Abstract
A key issue in both research and clinical work with youth at clinical high risk (CHR) of psychosis is that there are clearly heterogenous clinical outcomes in addition to the development of psychosis. Thus, it is important to capture the psychopathologic outcomes of the CHR group and develop a core outcomes assessment set that may help in dissecting the heterogeneity and aid progress toward new treatments. In assessing psychopathology and often poor social and role functioning, we may be missing the important perspectives of the CHR individuals themselves. It is important to consider the perspectives of youth at CHR by using patient-reported outcome measures (PROMs). This systematic review of PROMs in CHR was conducted based on a comprehensive search of several databases and followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines. Sixty-four publications were included in the review examining PROMs for symptoms, functioning, quality of life, self-perceptions, stress, and resilience. Typically, PROMs were not the primary focus of the studies reviewed. The PROMs summarized here fit with results published elsewhere in the literature based on interviewer measures. However, very few of the measures used were validated for CHR or for youth. There are several recommendations for determining a core set of PROMs for use with CHR.
Keywords: psychosis, self-report, clinical assessments, ultra high risk
Introduction
A key issue that has recently become a major focus in both research and clinical work with youth at clinical high risk (CHR) of psychosis is that there are heterogenous clinical outcomes, in addition to the development of psychosis. That is, even though CHR individuals may not develop a full-blown psychotic illness, they do not necessarily make a full recovery.1 A recent special issue of Schizophrenia Research was dedicated to the notion that “embracing heterogeneity creates new opportunities for understanding and treating those at clinical high risk for psychosis.” Indeed, it is vital to capture the psychopathologic outcomes of the CHR group and, as Woods et al.2 suggest, to develop a core outcomes assessment set (COS) that may help in dissecting the heterogeneity and aid progress toward new treatments.
However, in assessing psychopathology and often poor social and role functioning, we may be missing the important perspectives of the CHR individuals themselves. In a response to Woods et al.2 and Petros et al.,3 point out that the assessment of CHR individuals has typically focused on vulnerability and illness with an emphasis on the transition to psychosis, and that few studies have investigated favorable or good outcomes including the protective or resilience factors that might actually contribute to such outcomes. This group has developed tools to determine good outcomes that would include not just clinician perspectives, but also the perspectives of the young people who may be at risk of developing psychosis.4 These tools showcase the importance of considering the perspectives of youth at CHR.
Thus, there may be the need to develop, as part of a COS, a core set of patient-reported outcomes (PRO) that could be used across different outcome studies. In fact, the US Food and Drug Administration made a commitment to advancing patient-focused drug development including use of patient experience data in regulatory decision-making. Some of the rational behind this is that patient experience data often provide supporting information in cases where the condition may not be that well defined or may be useful in conjunction with biomarkers of symptom or health improvement.5 This is in line with the current Accelerating Medicines Partnership® Schizophrenia (AMP® SCZ) program that aims to develop algorithms of clinical and biomarker data to determine outcomes of CHR youth which in turn can advance the testing of new pharmacological treatments.6 PRO may be very useful in such clinical trials, yet little is known about their use in CHR research.
Reininghaus and Priebe (2012) reviewed the use of patient-reported outcome measures (PROMs) in individuals with established psychosis.7 This review focused on treatment satisfaction, subjective quality of life, need for care, and the quality of the therapeutic relationship. Conclusions from this review were that, first, despite the increased use of PROMs in research studies, the evidence of their methodological quality remains limited; and second, there was a great deal of overlap across the measures, conceptually, operationally, and empirically. A second recent review of adults undergoing pharmacological and non-pharmacological interventions in mental health care found that PRO and clinician-reported outcomes supplemented each other and usually provided matching study conclusions.8
In both research and clinical settings, the use of PROMs with CHR youth has been limited due to the focus on clinician-reported outcomes. To the best of our knowledge, no systematic review has been conducted to summarize the use of PROMs in CHR youth. The first goal of this systematic review is to systematically search and identify how many studies used PROMs that assessed key outcomes such as symptoms, functioning, quality of life, resilience, stress levels, and self-perception amongst individuals at CHR for psychosis. There are many possible domains to address. However, we selected a limited number of domains based on the work of Petros et al.3,4 who identified functioning, symptoms, distress and suicidality, and subjective well-being as domains that were deemed important by both clinicians and patients and on the known outcomes that are typically reported in CHR studies. Our domains, therefore, included clinical symptoms, functioning, quality of life, resilience which fits with subjective well-being, stress level as this is an important factor in possibly increasing attenuated symptoms, and self-perception which included self-esteem, self-schemas, self-perception, and defeatist beliefs. Our second goal was to determine whether the PROMs used were specifically validated for the CHR population.
Methods
The study protocol for this systematic review was registered with the International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42021261500) and conducted in accordance with the PRISMA.9
Search Strategy
A comprehensive search of the following online databases was conducted: MEDLINE, CINAHL, EBM reviews, Embase, and PsycINFO. In addition, google scholar was manually searched (using keywords from the PubMed search strategy) for gray literature that would have been missed by the online database search. The search was executed on April 28, 2021, with no other date or geographic restrictions applied. Only literature published in English was included. The search strategy is outlined in supplementary material.
Inclusion/Exclusion Criteria
The following Population, Intervention, Comparison and Outcomes (PICOS) inclusion criteria were applied: (1) study population consisted of CHR, ultrahigh risk or otherwise at risk for psychosis individuals, (2) any or no intervention/control group, (3) one or more of the PROMs of interest: Quality of life, clinical symptoms, functioning, levels of stress, self-perception (including self-esteem, self-schemas, and defeatist beliefs), and resilience, and (4) one of the following study designs: Observational studies (retrospective cohort, prospective cohort, case–control, and cross-sectional) or intervention studies (randomized controlled trial, single-arm intervention trial).
The following exclusion criteria were applied: (1) formal assessments conducted by raters or clinicians to assess PRO of interest, or (2) studies with the following designs: Case studies, reviews, protocols, conference proceedings (not peer-reviewed), or validity studies.
Procedures
After the search was executed, all citations were screened based on their titles and abstracts in duplicate. However, since some of the articles of interest may not have reported PROMs in the abstract, the full PICOS criteria were not applied at the title/abstract stage. Then, of those with a positive screen at the title/abstract phase, the full-text articles were retrieved and assessed for full eligibility, also in duplicate. Any discrepancies were resolved by a third reviewer.
Relevant systematic reviews were recursively searched for any studies that may have been missed by the online database search.
A pilot data extraction test was undertaken on a sample of included studies prior to starting full data extraction. After completion of the pilot test, for studies that met the inclusion criteria, data were extracted in duplicate including study characteristics, patient characteristics, and PROMs and results. All conflicts were resolved by a third reviewer. Study mapping was then conducted to determine if any overlapping study populations were identified. Occasionally there were several publications reporting on the same study population. For studies that generated more than one publication, the publication that addressed the highest number of participants completing a given PROM from the study was selected and then any publications from the study that included other unique PROMs of interest were also included. Publications from studies that did not offer data on unique PROMs of interest were excluded.
Qualitative Synthesis
After completion of data extraction, since this was to be the first broad descriptive of the use of PROMs in CHR youth, a qualitative synthesis was conducted.
A quality assessment of the included studies was conducted using a modified checklist similar to a previously published review.10 The categories scored in the quality assessment checklist were: (1) role of the funding source in data interpretation and analysis, (2) sample size, (3) clearly reported inclusion criteria, (4) exclusion criteria, (5) reported sex distribution, (6) reported race/ethnic origin distribution, (7) reported IQ, educational level, and (8) reported dropout rate. Each item in the checklist was assigned a score of 0–2, with 0 being the lowest quality and 2 being the highest quality. In cases where the information was partially reported, a score of one was assigned. See supplementary material 2 for the quality assessment scoring checklist.
Evaluation of Validation
To determine if the included studies used validated PROMs, the included publications were assessed to determine if the publication reported any validation of the measures being used in the study or if any relevant validation was referenced. Since many of the measures were designed for adult populations or populations with serious mental illness, such as schizophrenia, the aim was to determine if the PROMs had been validated with or developed for CHR populations or even with or for youth populations.
