Abstract
Background
The total prevalence of congenital heart defects (CHDs) varies by populations and over time. Studies that examine trends in the prevalence of CHD in different regions may shed light on our understanding of the occurrence of CHD and the impact of different risk factors.
Objectives
To examine trends in total and live birth prevalence of nonsyndromic CHD in Europe between the years 2008 and 2015 and to investigate if the decreasing trend reported by previous studies is continuing.
Methods
Cases of CHD delivered between January 1, 2008 and December 31, 2015 notified to 25 population‐based EUROCAT (European Surveillance of Congenital Anomalies) registries in 14 countries, formed the population‐based case‐series. Prevalence (total/live) rates and 95% confidence intervals were calculated as the number of cases per 10,000 births (live and stillbirths). Time trends in prevalence of all nonsyndromic CHDs and for three CHD severity groups (very severe, severe, and less severe) were plotted using a Poisson regression multilevel approach.
Results
The total prevalence of nonsyndromic CHD was 57.1 per 10,000 births (live births and stillbirths) for the 8‐year period and remained stable across the three CHD severity groups while the live birth prevalence was 60.2 per 10,000 births. There was considerable variation in the reported total CHD prevalence and the direction of trends by registry. A decreasing prevalence of CHD was observed for the Norway and England/Wales registries, whereas the CHD prevalence increased for registries in Italy and Croatia.
Conclusions
The total prevalence of CHD in Europe between the years 2008 and 2015 remained stable for all CHD and across the three CHD severity groups. The decreasing trend reported by previous studies has not continued. However, we found significant differences in the total and live birth prevalence by registry.
Keywords: congenital heart disease, European Surveillance of Congenital Anomalies, prevalence rate
1. INTRODUCTION
Congenital heart defects (CHDs) are the most frequently occurring group of congenital anomalies in newborns (Rankin et al., 2005) with a live birth prevalence of around 7 per 1,000 live births (Rankin et al., 2005). The total prevalence of CHD varies by region and over time (Khoshnood, Greenlees, Loane, & Dolk, 2011). The etiology of CHD remains largely unexplained for approximately 80% of cases (Rosano, Botto, Botting, & Mastroiacovo, 2000).
The global prevalence of CHD is difficult to accurately establish due to differences in genetic and environmental factors for CHD between populations. Differences in ascertainment of CHD between countries may also contribute to the difficulty in quantifying prevalence rates (PRs). Van der Linde et al. (2011) showed an increasing trend in global CHD prevalence between 1930 and 1995 and a stable trend from 1995 until 2009. A recent systematic literature review by Liu et al. (2019) suggested that the global prevalence of CHD continued to increase between the years 1970 and 2017 and identified regional differences in CHD prevalence. Khoshnood et al. (2013), using data from the European Surveillance of Congenital Anomalies (EUROCAT) for 1990–2007, found that the direction of CHD prevalence trends changed over time, with the total prevalence having increased prior to 2004 and reduced thereafter. Similarly, a population‐based study in Norway (Leirgul et al., 2014) reported that the prevalence of severe CHD (heterotaxia, conotruncal defect, atrioventricular septal defect [AVSD], anomalous pulmonary venous return [APVR], left ventricular outflow tract obstruction [LVOTO], right ventricular outflow tract obstruction [RVOTO], or other complex heart defect) increased from 1994 to 2004 and decreased thereafter by 3.4% annually from 2004 to 2009.
The aim of this study was to examine trends in total and live birth prevalence of nonsyndromic CHD in Europe between the years 2008 and 2015 and to investigate if the decreasing trend reported by previous studies (Khoshnood et al., 2013; Leirgul et al., 2014) is continuing.
2. METHODS
EUROCAT is a European network of population‐based registries for the epidemiological surveillance of congenital anomalies (https://eu-rd-platform.jrc.ec.europa.eu/eurocat_en). Forty‐three registries in 23 countries use high quality multiple sources to collect data on congenital anomalies occurring in live births, fetal deaths from 20 weeks gestation and terminations of pregnancy for fetal anomaly at any gestation (TOPFA). All registries use the WHO International Statistical Classification of Diseases and Related Health Problems version 9 or 10 (ICD‐9 or ICD‐10) according to the birth year; from birth year 2005 the cases must be reported to the Central Registry of EUROCAT coded in ICD‐10, with an additional digit extension (optional) for the British Paediatric Association (BPA) revision. For this study, cases with CHD (ICD‐10 codes Q20–26) with a delivery date between January 1, 2008 and December 31, 2015 notified to 25 population‐based EUROCAT registries (Table 1) that agreed to participate in this study, formed this population‐based case series. Denominator data (stillbirths and live births by registry and year) were provided by EUROCAT (2013). Cases of CHD occurring with any other major congenital anomaly, as defined by EUROCAT, were classified as associated anomalies.
TABLE 1.
