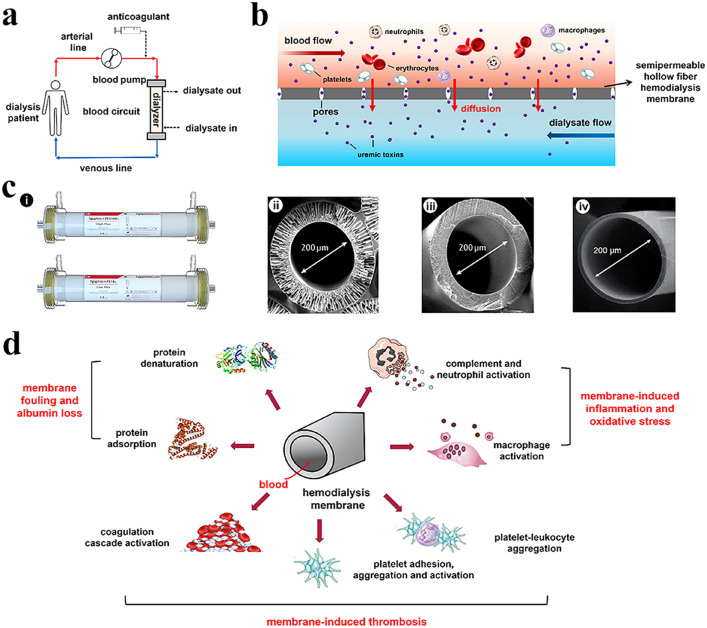
Fig. 1.
A brief introduction to hemodialysis procedures and adverse membrane-blood interactions. a Schematic diagram for hemodialysis procedures. Hemodialysis is performed by an extracorporeal method where blood is pumped through a semi-permeable hollow hemodialysis membrane (also termed a dialyzer or hemodialyzer) and then instilled into the intracorporeal blood circulation. Anticoagulants are usually administered to preserve the patency of the dialyzer and the blood flow. b Classical mechanism of solute exchange by diffusion during hemodialysis. Uremic toxins are transported across the dialyzer under the driving force of their concentration gradients between blood and dialysate. c Representative digital photographs of commercial polyethersulfone high-flux dialyzer (the upper) and polysulfone low-flux dialyzer (the lower) manufactured by NephroCan Inc. (i) and the cross-section scanning electron microscope (SEM) morphologies of polysulfone (ii), polyethersulfone (iii), and cellulose triacetate (iv) hollow-fiber hemodialysis membranes. d Adverse membrane-blood interactions when HFMs come into contact with blood. HFMs per se can induce protein adsorption and denaturation, as well as the activation of diverse blood cells, complement and coagulation systems, which finally result in unexpectedly decreased membrane diffusive permeability, increased serum albumin/protein loss, inflammatory cytokine release and oxidative stress and promote thrombus formation in the extracorporeal blood circuit, occlusion of hollow fibers and early termination of dialysis treatment in the worst situation