First, all the included papers were checked to determine if the authors reported on psychometrics for the specific PROMs used. Secondly, if a reference for psychometric properties of the PROM was provided that was reviewed. Thirdly, a search was done to determine if any information in the literature could be obtained on the PROM.
Results
Search Results
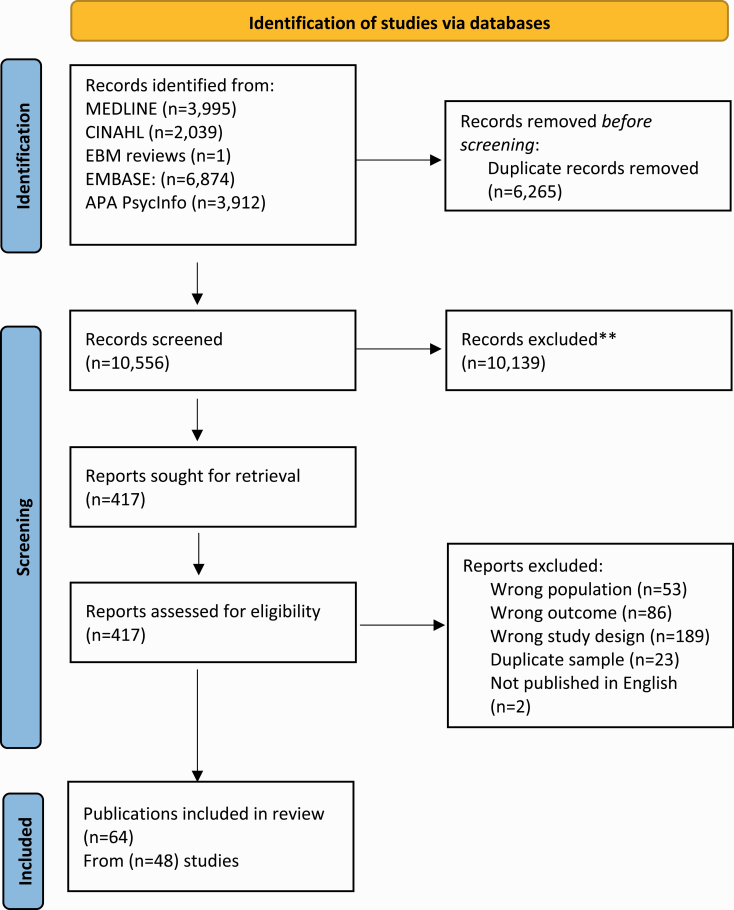
The search ascertained 16 821 citations, and after duplicates were removed, 10 556 were screened at the title/abstract phase. Of those, 417 were then assessed for eligibility to meet the PICOS criteria and ultimately, 64 publications met criteria coming from 48 unique studies (figure 1). Since participants in the included studies may be referred to as CHR, Ultra-High Risk, or At Risk For Mental State, in this paper and the tables we will use the term CHR to refer to all study participants.
Fig. 1.
PRISMA flow diagram.
Study Characteristics and Outcomes
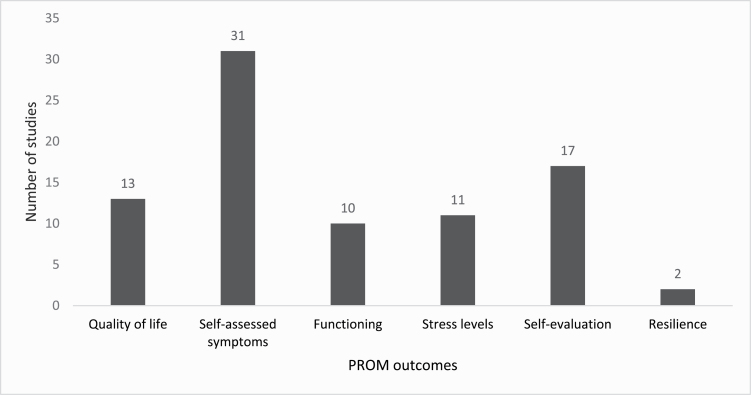
Supplementary material 3 summarizes the study characteristics of the 48 different studies included in this systematic review. Overall, 21 studies were conducted in Europe, 10 in North America, 9 in Asia, 3 in Australia, 3 in multiple continents, 1 in Israel, and 1 in Kenya. The range in CHR sample size, mean age and female distribution were 7–765 participants, 13.9–34.72 years, and 8.3%–84%, respectively. The most reported PROM amongst the included studies was clinical symptoms (n = 31), followed by self-perception (n = 17) and then quality of life (n = 13). See figure 2.
Fig. 2.
Number of studies reporting PROMs in CHR. Note: Counts are not mutually exclusive.
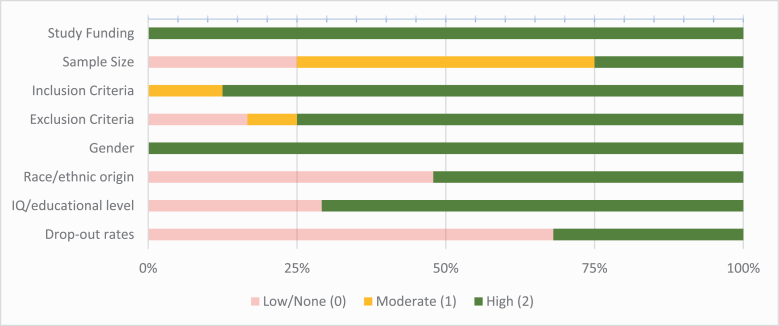
Quality Assessment
The quality of the included studies was assessed and reported in figure 3. Almost all studies reported the source of their study funding, inclusion/exclusion criteria, and at least some demographic characteristics that were of interest. However, most studies were observational, therefore overall dropout rate assessments were of low quality. Sample sizes were also on the smaller end with 75% of studies reporting CHR sample sizes of 100 or less.
Fig. 3.
Quality assessment of included studies.
Quality of Life
There were 13 studies that reported quality of life as a PROM.11–23 See table 1. The only quality of life tool used in more than one study was a variation of the World Health Organization Quality of Life questionnaire.11–16 Among the studies that compared CHR individuals and healthy controls, quality of life was consistently lower in CHR. Furthermore, among studies that reported quality of life over time, improvements were observed across most studies from baseline measurements, except for 2 of the treatment studies where there were no significant differences between baseline and 12 months of follow-up17 and 26 weeks of follow-up.18
Table 1.
Studies Using Quality of Life Measures
| First Author, Year | Questionnaire/Scale | Results |
|---|---|---|
| Glenthoj, 202017 | QoL-8D | CHR reported significantly poorer QoL than healthy controls. There were no significant differences in QoL between baseline and 12 months. |
| Ortega, 201922 | EQ-5D-3L | CHR reported significantly poorer QoL than healthy controls. |
| Nitka, 201619 | KIDSCREEN-27 Health-Related Quality of Life Questionnaire for Children and Adolescents | CHR reported significantly poorer physical well-being, psychological well-being, and school environment, than healthy controls. |
| Morrison, 201223 | MANSA | There were no significant treatment effects for QoL between CBT plus monitoring group versus monitoring only group at 6, 12, and 24 months. |
| Chang, 202020 | SF-12 | Those with comorbid diagnoses reported significantly poorer ratings on SF-12 mental and physical health domains compared to those with no comorbidity. |
| Kobayashi, 200921 | SWNS | Subjective well-being significantly improved between baseline and 4 weeks. There were no significant differences between baseline and 8 weeks. |
| Tsujino, 201318 | Subjective Well-being Under Neuroleptics - Short version | There were no significant differences in subjective well-being after 26 weeks of follow up. |
| Domínguez-Martínez, 201511 | WHOQoL-BREF | Poorer quality of life was associated with more severe symptoms and increased functional impairment. |
| Heinze, 201812 | BREF | CHR reported significantly poorer QoL than help seeking controls at baseline, and 3, 6, and 12 months. |
| Matsumoto, 201913 | BREF | CHR reported significantly improved QoL between baseline and 6 and 12 months. |
| Ohmuro, 201714 | BREF | CHR reported significantly poorer QoL than FEP except in domains of social relationships and environments. |
| Pelizza, 202115 | BREF | Poorer QOL was associated with increased levels of anhedonia. |
| Tsai, 202116 | BREF–Taiwan Version | Overall QoL and the psychological aspect of QoL significantly improved for the HASL program experimental group at post-test (1 week), and 6-, and 12-month follow-up. |
Note: CHR, clinical high risk; QoL, Quality of Life; FEP, first episode psychosis; HASL, Health-Awareness-Strengthening Lifestyle; AQoL-8D, Assessment of Quality of Life; EQ-5D-3L, Euro Quality of Life 5-dimensions Questionnaire – 3-level version; MANSA, Manchester short assessment of quality of life; SF-12, Short Form-12 Health Survey; SWNS, Subjective Well-being Under Neuroleptics, Short version; WHOQoL-BREF, World Health Organization Quality of Life-Brief Version.
