Abstract
Rotator cuff tears are among the most common orthopaedic injuries. If not treated, they can result in a massive irreparable tear because of tendon retraction and muscle atrophy. Mihata et al. in 2012 described the technique of superior capsular reconstruction (SCR) using fascia lata autograft. This has been considered an acceptable and effective method for treating irreparable massive rotator cuff tears. We describe an arthroscopically assisted superior capsular reconstruction (ASCR) technique using all soft anchors to preserve the bone stock and reduce possible hardware complications. Moreover, knotless anchors for the lateral fixation make the technique easier to reproduce.
Technique Video
The video shows all the crucial steps of the "all soft" anchor superior capsular reconstruction technique described in the article.
Rotator cuff tears are among the most common orthopaedic injuries. If not early treated, this injury can result in massive tears1 that can be irreparable because of tendon retraction, fat infiltration, and muscle atrophy.2
Different treatment options have been proposed for irreparable tear, including nonoperative rehabilitation, biodegradable spacer, partial functional tendon repair, patch augmentation, tendon transfer, and reverse shoulder arthroplasty.3, 4, 5, 6, 7, 8, 9 More recently, Mihata et al.10 described the arthroscopically assisted superior capsular reconstruction (ASCR). The superior capsule prevents superior translation of the glenohumeral joint, helping maintain passive stability.11,12
Despite showing promising short-term clinical results, ASCR remains a time-consuming, technically challenging, and hardly reproducible technique.
Our purpose is to present a technique that aims to minimize difficulties with graft and suture management (Video 1).
Methods
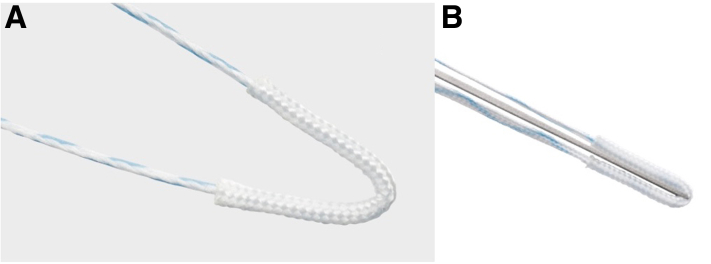
The Arthrex FiberTak soft anchor is an all-suture anchor loaded with a single fiberwire suture (Fig 1), requiring a 1.6-mm drill to create a bone socket to be inserted into the bone.
Fig 1.
(A, B) A single-tape FiberTak Arthrex 1.6-mm anchor used on the glenoid neck to medially fix the patch.
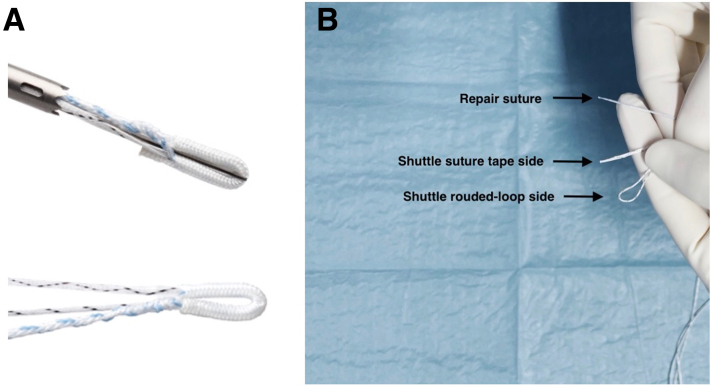
The Arthrex 1.8 knotless FiberTak anchor is an all-suture anchor with tensionable knotless technology. The anchor has a suture tape, nonsliding suture (blue and white), and a 2-ended fiberlink (all blue) sliding with 1 looped end (Fig 2). To knot the suture, the operator loads the nonsliding suture tape into the fiberlink looped end. The operator pulls the other end of the fiberlink, and the suture tape is shuttled into the anchor's locking mechanism. In this way, the operator can control the tension under direct vision.
