Abstract
Aim
The aim of this study was to assess the resuscitators' opinions of the usefulness and clinical value of using a respiratory function monitor (RFM) when resuscitating extremely preterm infants with positive pressure ventilation.
Methods
The link to an online survey was sent to 106 resuscitators from six countries who were involved in a multicentre trial that compared the percentage of inflations within a predefined target range with and without the RFM. The resuscitators were asked to assess the usefulness and clinical value of the RFM. The survey was online for 4 months after the trial ended in May 2019.
Results
The survey was completed by 74 (70%) resuscitators of which 99% considered the RFM to be helpful during neonatal resuscitation and 92% indicated that it influenced their decision‐making. The majority (76%) indicated that using the RFM improved their practice and made resuscitation more effective, even when the RFM was not available. Inadequate training was the key issue that limited the effectiveness of the RFM: 45% felt insufficiently trained, and 78% felt more training in using and interpreting the RFM would have been beneficial.
Conclusion
Resuscitators considered the RFM to be helpful to guide neonatal resuscitation, but sufficient training was required to achieve the maximum benefit.
Keywords: neonatal resuscitation, respiratory function monitor, training, user experience
Abbreviation
- RFM
respiratory function monitor
Keynotes.
An online survey collected feedback on using a respiratory function monitor (RFM) when resuscitating extremely preterm infants with positive pressure ventilation.
Most (99%) of the 74 respondents said that the RFM was helpful during neonatal resuscitation and 76% indicated that it improved their practice and made resuscitation more effective.
However, 45% felt insufficiently trained and 78% felt more training in using and interpreting the RFM would have been beneficial.
1. INTRODUCTION
A respiratory function monitor (RFM) can be used during neonatal resuscitation at birth to guide respiratory support. AN RFM provides a real‐time display of ventilation pressures, tidal volumes delivered, mask leak, airway obstruction, heart rate, oxygen saturation and inspired fraction of oxygen during assisted ventilation. It also displays tidal volumes during spontaneous breathing. Hence, an RFM enables resuscitators to deliver tidal volume‐targeted ventilation and determine whether corrective steps to improve ventilation are successful, such as mask repositioning and pressure adjustments. 1 A number of manikin and clinical studies have shown that using an RFM in the delivery room improved the consistency of positive pressure ventilation. 2 , 3 , 4 , 5 , 6 , 7 , 8 However, audits of resuscitation videos in 2010 showed that resuscitators did not use an RFM consistently, as it was difficult to assimilate this additional information during neonatal resuscitation. Resuscitators emphasised that extra training was necessary if they were to effectively use the RFM as part of standard care during neonatal resuscitation. 9
The multi‐centre randomised controlled trial of respiratory function monitoring during stabilisation of preterm infants at birth (MONitoR trial) 10 investigated the use of an RFM during neonatal resuscitation of extremely preterm infants at birth. It reported that with access to the visual display and physiological data provided by the RFM, there were no differences between the RFM and no RFM groups in the percentage of inflations within a predefined expired tidal volume target range or in the number of adjustments made to the ventilation settings. An ancillary study reported that resuscitators directed 29% of their total visual attention to the RFM when it was visible. 11 Therefore, it was unclear whether the resuscitators considered that the RFM provided helpful and beneficial guidance during neonatal resuscitation. As resuscitators become more familiar with RFMs, their opinions of them may have changed.
The aim of this follow‐up study was to assess the resuscitators' opinions of the usefulness and clinical value of the RFM they used for neonatal resuscitation during the MONitoR trial.
2. METHODS
This was an online survey that explored the experiences of resuscitators from seven neonatal intensive care units in six countries who took part in the multicentre MONitoR trial from October 2013 to May 2019. 10 It included participants from the Netherlands, Australia, Germany, Spain, Italy and the USA. The aim of that study was to compare two groups resuscitating extremely preterm infants born at 24–27 weeks of gestation with positive pressure ventilation. One group used the RFM, and the other group did not. The authors analysed data on 288 infants and 51 352 inflations. 10
During the MONitoR trial, the ALD resuscitation monitor (Advanced Life Diagnostics, Weener, Germany) displayed the following parameters (Figure 1): peak inspiratory pressure, positive end‐expiratory pressure, respiratory rate, inspiratory and expiratory tidal volumes, mask leak, heart rate, pulse oxygen saturation, fraction of inspired oxygen and time since birth. Most sites also video‐recorded the resuscitations. The pressure, flow, expiratory tidal volume (ml/kg) and pulse‐oximetry plethysmograph waves were displayed. The expiratory tidal volume target range (4–8 ml/kg) was displayed using two horizontal red lines. All personnel involved in the trial were trained in the use of the RFM by local neonatologists at each participating centre before the trial started. 10
FIGURE 1.