Clinical Symptoms
Table 2 presents the 31 studies that reported self-reported symptoms amongst CHR individuals.
Table 2.
Studies Using Measures of Clinical Symptoms
| First Author, Year | Questionnaire/Scale | Results |
|---|---|---|
| DeVylder, 201334 | BAI BDI |
CHR reported significantly more severe anxiety and depression than healthy controls. |
| Olvet, 201533 | BAI BDI CDI |
CHR reported significantly more severe anxiety and depression than healthy controls. |
| Atkinson, 201730 | BDI-II | CHR reported significantly more severe anxiety and depression than healthy controls. |
| Cowan, 201931 | BAI BDI-II |
CHR reported significantly more severe anxiety and depression than healthy controls. |
| Lederman, 201732 | BAI BDI-II |
CHR reported significantly more severe depression compared to healthy controls and FEP. |
| Popovic, 202041 | BDI | CHR reported significantly more severe depression scores than healthy controls. |
| Salokangas, 201942 | BDI | Among CHR, depression symptoms decreased significantly from baseline to follow-up. |
| Choi, 201740 | BDI-II | CHR reported significantly more severe depression symptoms than healthy controls. |
| Matsumoto, 201913 | BDI-II STAI |
CHR clinical measures significantly improved from baseline to 6 and 12 months. |
| Ohmuro, 201714 | BDI-II | CHR reported significantly more severe depressive symptoms than FEP. |
| Pelizza, 202115 | BDI-II BOL |
CHR reported significantly more severe depressive symptoms than FEP and non-CHR. |
| Appiah-Kusi, 201736 | BDI-II STAI |
CHR reported significantly more depression and anxiety than healthy controls. |
| Izon, 202123 | BDI-II SIAS |
Depression but not anxiety in CHR was associated with high expressed emotion in the CHR family. |
| Rietdijk, 201329 | BDI-II SIAS |
Among CHR, women reported significantly more severe depression and anxiety symptoms than men. |
| Morrison, 201223 | BDI-PC Social Interaction Anxiety Scale |
CHR treatment effects were nonsignificant on reported depression and anxiety symptoms. |
| Blessing, 201743 | BSI-18 | CHR reported significantly less severe symptoms on the BSI-18 after communication of diagnosis. |
| Tsai, 202116 | CMSTAI-Y | After CHR participated in the HASL program, the experimental CHR group reported significantly less severe state and trait anxiety than the nonexperimental CHR group. |
| Veling, 201628 | CAPE GPTS SIAS |
CHR and psychosis patients reported significantly more severe levels of all symptoms in comparison to healthy controls. |
| Geraets, 201824 | CAPE SIAS |
CHR reported significantly more severe positive, negative, depressive, and social anxiety symptoms than healthy controls. |
| González-Rodríguez, 201444 | FCQ | Reports of basic symptoms on the FCQ were not significantly different between CHR and FEP. |
| Barkus, 201047 |
GHQ | CHR reported higher scores on the GHQ than healthy controls. CHR reported significantly more severe psychiatric symptoms on the GHQ than healthy controls. |
| Morrison, 200648 | GHQ | CHR reported significantly more severe psychiatric symptoms on the GHQ than the healthy controls. |
| Marshall, 201226 | GHQ SAS SIAS |
CHR reported significant improvements in symptoms reported on the GHQ at each follow-up assessment compared with baseline; CHR reported significant improvements in anxiety symptoms over time at each assessment, relative to baseline. |
| Heinze, 201812 | K-10 OASIS |
CHR reported significantly more severe levels of depressive symptoms and psychological distress relative to non-CHR; there were no significant differences in reported anxiety compared to non-UHR. |
| Koren, 201638 | MASQ | Participants with APS reported significantly more severe symptoms (subscales: mixed, anxiety, depression, arousal, anhedonia) than non-APS. |
| Lincoln, 201835 | SAS | CHR reported significant improvements in anxiety symptoms over time compared to baseline. |
| McAusland, 201727 | SAS SIAS |
CHR reported significantly more severe anxiety symptoms than healthy controls; female participants reported more severe anxiety symptoms than males. |
| Cressman, 201537 | SAS-A | CHR reported significantly more severe social anxiety symptoms and social adjustment than healthy controls. |
| Valmaggia, 201539 | SSPS DASS |
CHR reported significantly more severe paranoid appraisals than healthy controls; CHR status was not significantly associated with depression or anxiety. |
| Langbein, 201845 | SCL-90-R | CHR, FEP and healthy controls reported significant differences in the global severity index and on all symptom subscales. |
| Manninen, 201446 | YSR | CHR met the clinical range significantly more often for anxious/depressed, withdrawn/depressed and thought problem symptoms than non-CHR. |
Note: CHR, clinical high risk; FEP, first episode psychosis; HASL, Health-Awareness-Strengthening Lifestyle; APS, attenuated psychosis syndrome; BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; CDI, Children’s Depression Inventory; BDI-II, Beck Depression Inventory II; STAI, state-trait anxiety inventory; SIAS, Social Interaction Anxiety Scale; BOL, Brief O-Life Questionnaire; BDI-PC, Beck Depression Inventory for Primary Care; BSI-18, Brief Symptom Inventory-18; CMSTAI-Y, Chinese Mandarin State and Trait Anxiety Inventory Form Y; CAPE, Community Assessment of Psychic Experiences; GPTS, Green Paranoid Thoughts Scale; FCQ, Frankfurt Complaint Questionnaire; GHQ, Goldberg Health Questionnaire; SAS, Social Anxiety Scale; K-10, Kessler Psychological Distress Scale; OASIS, Overall Anxiety Severity and Impairment Scale; MASQ, Mood and Anxiety Symptom Questionnaire; SAS-A, Social Anxiety Scale for Adolescents; SSPS, State Social Paranoia Scale; DASS, The Depression, Anxiety and Stress Scale; SCL-90-R, Symptom Checklist 1990 Revised; YSR, Youth self-report.
Nineteen studies had self-reported anxiety outcomes. Seven studies used the Social Interaction Anxiety Scale,23–29 5 used the Beck Anxiety Inventory,30–34 3 used the Social Anxiety Scale,26,27,35 3 studies used the State-Trait Anxiety Inventory form,13,16,36 and the remaining studies used other types of assessments.12,37–39 Overall, it was found that generally, CHR participants reported more anxiety and social anxiety symptoms than healthy controls and non-CHR. Over time, anxiety improved in CHR when compared to baseline measurements.13,26,35
Sixteen studies self-reported depression symptoms, fifteen of them using the Beck Depression Inventory. Across studies, it was consistently found that CHR reported more depressive symptoms than non-CHR participants.14,15,25,30–34,36,40,41 Similar to anxiety symptoms, depressive symptoms seemed to improve longitudinally.13,42 One study found that depressive symptoms were more prevalent in female CHR participants.29 Seven studies reported on general symptom scales typically including both anxiety and depression,38,39,43–47 where CHR participants usually presented with increased symptoms, relative to healthy controls with the one exception being on the Depression, Anxiety and Stress Scale.39
Psychotic-like experiences were self-reported in 2 studies,24,28 while only one study reported self-measured negative symptoms.24 Of the studies investigating positive and negative symptoms, only one measure was used in more than one study, the Community Assessment of Psychic Experiences.24,28 Overall, CHR participants had more positive and negative symptoms than non-CHR participants.