Study population and total prevalence of CHDs in 25 EUROCAT registries, 2008–2015
| Registry | Years included | Total births | Total number of CHD cases included PDA in term infants and few other CHD subtypes | Total prevalence (95% CI) of CHD cases included PDA in term infants and few other CHD subtypes (per 10,000 births) | Total number of CHD cases in Severity group I | Total Prevalence (95% CI) of CHD cases in Severity group I | Total number of CHD cases in Severity group II | Total Prevalence (95% CI) of CHD cases in Severity group II | Total number of CHD cases in Severity group III | Total Prevalence (95% CI) of CHD cases in Severity group III | Total CHD cases in severity groups |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Portugal, South | 2008–2015 | 145,292 | 361 | 24.85 [22.35, 27.54] | 20 | 1.38 [0.84, 2.13] | 88 | 6.06 [4.86, 7.46] | 238 | 16.38 [14.37, 18.60] | 346 |
| Ireland, South East | 2008–2014 | 53,378 | 163 | 30.54 [26.04, 35.59] | 22 | 4.12 [2.58, 624] | 51 | 9.55 [7.12, 12.56] | 84 | 15.74 [12.55, 19,48] | 157 |
| UK, Wessex | 2008–2015 | 244,878 | 771 | 31.50 [29.31, 3.78] | 139 | 5.68 [4.77, 6.70] | 331 | 13.52 [12.10, 15.05] | 268 | 10.94 [6.97, 12.34] | 758 |
| France, French W Indies | 2009–2015 | 68,665 | 232 | 33.79 [29.59, 38.42] | 40 | 5.83 [4.6, 7.39] | 69 | 10.05 [7.82, 12.72] | 115 | 16.75 [13.83, 20.10] | 224 |
| UK, South West England | 2008–2015 | 404,701 | 1,388 | 34.15 [32.38, 35.99] | 169 | 4.18 [3.57, 4.86] | 407 | 10.06 [9.10, 11.08] | 747 | 18.46 [17.16, 19.83] | 1,323 |
| UK, Thames Valley | 2008–2015 | 243,968 | 951 | 38.98 [36.55, 41.53] | 99 | 4.06 [3.30, 4.94] | 274 | 11.23 [9.94, 12.64] | 546 | 22.38 [20.54, 24.34] | 919 |
| Belgium, Antwerp | 2008–2015 | 168,597 | 700 | 41.52 [38.51, 44.71] | 47 | 2.79 [2.05, 3.71] | 158 | 9.37 [7.97, 10.95] | 443 | 26.28 [23.89, 28.84] | 648 |
| Spain, Basque Country | 2008–2014 | 144,180 | 725 | 50.28 [46.70, 54.07] | 69 | 4.79 [3.72, 6.06] | 228 | 15.81 [13.83, 18.00] | 381 | 26.43 [23.84, 29.21] | 678 |
| France, Paris | 2008–2015 | 210,058 | 1,152 | 54.84 [51.73, 58.09] | 97 | 4.62 [3.75, 5.63] | 255 | 12.14 [9.36, 12.21] | 792 | 37.70 [35.13, 40.42] | 1,144 |
| Netherlands, North | 2008–2015 | 134,703 | 743 | 55.16 [51.27, 59.26] | 75 | 5.57 [4.38, 6.98] | 178 | 13.21 [11.35, 15.30] | 470 | 34.89 [31.81, 38.19] | 723 |
| France, Ile de la Reunion | 2008–2015 | 115,675 | 649 | 56.11 [51.88, 60.58] | 75 | 6.48 [5.10, 8.13] | 112 | 9.68 [7.97, 11.65] | 436 | 37.69 [34.24, 41.39] | 623 |
| Spain, Valencia Region | 2008–2015 | 391,848 | 2,365 | 60.36 [57.95, 62.83] | 86 | 2.19 [1.76, 2.71] | 420 | 10.72 [9.72, 11.79] | 1,522 | 38.84 [36.92, 40.84] | 2,028 |
| UK, Northern England | 2008–2015 | 265,556 | 1,640 | 61.76 [58.81, 64.81] | 125 | 4.71 [3.92, 5.61] | 420 | 15.82 [14.34, 17.40] | 1,037 | 39.05 [36.71, 41.50] | 1,582 |
| Italy, Tuscany | 2008–2015 | 236,384 | 1,472 | 62.27 [59.14, 65.53] | 84 | 3.55 [2.84, 4.40] | 259 | 10.96 [9.66, 12.38] | 1,075 | 45.48 [42.80, 48.27] | 1,418 |
| Norway | 2008–2012 | 310,634 | 1,939 | 62.42 [59.68, 65.25] | 159 | 5.12 [4.35, 5.98] | 341 | 10.98 [9.84, 12.21] | 1,180 | 37.99 [35.85, 40.21] | 1,680 |
| Croatia, Zagreb | 2008–2015 | 55,155 | 364 | 66.00 [59.41, 73.11] | 20 | 3.63 [2.22, 5.60] | 40 | 7.25 [5.18, 9.87] | 283 | 51.31 [45.52, 57.63] | 343 |
| Italy, Emilia Romagna | 2008–2015 | 317,980 | 2,064 | 64.91 [62.15, 67.76] | 114 | 3.59 [2.96, 4.31] | 431 | 13.55 [12.31, 14.90] | 1,432 | 45.03 [42.74, 47.42] | 1,977 |
| Ukraine | 2008–2015 | 249,743 | 1,649 | 66.03 [62.89, 69.28] | 141 | 5.65 [4.75, 6.66] | 294 | 11.77 [10.47, 13.20] | 1,123 | 44.97 [42.38, 47.67] | 1,558 |
| Austria, Styria | 2008–2012 | 51,569 | 347 | 67.29 [60.41, 74.73] | 32 | 6.21 [4.25, 8.76] | 68 | 13.19 [10.24, 16.71] | 205 | 39.75 [34.51, 45.57] | 305 |