Fig 2.
(A) A single suture knotless 1.8-mm FiberTak Arthrex anchor used on the humeral greater tuberosity to laterally fix the patch. (B) The end of the suture tape and the 2 different ends of the shuttle suture.
Arthrex PassPort (12 mm, 3 cm) is positioned through the lateral portal to make it easier to keep all the sutures clear, avoiding difficulties in retrieving the suture for the lateral fixation of the patch.
Arthrex DX Reinforcement Matrix is a porcine dermal extracellular matrix that has been created as a biomechanically strong and biocompatible scaffold for the reinforcement and repair of soft tissues. Arthrex provides a sterile, ready to use, biologically intact scaffold while maintaining essential matrix components such as collagen, elastin, glycoproteins, glycosaminoglycans, and proteoglycans.
Technique
Indications for superior capsular reconstruction (SCR) include irreparable massive rotator cuff tears confirmed by magnetic resonance imaging (MRI), intolerable shoulder pain, and failure of conservative management (anti-inflammatory drugs, steroids, and physiokinesis therapy); diagnoses are confirmed by an MRI showing supraspinatus and/or infraspinatus tear, and tendons retract medially to the glenoid (Patte grade 3).
Patient Positioning
In our experience, patients are positioned in a lateral decubitus position under general anesthesia plus interscalenic block; the head must be kept in a neutral position to avoid plexus lesions. The patient is stabilized in a lateral decubitus position with a beanbag. The arm is then wrapped into a traction sleeve; traction is then applied, paying attention to avoid neurovascular injuries. The arm should be placed at approximately 15° of forward flexion and 70° of abduction for the intra-articular diagnosis.
Intra-articular Diagnosis
First, the surgeon performs the posterior portal and then the anterosuperior portal in order to proceed with a diagnostic arthroscopy, during which it may be necessary to repair other articular lesions, including subscapularis and biceps brachialis long head tear. During this phase, the surgeon evaluates and records arthrosis signs.
Surgical Technique
The patient arm position is then moved into the bursoscopy position with the arm at 30° of abduction, and a lateral subacromial portal is created to allow a cannula insertion (Arthrex PassPort 12 mm, 3 cm) to help suture management and graft passage.
Suture Anchor Placement
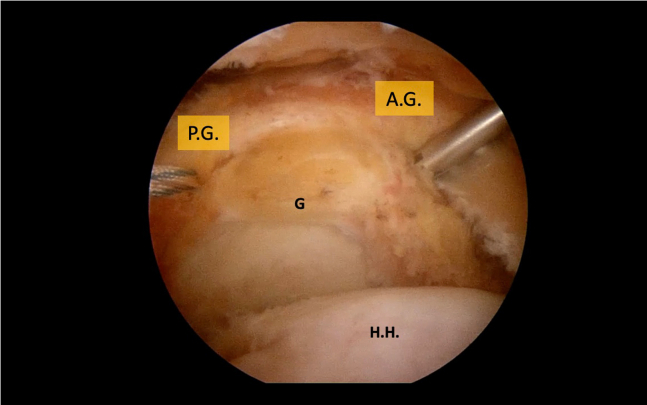
Glenoid Anchors
The surgeon uses 2 spinal needles to locate the correct position to place 2 soft anchors (Fibertak soft anchor) through 2 percutaneous skin incisions (anterior glenoid [AG] and posterior glenoid [PG] anchors) (Fig 3) on the glenoid neck. The spare is inserted through the skin incision and positioned on the glenoid neck. A bone socket is created, advancing a 1.6-mm drill through the spear. Next, insert the FiberTak soft anchor through the spear and into the bone socket by gentle impaction. One fiberwire end of each anchor is retrieved from the lateral PassPort cannula and anchored onto the external flange of the PassPort cannula with a clamp.