Finally, 2 studies reported on the general health questionnaire26,48 on which CHR had poorer ratings than healthy controls. One study used the Kessler Psychological Distress Scale,12 on which CHR presented with increased psychological distress relative to non-CHR.
Functioning
Functioning was self-reported in 10 studies as presented in table 3. Four studies used the Social Adjustment Scale,37,40,49,50 2 used the Social Functioning Scale,51,52 while the rest used 4 separate measures namely measures of adaptive functioning, social responsiveness, social adaptation, and the Sheehan Disability scale.17,22,33,53 Overall, those in the CHR group generally scored lower in functioning and social adjustment and higher in social impairment in comparison to healthy controls and non-CHR.17,22,33,37,40,49,50 Among CHR, premorbid functioning was shown to be related to poorer social functioning.52 One longitudinal study found no significant changes in social impairment when measuring CHR from baseline to a 12-month follow-up,17 nor was any change observed posttreatment.51
Table 3.
Studies Using Measures of Functioning
| First Author, Year | Questionnaire/Scale | Results |
|---|---|---|
| De Wit, 201453 | Adaptative Functioning Scale “Friends” on the ASEBA-ASR | There were no significant differences in social functioning between those who did and did not remit from CHR status. |
| Olvet, 201533 | SDS | CHR reported significantly poorer SDS percentage scores than healthy controls. |
| Ortega, 201822 | SASS | CHR reported significantly poorer social adaptation than healthy controls. |
| Cressman, 201537 | SAS-SR | CHR reported significantly more severe social anxiety and poorer social adjustment than healthy controls. |
| Choi, 201740 | SAS-SR | CHR reported significantly more severe anxiety, depression, and poorer social functioning than healthy controls. |
| Corcoran, 201149 | SAS-SR | CHR reported significantly more severe anxiety, depression, and poorer social functioning than healthy controls. |
| Lincoln, 201450 | SAS-SR | CHR reported significantly more severe social impairment than healthy controls. |
| Addington, 201151 | SFS | There were no significant differences in social functioning between the CBT and supportive therapy intervention groups at baseline, 6,12, or 18 months. |
| Lyngberg, 201552 | SFS | There was a significant correlation between good social functioning and good premorbid functioning during early and late adolescence. |
| Glenthoj, 202017 | SRS-A | There were no significant differences in functioning between baseline and 12-month follow-up. CHR reported significantly more severe social impairment than healthy controls. |
Note: Abbreviations are explained in the first footnote to table 1. ASEBA-ASR, Achenbach System of Empirically Based Assessment – Adult Self-Report; SDS, Sheehan Disability Scale; SASS, Social Adaptation Self-evaluation Scale; SAS-SR, Social Adjustment Scale Self-Report; SFS, Social Functioning Scale; SRS-A, Social Responsiveness Scale, Adult Version;
Stress Levels
Table 4 summarizes 11 studies that reported on self-rated stress or stress levels, and of those, 6 studies used the Perceived Stress Scale,22,34,54–57 and all other studies used unique stress assessment tools.58–62 Although the stress assessment tools varied across studies, CHR individuals consistently had higher stress levels relative to healthy controls, and no differences in stress between CHR, first episode of psychosis, or multiple episode psychosis individuals were observed.
Table 4.
Studies Reporting Stress Levels
| First Author, Year | Questionnaire/Scale | Results |
|---|---|---|
| Bentley, 201658 | BASC-2 | CHR reported a significant relation between parent–child relationships and social stress; significant negative association between positive parent–child relationships and lower social stress in CHR. |
| Cullen, 202059 | DSI | CHR reported significantly more severe daily stress relative to healthy controls and remitted CHR; symptomatic, progressed and converted groups also reported significantly more daily stressor exposures relative to remitted CHR. |
| Appiah-Kusi, 202057 | PSS | CHR reported significantly more severe stress than healthy controls. |
| DeVylder, 201334 |
PSS | CHR reported perceived stress at baseline which was associated with impaired stress tolerance assessed with SOPS. |
| Nordholm, 201654 |
PSS | CHR experienced significantly more severe perceived stress than healthy controls. |
| Phillips, 201255 |
PSS | CHR reported significantly more severe stress than healthy controls. |
| Ortega, 201822 | PSS HRSRS |
CHR reported significantly more severe perceived stress and more severe stressful life events, relative to healthy controls. |
| Studerus, 202156 | PSS-10 | CHR reported significantly more severe overall stress than healthy controls. |
| Kommescher, 201760 | SCQ | CHR, first episode or multiple episode psychosis individuals had no significant differences in any of the subscales except for devaluation. |
| Pruessner, 201162 | TICS | CHR reported significantly more severe perceived stress in the past month and past year, relative to healthy controls. |
| Mamah, 202061 | WERC | For CHR, stress and high harm avoidance, low self-directedness, low cooperativeness, and high self-transcendence were significantly related. |
Note: Abbreviation is explained in the first footnote to table 1. SOPS, Scale of Psychosis-Risk Symptoms; BASC-2, Behavior Assessment System for Children Second Edition; DSI, Daily Stress Inventory; PSS, Perceived Stress Scale; HRSRS, Holmes-Rahe Social Readjustment Scale; PSS-10, Perceived Stress Scale - 10-item version; SCQ, Stress Coping Questionnaire; TICS, Trier Inventory for Chronic Stress; WERC, Washington Early Recognition Center Stress Screen.
Self-Perception
Seventeen studies reported self-perception outcomes that included measures of self-esteem, self-schemas, self-perception, and defeatist beliefs, presented in table 5. Six studies measured self-esteem, 3 used the Rosenberg Self-Esteem Scale,30,63,64 2 studies used the Self-Esteem Rating Scale62 (one used the short-form version65) and one study used the Self-Perception Profile for Adults.66 Across several studies, CHR individuals were found to have lower self-esteem relative to healthy controls,30,62,64,66 and a longitudinal study reported that self-esteem in CHR did not significantly improve over time.65
Table 5.
