Abstract
Societal factors associated with ocular surface diseases were mapped using a framework to characterize the relationship between the individual, their health and environment. The impact of the COVID-19 pandemic and mitigating factors on ocular surface diseases were considered in a systematic review. Age and sex effects were generally well-characterized for inflammatory, infectious, autoimmune and trauma-related conditions. Sex and gender, through biological, socio-economic, and cultural factors impact the prevalence and severity of disease, access to, and use of, care. Genetic factors, race, smoking and co-morbidities are generally well characterized, with interdependencies with geographical, employment and socioeconomic factors. Living and working conditions include employment, education, water and sanitation, poverty and socioeconomic class. Employment type and hobbies are associated with eye trauma and burns. Regional, global socio-economic, cultural and environmental conditions, include remoteness, geography, seasonality, availability of and access to services. Violence associated with war, acid attacks and domestic violence are associated with traumatic injuries. The impacts of conflict, pandemic and climate are exacerbated by decreased food security, access to health services and workers. Digital technology can impact diseases through physical and mental health effects and access to health information and services. The COVID-19 pandemic and related mitigating strategies are mostly associated with an increased risk of developing new or worsening existing ocular surface diseases. Societal factors impact the type and severity of ocular surface diseases, although there is considerable interdependence between factors. The overlay of the digital environment, natural disasters, conflict and the pandemic have modified access to services in some regions.
Keywords: Dry eye, Infection, Inflammation, Trauma, Autoimmune disease, Biology, Lifestyle, Socioeconomic factors, Employment, Systematic review
1. Introduction
1.1. Approach
This report is part of the Tear Film & Ocular Surface Society (TFOS) Workshop, entitled ‘A Lifestyle Epidemic: Ocular Surface Disease,’ which was undertaken to establish the direct and indirect impacts that everyday lifestyle choices and challenges have on ocular surface health. It examines societal challenges in ocular surface diseases using an adaptation of a framework used to map the relationship between the individual, their environment and their health [1]. This approach was designed to enable interventions to be addressed at a health policy level and consequently it reflects the interplay and dependencies between the different factors. The model also recognises that certain factors can be considered to fit within one or more of the levels identified. The most recent iteration of this model considers the impact of the digital world directly and indirectly on human health [2].
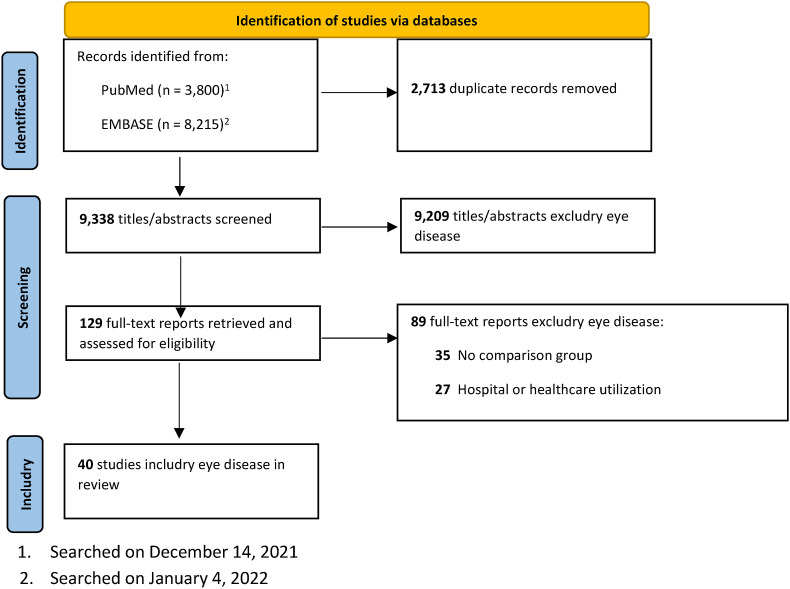
The direct impact of certain individual lifestyle factors in ocular surface diseases, including nutrition [3], cosmetics [4], elective medicine [5], lifestyle challenges [6], environment factors [7] and digital device use [8], is explored in detail in the respective Reports from the TFOS Lifestyle Workshop. The Societal Challenges Report will predominantly focus on how those factors contribute to societal norms that in turn influence presentation, outcome and management of ocular surface diseases and will refer to the relevant sub-committee reports for their direct effects. For example, the Societal Challenges Report will explore the impact of the digital world on access to education of practitioners and patients, telehealth or access to services, rather than the impact of digital devices per se on the ocular surface; or the effect of climate change on determinants such as clean water or access to services, rather than the effect of climate change on the ocular surface. Each section within this report will cross reference the relevant TFOS Lifestyle Reports to minimise overlap. As for the other TFOS Lifestyle Reports, evidence is summarised in a narrative style review that, wherever possible, refers to outcomes from high-quality systematic review (Level I) evidence. The Evidence Quality Subcommittee provided a comprehensive database of appraised Level 1 evidence judged to be of potential relevance, which was factored into the writing of the report [9]. A key issue given the timing of this report was the impact of COVID-19 on the ocular surface. A systematic review to summarize the impact of the COVID-19 pandemic on the frequency and severity of ocular surface disease in both the general population and amongst those who had COVID-19, was conducted and is included in this report.
1.2. Scope
For this Workshop, the ‘Ocular Surface’ is defined as the cornea, limbus, conjunctiva, eyelids and eyelashes, lacrimal apparatus and tear film, along with their associated glands and muscular, vascular, lymphatic and neural support. ‘Ocular Surface Disease’ includes established diseases affecting any of the listed structures, as well as etiologically-related perturbations and responses associated with these diseases.
Ocular surface diseases can be acute or chronic conditions that may require long term management. For this report, conditions are considered from an etiological perspective and will broadly include trauma, infection, inflammation, allergy, neoplasia and hereditary/congenital conditions. Societal factors as described in Fig. 1 will be mapped to these etiological classifications, where possible.
Fig. 1.
Framework used in this report (modified from Rice and Sara (2019) [2]).
2. Biology and genetic factors
2.1. Age
Age-related progressive decline of physiological function affects a broad range of organs, including the eye. The degradative effects of aging may contribute to multiple ocular surface diseases.
Dry eye disease (dry eye disease) is one of the major age-related diseases of the ocular surface. Increasing age is a fairly robust risk factor for dry eye disease in population-based cross-sectional studies [[10], [11], [12], [13], [14], [15]], although unexpectedly high rates of disease have been reported in several studies in young adults [[16], [17], [18]]. In a large study of health care records from the United States of America (USA), older adults were confirmed to be at higher risk and there was evidence of an increase in both incidence and prevalence of dry eye disease over time [19]. Four systematic reviews and meta-analyses in a Chinese population, Japanese population, and visual display terminal workers have also supported an increase in dry eye prevalence with age [[20], [21], [22], [23]]. Conversely, there was no significant association between dry eye disease and age in one systematic review with meta-analysis in Africa, although non-population-based studies were included in this analysis [24].
There is some evidence to suggest that the age-related association with dry eye disease is not linear and high rates of dry eye disease have been reported in children and young adults [15,19,[25], [26], [27], [28], [29], [30], [31], [32], [33], [34]], suggesting the relevance of other non-age-related risk factors, including sex, genetics and exogenous variables [31,35].
The unexpectedly high rate of dry eye disease in children and young adults could be partially explained by societal or behavioural factors and lifestyle activities linked to young age. Contact lens use and high screen time were two significant risk factors among youth [15,17,[30], [31], [32], [33]]. Poor sleep quality [33,34], allergies [25], arthritis [17], smoking [28], use of oral contraceptives [25,33], antidepressants, and anti-allergy medications [33], ocular surgery [33], windy conditions, very low humidity, and air-conditioning [25] have also been associated with dry eye disease in youth. Furthermore, the younger age group (<18 years) had the highest risk of corneal surface damage in aqueous-deficient dry eye [29]. These findings suggest that patients who have dry eye symptoms warrant early evaluation and timely intervention regardless of their age.
Age is also an established risk factor for meibomian gland dysfunction [36,37]. The consensus that the prevalence of meibomian gland dysfunction increases with age is supported by recent population-based cross-sectional studies and a multicentre hospital-based study [11,38,39]. A recent systematic review with meta-analysis concluded that older people are at increased risk of developing meibomian gland dysfunction [40]. Demodex blepharitis may also increase with age as Demodex infestation on the ocular surface is more prevalent in older individuals [41].
Meibomian gland acinar epithelial cell atrophy, resulting in decreased lipid expression and altered meibum composition with changes in non-polar and polar lipid profiles, may underpin the age-related effect [36,42,43]. Histological analysis of aged human meibomian glands revealed several morphological alterations, including cystic dilatation of acini and/or ducts, atrophy of acini, thickening of the acini basement membrane, granulation tissue, and lipogranulomatous inflammation [44]. Nevertheless, the clinical significance of such apparent changes and whether they result directly from aging or whether they are secondary to other age-related biological effects, including the changes in the levels of sex hormones and/or age-related co-morbidities are yet to be determined.
The relationship between meibomian gland dysfunction and age was not observed in African and some Asian populations [45,46] This may be due to a more limited age distribution in those study populations compared with others [45,47].
Conjunctivochalasis is characterised by loose, redundant, non-edematous conjunctival folds, typically in the inferior bulbar conjunctiva interposed between the globe and the lower eyelid [48,49] Both the prevalence and severity of conjunctivochalasis increase with age [48,[50], [51], [52], [53]].
Pinguecula and pterygium are common ocular surface diseases affecting the bulbar conjunctiva. There is robust evidence in the literature demonstrating the effect of long-term exposure to ultraviolet light from the sun on pinguecula and pterygium [[54], [55], [56], [57]]. Four systematic reviews and meta-analyses have shown a significant positive association between age and the prevalence of pterygium [[55], [56], [57], [58]]. Two recent population-based, cross-sectional studies from China and Russia [59,60] and one population-based, cohort study from Korea [61], correspondingly found that older age was associated with higher risk of pterygium. A large population-based, cross-sectional study from China revealed that age is an independent risk factor for pinguecula [54].
The effect of age on corneal infection is confounded by predisposing factors for the disease, demographic factors, systemic disease and social, environmental and cultural factors and by study design [62]. Older age was an independent risk factor for non-viral infectious keratitis in a well conducted case control study in Uganda [63] and there were similar findings in a large multicentre cross sectional case control study in China [64]. Older age is a risk factor for a more severe disease outcome [65], infectious corneal blindness [64], hospitalisation and surgical interventions [66].
Four systematic reviews and one meta-analysis have established that age is the most relevant independent risk factor for herpes zoster, especially in those above 50 years of age [[67], [68], [69], [70]], which may increase the likelihood of developing herpes zoster ophthalmicus [71]. The prevalence of herpes zoster ophthalmicus among those with herpes zoster varied from 10% to 15% [68,72]. Various ocular surface diseases, including conjunctivitis, keratitis, and anterior uveitis have been reported, ranging from 30% to 78% of herpes zoster ophthalmicus cases [68]. Older age is also associated with severe visual loss secondary to herpes zoster ophthalmicus [73].
Most allergic conjunctivitis, including seasonal allergic conjunctivitis, perennial allergic conjunctivitis, vernal keratoconjunctivitis, atopic keratoconjunctivitis, and giant papillary conjunctivitis, commonly presents in the first three decades of life and tend to diminish with age, although some of these diseases may persist or occur de novo in older adults [74]. However, there is limited evidence regarding the prevalence, clinical manifestations, natural history, and management of allergic conjunctivitis in the elderly [[74], [75], [76]]. Most evidence suggests that perennial allergic conjunctivitis, atopic keratoconjunctivitis and contact blepharoconjunctivitis are more freqently observed in middle-aged or older adults and are possibly associated with the use of topical ocular medications, particularly anti-glaucoma drugs, and an impaired lacrimal function in the aged population. Changes in climate, diet, living conditions, lifestyles, air pollutants, comorbidities, and concomitant medications may impact the immune system and increase exposure to the diversity of allergens, causing changed sensitization in elderly individuals [74,[76], [77], [78], [79], [80]].
Ocular surface squamous neoplasia is the most common non-pigmented ocular surface tumor, covering a spectrum of disease ranging from non-invasive intra-epithelial dysplasia of the conjunctiva and cornea to invasive squamous cell carcinoma [81]. Many epidemiological studies have demonstrated that in temperate countries, aside from male sex, advanced age is an important non-modifiable risk factor for ocular surface squamous neoplasia [[81], [82], [83], [84], [85], [86], [87], [88]]. Nonetheless, ocular surface squamous neoplasia usually develops at a relatively younger age in populations in tropical climates, where human immunodeficiency virus and human papillomavirus infections are more prevalent [[89], [90], [91], [92], [93], [94], [95]]. These findings have been supported by a systematic review from Africa [96]. Two recent systematic reviews and meta-analyses have confirmed the role of human immunodeficiency and papillomavirus infections as etiologic factors in ocular surface squamous neoplasia [97,98]. Additionally, the earlier onset of ocular surface squamous neoplasia in the tropical regions may be attributed to their proximity to the equator and consequently high levels of ultraviolet radiation [91,99].
Conjunctival melanoma is a rare but sight and life threatening ocular surface malignancy [100]. It is primarily a disease of middle-aged and elderly people, with the majority of patients presenting between 55 and 75 years of age, and it is seldom reported in children [88,[101], [102], [103], [104], [105]]. A large, multicenter, population-based cohort study found that the incidence of conjunctival melanoma increased with age [105]. Older age is also a predictor of more extensive disease and increased risk for visual acuity loss, as well as locally recurrent or new tumor formation following treatment [104,106].
Conjunctival lymphoma, which is the third most common malignancy involving the conjunctiva, after squamous cell carcinoma and melanoma, consists mainly of 4 subtypes of B-cell non-Hodgkin lymphoma, including extranodal marginal zone lymphoma, follicular lymphoma, diffuse large B-cell lymphoma, and mantle cell lymphoma [107,108]. Increasing age is one of the risk factors for conjunctival lymphoma and it typically presents in the seventh to eighth decades of life as a painless salmon-pink patch [107,108]. Age older than 60 years is likewise predictive of a poor outcome for extranodal marginal zone lymphoma [107].
In summary, age is a significant risk factor for many ocular surface diseases, including dry eye disease, meibomian gland dysfunction, blepharitis, conjunctivochalasis, pinguecula, pterygium, infectious keratitis and ocular surface tumors. With an increase in longevity and the rapidly growing number of older populations, it is expected that these ocular surface diseases will result in significant social and economic cost. Research focused specifically on better understanding, preventing and treating age-related ocular surface conditions is required.
2.2. Sex
Both sex and gender impact the prevalence of, severity of, access to and use of care and seeking care for a range of ocular surface diseases [109]. Sex-related effects include those related to chromosomes, that is, the presence of two X chromosomes (female) with different degrees of mosaicism and one X and one Y chromosome (male); sex hormones and the interplay with hypothalamic-pituitary hormones, thyroid, glucocorticoid hormones and others; epigenetics modulated by microRNA, DNA methylation and acetylation and environmental factors. Taken together, these factors may contribute to sex-related differences in the prevalence and clinical course of ocular surface diseases. Gender refers to self-identification and representation based on social and environmental experience [109,110]. The effects of gender are discussed in Section 5.5.
Sex-related biological and physiological differences have been identified in all ocular surface structures, including the cornea, conjunctiva, lacrimal gland, meibomian glands, tear film and in immune function which may be modulated by sex hormones. This may suggest a greater sex-related impact, particularly on those conditions related to inflammatory or immune related mechanisms [109]. Females are more susceptible than males to a range of ocular and systemic autoimmune diseases, including systemic lupus erythematosus, multiple sclerosis, rheumatoid arthritis and Hashimoto's thyroiditis [111].
Most population studies of adult dry eye disease (including both Sjӧgren and non-Sjӧgren disease) show females as having twice the risk of men in studies where the disease definition is based on dry eye symptoms, signs and symptoms of dry eye disease or a prior diagnosis of dry eye disease [10,15]. There is some evidence to suggest that the differences in certain dry eye signs, for example tear film break-up time, between the sexes reduces with age [10,[112], [113], [114]]. Similar to findings in adults, most evidence suggests that young females are more affected than young males [23,28,33], although significant sex differences were not apparent in two studies from Asia [31,34].
There are conceivably sex-related differences in the perception and reporting of pain and pain tolerance [115] which may influence the report of ocular surface and dry eye symptoms, although this is a complex area and there is considerable confounding in published studies, for example between chronic pain and depression and gender differences in reporting depression or seeking care (see Section 5.5). Women are more likely than men to experience chronic pain syndromes, such as fibromyalgia [15], and report more severe, more frequent and more widespread body pain [116,117].
There is a higher rate of asymptomatic meibomian gland dysfunction in Caucasian males [39]. In population-based studies from Japan and in Singapore Malays, males had a higher risk of meibomian gland dysfunction compared with females [11,46]. A higher unadjusted prevalence of meibomian gland dysfunction was reported in males in a population-based study of adults in Iran, although this effect did not persist in multivariable analysis [47]. No sex-related differences were observed in a study in an older (65 years and above) Japanese population [118], however a population study in Iran in those 60 years and over, reported a higher prevalence of meibomian gland dysfunction in men [119]. A recent systematic review and meta-analysis of population-based and hospital-based studies demonstrated male sex as an independent risk factor for meibomian gland dysfunction [40], however a meta-analysis of hospital-based studies in Africa suggested no effect of sex on meibomian gland dysfunction [45], although the age of patients in the African studies tended to be lower. There are challenges in the diagnosis and reporting of meibomian gland dysfunction; most studies have used symptoms plus the presence of either telangiectasia, lid abnormalities, altered meibum expressibility or meibum quality, in at least one eye. It is recognized that telangiectasia is not a unique sign of meibomian gland dysfunction, and most studies do not report the proportion of participants with telangiectasia alone. Given the strong association between symptomatic dry eye disease and female sex and the understanding that evaporative dry eye disease, often due to meibomian gland dysfunction, is a major contributor to the overall disease load in symptomatic dry eye disease, the finding of either no effect of sex or a higher rate of meibomian gland dysfunction in males is perhaps unexpected. Future appropriately-powered studies should apply clear diagnostic criteria for meibomian gland dysfunction, perform analyses disaggregated by age and sex and include younger age groups.
In corneal transplantation, male grafts tend to last longer [120], whereas females function as better graft recipients [120,121]. Males have higher conjunctival goblet cell density [122] and resistance to infection and females have more superior limbic keratoconjunctivitis [123]. Women are more prone to primary acquired nasolacrimal duct obstruction [124]. Pterygium is more common among men, most likely due to occupational exposures [56].
Despite males having a higher risk of corneal infection due to trauma and contact lens wear, females had a higher risk of corneal infection in a large study from South India [65]. In a large case control study in China, sex was not an independent risk factor for infectious keratitis, however there was a higher prevalence of corneal blindness in females [57]. One study has shown that females tend to take longer to re-epithelialize following a fungal ulcer [125].
In summary, there are sex-related differences in a number of ocular surface diseases. In population-based studies, inflammatory or immune related ocular surface diseases appear to be more common in females. Despite the strong association with female sex and dry eye disease, there is no evidence, however, for a higher risk of meibomian gland dysfunction in females. There is robust evidence for males having a higher risk of ocular surface squamous neoplasia compared with females, after controlling for age and ultraviolet light exposure. For several other conditions, sex-related predisposition is more equivocal. Studies may be underpowered to explore sex as an independent risk factor, there may be confounding due to other social or gender constructs, including access to health care, employment, poverty and education.
