Abstract
Aims and Methods
To find a simpler cure for stress urinary incontinence (SUI) without tapes. Proposed is a paraurethral operation with incisions in both sulci to plicate pubourethral ligaments (PUL) with thick polyester sutures.
Results
VIDEO and ultrasound experiments showed the main cause of SUI was weak PULs extending on effort, allowing the posterior pelvic muscles to open out posterior urethral wall, so urine was lost on effort. Midurethral sling (MUS) tapes prevent PUL extension and SUI. The research question: “Would PUL plication by 0.5 or 0.25 mm polyester tapes create sufficient new collagen to cure SUI in the longer term?” Instron‐testing of collagen from a rejected polyester aortic graft indicated sufficient potential collagen strength. Five surgeons unrelated to the authors who tested the new operation, reported negative cough tests on 30/31 women before patient discharge; these data were encouraging, but not conclusive.
Conclusions
PUL ligament repair by large polyester sutures, like the MUS, appears to prevent PUL elongation and cure SUI in the very short term, thereby validating the predictions of the Integral Theory as regards the role of ligaments in continence. If successful long term, this operation could avoid many problems associated with MUS operations.
-
1.
Simplicity: less surgical skill is required; the local anesthetic methodology makes the operation widely scalable especially in poor countries with few health facilities.
-
2.
Built‐in safety: there is no tape to compress urethra, no applicators to damage bladder, nerves, blood vessels, bowel.
-
3.
Cost: a polyester suture.
Keywords: artificial neoligament, collagenopoiesis, integral theory, polyester repair of pubourethral ligament, SUI surgery
1. INTRODUCTION
This is not a criticism of the midurethral sling (MUS). Performed by skilled, experienced surgeons, it has high cure rates with acceptable complications. The MUS is the gold standard operation for stress urinary incontinence (SUI) with an estimated 10,000,000 operations to date, and some 2000 scientific papers. The scientific breakthrough was the prototype MUS sling in 1990 and the Integral Theory on which it was based. 1 https://obgyn.onlinelibrary.wiley.com/toc/16000412/1990/69/S153. The suburethral sling prevented the pubourethral ligament (PUL) from elongating under stress to cause SUI, Figure 1A,B and which stimulated collagenopoiesis (new collagen) to structurally reinforce PULs. 3
Figure 1.
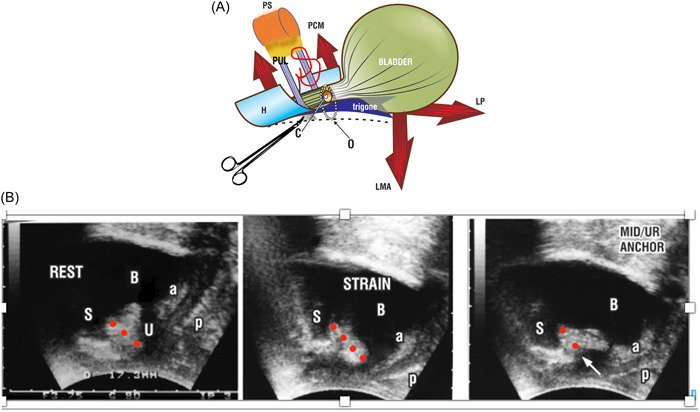
(A) Sagittal schematic view, woman with stress urinary incontinence (SUI) AT REST(unbroken lines). Pubourethral ligament (PUL) extends from pubic symphysis (PS) to attach to midurethra. STRAIN (broken lines) On effort, LMA pulls down the trigone. A weak or loose PUL is stretched by LMA, opening posterior urethral wall from “C” closed to “O” open; urine is lost (SUI). Hemostat test Hemostat inserted behind the symphysis as in the VIDEO supports PUL. Urethral closure at bladder neck and distally by pelvic muscles (arrows) is restored (white arrow, panel B). No.5 (0.5 mm) polyester suturing (red) of both PULs would prevent USL elongating on stress in the same manner as a sling below the urethra. C, closed urethra; H, distal vagina “hammock”; LMA, conjoint longitudinal muscle of the anus; LP, levator plate; O, open urethra; PCM, pubococcygeus muscle; PS, symphysis. (B) Transperineal ultrasound of a woman with SUI 2 At rest a&p are the anterior and posterior walls of the vagina; b, bladder; S, symphysis; U, urethra; red circles indicate PUL extending from behind lower border of the symphysis to the midurethra. Strain PUL extends. a&p move backwards/downwards to open out the posterior wall of the urethra, opening the urethra along its length. Mid/urethral anchor A hemostat (white arrow) inserted behind the symphysis as in the VIDEO creates closure at the bladder neck and distally; a&p are obviously tensioned.
