Figure 1.
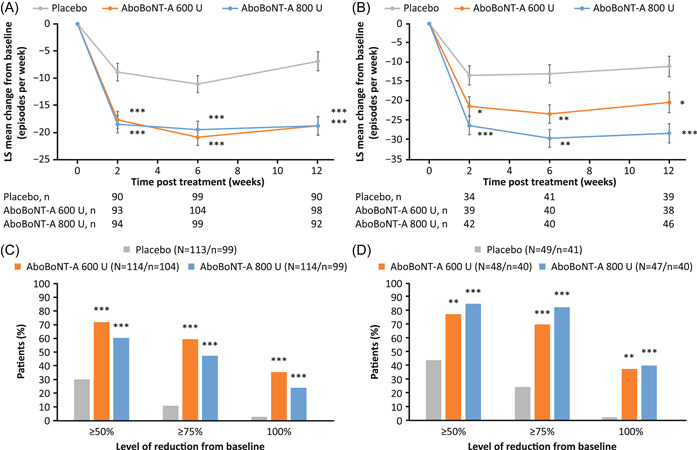
Change in weekly number NDOI episodesa in patients with (A) SCI and (B) MS, and proportion of patientsb with different thresholds of improvements from baseline at Week 6 with (C) SCI and (D) MS. *p < 0.05; **p < 0.01; ***p < 0.001. Data in (A) and (B) are LS mean ± SE. Data shown are for the randomized pooled population (DBPC period). aBased on the MMRM model to assess difference in change from baseline between each aboBoNT‐A dose group (600 or 800 U) versus placebo at each timepoint (Weeks 2, 6, and 12) with treatment group, visits (Weeks 2, 6, and 12), treatment by‐visit interaction, etiology of NDOI [SCI or MS], prior intradetrusor use [BoNT‐A‐naïve or BoNT‐A‐non‐naïve]), treatment‐by‐visit‐by‐etiology group interaction, study as fixed effect variables, study baseline value as covariate, and patient as a random effect. bThe outcomes are based on logistic GLMM model to assess difference between each aboBoNT‐A dose group (600 or 800 U) versus placebo with treatment group, stratification factors, visit (Weeks 2, 6, and 12), treatment‐by‐visit interaction, study baseline‐by‐visit interaction, treatment‐by‐visit‐etiology group interaction, study as fixed effect, and study baseline covariate and patient as random effect. Week 6 data only are presented. AboBoNT‐A, abobotulinumtoxinA; BoNT‐A, botulinum toxin type A; DBPC, double‐blind placebo‐controlled; LS, least square; GLMM, generalized linear mixed model; MMRM, mixed‐model repeated measures; MS, multiple sclerosis; N, number of patients in treatment group; n, number of patients with data; NDOI, neurogenic detrusor overactivity incontinence; SCI, spinal cord injury; SE, standard error; U, units