Studies Reporting Measures of Self-perceptions
| First Author, Year | Questionnaire/Scale | Results |
| Cowan, 201931 | BCSS | CHR reported significantly more negative beliefs about self and others and significantly fewer positive beliefs about self and other, relative to health controls. |
| Stowkowy, 201267 | BCSS | CHR reported significantly more negative schemas about the self and others. |
| Stowkowy, 201668 |
BCSS | CHR reported significantly more severe negative schemas about the self and about other people compared to healthy controls. |
| Taylor, 201469 | BCSS | CHR had no significant differences in negative or positive beliefs about the self, relative to FEP. |
| Clay, 202073 | DPB | CHR reported significantly more severe DPBs than healthy controls. |
| Morrison, 200648 | DAS PQQ |
CHR reported significantly more severe beliefs about rejection and criticism from others, and significant discrepancies in self-perception, and general mental distress. |
| Blessing, 201743 | LCS | CHR reported significantly increased internal locus of control ratings after communication of diagnosis. |
| Pyle, 201571 | PBEQ | Internalized stigma was significantly related to depression, social anxiety, distress due to unusual psychological experiences, and suicidal thinking in CHR. |
| Stowkowy, 201572 | PBEQ | CHR who transitioned to psychosis agreed more to statements concerning lack of control over experiences; all sub-scores were significantly related to the CDSS and to SOPS negative symptoms with the exception of self as experiences, which was unrelated to negative symptoms. |
| Atkinson, 201730 | RSES | CHR participants reported significantly poorer self-esteem than healthy controls. |
| Jhung, 201663 | RSES | In CHR, no significant correlations of noncurrent or current emotional experiences (anhedonia and SAM scales) were found with self-esteem. |
| Shi, 201764 |
RSES | CHR reported significantly poorer self-esteem relative to healthy controls; in CHR, poorer self-esteem was significantly associated with more severe positive, negative, and depressive symptoms. In CHR, higher self-esteem was significantly and positively correlated with GAF; Self-esteem significantly improved in CHR after treatment (6 months). |
| Pruessner, 201162 |
SERS | CHR reported significantly poorer protective factors (self-esteem, social support, and active coping), relative to healthy controls; more severe stress in the past month was significantly related to lower self-esteem. |
| Alvarez-Jimenez, 201865 | SERS-SF SES |
No significant improvement in self-esteem or self-efficacy between baseline and follow-up were found. |
| Seo, 201870 | SPS | CHR reported significantly poorer self-perception than healthy controls. |
| Benavides, 201866 | SPPA | CHR and SCZ had significantly poorer GSE compared to healthy controls, but no significant differences between CHR and SCZ. |
| Valmaggia, 201539 | Social Entrapment and Defeat Scales | CHR reported significantly more severe levels of social defeat than healthy controls. |
Note: Abbreviations are explained in the first footnote to table 1. CDSS, Calgary Depression Scale for Schizophrenia; SOPS, Scale of Psychosis-Risk Symptoms; SAM, Self-Assessment Manikin; GAF, Global Assessment of Functioning; SCZ, Schizophrenia; GSE, Global Self-Esteem; BCSS, Brief Core Schema Scale; DPB, Defeatist Performance Beliefs Questionnaire; DAS, Dysfunctional Attitudes Scale; PQQ, Personal Qualities Questionnaire; LCS, Locus of Control Scale; PBEQ, Personal Beliefs about Experiences Questionnaire; RSES, Rosenberg Self-Esteem Scale; SERS, Self-Esteem Rating Scale; SERS-SF, Self-Esteem Rating Scale Short Form; SES, Self-Efficacy Scale; SPS, Self-Perception Scale; SPPA, Self-Perception Profile for Adults.
Six studies reported on self-schemas or self-perception: Four used the Brief Core Schema Scale,31,67–69 one used the Self-Perception Scale,70 and one used the Personal Qualities Questionnaire.48 Among studies comparing CHR and healthy controls, CHR reported increased negative schemas and decreased positive schemas about themselves and others.31,48,67,68,70 It was also found that CHR had greater negative self-perception when compared to a healthy control group.70 Negative schemas/beliefs were found to be correlated with non-bizarre thoughts and perceptual abnormalities severity subscales as rated on the CAARMS69 and attenuated psychotic positive symptoms rated on the Scale of Psychosis-risk Symptoms.67
For defeatist beliefs, 7 studies reported outcomes: Two studies used the Personal Beliefs About Experience Questionnaire,71,72 one study used the Dysfunctional Attitudes Questionnaire,48 one study used the Defeatist Performance Beliefs Questionnaire,73 one used the Self-Efficacy Scale,65 one used the Locus of Control Ratings Scale,43 and one used Social Entrapment and Defeat Scales.39 CHR individuals endorsed more defeatist performance beliefs,73 and social defeat39 relative to healthy controls. A study examining self-efficacy longitudinally found that it did not improve over time in individuals at CHR.65 Although another study found that after communication of a diagnosis, internal locus of control ratings increased.43
Resilience
Two studies reported resilience as a PROM.74,75 One study measured resilience using the Connor-Davidson Resilience Scale,74 while the other study used the Child and Youth Resilience Measure.75 Both studies found that CHR individuals were less resilient than healthy controls and those CHR individuals who transitioned to psychosis or had persistent symptoms were less resilient than those who did not make the transition or had remitted at follow-up assessments.
Validation
In total, 8 of the 84 PROMs included had been reportedly validated in varying degrees in CHR populations, with an additional 19 that had been developed or validated for youth. A total list of all PROMs noting those that had been validated for youth and/or CHR can be found in supplementary material 4. Table 6 reports on the psychometrics of the 8 measures that have some validation for CHR populations. Detailed description of the sources of this information is presented in supplementary material 5.
Table 6.
Psychometric Properties of PROMs Validated for CHR
| Measure | Test–Retest Reliability | Internal Consistency | Construct Validity | Convergent Validity | Discriminative Validity |
Criterion Validity | Group Differences | Responsiveness to Change |
|---|---|---|---|---|---|---|---|---|
| BDI | NR | √ | √ | √ | √ | √ | √ | √ |
| BASC-2 | NR | NR | NR | √ | NR | √ | √ | NR |
| CAPE | √a | √ | NR | √ | LIMITED | √ | √ | NR |
| FCQ | NR | √ | NR | NO | NR | NO | NR | NR |
| LSHS-R | NR | √ | NR | √ | √ | √ | √ | NR |
| SFS | NR | √ | NR | √ | √ | NR | √ | NR |
| WERCAP | √ | √ | NR | NR | √ | √ | √ | √ |
| BCSS | NR | √ | NR | √ | √ | √ | NR | NR |
Note: BDI, Beck Depression Inventory; BASC-2, Behaviour Assessment System for Children Second Edition; CAPE, Community Assessment of Psychic Experiences; FCQ, Frankfurt Complaint Questionnaire; LSHS-R, Launay-Slade Hallucinations Scale; SFS, Social Functioning Scale; WERCAP, Washington Early Recognition Center Affectivity and Psychosis Screen; BCSS, Brief Core Schema Scale, NR, not reported; NO, tested but did not meet that criteria; PROMs, patient-reported outcome measures; CHR, cilinical high risk.
aJust for positive symptoms.
Discussion
This review presented a variety of PROMs examined among CHR individuals. We identified 64 publications from 48 unique CHR study populations measuring the PROMs of interest. The most common PROs reported in the included studies were symptoms (mainly anxiety and depression), followed by self-perception measures, and then stress levels. In general, outcomes of the different PROMS suggested that CHR participants tended to present with more symptoms, poorer self-perception, increased stress, poorer functioning, and quality of life than healthy controls. Furthermore, over time symptoms, but not functioning, tended to improve. All of these outcomes are, for the most part, supported in the CHR literature with the use of interviewer measures.76
To the best of our knowledge, this is the first systematic review to synthesize the reporting of a wide range of PROMs used with CHR populations, and therefore, provides an overview of the current state of the field highlighting the need for further research in this area. A strength of this review was the inclusion of 64 publications representing 48 unique study populations of CHR individuals. We searched numerous online databases, screened, and extracted publications in duplicate, published our protocol a priori, and followed PRISMA guidelines for systematic review conduct, thus making this review the most comprehensive systematic review reporting the PROMs of interest in CHR to date.
However, this study had several limitations that need to be acknowledged. We made an informed decision to explore specific domains of PROs. This meant that certain domains were missing. We did not include any concepts in the cognitive domain such as metacognitions. There is a wide literature on metacognitions in CHR where much of the literature does not particularly focus on outcome but rather on whether this could be a difficulty that could be considered as a predictor of psychosis.77 We did not include domains such as social support or coping styles that may be useful as correlates of different outcomes.
Secondly, there were limited treatment studies (particularly randomized controlled trials),78 that used the PROMs of interest in this review, more often these studies used clinician-reported measures to assess the main outcome. Many of the treatment studies made use of PROMs, such as perceived self-support, coping skills, appraisal of the therapeutic relationship, and treatment satisfaction that were not under review in this paper. These measures would be of value in treatment studies, yet the use of these PROMs is limited in the literature. Of note, one useful method to capture PRO that was not addressed in this review is the use of experience sampling methods, for example, the work of van der Steen et al.79 and Gerritsen et al.80
Secondly, although PROMs provide observations of experiences from the participant’s perspective, self-reported outcomes can be subject to social desirability bias or recall error that may lead to misclassification of these outcomes. Careful assessment and focus on participant experience through standardized/validated measures would help to mitigate these concerns.