| Wales | 2008–2015 | 279,314 | 1,892 | 67.74 [64.73, 70.85] | 125 | 4.48 [3.73, 5.33] | 485 | 17.36 [15.84, 18.98] | 1,146 | 41.03 [38.69, 43.47] | 1756 |
| France, Brittany | 2011–2015 | 179,180 | 1,529 | 85.33 [81.13, 89.70] | 75 | 4.19 [3.29, 5.25] | 244 | 13.62 [11.96, 15.44] | 1,168 | 65.19 [61.51, 69.02] | 1,487 |
| France, Auvergne | 2008–2012 | 68,218 | 622 | 91.18 [84.18, 98.60] | 44 | 6.45 [4.69, 8.66] | 70 | 10.26 [8.00, 13.00] | 496 | 72.71 [66.47, 79.37] | 610 |
| Switzerland, Vaud | 2008–2015 | 65,227 | 617 | 94.59 [917.05, 961.98] | 39 | 5.98 [4.25, 8.17] | 86 | 13.18 [10.55, 16.28] | 471 | 72.21 [65.86, 79.01] | 596 |
| Malta | 2008–2015 | 34,068 | 353 | 103.62 [93.14, 114.94] | 20 | 5.87 [2.82, 4.95] | 56 | 16.44 [13.53, 17.77] | 265 | 77.79 [71.18, 80.41] | 341 |
| Germany, Saxony‐Anhalt | 2008–2015 | 137,670 | 1,433 | 104.09 [98.80, 109.59] | 52 | 3.78 [4.11, 4.49] | 214 | 15.54 [11.87, 12.51] | 1,042 | 75.69 [71.20, 80.41] | 1,308 |
| Total | 2008–2015 | 4,576,641 | 26,115 | 57.06 [56.37, 57.76] | 1,968 | 4.30 [4.11, 4.49] | 5,579 | 12.19 [11.87, 12.51] | 16,965 | 37.07 [36.51, 37.63] | 24,532 |
2.1. Case exclusion
Minor anomalies as listed in the EUROCAT list of minor anomalies were excluded because they have lesser medical, functional, or cosmetic consequences for the child and their definitions and diagnosis vary considerably (EUROCAT, 2013). Cases with patent ductus arteriosus (PDA) associated with preterm birth only, were also excluded in line with the EUROCAT exclusion list (EUROCAT, 2013). Cases occurring in multiple pregnancies were excluded from the analysis because twins are known to be at increased risk of CHD, especially among monochorionic twins (Best & Rankin, 2015; Tang et al., 2006). Congenital anomalies due to maternal infections and teratogenic syndromes were excluded from the analysis due to a known under‐ascertainment of these conditions (Ardinger et al., 1988; Jones, 1986). Cases of CHD with amniotic band syndrome were also excluded as there is clinical evidence of a pathogenetic mechanism underlying the amniotic band (Cignini et al., 2012). Finally, we excluded cases of CHD and a chromosomal anomaly and/or genetic syndrome as chromosomal anomalies are known to increase the risk of CHD (Richards & Garg, 2010). All other CHD cases were included and coded as nonsyndromic where these CHD occurred without the presence of any other noncardiac major congenital anomaly.
Total PR of nonsyndromic CHD was defined as: the total number of CHD cases whether ending in fetal deaths (pregnancy losses ≥20 weeks), TOPFAs or live births per 10,000 total births (live births and stillbirths). Live birth prevalence was defined as: the number of live births with CHD per 10,000 live births. Ninety‐five percent confidence intervals (CIs) were derived from the binomial distribution.
Live birth prevalence is essential when considering service utilization. Different intervention programs can use live birth prevalence to better understand changes in the population and for resource allocation.
We plotted time trends for the period 2008–2015 for both total and live birth PRs of all nonsyndromic CHDs (from here on referred to as total and live birth prevalence of CHD) and for three CHD severity groupings based on the EUROCAT classification of the severity (EUROCAT Central Registry University of Ulster, 2009) as follows:
Severity group I—Very severe (single ventricle, hypoplastic left heart syndrome, hypoplastic right heart syndrome, Ebstein anomaly, tricuspid atresia); accounted for approximately 8% of all cases.
Severity group II—Severe (pulmonary valve atresia, common arterial truncus, AVSD, aortic valve atresia/stenosis, transposition of great vessels, tetralogy of Fallot, total anomalous pulmonary venous return, coarctation of aorta); accounted for approximately 21% of cases excluding cases with coexisting Severity I CHD anomalies.