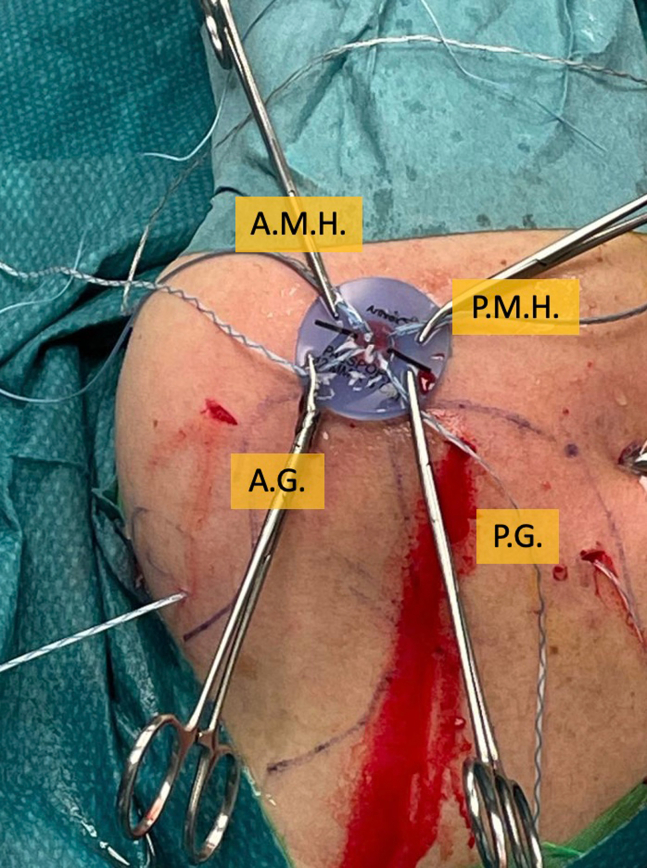
Fig 3.
View of a right shoulder in the lateral decubitus position from the lateral subacromial portal of the 2 FiberTak anchors placed on the glenoid neck to medially fix the patch: the anterior glenoid anchor (A.G.) and the posterior glenoid anchor (P.G.). (G, glenoid; H.H., humeral head.)
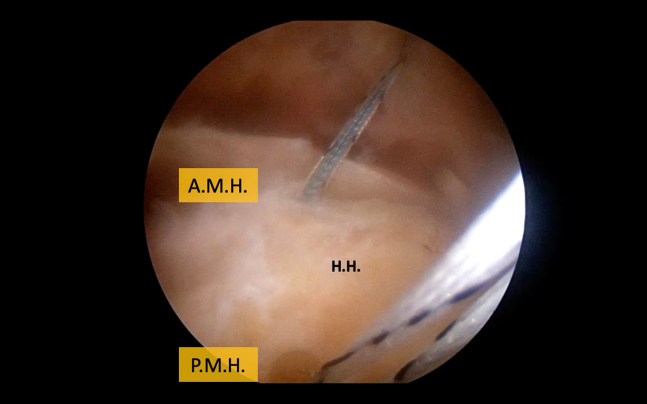
Greater Tuberosity Medial Row Anchors
Two knotless soft anchors (Knotless 1.8 FiberTak; Arthrex) loaded with 1 repair suture tape and a 2-ended shuttle fiberwire are then placed on the medial aspects of the greater tuberosities (Fig 4), one anteriorly (anteromedial humeral anchor [AMH]) and one posteriorly (posteromedial humeral anchor [PMH]). We use 2 spinal needles to identify the correct position as we did before. We insert the spear through a skin portal, a 1.8-mm drill is inserted to create a bone socket, and then the anchor is positioned by gentle impaction. Each anchor suture tape and the rounded loop side of the shuttle suture are retrieved separately through the lateral PassPort cannula and anchored on the external flange of the cannula with a clamp, to be kept separated from one another (Fig 5).