2.3. Demographic population group
Variations in population group demographics have been reported using self-report of race, ethnicity or ancestral history. The criteria for human classification may differ between studies. These terms may be used to describe both biological or genetic variations and social constructs [126], however, the term ‘race’, does not have an inherent biological meaning. This report will use the terminology reported in the literature, acknowledging those limitations.
There are clear differences in the prevalence of dry eye disease with self-reported ethnicity. South-east Asians, particularly, appear to have 1.5-2x the risk of dry eye disease and meibomian gland dysfunction compared with Caucasians in studies of similar diagnostic inclusion criteria and population-based design [10,127]. In a cross sectional study of dry eye signs and symptoms amongst a co-located migrant population in New Zealand, East Asian participants reported more dry eye symptomatology and had poorer tear film stability, lipid layer thickness and more meibomian gland abnormalities compared with Caucasian participants [128].
While there are clear regional differences in the incidence of fungal keratitis and infectious keratitis more broadly, the impact of ethnicity has not been clearly aticulated, as differences between population groups have been attributed to climate, social, environmental and occupational risk factors [129]. Ethnicity has been identified as a risk factor in Indigenous compared with non-Indigenous individuals in Brazil [130,131], however a systematic review and meta-analysis has identified outdoor occupations and living in rural environments as independent risk factors rather than ethnicity [56]. Similarly, the rates of trachoma [132,133] and onchocerciasis [133], are significantly higher in Indigenous compared with non-Indigenous populations. Pterygium is more common in certain ethnic groups and in a multiethnic study in Asia, Malays had a higher risk of pterygium than Indian or Chinese participants, when controlling for other risk factors [134]. Addressing other societal confounding factors is important in the design and analysis of epidemiological studies to interrogate ethnicity as a risk factor in ocular surface diseases.
2.4. Genetics and hereditary factors
The pathogenesis of ocular surface diseases likely involves complex interactions between genes and the environment. However, little is generally known about the genetic factors involved in the susceptibility to the different diseases. Heritability in dry eye disease was explored in a twin cohort of middle aged and elderly British women [35]. There is moderate heritability of approximately 30% for dry eye disease symptoms and 40% for report of a prior diagnosis of dry eye disease by a clinician, and a varying heritability of 25%–80% for the various dry eye disease signs. Interestingly, tear break-up time showed no evidence of genetic effects.
There are a limited number of studies exploring the most common gene variants such as single nucleotide polymorphisms. A Korean study [135] extracted genomic DNA from blood samples of 251 unrelated non-Sjӧgren dry eye patients and 109 healthy control individuals and demonstrated significant changes among the polymorphisms, rs1143634 (F105F) in exon 5 of IL1B, and for the IL6R gene, the genotypic and allelic distribution of rs8192284, concluding that at least in Korean non-Sjӧgren dry eye patients, alterations in proinflammatory cytokine genes may play a pathogenic role.
The association between polymorphism of the estrogen receptor gene and dry eye disease in Chinese postmenopausal women has been explored in a Korean population [136]. The Xba I and Pvu II polymorphism of the estrogen receptor gene were studied by polymerase chain reaction-restriction fragment length polymorphism in 65 postmenopausal women with dry eye disease and 73 without dry eye disease. There was a significant difference of Pvu II polymorphism of the gene between the dry eye disease and controls in postmenopausal women, but no significant difference was found in the Xba I polymorphism. There was no report of dry eye disease phenotype in this Korean study, however. A study in Caucasians showed no association of the estrogen receptor gene polymorphism with either aqueous-deficient dry eye or evaporative dry eye [137], but the same authors showed an association between MUC1 polymorphisms and both aqueous-deficient dry eye and evaporative dry eye [138].
A retrospective cohort study in soldiers from the USA aged 21–40 [139], evaluated expression of thrombospondin 1 and its association with both post-surgical inflammation and dry eye disease one year post-PRK or LASIK. The association between refractive surgery and dry eye disease is well known, but the extent to which genetic factors may contribute has not been adequately investigated. Conjunctival impression cytology samples collected from participants were used to harvest DNA before the surgery and ribonucleic acid after surgery for gene expression analysis using reverse transcriptase polymerase chain reaction [139]. In this cohort study, patients with dry eye were 2.8x more likely to carry the single nucleotide polymorphism 1 minor allele of the thrombospondin 1 gene. This gene was also correlated with a significant decrease in TSP1 expression in the conjunctival epithelium, along with a concomitant significant increase in the expression of IL-1β, an inflammatory marker associated with dry eye disease [139]. Although this study investigated dry eye disease only in refractive surgery patients, it is nevertheless interesting to note the report of a genetic predisposition to dry eye. The association between single nucleotide polymorphism 1 minor allele of the thrombospondin 1 gene and dry eye disease was not perfect, supporting current understanding that dry eye disease is a multifactorial condition.
The pathogenesis of Sjögren syndrome likely involves complex interactions between genes and the environment. While the candidate gene approach has been used previously to identify several genes associated with disease, two recent large-scale genome-wide association studies, reviewed by Ref. [140], have implicated many more loci as genetic risk factors. Of relevance, was the significant association of Sjögren syndrome with additional immune-related genes including IL12A, BLK, and CXCR5. Other loci and suggestive gene associations in Sjögren syndrome were revealed, but none relating to genes encoding salivary or lacrimal components, secretion machinery or neuronal proteins involved in innervation of the glands [140].
Allergic eye disease affects a wide range of people of all ages and has varying degrees of severity and clinical manifestation. Allergens (pollen, ragweed, trees, and animal dander) are antigens that cause a response of the ocular surface in susceptible or atopic individuals. Atopic conditions frequently occur within families, which has been attributed to both genetic and environmental factors [141]. There is a strong hereditary predisposition for acute allergic conjunctivitis, although the rate of transmission is somewhat less for vernal keratoconjunctivitis. Genetic factors may influence several mechanisms involved in the pathogenesis of vernal keratoconjunctivitis, such as increased presence of eosinophils along with CD4 cells in blood, tears, and conjunctival scrapings and expression of different cytokines; however, genetics in vernal keratoconjunctivitis is mostly undefined [142]. It has been hypothesized that up-regulation of the cytokine gene cluster on chromosome 5q may be relevant, considering the increased accumulation of eosinophils, expression of a multitude of mediators and cytokines (IL-3, IL-4, IL-5, and granulocyte/macrophage colony stimulating factor) [142].
Atopic keratoconjunctivitis is almost exclusively associated with atopic dermatitis, with both genetic and environmental causes [143]. While ocular allergic diseases clearly have a strong hereditary component, the evidence shows that the inheritance of these diseases does not follow a classical Mendelian pattern, suggesting that the genetics of ocular allergic disease are complex and multifactorial.
2.5. Co-morbidities
Chronic co-morbid conditions influence the prevalence and severity of ocular surface diseases, particularly those conditions which alter immune function, such as chronic renal failure, diabetes mellitus, malnutrition, human immunodeficiency virus status, chemotherapy, hypertension, autoimmune disease and alcohol abuse. Conceivably, there are shared genetic associations between co-morbid conditions with certain ocular surface diseases. Many of these factors are covered in depth in the TFOS Lifestyle Impacts [6], Nutrition [3] and Elective Medications [144] Reports, therefore are described here only in brief, to expose their interdependencies with other societal factors.
Population and case-based studies conducted across different countries, ethnicities and environments have shown clear links between co-morbid diseases and either the risk of dry eye disease or the risk of more severe disease. In the Beaver Dam Offspring Study, a population-based study of 3275 young adults in the USA, common conditions associated with dry eye disease included allergies, arthritis and thyroid disease [17]. Similarly, a population-based study in Korea examined 16,408 adults and showed that dyslipidaemia, degenerative arthritis, rheumatoid arthritis, thyroid disease and renal failure were associated with significantly higher prevalence of dry eye disease [145]. A case-control study in Taiwan compared 12,007 participants with dry eye disease with 36,021 controls, and showed ischemic heart disease, hyperlipidemia, cardiac arrhythmias, peripheral vascular disease, stroke, migraines, myasthenia gravis, rheumatoid arthritis, systemic lupus erythematosus, asthma, pulmonary circulation disorders, diabetes, hypothyroidism, liver disease, peptic ulcer, hepatitis B carrier status, deficiency anemias, depression, psychoses and cancers were more common in the dry eye disease group [146].
In a large population-based cohort of 79,606 adult patients in the Netherlands, investigators examined medication classes and individual drugs and their association with dry eye disease, using a hypothesis-free approach [147]. Proton pump inhibitors, anticholinergic drugs and topical anti-glaucoma medications were independently associated with dry eye symptoms.
The Dry Eye Assessment and Management study, was a prospective randomized placebo-controlled trial examining the effectiveness of oral omega-3 supplementation in the treatment of dry eye disease [148]. Using the same cohort of 535 primarily Caucasian female participants, investigators identified systemic conditions associated with worse dry eye symptoms at baseline [149], including Sjӧgren syndrome, acne rosacea, rheumatoid arthritis, and peripheral vascular disease. While the relationship between certain co-morbidities and dry eye disease may have an obvious biological rationale, for example Sjӧgren syndrome results in lymphocytic infiltration of the lacrimal glands [150], directly causing keratoconjunctivitis sicca, or dermatological or sebaceous gland diseases showing associations with meibomian gland dysfunction and posterior blepharitis [151], other robust associations are less easily explained, for example, that between dry eye disease and peripheral vascular disease.
Co-morbidities associated with more severe dry eye disease have been explored in a Spanish Sjӧgren syndrome registry study of 437 patients, where inflammatory articular involvement predicted more severe dry eye disease [152]. Using the Netherlands Lifeline Cohort, co-morbidities associated with more severe dry eye disease among the 78,165 population-based participants included irritable bowel syndrome, fibromyalgia, chronic fatigue syndrome, eye surgery, keratoconus, osteoarthritis, connective tissue diseases, atherosclerosis, Graves' disease, autistic disorder, depression, ‘burnout’, Crohn's disease, sarcoid, lichen planus, rosacea, liver cirrhosis, sleep apnea and sinusitis [15]. Importantly, this study identified several chronic pain syndromes, namely fibromyalgia, chronic fatigue syndrome and irritable bowel syndrome, and neuropsychiatric diseases that worsened dry eye disease [15]. Patients suffering from chronic pain syndrome are more likely to have depression and anxiety, and as a result may take up a more withdrawn societal role [153]. Sufferers have negative perceptions of their interactions with care providers and conceivably these patients may have more difficulty seeking treatment for dry eye disease or other ocular surface diseases [153].
The association between neuropsychiatric diseases and more severe dry eye disease has been supported by other studies, with varying degrees of evidence. In a survey of 100 optometrists and ophthalmologists in North Carolina, USA, the most common comorbidities in dry eye disease patients were rheumatoid arthritis, Sjӧgren syndrome, affective disorders such as anxiety and depression, history of photorefractive surgery, smoking, and thyroid disease [154]. A significantly increased risk of dry eye disease was present in USA military veterans suffering from post-traumatic stress disorder and depression using data from a large case control study of over two million patients at a Veteran Affairs eye clinic [155]. This was further confirmed by a study from the same authors in 248 male USA military veterans, aged 50 and above, suffering from post-traumatic stress disorder [156]. Using multivariable logistic regression, both a diagnosis of post-traumatic stress disorder and use of selective serotonin reuptake inhibitors significantly increased the risk of more severe dry eye symptoms [156]. Clearly though, the pathogenesis of dry eye disease in such patients is complex and beyond the pharmacological side-effects alone. A possible approach is to investigate the societal context in which neuropsychiatric patients live, to identify known or new lifestyle risk factors for dry eye disease.
The impact of systemic comorbidities on ocular surface diseases were examined in 449 Japanese patients with dry eye disease at 10 eye clinics in Japan [157]. The most common comorbidities in this elderly cohort (mean age of 62.6 years) were hypertension, depression, and insomnia, together accounting for more than 40% of concurrent conditions. Patients with dry eye disease and systemic comorbidities had significantly worse ocular surface disease and health-related utility than those without comorbidities. Furthermore, certain comorbidities were associated with specific types of ocular surface diseases. For example, patients with insomnia and depression had higher prevalence of friction-related ocular surface diseases, which included conjunctivochalasis, superior limbic keratoconjunctivitis and lid-wiper epitheliopathy [157]. This may suggest specific bedtime behavioral patterns in patients with insomnia and depression that conceivably predispose to repeated ocular surface rubbing.
While the impact of comorbidities on ocular surface disease is important, it is also vital to recognize the impact of long-standing dry eye disease on mental and physical wellbeing. In the Lifeline Cohort, investigators examined the relationship between dry eye disease and quality of life in 78,165 participants [158]. Significantly, the study found that dry eye disease was associated with lower mental and physical health-related quality of life. Increasing dry eye disease severity was associated with decreasing health-related quality of life. Furthermore, those with undiagnosed dry eye disease had significantly worse mental health-related quality of life than those who already had a diagnosis. Using the same cohort, investigators examined the relationship between dry eye disease and poor sleep quality [159]. dry eye disease patients had higher prevalence of poor sleep quality compared to controls. Correcting for all comorbidities, dry eye disease was still significantly associated with poor sleep quality. Almost half of the participants who reported dry eye symptoms ‘often’ or ‘constantly’, had poor sleep quality. Similar findings of more severe dry eye disease and insomnia or poor sleep quality were reported in 187 USA veterans [160] and in a Chinese community study of 3070 participants [161].
In a prospective interventional case series on 45 adult patients who were receiving dry eye treatment in the USA, an improvement in dry eye severity resulted in reduction in anxiety and depression symptoms [162]. This was consistent regardless of whether the patient had an existing diagnosis of generalized anxiety disorder or major depressive disorder. A study using data from the Fifth Korea NHANE survey on 16,408 participants, confirmed an association between dry eye disease and increased odds of depressive symptoms and suicidal ideation [163].
Systemic co-morbidities, anxiety and depression and medication use are frequently associated with dry eye disease and with increased severity of dry eye disease (see also TFOS Lifestyle [6] and Elective Medications [144] Reports). There is considerable complexity as dry eye disease is associated with reduced societal participation and impact on daily activities, which may predispose to other systemic conditions. Conversely, persistent ocular discomfort may cause patients with dry eye disease to become less physically active, lose their ability to work and experience societal withdrawal. This in turn may predispose affected patients to chronic physical and mental health conditions.
The effect of co-morbidities in non-viral infectious keratitis has not been systematically explored in appropriately powered population-based studies, although there is evidence for certain conditions to be associated with more severe infections or infectious corneal blindness. Risk factors for infectious keratitis include diabetes [63], alcohol [63] or recreational drug use [64]. Alcohol use is an independent risk factor for infectious corneal blindness [64] and rheumatoid arthritis for severe infectious keratitis [66]. Systemic risk factors for contact lens related infectious keratitis include diabetes as a probable risk factor and there is some evidence for associations with thyroid eye disease and self-reported poor health [164]. Herpes simplex virus keratitis and more severe herpes simplex virus disease are associated with diabetes [165,166], although a similar association has not been shown with Herpes zoster keratitis [166], nor with human immunodeficiency virus status [165,167].
3. Individual lifestyle/social or community factors, including nutrition, smoking, exercise
3.1. Nutrition
Eating behaviour and nutritional status play important roles in ocular surface health and disease [168,169]. Societal factors are crucial determinants of adequate nutritional intake and healthy eating pattern [170,171]. The ‘double burden of malnutrition’, referring to undernutrition on one side and being overweight and obesity on the other side, was introduced into the literature at the beginning of the 21st century [172,173]. The rate of the double burden of malnutrition has increased over the past decades, and this increase was accelerated during the coronavirus disease 2019 (COVID-19) pandemic [174,175]. Ocular surface signs of nutritional disorders and the underlying mechanisms have been reviewed in detail in the TFOS Nutrition Report [3]. In this section, societal challenges with potential ocular surface consequences through nutritional or eating imbalances are reviewed.
3.1.1. Food insecurity
Food insecurity is understood as not having access to sufficient food, or food of an adequate quality, to meet one's basic needs. It is associated with multiple nutritional deficiencies with known ocular surface consequences [176,177] However, the relationship between food insecurity and ocular surface disorders has been infrequently studied. Several longstanding and emerging global and regional societal challenges threaten food security. Poverty is a well-known cause of food insecurity, not only in developing countries [178,179], but also in certain groups in high-income countries [180,181]. Climate change is an emerging challenge that may impose direct and indirect impact on food security. Extreme weather conditions result in increased poverty and reduced food consumption [182], and conversely, climate policies may impose a financial burden on developing countries through increased food and energy prices [183]. The emergence of the COVID-19 pandemic raised concerns for the exacerbation of poverty and food insecurity [[184], [185], [186]]. Unemployment, stay-at-home orders, and distribution shortages are potential causes of both short and long-term impacts of the COVID-19 pandemic on food security, which have a greater impact in low- and middle-income countries [187,188]. Mass immigration due to environmental, economic and security crises, remains a global challenge. Food insecurity is a common health problem among immigrants, especially among undocumented immigrants and those seeking asylum [[189], [190], [191]]. Immigration has been associated with lower nutritional quality for multiple nutrients, including vitamins and minerals [192,193]. However, there is a lack of evidence regarding the impact on food insecurity specifically on the prevalence or severity of ocular surface diseases among immigrants and refugees (see Section 5.8).
3.1.2. Eating disorders
Anorexia nervosa is a psychological disorder characterized by fear of gaining weight, loss of appetite, and distorted body image. The incidence and lifetime prevalence of anorexia nervosa is 8/100,000 and 0.5%–2%, respectively [194,195], with a remarkable increase among young females over the past two decades [196]. Of note, there have been reports of increased risk of episodes of eating disorders during the COVID-19 pandemic, possibly due to changes in living conditions, social distancing, self-isolation, changes in food access, more intense use of social media, and more limited access to healthcare services [[197], [198], [199]]. There are no systematic reviews or meta-analyses on the ocular surface manifestations of eating disorders and their reversibility. A population-based study in the Netherlands with almost 80,000 participants, found eating disorders to be associated with a 1.6x increased prevalence of dry eye disease, after correction for age and sex. However, after correction for an additional 48 comorbidities, this increased risk was no longer significant [15]. Various ocular surface complications with different underlying mechanisms have been reported including a lower spontaneous blink rate during fixation tasks in patients with anorexia nervosa compared with healthy controls, which has been attributed to reduced dopaminergic activity [200]. In addition, incomplete eye closure due to neuromyopathy of the orbicularis oculi muscle was reported in an anorexic patient with vitamin C deficiency [201] and ocular surface symptoms secondary to lagophthalmos have been reported [202]. Although vitamin A deficiency may have implications for ocular surface signs of chronic anorexia nervosa, superficial punctate keratopathy, reduced tear production, and conjunctival squamous metaplasia may occur in the absence of vitamin A deficiency [203]. Further studies are required to determine the role of societal factors in eating disorders and their ocular surface consequences.
