Figure 2.
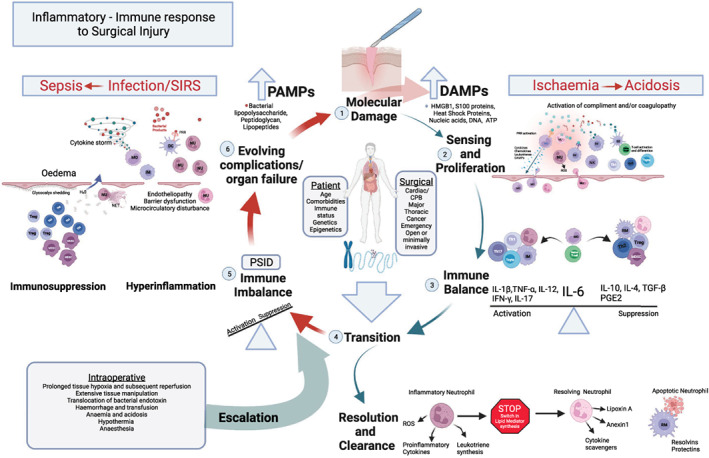
The inflammatory‐immune response to surgical injury. (1) The host response is primarily driven by damage that is apparent at a molecular level; (2) danger‐associated molecular patterns (DAMPs), sensed by cells of the innate immune system, proliferate the response and activate the adaptive immune system further bolstering cell‐mediated immunity; (3) the response is balanced with the actions of interleukin 6 (IL‐6) driving the initial host response and simultaneously contributing to immune regulation and suppression; (4) Transition towards resolution and clearance is marked by a switch within inflammatory neutrophil lipid mediator (LM) biosynthesis pathways away from strongly chemoattractant and proinflammatory leukotrienes to lipoxins (Lipoxin A), proresolving LMs (resolvins and protectins) and resolving proteins (annexin 1). Monocyte‐derived macrophages reprogramme to a resolving macrophage (RM) promoting neutrophil apoptosis and tissue repair; (5) patient and surgical factors combine with intra‐operative events to escalate the response resulting in a pathophysiological state of immune imbalance and postoperative systemic inflammatory dysregulation (PSID); (6) this response may become a cycle of increasing tissue injury, with endotheliopathy, barrier dysfunction, further DAMP production and the release pathogen‐associated molecular patterns (PAMPs). Uncontrolled hyperinflammation simultaneously triggers significant immunosuppression, the net effect being increased risk of organ dysfunction, infection and complications.
CPB, cardiopulmonary bypass; DC, dendritic cells; ROS, reactive oxygen species; HMGB1, high‐mobility group box protein B; IFN‐γ, interferon gamma; IL‐1β, interleukin 1 beta; IL‐6, interleukin 6; IL‐10, interleukin 10; IL‐12, interleukin 12; IM, inflammatory macrophage; MDSC, myeloid‐derived suppressor cells; MO, monocytes; NET, neutrophil extracellular traps; NK, natural killer; NU, neutrophil; PGE2, prostaglandin E2; PRR, pattern recognition receptor; SIRS, systemic inflammatory response syndrome; TGF‐β, transforming growth factor β; TNF‐ɑ, tumour necrosis factor alpha; T reg, regulatory T cell; T cyto, cytotoxic T cell; Th1, T helper type 1; Th2, T helper type 2; Th17, T helper type 17. Adapted with permission from reference [20].