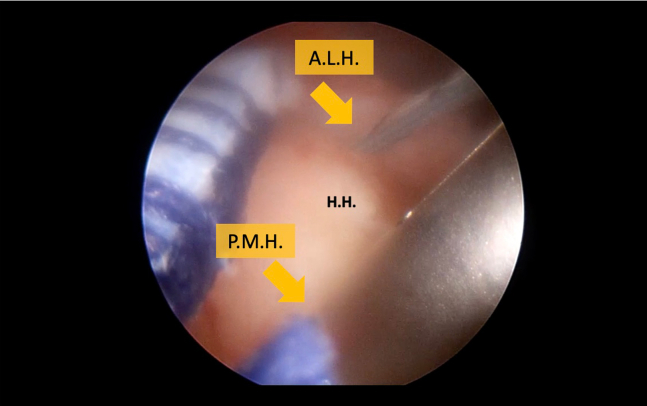
Fig 4.
View of a right shoulder in the lateral decubitus position from the posterior portal of the 2 knotless FiberTak anchors of the medial row placed on the humeral head greater tuberosity. (A.M.H., anteromedial humeral anchor; H.H., humeral head; P.M.H., posteromedial humeral anchor.)
Fig 5.
View of a right shoulder in the lateral decubitus position from outside of the suture of the 2 glenoid anchors (A.G. and P.G.) and the medial sutures of the greater tuberosity (A.M.H. and P.M.H.) secure to the outer flange of the PassPort cannula inserted in the lateral subacromial portal, each in the corresponding position of the anchor.
The 2 lateral anchors of the greater tuberosity (anterolateral humeral [ALH] and posterolateral humeral [PLH]) are inserted after the patch medial fixation to identify the correct distance from AMH and PMH that guarantees the best lateral patch fixation. Moreover, placing it later reduces the amount of tape before the patch positioning, simplifying the insertion and the medial fixation.
Patch Preparation
At this point, it is necessary to measure the distance between the anchors using a ruler. The medial border is the distance between the 2 glenoid anchors AG and PG; the lateral border is the distance between the 2 anchors on the medial row placed on the greater tuberosities (AMH and PMH). The anterior and posterior borders are the distance between the 2 anterior anchors, AG and AMH, and the 2 posterior anchors, PG and PMH, adding 10 mm each (anterior border = AM–AL + 10 mm; posterior border = PM–PL + 10 mm). These measurements are recorded and used to shape the graft (Fig 6); the patch is shaped of twice the defect width, and it is then folded and harvested to double its thickness (Fig 6).
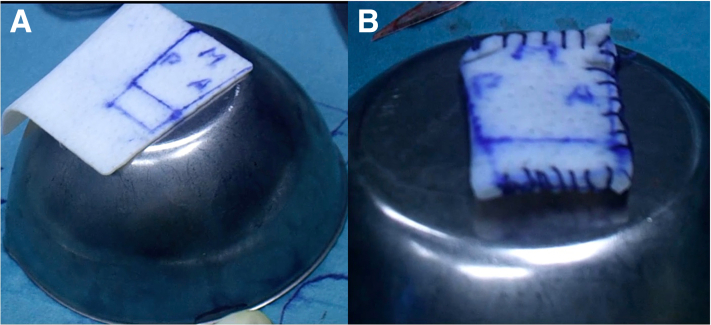
Fig 6.
(A) An outer view of the reported measures of the distances between the anchors on the graft. (B) The graft shaped and doubled in its thickness and basted with a suture.
The 2 medial anchors (FiberWire) are passed through the patch in the corresponding anchor position and knotted around the patch corners, while the suture tape and the shuttle suture of the humeral Knotless FiberTak Arthrex anchors are passed through the patch in the corresponding anchor position.
Patch Positioning
At this point, we grasp the medial side of the patch with a grasper and slide it into the subacromial space through the lateral cannula while pulling the other end of the suture of the glenoid anchors.
Medial Fixation
Once the patch is correctly positioned on the glenoid, it is fixed, knotting the suture of the glenoid anchors through the lateral portal.