Thirdly, in most of the included studies, the PROMs were not the primary focus of the study’s aims. Thus, sample sizes of CHR individuals may have not been powered to appropriately assess the PROMs, and therefore, future studies focusing on these outcomes in larger samples would be of interest. Next, none of the papers offered comparisons between the PROMs and interviewer-administered measures as was done in a previously published PROM review.8
Finally, there was limited evidence as to whether many of these PROMs were validated for CHR or even youth. We reported that less than 10% of the reported PROMs had been validated for CHR and one-third with youth populations. We searched for reports on psychometrics for these PROMs to the best of our ability but are aware that there may be more recent papers or papers that were missed that might have been added to our reported psychometrics. Regardless it was still a small proportion that had been validated. A recent publication by Buck et al.81 advocated strongly for psychometrically sound instruments to track and evaluate clinical outcome. In their comprehensive review of PROMs for treatment outcome in schizophrenia they reported on 12 PROMs. Their findings demonstrated that most measures showed strengths in internal consistency and test–retest reliability with several of the 12 having evidence of convergent or criterion validity.
Future Directions
Thus, in order to include PROMs in a core outcomes assessment certain criteria should be considered. The first recommendation is to use PROMs that are validated for CHR and/or youth that have demonstrated psychometric strengths. This may mean that the choice of measures will be limited to a few in each of the different clinical domains to ensure having PROMs with good psychometrics vs. the wide range that has been reported in this review. Other important methodological criteria to consider would be, in addition to validity, sensitivity, reliability, generalizability, and feasibility. The measure should have relevance for a youth population, something that might be achieved by obtaining the individual perspectives and involvement of CHR individuals in developing PROMs. For example, Petros et al.4 determined what PROs, in particular good outcomes, were meaningful to CHR youth who were service users. Furthermore, the measure should be brief and the use of several PROMs should be avoided unless they address clearly distinct domains.7 Finally, PROMs should be matched to the aims of the specific study in that the participant perspective is being considered as a healthcare outcome.82 For clinical and functional outcomes, it might mean selecting measures that match the interviewer-rated domains to determine how the participant sees the clinical change. For both clinical and observational studies an aim might be to understand the participants’ sense of subjective well-being.
There have been efforts to identify, evaluate and recommend validated PROMs through various national guidelines. Most notable was the collaboration in the US between the National Institute of Health and several outcome scientists to develop the patient-reported outcomes measurement information system.83,84 Thus, one option might be to work through the patient-reported outcomes measurement information system (www.healthmeasures.net) to find relevant measures or learning from patient-reported outcome measurement information system how to adapt and validate the most relevant measures for CHR youth.
Thus, in summary, determining a core set of well-validated PROMs, specifically for CHR individuals, would allow for a more robust understanding of CHR individuals to aid in determining future treatments and improved care.
Supplementary Material
Acknowledgment
We would like to thank Thea Placsko for her help in reviewing abstracts and manuscripts.
Contributor Information
Jean Addington, Department of Psychiatry, Hotchkiss Brain Institute, University of Calgary, Calgary, AB, Canada.
Amanda Chao, Department of Psychiatry, Hotchkiss Brain Institute, University of Calgary, Calgary, AB, Canada.
Amy Braun, Department of Psychiatry, Hotchkiss Brain Institute, University of Calgary, Calgary, AB, Canada.
Madeline Miller, Department of Psychiatry, Hotchkiss Brain Institute, University of Calgary, Calgary, AB, Canada.
Megan S Farris, Department of Psychiatry, Hotchkiss Brain Institute, University of Calgary, Calgary, AB, Canada.
Funding
This work was supported by the Novartis Chair in Schizophrenia Research held by J. Addington and by the National Institutes of Health (NIH) subaward grant (GR110977) to J. Addington as part of the ProNET: Psychosis-Risk Outcomes Network NIH grant (MH124639).
References
- 1.Addington J, Cornblatt BA, Cadenhead KS, et al. . At clinical high risk for psychosis: outcome for nonconverters. Am J Psychiatry. 2011;168(8):800–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woods SW, Mourgues-Codern CV, Powers AR.. Commentary. Toward a core outcomes assessment set for clinical high risk. Schizophr Res. 2021;227:78–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petros N, Cullen AE, Fusar-Poli P, Mechelli A, McGuire P.. Towards standardising the assessment of good outcome in people at clinical high risk for psychosis: a collaborative approach. Schizophr Res. 2020;223:361–362. [DOI] [PubMed] [Google Scholar]
- 4.Petros N, Cullen AE, Vieira S, et al. . Examining service‐user perspectives for the development of a good outcome checklist for individuals at clinical high risk for psychosis. Early Interv Psychiatry. 2020;15(3):606–615. [DOI] [PubMed] [Google Scholar]
- 5.Group ER. Assessment of the use of patient experience data in regulatory decision-making. In: Services HaH, ed. USA: Food and Drug Administration; 2021. https://www.fda.gov/drugs/development-approval-process-drugs/assessment-use-patient-experience-data-regulatory-decision-making. [Google Scholar]
- 6.Brady LS, Larrauri CA, Committee ASS.. Accelerating medicines partnership® schizophrenia (AMP® SCZ): developing tools to enable early intervention in the psychosis high risk state. World Psychiatry. 2023;22(1):42–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reininghaus U, Priebe S.. Measuring patient-reported outcomes in psychosis: conceptual and methodological review. Br J Psychiatry. 2012;201(4):262–267. [DOI] [PubMed] [Google Scholar]
- 8.Baandrup L, Rasmussen J, Mainz J, Videbech P, Kristensen S.. Patient-reported outcome measures in mental health clinical research: a descriptive review in comparison with clinician-rated outcome measures. Int J Qual Health Care. 2021;34(supplement_1):ii70–ii97. [DOI] [PubMed] [Google Scholar]
- 9.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Metzak PD, Farris MS, Placsko T, et al. . Social functioning and brain imaging in individuals at clinical high-risk for psychosis: a systematic review. Schizophr Res. 2021;233:3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Domínguez-Martínez T, Kwapil TR, Barrantes-Vidal N.. Subjective quality of life in at-risk mental state for psychosis patients: relationship with symptom severity and functional impairment. Early Interv Psychiatry. 2015;9(4):292–299. [DOI] [PubMed] [Google Scholar]
- 12.Heinze K, Lin A, Nelson B, et al. . The impact of psychotic experiences in the early stages of mental health problems in young people. BMC Psychiatry. 2018;18(1):214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsumoto K, Ohmuro N, Tsujino N, et al. . Open-label study of cognitive behavioural therapy for individuals with at-risk mental state: feasibility in the Japanese clinical setting. Early Interv Psychiatry. 2019;13(1):137–141. [DOI] [PubMed] [Google Scholar]
- 14.Ohmuro N, Matsumoto K, Ishii Y, et al. . The associations between quality of life and clinical symptoms in individuals with an at-risk mental state and first-episode psychosis. Psychiatry Res. 2017;254:54–59. [DOI] [PubMed] [Google Scholar]
- 15.Pelizza L, Azzali S, Paterlini F, et al. . Anhedonia in the psychosis risk syndrome: state and trait characteristics. Psychiatr Danub. 2021;33(1):36–47. [DOI] [PubMed] [Google Scholar]