Despite these encomiums, reports continue to appear quoting low cure rates, urinary retention, and other complications, some serious. Skill‐related, 4 or not, these reports have to be taken seriously; an operation which affects some 30% of all women should ideally be simple, available, inexpensive, effective, with minimal complications. On analysis, most MUS problems seem to arise from the tape itself and how it is inserted. Even a 0.5 mm change from the optimal urethral diameter, whether marginally tight or loose, can have an exaggerated effect, because the change in urethral diameter alters the resistance to urine flow from the detrusor, as it is determined by the inverse of the 4th power of the urethral radius (Poiseuille's Law). 2 For example, reducing the urethral diameter from 4 mm radius to just 3.5 mm increases the detrusor pressure required to expel urine from 100 cm H2O to 172 cm at a flow of 50 ml/s. 2 This contribution asks the question, “Is there a simpler way to surgically address the major cause of SUI, elongation of the PUL under stress, 5 Figure 1A,B, other than using an MUS tape, for example, by using polyester sutures to plicate PUL, VIDEO 1.
A simplified operation for cure of SUI and its anatomical rationale is presented. This is not a new operation. It formed the 2nd part of the 1997 MUS 6 methodology, which was to repair the suburethral vagina, similar in principle to Figure 2 (left) after the MUS tape had been inserted via two parallel incisions as a “U,” but using vicryl sutures. Like the hemostat in VIDEO 2, 6 the ultrasound, Figure 1B, and the MUS sling, the new operation seeks to prevent PUL elongation and SUI.
Figure 2.
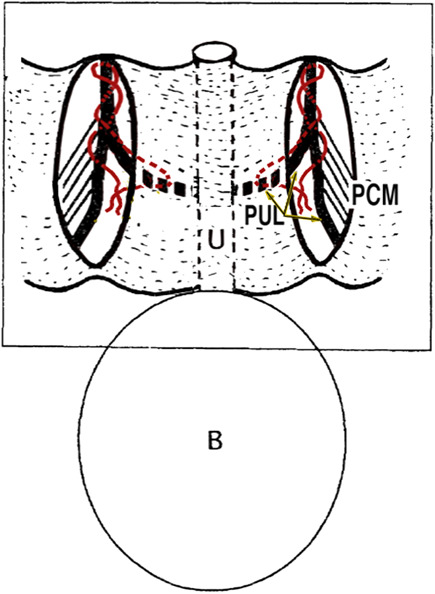
Proposed operation for cure of stress urinary incontinence. The proposed operation uses No.5 or No.2 polyester sutures (red) to bind together both branches of pubourethral ligaments (PUL) to symphysis, midurethra medially and pubococcygeus muscle (PCM) laterally below the level of the vagina. The vaginal skin is closed with 00 vicryl sutures.
Ideally, nonabsorbable No.5 or even No.2 polyester sutures would be used to prevent PUL elongation by binding PUL to connective tissue structures behind the symphysis, vagina and pubococcygeal muscle laterally, as shown schematically in Figure 2 and anatomically in Figure 3. 7
Figure 3.