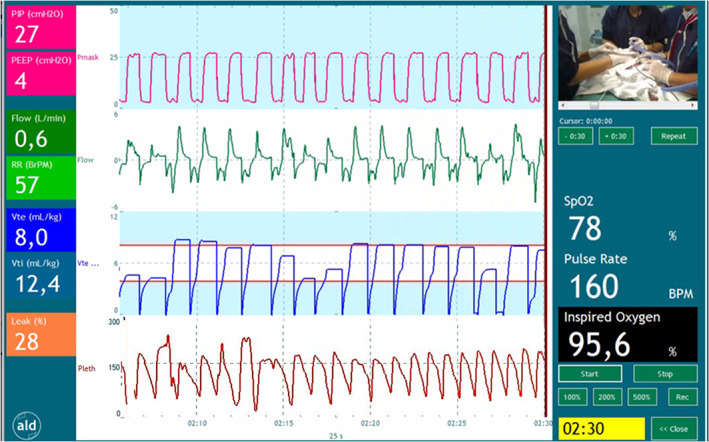
Respiratory function monitor display. Numeric data displayed on the left side of the screen include peak inspiratory pressure (cm H2O), positive end‐expiratory pressure (cm H2O), flow (L/min), respiratory rate (inflations per minute), expired and inspired tidal volume (ml/kg) and mask leak (%). Waveform data displayed in the middle of the screen include inflation pressure (cm H2O), flow (mL/min), expired tidal volume (ml/kg) and the plethysmograph of the pulse oximeter. The red horizontal lines in the expiratory tidal volume waveform delineate the target range of 4–8 ml/kg. The right side of the screen includes the camera view, oxygen saturation (%), heart rate (pulse rate, beats per minute), fraction of inspired oxygen (%) and the time (min:sec) from birth. The data displayed on the screen represent real‐time values of each respiratory parameter at the vertical red line at the right end of the waveform data.
The principal investigators involved in the MONitoR trial 10 provided a list of 106 resuscitators, who had taken part in the trial and were accredited to provide respiratory support to very preterm infants at birth using the RFM. They were approached by email and invited to complete the online survey, which ran for 4 months after the MONitoR trial finished. This survey (Appendix S1) consisted of 13 multiple choice questions that were sub‐divided into six sections: provider demographics (three items), RFM screen (one item), training (three items), interpretation of different scenarios (two items), clinical value of the RFM (three items) and suggested improvements (one item). Resuscitators had the opportunity to explain their answers and provide recommendations on training, usefulness and suggested improvements in an open text field. Another open question allowed the respondents to provide feedback on any other aspect of the RFM.
The four‐month survey was hosted by the Castor online platform (Castor EDC, Amsterdam, the Netherlands). Resuscitators were informed that completion of the survey demonstrated consent to participate, analyse their responses and use them for publication.
Quantitative data were analysed using SPSS Statistics, version 25 (IBM Corp, New York, USA). Categorical data are presented as numbers and percentages. Qualitive data were analysed using content analysis.
The study was conducted according to the principles of the Declaration of Helsinki and approved by the Ethics Review Committee of Leiden University Medical Centre (N20.155).
3. RESULTS
3.1. Study population
The link was sent to 106 eligible resuscitators and 74 (70%) completed the survey (Figure 2). Their professional levels were as follows: residents (16%), physician assistants (5%), neonatology fellows (18%) and neonatologists (61%). Half of the respondents were involved in 10–30 RFM‐guided resuscitations per year. Most respondents (92%) agreed that the main potential clinical benefit of using the RFM in the delivery room was delivering more effective ventilation.
FIGURE 2.
