Figure 10.
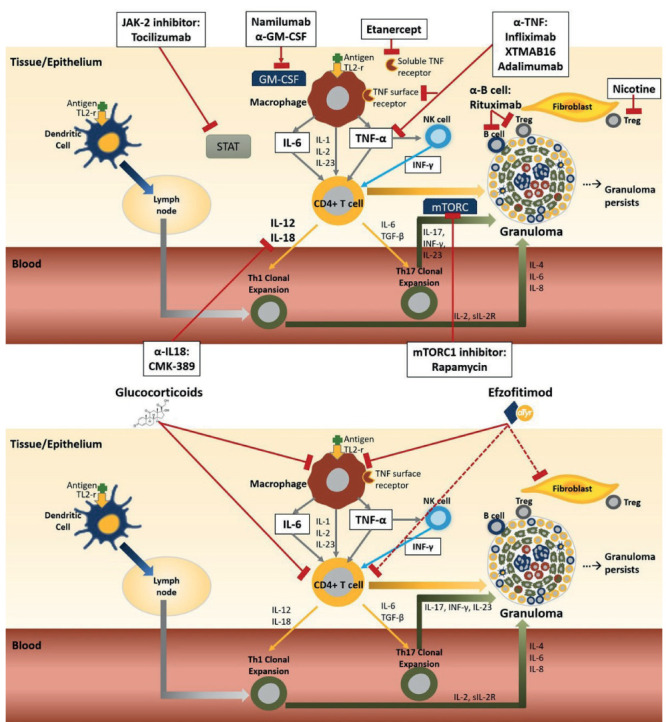
Inhaled antigen comes into contact with cells at the epithelial layer. Activation of both macrophages and dendritic cells occurs through the toll-like receptor-2 (TLR-2). The dendritic cells transport the antigen across the epithelium to the lymph node, where it is processed leading to differentiation and clonal expression of T helper cells (Th1 and Th17). The antigen also stimulates macrophages on the surface of the epithelium and leads to the release of tumor necrosis factor alpha (TNF-α) and several other pro-inflammatory cytokines including IL-1, IL-2. IL-6 and IL-23. TNF-α crosses epithelial layer where it activates tissue macrophages and natural killer (NK) cells. Activated NK releases interferon gamma (IFN-γ) which act in concert with TNF-α to upregulate the inflammatory response by attracting CD4+ cells, monocytes and Tregs to the site of inflammation. TNF-α along with the other pro-inflammatory cytokines also activates CD4+ cells and causes them to further differentiate down the Th1 and Th17 effector pathways. The activated macrophages and clonal Th1/Th17 cells form the core of the granuloma. Other cells in the granuloma include T regulatory cells (Treg) and B cells. The Th17 pathway has been more implicated in chronic disease as has impaired Treg cell function and persistent accumulation of serum amyloid A within the granuloma. Biologic therapies for sarcoidosis specifically targeted for one or two cytokines or cell types (Figure 10A). Targets of therapy for two broad based anti-inflammatory therapies for sarcoidosis: glucocorticoids and efzofitimod (Figure 10B). Dashed lines indicate potential targets. Adapted from Obi et al 32.