3.1.3. Obesity and metabolic syndrome
Obesity is a multifactorial disease with complex genetic and environmental risk factors [204]. Alongside high blood pressure, hyperglycemia, and hyperlipidemia, obesity is a risk factor for metabolic syndrome (a cluster of conditions which together increase the risk of heart disease, stroke and type 2 diabetes). The global prevalence of obesity and metabolic syndrome has increased significantly over the past few decades due to imbalanced nutrition, socioeconomic conditions and sedentary lifestyles [[204], [205], [206]]. Obesity has been associated with lower tear break-up time and greater meibomian gland dysfunction and ocular surface disease index scores, relative to a non-obese control group [207]. A study in Chinese adults revealed significant associations between moderate-to-severe meibomian gland dysfunction and being overweight or obese [208]. In a paediatric population, body mass index was associated with meibomian gland tortuosity and reduced lipid layer thickness [209]. Obese participants were more likely to develop dry eye disease compared with those with low body mass index (<23 kg/m2) [210]. This relationship was reversed in the Lifelines study, which found a strong association between both high (measured) body mass index and (measured) hypertension and less dry eye disease, when controlling for other variables [15]. This would suggest there is not a simple relationship between metabolic syndrome, its risk factors, conditions reflective of systemic inflammation and meibomian gland dysfunction or/and dry eye disease, in different population groups [[211], [212], [213]].
3.1.4. Fasting
Daytime fasting, either as a ritual practised for religious reasons or as a diet regimen (also known as intermittent fasting), may have impacts on tear production and ocular surface health. After 12 h of fasting, there is a temporary increase in basal tear secretion followed by a decrease [214]. Also, significant changes in the pattern of tear proteins and activity of tear enzymes were observed during fasting in Ramadan (the holy month for Muslims) compared with the previous month [215]. Moreover, religious fasting was associated with significantly increased tear osmolarity, ocular surface disease index score [216] and inflammatory markers [217] and decreased unanesthetized Schirmer value [216] and tear break-up time [217]. There is no report on the ocular surface effects of non-religious intermittent fasting (which is less strict than religious fasting), though potential impacts have been proposed [218]. Since intermittent fasting as a diet regimen is gaining popularity [219], further studies to explore its impact on ocular surface health are recommended.
3.2. Smoking
Nicotine is a drug that can act as both a depressant and a stimulant. It is a naturally occurring alkaloid which is present in cigarettes and tobacco [220]. Smoking is a known cause of tear film alterations [221,222] but the relationship between smoking and ocular surface diseases is less clear (also see TFOS Lifestyle Report [6]). Cigarette smoke can increase tear interleukin-6, decrease goblet cell density, decrease the secretion of tear MUC5AC [223] and can irritate the ocular surface, resulting in symptoms [224]. Unanesthetized Schirmer score is reduced in smokers compared to non-smokers (13.3 ± 11.5 mm vs 19.0 ± 11.7 mm) [223]. The decrease in goblet cell density in smokers is associated with lissamine green staining of the ocular surface [223].
Population-based studies have not confirmed an elevated risk for dry eye disease with smoking, however. One study established smoking as a risk factor for dry eye disease [149] but this has not been confirmed in a systematic review of smoking and eye diseases [225], and the largest population-based Lifelines study has shown a reduced risk of dry eye disease in current smokers, but a higher risk in previous smokers, a result confirmed in a UK-based population study reported in the same paper [15]. The rate of smoking has increased in certain population groups, including women and adolescents [226,227]. Smoking is often associated with other demographic and societal factors, including family history and social factors [228], unemployment [229], low-income [230], and immigration [231]. There is a positive relationship between smoking and depression, anxiety, and psychological distress, although the evidence does not support a causal role for smoking in developing mental illnesses [232,233]. Independent relationships between smoking and ocular surface diseases may therefore be confounded by other societal factors.
The use of e-cigarettes and vaping may be considered an emerging societal factor, and this may expand the demographic exposed to nicotine. Smoking nicotine-containing e-cigarettes significantly reduces tear film stability and increases ocular surface staining [234], adversely impacts the tear lipid layer [221], causes changes in conjunctival impression cytology [235], reduces corneal and conjunctival sensitivity [236], increases ocular irritation and decreases anesthetised Schirmer scores [237], alters tear ferning grade [238], increases tear osmolarity [239], increases eyelid margin abnormalities and decreases meibum quality [240]. E-cigarettes may be equally as harmful to the ocular surface as traditional tobacco or cigarettes, although this has not been confirmed in population-based studies. Vaping decreases non-invasive tear break-up time, fluorescein tear break-up time, and tear meniscus height compared to non-vaping controls, with the effect on these ocular surface parameters being worse with higher vaping voltage [241]. However, this study also reported significantly higher Schirmer scores in vapers compared to non-vapers [241], conceivably due to increased tear production from vaping smoke, although this was unproven.
3.3. Exercise
Exercise is an effective treatment for chronic systemic diseases including cardiovascular disease [242], where it can reduce systolic blood pressure, fasting glucose, fasting insulin and improve vascular and cognitive function [242,243]. In diabetic mice, eight weeks of aerobic exercise increased tear secretion and reduced oxidative stress markers in tears [244].
A large population-based study in Japan showed that a lack of physical exercise and sedentary behaviour were strongly linked with increased susceptibility to dry eye [245]. This association was also found in a large population-based study in the Netherlands, but was not present after further correction for 48 comorbidites including conditions that are consequently associated with decreased exercise, such as connective tissue disease and depression, indicating the importance of correction for associated comorbidities in these analyses [15]. In Japanese children, screen time and decreased physical activity was associated with obesity, dry eye and reduced academic performance [246]. In a small study in humans, 30 min of aerobic exercise improved Schirmer score, invasive and non-invasive tear break-up time and reduced levels of inflammation and stress markers in the tear film [247]. Ten weeks of aerobic exercise performed three times per week in 11 participants with dry eye disease improved dry eye symptoms as measured with the DEQ-5 [248]. It is conceivable that parasympathetic innervation to the lacrimal gland, specifically to the acinar blood vessels, is stimulated with exercise, which may increase the secretion of electrolytes and water [249]. There are limited published studies in both dry eye disease and normal participants for a conclusive statement to be made, however.
3.4. Alcohol/caffeine/recreational drug use/abuse
3.4.1. Alcohol (see TFOS lifestyle challenges [6] and nutrition [3] reports)
Orally administered ethanol can be detected in tears, leading to decreased tear break-up time and unanesthetized Schirmer scores [250], and increased corneal staining and tear osmolarity compared to controls [251]. In a meta-analysis of 10 studies, alcohol consumption was a significant risk factor in dry eye disease, irrespective of age and sex [252]. A large population-based study reported alcohol consumption increased the risk of symptomatic dry eye disease in females (odds ratio [OR] 1.095, 95%CI 1.045–1.148) after correction for confounding variables such as demographic and systemic disease factors; but this finding was not significant in males in whom alcohol consumption was found to be protective against symptomatic dry eye disease [253]. The oral consumption of alcohol may also induce an upregulation of proinflammatory cytokines in the cornea [251].
Chronic consumption of alcohol has been linked to vitamin A deficiency via the induction of ethanol-inducible cytochrome P-450 in the liver [254], leading to morphological changes on the ocular surface in the form of conjunctival and corneal keratinization, goblet cell loss [255], punctate keratitis, necrosis and corneal ulceration [256].
Some large epidemiological studies have reported no impact of alcohol consumption on dry eye disease [224,257,258]. Alcohol consumption, however, was noted to be protective for dry eye disease in an older Australian population [259].
3.4.2. Caffeine (see TFOS lifestyle challenges report [6])
Caffeine is a central nervous stimulant belonging to the methylxanthine family. It is one of the most consumed psychoactive substances and is known to have mild diuretic effect [260]. Due to this diuretic effect, caffeine, when consumed in large quantities, has been thought to exacerbate dry eye disease, however, there is little evidence to support this. In a large population survey study of 19,599 participants, the frequency of coffee consumption, based on the number of cups of coffee consumed per day showed no relationship with the risk of dry eye disease [261]. In a population-based study in the Netherlands, including 85,302 participants, caffeine intake was calculated by assessing dietary intake of coffee, tea, cola, and energy drinks [262]. Caffeine intake was associated with a slightly protective effect on dry eye, after correction for age and sex only. This association disappeared however after additional correction for over 50 possible confounding factors including smoking, alcohol intake and numerous comorbidities [262]. Similar findings have been observed using diagnostic criteria other than the Women's Health Study questionnaire for dry eye disease [259,263]. There is some evidence for a protective effect of caffeine in dry eye disease from the Beaver Dam Eye study cohort, where participants who did not consume coffee had significantly higher prevalence of dry eye disease compared with those who did (16.6% vs 13.0%) [224]. Confounding factors may have influenced this result, however.
The effect of caffeine on tear secretion was studied in a randomised controlled trial of 41 healthy young adults, with a mean age of 23 ± 2.1 years [264]. Consumption of caffeine (5 mg/kg of body weight dissolved in 200 mL of water) resulted in increased Schirmer scores (without anesthetic) assessed at 45 min and 90 min post-consumption [264]. Caffeine intake between 5 and 7 mg/kg of body weight increased tear meniscus height in a randomized controlled trial of 78 healthy participants [265]. The underlying mechanism is unclear, but polymorphisms in cytochrome P450 1A2 and the adenosine A2a receptor gene may be implicated [265]. The effect of caffeine on other ocular surface disease parameters such as tear break-up time, tear osmolarity and ocular surface staining has not been explored in well-controlled studies.
Green tea contains xanthines (such as caffeine), amino acids (such as theanine, glutamic acid, tryptophan, lysine, aspartic acid, glycine, serine, tyrosine, valine, leucine, threonine, and arginine); catechins; polyphenols (such as flavanols, flavandiols, and flaconoids) and trace elements [266,267]. Green tea is mostly consumed for its benefits in cardiovascular disease, anti-stress, anti-inflammatory and antioxidative properties, as well as neuroprotective and cholesterol-reducing properties [266].
The effect of a single dose of green tea on tear production and quality was assessed in a case control study using the phenol red thread test and tear ferning test [268]. Tear film ferning is a measure of tear film quality and the tear fern pattern formed following the drying of tears collected on a glass slide under normal room temperature conditions is assessed qualitatively [269]. Normal tears produce a dense fern pattern while in patients with dry eye disease, the pattern is either absent or fragmented [270]. There was a reduction in median phenol red thread test length, with 80% of participants showing a reduction in length, and an increase in tear ferning fragmentation 1 h after consumption (2.0 g in 150 mL) [267]. The authors hypothesized that the serum lipid oxidative properties of polyphenols observed in a rat model, may be similarly exhibited in human tear film lipids and impact tear film quality. A further hypothesis is that a low concentration of caffeine, between 2 and 4%, may also contribute to the findings [267]. In contrast, a comparative study which evaluated the effect of topically-instilled green tea extract compared with artificial tears, reported an improvement in dry eye symptoms (ocular surface disease index), tear break-up time and meibum quality [271].
The available evidence would suggest that caffeine seems to offer a benefit to the ocular surface by decreasing dry eye symptoms, increasing tear secretion and tear film stability but the effect of green tea on the ocular surface is equivocal.
3.4.3. Recreational drugs
Recreational drug use refers to the unsupervised use of illegal or legal drugs for leisure or pleasure, including analgesics, depressants, hallucinogens and stimulants. Analgesic drugs in this context include narcotics such as heroine, codeine, fentanyl, tramadol and morphine. Depressant drugs inhibit the central nervous system and may lead to drowsiness, coma, sleep, anesthesia, and death, including alcohol, nicotine, barbiturates, and tranquilizers. Hallucinogens induce psychological effects such as distortions from reality, illusions and hallucinations, including marijuana, psilocybin, lysergic acid diethylamide, phencyclidine, peyote and ketamine. Stimulants increase the activity of the central nervous system and bodily activity in general, including cocaine, methamphetamine, and 3,4 methylenedioxymethamphetamine.
The prescribing of opiate analgesics for ophthalmic indications has increased, particularly in people with African heritage, individuals with higher income, and a lower level of education [272]. Despite the increasing use of these drugs in ophthalmology in both post-operative cases and in the treatment of neuropathic pain [273,274] and evidence of persistent opioid use after ocular surgery [275], the effect of opiate analgesics on the ocular surface has not been widely studied (See TFOS Elective Medicines Subcommittee Report [144]). Opioid receptors are present on the human cornea and topically applied opioids may stimulate these receptors to decrease ocular pain [276].
Morphine is used in pain management [277] and is one of the most commonly abused medications [278]. Users of morphine are more likely to be male, experiencing homelessness and unemployment [278]. Topically-applied morphine sulphate in post-surgical abrasions reduced pain and corneal sensation without retarding corneal wound healing [277]. Tramadol, another opiate analgesic, is an analogue of codeine that has been used to manage post-surgical eye pain [279]. There are no randomised controlled trials of its effects on the ocular surface in humans, but corneal sensitivity is reduced within 1–25 min of topical application [280] and temporary blepharospasm has been induced in animal models [281].
While corneal wound healing appears to be unaffected by the topical use of opioids, corneal anaesthesia may alter tear secretion and corneal epithelial physiology [282,283]. Importantly, the corneal analgesic effect is effective only in the presence of inflammation [277].
In animal studies, there was no impact of tear production measured with the Schirmer test following intramuscular tramadol in dogs [284,285] or with morphine [286] or fentanyl [287]. Heroin use may lead to conjunctival injection [288] and a case of atypical kerato-conjunctival lesions due to transconjunctival heroin abuse has been reported [289].
Barbiturates are sedative and hypnotic agents used in the management of seizures, pre-operative anxiety, insomnia, and the induction of coma. There are limited human studies that directly explore the impact of barbiturates on ocular surface diseases, but one study did find that phenobarbital leads to a transient sicca effect in a patient being managed for seizures [290]. In animal studies, thiopental decreased tear production assessed by unanesthetized Schirmer scores in dogs when used in the induction of anesthesia [291]. The use of anxiolytic medications in patients with depressive or anxiety disorders has been linked to a higher odds ratio of dry eye disease [292,293]. Ketamine, a sedative medication used during surgery reduces tear production in both cats [294] and dogs [295]. Although there are few direct studies, the indirect evidence would suggest that these sedative medications may worsen dry eye disease by decreasing tear production.
Marijuana has psychoactive properties and has been used in medicine for increasing appetite, treating eating disorders and nausea, in the management of pain and chronic inflammation, multiple sclerosis and epilepsy [296]. In humans, marijuana use has been associated with reduced tear secretion [297] and decreased corneal endothelial cell density [298]. In mouse studies, the ocular effect of marijuana via its derivative, tetrahydrocannabinol, through acting on the ocular surface cannabinoid CB1 receptors, appears to be sex dependent as it leads to decreased tear production in males but increased tear production in female mice [299]. While marijuana use may lead to dry eye symptoms [300,301] and a decrease in tear production [297], it may however be useful in the management of corneal neuropathic pain [302]. Topical administration of 1% delta 9- tetrahydrocannabinol results in increased ocular irritation [303]. There is limited evidence of the benefits of cannabis on ocular surface disease and based on available data, marijuana use, especially when smoked, may worsen dry eye disease.
The data regarding the impact of hallucinogens such as psilocybin, and lysergic acid diethylamide are limited, however, conjunctival and corneal erosions have been reported in a case of trans-conjunctival lysergic acid diethylamide application to the inferior conjunctival fornix [304].
Other stimulant drugs such as snorted cocaine have been linked to decreased tear production assessed by unanesthetized Schirmer wetting scores (16.5 ± 10.1 mm in eyes following cocaine use vs 22.5 ± 12.9 mm in control eyes) [305]. Similarly, in individuals who snorted cocaine, there was a significant decrease in tear production, decreased corneal sensitivity, neurotrophic keratitis, and decreased blink rate [306]. Other conditions associated with the use of cocaine include anterior staphyloma [307], corneal ulceration [308,309], epithelial defects and corneal infiltration [310], and infectious keratitis [311]. Similarly, methamphetamine use has been reported to lead to conjunctivitis and corneal melting [312], and keratitis [313]. The mechanism of damage of cocaine and methamphetamine to the ocular surface has not been well studied, but it may well be related to the excessive release of dopamine, which leads to sensory nerve damage [314]. This may lead to a decreased blink rate, worsening exposure keratopathy, neurotrophic keratitis, corneal ulceration and ultimately corneal blindness.
3.5. Cultural and religious beliefs, including traditional medicines
Traditional medicines describe health practices based on animal or plant sources, spiritual or mineral therapies used in the diagnosis, prevention or management of illness or maintenance of general well-being [315]. There is widespread use of traditional medications and practices in developing countries, especially in Africa, India, and South America. Traditional medications may be in the form of vegetative matter, breast milk, plant extracts or animal waste products.
Breast milk has been traditionally used by mothers for the management of conjunctivitis in rural areas in developing countries [316]. The protective mechanism is believed to be due to immunoglobulin A, lysozyme, lymphocytes, macrophages and protease inhibitors present in the colostrum, which confer antibacterial properties [317]. However, complications, including corneal infection and endophthalmitis, have been reported in a prospective study in a tertiary health setting [317]. Another prospective study also reported breast milk to be the most commonly applied traditional eye medicine in patients with corneal ulcers (45.2%) [318]. Other traditional eye medicines include vegetative matter (29.6%), castor oil (11.9%), and hen's blood (5.9%) [318]. The use of traditional eye medications has been associated with hypopyon at presentation, with a risk of central dense corneal scarring [319] and infectious keratitis as well as peripheral corneal ulcers [320]. Patients using traditional eye medicines tend to have a delayed presentation to seek medical attention compared to those using Western medicine [321].
While the harmful effects of breast milk on the ocular surface are well documented, there is also some evidence of benefit. In mouse models, human breast milk improves corneal epithelial damage comparably to cyclosporine [316]. In a prospective animal study comparing the use of breast milk, autologous serum and artificial tears in mice with corneal abrasions, the group receiving topical breast milk drops experienced faster corneal re-epithelization compared to other groups [322]. In a study of breast-fed infants ≤180 days, breast milk was equally effective in treating eye discharge when compared to sodium azulene sulphonate hydrate 0.02% ophthalmic solution [323]. In patients with neurotrophic corneal opacity, especially post-viral infections, breast milk appeared to be effective in improving corneal sensitivity and visual acuity [324]. However, some patients developed bacterial conjunctivitis during treatment and the efficacy was poor in diabetics [324]. Topical bovine colostrum improves corneal re-epithelization following alkali burns in mice [325].
Castor oil is derived from the Ricinus communis plant and is used in cosmetics as an emollient (See TFOS Cosmetics Subcommittee Report [4]). It has been used as a wound dressing and a drug delivery system [326]. It has antibacterial, anti-cancer [327], anti-inflammatory, anti-oxidant and wound healing properties, making its use on the ocular surface logical [326]. In vivo, ricinoleic acid contained in castor oil is able to produce esters, amides and polymers which cover the ocular surface, decreasing the evaporation of aqueous tears and thus improving tear stability and decreasing ocular surface staining and dry eye symptoms [326]. In a randomized controlled trial, topical periocular castor oil significantly decreased ocular surface disease index scores, lid margin thickening, telangiectatic vessels, lash matting, madarosis, cylindrical dandruff and lid wiper epitheliopathy in patients with blepharitis after 4 weeks of use compared to untreated eyes [326]. Castor oil, applied topically, appeared safe and effective in decreasing tear film instability, symptoms, and ocular surface staining in strengths of 2% and 5% compared to placebo in a randomised controlled study [328]. Though widely believed to be of benefit in eye lash growth, the evidence suggesting the use of castor oil for eye lash elongation is lacking and the evidence for its use in hair growth is weak [329].