Lateral Patch Fixation
Greater tuberosity lateral row anchors: We position the 2 lateral humeral knotless FiberTak Arthrex (ALH and PLH) on the lateral aspects of the greater tuberosity (Fig 7) using the same technique we used for the 2 medial humeral anchors. The suture tape and the looped side of the shuttle are retrieved from the lateral portal and secured to the lateral aspects of the cannula to keep them separated from those of the other humeral anchors.
Fig 7.
Images of a right shoulder in the lateral decubitus position viewing from the posterior portal of the position of the anterolateral humeral (A.L.H.) and posterolateral humeral (P.L.H.) anchors on the humeral greater tuberosity. (H.H., humeral head.)
Lateral fixation: The patch is laterally fixed, reproducing a knotless SpeedBridge repair. To do so, we insert the suture of AMH into the hole of the looped side shuttle of the PLH and shuttle it into the locking mechanism of the PLH anchor and the PMH into the ALH to obtain an X shape; then, we shuttle the ALH into the AMH and the PLH into the PMH to complete the fixation (Fig 8).
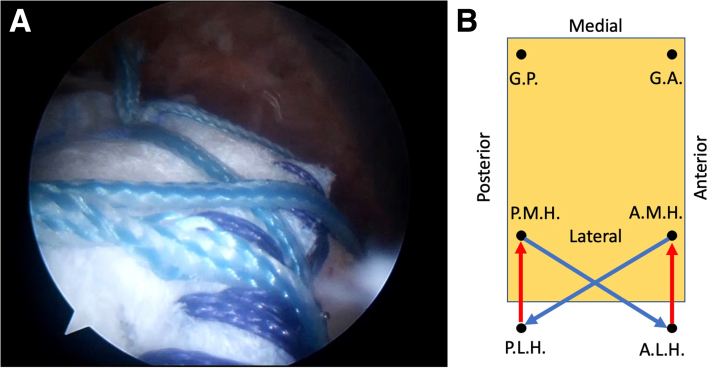
Fig 8.
(A) Images of a right shoulder in the lateral decubitus position viewing from the posterior portal of the final lateral fixation of the patch on the humeral greater tuberosity. (B) Method (view from above) for sizing the graft (in millimeters) used for superior capsular reconstruction. G.P., G.A. are anchors located on the superior glenoid neck. P.M.H., A.M.H. are anchors located on the medial row of the humeral head greater tuberosity. The distance between each hole and the border is 5 mm. The 10 mm added to the lateral border is the distance between anchors placed in the medial row (P.M.H. and A.M.H.) and those of the lateral row (P.L.H. and A.L.H.).
Discussion
Irreparable supraspinatus tear and superior capsule deficiency causes an unbalanced force couple in the coronal plane; this increases superior translation of the humeral head that results in decreased glenohumeral pressure and increased subacromial contact.11,13 Ishihara et al.14 in 2014 found that superior capsule deficiency increased anterior and superior humeral translation compared with intact capsule. On these findings, Mihata et al.10 based the SCR technique, to fully restore the humeral stability. They proposed that in a situation where the repair of the supraspinatus tendon is not possible to attach a patch on the superior glenoid neck and on the greater tuberosity.
Mihata et al.10 subsequently reported a series of 23 patients treated with SCR with fascia lata autograft fixed with a single row on the glenoid neck and a double row on the greater tuberosity; the repair was completed with side-to-side suture with the infraspinatus. After a minimum 2-year follow-up, patients showed significant abduction strength improvements. Postoperative MRI showed no improvements in muscle atrophy and arthrosis in 83% of patients.
Arthroscopic SCR is a relatively new procedure that remains technically challenging and time-consuming.12,15,16 Previous techniques used metal or peek anchors to fix the patch on the glenoid and greater tuberosity. The greater diameter of these anchors can cause complications: glenoid fractures or the impossibility to complete the technique in case of pull-out of the anchor during the procedure. The presence of hardware can also make more challenging future revision surgeries.