Severity group III—Less severe (ventricular septal defect [VSD], atrial septal defect [ASD], pulmonary valve stenosis); accounted for approximately 65% excluding cases with coexisting Severity I or Severity II CHD anomalies. Cases with different CHDs occurring together were assigned according to the subtype of greatest severity. For example, a case with coarctation of aorta and VSD was included in the Severity II group.Altogether, these groups accounted for approximately 94% of all cases of CHDs (Table 1). The other 6% included those with PDA in term infants and a few other CHD subtypes which are not included in any of the above severity categories such as double outlet right ventricle, mitral valve anomalies, aortic atresia/interrupted aortic arch.
We plotted time trends for the period 2008–2015 for both total and live birth PRs of all nonsyndromic CHDs and for the three CHD severity groups. As the data from the different registries were for different time periods, a simple analysis of CHD prevalence over time might introduce confounding. Thus, a Poisson multilevel regression approach was used for all nonsyndromic CHDs and for the three CHD severity groups. The total number of CHD births per year were nested within registry and modeled by random‐effects models (Poisson regression) with a random intercept, an offset equal to the log of the expected number of CHD births, and time (year) as a continuous predictor. The random component of the intercept was used to take into account heterogeneity that may exist across the registry.
All analyses were performed using Stata software (version 14; StataCorp, College Station, TX) for both descriptive and multilevel analysis.
3. RESULTS
A total of 36,695 cases of CHD were reported to the 25 participating EUROCAT registries between 2008 and 2015. The maximum age of diagnosis in our analysis is up to 1 year for 13 (52%) of the registries, up to 1 month for 16% and more than 1 year for 28% of registries according to the coding of the collected variable on timing of CA discovery (EUROCAT, 2013). There were 7,504 cases associated with a chromosomal anomaly and/or genetic syndromes and/or noncardiac malformations that were excluded and 26,115 were cases of nonsyndromic CHD (Figure 1). Specifically, 1,968 cases were classified as Severity I group, 5,579 cases as Severity II group, and finally 16,965 cases as Severity III group (Table 1).
FIGURE 1.

Derivation of the study sample
Figure 2 shows the total prevalence of CHDs over time. There was no evidence of a trend in total prevalence for all CHDs combined. The total prevalence of CHD was 57.1 per 10,000 births during the study period. Table 2 shows the results of the random‐effects Poisson regression models in the total prevalence of CHDs. Estimates showed that the total prevalence of CHDs (for all CHDs combined) remained stable during 2008–2015 (annual PR 1.00, 95% CI 0.99, 1.00).
FIGURE 2.

Time trend in total prevalence per 10,000 live and stillbirths notified to 25 EUROCAT registries, 2008–2015 of: (a) All nonsyndromic CHDs; (b) Severity group I; (c) Severity group II; (d) Severity group III
TABLE 2.
Random‐effects Poisson regression of the trends in total and live birth prevalence of CHDs (all defects combined) in 25 Eurocat registries, 2008–2015
| Total prevalence | Live birth prevalence | |||||
|---|---|---|---|---|---|---|
| Annual PR a | 95% CI | Annual PR a | 95% CI | |||
| Overall CHD | 1.00 | 0.99 | 1.00 | 1.00 | 0.99 | 1.00 |
| Severity I | 1.00 | 0.98 | 1.02 | 1.00 | 0.98 | 1.02 |
| Severity II | 0.99 | 0.98 | 1.00 | 0.99 | 0.98 | 1.00 |
| Severity III | 1.00 | 0.99 | 1.01 | 1.00 | 0.99 | 1.01 |
Annual trend in PR over the specific time period (2008–2015).
For the most severe group (Severity group I), the total prevalence of CHD was relatively stable at 4.3 per 10,000 (Figure 2 and Table 1). Additionally, there was no evidence of a trend in total prevalence for Severity group II with a total prevalence of 12.2 per 10,000 (Figure 2 and Table 1) (annual PR 0.99, 95% CI 0.98, 1.00). Similarly, for Severity group III (Figure 2 and Table 1), the most prevalent group, there was no evidence of a trend in total prevalence, with a total prevalence of 37.1 per 10,000 (annual PR 1.00, 95% CI 0.99, 1.01).
Figure 3 and Table 2 show the time trends for live birth prevalence for all CHDs combined and for each CHD severity group between 2008 and 2015. The trends in live birth prevalence were similar to those for the total prevalence of CHDs. Figure 4 presents the time trends in total prevalence of all CHDs separately for the 25 participating registries. Collapsing the registries of a nation the trend in total prevalence reached statistical significance for Norway, England/Wales, Italy, and Croatia (Figure 5 and Table 3).
FIGURE 3.

Time trend in live birth prevalence per 10,000 live births notified to 25 EUROCAT registries, 2008–2015 of (a) all nonsyndromic CHDs, (b) Severity group I, (c) Severity group II, and (d) Severity group III
FIGURE 4.

Time trend in total prevalence per 10,000 live and stillbirths of all nonsyndromic CHDs for the 25 registries, 2008–2015
FIGURE 5.