Poor access to health care facilities, distance from hospitals and illiteracy are some of the reasons for the use of practices that may lead to severe ocular surface diseases due to traditional medicines. Education of, and collaboration with, traditional healers led to a decrease in corneal blindness and changes in the pattern of corneal disease in rural areas in Africa [330]. In this study, traditional healers were discouraged from using traditional medicines applied directly to the eyes and they were advised to refer patients if there was no resolution of the ocular disease in three days. After one day of training the healers, a change in the pattern of corneal disease was observed, with bilateral corneal disease decreasing from 31% to 10% [330].
Due to religious beliefs, certain traditional practices have become popular in rural areas. Ayuverdic medicine is a form of traditional Indian medicine derived from natural substances such as roots, and herbs for the treatment of the mind and soul. Cow urine is notably used in the preparation of some of the formulations of this type of medicine and this has been used for treating a range of diseases, including coronary artery disease, hypertension, asthma [331] and cancer [332]. The cow urine is either boiled, or the distillate used [331]. Cow urine applied to the eye leads to corneal epithelial defects, corneal edema and decreased vision [331].
The type of traditional medicine use varies with cultural practices and geographic diversity. A systematic review reported the widespread use of Kermes, a red dye obtained from an insect Kermes ilicis in Saudi Arabia [315]. Kermes leads to severe ocular surface toxicity and cicatricial conjunctivitis [333]. Alum, a hydrated salt comprised of potassium aluminium sulphate used in making foods, as an astringent agent, and also as a flocculating agent [315], causes severe keratitis, corneal thinning, scarring and decreased vision [334]. In animal models, garlic extract has exhibited antibiotic properties similar to gentamycin and has been used traditionally in parts of Nigeria, Western Africa [335], however, such vegetative extracts may also act as sources of ocular infections. Similarly, honey, used for its anti-inflammatory, anti-bacterial and anti-oxidant properties, has been used in the management of ocular surface diseases such as blepharitis [336], conjunctivitis [337], dry eye disease and tear film stability in meibomian gland dysfunction [338,339], and even vernal keratoconjunctivitis [340]. Despite these numerous benefits, honey can become contaminated and has been implicated in Acanthamoeba keratitis [341]. Aloe vera is another naturally occurring plant with sap that has many benefits [342]. However, it has also been associated with ocular infections [343], and these plants (or their sap), when not properly stored, may become contaminated and become potential sources of infection [315]. Ushaar (Calotropis procera) is a xerophytic shrub found in Asia, Africa and some parts of South America, which can induce corneal toxicity [344]. The traditional Chinese medicine, Qiming may hold promise in improving tear film stability and secretion, as well as corneal wound healing properties [345]. Further studies are needed to thoroughly determine its therapeutic value.
Homeopathic medicines have been used to reduce ocular symptoms associated with allergic rhinitis, and a systematic review determined a small positive effect of Galphimia glauca or a homeopathic nasal spray on ocular and nasal symptoms [346]. However, risk of bias and lack of appropriate masking in these studies warrants further randomised control trials to determine their true efficacy.
While some traditional medicines clearly have benefits to the ocular surface, they may act as a source of microorganisms, induce toxic keratopathy and pose a threat to vision. Where medications are not manufactured with strict hygiene protocols and tested for efficacy and safety, they should be used with caution. Their use should be restricted to those with no or limited history of ocular toxicity and by trained skilled practitioners with a low threshold for early referral, if conditions do not resolve quickly. In the absence of obvious improvement, or with worsening of the condition, the use of these agents should be discontinued, and appropriate management instituted.
3.6. Hobbies, recreational and sport-related factors
3.6.1. Recreational and sport-related factors
Although sports and recreation have numerous physical and mental benefits, traumatic injuries to the ocular surface may occur. In a retrospective study in the USA, the most common sports and recreation activities associated with eye injury in children younger than 17 years of age, were basketball (15.9%), baseball and softball (15.2%), and non-powder guns (10.6%) [347]. In Australia, cycling, football, tennis, trampolining, fishing and swimming were the sports responsible for the greatest number of eye injuries [348].
Sports such as soccer and hockey increase the risk of sight threatening eye injuries. A study analyzed the trends of soccer-related ocular injuries in the USA from 2010 to 2019, and found that serious visual consequences were associated with soccer-related ocular injury [349]. Field hockey is a popular high school sport among girls in the USA. Although not common, serious eye injuries and vision damages can happen when players are struck by the stick or ball during the game [350]. The National Federation of State High School Associations in the USA issued a protective eyewear mandate in sanctioned competitions in 2011. A prospective cohort study evaluated the incidence of eye/orbital injuries during two seasons of play before and after the national protective eyewear mandate and demonstrated that the mandate was associated with a decreased incidence and severity of eye/orbital injuries [351].
Toy guns, usually a miniature non-functioning replica of a gun, but those which may fire caps or pellets, can also cause a range of traumatic injuries. A study from Finland found that toy guns can cause serious eye trauma, including blunt ocular trauma and corneal abrasions [352]. Both players and bystanders are recommended to use protective eyewear during the entire game [352]. Similar results were reported from a study on children in Canada [353]. A retrospective study reviewed the characteristics and outcomes of patients treated for ball bearing and pellet gun-related open globe injuries from January 2002 to November 2017 [354]. The result indicated that ball bearing or pellet guns could cause devastating visual damage, associated with multiple complications and the need for further surgery beyond the initial repair [354]. These results emphasize the importance of eye protection during the use of toy guns.
Based on a review of publications from 1980 to 2014 describing eye trauma and recreational fishing, sharp hooks and heavy sinker weights projected at high speed, can cause severe eye injuries and significant vision loss [355]. Open and closed globe Injuries occurred 9x more commonly in males and were most likely to occur via a hook [355]A retrospective observational analysis of the data from The United States Eye Injury Registry found that fishing-related eye injuries accounted for 19.5% of all sports related eye injuries and 28.2% of the open-globe injuries reported to the registry from 1998 to 2004 [356].
3.6.1.1. Firework injuries
Fireworks are popular but can lead to severe eye injuries. Firework-related eye injuries and associated consequences were reviewed by the International Globe and Adnexal Trauma Epidemiology Study: Fireworks Study Group [357]. Cross-sectional or retrospective studies have been carried out in various countries, including the USA [358], China [359], India [360], Germany [361,362], Nepal [363] and the Netherlands and Finland [364], to quantify the national prevalence of firework-related ocular injuries. Firework-related ocular injuries mostly occur in young males and the severity of the injuries ranged from mild irritation to ruptured globes. More severe injuries have major impacts on ocular morbidity and visual acuity. To significantly reduce firework-inflicted trauma, a ban of private fireworks in densely populated areas and in the vicinity of children should be considered. Greater education about, and prophylaxis for, firework-related eye injuries would help to reduce the risk of severe consequences.
3.6.2. Ultraviolet light exposure
Outdoor or indoor exposure to ultraviolet light is common due to sporting or vocational exposures, or due to societal expectations of having a tanned appearance (See also Section 4.2 and TFOS Environmental Subcommittee Report [7]). Persistent exposure can occur in outdoor and winter sports, including water sports, skiing, snowboarding and distance running, and persistent exposure is related to ocular surface diseases including pterygium, droplet keratopathy and snow blindness [365]. The level of protection for athletes and workers is dependent on the jurisdiction and level of regulation. Ultraviolet light eye protection in athletics is frequently mandated through uniform and eye protection policies at club and competition level [366].
Indoor suntanning is a popular way of enhancing skin tones for people with light skin color (See TFOS Cosmetics Subcommittee Report [4]). Because of a lack of universally adopted laws or guidelines, eye protection during indoor suntanning is not obligatory. A prospective study found ultraviolet light exposure during indoor suntanning could cause significant microstructural changes to the cornea and the bulbar conjunctiva [367]. Identifying sports and recreation-associated risk factors will help in the development of injury prevention strategies to protect eye health.
3.7. Societal supports or societal pressures (see TFOS Elective Medications subcommittee report [144])
Disfiguring eye conditions have major impacts on psychosocial functioning. In a multicenter study, 10–49% of the patients with disfiguring eye conditions had high levels of psychosocial distress, evidenced by lower scores in standardized measures of anxiety, depression, appearance-related distress, and quality of life [368]. Similarly, almost 40% of ophthalmic clinic patients reported high levels of distress and dysfunction in relation to their appearance [369]. A prospective observational study in adolescents with manifest exotropia showed these individuals to experience abnormal scores on psychological distress evaluation scales and surgical correction significantly improved the outcomes of all these scales [370]. Patients wearing eye prosthetics tend to have a higher risk of depression, anxiety and stress, especially in employment, leisure and social functioning issues [371].
While appearance-changing diseases significantly impact mental health, cosmetic surgeries can improve personal wellbeing, self-esteem, and different aspects of daily life. A retrospective study found that blepharoplasty operations significantly improved quality of life for patients [372]. Cosmetic surgeries can impact ocular surface health (See TFOS Cosmetics Subcommittee Report). To create the appearance of a double eyelid, cosmetic blepharoplasty and double eyelid tapes have become popular in East Asian countries (TFOS Cosmetics Subcommittee Report [4]). Upper eyelid surgery results in a temporary decrease in ocular surface sensation that returns to baseline after one month [373]. Cosmetic double-eyelid blepharoplasty may temporarily affect tear film dynamics and aggravate dry eye symptoms in young female patients, which generally recover within 3 months [374]. Similar results were observed in patients undergoing cosmetic transcutaneous lower blepharoplasty, which affects the ocular surface and tear stability for three months [375]. Double eyelid tapes worn for two weeks can increase conjunctival staining, corneal staining, signs of meibomian gland dysfunction and incomplete blinking, and significantly decrease tear break-up time and intraocular pressure [376]. The association between cosmetic blepharoplasty and dry eye disease has been previously reviewed [374].
Botulinum toxin type A is an injectable neurotoxin that is widely used to treat eye diseases including strabismus, blepharospasm and facial wrinkles around the eyes (see TFOS Elective Medications [144] and TFOS Cosmetics Subcommittee [4] Reports). The impact of Botulinum toxin injection on the ocular surface is controversial, as periocular Botulinum toxin may cause dry eye disease through reduced lacrimal gland secretion and increased tear evaporation due to adverse events, such as eyelid malposition and abnormal blinking [345]. Conversely, injection in the medial eyelids can improve dry eye disease by decreasing tear drainage from the nasolacrimal duct [345].
3.8. Other determinants or choices
Cosmetic, sporting, occupational or other lifestyle preferences may influence an individual's choice to wear contact lenses (see TFOS Contact Lenses Subcommittee Report [377]) or undertake corneal refractive surgery (see TFOS Elective Medications Subcommittee Report [144]). Appearance concerns are more frequently reported by women than men and there is greater uptake of contact lens wear [378] with attendant ocular surface sequelae, and particularly complications associated with dry eye symptoms are more prevalent in females than males [378]. Women are also more frequent candidates for corneal refractive surgery than men [379] and more prone to iatrogenic dry eye disease following refractive or cataract surgery [380]. While such refractive choices may be associated with the development of ocular surface diseases, including dry eye disease [381], they may also exacerbate existing ocular surface diseases.
Eyelid tattooing is a popular cosmetic procedure for women in certain countries, although there are adverse effects on the ocular surface (See TFOS Elective Medications [144] and TFOS Cosmetic Subcommittee [4] Reports). These include a risk of direct mechanical trauma from the needle, which may conceivably cause damage to the meibomian glands. Meibomian gland loss, evidenced by a lower meiboscore, has been reported in those with eyelid tattoos [382]. Tattoo ink pigments persist as pigment granules in the epidermis and dermis [383]. Most of the residual pigment is located within the macrophages in the dermis and, focally, in the endomysial connective tissue of the superficial orbicularis oculi muscle [383]. Tattoo ink, particularly those containing para-phenylenediamine [384] or black henna [385] may induce contact dermatitis.
4. Living and working conditions
4.1. Unemployment
The rate of unemployment increases during economic downturns and financial crises and directly impacts physical and mental health of those affected [386]. Unemployment and retirement have been linked to various health problems, including dry eye disease [210,387]. This might be explained by the higher rate of ocular surface disease risk factors among unemployed individuals. For example, obesity [388], smoking [389], alcohol consumption [390], and depression [391] are more common among unemployed individuals. Over the past two years, the COVID-19 pandemic has impacted the global economy, including causing a rise in unemployment and related health problems [392]. Further studies are required to explore the impact of employment status on ocular surface health.
4.2. Type of occupation (see TFOS Environmental Subcommittee Report [7])
The nature of an individual's occupation may increase their risk of ocular surface disease in several ways [393]. Occupational exposure to chemicals, corrosives and excessive heat may cause acute or chronic ocular surface injury, which may result in devastating short and long-term complications [394,395]. Registry data in the USA from January 2013 to December 2017, indicates there are 13,181 newly diagnosed ocular burn cases each year, with a modest increase in prevalence over time [396]. Jobs that carry a higher risk of ocular surface burn include cleaners, miners, construction workers, laboratory staff, food service industry workers, agricultural workers, fire workers, and mechanics [397]. Factors associated with occupational ocular injury are lack of use of protective eyewear at time of injury, male sex, exposure to biological or chemical hazards and risk-taking behaviour [398].
In rural populations, open globe injuries are more commonly seen in association with agricultural occupations [399]. While ocular trauma is a well-established predisposing factor for infectious keratitis, particularly in rural and low income regions [62], ocular trauma due to agricultural injuries in farmers is associated with a higher risk of infectious keratitis [63].
Environmental factors such as sunlight and air pollution increase the risk of ocular surface diseases in outdoor workers compared with indoor workers [393,400,401]. Outdoor workers with prolonged sunlight exposure are at higher risk of developing pterygium and climatic droplet keratopathy [402,403]. One large scale study showed agricultural workers to have a lower risk of dry eye disease [393]. Certain indoor environments, such as those having low humidity and high levels of particulate matter of 2.5 μm or less, have been associated with dry eye symptoms [404]. The prevalence of dry eye disease in office workers with prolonged use of visual display terminals ranged between 9.5% and 87.5% [20,405]. This very wide range in prevalence has been attributed to the use of different diagnostic criteria in studies of dry eye disease [20].
Animal handlers might be at higher risk for developing ocular surface injuries. Keratitis and ophthalmia nodosa have been reported repeatedly following handling of Tarantula spiders, which have become popular pets [[406], [407], [408]]. Ocular surface chemical injuries following exposure to sheep, turkey, and fish bile have been reported in abattoir workers [[409], [410], [411]]. Ocular bee stings may occur as an occupational hazard in beekeepers or farmers and can cause severe corneal or conjunctival inflammation, especially if there is a retained stinger [[412], [413], [414]].
Since the emergence of the COVID-19 pandemic, working and studying from home and prolonged use of face masks have resulted in an increased prevalence of dry eye symptoms (see Section 8). Occupations that require longer screen time [393] and/or continued face mask use (see section 8) or a combination of both might conceivably be at higher risk for developing or worsening of dry eye disease. Working night shifts is another occupational risk factor which is associated with meibomian gland dysfunction, tear film instability and exacerbation of dry eye symptoms [415,416].
4.3. Water and sanitation
Reduced access to clean water and sanitation may increase the risk of ocular surface diseases, particularly in the context of trachoma. A systematic review of 47 studies found that access to sanitation was associated with less trachoma, as measured by the presence of trachomatous inflammation-follicular, trachomatous inflammation-intense or C. trachomatis infection [417]. Reduced odds of trachomatous inflammation, of either form, were also found with having a clean face, and at least once daily face washing, soap use and daily bathing practices [417]. Conversely, living within 1 km of a water source was not significantly associated with trachomatous inflammation or C. trachomatis infection [417]. In Ethiopia, where 77 million people live in trachoma-endemic areas, a systematic review of 29 studies investigating associations between trachoma and access to water supply, sanitation and face hygiene revealed that households with no toilet facilities, no access to improved water and the lack of daily face washing in children showed increased odds of exhibiting active trachoma [418].
There are many other ocular diseases that can be directly attributable to contamination of water bodies by various chemical and pathogens. These can occur through toxic, allergic, inflammatory or infective mechanisms [419]. Specific water-borne ocular infections include Acanthamoeba keratitis, Giardiasis, Toxoplasmosis, Gnathostomiasis, Coenurosis, Pseudomonas aeruginosa keratitis, Melioidosis, Leptospirosis, Toxocariasis, and Adenoviral disease [419], although some organisms are recognized to have additional environmental sources. Climate change will likely result in new hazards and water contaminants that may lead to further or changed ocular diseases [419].
4.4. Education and childhood education
Education and childhood education may impact the risk of ocular surface diseases. There is a well-established link between education and poverty, socioeconomic class and access to health services, which affects both the prevalence and severity of a range of both systemic diseases [420] and ocular diseases [421]. Education is linked to better nutrition and therefore health consequences. Likewise, ocular diseases may conceivably impact societal factors, particularly those diseases which affect the quality of vision and may impact academic performance.
Infectious keratitis is more common in those with a low educational level [[63], [64], [65]]. There is a strong association between a low education level and a higher risk of both poorer visual outcome and infectious corneal blindness [64,65]. Having a higher education diploma was associated with an increased risk of dry eye disease in a large population-based study in the Netherlands, which persisted after correction for age, sex and other possible confounding comorbidities [15]. A possible residual confounding factor in this relationship may be increased screen use with higher education occupations.
Reduced attention and concentration is reported in dry eye disease models [422], conceivably due to reduced blinking and resulting pathways to neural connections and brain stimulation, as well as diminished and variable optical performance in dry eye disease [423]. It could be argued that in the context of the increasing dominance of digital screens, eye strain and dry eye symptoms further increase, leading to a deeper lack of concentration and perpetuating this reduced performance cycle. There is evidence for increasing screen time and more time spent on remote education during the pandemic, with screen time reportedly doubling [424] (See sections 6, 7, 8, and the TFOS Digital Subcommittee Report [8]). Screen time has also been reported to be linked to dry eye symptoms in children [425], especially with the use of screens before bedtime [246] and higher screen times are associated with worse school performance [246]. While the mechanisms underlying these effects are unclear, it does appear that screen use is associated with dry eye disease and reduced academic performance [426]. Evidence for the influence of short-wave blue light on these diseases is limited and there is no evidence of the efficacy of protective devices [427,428].
4.5. Poverty and socioeconomic status
Socioeconomic status is an identifiable and well-reported societal factor contributing to the burden of ocular surface disease. There is a higher prevalence of a range of eye diseases in the homeless [429]. Neglected tropical diseases such as trachoma are highly prevalent in low- and middle-income countries and poorer individuals. The SAFE strategy (Surgery, Antibiotics, Facial Cleanliness and Environmental Improvement), proposed by the World Health Organization, includes many lifestyle modifications in endemic areas to eliminate trachoma. Several studies have demonstrated the efficiency of these strategies, however, the way of implementing them varies from study to study, as well as from region to region [417]. Several countries have developed intensive brigades, as well as prevention and control programs to target this disease. Implementing effective policies largely relies on targeting core groups and relevant societal factors in the remaining endemic areas, worldwide [430].