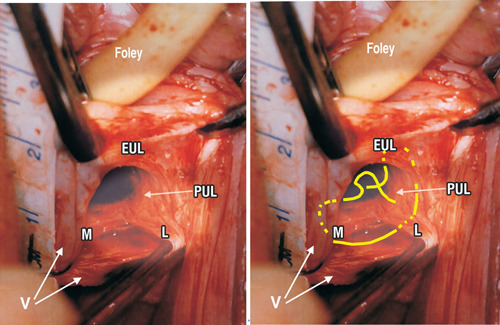
Live anatomy—surgical binding of loose pubourethral ligaments (PUL). Left: Original live anatomical dissection 6 of PUL (left incision) during a two incision IVS operation. 2 The tape measure overlies the urethra. The left paraurethral sulcus has been incised along its length and opened out laterally with forceps. External urethral ligament (EUL) is the EUL which sits in front of the pubic symphysis (PS). The PUL, originates behind PS from its lower posterior part. Coming down from PS, PUL splits into two parts, medial (M) to insert into the side of the midurethra and L (lateral). “L” attaches laterally to pubococcygeus muscle (not seen) then comes down to attach to the vagina (V). Right: No.2 or preferably, No.5 polyester sutures bind both branches of PUL to fascias attached to pubic bone, urethra, vagina and pubococcygeus muscle (PCM), essentially as performed in the original operation. 1
The research question driving this initiative was, “If the Integral Theory statement is correct, and it is reinforcement of PUL by collagen‐producing tapes which cures the SUI, why wouldn't PUL repair by polyester sutures, without any tapes, not cure SUI, if they could create sufficient collagen to strengthen the PULs?” Biomechanical testing relative to a natural ligament 8 indicated that it may; the structural support of the collagen created by the polyester implant 9 was two orders of magnitude greater (x100) than the estimated requirement for a ligament. 8
Scope of the surgery: The centimeter measure, Figure 3, gives an accurate perspective of the scope of the surgery. With reference to Figure 3, the operating field, a space of 2 cm, contains the distal urethra, both branches of PUL originating behind the symphysis, pubococcygeus muscle (PCM) (lateral and unexposed) External urethral ligament (EUL). EUL is the main anatomical support of the external urethral meatus, which lies on the anterior surface of the symphysis. 7
The surgical technique performed, VIDEO 3 Figures 2 and 3 (right) is, in principle, similar to the paraurethral operation that was described previously. 6 Under tension, two parallel incisions are made in each sulcus, from bladder neck to pubic bone. The incisions are opened out laterally with forceps or dissecting scissors to reveal the two branches of PUL, Figure 3. 7 A No.5 polyester suture, Figure 3, penetrates the PUL, fascial tissues behind the pubic bone and the proximal part of the PCM.
How the sutures are tied is important, so as not to distort the longitudinal direction of the urethra. The sutures are inserted, one at a time, but tied at the same time after the insertion is complete, but not tied tightly. In the ultrasound, Figure 1B, the normal position of the structures at REST, Figure 1B, (left frame), indicates the suture should be tension‐free, just sufficient to bind the structures together, so as to prevent the extension of the PUL which causes SUI, (middle frame, STRAIN, Figure 1B). The vaginal skin incisions are approximated with 00 Vicryl.
2. EVIDENCE TO JUSTIFY THE PROPOSED SUI SURGERY
Concurrent study of a midurethral hemostat test VIDEO and its ultrasound equivalent, Figure 1B, provide strong anatomical evidence for the proposed operation, Figures 2 and 3. NOTE that the patient does not lose urine except when she coughs. This is an important observation. It means that the organs are in the correct position at rest. The left ultrasound image, “REST” Figure 1B, confirms this statement; the urethra is closed and in the correct anatomical position. The PUL is outlined by three red circles. In the middle ultrasound frame, (STRAIN), the urethra opens along its length on straining, from the bladder neck to the external meatus, and the patient loses urine; the PUL visibly lengthens (four red circles); the anterior and posterior vaginal walls (a&p) are tensioned and pulled back and down, obviously by a downward/backward force. In the far‐right ultrasound image (MID UR ANCHOR), Figure 1B, the urethral opening along its length which is seen in the “STRAIN” frame, is prevented by the hemostat (white arrow) which supports the PUL (red circles). The urethra is closed distally and at bladder neck.
A perspective: The measuring tape over the urethra in the live anatomical study, Figure 3, shows the PUL structures occurring within a space of only 2 cm. 7 One or two sutures would be sufficient to bind PUL to the fascia behind the pubic bone, urethra medially and PCM laterally, so as to prevent PUL extension on stress. The same procedure would also repair the loose suburethral vaginal hammock, like taking a fold of the vagina in VIDEO 2.
2.1. What the video and ultrasound examples mean for the surgery
Any PUL operation for SUI cure, for example, MUS, needs to prevent PUL lengthening and needs to provide new collagen to strengthen the PUL. The MUS does both. The proposed vaginal operation, Figures 2 and 3, potentially do both. The polyester suture binds both PULs in the resting position, so the PUL does not extend on effort as in the middle frame, Figure 1B. Also, it creates new collagen to strengthen the PUL, exactly as does the MUS, but without the tape.