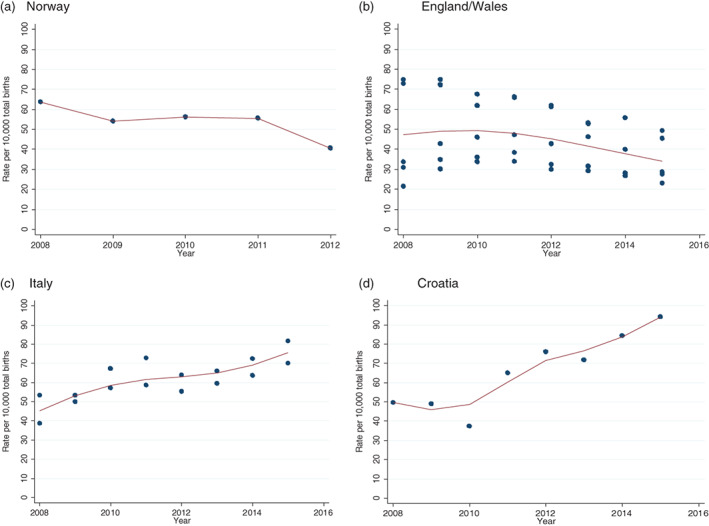
Time trend in total Prevalence per 10,000 live and stillbirths of all nonsyndromic CHDs in Norway register, England/Wales, Italy, and Croatia, 2008–2015
TABLE 3.
Random‐effects Poisson regression of the trends in total and live birth prevalence of CHDs (all defects combined) in Norway, England/Wales, and Italy EUROCAT registers, 2008–2015
| Countries | Total prevalence | Live birth prevalence | ||||
|---|---|---|---|---|---|---|
| Annual PR a | 95% CI | Annual PR a | 95% CI | |||
| Norway | 0.92 | 0.85 | 1.00 | 0.92 | 0.85 | 0.99 |
| England and Wales registers (total number: 5) | 0.95 | 0.93 | 0.97 | 0.95 | 0.93 | 0.97 |
| Italy registers (total number: 2) | 1.05 | 1.03 | 1.08 | 1.05 | 1.03 | 1.08 |
| Croatia | 1.11 | 1.07 | 1.16 | 1.12 | 1.07 | 1.16 |
Annual trend in PR over the specific time period (2008–2015).
For Norway (national registry), the overall and Severity III prevalence (per 10,000) of CHDs decreased from 2008 (annual PR 0.92, 95% CI 0.85, 1.00). Similarly, for England/Wales (five registries), the overall and Severity III prevalence of CHDs decreased from 2010 (annual PR 0.95, 95% CI, 0.93, 0.97).
For Italy (two registries), the overall and Severity III prevalence of CHDs increased from 2008 (annual PR 1.05, 95% CI 1.03, 1.08), while the overall and Severity III prevalence of CHDs increased from 2009 (annual PR 1.11, 95% CI, 1.07, 1.16) for Croatia (one registry). Similar results are also presented in the live birth prevalence of CHDs (Table 3).
4. DISCUSSION
This study examined trends in prevalence of nonsyndromic CHD in Europe overall and by CHD severity group between the years 2008 and 2015 and investigated whether the rates have continued to decline as had been reported previously (Rankin et al., 2005). Based on data for 26,115 cases of nonsyndromic CHD from 25 European population‐based registries, we found that both total and live birth prevalence remained stable overall and across the three CHD severity groups.
Khoshnood et al. (2013) using EUROCAT data for the period 1990–2007, found that the direction of trends in total prevalence of CHD cases not associated with a chromosomal anomaly changed over time with the total prevalence having increased prior to 2004 and reduced thereafter. However, the Khoshnood study found no trend in total prevalence of the most severe group (Severity group I), while the prevalence of Severity group II increased until 2000 and reduced thereafter. Trends for Severity group III paralleled those for all CHDs combined. The pattern of time trends reported in the Khoshnood study (Khoshnood et al., 2013) was similar to a population‐based study in Norway with an increase from 1990 to 2004 and a decrease thereafter (Van der Linde et al., 2011). However, based on our analysis, this decreasing trend does not seem to have continued after 2008, except for Norway. Additionally, both Khoshnood and the Norwegian studies (Khoshnood et al., 2013; Leirgul et al., 2014) applied substantially similar exclusion criteria, however, differences in classification of the severity might potentially confound comparisons.
Some variation was found in the reported CHD total prevalence and direction of trends between different populations (Rosano et al., 2000). There were considerable differences in trends in total and live birth prevalence by registry in our study. The total and live birth prevalence remained stable for most registries apart from those in Norway, England/Wales, Italy, and Croatia. Specifically, we found a significant decreasing overall and Severity III group prevalence of nonsyndromic CHD for registers from Norway and England/Wales, whereas the prevalence significantly increased for the Italy and Croatia registries for all CHDs and for Severity group III.
The decreasing trends in Norway and UK are most likely because they stopped reporting small muscular VSDs and followed the EUROCAT recommendation from 2007 of only including ASD if the defect was open 6 months after birth. There are many preterm and term born babies that have a neonatal echo with a persistent foramen ovale coded as ASD without any ASD diagnosis later in infancy or childhood (Garne et al., 2012).