In addition to trachoma, fungal keratitis has a strong relationship with gross domestic product per capita of the region. A higher proportion of fungal keratitis compared with all infectious keratitis is strongly associated with low gross domestic product per capita [129]. Similarly, a low socioeconomic status and/or poverty are associated with a higher risk of infectious corneal blindness [64].
Evaluating and improving accessibility to ophthalmic diagnosis and treatment for all strata of society is important in improving treatable and preventable ocular surface diseases. Health economic analyses in ocular surface diseases are scarce, however, the great majority of them demonstrate interventions and treatments to be cost-effective [431]. Conceivably, the surge in uptake of telemedicine could prove to be a cost-minimizing alternative for screening and management of some ocular conditions [432], particularly for patients in remote areas or those lacking access to appropriate care.
4.6. Incarceration
Prison populations experience adverse health outcomes due to lack of access to services, delay in accessing appropriate care, limitations in nutrition and lack of awareness. Health and eye health outcomes may be further compromised due to the overlay of other societal factors, including the overrepresentation of marginalized groups in prisons, low education, and poverty [433] and may be exacerbated in regions with low gross domestic product per capita. There are limited studies of ocular surface disease in prison populations. Ocular surface conditions that are over-represented in prison populations include allergic conjunctivitis, pterygia and xeropthalmia [434]. In a cross-sectional study in a Kenyan prison population, 24% of male prisoners had xerophthalmia [435].
5. Regional/global socio-economic, cultural and environmental conditions (see TFOS lifestyle challenges [6] and TFOS Environmental Conditions Reports [7])
5.1. Remoteness/geography/seasonality (see TFOS Environmental Conditions Report [7])
Geographic location, social factors such as high- or low-income regions and remoteness influence access to eyecare services and the profile and severity of ocular surface diseases. In low-income countries, while there are no randomized controlled trials or systematic reviews that are powered to explore the prevalence of dry eye disease in urban and rural communities, the prevalence and severity of symptomatic dry eye disease, meibomian gland dysfunction and meibomian gland loss is higher in rural communities compared to urban areas [436,437]. Individuals living in rural areas experience more outdoor time, poorer hygiene, decreased access to medical facilities, inadequate amenities [438,439] and are predominantly farmers [436]. Such conditions predispose those in rural areas to ocular surface infections such as trachoma [417], eyelid disease and infections, meibomian gland loss and dry eye disease [436]. Other societal factors predominate in urban areas, including the use of digital devices, air conditioning and exposure to pollutants [436]. Dry eye disease is more common at high altitude [440], although there is considerable confounding with altitude and other weather conditions such as humidity (See TFOS Environmental Conditions Report [7]).
Rural and remote communities, particularly those which are home to Indigenous peoples, have greater morbidity and mortality rates from a range of health conditions and communicable diseases, including those related to skin, eye, and respiratory diseases, particularly in children [132]. Indigenous peoples are often marginalised and disadvantaged, with higher rates of poverty and remoteness to health care than non-indigenous populations. Most studies have evaluated blinding eye diseases, but there is also evidence for higher rates of ocular surface diseases, including trachoma and onchocerciasis [133]. Trachoma rates are significantly higher in Indigenous compared with non-Indigenous populations in Australia, with no evidence of a reduction in prevalence between 1993 and 2008 [132]. High rates of pterygium associated with visual impairment have been reported in Indigenous populations in Brazil [130,131].
Outdoor conditions are associated with variations in environmental factors including pollution, level of pollens, humidity levels, weather and seasonality, which influence the prevalence of ocular surface diseases [441], including dry eye [10], allergic eye disease [442] and ocular surface infections [62]. These associations are described in detail in the TFOS Environmental Conditions Report [7].
These seasonal variations may be due to increased pollen outdoors during spring and low indoor humidity during winter in the case of dry eye disease [441]. Allergic eye disease is more prevalent in warmer, tropical climates such as in Arabian, African, and some Asian countries [[443], [444], [445]]. Warm and dusty weather [445], elevated temperature and relative humidity in semi-tropical weathers, which increase growth of moulds and filamentous fungi indoors [446] and the wet rainy season have all been linked to allergic conjunctivitis [445] and dry eye disease [441]. Warm and dusty conditions are exacerbated, for example, during the harmattan season in West African countries, which carries dust via the northeast trade winds from the Sahara desert over West African countries [445].
Seasonal and geographic variations have been reported in ocular surface infections [[447], [448], [449], [450]] and there are wide regional differences in causative organisms and predisposing factors in infectious keratitis [62]. Warmer summer months appear to be associated with an increase in the reporting of infectious keratitis, and an increase in Gram-negative bacterial keratitis, particularly Pseudomonas sp [448,[451], [452], [453]]. Similarly the onset of Acanthamoeba keratitis appears to be higher in the summer and autumn months [454]. There is less evidence for a summer peak in the onset of Candida sp. keratitis [451]. Fungal keratitis appears to peak in hot windy climates in the tropics [455,456], surrounding the months of harvest in farming communities in India. The incidence of fungal disease is significantly higher in Asia and Africa than in other regions of the world [129]. Climate influences the rate and severity of contact lens-related infectious keratitis, with more severe disease caused by environmental organisms more common in tropical regions and with high daytime temperatures [457].
5.2. Availability of services (treatment/devices/practitioner education)
Many ocular surface diseases have significant morbidity, including vision loss, and these may require long term management and frequent follow-up care. Such conditions include severe dry eye disease, ocular chemical injuries, Stevens Johnson syndrome and ocular pemphigoid, and frequently require tertiary eye care for diagnosis and ongoing management. This is an issue for rural and low-income communities particularly, and the primary health care center is generally the first point of contact for rural patients. Barriers to accessing services and a delay in accessing appropriate treatment for a range of health conditions underpin the higher prevalence of, and increased severity of, disease in rural and low-income regions [458].
Non-sight threatening diseases including conjunctivitis, pterygium and dry eye are consistently ranked amongst the most common reasons for presentation at health facilities in low- and middle-income countries, in both pediatric and adult populations [[459], [460], [461], [462]].
5.3. Access to affordable services
In the World Report on Vision, the World Health Organization called for integrated people-centered eye care as part of universal health coverage, which includes quality essential health-care services and quality and affordable eye care [463]. A vertically running, stand-alone program focusing on a specific disease is no longer believed to be an effective approach. The World Report on Vision emphasizes strengthening primary eye care as an approach to achieve Universal Eye Health Coverage [463]. The World Health Organization defines universal eye health coverage as “ensuring that all people have access to required promotive, preventive, curative and rehabilitative health services, of sufficient quality to be effective, while also ensuring that people do not suffer financial hardship when paying for these services” [463]. This implies that all people should have access to the best quality health care without the risk of impoverishment. Universal eye health coverage should be comprehensive, equitable, of high quality, accessible, and affordable to all without any financial hardship. Corneal blindness fits within this directive and factors limiting access include socioeconomic characteristics, poverty, education, employment, sex, religion, caste, regional or geographical constraints, war and displacement.
Access to timely health services is the first step in achieving holistic health care. This involves the processes of eligibility to be allowed entry into the system, having an accessible health care location where the required services are available and enabling patients to source a health care provider that they trust and with whom they can communicate. Affordability is the ability of an individual to be able to cover the costs for health care within the parameters of their income. Thus, affordability of health services is determined by the cost of treatment as well as the ability of households to manage these costs, and their impact on the livelihood of household members [464].
Several reports have described a large variation in both the use and understanding of primary eye care from different regions and between various stakeholders. A good primary eye care program should ensure equity, community participation, inter-sectoral collaboration, and long-term sustainability for wider impact and healthy communities. However, the scope of primary eye care varies significantly throughout regions. While primary health workers provide primary eye care as one of their responsibilities in most parts of Africa, in high-income nations such as the UK, USA, Canada and Australia, it is provided by specialized personnel such as optometrists, who are independent eye care service providers in these countries.
In countries, such as India, in the government sector, primary eye care is provided by trained para-medical ophthalmic personnel located in primary health centers, who work in liaison with medical officers. In the private sector/non-governmental sector, trained ophthalmic personnel provide care, most of whom are termed ‘vision technicians’ [465]. In the government sector however, there are integrated primary health and eyecare networks through primary health centers as well as community centers; however, the government system, as a whole, is weak in implementation [466]. The next section describes an example of this approach as it applies in India, recognising that this is one of several models.
5.3.1. Model of vision centers in India
As an example of an approach to overcome barriers to affordability and accessibility in eye care, a proportion of non-government organizations have implemented universal eye health coverage through their primary eyecare network of vision centers. Vision centers in India operate in line with India's National Program for Control of Blindness (http://npcb.nic.in/). The specific objective of the National Program for Control of Blindness is to provide and improve upon basic and advanced eye care respectively in all parts of the country. Vision centers are permanent small eye care centres that are situated in remote areas, that allow the rural population to access eye care services within their community and which utilise the local resources available within the community to operate. Every vision center is manned by a well-trained technician and offers services that include refraction, basic ophthalmic examination, diagnosis of common ailments and referral as needed to a tertiary eye care institute attached to the vision center [467]. Vision centers are compact, with usually two or three rooms, and staffing that ranges from one to three staff to serve a target population of around 50,000 patients and is located within a 50 km radius of the base hospital, although this may be further, depending on the ease of accessing the base hospital [467].
Barriers to access to care in India have been particularly explored in the context of cataract surgery. These include economic or transportation issues [468,469], fear of surgery [470], and lack of awareness about the disease [468]. Vision centers provide immediate triage of patients, based on disease severity, and patients with moderate to severe ocular surface disease can be referred to referral centres for advanced management. Vision centers work with the patients, their families and community, arrange hospital transport and systematically aid in removing barriers that keep patients from surgery and/or advanced care, in a cost-effective manner.
Moreover, they improve health-seeking behaviour. Staff from within the local community are considered more approachable and accessible for those seeking health care. This prevents a delay in the referral of complex eye conditions and allows for follow-up closer to home, to monitor chronic ocular surface disorders without over-taxing the scarce services of the referral hospital, which are needed for more critical surgeries and care. Vision centers reduce dependency on outreach programs to transport patients, and result in better compliance, as well as follow-up care, in a financially sustainable fashion.
5.4. Culturally appropriate services, free of bias or discrimination
Eye care service utilization is a function of the availability, accessibility, affordability, and acceptability of services [463]. Cultural factors such as trust, perceptions of health, communication and language play a critical role in the acceptability of health services. Furthermore, distrust, racism, and discrimination can negatively influence the ability of some patients to seek care. For example, Indigenous peoples are more likely to access eye care if it is culturally appropriate and well-integrated within their community-based health service [471]. Similarly, higher levels of patient engagement and satisfaction have been reported when there is concordance in language and/or ethnicity (and in some cases gender) between patients and health care professionals [472]. In some cultures, gender-sensitivities arise when care is provided by a health care worker of the opposite gender [463].
In the context of ocular surface, culturally appropriate services are essential for elimination of trachoma in specific populations. In Australia, culturally safe and relevant health promotion resources have been developed with the aim to eliminate trachoma in remote Indigenous communities [473]. However, there is a need for more high-quality studies that provide insights on culturally relevant beliefs and practices [474,475].
5.5. Effect of sex and (trans) gender on access to services
Section 2.2 describes sex-related differences in the prevalence of various ocular surface diseases due to the impact of biology. The societal impact of sex or (trans) gender on ocular surface diseases may manifest as a lack of timely access to services for a range of reasons. Women in most low-income regions have worse visual impairment compared to their male counterparts [476] and the Lancet Global Health Commission on Global Eye Health reported 55% of global vision loss is experienced by women and girls and women are 8% more likely to be blind [477]. Several studies have demonstrated that women have more limited access to eye care services in certain regions [478,479]. Factors affecting the ability of women to seek eye care services include social and cultural factors, for example in some cultures women may not have freedom of mobility and lack independence to make decisions about their health. Women with childcare responsibilities may prioritise others before themselves for health and eye health including children, or their male counterparts [478]. Access to local female vision technicians, for example in the Indian vision center model, may improve uptake of services by females and help to reduce gender inequity.
There is evidence of discrimination and decreased access to health care services for transgender individuals in both developing and high-income countries [[480], [481], [482]]. Transgender individuals have reported discrimination from health workers, fear of rejection and stigma and financial constraints as factors hindering access to health care services in general, and to eye care services in particular [482].
5.6. Cost of diagnosis/treatment – insurance coverage/out of pocket expenses
The costs of diagnosis and management of ocular surfaces diseases and the bearer of these costs varies enormously by region. The cost of primary eyecare in some countries is borne by a public system but medical devices, surgical or medical therapies are variably subsidised [483]. Various means can be adopted in the public and private health sector to reduce the economic burden of health care to ensure that out-of-pocket expenses do not prevent the individual from accessing essential eye care services [[484], [485], [486]].
This in turn is largely determined by several factors, including per capita income, with high-income countries being able to spend more for out-of-pocket expenses [487]. From an individual perspective however, out-of-pocket expenditures for eye care services vary considerably within income groups, ranging from $32 in Sweden to $1200 in Switzerland in the high-income group, and from $6 in Madagascar to over $100 in Cambodia, Haiti, and Nepal in the low-income group [487]. Apart from the direct out-of-pocket expenses, the indirect costs borne by the individual tends to be equally impactful on the affordability of eye care. Ocular surface disorders, primarily those associated with dry eye disease or trichiasis, incur indirect costs, such as loss of earnings. These unaccounted-for factors generally underestimate the economic burden of the individual. In India, more than 80% of the total health care expenditure is borne through out-of-pocket expenses, primarily spent on purchase of medicines [488].
Apart from factors that differ across countries, interstate differences in financing and providing state of art health care in federated countries further contribute to widening the chasm of affordability among individuals.
5.7. Impact of climate change (see also TFOS lifestyle challenges [6]and TFOS Environmental Conditions Reports [7])
As with other possible factors which impact the ocular surface, changes in climate, air pollution and temperature affect the prevalence and severity of ocular surface disease [[489], [490], [491]]. Climate change and the resultant global warming and increased mean temperatures decreases crop yield [492]. This preferentially affects the poor and less privileged in society, especially in developing countries, leading to increased levels of food insecurity [493] (Section 3.1). The increased rate of natural disasters, continuous crop losses and loss of livelihood to farmers affected by these extreme weather conditions and their impact on agricultural yield adds to the very present threat to food security [492]. Such an effect on food security may impact children, increasing the prevalence of diseases associated with malnutrition such as vitamin A deficiency [494], and may compound other societal factors such as childhood education and poverty.
Climate change impacts water security and access to clean water as a direct consequence of flash flooding, heavy rainfall and precipitation, heatwaves and drought. These factors directly impact access to clean water and increase water pollution [495]. Climate change and the consequent rise in the frequency and severity of natural disasters, including floods, fires, drought and other extreme weather events, may disrupt services and amenities such as transportation network systems, which may decrease the ability of individuals to access health care services [496].
5.8. Conflict/displacement – refugee eye health, food and water security
Displacement and conflict affect physical, mental and emotional health [497]. Access to eye care services frequently has a low priority in crises such as war or displacement [498] and refugees are one of the most vulnerable groups for poor health outcomes. Blindness and visual impairment amongst refugees are significantly higher in displaced individuals than in other populations [[498], [499], [500]]. The prevalence of blindness in refugees varies widely depending on geographical location, from as low as 1.3% in Malawi [501], 11% in South Sudan [502], 21% in Uganda [500], and as high as 26% in Ethiopia [499]. In Canada and Australia, refractive error appears to be a leading cause of visual impairment in refugees [503,504]. The main causes of visual impairment in most of the refugee populations from the African continent includes cataracts, trachoma, glaucoma and refractive errors [499]. In a systematic review of causes of visual impairment in refugees internationally, trachoma was the leading infectious cause [505]. However, xerophthalmia resulting from vitamin A deficiency also appears to be common in refugee populations [500,506]. The prevalence of vitamin A deficiency among African refugees varies between 20.5% and 61.7% [507] and vitamin A deficiency is most prevalent in children and women. Displacement, poverty and war compound malnutrition and food security is vital to limit vitamin A deficiency and its blinding complications. Access to both adequate nutrition and sanitation would help to reduce the burden of ocular surface diseases in refugee populations.
5.9. Violence – war, acid attack, domestic violence, tear gas, rubber bullets
War and violent attacks may affect the eye and ocular health in several ways, most notably through ocular trauma from penetrating and perforating injuries to the cornea or globe, endophthalmitis, and secondary ocular infections [508]. While the need for protective eye wear has been advised in an effort to reduce the incidence of war-related eye injuries, there seems to be little evidence of mitigation in the rate of severe injuries [509], and it is noteworthy that open globe injuries are just as likely to occur as closed globe injuries from non-lethal weapons [510]. High morbidity in these situations is exacerbated by the destruction of hospitals during war time, compounding difficulties in accessing health care amidst serious sight-threatening and life threatening injuries [511]. This is especially relevant for ocular injuries, as surgical intervention is typically required for injuries from non-lethal weapons. Types of surgeries include lid, retinal detachment or globe repair, foreign body removal (including bullets) and evisceration [510]. Following the Syrian Civil war, approximately 57% of public hospitals were damaged, with 50% of their medical staff fleeing the country to safety [511]. Males tend to suffer greater eye injuries from war, however women and children are also affected [508]. Rubber bullets used by law enforcement may not be lethal in most cases, however they are known to cause ocular injuries such as lid lacerations, corneal tears, hyphema, and retinal detachment [512]. Projectile stones and pellets can cause traumatic ocular injuries with serious visual consequences [510]. In war or conflict situations, the combined effect of decreased security, inadequate access to health services and absence of health workers reduces access to eye care services, and diseases of the ocular surface are not given priority in these situations.
In addition to chemical injuries that may occur accidentally in the domestic setting, violent chemical attacks, such as acid attacks impact the ocular surface significantly and lead to significant epithelial loss, limbal ischemia, and even blindness [513]. In a hospital setting, of the 180 cases of chemical eye injuries reported, 19 cases were violent chemical injuries [514]. Assault represents 3.3–8.1% of ocular surface chemical injury cases in Finland and the UK [[514], [515], [516]], but 45.5% in Martinique [517] and 26%–83% in two retrospective Nigerian studies [518,519].
Chemical injuries significantly impact vision, quality of life, functional status and mental and physical well-being, resulting in considerable socioeconomic burden and psychological impact [394]. Injuries caused by alkaline chemicals cause saponification of ocular tissues, leading to deeper penetration and more extensive damage, while acids lead to protein coagulation within the ocular surface tissues preventing deeper penetration [520]. A systematic review has indicated that lengthy irrigation immediately after alkali burns with water is associated with better outcomes [521]. Other fluids suitable for irrigation are normal saline, lactated Ringer's solution, normal saline with sodium bicarbonate added, balanced salt solution, and diphoterine [521].
