Abstract
Background
Prehospital critical care is a rapidly evolving field. There is a paucity of evidence relating to its practice, with limited progress in answering those research questions identified over a decade ago. It is vital that evidence gaps are identified and addressed. This study aimed to define the current research priorities in UK prehospital critical care.
Methods
This modified national Delphi study was coordinated by the Pre-HOspital Trainee Operated research Network and conducted in four rounds between October 2021 and April 2022. Rounds 1 and 2 were conducted online with clinicians involved in prehospital critical care delivery and non-clinical prehospital researchers. Rounds 3 and 4 were completed online by a subject matter expert (SME) panel.
Results
In round 1, 78 participants submitted 394 research questions relating to prehospital critical care delivery in the UK. These were refined and categorised into 192 questions, which were scored for importance in round 2. Fifty questions were discussed and scored by the SME panel in round 3. Round 4 created a ranked top 20 list. The top research priority was ‘Which cardiac arrest patients should critical care teams be dispatched to; how do we identify these patients during the emergency call?’. Other priorities included dispatch optimisation, out-of-hospital medical cardiac arrest management, optimising resuscitation in haemorrhagic shock, improving traumatic brain injury outcomes and optimising management of traumatic cardiac arrest.
Conclusions
This modified Delphi study identified 20 research priorities where efforts should be concentrated to develop collaborative prehospital critical care research within the UK over the next 5 years.
Keywords: pre-hospital care, advanced practitioner, doctors in PHC
WHAT IS ALREADY KNOWN ON THIS TOPIC
Prehospital critical care delivery in the UK often lacks evidence due to factors such as the time critical nature of patient encounters and challenges around patient recruitment and consent.
The last consensus report defining research priorities in physician-delivered prehospital critical care in Europe was published in 2011.
Current literature suggests that there is still a paucity of evidence in several of the previously prioritised areas. Additionally, as this is a rapidly evolving field, it is likely that there are emerging areas requiring attention.
WHAT THIS STUDY ADDS
This modified Delphi study identified current research priorities in UK prehospital critical care.
Key areas include management of cardiac arrest and improving post return of spontaneous circulation care, management of patients with moderate-to-severe head injury and major haemorrhage and improvement of dispatch and triage decisions.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Results can help direct efforts for research and funding in prehospital critical care in the UK over the coming years.
Background
Within the UK, prehospital critical care teams provide enhanced care to critically ill and injured patients, supplementing care delivered by ground ambulance services. Critical care teams comprise clinicians working at the level of an advanced prehospital practitioner1 capable of delivering level 2 and 3 critical care interventions,2 including within Helicopter Emergency Medical Services (HEMS), ground-based services such as those within the British Association for Immediate Care (BASICS) and in advanced paramedic practitioner roles. Services often use a doctor-paramedic model, but variations include double and single critical care paramedic models and solo physician responders.
Prehospital critical care practice lacks a robust evidence base.3 4 Prehospital emergency medicine as a subspeciality is relatively new, with formal subspecialist qualification available only within the last decade.5 Other factors hindering research relate to challenges around patient recruitment and consent in prehospital trials, in-hospital follow-up data acquisition6 and ascertaining a causal link between prehospital interventions and longer-term outcomes. However, notable large prehospital studies have now been conducted successfully in the UK.7 8
Previous reports have described prehospital research priorities, including a 2011 European Consensus report which outlined five areas for future development in prehospital physician-provided critical care delivery,3 appropriate staffing and training and effect on outcomes, advanced airway management, time windows for key prehospital interventions, role of prehospital ultrasound and defining dispatch criteria. The Netherlands national research agenda concerning wider prehospital emergency medical services9 was updated in 202110 and again highlighted several priority areas necessitating further research. Despite these reports, there has been limited demonstrable progress.11–13 More recently, the top five research priorities for a single UK HEMS organisation were published,14 but generalisability to other organisations is unknown.
Therefore, the aim of this study was to ascertain the research priorities for UK prehospital critical care using a modified Delphi process.