2.2. A critical question for this surgery
Do the No.5 or No.2 polyester sutures produce sufficient collagen to bind the muscle/ligament structures, Figures 1, 2, 3, which are key to preventing the PUL elongating to cause SUI? This question was examined in the 1st author's Doctor of Surgery thesis, 9 where collagen from a rejected polyester aortic graft was tested on an Instron tensiometer; it pulled out of the grips at a force of 0.64 MPa (92 lbs/sq inch). 9
The known breaking strain of collagen, 18,000 lbs/sq inch 10 (124 MPa) was confirmed by Svensson et al. 11 who tested collagen fibrils to a mean strain value corresponding to a stress of 89 ± 15 MPa. Collagen fascicles tested by Svensson et al. had a mean diameter of 0.27 ± 0.16 mm. The value of the target stress was 12.9 ± 3.9 MPa. 11
Based on the experimental animal and human studies, 3 , 5 , 6 , 9 it can be assumed that the No.5 polyester sutures, diameter of 0.5–0.6 mm, would create a cylinder of collagen 0.5 mm in diameter, twice the diameter of the fascicles tested by Svensson et al. 11 It can be calculated that the collagen reaction from a No.5 polyester suture should sustain a force twice Svensson et al.'s fascicles, approximately 26 MPa. According to Yamada, 8 a ligament can sustain a force of 300 mg/mm2 (0.00294 MPa). Even when calculating on the 0.64 MPa of the collagen from the polyester graft which pulled out of the Instron tensiometer, 9 the collagen strength from even a No.2 polyester suture would be at least two orders of magnitude (x100) greater than for a Yamada ligament. 8
2.3. Initial external postoperative data
Thirty‐one women have so far been treated by ethical committee approved experimental surgery for SUI by PUL plication in four different countries, Turkey (Professor Akin Sivaslioglu‐No.3 polyester) Australia (A/Professor Ray Hodgson‐No.2 polyester), Romania (Professors P&E Bratila) and China (Professor Xiuli Sun‐No.2 polyester). Of 31 patients treated with this operation, 30 reported negative cough tests immediately before discharge. One woman had urinary retention postoperatively, but passed urine normally within 24 h. VIDEO 3 of the operation is by permission of Professor Akin Sivaslioglu.
3. DISCUSSION
The proposed surgery, Figures 2 and 3, VIDEO 3, is based on basic science experiments 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 and the clinical experience of the bilateral incision methodology, Figures 2 and 3, extending over many hundreds of cases. 6 If the assumptions on neocollagen formation are correct, two polyester sutures, one on each side, as in Figure 2, would bind PUL to the urethra, PCM, EUL and symphysis to restore both the distal and bladder neck closure mechanisms. 1 Theoretically, a No.2 polyester suture (0.2–0.25 mm) should be sufficient. Very early preliminary results in 31 women confirm the anatomical validity of the surgery and the Integral Theory on which the operations are based. The initial postoperative data are encouraging, but numbers are small and follow‐up extremely short. However, if a high level of continence can be maintained for 12 months in sufficient numbers, it is likely that a cure may last much longer, as shown by Nilsson with the TVT. 12 In a 17‐year follow‐up study of the TVT, Nilsson et al. showed minimal deterioration of 12‐month SUI cure data. 12
4. CONCLUSIONS
If still successful by 12 months, this operation could solve many problems which are at the core of criticisms of existing MUS operations.
-
1.
Simplicity. There is no need for a tape; far less surgical skill is required than for an MUS. The whole operation is performed in a space of 2 cm. Based on calculations from the first author's Doctor of Surgery thesis, 9 No.5 or even No.2 polyester sutures on each side should be sufficient to repair weakened ligaments. The operation can be performed safely under spinal or local anesthetic by any surgeon knowledgeable in vaginal anatomy. As such, it is widely scalable especially in poorer countries with limited health facilities.
-
2.
Built‐in safety. The operation is far less invasive. It has no applicators which can damage bladder, nerves, blood vessels, bowel. It has no tape to compress the urethra to cause postoperative urinary retention or urethral perforations.
-
3.
The cost is that of a polyester suture rather than a $1000 kit.
AUTHOR CONTRIBUTIONS
Planning, data, figures, writing: Peter Petros. Discussions of content: Peter Petros and Paolo Palma.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supporting information
VIDEO 1 Anatomical basis of the proposed plicate pubourethral ligaments operation for cure of stress urinary incontinence.
VIDEO 2 Mechanically supporting the plicate pubourethral ligaments prevents forcible opening by the posterior pelvic muscles.