Inflammation of the ocular surface results in corneal and scleral shrinkage leading to increased intraocular pressure, corneal and conjunctival inflammation, loss of goblet cells, severe ocular surface dryness and scarring [522]. Surgical intervention is required in addition to medical therapy in more severe cases of ocular surface disease secondary to chemical burns, including amniotic membrane transplantation [523,524], limbal stem cell transplantation [522,525], penetrating keratoplasty or lamellar keratoplasty [522,526] and keratoprosthesis implantation [522]. Limited access to services following chemical injuries is associated with a poorer disease prognosis. A systematic review and meta-analysis indicated that surgery within a month of ocular burns to eyes, eyelids and eyelashes is likely to result in better long-term visual acuity, improved healing of epithelial defects and reduced limbal ischemia, however there may be a higher risk of infectious keratitis post-surgery [527].
Chemical injuries to the ocular surface may arise with other chemical agents used as riot control gases, such as chloroacetophenone, o-chlorobenzylidene malononitrile, and oleoresin capsicum [510,528]. These gases cause conjunctival congestion, corneal epithelial defects, corneal conjunctivalization, corneal vascularization and opacities and decreased vision [528].
Cases of violence are certainly not limited to war or law enforcement confrontation; domestic violence also leads to eye injuries from blunt trauma or even chemical injuries. About 45% of intimate partner violence is associated with ocular injury [529]. Injuries which may occur in cases of domestic violence include orbital fractures, closed globe injuries and chemical injuries such as intentional acid attacks (vitriolage) [530].
Vitriolage or vitriolic injuries, where acid or corrosive materials are used to maim, disfigure, torture or kill are associated with severe, permanent, disfiguring and incapacitating injuries with loss of tissue and organ function [531]. The motive behind vitriolage is largely an intent to cause long-term psychosomatic suffering from disfigurement, societal shaming and subsequent loss of identity. The perpetrators are commonly spurned suitors, disgruntled and violent domestic partners or business associates in dispute.
Vitriolage cases have been reported in the UK, Asia and Africa, although with the introduction of more stringent laws in Bangladesh, cases have been steadily decreased [531]. In neighbouring India and Pakistan, however, media reports indicate a disturbing increasing trend [532,533]. These numbers could be under representative due to underreporting in several instances related to fatal cases, subsequent suicide of the victim or fear of legal recourse [[533], [534], [535], [536]]. Preventive measures include effective advocacy of legislative changes to regulate acid sale, enforcement of stricter punishments for perpetrators, and opportunities for redress and provision of support for victims [531,535].
5.10. Access to/regulation of dangerous substances
Ocular surface chemical injuries in children including conjunctivitis and keratitis have been attributed to leaking or burst detergent pods, particularly in children under 5 [[537], [538], [539]], lye, sodium hydroxide, accidental exposure to cleaning products, and residues from domestic products used by other household members, such as deodorants and perfumes [[540], [541], [542], [543]].
Of 134 cases of ocular surface chemical injuries in children in India, 65% were caused by rupture of packets of ‘chuna’, a calcium hydroxide paste mixed into chewing tobacco where the alkaline contents caused ocular surface damage [541]. Similarly, alkali injuries due to exposure to calcium hydroxide during betel nut chewing have also been reported as important causes of ocular injury [544].
6. Information communication and technology – health communication
Digital technology can impact ocular diseases through effects on physical and mental health, health communication and access to services, in both positive and negative manners. For example, personalised medicine, telehealth, practitioner and patient education and connectedness of health care facilitated by digital technology and information communication may enhance diagnosis and management of disease. Conversely there may be physical impacts of the digital environment (See TFOS Digital Subcommittee Report [8]) and social impacts due to isolation, self-image perception and misinformation, which may depend on the type and degree of usage, age of consumer and underlying physical and mental health status.
6.1. Impact on mental, physical and social health
The speed and ease of information communication in the digital era has changed the way in which consumers access information, which may significantly impact mental, physical and social health.
Younger people increasingly use social media, thus may be at a higher risk of impact. Both screen viewing and mobile phone use may contribute to the development of depressive symptoms in young adolescents [545]. A cross-sectional study from Norway indicated that self-presentation in social media was associated with increased mental health problems and decreased quality of life in adolescents [546]. Two cross-sectional studies have similarly indicated that older adults may experience depression and reduced quality of life associated with different types of media exposure and the degree of usage [547,548]. Conversely, older adults may derive benefits, including reduced loneliness and the building of social connections in both assisted and independent living communities [549], which may positively impact ocular surface diseases.
Self-image perception can be influenced by social media use. Taking ‘selfies’ can be associated with significant increased social anxiety, decreased self-confidence and an increased desire to undergo cosmetic surgery [550]. In a cross-sectional study, prolonged exposure to social media, especially cosmetic surgery–related material, is associated with an increased likelihood of considering cosmetic procedures in the future [551].
6.2. Patient- and practitioner specific issues which impact access to care
The digital population as of January 2023 was over five billion internet users worldwide or approximately 63% of the global population [552]. Likely due to the ease of access and convenience, patients are increasingly utilizing and searching the Internet for healthcare information, which can affect interactions between patients and their doctors in both a positive and negative way. A national survey in 2013 showed approximately one in three American adults having used the internet to search for a medical condition for diagnosis [553]. Less than half of those searching (46%) report that the information discovered on the internet led them to seek the attention of a medical professional, whereas 38% reported taking care of the medical condition at home. While this broad survey was not based on ocular conditions specifically, it is apparent that access to health care information via the internet can influence whether a patient presents to a clinician for advice. This same survey reported that 72% of internet users used the medium to search for health information online. However, a survey from Canada revealed that most patients value a physician's advice and opinion over information found on the internet [554]. Peer interaction through advocacy and social media groups may provide patient support and assist with feelings of isolation, although there is limited evidence to confirm this.
With digital access, telemedicine, or the ability for a physician to provide care remotely without an in-office visit becomes available [555]. While patients generally view telemedicine as a favourable modality due to elimination of the need for travel and improved ability to be able to communicate with a provider, the opinion of physicians is less definitive, with a perception of superior overall quality for in-person visits, which may in part be due to a lack of experience with telehealth [556]. Education, guidelines and technological support through professional organisations may help to facilitate this approach.
7. Impact of the COVID-19 pandemic (see TFOS lifestyle challenges [6]and TFOS environmental conditions subcommittee [7] reports)
The impact of the COVID-19 pandemic and associated precautionary measures, including wearing of masks or protective equipment, online work and education and limited mobility and travel, on ocular surface diseases and societal factors, including mental health and access to eyecare services was explored in publications between January 2020 and January 2022.
7.1. Mental health
The prevalence of mental illness has increased during the pandemic, specifically depression, anxiety and harmful behaviors [381]. Social isolation and loneliness may underpin these adverse psychiatric co-morbidities [381], along with reduced access to appropriate services, which may increase the risk or severity of ocular surface disease, including dry eye disease. A large longitudinal study in the UK has shown that the effects of the pandemic and associated precautionary measures on mental health differ by demographic and social factors [557], which may help to identify populations most vulnerable to pandemic-related sequalae.
Medical treatments for mental health conditions including antipsychotic drugs such as phenothiazines and lithium, and tricyclic antidepressants, have themselves been linked to abnormal ocular surface pigmentation, corneal edema, eye irritation, ocular itching, reduced tear break-up time, and decreased lacrimation [558,559] (See TFOS Lifestyle Challenges Subcommittee Report [6]).
7.2. Access to services
During the pandemic many clinics were forced to close due to government or state mandates, limiting access to services for those with ocular surface disease [560,561]. A reduction in the number of eye exams being performed and postponement of visits for comprehensive eye exams and follow ups for management of chronic eye conditions, likely negatively affected the eye health of many patients [562]. In the United Kingdom, it is estimated that more than 10,000 patients at risk of sight-threatening macular disease missed out on essential eye care [562].
During the pandemic, the demand for telemedicine increased, such that virtual visits increased by 257%–700% [563]. While virtual visits directly benefited some patients, for others requiring a more thorough examination of the ocular surface, for example, telemedicine may have had less direct benefit, although it may have helped to triage these patients.
The pandemic confirmed that utilization of telehealth in eye care may not increase access to care for all patient types and groups. A retrospective study analyzed clinical visits at a university eye care center in 2020 during the pandemic and evaluated patient variables associated with the use of telehealth [564]. Male, black, older, non-English speakers and those with no more than a high school education were less likely to choose telehealth in preference to in-person visits.
8. Systematic review of the impact of the COVID-19 pandemic on the frequency and severity of ocular surface diseases
8.1. Introduction
The COVID-19 pandemic has exerted a profound influence on society and people's lives due to either the disease itself, the conditions that arose from the disease, or the public health measures and their psychological and societal consequences. COVID-19 infection and the pandemic have affected the systemic health of the population. There is also the possibility that specific body systems, such as that of the eye, are affected. In particular, the ocular surface, may be vulnerable to COVID-19 infection and associated consequences.
Studies have described both direct and indirect impacts of COVID-19 on several aspects of the ocular surface [[565], [566], [567], [568], [569], [570], [571]], including ocular surface manifestations of COVID-19 or related conditions, such as long COVID and multisystem inflammatory syndrome in children and adults following COVID-19 infection. Development or progression of ocular surface diseases secondary to (1) various public health measures, such as face mask wearing, eye protection, hygiene practices (such as use of hand sanitizer and other disinfectants, ultraviolet C disinfection), vaccinations; lockdowns, isolation, quarantine, physical distancing, online learning, and working from home; (2) therapeutic interventions, such as high-dose steroids, ventilation, and other intensive care unit care; (3) emotional and behavioral consequences of the pandemic, such as mental health problems, sleep disturbances, restricted access to medical services, poor compliance to treatments, telehealth, and the economic downturn (See Section 7).
The objective of this systematic review was to summarize the impact of the COVID-19 pandemic on the frequency and severity of ocular surface diseases, both the impact of COVID-19 pandemic on the general population (with or without baseline ocular surface diseases), and among those who had COVID-19 infection.
8.2. Methods
The systematic review was prospectively registered through PROSPERO (CRD42022299681) and was conducted by 6 authors of this report (TL, RQ, KL, YL, DR, FS).
8.2.1. Eligibility criteria
The review included studies of human populations from any country or region affected by the COVID-19 pandemic, without restriction by age, sex, race, or other factors. The study populations were not required to have baseline ocular surface diseases. The exposures of interest included the direct impact of COVID-19 infection on ocular surface diseases, as well as COVID-19 pandemic related public health measures (face mask wearing, lockdown, vaccination) and their societal consequences (increased remote learning, digital device use and screen time). Comparators could include no COVID-19 infection, a period prior to the COVID-19 pandemic, or a lower exposure to the same COVID-19 related public health measures and their societal consequences. Outcomes of interest included incidence, prevalence, and severity of ocular surface disease-related diagnoses, signs, or symptoms at any time point. There was no restriction related to the study context/settings. Eligible studies could be population-, hospital-, clinic-, community-, school-, or university-based.
Published primary comparative studies with at least 50 participants overall, were included. Comparative studies could utilize a cohort, a case-control, a cross-sectional (including survey), or a pre-post design. Studies without a comparison group or a comparison period were excluded. There was no restriction regarding how studies controlled for potential confounders or how the between group comparison was made. Studies that assessed hospital, emergency room, or healthcare utilization (even when a comparison with a pre-COVID period was made) were also ineligible because these studies did not provide direct measures of the frequency or severity of ocular surface disease. Studies that did not report any ocular surface disease-related outcomes were excluded as were conference abstracts and narrative reviews.
8.2.2. Search strategy
Given that the topic concerns the COVID-19 pandemic, PubMed was searched from January 1, 2019 to December 14, 2021 and Embase from January 1, 2019 to January 4, 2022 without language restrictions. With input from experienced information specialists, the search strategies were designed to include MeSH (for PubMed) or Emtree (for Embase) controlled-vocabulary terms, along with free-text words, related to COVID-19 and various ocular surface diseases. Appendix 1 includes the full search syntaxes for both databases. Reference lists of the included studies or for unpublished studies were not searched.
8.2.3. Study selection
The PubMed and EMBASE search results were imported into Covidence (Veritas Health Innovation, Melbourne, Australia) and duplicates were removed before screening. After pilot testing, two authors independently screened each title/abstract and then each full text report for potentially eligible studies. At both stages, discrepancies were resolved through discussion and/or consultation with a third author.
8.2.4. Data extraction and risk of bias assessment
A Google form was used for data extraction and risk of bias assessment. For each included study, one author extracted data and a senior author verified the data including study topic, objective, main conclusion, study design, study location, study population, details about exposure and comparator, and ocular surface disease-related outcomes and results.
For risk of bias assessment, domains from the Newcastle-Ottawa Scale were used to assess: (1) risk of selection bias in cohort and case-control studies (or the representativeness of the sample in cross-sectional studies); (2) risk of bias in the measurement of exposures; (3) risk of bias in the measurement of outcomes; and (4) risk of bias due to confounding [572]. Risk of bias was assessed by two senior authors using single extraction and verification. Discrepancies were resolved through discussion.
8.2.5. Syntheses
The following study characteristics were summarized, study design features, study participant characteristics, descriptions of exposures, outcomes, results, and risk of bias. Although planned, it was not possible to conduct any meta-analysis because of the heterogeneity in study designs, populations, and outcomes. The wide range of outcomes and inadequacy in reporting of many also prohibited calculation of effect sizes or other meaningful quantitative summaries. Consequently, studies that were similar were grouped and the evidence was qualitatively synthesized, following published guidance [573]. The certainty of the body of evidence was not graded.
8.2.5.1. Results
Fig. 2 shows the PRISMA flow diagram for this systematic review. The database searches yielded 9338 unique records. After screening 129 full-text reports, 40 studies were included in this systematic review [424,425,[574], [575], [576], [577], [578], [579], [580], [581], [582], [583], [584], [585], [586], [587], [588], [589], [590], [591], [592], [593], [594], [595], [596], [597], [598], [599], [600], [601], [602], [603], [604], [605], [606], [607], [608], [609], [610], [611]]
Fig. 2.
PRISMA flow diagram.
Table 1 presents a summary of the study characteristics. Individual study characteristics are presented in Appendix 2. The studies included covered four broad topic areas: effects of increased digital device use, screen time, and online classes on ocular surface diseases (n = 14, 35%); effects of face masks and other personal protective equipment on ocular surface diseases (n = 10, 25%); effects of COVID-19 infection on the frequency and severity of ocular surface diseases (n = 11, 28%); and effects of COVID-19 pandemic related public health measures (such as social distancing, vaccination) and hygiene practices (such as hand-sanitizer use) on ocular surface diseases (n = 5, 12%). Twenty-six (65%) studies utilized a cross-sectional design; only eight (20%) and one (3%) respectively used a cohort or case-control design. The remaining five studies (13%) were retrospective chart reviews.
Table 1.
Characteristics of studies included in the systematic review.
| Characteristic | n | (%) |
|---|---|---|
| Study topic | ||
| Effects of digital device use, screen time, and online classes on ocular surface diseasesc | 14 | (35%) |
| Effects of face masks and other personal protective equipment on ocular surface diseases | 10 | (25%) |
| Effects of COVID-19 on the frequency and severity of ocular surface diseases | 11 | (28%) |
| Effects of COVID-19 pandemic related public health measures and hygiene practices on ocular surface diseases | 5 | (13%) |
| Study design (excluding healthcare utilization: n = 40) | ||
| Cross-sectional (survey or non-survey) | 26 | (65%) |
| Cohort | 8 | (20%) |
| Case-control | 1 | (3%) |
| Retrospective chart review | 5 | (13%) |
| Location of study | ||
| India | 7 | (18%) |
| Italy | 6 | (15%) |
| Turkey | 6 | (15%) |
| United States | 4 | (10%) |
| China | 4 | (10%) |
| Spain | 2 | (5%) |
| Other (single study each) a | 11 | (28%) |
| Study population | ||
| COVID-19 patients (current or recovered) | 7 | (18%) |
| General patients | 6 | (15%) |
| General public | 6 | (15%) |
| College/university students | 6 | (15%) |
| Children (<18) | 4 | (10%) |
| Healthcare workers | 3 | (8%) |
| Other b | 8 | (21%) |
| Number of participants (total reported n across 38 studies = 19,841) | median | (IQR) |
| Total number of participants | 236 | (109,439) |
| Exposure group (among studies assessing and reporting separate exposures and controls (n = 14)) | 64 | (33,127) |
| Control group (among studies assessing and reporting separate exposures and controls (n = 14)) | 62 | (39,91) |
Chile, Croatia, Egypt, France, Germany, Japan, Portugal, Romania, Russian Federation, Saudi Arabia, United Kingdom.
Patients with previous diagnosis of Sjogren syndrome, dry eye disease, photokeratitis, or pollen allergy; Students and the general public; Contact lens wearers; Individuals receiving COVID tests.
COVID-19: coronavirus disease 2019, sd: standard deviation.
The included studies were conducted across multiple countries; India, Italy, Turkey, USA, China, and Spain contributed more than one study. One survey study had participants from multiple countries [424]. The study populations were variable, including COVID-patients, general (non-COVID) patients, public, college/university students, children, and healthcare workers. 19,841 participants were studied across all included studies (median = 237, interquartile range: 110 to 439). A wide range of outcomes were measured in these studies, including clinical tests (for example, tear break-up time), self-reported symptoms and events (for example, dryness, redness, eye pain), and patient-reported questionnaires (such as the ocular surface disease index).
Table 2 shows the results of the risk of bias assessment. In summary, 9/40 (23%) studies were rated at high risk of bias, 25/40 (63%) were rated at moderate risk of bias, and the remaining 6/40 (15%) were rated at low risk of bias. For all studies, the assessment of exposure and outcome were judged to be either free from bias or somewhat free from information bias, although one can argue that self-reported exposure and/or outcome information could be subject to inaccurate or biased recall. The study sample selection and representativeness were often unclear or not free from bias and very few studies adjusted for potential confounders in their analysis. Consequently, the association not being free from confounding was another major cause for increasing the overall risk of bias to moderate or high.
Table 2.