Another possible explanation that could contribute to the decreasing trend for the live birth prevalence of nonsyndromic CHD for the Norwegian and UK registries, might be the better access to specialized perinatal care for women whose pregnancies are affected with CHD and higher prenatal detection rates that might lead to an increase in termination of pregnancies complicated by severe CHD over time and resulting decrease in live birth prevalence.
It is well known that risk factors such as maternal diabetes and rubella, advanced maternal age and maternal smoking during pregnancy are associated with the occurrence of CHD (Correa, Levis, Tinker, & Cragan, 2015; Leirgul et al., 2014; Reefhuis et al., 2009). Therefore, alternative explanations for this decline in prevalence might include the reduction in these factors and better management of women with chronic health conditions such as diabetes (Correa et al., 2015). For example, the Scandinavian countries and the UK have greater smoking cessation rates than the rest of Europe (Pesce et al., 2019). In the past decade, most countries have experienced a decline in daily smoking rates, however, the rate of smoking in Norway has almost halved while the percent decline in daily smoking rates between 2002 and 2012 was 27% for UK (Connelly, 2015). Additionally, in Norway there was a period (around 1990–2000) with a significant increase in the proportion of heavy singleton births (Grundt, Eide, Brantsaeter, Haugen, & Markestad, 2017). There has been speculation around what might have caused this rise in heavy singleton births, and one possible explanation is that it coincided with the increase in consuming sugar‐sweetened soft drinks during pregnancy (Carlsen et al., 2020). However, this consumption of soft drinks later declined. Interestingly, Dale et al. evaluated the intake of sucrose‐sweetened soft beverages during pregnancy and risk of CHD, and concluded that this can increase the risk (Dale et al., 2019). Thus, in Norway, the decrease during these years may be related to changes in diet.
The increase of cases of CHD from 2008 onwards is perhaps explained by improvements in case ascertainment. In Tuscany (Italy), an increasing trend for coarctation of aorta has been observed in the 2008–2017 period. This increase may be due to the inclusion of the Paediatric Surgery Unit of the Heart Hospital in Massa as a data source of the registry since 2013 (Kinsner‐Ovaskainen, Morris, Garne, Loane, & Lanzoni, 2020). This change improved data quality and increased the number of reported cases, in particular of cardiac cases.
Improved case detection using echocardiography techniques has increased the prevalence of mild lesions. Specifically, the use of 2D echocardiography examination of patients has resulted in the detection of lesions such as small VSD, ASD, and PDA that may have remained unnoticed (Bhardwaj et al., 2015).
The “true” prevalence of a condition depends on the age distribution of the sample population. For example, ASDs and VSDs present at different times and some undergo spontaneous closure, while many less severe CHDs are diagnosed later in life (American Heart Association, 2021; Liu et al., 2019). Also, the average age at diagnosis varies according to the intensity of prenatal and early neonatal screening and the follow‐up that takes place in each region (Dolk et al., 2011).
In our dataset, the maximum age at diagnosis varies according to the registry policies of registration (some registries include anomalies diagnosed up to 1 week, up to 1 year of after 1 year). This difference in methodology contributes to the difficulty in comparing prevalence between registries, especially in the less severe group of CHDs that can be diagnosed several months after birth and therefore may not reported in all registries. This is consistent with the study by Hoffman et al. who reviewed 62 studies and found large variations in the age of diagnosis (EUROCAT Central Registry University of Ulster, 2009).
The main strength of this study is the use of high‐quality population‐based data derived from an established network of European congenital anomaly registries where both multisource case ascertainment and accurate diagnoses are achieved. EUROCAT registries use similar methodology which enables comparisons between regions to be made. A further strength is that we used a multilevel approach method for the analysis of prevalence that takes into account the effects of variables at different levels of analysis in addition to the more classically used individual‐level ones.
Our study also had some limitations. First, the results from one regional EUROCAT registry might not represent the situation for the entire country as studies have shown that several risk factors such as socioeconomic, air‐pollution, and environmental exposures might influence the incidence of CHD in some areas of the countries (Cignini et al., 2012; Zhang et al., 2016). Thus, some variations between European countries might be under or overestimated. Second, some caution should be considered in interpreting the prevalence outcome of the trend analysis, as we used 25 registries in comparison with the Khoshnood et al. 2013 study which included 29 registries.
We found that the decreasing trend in the overall prevalence of CHD reported by previous studies (Khoshnood et al., 2013; Leirgul et al., 2014) has not continued between the years 2008 and 2015 for all registries combined. However, we report a significant overall decreasing prevalence for Norway, England/Wales, and an increasing prevalence for Italy and Croatia which is probably attributable to advances in CHD ascertainment, rather than a true increase in the prevalence of CHD in the population.
