf. Accessed 11 August 2021.
- 57.Pharmasmart. Accurate, Integrated and Easy to Use. http://pharma-smart.com/product/ps-2000-d/. Accessed 18 August 2021.
- 58.National Association of Chronic Disease Directors. A National Analysis of Self-Measured Blood Pressure Monitoring Coverage and Reimbursement. February 2020. https://chronicdisease.org/resource/resmgr/website-2020/consultants/cvh/smbp/synthesis_of_smbp_coverage_f.pdf. Accessed 13 August 2021. [Google Scholar]
- 59.Centers for Medicare & Medicaid Services. Patient Protection and Affordable Care Act; HHS Notice of Benefit and Payment Parameters for 2021; Notice Requirement for Non-Federal Governmental Plans. Fed Reg 2020; 85. https://www.govinfo.gov/content/pkg/FR-2020-05-14/pdf/2020-10045.pdf. Accessed 13 August 2021. [Google Scholar]
- 60.Jackson SL, Ayala C, Tong X, Wall HK. Clinical implementation of self-measured blood pressure monitoring, 2015–2016. Am J Prev Med 2019; 56:e13–e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Target:BP. Tools and Downloads—Patient-Measured BP. 2021. https://targetbp.org/tools-downloads/?keyword=loaner&sort=topic&. Accessed 20 August 2021. [Google Scholar]
- 62.Improving Health Outcomes: Blood Pressure; L Murakami, M Rakotz. Self-measured Blood Pressure Monitoring Program: Engaging Patients in Self-measurement, 1st edn. D Daniel, M Prall (eds). American Medical Association and the Johns Hopkins University School of Medicine, February 2015. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/about-ama/iho-bp-engaging-patients-in-self-measurment_0.pdf. Accessed 20 August 2021. [Google Scholar]
- 63.Centers for Disease Control and Prevention. Hypertension Control Change Package. Establish a Self-Measured BP (SMBP) Monitoring Program, 2nd edn. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services: Atlanta, GA, 2020. https://millionhearts.hhs.gov/files/HTN_Change_Package.pdf#page=16. Accessed 18 August 2021. [Google Scholar]
- 64.Million Hearts. An Economic Case for Self-Measured Blood Pressure (SMBP) Monitoring. 2021. https://millionhearts.hhs.gov/files/SMBP_economic_case-508.pdf. Accessed 13 August 2021. [Google Scholar]
- 65.Centers for Disease Control and Prevention. Advancing Team-Based Care Through Collaborative Practice Agreements: A Resource and Implementation Guide for Adding Pharmacists to the Care Team. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services: Atlanta, GA, 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