Methods
This study was designed and conducted between October 2021 and April 2022 by the Pre-HOspital Trainee Operated research Network (PHOTON), in collaboration with the National HEMS Research and Audit Forum (NHRAF) and Essex and Herts Air Ambulance. Although conducted by a trainee-led organisation, study participants involved the wider prehospital critical care community.
The Delphi method is a structured and iterative approach to achieving consensus to address a particular problem or issue, typically comprising identification of an expert panel, repeated rounds of data collection and structured feedback to participants following each round.15 This current study adopted a modified Delphi methodology, incorporating a subject matter expert (SME) meeting.
This Delphi has been reported according to the Conducting and Reporting Delphi Studies criteria16 which was originally developed to allow appraisal of the Delphi method in creating best practice guidelines in palliative care and consists of recommendations to improve rigour and transparency in the conduct and reporting of studies employing the Delphi method.
Participant recruitment
To be eligible to participate in rounds 1 and 2, participants were required to be either a UK-based clinician working in a prehospital critical care role with at least 6 months full-time experience or have a non-clinical role within a prehospital critical care team involving an active research component.
The term ‘clinician’ included anyone working in a clinical role within a prehospital critical care team; in the UK, such clinicians are typically doctors and paramedics but could be any other relevant healthcare provider. Clinicians working within BASICS were included were eligible. The study was advertised to all UK HEMS organisations through established communication channels, to NHRAF members and on social media channels by PHOTON. To maintain participant anonymity during rounds 1 and 2, a mailing list was generated to facilitate blanket communication to all who expressed interest. Those who expressed interest were encouraged to share details of the study with others eligible to participate using a snowballing technique. As a result, the denominator of those invited to participate is unknown.
All further correspondence and invitations to participate in successive rounds were communicated through the mailing list, with instructions regarding how to opt out if they no longer wished to be included.
SMEs for rounds 3 and 4 were defined as having clinical experience of working within prehospital critical care (HEMS or land-based) at a senior grade for at least 2 years, and/or research and/or substantial leadership responsibilities within a prehospital team capable of delivering critical care interventions or being selected specialists who have previously documented areas of interest in the development of prehospital research.
Potential SMEs were identified using several means. We aimed to have representation from all UK HEMS services, other relevant land-based resources such as BASICS and an approximately equal split of critical care paramedics and doctors. At the point of enrolment onto the mailing list, participants were asked to self-identify if they fulfilled the criteria above and if so, to indicate their willingness to participate in round 3. Services without representation were approached and service leads were asked to nominate someone from their team to attend. Additionally, several UK-based specialists with a known reputation in prehospital critical care research, based on publication of at least three papers in the field, were approached. A meeting date was set and all those identified as potential SMEs were invited.
Patient and public involvement
The original study design sought patient involvement to ensure the output was representative of patients’ perspectives. Despite exhaustion of several channels of potential recruitment, no patient volunteers were identified which is recognised as a significant limitation.