Risk of bias assessments for studies included in the systematic review (n = 40).
| Was the sample representative (cross-sectional studies)? | Was the study sample free of selection bias (other study designs)? | Is the assessment of exposure free from information bias? | Is the assessment of outcome free from information biases? | Is the association examined free from confounding? | Overall Risk of Bias (RoB) |
|---|---|---|---|---|---|
| Cross-sectional studies | |||||
| Cartes 2022 [580] | Yes | Somewhat | Somewhat | Yes | Low RoB |
| Li 2022 [610] | Yes | Somewhat | Somewhat | Somewhat | Low RoB |
| Saldanha 2021 [424] | Yes | Yes | Somewhat | Somewhat | Low RoB |
| Alabdulkader 2021 [578] | No | Somewhat | Somewhat | Somewhat | Moderate RoB |
| Bahkir 2020 [575] | Somewhat | Yes | Somewhat | No | Moderate RoB |
| Bitirgen 2021 [576] | Unclear | Yes | Yes | No | Moderate RoB |
| Boccardo 2021 [577] | No | Somewhat | Somewhat | Somewhat | Moderate RoB |
| Bozkurt 2021 [579] | Unclear | Yes | Yes | No | Moderate RoB |
| Galindo-Romero 2021 [582] | No | Somewhat | Somewhat | No | Moderate RoB |
| Gangaputra 2020 [584] | Somewhat | Yes | Somewhat | No | Moderate RoB |
| Ganne 2021 [585] | Somewhat | Somewhat | Somewhat | Somewhat | Moderate RoB |
| Garcia-Ayuso 2021 [27] | Somewhat | Somewhat | Somewhat | Somewhat | Moderate RoB |
| Krolo 2021 [586] | Yes | Somewhat | Somewhat | No | Moderate RoB |
| Kuroyedov 2020 [587] | Unclear | Somewhat | Somewhat | No | Moderate RoB |
| Martinez-Perez 2021 [592] | Unclear | Yes | Somewhat | No | Moderate RoB |
| Mengi 2022 [594] | No | Yes | Somewhat | No | Moderate RoB |
| Pardhan 2020 [599] | No | Yes | Somewhat | No | Moderate RoB |
| Shah 2021 [605] | Somewhat | Somewhat | Somewhat | No | Moderate RoB |
| Wang 2021 [608] | Somewhat | Somewhat | Somewhat | No | Moderate RoB |
| Elhusseiny 2021 [425] | No | No | No | No | High RoB |
| Long 2020 [589] | No | Somewhat | Somewhat | Unclear | High RoB |
| Nivedetha 2020 [596] | Unclear | Somewhat | Somewhat | No | High RoB |
| Oruc 2020 [597] | No | Somewhat | Somewhat | No | High RoB |
| Pavithra 2020 [600] | Unclear | Somewhat | Somewhat | No | High RoB |
| Serban 2021 [604] | No | Yes | Somewhat | No | High RoB |
| Usgaonkar 2021 [607] | No | Somewhat | Somewhat | No | High RoB |
| Cohort studies | |||||
| Acet 2021 [574] | Unclear | Yes | Yes | No | Moderate RoB |
| Gambini 2021 [583] | Somewhat | Yes | Yes | No | Moderate RoB |
| Mastropasqua 2021 [593] | Unclear | Somewhat | Yes | No | Moderate RoB |
| Ozturk 2021 [598] | Unclear | Somewhat | Yes | No | Moderate RoB |
| Rokohl 2020 [601] | Yes | Yes | Somewhat | No | Moderate RoB |
| Sarkar 2021 [602] | Somewhat | Yes | No | No | Moderate RoB |
| Maniaci 2021 [590] | Unclear | Somewhat | Somewhat | No | High RoB |
| Scalinci 2021 [603] | Unclear | Somewhat | Yes | No | High RoB |
| Retrospective chart reviews | |||||
| Lavista 2021 [483] | Yes | Yes | Yes | Somewhat | Low RoB |
| Martin 2021 [591] | Yes | Yes | Yes | No | Low RoB |
| Wang 2021 [609] | Yes | Yes | Yes | No | Low RoB |
| Negishi 2021 [595] | Somewhat | Yes | Yes | Somewhat | Moderate RoB |
| Silkiss 2021 [606] | Yes | Yes | Yes | No | Moderate RoB |
| Case-control studies | |||||
| D'Amico Ricci 2021 [581] | Somewhat | Somewhat | Yes | No | Moderate RoB |
Table 3a, Table 3b, Table 3c, Table 3da-3d presents the results from included studies by topic. Meaningful duration of use could not be extracted and presented for any exposure due to inconsistent reporting and different measures of “increased” use (for example, different categorizations, continuous estimated time, dichotomized “increase” in time, etc.). Narratively, during the COVID-19 pandemic, increased screen time, digital device use, or online classes resulted in new symptoms of dry eye disease in participants and worsening of ocular surface disease-related signs and symptoms across all age groups (Table 3 a). Prolonged use of digital devices and associated digital eye strain exacerbated signs and symptoms of existing dry eye disease. The overall number and severity of symptoms was positively associated with the duration of screen time. Despite the findings being consistent, most of these studies were based on surveys of students or the public recruited from the Internet; these samples were selective in nature and their responses were subject to inaccurate or biased recall.
Table 3a.
Results from studies of the effects of screen time, digital device use, or online classes on ocular surface diseases (n = 14).
| Study outcomes (n = # studies with that outcome) | Improved with exposure |
No change with exposure |
Worsened with exposure |
|||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| ‘Digital eye strain’ or ‘computer vision syndrome’ symptoms a (n = 7) | 0 | (0%) | 0 | (0%) | 7 | (100%) |
| Dry Eye Symptom Questionnaires b (n = 3) | 0 | (0%) | 0 | (0%) | 3 | (100%) |
| Ocular Surface Disease Index (n = 2) | 0 | (0%) | 0 | (0%) | 2 | (100%) |
| Tear Break Up Time (n = 1) | 0 | (0%) | 0 | (0%) | 1 | (100%) |
| Central Corneal Thickness (n = 1) | 0 | (0%) | 1 | (100%) | 0 | (0%) |
| Single Ocular Surface Disease Symptoms and Events | ||||||
| Dryness (n = 4) | 0 | (0%) | 0 | (0%) | 4 | (100%) |
| Redness (n = 4) | 0 | (0%) | 1 | (25%) | 3 | (75%) |
| Eye pain (n = 4) | 0 | (0%) | 1 | (25%) | 3 | (75%) |
| Tearing/watering (n = 4) | 0 | (0%) | 1 | (25%) | 3 | (75%) |
| Blurred vision (n = 4) | 0 | (0%) | 2 | (50%) | 2 | (50%) |
| Itching (n = 3) | 0 | (0%) | 1 | (33%) | 2 | (66%) |
| Aching/sore eyes (n = 2) | 0 | (0%) | 0 | (0%) | 2 | (100%) |
| Excessive blinking (n = 2) | 0 | (0%) | 1 | (50%) | 1 | (50%) |
| Burning sensation (n = 2) | 0 | (0%) | 1 | (50%) | 1 | (50%) |
| Sensitivity to light (n = 2) | 0 | (0%) | 1 | (50%) | 1 | (50%) |
| Tired eyes (n = 1) | 0 | (0%) | 0 | (0%) | 1 | (100%) |
| Double vision (n = 1) | 0 | (0%) | 0 | (0%) | 1 | (100%) |
| Gritty eyes (n = 1) | 0 | (0%) | 0 | (0%) | 1 | (100%) |
| Excessive rubbing of eyes (n = 1) | 0 | (0%) | 0 | (0%) | 1 | (100%) |
| Eye strain (n = 1) | 0 | (0%) | 0 | (0%) | 1 | (100%) |
| Foreign body sensation (n = 1) | 0 | (0%) | 0 | (0%) | 1 | (100%) |
| Heavy eyelids (n = 1) | 0 | (0%) | 0 | (0%) | 1 | (100%) |
Feeling of a foreign body, blurring of vision, excessive blinking, itching, dryness of eyes, burning, watering of eyes, redness of eyes, eye pain.
m-SPEED, Dry Eye Questionnaire - 5, Overall “dry eye symptoms".
Table 3b.
Results from studies of the effects of facemasks and other personal protective equipment on ocular surface diseases (n = 10).
| Study outcomes (n = # studies with that outcome) | Improved with exposure |
No change with exposure |
Worsened with exposure |
|||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| Ocular Surface Disease Index (Continuous - Score) (n = 3)* | 1 | (25%) | 1 | (25%) | 2 | (50%) |
| Ocular Surface Disease Index (Binary - Symptomatic) (n = 1)* | 2 | (100%) | ||||
| Dry Eye Symptom Questionnaires a (n = 2) | 2 | (100%) | ||||
| Overall Ocular Symptoms b (n = 2) | 2 | (100%) | ||||
| Schirmer Test I (n = 2) | 2 | (100%) | ||||
| Central Dendritic Cell Density (n = 1) | 1 | (100%) | ||||
| Fluorescein and Lissamine Green Staining (n = 1) | 1 | (100%) | ||||
| Tear Break Up Time (n = 1) | 1 | (100%) | ||||
| Allergic ocular symptoms (n = 1) | 1 | (100%) | ||||
| Single Ocular Surface Disease Symptoms and Events | ||||||
| Dryness (n = 1) | 1 | (100%) | ||||
| Eye discomfort (n = 1) | 1 | (100%) | ||||
| Blurred vision (n = 1) | 1 | (100%) | ||||
| Foreign body sensation (n = 1) | 1 | (100%) | ||||
| Need to remove contact lenses (n = 1) | 1 | (100%) | ||||
| Chalazion (n = 1) | 1 | (100%) | ||||
*One study examined ODSI as continuous and binary for two different exposures.
Dry Eye related Symptoms (DEQS), Dry Eye Symptoms Overall.
“Overall ocular symptoms” include: itching, tearing, and redness.
Table 3c.
Results from studies of the effects of COVID-19 infection on ocular surface diseases (n = 11).
| Study outcomes (n = # studies with that outcome) | Improved with exposure |
No change with exposure |
Worsened with exposure |
|||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| Tear Break-Up Time (n = 4) | 2 | (50%) | 2 | (50%) | ||
| Overall Ocular Symptoms a (n = 2) | 2 | (100%) | ||||
| Ocular Surface Disease Index (Continuous - Score) (n = 2) | 1 | (50%) | 1 | (50%) | ||
| Schirmer Test II (n = 2) | 1 | (50%) | 1 | (50%) | ||
| Corneal staining (n = 2) | 2 | (100%) | ||||
| Non-invasive First Tear Break-Up Time (n = 1) | 1 | (100%) | ||||
| Tear film damage (n = 1) | 1 | (100%) | ||||
| Tear osmolarity (n = 1) | 1 | (100%) | ||||
| Conjunctival impression cytology | ||||||
| Conjunctival hyperemia (n = 1) | 1 | (100%) | ||||
| Nelson classification (n = 1) | 1 | (100%) | ||||
| Tseng classification (n = 1) | 1 | (100%) | ||||
| Nucleus to cytoplasm ratio (n = 1) | 1 | (100%) | ||||
| Neutrophil presence (n = 1) | 1 | (100%) | ||||
| Lymphocyte presence (n = 1) | 1 | (100%) | ||||
| Corneal confocal microscopic parameters | ||||||
| Corneal nerve branch density (n = 1) | 1 | (100%) | ||||
| Corneal nerve fiber density (n = 1) | 1 | (100%) | ||||
| Corneal nerve fiber length (n = 1) | 1 | (100%) | ||||
| Single Ocular Surface Disease Symptoms and Events | ||||||
| Itching/irritation (n = 3) | 1 | (33%) | 2 | (66%) | ||
| Painful/sore eyes (n = 3) | 1 | (33%) | 2 | (66%) | ||
| Foreign body sensation (n = 3) | 1 | (33%) | 2 | (66%) | ||
| Red eyes (n = 3) | 1 | (33%) | 2 | (66%) | ||
| Conjunctivitis (n = 3) | 1 | (33%) | 2 | (66%) | ||
| Dryness (n = 2) | 1 | (50%) | 1 | (50%) | ||
| Epiphora (n = 2) | 1 | (50%) | 1 | (50%) | ||
| Blurred vision (n = 2) | 2 | (100%) | ||||
| Eye swelling (n = 1) | 1 | (100%) | ||||
| Burning sensation (n = 1) | 1 | (100%) | ||||
| Watery eyes (n = 1) | 1 | (100%) | ||||
| Mucous discharge (n = 1) | 1 | (100%) | ||||
| Changes in the eyelids (n = 1) | 1 | (100%) | ||||
| Gritty eyes (n = 1) | 1 | (100%) | ||||
“Overall ocular symptoms” include: burning sensations, itching, watering, mucoid and purulent discharge, photophobia, foreign body sensation, conjunctival swelling, eyelid swelling, feeling of pressure, double images, metamorphopsia, redness, reduced visual acuity, and pain.
Table 3d.
Results from studies of the effects of public health measures and hygiene practices on ocular surface diseases (n = 5).
| Study outcomes (n = # studies with that outcome) | Improved with exposure |
No change with exposure |
Worsened with exposure |
|||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| Overall Ocular Symptoms a (n = 1) | 1 | (100%) | ||||
| Single Ocular Surface Disease Symptoms and Events | ||||||
| Dryness (n = 1) | 1 | (100%) | ||||
| Use of artificial tears (n = 1) | 1 | (100%) | ||||
| Corneal ulceration (n = 1) | 1 | (100%) | ||||
| UV keratitis (n = 1) | 1 | (100%) | ||||
| Ocular injury due to hand sanitizer (n = 1) | 1 | (100%) | ||||
| Nonallergic conjunctivitis emergency department visits (n = 1) | 1 | (100%) | ||||
| Corneal abrasion emergency department visits (n = 1) | 1 | (100%) | ||||
| Eye pain (n = 1) | 1 | (100%) | ||||
| Losing access to dry eye treatments (n = 1) | 1 | (100%) | ||||
“Overall ocular symptoms” include: dryness, burning, itching, foreign body sensation, frequent and/or rapid blinking, sensitivity to light, watering, redness, ocular tiredness/fatigue, eye pain, difficulty keeping eyes open because of symptoms, blurry vision, fluctuating vision, eye symptoms interfered with screen use, reading, or work.
Similarly, prolonged and consistent face mask wearing negatively affected people with dry eye, as evidenced by increased ocular surface inflammation; decreased Schirmer scores; decreased tear break-up time; increased dryness, discomfort, foreign body sensation, contact lens intolerance, and other patient-reported symptoms (Table 3 b). However, face mask use reduced nasal and ocular allergic symptoms among individuals with pollen allergy, likely due to the protection provided by face masks against exposure to the airborne allergen. The risk of bias in these studies seems to be acceptable.
Although many primary studies and systematic reviews on the ocular surface manifestations of COVID-19 infection were identified in the searches, most were excluded due to an absence of a comparison group. Of the 11 included studies that examined the effects of COVID-19 infection on ocular surface diseases (Table 3 c), the findings were mixed as to whether there was any association between COVID-19 infection and conjunctivitis (infectious, non-infectious, and non-specific types). Studies revealed that, compared with healthy controls, COVID-19 positive patients reported ocular surface symptoms more frequently and may have impaired stability of the tear film. COVID-19 patients reported soreness and dryness of their eyes and the severity of symptoms seemed to be correlated with the severity of the infection. Of note, most of these studies did not adequately control or adjust for confounding factors (such as age, sex, other comorbidities).
The remaining studies summarized an increased trend of pediatric eye exposures to alcohol-based hand sanitizers, increased incidence of photokeratitis due to UV lamp exposure, and the effects of public health measures on ocular surface diseases and changes in internet searching patterns about conjunctivitis (Table 3 d). One survey showed that individuals with moderate dry eye disease, particularly those with Sjögren syndrome, may disproportionately experience consequences of increased eye strain and individuals with severe dry eye disease may disproportionately experience reduced access to dry eye treatments.
8.3. Discussion
During the ongoing COVID-19 pandemic, a growing body of evidence has described the impact of COVID-19 on ocular surface health. In this systematic review, 40 comparative studies of various exposures related to the COVID-19 pandemic were identified. Most studies reported increased screen time, extensive use of digital and screen-based technologies, or distance learning because of the pandemic, and consistently reported the development or progression of digital eye strain or computer vision syndrome symptoms, and dry eye symptoms and signs. These findings were independent of geographical region. Most studies did not report other concurrent health interventions related to the pandemic (such as vaccination timing, lockdowns, mask-wearing).
Prolonged and consistent face mask wear appeared to induce or exacerbate symptoms and signs of dry eye disease, intolerance to contact lenses, and increase the prevalence of chalazia. The drying effects may arise due to the change of direction of air flow upwards while breathing while wearing a mask [577,612], creating airflow across the ocular surface. This was demonstrated using thermal imaging and many face mask wearers report the sensation of air blowing upwards into their eyes [[612], [613], [614]]. In an anterior segment optical coherence tomography study of dry eye patients, there was a significant decrease in tear meniscus height and area with a significant increase in blink frequency after exposure of the ocular surface to airflow [615], which may be increased in a poorly fitting mask [616]. Conceivably, in those using both masks and goggles, the temperature and humidity of the periorbital region may increase [606,617], which may increase the likelihood of eyelid inflammation [606,618,619].
In contrast to symptoms of dry eye, allergic ocular symptoms improved with the use of face masks, most likely due the barrier properties of face masks against nasal exposure to airborne allergens.
With ocular surface manifestations of COVID-19, long COVID, or multisystem inflammatory syndrome after COVID-19, numerous studies have investigated ocular surface symptoms and signs in patients with these conditions or evaluated the association with timing and severity with ocular surface presentations to systemic disease, however, the majority are non-comparative studies. Previous systematic reviews and meta-analyses included small case series and case reports and were generally inconclusive [565,566,571,574,[620], [621], [622], [623], [624], [625]]. In the current systematic review, only 11 comparative studies involving patients with COVID-19 were selected for analysis. The present review found that COVID-19 patients could present with a wide range of non-specific ocular surface symptoms and signs, largely depending on the systemic disease severity. Studies that examined conjunctivitis as an outcome had mixed results, thus, the link between COVID-19 and conjunctivitis remains controversial. The relationships between the occurrence of ocular surface symptoms or signs, the detection of virus on the conjunctiva or in tears, and the possibilities of ocular transmission are beyond the scope of this systematic review.
A few studies confirming the adverse effects of other countermeasures against COVID-19 on the ocular surface, such as hand sanitizers and ultraviolet C germicidal lamps were identified [547,588,591,604,626]. Hand sanitizer caused ocular surface burns with toxic keratopathy, photophobia, limbal involvement and epithelial loss in children [627], adults [628] and healthcare workers [629]. Compared with pre-pandemic, where most injuries were seen in healthcare workers, most cases during the pandemic occurred in children [630]. Ultraviolet germicidal lamps became widespread during the pandemic, and adverse effects included irradiation-induced photokeratitis.
There were no studies that investigated the effects of COVID-19 treatments, such as high-dose steroids, ventilator, and other intensive care unit care, as well as the psychological and behavioral consequences of the pandemic on the ocular surface (Section 7).
The studies included were limited to those with at least 50 participants and those which included a comparison group. The risk of bias assessment revealed that 85% of the studies exhibited moderate-to-high risk of bias. When interpreting the results of this review, it should be emphasized that these findings were derived from heterogeneous studies because of the diversity in the study designs, populations, and outcomes.
Although widespread vaccination has reduced the case number and hospital admissions, preventive measures such as face mask wearing and working/studying from home are still recommended in many countries/regions at the time of writing this report. In addition, emergence of new variants may result in an extension of the mitigating strategies for an uncertain period. As the virus continues to mutate, the far-reaching impact of COVID-19 will likely persist. Further research, especially prospective cohort studies with large numbers of participants, is warranted to explore and better understand the direct and indirect effects of the COVID-19 pandemic on ocular surface health. These studies will have the added effect of improving our understanding of societal/public health measures during a pandemic and their associations with health and wellbeing of the population to better prepare for a possible future pandemic.
8.4. Conclusion
The COVID-19 pandemic and related mitigating strategies appear to be associated with an increased risk of developing new or worsening pre-existing ocular surface symptoms and signs in most populations studied. Determining the role of individual risk factors may be challenging due to the nature of the studies and multiple confounding factors.