VIDEO 3 of plicate pubourethral ligaments plication surgery‐ by permission, Professor Akin Sivaslioglu. Two parallel full thickness incisions from the bladder neck to the external urethral meatus (EUM). Opening out of the incision to reveal the two branches of PUL, to urethra and to the vagina. No.3 polyester suture commencing at midurethra, ascending to the external urethral ligament just lateral to EUM with insertion into the pubococcygeus muscle laterally.
Supporting information.
ACKNOWLEDGMENTS
Initial surgical data of the new PUL operation: Akin SIvaslioglu; Ray Hodgson, Petre and Elvira Bratila, Xiuli Sun. VIDEO Akin Sivaslioglu. Open access publishing facilitated by The University of Western Australia, as part of the Wiley ‐ The University of Western Australia agreement via the Council of Australian University Librarians.
Petros P, Palma P. Conceptualizing stress urinary incontinence surgery beyond midurethral slings: very early results from simplified ligament repair without tapes. Neurourol Urodyn. 2023;42:383‐388. 10.1002/nau.25049
DATA AVAILABILITY STATEMENT
All relevant data is contained in the manuscript.
REFERENCES
- 1. Petros PE, Ulmsten U. An integral theory of female urinary incontinence. Acta Obstet Gyn Scand. 1990;69(suppl 153):7‐31. [DOI] [PubMed] [Google Scholar]
- 2. Petros PE, Bush MB. A mathematical model of micturition gives new insights into pressure measurement and function. Int Urogynecol J. 1998;9:103‐107. [DOI] [PubMed] [Google Scholar]
- 3. Petros PE, Ulmsten U, Papadimitriou J. The autogenic neoligament procedure: a technique for planned formation of an artificial neo‐ligament. Acta Obstet Gyn Scan. 1990;69(suppl 153):43‐51. [DOI] [PubMed] [Google Scholar]
- 4. Petros PE. Understanding the mechanics of closure is key to optimal midurethral sling technique. Int Urogynecol J. 2020;32(1):39‐45. 10.1007/s00192-020-04533-9 [DOI] [PubMed] [Google Scholar]
- 5. Petros PE, Von Konsky B. Anchoring the midurethra restores bladder neck anatomy and continence. Lancet. 1999;354(9193):997‐998. [DOI] [PubMed] [Google Scholar]
- 6. Petros PE. New ambulatory surgical methods using an anatomical classification of urinary dysfunction improve stress, urge, and abnormal emptying. Int Urogynecol J. 1997;8(5):270‐278. [DOI] [PubMed] [Google Scholar]
- 7. Petros PE. The pubourethral ligaments‐an anatomical and histological study in the live patient. Int Urogynecol J. 1998;9:154‐157. [DOI] [PubMed] [Google Scholar]
- 8. Yamada H. Aging Rate for the Strength of Human Organs and Tissues. Strength of Biological Materials. Williams & Wilkins Co; 1970:272‐280. [Google Scholar]
- 9. Petros PE. Development of the Intravaginal Slingplasty and other Ambulatory Vaginal Operations. Doctor of Surgery Thesis. University of Western Australia; 1999.
- 10. Florey H. General Pathology. Lloyd Luke; 1971. [Google Scholar]
- 11. Svensson RB, Hassenkam T, Grant CA, Magnusson SP. Tensile properties of human collagen fibrils and fascicles are insensitive to environmental salts. Biophys J. 2010;99(12):4020‐4027. 10.1016/j.bpj.2010.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nilsson CG, Palva K, Aarnio R, Morcos E, Falconer C. Seventeen years' follow‐up of the tension‐free vaginal tape procedure for female stress urinary incontinence. Int Urogynecol J. 2013;24:1265‐1269. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
VIDEO 1 Anatomical basis of the proposed plicate pubourethral ligaments operation for cure of stress urinary incontinence.
VIDEO 2 Mechanically supporting the plicate pubourethral ligaments prevents forcible opening by the posterior pelvic muscles.
VIDEO 3 of plicate pubourethral ligaments plication surgery‐ by permission, Professor Akin Sivaslioglu. Two parallel full thickness incisions from the bladder neck to the external urethral meatus (EUM). Opening out of the incision to reveal the two branches of PUL, to urethra and to the vagina. No.3 polyester suture commencing at midurethra, ascending to the external urethral ligament just lateral to EUM with insertion into the pubococcygeus muscle laterally.
Supporting information.
Data Availability Statement
All relevant data is contained in the manuscript.