- 16.Tsai CL, Lin YW, Hsu HC, et al. . Effects of the health-awareness-strengthening lifestyle program in a randomized trial of young adults with an at-risk mental state. Int J Environ Res Public Health. 2021;18(4):1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glenthoj LB, Kristensen TD, Wenneberg C, Hjorthoj C, Nordentoft M.. Experiential negative symptoms are more predictive of real-life functional outcome than expressive negative symptoms in clinical high-risk states. Schizophr Res. 2020;218:151–156. [DOI] [PubMed] [Google Scholar]
- 18.Tsujino N, Nemoto T, Morita K, Katagiri N, Ito S, Mizuno M.. Long-term efficacy and tolerability of perospirone for young help-seeking people at clinical high risk: a preliminary open trial. Clin Psychopharmacol Neurosci. 2013;11(3):132–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nitka F, Richter J, Parzer P, Resch F, Henze R.. Health-related quality of life among adolescents: a comparison between subjects at ultra-high risk for psychosis and healthy controls. Psychiatry Res. 2016;235:110–115. [DOI] [PubMed] [Google Scholar]
- 20.Chang WC, Ng CM, Chan KN, et al. . Psychiatric comorbidity in individuals at-risk for psychosis: relationships with symptoms, cognition and psychosocial functioning. Early Interv Psychiatry. 2020;5(3):616–623. [DOI] [PubMed] [Google Scholar]
- 21.Kobayashi H, Morita K, Takeshi K, et al. . Effects of aripiprazole on insight and subjective experience in individuals with an at-risk mental state. J Clin Psychopharmacol. 2009;29(5):421–425. [DOI] [PubMed] [Google Scholar]
- 22.Ortega L, Montalvo I, Monseny R, Vilella E, Labad J.. Perceived stress mediates the relationship between social adaptation and quality of life in individuals at ultra high risk of psychosis. Early Interv Psychiatry. 2019;13(6):1447–1454. [DOI] [PubMed] [Google Scholar]
- 23.Morrison AP, French P, Stewart SL, et al. . Early detection and intervention evaluation for people at risk of psychosis: multisite randomised controlled trial. BMJ. 2012;344:e2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Geraets CNW, van Beilen M, Pot-Kolder R, Counotte J, van der Gaag M, Veling W.. Social environments and interpersonal distance regulation in psychosis: a virtual reality study. Schizophr Res. 2018;192:96–101. [DOI] [PubMed] [Google Scholar]
- 25.Izon E, Berry K, Wearden A, Carter LA, Law H, French P.. Investigating expressed emotion in individuals at-risk of developing psychosis and their families over 12 months. Clin Psychol Psychother. 2021;28(5):1285–1296. [DOI] [PubMed] [Google Scholar]
- 26.Marshall C, Addington J, Epstein I, Liu L, Deighton S, Zipursky RB.. Treating young individuals at clinical high risk for psychosis. Early Interv Psychiatry. 2012;6(1):60–68. [DOI] [PubMed] [Google Scholar]
- 27.McAusland L, Buchy L, Cadenhead KS, et al. . Anxiety in youth at clinical high risk for psychosis. Early Interv Psychiatry. 2017;11(6):480–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Veling W, Pot-Kolder R, Counotte J, van Os J, van der Gaag M.. Environmental social stress, paranoia and psychosis liability: a virtual reality study. Schizophr Bull. 2016;42(6):1363–1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rietdijk J, Ising HK, Dragt S, et al. . Depression and social anxiety in help-seeking patients with an ultra-high risk for developing psychosis. Psychiatry Res. 2013;209(3):309–313. [DOI] [PubMed] [Google Scholar]
- 30.Atkinson RJ, Fulham WR, Cooper G, et al. . Electrophysiological, cognitive and clinical profiles of at-risk mental state: the longitudinal minds in transition (MinT) study. PLoS One. 2017;12(2):e0171657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cowan HR, McAdams DP, Mittal VA.. Core beliefs in healthy youth and youth at ultra high-risk for psychosis: dimensionality and links to depression, anxiety, and attenuated psychotic symptoms. Dev Psychopathol. 2019;31(1):379–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lederman O, Rosenbaum S, Maloney C, Curtis J, Ward PB.. Modifiable cardiometabolic risk factors in youth with at-risk mental states: a cross-sectional pilot study. Psychiatry Res. 2017;257:424–430. [DOI] [PubMed] [Google Scholar]
- 33.Olvet DM, Carrión RE, Auther AM, Cornblatt BA.. Self-awareness of functional impairment in individuals at clinical high-risk for psychosis. Early Interv Psychiatry. 2015;9(2):100–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Devylder JE, Ben-David S, Schobel SA, Kimhy D, Malaspina D, Corcoran CM.. Temporal association of stress sensitivity and symptoms in individuals at clinical high risk for psychosis. Psychol Med. 2013;43(2):259–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lincoln TM, Sundag J, Schlier B, Karow A.. The relevance of emotion regulation in explaining why social exclusion triggers paranoia in individuals at clinical high risk of psychosis. Schizophr Bull. 2018;44(4):757–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Appiah-Kusi E, Fisher HL, Petros N, et al. . Do cognitive schema mediate the association between childhood trauma and being at ultra-high risk for psychosis? J Psychiatr Res. 2017;88:89–96. [DOI] [PubMed] [Google Scholar]
- 37.Cressman VL, Schobel SA, Steinfeld S, et al. . Anhedonia in the psychosis risk syndrome: associations with social impairment and basal orbitofrontal cortical activity. NPJ Schizophr. 2015;1:15020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Koren D, Lacoua L, Rothschild-Yakar L, Parnas J.. Disturbances of the basic self and prodromal symptoms among young adolescents from the community: a pilot population-based study. Schizophr Bull. 2016;42(5):1216–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Valmaggia LR, Day F, Garety P, et al. . Social defeat predicts paranoid appraisals in people at high risk for psychosis. Schizophr Res. 2015;168(1–2):16–22. [DOI] [PubMed] [Google Scholar]
- 40.Choi J, Corcoran CM, Fiszdon JM, et al. . Pupillometer-based neurofeedback cognitive training to improve processing speed and social functioning in individuals at clinical high risk for psychosis. Psychiatr Rehabil J. 2017;40(1):33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Popovic D, Ruef A, Dwyer DB, et al. . Traces of trauma: a multivariate pattern analysis of childhood trauma, brain structure, and clinical phenotypes. Biol Psychiatry. 2020;88(11):829–842. [DOI] [PubMed] [Google Scholar]
- 42.Salokangas RKR, Patterson P, Hietala J, et al. . Childhood adversity predicts persistence of suicidal thoughts differently in females and males at clinical high-risk patients of psychosis. Results of the EPOS project. Early Interv Psychiatry. 2019;13(4):935–942. [DOI] [PubMed] [Google Scholar]
- 43.Blessing A, Studer A, Gross A, Gruss LF, Schneider R, Dammann G.. Disclosure of diagnosis in early recognition of psychosis. J Nerv Ment Dis. 2017;205(10):757–761. [DOI] [PubMed] [Google Scholar]
- 44.González-Rodríguez A, Studerus E, Spitz A, et al. . Gender differences in the psychopathology of emerging psychosis. Isr J Psychiatry Relat Sci. 2014;51(2):85–92. [PubMed] [Google Scholar]
- 45.Langbein K, Schmidt U, Schack S, et al. . State marker properties of niacin skin sensitivity in ultra-high risk groups for psychosis - an optical reflection spectroscopy study. Schizophr Res. 2018;192:377–384. [DOI] [PubMed] [Google Scholar]
- 46.Manninen M, Lindgren M, Therman S, et al. . Clinical high-risk state does not predict later psychosis in a delinquent adolescent population. Early Interv Psychiatry. 2014;8(1):87–90. [DOI] [PubMed] [Google Scholar]
- 47.Barkus E, Stirling J, French P, Morrison A, Bentall R, Lewis S.. Distress and metacognition in psychosis prone individuals: comparing high schizotypy to the at-risk mental state. J Nerv Ment Dis. 2010;198(2):99–104. [DOI] [PubMed] [Google Scholar]
- 48.Morrison AP, French P, Lewis SW, et al. . Psychological factors in people at ultra-high risk of psychosis: comparisons with non-patients and associations with symptoms. Psychol Med. 2006;36(10):1395–1404. [DOI] [PubMed] [Google Scholar]