Differences in trends in the CHD prevalence (especially in severe categories) of different populations confirms the importance of regular monitoring of temporal trends in congenital anomaly prevalence, including CHDs, in Europe. This could help identify any major increases in prevalence and differences between countries/regions and identify modifiable risk factors such as maternal age and obesity, maternal exposure to environmental factors, socioeconomic factors that contribute to an increase/decrease in the prevalence of CHD so that this information can be used to apply relevant public health measures (Cignini et al., 2012; Egbe, Uppu, Lee, Ho, & Srivastava, 2014). Thus, future epidemiological studies are needed in order to take into account possible confounding factors and to establish the true CHD burden while due to the rarity of specific CHD subtypes, larger studies with sufficient power are also important for a more in‐depth analysis of CHD phenotypic subgroups.
AUTHOR CONTRIBUTIONS
Chrysovalanto Mamasoula, Judith Rankin, and Lindsay Pennington conceptualized and designed the study and contributed to drafting the manuscript. Chrysovalanto Mamasoula conducted the analysis and drafted the initial manuscript. All authors contributed to data interpretation, reviewed the manuscript, and approved the final version for submission.
CONFLICT OF INTEREST
The authors have no conflicts of interest relevant to this article to disclose.
ACKNOWLEDGMENTS
We thank Dr Thomas Chadwick and Dr Theophile Bigirumurame for providing guidance in data analysis and the review of the manuscript.
Mamasoula, C. , Addor, M.‐C. , Carbonell, C. C. , Dias, C. M. , Echevarría‐González‐de‐Garibay, L.‐J. , Gatt, M. , Khoshnood, B. , Klungsoyr, K. , Randall, K. , Stoianova, S. , Haeusler, M. , Nelen, V. , Neville, A. J. , Perthus, I. , Pierini, A. , Bertaut‐Nativel, B. , Rissmann, A. , Rouget, F. , Schaub, B. , … Rankin, J. (2022). Prevalence of congenital heart defects in Europe, 2008–2015: A registry‐based study. Birth Defects Research, 114(20), 1404–1416. 10.1002/bdr2.2117
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- American Heart Association . (2021). About congenital heart defects. Retrieved from https://www.heart.org/en/health-topics/congenital-heart-defects/about-congenital-heart-defects.
- Ardinger, H. H. , Atkin, J. F. , Blackston, R. D. , Elsas, L. J. , Clarren, S. K. , Livingstone, S. , … Reynolds, J. F. (1988). Verification of the fetal valproate syndrome phenotype. American Journal of Medical Genetics, 29(1), 171–185. [DOI] [PubMed] [Google Scholar]
- Best, K. E. , & Rankin, J. (2015). Increased risk of congenital heart disease in twins in the North of England between 1998 and 2010. Heart, 101(22), 1807–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhardwaj, R. , Rai, S. K. , Yadar, A. K. , Lakhotia, S. , Agrawal, D. , Kumar, A. , & Mohapatra, B. (2015). Epidemiology of congenital heart disease in India. Congenital Heart Disease, 10(5), 437–446. [DOI] [PubMed] [Google Scholar]
- Carlsen, E. Ø. , Magnus, M. C. , Omsland, T. K. , Magnus, P. M. , Håberg, S. E. , & Wilcox, A. J. (2020). Stumped by the hump: The curious rise and fall of Norwegian birthweights, 1991–2007. Epidemiology, 31(4), 587–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cignini, P. , Giorlandino, C. , Padula, F. , Dugo, N. , Cafà, E. V. , & Spata, A. (2012). Epidemiology and risk factors of amniotic band syndrome, or ADAM sequence. Journal of Prenatal Medicine, 6(4), 5–63. [PMC free article] [PubMed] [Google Scholar]
- Connelly, D. (2015). A decade of smoking cessation in Europe. The Pharmaceutical Journal, 294(7848). 10.1211/PJ.2015.20067801 [DOI] [Google Scholar]
- Correa, A. , Levis, D. M. , Tinker, S. C. , & Cragan, J. D. (2015). Maternal cigarette smoking and congenital heart defects. The Journal of Pediatrics, 166(4), 801–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale, M. T. G. , Magnus, P. , Leirgul, E. , Holmstrøm, H. , Gjessing, H. K. , Brodwall, K. , … Øyen, N. (2019). Intake of sucrose‐sweetened soft beverages during pregnancy and risk of congenital heart defects (CHD) in offspring: A Norwegian pregnancy cohort study. European Journal of Epidemiology, 34(4), 383–396. [DOI] [PubMed] [Google Scholar]
- Dolk, H. , Loane, M. , Garne, E. , & European Surveillance of Congenital Anomalies (EUROCAT) Working Group . (2011). Congenital heart defects in Europe: prevalence and perinatal mortality, 2000 to 2005. Circulation, 123(8), 841–849. [DOI] [PubMed] [Google Scholar]
- Egbe, A. , Uppu, S. , Lee, S. , Ho, D. , & Srivastava, S. (2014). Changing prevalence of severe congenital heart disease: A population‐based study. Pediatric Cardiology, 35(7), 1232–1238. [DOI] [PubMed] [Google Scholar]
- EUROCAT (2013). Chapter 3.2: Minor anomalies for exclusion (version 14.10.14). In EUROCAT Guide 1.4: Instruction for the registration of congenital anomalies (Last update version December 20, 2016). Newtownabbey, UK: EUROCAT Central Registry, University of Ulster. [Google Scholar]
- EUROCAT Central Registry University of Ulster . (2009). EUROCAT special report: Congenital heart defects in Europe, 2000–2005. Retrieved from https://eu-rd-platform.jrc.ec.europa.eu/sites/default/files/eurocat-pub-docs/Special-Report-CHD.pdf.