Modified Delphi process
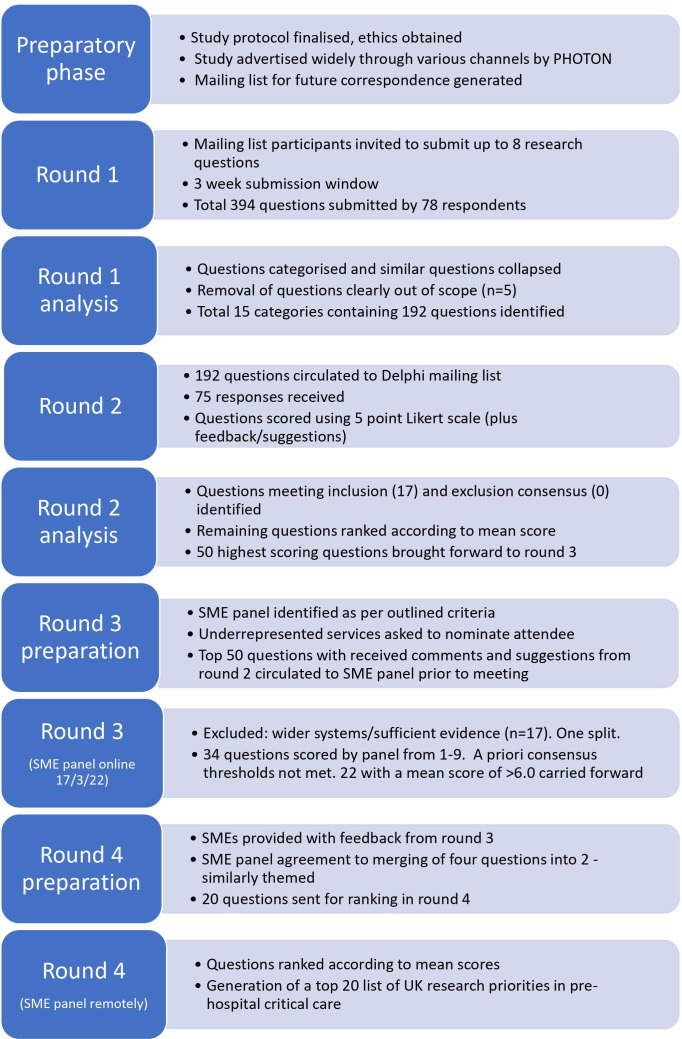
This modified Delphi was conducted in four rounds (figure 1). The fourth round was not planned within the original study protocol and was added to address a lack of consensus and the requirement for further refinement to the wording of research questions following round 3. All protocol amendments were approved by the ethics committee.
Figure 1.
Flowchart documenting modified Delphi process. SME, subject matter expert.
Round 1: qualitative assessment
The first round was delivered online using Online Surveys (Jisc), a survey tool that is General Data Protection Regulation (GDPR) compliant and certified to ISO 27001 standard, and with anonymity. Participants were invited to identify up to eight research questions or areas of equipoise they felt most important to the development of prehospital critical care delivery. A limit of eight questions was set to encourage participants to prioritise questions they perceived as most important and was less conservative than limits set in previous studies using consensus approaches to establish research priorities.3 14 17 Round 1 remained open for 3 weeks, with regular reminders sent to those on the mailing list. Subsequent additions to the mailing list were permitted to maximise participation. Round 1 participants were asked to self-generate an anonymous study identifier in order to link responses between rounds 1 and 2.
After closure of round 1, submitted questions were categorised into broad themes, and similar questions amalgamated. The initial process was undertaken separately by two subgroups within the study team (LR and KW, and SM), before jointly confirming question categories and the questions to be distributed in round 2. Extreme care was taken not to inadvertently lose content of submitted questions during the process. Five questions clearly outside the scope of prehospital critical care were removed (online supplemental file 1).
emermed-2022-212622supp001.pdf (7.7KB, pdf)
Round 2: importance ratings
Round 2 was conducted online over 3 weeks. Participants individually rated the questions developed in round 1 on a 5-point Likert scale anchored by 1: ‘not important’ and 5: ‘very important’. Each question received one score, with participants asked to consider scientific merit, significance to prehospital critical care delivery, innovation, relevance and feasibility of further study when assigning the score, as well as whether sufficient evidence existed within existing literature. Participants could add comments or suggest amendments for each question. There was no requirement for participation in the previous round; recent research demonstrated that allowing participation in subsequent rounds regardless of prior participation results in better representation of the invited panel and does not affect the outcome of the Delphi process.18 All received responses were anonymous. A priori consensus thresholds for round 2 were defined as follows: If a research question scored 4 or greater from 75% or more respondents, it was automatically included in round 3. If a research question scored 2 or less from 75% or more respondents, it was automatically excluded from round 3.