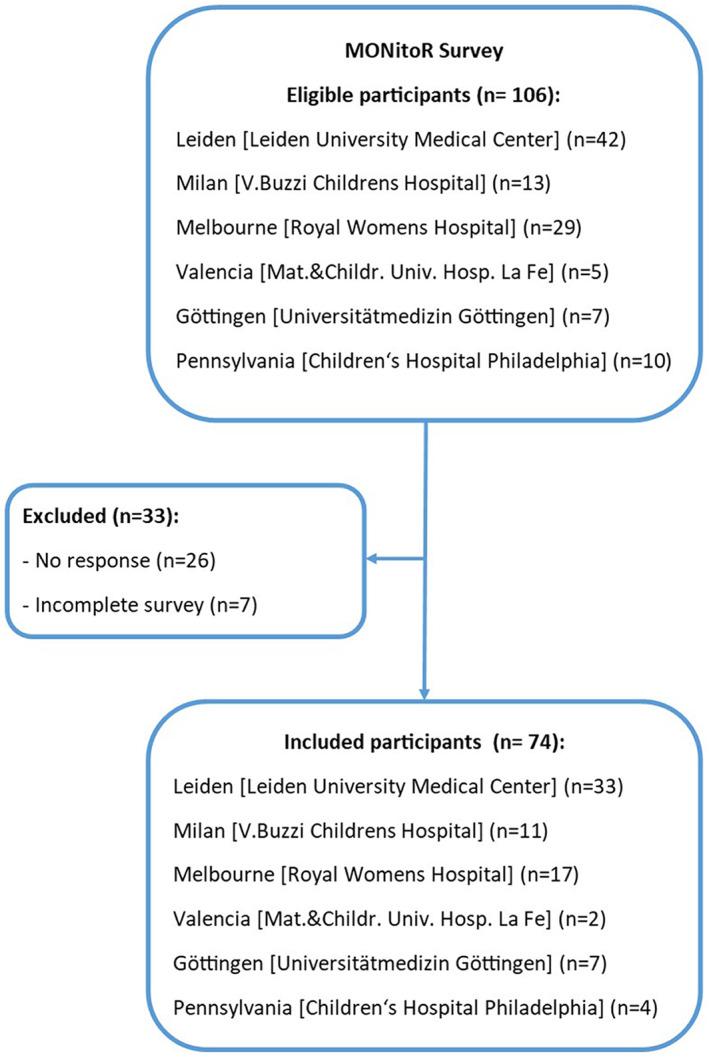
Flow chart
3.2. Training and auditing
Of all the respondents, 45% felt they had insufficiently training in the use of the RFM and 78% felt more training in using and interpreting the RFM would be beneficial. Many felt that this should entail a digital introductory course, simulation sessions, regular reviews of neonatal resuscitations and the opportunity discuss interesting RFM data and videos with different centres (Table S1).
Two‐thirds of the respondents (66%) stated that they had the opportunity to review their resuscitations with the team involved at least once a month.
3.3. Use of the RFM
Most respondents (87%) stated that they looked at the data provided by the RFM during neonatal resuscitation. The most commonly cited parameters that were used to guide resuscitation by respondents were as follows: mask leak (%), tidal volume (graph), pulse oxygen saturation (%) and heart rate (beats per minute; Table S2).
3.4. Interpreting the RFM and its effect on decision‐making
Most respondents (81%) indicated that information from the RFM was used by both the airway provider and the resuscitation leader during resuscitation. The vast majority (99%) considered the RFM to be helpful to guide ventilation during neonatal resuscitation and most (92%) indicated that it influenced their decisions and/or actions during resuscitation. The majority (76%) believed that the knowledge gained by using the RFM during resuscitation, and retrospective reviews of resuscitations with supportive RFM data, reinforced their decisions and/or actions during resuscitation. They also stated that their experience with the RFM would theoretically guide their actions during future resuscitations, even if the RFM was unavailable.
Respondents reported that the RFM provided information and direct feedback on mask leak, expired tidal volumes during ventilation, airway obstruction and spontaneous breathing. In addition, the indirect feedback that they received by retrospectively reviewing neonatal resuscitations enabled them to learn from colleagues and increase their knowledge of the physiology of breathing and factors that influence ventilation at birth (Table S3).
3.5. Suggested improvements
The majority of respondents (61%) would not change the current RFM display and data outputs. A less complex interface was the most frequent suggestion and was mentioned by 15% of the respondents (Table S4).
Other feedback included that the mask ventilation could be hampered by the heavy top that the flow sensor created between the T‐piece and the face mask. Other findings from this survey included a request for improved communication between centres on their experiences with the RFM and better customer support from the manufacturer.
4. DISCUSSION
We conducted a survey of users' experience of the RFM in order to assess its clinical usefulness during neonatal resuscitation. The respondents had all participated in the largest clinical trial of this device. 10 Most said they used the RFM to guide their ventilation and valued constructive and objective feedback when data from individual cases were reviewed as part of quality improvements and training activities. The survey highlighted the need for improved training, as a large proportion of respondents felt insufficiently trained to effectively use and interpret data from the RFM. As most respondents would not change the current RFM design, the findings from our survey suggest that training should focus on appropriate interpretation of data and tips on troubleshooting common scenarios. These could include identifying and correcting airway obstruction, leak or excessive tidal volumes. Most of the participants recommended regular reviews, at least monthly, to share knowledge gained from the recordings.