- 49.Corcoran CM, Kimhy D, Parrilla-Escobar MA, et al. . The relationship of social function to depressive and negative symptoms in individuals at clinical high risk for psychosis. Psychol Med. 2011;41(2):251–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lincoln SH, Hooker CI.. Neural structure and social dysfunction in individuals at clinical high risk for psychosis. Psychiatry Res. 2014;224(3):152–158. [DOI] [PubMed] [Google Scholar]
- 51.Addington J, Epstein I, Liu L, French P, Boydell KM, Zipursky RB.. A randomized controlled trial of cognitive behavioral therapy for individuals at clinical high risk of psychosis. Schizophr Res. 2011;125(1):54–61. [DOI] [PubMed] [Google Scholar]
- 52.Lyngberg K, Buchy L, Liu L, Perkins D, Woods S, Addington J.. Patterns of premorbid functioning in individuals at clinical high risk of psychosis. Schizophr Res. 2015;169(1–3):209–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.de Wit S, Schothorst PF, Oranje B, Ziermans TB, Durston S, Kahn RS.. Adolescents at ultra-high risk for psychosis: long-term outcome of individuals who recover from their at-risk state. Eur Neuropsychopharmacol. 2014;24(6):865–873. [DOI] [PubMed] [Google Scholar]
- 54.Nordholm D, Poulsen HE, Hjorthoj C, et al. . Systemic oxidative DNA and RNA damage are not increased during early phases of psychosis: a case control study. Psychiatry Res. 2016;241:201–206. [DOI] [PubMed] [Google Scholar]
- 55.Phillips LJ, Edwards J, McMurray N, Francey S.. Comparison of experiences of stress and coping between young people at risk of psychosis and a non-clinical cohort. Behav Cogn Psychother. 2012;40(1):69–88. [DOI] [PubMed] [Google Scholar]
- 56.Studerus E, Ittig S, Beck K, et al. . Relation between self-perceived stress, psychopathological symptoms and the stress hormone prolactin in emerging psychosis. J Psychiatr Res. 2021;136:428–434. [DOI] [PubMed] [Google Scholar]
- 57.Appiah-Kusi E, Wilson R, Colizzi M, et al. . Childhood trauma and being at-risk for psychosis are associated with higher peripheral endocannabinoids. Psychol Med. 2020;50(11):1862–1871. [DOI] [PubMed] [Google Scholar]
- 58.Bentley E, Millman ZB, Thompson E, et al. . High-risk diagnosis, social stress, and parent-child relationships: a moderation model. Schizophr Res. 2016;174(1-3):65–70. [DOI] [PubMed] [Google Scholar]
- 59.Cullen AE, Addington J, Bearden CE, et al. . Stressor-cortisol concordance among individuals at clinical high-risk for psychosis: novel findings from the napls cohort. Psychoneuroendocrinology. 2020;115:104649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kommescher M, Gross S, Pützfeld V, Klosterkötter J, Bechdolf A.. Coping and the stages of psychosis: an investigation into the coping styles in people at risk of psychosis, in people with first-episode and multiple-episode psychoses. Early Interv Psychiatry. 2017;11(2):147–155. [DOI] [PubMed] [Google Scholar]
- 61.Mamah D, Cloninger CR, Mutiso VN, Gitonga I, Tele A, Ndetei DM.. Personality traits as markers of psychosis risk in kenya: assessment of temperament and character. Schizophr Bull Open. 2020;1(1):sgaa051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pruessner M, Iyer SN, Faridi K, Joober R, Malla AK.. Stress and protective factors in individuals at ultra-high risk for psychosis, first episode psychosis and healthy controls. Schizophr Res. 2011;129(1):29–35. [DOI] [PubMed] [Google Scholar]
- 63.Jhung K, Park JY, Song YY, Kang JI, Lee E, An SK.. Experiential pleasure deficits in the prodrome: a study of emotional experiences in individuals at ultra-high risk for psychosis and recent-onset schizophrenia. Compr Psychiatry. 2016;68:209–216. [DOI] [PubMed] [Google Scholar]
- 64.Shi J, Wang L, Yao Y, et al. . Protective factors in Chinese university students at clinical high risk for psychosis. Psychiatry Res. 2016;239:239–244. [DOI] [PubMed] [Google Scholar]
- 65.Alvarez-Jimenez M, Gleeson JF, Bendall S, et al. . Enhancing social functioning in young people at Ultra High Risk (UHR) for psychosis: a pilot study of a novel strengths and mindfulness-based online social therapy. Schizophr Res. 2018;202:369–377. [DOI] [PubMed] [Google Scholar]
- 66.Benavides C, Brucato G, Kimhy D.. Self-esteem and symptoms in individuals at clinical high risk for psychosis. J Nerv Ment Dis. 2018;206(6):433–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Stowkowy J, Addington J.. Maladaptive schemas as a mediator between social defeat and positive symptoms in young people at clinical high risk for psychosis. Early Interv Psychiatry. 2012;6(1):87–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Stowkowy J, Liu L, Cadenhead KS, et al. . Core schemas in youth at clinical high risk for psychosis. Behav Cogn Psychother. 2016;44(2):203–213. [DOI] [PubMed] [Google Scholar]
- 69.Taylor HE, Stewart SL, Dunn G, Parker S, Fowler D, Morrison AP.. Core schemas across the continuum of psychosis: a comparison of clinical and non-clinical groups. Behav Cogn Psychother. 2014;42(6):718–730. [DOI] [PubMed] [Google Scholar]
- 70.Seo E, Bang M, Lee E, An SK.. Aberrant tendency of noncurrent emotional experiences in individuals at ultra-high risk for psychosis. Psychiatry Investig. 2018;15(9):876–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pyle M, Stewart SL, French P, et al. . Internalized stigma, emotional dysfunction and unusual experiences in young people at risk of psychosis. Early Interv Psychiatry. 2015;9(2):133–140. [DOI] [PubMed] [Google Scholar]
- 72.Stowkowy J, Perkins DO, Woods SW, Nyman K, Addington J.. Personal beliefs about experiences in those at clinical high risk for psychosis. Behav Cogn Psychother. 2015;43(6):669–675. [DOI] [PubMed] [Google Scholar]
- 73.Clay KB, Raugh IM, Bartolomeo LA, Strauss GP.. Defeatist performance beliefs in individuals at clinical high-risk for psychosis and outpatients with chronic schizophrenia. Early Interv Psychiatry. 2020;15(4)865–873. [DOI] [PubMed] [Google Scholar]
- 74.Shi J, Wang L, Yao Y, Zhan C, Su N, Zhao X.. Systemic therapy for youth at clinical high risk for psychosis: a pilot study. Front Psychiatry. 2017;8:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Marulanda S, Addington J.. Resilience in individuals at clinical high risk for psychosis. Early Interv Psychiatry. 2016;10(3):212–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Addington J, Farris M, Devoe D, Metzak P.. Progression from being at-risk to psychosis: next steps. npj Schizophr. 2020;6(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Barbato M, Penn DL, Perkins DO, Woods SW, Liu L, Addington J.. Metacognitive functioning in individuals at clinical high risk for psychosis. Behav Cogn Psychother. 2014;42(5):526–534. [DOI] [PubMed] [Google Scholar]
- 78.Addington J, Devoe DJ, Santesteban-Echarri O.. Multidisciplinary treatment for individuals at clinical high risk of developing psychosis. Curr Treat Options Psychiatry. 2019;6(1):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.van der Steen Y, Gimpel-Drees J, Lataster T, et al. . Clinical high risk for psychosis: the association between momentary stress, affective and psychotic symptoms. Acta Psychiatr Scand. 2017;136(1):63–73. [DOI] [PubMed] [Google Scholar]
- 80.Gerritsen C, Bagby RM, Sanches M, et al. . Stress precedes negative symptom exacerbations in clinical high risk and early psychosis: a time-lagged experience sampling study. Schizophr Res. 2019;210:52–58. [DOI] [PubMed] [Google Scholar]
- 81.Buck B, Gagen EC, Halverson TF, Nagendra A, Ludwig KA, Fortney JC.. A systematic search and critical review of studies evaluating psychometric properties of patient-reported outcome measures for schizophrenia. J Psychiatr Res. 2022;147:13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Weldring T, Smith SM.. Article commentary: patient-reported outcomes (pros) and patient-reported outcome measures (PROMs). Health Serv Insights. 2013;6:HSI.S11093HSI–HSI.S11S11093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Carle AC, Cella D, Cai L, et al. . Advancing PROMIS’s methodology: results of the Third Patient-Reported Outcomes Measurement Information System (PROMIS®) Psychometric Summit. Expert Rev Pharmacoeco Outcomes Res. 2011;11(6):677–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cella D, Yount S, Rothrock N, et al. . The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care. 2007;45:S3–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.