Questions not meeting the automatic inclusion or exclusion criteria were ranked by overall score by the study team and those ranking highest were taken forward, along with those meeting the automatic inclusion criterion to give a total of 50 questions for discussion at the round 3 panel meeting. A cut-off of 50 questions was felt to be a manageable number to be discussed by the panel within the time constraints of the meeting.
Round 3: SME meeting
The meeting was held online on the 17 March 2022 using Zoom. Prior to the meeting, SMEs received a copy of the results from round 2, including mean scores and comments or suggestions pertaining to individual questions received from participants. Within the meeting, the 50 questions were discussed, including review of any comments received in round 2, revision of wording and exclusion of any questions not felt by the SME panel to fall directly within the remit of prehospital critical care research.
Remaining questions were voted on in terms of their priority for future research using the anonymous live voting software, Slido. Voting used a scoring system drawn from Schneider et al,17 with a score of 1 being assigned if the individual felt the question should not be studied, and 9 if they felt it was of the highest priority.
Predefined consensus threshold for retention of questions was that 100% of SMEs scored the research question as a 7, 8 or 9.17 Questions meeting this threshold would automatically be brought forward for a final ranking exercise. If less than 10 questions met this criterion, then it was planned a priori that questions with the highest mean scores would be taken forward for final ranking.
None of the questions met the predefined consensus threshold, therefore an unplanned fourth round was added where the SME panel ranked the highest scoring questions from round 3 and made final amendments to the wording. Questions scoring a mean of 6.0 (indicating ‘slightly high priority’) or more in round 3 were included in the ranking exercise.
Round 4: final ranking
The fourth round was open only to the SMEs who had participated in round 3. Participants were asked to rank the highest scoring questions from round 3 in order of importance. The mean ranking was generated with its corresponding SD for each question. A final opportunity was given for minor amendments to wording prior to publication of results.
Results
A total of 135 people signed up to the mailing list to receive information about the study and links to the online surveys (62% doctors; 31% paramedics; 5% ‘other’ background; 2% missing data).
Seventy-eight (57.8%) of those on the mailing list participated in round 1, submitting a total of 394 research questions. Of the 78 participants, 74.4% were doctors, 23.1% were Critical Care Paramedics and 2.6% were ‘other’. Further participant demographics for rounds 1 and 2 are presented in table 1. Suggested research questions were categorised under the following headings: medical cardiac arrest; prehospital emergency anaesthesia/analgesia/sedation; neurological emergencies; major haemorrhage and blood products; paediatrics; major trauma (including traumatic cardiac arrest); operational; impact or benefit of prehospital critical care teams; dispatch; triage; patient experience; staff well-being; training and education; kit; miscellaneous. After amalgamation of similar questions and exclusion of those not felt to be directly related to prehospital critical care delivery, 192 questions were circulated for round 2 (online supplemental file 2).
Table 1.
Participant demographics for rounds 1 and 2
| Demographics | Round 1 n (%) | Round 2 n (%) |
| Role | ||
| Prehospital care doctor | 11 (14.1%) | 6 (8%) |
| Hospital doctor | 1 (1.3%) | 1 (1.3%) |
| Prehospital care doctor and hospital doctor | 46 (59%) | 38 (50.7%) |
| Critical care paramedic | 18 (23.1%) | 9 (12%) |
| Other | 2 (2.6%) | 3 (4%) |
| Missing | 0 (0%) | 18 (24%) |
| Hospital doctor specialty | ||
| Anaesthetics | 13 (27.7%) | 10 (25.6%) |
| Emergency Medicine | 29 (61.7%) | 25 (64.1%) |