Most of the respondents would like to receive more training in using and interpreting the RFM during neonatal resuscitation. The need for extra training on using the RFM used in our multi‐centre MONitoR trial was also reported by Schilleman et al. 9 Previous studies 12 , 13 , 14 , 15 , 16 have showed that knowledge and skills diminish 2–4 months after completing neonatal resuscitation training and that booster sessions and activities are needed. Regular reviews of recordings of neonatal resuscitations may be useful, as this would improve the skills needed for successful delivery room management. 13 , 17 These related to cognitive skills, such as knowledge of physiology and clinical decision‐making, technical skills, including mask techniques and interpreting RFM signals, and behavioural skills like communication. Having combined these results with the feedback from our respondents, we suggest the following regime for RFM training. First, there should be an introductory course in using and interpreting the RFM. Second, simulation sessions should be held. Third, resuscitators should review their own resuscitations with a local expert, as part of monthly resuscitation reviews highlighting the interpretation of RFM data.
Most respondents agreed that the main clinical benefit of using the RFM in the delivery room was the potential to deliver more effective ventilation. However, our multi‐centre randomised controlled trial reported no differences between the RFM and no RFM group in the percentage of inflations within a predefined expired tidal volume target range or in the number of adjustments made to ventilation settings. 10 The lack of effect may have been due to insufficient training before using the RFM and lack of training opportunities throughout the 6‐year study period. Whether the results may also have been influenced by the gained knowledge to theoretically guide ventilation remains uncertain.
This survey found that 15% of the respondents would have preferred the RFM to have a simpler visual interface. Based on the most frequently used parameters, and the proposed changes, the screen should at least provide information on key factors. These should be the applied pressures, coloured flow curves showing leaks and obstructions, a colour‐coded graph showing tidal volumes and heart rate, pulse oxygen saturation and fraction of inspired oxygen.
Using the RFM in the delivery room enabled resuscitators to objectively assess an infant's clinical condition and evaluate the effect of their resuscitative interventions. In addition, retrospective reviews of videos and RFM recordings of neonatal resuscitations enabled them to learn from their colleagues' experiences. Den Boer et al. studied the benefits of recording and reviewing neonatal resuscitation. The authors reported that indirect feedback was valuable for reassurance and self‐improvement and reflecting on compliance with guidelines. It also taught resuscitators to only intervene when necessary during neonatal resuscitation. 13 However, there are two questions that need to be answered before claims about the clinical validation and utility of the RFM used in this study can be made. These are whether interpreting the data leads to appropriate decision‐making and whether clinical reviews improve provider performance during neonatal resuscitation, independent of the availability of the RFM. The evidence so far shows that using the RFM in the delivery room has raised clinically important research questions and provided insights into scientific knowledge gaps. 17 , 18
Our exploratory survey had several limitations. The training and review strategies and the total number of resuscitations performed using the RFM differed by centre. Although this influenced our results, it also enabled us to provide realistic and generalisable recommendations for using this RFM in the delivery room.
To guide resuscitation and influence decision‐making, resuscitators require knowledge about the physiology of neonatal transition and the factors that influence ventilation. They also need practice assimilating and interpreting the physiological measurements so that they can integrate the information displayed by the RFM. This is a skill that may be learned through simulation training and real‐time resuscitations, as well as reviewing them. Further research is necessary to evaluate whether sufficient and continuous training and/or a simplified visual interface would improve the helpfulness and effectiveness of the RFM.