- Garne, E. , Olsen, M. S. , Johnsen, S. P. , Hjortdal, V. , Andersen, H. Ø. , & Nissen, H. (2012). How do we define congenital heart defects for scientific studies? Congenital Heart Disease, 7(1), 46–49. [DOI] [PubMed] [Google Scholar]
- Grundt, J. H. , Eide, G. E. , Brantsaeter, A. L. , Haugen, M. , & Markestad, T. (2017). Is consumption of sugar‐sweetened soft drinks during pregnancy associated with birth weight? Maternal & Child Nutrition, 13(4), e12405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, K. L. (1986). Fetal alcohol syndrome. American Academy of Pediatrics, 8(4), 122–127. [DOI] [PubMed] [Google Scholar]
- Khoshnood, B. , Greenlees, R. , Loane, M. , & Dolk, H. (2011). Paper 2: EUROCAT public health indicators for congenital anomalies in Europe. Birth Defects Research Part A: Clinical and Molecular Teratology, 91(Suppl 1), S16–S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoshnood, B. , Loane, M. , Garne, E. , Addor, M. C. , Arriola, L. , Bakker, M. , … Dolk, H. (2013). Recent decrease in the prevalence of congenital heart defects in Europe. The Journal of Pediatrics, 162(1), 108–13.e2. [DOI] [PubMed] [Google Scholar]
- Kinsner‐Ovaskainen, A. , Morris, J. , Garne, E. , Loane, M. , & Lanzoni, M. (2020). European monitoring of congenital anomalies: JRC‐EUROCAT report on statistical monitoring of congenital anomalies (2008–2017). Retrieved from https://publications.jrc.ec.europa.eu/repository/bitstream/JRC120236/eurocat_statmon_report_2020_final_online.pdf.
- Leirgul, E. , Fomina, T. , Brodwall, K. , Greve, G. , Holmstrøm, H. , Vollset, S. E. , … Øyen, N. (2014). Birth prevalence of congenital heart defects in Norway 1994–2009: A nationwide study. American Heart Journal, 168(6), 956–964. [DOI] [PubMed] [Google Scholar]
- Liu, Y. , Chen, S. , Zühlke, L. , Black, G. C. , Choy, M. K. , Li, N. , & Keavney, B. D. (2019). Global birth prevalence of congenital heart defects 1970–2017: Updated systematic review and meta‐analysis of 260 studies. International Journal of Epidemiology, 48(2), 455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesce, G. , Marcon, A. , Calciano, L. , Perret, J. L. , Abramson, M. J. , Bono, R. , … Ageing Lungs in European Cohorts (ALEC) Study . (2019). Time and age trends in smoking cessation in Europe. PLoS One, 14(2), e0211976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rankin, J. , Pattenden, S. , Abramsky, L. , Boyd, P. , Jordan, H. , Stone, D. , … Dolk, H. (2005). Prevalence of congenital anomalies in five British regions, 1991–99. Archives of Disease in Childhood. Fetal and Neonatal Edition, 90(5), F374–F379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reefhuis, J. , Honein, M. A. , Schieve, L. A. , Correa, A. , Hobbs, C. A. , & Rasmussen, S. A. (2009). Assisted reproductive technology and major structural birth defects in the United States. Human Reproduction, 24, 360–366. [DOI] [PubMed] [Google Scholar]
- Richards, A. A. , & Garg, V. (2010). Genetics of congenital heart disease. Current Cardiology Reviews, 6(2), 91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosano, L. , Botto, B. , Botting, P. , & Mastroiacovo, P. (2000). Infant mortality and congenital anomalies from 1950 to 1994: An international perspective. Journal of Epidemiology and Community Health, 54(9), 660–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang, Y. , Ma, C. X. , Cui, W. , Chang, V. , Ariet, M. , Morse, S. , … Roth, J. (2006). The risk of birth defects in multiple births: A population‐based study. Maternal and Child Health Journal, 2006(10), 75–81. [DOI] [PubMed] [Google Scholar]
- Van der Linde, D. , Konings, E. E. , Slager, M. A. , Witsenburg, M. , Helbing, W. , Takkenberg, J. M. , & Roos‐Hesselink, J. W. (2011). Birth prevalence of congenital heart disease worldwide: A systematic review and meta‐analysis. Journal of the American College of Cardiology, 58, 2241–2247. [DOI] [PubMed] [Google Scholar]
- Zhang, B. , Liang, S. , Zhao, J. , Qian, Z. , Bassig, B. A. , Yang, R. , … Yang, S. (2016). Maternal exposure to air pollutant PM2.5 and PM10 during pregnancy and risk of congenital heart defects. Journal of Exposure Science & Environmental Epidemiology, 26(4), 422–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