| Intensive Care Medicine | 1 (2.1%) | 1 (2.6%) |
| Dual Specialty | 4 (8.5%) | 2 (5.1%) |
| Missing | 0 (0%) | 1 (2.6%) |
| Years of experience in the prehospital setting | ||
| ≥6 months, ≤6 years | 26 (33.3%) | 21 (28%) |
| >6 years, ≤12 years | 21 (26.9%) | 15 (20%) |
| >12 years | 30 (38.5%) | 20 (26.7%) |
| Missing | 1 (1.3%) | 19 (25.3%) |
| Country or countries in which participant is based* | ||
| England | 70 (89.7%) | 51 (68%) |
| Scotland | 6 (7.7%) | 4 (5.3%) |
| Wales | 8 (10.3%) | 3 (4%) |
| Ireland | 3 (3.8%) | 2 (2.7%) |
| Missing | 0 (0%) | 18 (24%) |
| Prehospital research experience* | ||
| None | 17 (21.8%) | 15 (20%) |
| Previous involvement with research | 0 (0%) | 6 (8%) |
| Currently involved with some prehospital research projects | 39 (50%) | 26 (34.7%) |
| Publication of 1–4 peer-reviewed prehospital research papers (any authorship) | 18 (23.1%) | 12 (16%) |
| Publication of≥5 peer-reviewed prehospital research papers (any authorship) | 10 (12.8%) | 4 (5.3%) |
| Other (eg, principal investigator on funded project) | 6 (7.7%) | 2 (2.7%) |
| Missing | 0 (0%) | 19 (25.3%) |
*Some participants reported being based in more than one country of the UK, and some participants selected more than one response for prehospital research experience, therefore total numbers exceed 78 and 75 for rounds 1 and 2, respectively.
emermed-2022-212622supp002.pdf (83.2KB, pdf)
Round 2 was completed by 75 respondents; 78.7% had completed round 1. Sixty per cent of respondents were doctors, 12% were CCPs and 4% were ‘other’. It was not possible to match 18 (24%) of these participants across rounds 1 and 2, due to discrepancies in their self-generated anonymisation code resulting in missing demographic data for a substantial proportion of round 2 participants.
On review of the results from round 2, 17 questions met the predefined threshold for inclusion in round 3. None met the threshold for automatic exclusion. The remaining questions were assigned a mean score and the next 33 highest scoring questions brought forward to give a total of 50 questions for review by the SME panel.
A total of 35 subject matter experts (SMEs) confirmed their willingness to participate in the round 3 meeting and 25 SMEs were available to participate. Of those who participated, seven (28%) had been approached separately and invited to participate due to their significant contributions to prehospital critical care research and development. Six (24%) of the participating SMEs were critical care paramedics and 19 (76%) were doctors; 64% of the SMEs had conducted prehospital care research and all had significant clinical experience. Participating SMEs were from 14 of the 22 (63.64%) UK HEMS, including services in England, Scotland and Wales, and several BASICS services.
During the online meeting, 17 questions were excluded from the voting process. Reasons for exclusion included a wider system of healthcare of public health focus, a substantial existing evidence base, being the focus of a current or imminent large-scale study, or some degree of overlap with other questions. One retained question was split into two questions, as it was felt to represent two distinct areas. Therefore, 34 questions were brought forward for voting.
Following the scoring process, none of the questions met the predefined consensus threshold for the final ranking exercise and therefore all 34 questions were ranked according to mean score (online supplemental file 3). A total of 22 questions had a mean score of 6.0 (‘slightly high priority’) or greater; these were taken forward to round 4. However, following further discussion after the scoring process, it was agreed by the SME panel that four of these retained questions should be collapsed into two questions, resulting in 20 questions for final ranking by the SME panel in round 4.
emermed-2022-212622supp003.pdf (84.8KB, pdf)
Twenty-three responses were received in round 4, constituting a response rate of 92% from the SME panel. table 2 contains the top 20 questions with their associated mean ranking and SD.
Table 2.
