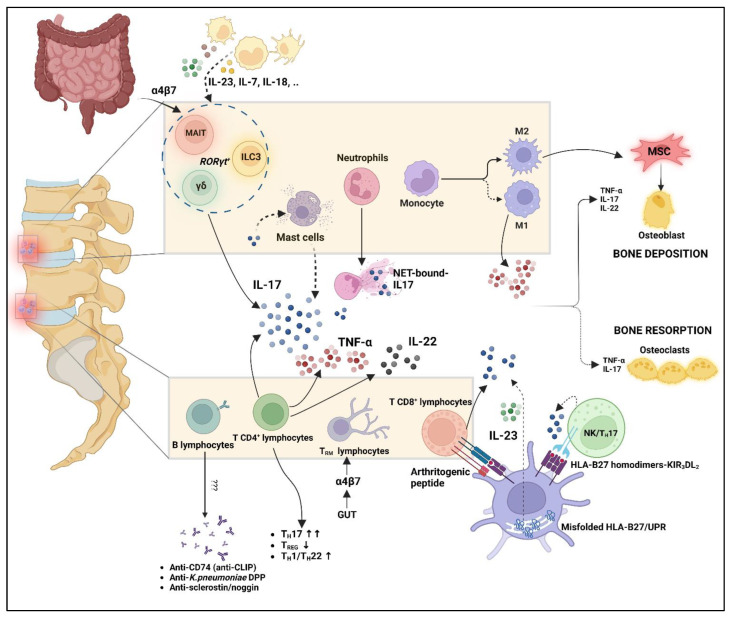
Figure 2.
Interplay of innate and adaptive immune system in axial-SpA pathogenesis. Mast cells are not able to produce IL-17; however, they may capture it from extracellular environments and release it after unknown stimulus. NET-bound-IL17 has been demonstrated useful, along with its capability to induce osteogenic differentiation of MSC. Myeloid cells can produce a large amount of proinflammatory cytokines, which may also act on innate-like lymphocytes and innate lymphoid cells such as MAIT, ILC3, and γδ T cells. Not only these cells, but also the TRM lymphocytes, may concentrate in axial enthesis following migration from the gut, as suggested by intestinal homing markers such as the α4β7 integrin on their surface (gut–joint axis). T cells play a predominant role among adaptive immunity, with an imbalance between TH17 and TREG cells, but also TH1/22 upregulation. T CD8+ cells may be activated after presentation of arthritogenic peptide by HLA-B27. HLA-B27 may also contribute to IL-23/IL17 upregulation due to UPR activation and B272 binding of KIR3DL2 receptors on the NK/ TH17 cell surface. This cellular interplay leads to an aberrant production of proinflammatory cytokines such as TNF-α, IL-17, and IL-22, which in turn may dysregulate bone homeostasis along with M2 macrophages. B lymphocytes are traditionally considered less relevant even if antibody production has been demonstrated. MAIT: mucosal-associated invariant T cells; ILC3: innate lymphoid cells 3; MSC: mesenchymal stem cells; UPR: unfolded protein response. “Created with BioRender.com”.