Figure 3. ALS differential diagnosis.
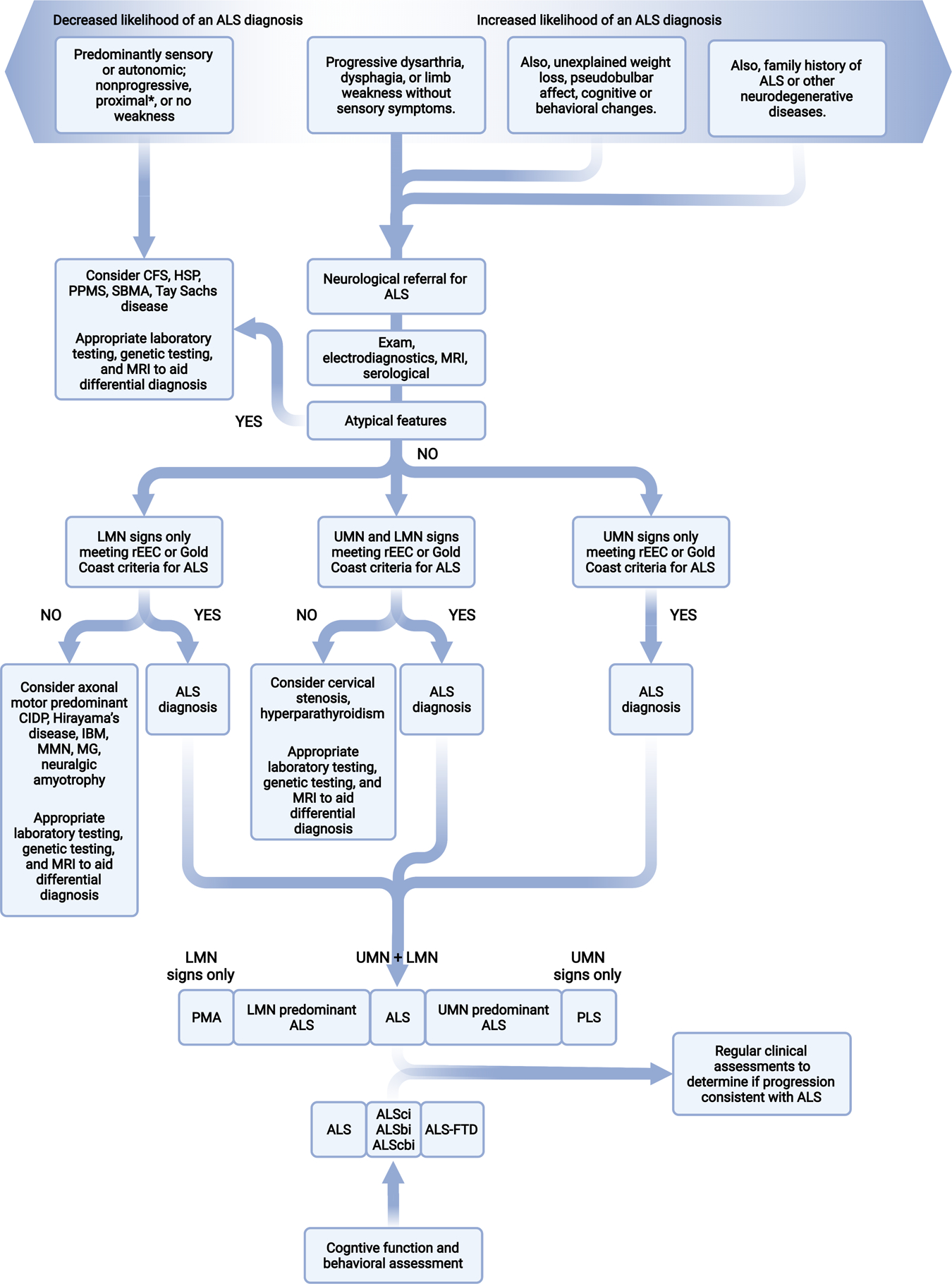
Differential diagnosis, represented here by a flowchart for the classical process using symptoms and signs, is central to the diagnostic process in ALS. At minimum, individuals suspected of ALS will undergo physical and neurological exams, electrodiagnostic assessment, MRI of involved regions, and relevant serological testing. This figure is based on a summary of potential differential diagnoses for diseases more common or as common as ALS is outlined in Appendix Table 3. Overlap of known ALS genes with other diseases and syndromes also occurs and is outlined in Appendix Table 4. CFS, cramp-fasciculation syndrome; CIDP, chronic inflammatory demyelinating polyneuropathy; HSP, hereditary spastic paraparesis; IBM, inclusion body myositis; LMN, lower motor neuron; MMN, multifocal motor neuropathy; MG, myasthenia gravis; PPMS primary progressive multiple sclerosis; rEEC, revise El Escorial criteria; SBMA, spinobulbar muscular atrophy; UMN, upper motor neuron. *Several potential differential diagnoses present with proximal weakness and should be considered along with flail arm ALS, which also presents with proximal greater than distal upper extremity weakness. Thus, check for increased proximal reflexes on exam and neurogenic motor unit action potentials on electromyography.