Round 4 results: top 20 ranked questions
| No. | Question | Mean ranking (SD)* |
| 1 | Which cardiac arrest patients should critical care teams be dispatched to, and how do we identify these patients during the emergency call? | 4.56 (4.75) |
| 2 | How can dispatch of critical care teams to patients be improved? Can the use of digital health technology assist? | 5.96 (5.24) |
| 3 | In patients with medical OHCA attended by prehospital critical care teams, which interventions beyond current ALS guidelines improve outcomes? | 6.00 (4.97) |
| 4 | What strategy of volume resuscitation improves outcomes in injured patients with haemorrhagic shock? | 7.13 (5.47) |
| 5 | In patients with ROSC following OHCA, does PHEA improve patient outcomes? | 8.04 (5.41) |
| 6 | What clinical features and interventions are associated with survival to hospital discharge in patients in traumatic cardiac arrest? | 8.52 (5.40) |
| 7 | In patients with severe traumatic brain injury, does prehospital administration of osmotic agents result in improved neurological outcome and survival, and if so, what is the optimal dose? | 9.39 (5.72) |
| 8 | What strategy for volume resuscitation improves outcomes in patients with traumatic brain injury? | 9.48 (4.88) |
| 9 | What is the benefit offered to patients with moderate to severe head injury by prehospital critical care teams? | 9.61 (5.73) |
| 10 | Does prehospital reversal of anticoagulation improve outcomes in patients with traumatic brain injury? | 9.96 (4.69) |
| 11 | Does transfer to a neurological centre for consideration of time critical thrombectomy improve outcome in patients with suspected stroke in the prehospital setting? | 10.61 (5.39) |
| 12 | Which adult trauma patients with frailty benefit from triage to a Major Trauma Centre? | 10.87 (4.62) |
| 13 | In trauma patients undergoing PHEA, does the time interval between the 999 call and PHEA delivery impact on patient focused outcomes? | 11.09 (5.30) |
| 14 | Does prehospital administration of calcium in major traumatic haemorrhage improve patient outcomes, and if so, what is the optimal dose? | 11.91 (4.66) |
| 15 | Is prehospital critical care clinician dispatch superior to standard ambulance service dispatch? | 12.17 (6.31) |
| 16 | Is there any benefit to patients by using prehospital point of care testing? | 12.22 (4.24) |
| 17 | How can we identify risks to well-being and protect the mental health of prehospital critical care providers? | 12.74 (4.95) |
| 18 | In cases of prehospital death, what strategies can be used by prehospital practitioners to improve the experience for friends, family and bystanders? | 12.83 (5.31) |
| 19 | Does the use of POCUS in prehospital critical care improve patient outcomes? | 13.09 (4.88) |
| 20 | Which prehospital simulation strategies are optimal to improve patient, clinician and procedural outcomes? | 16.83 (4.05) |
*Values are expressed as the mean (SD) final ranking assigned during round 4 of the process, with a lower value indicating a higher priority.
OHCA, out-of-hospital cardiac arrest; PHEA, prehospital emergency anaesthetic; POCUS, point-of-care ultrasound; ROSC, return of spontaneous circulation.
Discussion
This study has identified the current national research priorities for prehospital critical care through use of an evidence-based modified Delphi process. The top research priority was ‘Which cardiac arrest patients should critical care teams be dispatched to, and how do we identify these patients during the emergency call?’.
The SMEs agreed that identified priority areas should be presented as broad research questions, permitting several research studies to be conceptualised from within each topic, in keeping with similar previously published outputs such as the James Lind Alliance Emergency Medicine Priority Setting Partnership statement.19
Three questions in this current top 20 relate to critical care team dispatch, previously identified over ten years ago in the 2011 European Delphi.3 Similarly, questions on the role of prehospital emergency anaesthesia and advanced airway management, and ultrasound use in prehospital critical care persist. There is considerable overlap in identified priorities between this study and the European one, particularly around the impact of prehospital critical care interventions on patient outcomes in head injury and postresuscitation care following out of-hospital cardiac arrest.14
Regarding strengths of the study, initial question generation and scoring in rounds 1 and 2 were undertaken by a considerable number of clinicians directly involved in prehospital critical care delivery in the UK as well as non-clinical researchers with relevant expertise. The SME panel involved in the third and fourth rounds comprised experienced prehospital critical care practitioners, representing almost two-thirds of air ambulance services nationally in addition to BASICS schemes.