We aim to describe a more straightforward and safer procedure to make it more reproducible and less technically demanding.
Advantage/Disadvantages
Using soft anchors for medial and lateral fixation reduces possible intra/postoperative hardware complications.
Knotless anchors for the lateral row make the technique more accessible, making it easier to tension the lateral fixation, avoiding knot and hardware on the greater tuberosity.
All-suture anchors show biomechanical equivalence to conventional implants17, 18, 19, 20; they have smaller diameters that make them bone preserving,19,21,22 enabling the insertion of anchors closer to one another. Future revision surgeries will also be less challenging because of the absence of hardware and bone sparing.17,21,23,24
The significant number of sutures because of the 4 anchors on the greater tuberosity makes it difficult to correctly retrieve the suture in order to obtain the SpeedBridge repair. It is mandatory to understand the correct technique in order to avoid mistakes at this stage of the surgery.
Pearls and Pitfalls
It may be challenging to retrieve the suture tape from an anchor with the loop-ended shuttle suture of the other anchor. Having the lateral PassPort cannula helps make it easy to keep the suture in clear.
Positioning the lateral anchors on the greater tuberosity after the medial fixation of the patch on the glenoid neck reduces the number of sutures in the first part of the surgery, making it easier to manage the sutures; moreover, having the patch already in place helps in the positioning of the lateral anchors.
Footnotes
The author reports no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The video shows all the crucial steps of the "all soft" anchor superior capsular reconstruction technique described in the article.
References
- 1.Habermeyer P., Krieter C., Tang K lai, Lichtenberg S., Magosch P. A new arthroscopic classification of articular-sided supraspinatus footprint lesions: A prospective comparison with Snyder’s and Ellman’s classification. J Shoulder Elbow Surg. 2008;17(6):909–913. doi: 10.1016/j.jse.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 2.Juhan T., Stone M., Jalali O., et al. Irreparable rotator cuff tears: Current treatment options. Orthop Rev (Pavia) 2019;11(3):123–128. doi: 10.4081/or.2019.8146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sevivas N., Ferreira N., Andrade R., et al. Reverse shoulder arthroplasty for irreparable massive rotator cuff tears: A systematic review with meta-analysis and meta-regression. J Shoulder Elbow Surg. 2017;26(9):e265–e277. doi: 10.1016/j.jse.2017.03.039. [DOI] [PubMed] [Google Scholar]
- 4.Wagner E.R., Elhassan B.T. Surgical management of massive irreparable posterosuperior rotator cuff tears: Arthroscopic-assisted lower trapezius transfer. Curr Rev Musculoskelet Med. 2020;13(5):592–604. doi: 10.1007/s12178-020-09657-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stoll L.E., Codding J.L. Lower trapezius tendon transfer for massive irreparable rotator cuff tears. Orthop Clin North Am. 2019;50(3):375–382. doi: 10.1016/j.ocl.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Wall K.C., Toth A.P., Garrigues G.E. How to use a graft in irreparable rotator cuff tears: A literature review update of interposition and superior capsule reconstruction techniques. Curr Rev Musculoskelet Med. 2018;11(1):122–130. doi: 10.1007/s12178-018-9466-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Castricini R., Galasso O., Riccelli D.A., et al. Arthroscopic partial repair of irreparable, massive rotator cuff tears. Arthrosc Tech. 2017;6(1):e143–e147. doi: 10.1016/j.eats.2016.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ho J.C., Kane L., Stone M.A., Romeo A.A., Abboud J.A., Namdari S. Arthroscopic débridement of irreparable rotator cuff tears: Predictors of failure and success. J Shoulder Elbow Surg. 2020;29(4):e118–e123. doi: 10.1016/j.jse.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 9.Cvetanovich G.L., Waterman B.R., Verma N.N., Romeo A.A. Management of the irreparable rotator cuff tear. J Am Acad Orthop Surg. 2019;27(24):909–917. doi: 10.5435/JAAOS-D-18-00199. [DOI] [PubMed] [Google Scholar]