5. CONCLUSION
The resuscitators who took part in our online survey reported that, overall, the RFM was a helpful tool to guide resuscitation. However, most of them felt that additional training was required in order to achieve the greatest benefits.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
Supporting information
Appendix S1
Table S1–S4
Kuypers KLA, van Zanten HA, Heesters V, Kamlin O, Springer L, Lista G, et al. Resuscitators' opinions on using a respiratory function monitor during neonatal resuscitation. Acta Paediatr. 2023;112:63–68. 10.1111/apa.16559
REFERENCES
- 1. Foglia EE, Te Pas AB. Effective ventilation: the most critical intervention for successful delivery room resuscitation. Semin Fetal Neonatal Med. 2018;23(5):340‐346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Schmolzer GM, Morley CJ, Wong C, et al. Respiratory function monitor guidance of mask ventilation in the delivery room: a feasibility study. J Pediatr. 2012;160(3):377‐381.e2. [DOI] [PubMed] [Google Scholar]
- 3. van Vonderen JJ, van Zanten HA, Schilleman K, et al. Cardiorespiratory monitoring during neonatal resuscitation for direct feedback and audit. Front Pediatr. 2016;4:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zeballos Sarrato G, Sanchez Luna M, Zeballos Sarrato S, Perez Perez A, Pescador Chamorro I, Bellon Cano JM. New strategies of pulmonary protection of preterm infants in the delivery room with the respiratory function monitoring. Am J Perinatol. 2019;36(13):1368‐1376. [DOI] [PubMed] [Google Scholar]
- 5. Jain D, D'Ugard C, Aguilar A, Del Moral T, Bancalari E, Claure N. Use of a mechanical ventilator with respiratory function monitoring provides more consistent ventilation during simulated neonatal resuscitation. Neonatology. 2020;117(2):151‐158. [DOI] [PubMed] [Google Scholar]
- 6. O'Currain E, Thio M, Dawson JA, Donath SM, Davis PG. Respiratory monitors to teach newborn facemask ventilation: a randomised trial. Arch Dis Child Fetal Neonatal Ed. 2019;104(6):F582‐F586. [DOI] [PubMed] [Google Scholar]
- 7. Wood FE, Morley CJ, Dawson JA, Davis PG. A respiratory function monitor improves mask ventilation. Arch Dis Child Fetal Neonatal Ed. 2008;93(5):F380‐F381. [DOI] [PubMed] [Google Scholar]
- 8. Milner A, Murthy V, Bhat P, et al. Evaluation of respiratory function monitoring at the resuscitation of prematurely born infants. Eur J Pediatr. 2015;174(2):205‐208. [DOI] [PubMed] [Google Scholar]
- 9. Schilleman K, Siew ML, Lopriore E, Morley CJ, Walther FJ, Te Pas AB. Auditing resuscitation of preterm infants at birth by recording video and physiological parameters. Resuscitation. 2012;83(9):1135‐1139. [DOI] [PubMed] [Google Scholar]
- 10. van Zanten HA, Kuypers K, van Zwet EW, et al. A multi‐Centre randomised controlled trial of respiratory function monitoring during stabilisation of very preterm infants at birth. Resuscitation. 2021;167:317‐325. [DOI] [PubMed] [Google Scholar]
- 11. Herrick H, Weinberg D, Cecarelli C, et al. Provider visual attention on a respiratory function monitor during neonatal resuscitation. Arch Dis Child Fetal Neonatal Ed. 2020;105(6):666‐668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Matterson HH, Szyld D, Green BR, et al. Neonatal resuscitation experience curves: simulation based mastery learning booster sessions and skill decay patterns among pediatric residents. J Perinat Med. 2018;46(8):934‐941. [DOI] [PubMed] [Google Scholar]
- 13. den Boer MC, Houtlosser M, Foglia EE, Tan R, Engberts DP, Te Pas AB. Benefits of recording and reviewing neonatal resuscitation: the providers' perspective. Arch Dis Child Fetal Neonatal Ed. 2019;104(5):F528‐F534. [DOI] [PubMed] [Google Scholar]
- 14. Sawyer T, Ades A, Ernst K, Colby C. Simulation and the neonatal resuscitation program 7th edition curriculum. NeoReviews. 2016;17(8):e447‐e453. [Google Scholar]
- 15. Sawyer T, Sierocka‐Castaneda A, Chan D, Berg B, Lustik M, Thompson M. Deliberate practice using simulation improves neonatal resuscitation performance. Simul Healthc. 2011;6(6):327‐336. [DOI] [PubMed] [Google Scholar]
- 16. Cordero L, Hart BJ, Hardin R, Mahan JD, Nankervis CA. Deliberate practice improves pediatric residents' skills and team behaviors during simulated neonatal resuscitation. Clin Pediatr. 2013;52(8):747‐752. [DOI] [PubMed] [Google Scholar]
- 17. den Boer MC, Martherus T, Houtlosser M, Root L, Witlox R, Te Pas AB. Improving the quality of provided care: lessons learned from auditing neonatal stabilization. Front Pediatr. 2020;8:560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. den Boer MC, Houtlosser M, Witlox R, et al. Reviewing recordings of neonatal resuscitation with parents. Arch Dis Child Fetal Neonatal Ed. 2021;106(4):346‐351. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Table S1–S4