There are several limitations. Despite considerable efforts, we were unable to identify any patient participants. We plan to address this in a future study focusing on patient and family member experience. Additionally, we cannot be sure that participants were representative of the whole UK prehospital critical care community. Although rounds 1 and 2 included participants from services in England, Scotland, Wales and Ireland, it is unknown if all services were represented as participants were not asked to provide work details to ensure anonymity. Further, approximately one-third of HEMS were not represented within the SME panel. There was also an imbalance in the clinical roles of participants across the four rounds, with considerably more prehospital critical care doctors participating than paramedics. Consensus was not reached in round 3, necessitating addition of a fourth round. This may have been partly due to similarly themed questions being put forward for scoring by the SME panel. Additionally, priorities may differ at a personal and service level based on local project involvement.
Nevertheless, our defined top research priorities should be regarded as important for the conception and design of future research studies, having undergone a selection process with involvement of many recognised experts in prehospital critical care in the UK. The results of this Delphi should inform development of future funding applications and encourage collaborative working with a view to addressing remaining evidence gaps.
Footnotes
Handling editor: Jason E Smith
Twitter: @LisaRamage
Collaborators: Subject Matter Experts: Steve Bell, Flora Bird, Simon Carley, Louisa Chan, David Clutton, Stephanie Cowan, Matthew Creed, David Dungay, Sarah Folley, Caroline Leech, Amy Hughes, Nigel Lang, Rob Major, Roderick MacKenzie, Zane Perkins, Laurie Phillipson, James Plumb, David Rawlinson, Matthew Taylor, Glyn Thomas, Harriet Tucker, James Raitt, Rishi Rallan, Andy Smith, Simon Walsh.
Contributors: LR: Responsible for overall study content and is the guarantor. Involved in protocol drafting, ethics applications, survey design, study rollout, result analysis, chairing SME meeting, manuscript drafting, manuscript approval. SMcL: involved in protocol drafting, ethics applications, survey design, study rollout, result analysis, chairing SME meeting, manuscript drafting, manuscript approval. KW: involved in study rollout, analysis of results, manuscript approval.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
PreHOspital Trainee Operated research Network (PHOTON):
Steve Bell, Flora Bird, Simon Carley, Louisa Chan, David Clutton, Stephanie Cowan, Matthew Creed, David Dungay, Sarah Folley, Caroline Leech, Amy Hughes, Nigel Lang, Rob Major, Roderick MacKenzie, Zane Perkins, Laurie Phillipson, James Plumb, David Rawlinson, Matthew Taylor, Glyn Thomas, Harriet Tucker, James Raitt, Rishi Rallan, Andy Smith, and Simon Walsh
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. Most data relevant to the study are either included in the article or uploaded as a supplementary file. Other data if required are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Allied Health, Nursing & Midwifery & Medicine School Research Ethics Panel at Anglia Ruskin University (Study ref AH-SREP-20-100). Participants gave informed consent to participate in the study before taking part.
References
- 1. FPHC . Phem competency descriptors and framework. Available: https://fphc.rcsed.ac.uk/media/2911/phem-competency-descriptors-and-framework.pdf [Accessed 18 Nov 2022].
- 2. RCOA . Pre-Hospital emergency medicine. Available: https://rcoa.ac.uk/training-careers/training-hub/2010-curriculum/pre-hospital-emergency-medicine [Accessed 18 Nov 2022].
- 3. Fevang E, Lockey D, Thompson J, et al. The top five research priorities in physician-provided pre-hospital critical care: a consensus report from a European research collaboration. Scand J Trauma Resusc Emerg Med 2011;19:57. 10.1186/1757-7241-19-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rehn M, Krüger AJ. Quality improvement in pre-hospital critical care: increased value through research and publication. Scand J Trauma Resusc Emerg Med 2014;22:34. 10.1186/1757-7241-22-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. IBTPHEM . Curriculum. Available: http://www.ibtphem.org.uk/curriculum/ [Accessed 14 Sep 2022].