- 10.Mihata T., Lee T.Q., Watanabe C., et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29(3):459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 11.Mihata T., McGarry M.H., Pirolo J.M., Kinoshita M., Lee T.Q. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am J Sports Med Published online. 2012;40(10):2248–2255. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 12.Kim D.H., Jung Y.S., Kim K.R., Yoon J.P. The best options in superior capsular reconstruction. Clin Shoulder Elb. 2021;24(2):114–121. doi: 10.5397/cise.2021.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohn M.R., Vadhera A.S., Garrigues G.E., Verma N.N. Superior capsular reconstruction: Proposed biomechanical advantages. Arthroscopy. 2022;38(1):20–21. doi: 10.1016/j.arthro.2021.11.011. [DOI] [PubMed] [Google Scholar]
- 14.Ishihara Y., Mihata T., Tamboli M., et al. Role of the superior shoulder capsule in passive stability of the glenohumeral joint. J Shoulder Elbow Surg. 2014;23(5):642–648. doi: 10.1016/j.jse.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 15.Kholinne E., Jeon I.H. Arthroscopic superior capsular reconstruction of the shoulder: A narrative review. Ann Transl Med. 2021;9(3):268. doi: 10.21037/atm-20-5925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mancuso F., di Benedetto P., Tosolini L., Buttironi M.M., Beltrame A., Causero A. Treatment options for massive rotator cuff tears: A narrative review. Acta Biomedica. 2021 doi: 10.23750/abm.v92iS3.11766. 92:e2021026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nagra N.S., Zargar N., Smith R.D.J., Carr A.J. Mechanical properties of all-suture anchors for rotator cuff repair. Bone Joint Res. 2017;6(2):82–89. doi: 10.1302/2046-3758.62.BJR-2016-0225.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ntalos D., Sellenschloh K., Huber G., et al. Conventional rotator cuff versus all-suture anchors—A biomechanical study focusing on the insertion angle in an unlimited cyclic model. PLoS One. 2019;14(11):e0225648. doi: 10.1371/journal.pone.0225648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alan Barber F., Herbert M.A., Hapa O., et al. Biomechanical analysis of pullout strengths of rotator cuff and glenoid anchors: 2011 update. Arthroscopy. 2011;27(7):895–905. doi: 10.1016/j.arthro.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 20.Barber F.A., Herbert M.A. Cyclic loading biomechanical analysis of the pullout strengths of rotator cuff and glenoid anchors: 2013 update. Arthroscopy. 2013;29(5):832–844. doi: 10.1016/j.arthro.2013.01.028. [DOI] [PubMed] [Google Scholar]
- 21.Erickson J., Chiarappa F., Haskel J., et al. Biomechanical comparison of a first- and a second-generation all-soft suture glenoid anchor. Orthop J Sports Med. 2017;5(7) doi: 10.1177/2325967117717010. 2325967117717010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mazzocca A.D., Chowaniec D., Cote M.P., et al. Biomechanical evaluation of classic solid and novel all-soft suture anchors for glenoid labral repair. Arthroscopy. 2012;28(5):642–648. doi: 10.1016/j.arthro.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 23.Fleischli J.E. Editorial commentary: Biomechanics of all suture anchors: What we know so far. Arthroscopy. 2018;34(10):2796–2798. doi: 10.1016/j.arthro.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 24.Ruder J.A., Dickinson E.Y., Peindl R.D., Habet N.A., Fleischli J.E. Greater tuberosity decortication decreases load to failure of all-suture anchor constructs in rotator cuff repair. Arthroscopy. 2018;34(10):2777–2781. doi: 10.1016/j.arthro.2018.05.030. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The video shows all the crucial steps of the "all soft" anchor superior capsular reconstruction technique described in the article.
The video shows all the crucial steps of the "all soft" anchor superior capsular reconstruction technique described in the article.