- 6. Armstrong S, Langlois A, Siriwardena N, et al. Ethical considerations in prehospital ambulance based research: qualitative interview study of expert informants. BMC Med Ethics 2019;20:88. 10.1186/s12910-019-0425-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Perkins GD, Quinn T, Deakin CD, et al. Pre-Hospital assessment of the role of adrenaline: measuring the effectiveness of drug administration in cardiac arrest (PARAMEDIC-2): trial protocol. Resuscitation 2016;108:75–81. 10.1016/j.resuscitation.2016.08.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Crombie N, Doughty HA, Bishop JRB, et al. Resuscitation with blood products in patients with trauma-related haemorrhagic shock receiving prehospital care (RePHILL): a multicentre, open-label, randomised, controlled, phase 3 trial. Lancet Haematol 2022;9:e250–61. 10.1016/S2352-3026(22)00040-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. van de Glind I, Berben S, Zeegers F, et al. A national research agenda for pre-hospital emergency medical services in the Netherlands: a Delphi-study. Scand J Trauma Resusc Emerg Med 2016;24:2. 10.1186/s13049-015-0195-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vloet LCM, Hesselink G, Berben SAA, et al. The updated national research agenda 2021-2026 for prehospital emergency medical services in the Netherlands: a Delphi study. Scand J Trauma Resusc Emerg Med 2021;29:162. 10.1186/s13049-021-00971-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bache KG, Rehn M, Thompson J. Seven years since defining the top five research priorities in physician-provided pre-hospital critical care - what did it lead to and where are we now? Scand J Trauma Resusc Emerg Med 2018;26:101. 10.1186/s13049-018-0562-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Samdal M, Thorsen K, Græsli O, et al. Dispatch accuracy of physician-staffed emergency medical services in trauma care in south-east Norway: a retrospective observational study. Scand J Trauma Resusc Emerg Med 2021;29:169. 10.1186/s13049-021-00982-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rehn M, Bache KG, Lossius HM, et al. Top five research priorities in physician-provided pre-hospital critical care - appropriate staffing, training and the effect on outcomes. Scand J Trauma Resusc Emerg Med 2020;28:32. 10.1186/s13049-020-00724-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McLachlan S, Bungay H. Consensus on research priorities for Essex & Herts Air Ambulance: a Delphi study. Scand J Trauma Resusc Emerg Med 2021;29:25. 10.1186/s13049-021-00835-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs 2000;32:1008–15. [PubMed] [Google Scholar]
- 16. Jünger S, Payne SA, Brine J, et al. Guidance on conducting and reporting Delphi studies (CREDES) in palliative care: recommendations based on a methodological systematic review. Palliat Med 2017;31:684–706. 10.1177/0269216317690685 [DOI] [PubMed] [Google Scholar]
- 17. Schneider P, Evaniew N, Rendon JS, et al. Moving forward through consensus: protocol for a modified Delphi approach to determine the top research priorities in the field of orthopaedic oncology. BMJ Open 2016;6:e011780. 10.1136/bmjopen-2016-011780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Boel A, Navarro-Compán V, Landewé R, et al. Two different invitation approaches for consecutive rounds of a Delphi survey led to comparable final outcome. J Clin Epidemiol 2021;129:31–9. 10.1016/j.jclinepi.2020.09.034 [DOI] [PubMed] [Google Scholar]
- 19. Smith J, Keating L, Flowerdew L, et al. An emergency medicine research priority setting partnership to establish the top 10 research priorities in emergency medicine. Emerg Med J 2017;34:454–6. 10.1136/emermed-2017-206702 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
emermed-2022-212622supp001.pdf (7.7KB, pdf)
emermed-2022-212622supp002.pdf (83.2KB, pdf)
emermed-2022-212622supp003.pdf (84.8KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. Most data relevant to the study are either included in the article or uploaded as a supplementary file. Other data if required are available on reasonable request.