9. Conclusions and recommendations
This report has explored societal challenges in ocular surface diseases through interactions between the individual, social, cultural, regional and global factors and has also considered the impact of information technology on access to eyecare services, which may influence the likelihood of ocular surface disease and the risk and impact of more severe disease (Table 4 ). The COVID-19 pandemic has offered a further level of interaction by directly or indirectly impacting many of these societal factors. This report also considered a key clinical question in the form of a systematic review to critically evaluate the available evidence to understand whether the COVID-19 pandemic has changed the severity or outcome of ocular surface diseases.
Table 4.
Summary of main societal factors by ocular disease classification.
| Classification | Disease | Biology, genetics & co-morbidities | Individual lifestyle/societal factors | Living and working conditions | Socioeconomic/cultural/Environmental conditions | Pandemic-related |
|---|---|---|---|---|---|---|
| Trauma | Eye/orbital injuries | Male (employment/hobbies); | Sports such as soccer and hockey, recreational fishing, fireworks, eye lid tattooing; toy guns | Occupational exposure to projectiles, observed in miners, construction workers, law enforcement, armed services, laboratory staff, food service industry workers, agricultural workers, fire workers, and mechanics | War and violent attacks; rural and low-income regions | Access to practitioners |
| female (domestic violence) | ||||||
| Lid-wiper epitheliopathy | Insomnia; depression | Contact lens wear; eye rubbing | ||||
| Ocular surface chemical injuries (OSCI) | Children under 5 (domestic accident); Female (acid attacks, domestic violence); Male (employment/hobbies) | Leaking or burst detergent pods; calcium hydroxide paste mixed in chewing tobacco or betel nut | Occupational exposure to chemicals, observed in abattoir workers exposed to sheep, turkey, and fish bile; chemical or construction workers; health care workers | Violent chemical attacks and assault; domestic violence (vitriolage); conflict associated with riot/tear gas; health-seeking behaviour | Hand sanitizer injury in non-healthcare workers | |
| Toxic conjunctivitis | Use of hand sanitizer; surface disinfectant; contact lens wear | Traditional medicine use such as Kermes (red dye from insect), honey, cow dung, Ushaar (xerophytic shrub) | ||||
| Infection | Non-viral corneal infection | Sex and age (dependent on indication); prior ocular surgery, ocular surface disease; trauma; diabetes; HSV; HIV; rheumatoid arthritis | Contact lens wear; recreational drug use; alcohol use, snorting cocaine | Ocular trauma; agricultural work; animal handlers | Low educational level; low GDP; limited access to appropriate services (war, displacement, religious, gender); traditional medicines, breastmilk, honey or alum; higher daytime temperature (Contact lenses); warmer months | |
| Fungal keratitis | Male; Malay ethnicity (in Asia); Indigenous populations | Ocular trauma with vegetative material; agricultural work; outdoor occupations; rural environments | Hot windy climates in the tropics; high daytime temperatures; poverty; educational level; low gross domestic product per capita; higher rates in India and Africa | |||
| Acanthamoeba keratitis | All ages | Contact lens wear | Ocular trauma; contaminated water; fishing; water sports | Summer and autumn months | ||
| Infectious corneal blindness | Female; ↑ age; diabetes, HIV | Snorting cocaine, methamphetamine use | Rural areas | Low educational level; low socioeconomic status and/or poverty; traditional medicines | ||
| Trachoma | Childhood (active conjunctival disease); age; female (corneal scarring); Indigenous populations | Face washing | Poor sanitation; overcrowding; lack of access to clean water; | Low-income countries; low socioeconomic status and/or poverty; rural communities; low education status; migrants; possible climate change effects on water quality; remoteness and access to care (religious, regional, geographic constraints, war, displacement); health-seeking behaviours; absence of culturally-appropriate services; climate change impacts access to clean water | Altered access to services during pandemic | |
| Oncocerciasis | Indigenous populations | Contaminated river water | Remoteness; poverty; limited access to services; possible climate change effects on water quality; | |||
| Demodex blepharitis | ↑ Age; meibomian gland dysfunction | Contact lens wear | ||||
| Herpes zoster keratitis/Herpes zoster ophthalmicus (HZO) | ↑ Age (also associated with severe vision loss); prior exposure | |||||
| Herpes simplex virus keratitis | Diabetes; immunocompromise | |||||
| Inflammation | Dry eye disease | ↑ Age; female; Asian or East Asian ethnicity. Co-morbidities – Sjӧgren syndrome; chronic pain syndromes; atopy, arthritis; thyroid disease; acne rosacea; prior ocular surgery, menopause; diabetes; pterygia, forms of arthritis; dys- or hyper-lipidemia; renal failure; ischemic heart disease; cardiac arrhythmias; peripheral vascular disease; stroke; migraine; myasthenia gravis; autoimmune diseases; pulmonary circulation disorders; diabetes; hypothyroidism; liver disease; peptic ulcer; hepatitis B status; deficiency anemias, depression, psychoses; certain cancers; chronic fatigue syndrome; osteoarthritis; connective tissue diseases; Graves' disease; autistic disorders; Crohn's disease; sarcoidosis, rosacea; liver cirrhosis; sleep apnea; sinusitis; nasolacrimal duct obstruction; moderate heritability |
Systemic/topical medications (Proton pump inhibitors; anticholinergic drugs; anti-glaucoma medications; oral contraceptives; antidepressants; antiallergy medications; contact lens use; smoking, obesity, metabolic syndrome; lack of physical exercise; sedentary lifestyle; excessive caffeine consumption; diet; elective eye surgeries; former smokers | Visual display terminal workers; digital device use; night shift work; air-conditioning; unemployment; retirement; higher education (may be confounded by higher screen time) | Windy conditions; low humidity; low humidity and particulate matter of 2.5 μm or less (PM2.5); air pollution – bushfire and other smoke; low income countries rural communities | Face mask wear; increased screen time; increased time spent in remote learning or working online from home; access to services changed – increased telehealth and education of patients and practitioners through the digital transformation; unemployment or reduced employment increased health related problems |
| Meibomian gland dysfunction | ↑ Age; no increased risk in females; increased risk of asymptomatic disease in males; rosacea; demodex | Contact lens wear | Night shift work | Low income countries – rural communities | ||
| Neurotrophic keratitis | Diabetes; HSV | Snorting cocaine, methamphetamine use | ||||
| Conjunctivochalasis | ↑ Age | |||||
| Autoimmune diseases | Female; ↑age; | |||||
| Chalazion/hordeolum | Face mask wear | |||||
| Cicatricial conjunctivitis | Ocular pemphigoid; Steven Johnson syndrome; | Topical use of Kermes, a red dye obtained from an insect | ||||
| Superior limbic keratoconjunctivitis | Female; thyroid disease; insomnia; depression | Contact lens wear | ||||
| Allergy | Seasonal/perennial allergic conjunctivitis | Children and young adults (first three decades); may occur in older adults; atopy | Use of topical ocular medications, particularly anti-glaucoma drugs | Farmer, animal handler; gardener; higher rate in prison populations | Wet rainy season; warm & dusty weather, seasonal variations with increased pollen conditions; low indoor humidity | Reduced symptoms with mask use |
| Giant papillary conjunctivitis | Children and young adults (first three decades); atopy; | Contact lens wear; keratoconus; prosthetic shell; | ||||
| Vernal keratoconjunctivitis | Children and young adults (first three decades); atopy; keratoconus | Traditional medicine use such as honey | ||||
| Atopic keratoconjunctivitis | Children and young adults (first three decades); may occur in older adults; atopic dermatitis | Use of topical ocular medications, particularly anti-glaucoma drugs | Changes in climate, diet, living conditions, lifestyles, air pollutants, comorbidities, and concomitant medications | |||
| Contact blepharo-conjunctivitis | Middle aged or older adults | Use of topical ocular medications, particularly anti-glaucoma drugs; hand sanitiser | ||||
| Neoplasia | Pinguecula | ↑ Age | Sun exposure | |||
| Pterygium | ↑ Age, male | Sun exposure | Outdoor employment; occupational exposures; higher rate in prison populations | Low- and middle-income countries | ||
| Conjunctival melanoma | ↑ Age (55–75 years, also risk for more severe presentation and outcome); Caucasian; other ocular melanosis | |||||
| Conjunctival lymphoma | ↑ Age (7th - 8th decade, also risk for poorer outcome) | |||||
| Conjunctival squamous metaplasia/xerophthalmic | Vitamin A deficiency; usually children; young females in high-income countries | Poor nutrition; anorexia nervosa; eating disorders; chronic alcohol consumption | Higher rate in prison populations | Migrant/displaced populations; childhood education; poverty; natural disasters reduce access to nutritious food particularly in children | Food chain supplies may have been affected during pandemic | |
| Ocular surface squamous neoplasia (OSSN) | ↑ Age, male; HIV/HPV status in younger age groups | Temperate climate for older age groups; high solar UV radiation exposure in younger individuals | ||||
| Hereditary/Congenital | Corneal thinning | Keratoconus | Topical use of traditional medicine, Alum, a hydrated salt comprised of potassium aluminium sulphate used in making foods | |||
| Corneal epithelial defects | Corneal dystrophy | Topical use of cow urine, hand sanitizer splash |
Societal challenges are associated with both acute and chronic ocular surface diseases. While the impact of age, race and biological factors on many ocular surface diseases are well established, the effects of sex may be confounded by other social or gender constructs including access to health care, employment, poverty and education. In addition, differences in rate of disease in different populations for example Indigenous vs non-Indigenous may be confounded by broader societal issues such access to health care resources, poverty, education and disadvantage/marginalisation. Data needs in the future would include appropriately powered and stratified studies to enable the impact of individual factors to be assessed.
Individual choices, social or lifestyle factors included those with both positive and negative effects on ocular surface diseases, such as exercise, recreational drug use, hobbies, traditional medicines and the effects of societal supports or societal pressures. The relative impact of these factors is closely related to regional and socioeconomic variations.
Living and working conditions can significantly impact ocular surface diseases. The type of occupation may clearly predispose to certain injuries or diseases, however, the morbidity of these conditions is strongly influenced by poverty, (childhood) education, water and sanitation, housing and socioeconomic factors.
Regional and global socioeconomic, cultural and environmental conditions relevant to ocular surface diseases include the impact of remoteness to treatment, the change in the spectrum of disease with seasonality or climate variations, availability and affordability of eyecare services and culturally appropriate services. The effects of climate change on water quality, access to services and food security may influence the type and severity of ocular surface diseases. Gendered violence, conflict, and mass immigration challenge financial and food security, and may limit access to care. During wartime or conflict, decreased personal security, inadequate access to health services and the absence of health workers reduces ability to access to eye care services and diseases of the ocular surface are not prioritised in these situations.
In the information technology era, health communication patterns have changed and patient- and practitioner-specific issues impact both access to and the different types of eye care services available. The impact of the digital environment on physical, mental and social health includes the effect of social isolation on both the risk and severity of ocular surface diseases.
The impact of the pandemic on ocular surfaces diseases through the impact on mental health, access to services, face mask and hand sanitizer use and changes to the work environment was considered. The systematic review established that the COVID-19 pandemic and the various mitigating strategies or their consequences, including increased screen time and online learning were associated with an increased risk of developing new or worsening pre-existing ocular surface diseases. Given the longer-term changes in remote or flexible work and study practices, it seems reasonable to assume that increased frequency and severity of these conditions will persist beyond the immediate pandemic.
Disclosures
Fiona Stapleton: Alcon (C,F), Allergan (F), Azura Ophthalmics (F), Coopervision (C), Exonate (F), Menicon (F), nthalmic (F), Novartis (C,F), CSL Seqirus (C), Sun Pharmaceuticals (C); Juan Carlos Abad: Allergan (C,P); Stefano Barabino: Oftalab (P), TRB Chemedia (C), Sifi (C), Novartis (C), Alfa (C), Intes (C), Poufarma (C), Théa (C); Anthea Burnett: None; Geetha Iyer: None; Kaevalin Lekhanont: None; Tianjing Li: None; Yang Liu: ESSIRI (I); Alejandro Navas: None; Chukwuemeka Junior, Obinwanne: None; Riaz Qureshi: PICO Portal (C); Danial Roshandel: None; Afsun Sahin: None; Anna Tichenor: None; Lyndon Jones: Alcon (F,C,R), Azura Ophthalmics (F), Bausch + Lomb (F), CooperVision (F,C,R), Essilor (F), Hoya (F), I-Med Pharma (F), Johnson & Johnson Vision (F,C,R), Menicon (F), Novartis (F), Ophtecs (F,C), Ote Pharma (F), Santen (F), SightGlass (F), SightSage (F), Topcon (F), Visioneering (F,C).
Acknowledgments
The authors of this report and broader TFOS Lifestyle Workshop membership would like to acknowledge and recognise Professor Juan Carlos Abad, who sadly passed away during the preparation of the reports. We wish to acknowledge his contribution to the field [631].
The TFOS Lifestyle Workshop was conducted under the leadership of Jennifer P Craig, PhD FCOptom (Chair), Monica Alves, MD PhD (Vice Chair) and David A Sullivan PhD (Organizer). The Workshop participants are grateful to Amy Gallant Sullivan (TFOS Executive Director, France) for raising the funds that made this initiative possible. The TFOS Lifestyle Workshop was supported by unrestricted donations from Alcon, Allergan an AbbVie Company, Bausch + Lomb, Bruder Healthcare, CooperVision, CSL Seqirus, Dompé, ESW-Vision, ESSIRI Labs, Eye Drop Shop, I-MED Pharma, KALA Pharmaceuticals, Laboratoires Théa, Santen, Novartis, Shenyang Sinqi Pharmaceutical, Sun Pharmaceutical Industries, Tarsus Pharmaceuticals, Trukera Medical and URSAPHARM.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jtos.2023.04.006.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Whitehead M., Dahlgren G. Institute for Future Studies; Stockholm, Sweden: 1991. Policies and strategies to promote social equity in health. [Google Scholar]
- 2.Rice L., Sara R. Updating the determinants of health model in the Information Age. Health Promot Int. 2019;34:1241–1249. doi: 10.1093/heapro/day064. [DOI] [PubMed] [Google Scholar]
- 3.Markoulli M., Arcot J., Ahmad S., Arita R., Benitez-del-Castillo J., Caffery B., et al. TFOS Lifestyle: impact of nutrition on the ocular surface. Ocul Surf. 2023 doi: 10.1016/j.jtos.2023.04.003. [DOI] [PubMed] [Google Scholar]
- 4.Sullivan D.A., da Costa A.X., Del Duca E., Doll T., Grupcheva C.N., Lazreg S., et al. TFOS Lifestyle: impact of cosmetics on the ocular surface. Ocul Surf. 2023 doi: 10.1016/j.jtos.2023.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gomes J.A.P., Azar D.T., Baudouin C., Bitton E., Chen W., Hafezi F., et al. TFOS Lifestyle: impact of elective medications and procedures on the ocular surface. Ocul Surf. 2023 doi: 10.1016/j.jtos.2023.04.011. [DOI] [PubMed] [Google Scholar]
- 6.Galor A., Britten-Jones A.C., Feng Y., Ferrari G., Goldblum D., Gupta P.K., et al. TFOS Lifestyle: impact of lifestyle challenges on the ocular surface. Ocul Surf. 2023 doi: 10.1016/j.jtos.2023.04.008. [DOI] [PubMed] [Google Scholar]
- 7.Alves M., Asbell P., Dogru M., Giannaccare G., Grau A., Gregory D., et al. TFOS Lifestyle: impact of environmental conditions on the ocular surface. Ocul Surf. 2023 doi: 10.1016/j.jtos.2023.04.007. [DOI] [PubMed] [Google Scholar]
- 8.Wolffsohn J.S., Lingham G., Downie L.E., Huntjens B., Inomata T., Jivraj S., et al. TFOS Lifestyle: impact of the digital environment on the ocular surface. Ocul Surf. 2023 doi: 10.1016/j.jtos.2023.04.004. [DOI] [PubMed] [Google Scholar]
- 9.Downie L.E., Britten-Jones A.C., Hogg R.E., Jalbert I., Li T., Lingham G., et al. Advancing the evaluation and synthesis of research evidence for the TFOS lifestyle workshop: report of the evidence quality subcommittee. Ocul Surf. 2023 doi: 10.1016/j.jtos.2023.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stapleton F., Alves M., Bunya V.Y., Jalbert I., Lekhanont K., Malet F., et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15:334–365. doi: 10.1016/j.jtos.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Arita R., Mizoguchi T., Kawashima M., Fukuoka S., Koh S., Shirakawa R., et al. Meibomian gland dysfunction and dry eye are similar but different based on a population-based study: the hirado-takushima study in Japan. Am J Ophthalmol. 2019;207:410–418. doi: 10.1016/j.ajo.2019.02.024. [DOI] [PubMed] [Google Scholar]
- 12.Castro J.S., Selegatto I.B., Castro R.S., Miranda E.C.M., de Vasconcelos J.P.C., de Carvalho K.M., et al. Prevalence and Risk Factors of self-reported dry eye in Brazil using a short symptom questionnaire. Sci Rep. 2018;8:2076. doi: 10.1038/s41598-018-20273-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farrand K.F., Fridman M., Stillman I., Schaumberg D.A. Prevalence of diagnosed dry eye disease in the United States among adults aged 18 Years and older. Am J Ophthalmol. 2017;182:90–98. doi: 10.1016/j.ajo.2017.06.033. [DOI] [PubMed] [Google Scholar]
- 14.Millán A., Viso E., Gude F., Parafita-Fernández A., Moraña N., Rodríguez-Ares M.T. Incidence and risk factors of dry eye in a Spanish adult population: 11-year follow-up from the salnés eye study. Cornea. 2018;37:1527–1534. doi: 10.1097/ICO.0000000000001713. [DOI] [PubMed] [Google Scholar]
- 15.Vehof J., Snieder H., Jansonius N., Hammond C.J. Prevalence and risk factors of dry eye in 79,866 participants of the population-based Lifelines cohort study in The Netherlands. Ocul Surf. 2021;19:83–93. doi: 10.1016/j.jtos.2020.04.005. [DOI] [PubMed] [Google Scholar]
- 16.Man R.E.K., Veerappan A.R., Tan S.P., Fenwick E.K., Sabanayagam C., Chua J., et al. Incidence and risk factors of symptomatic dry eye disease in Asian Malays from the Singapore Malay Eye Study. Ocul Surf. 2017;15:742–748. doi: 10.1016/j.jtos.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 17.Paulsen A.J., Cruickshanks K.J., Fischer M.E., Huang G.H., Klein B.E., Klein R., et al. Dry eye in the Beaver Dam Offspring Study: prevalence, risk factors, and health-related quality of life. Am J Ophthalmol. 2014;157:799–806. doi: 10.1016/j.ajo.2013.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan L.L., Morgan P., Cai Z.Q., Straughan R.A. Prevalence of and risk factors for symptomatic dry eye disease in Singapore. Clin Exp Optom. 2015;98:45–53. doi: 10.1111/cxo.12210. [DOI] [PubMed] [Google Scholar]
- 19.Dana R., Bradley J.L., Guerin A., Pivneva I., Stillman I., Evans A.M., et al. Estimated prevalence and incidence of dry eye disease based on coding analysis of a large, all-age United States health care system. Am J Ophthalmol. 2019;202:47–54. doi: 10.1016/j.ajo.2019.01.026. [DOI] [PubMed] [Google Scholar]
- 20.Courtin R., Pereira B., Naughton G., Chamoux A., Chiambaretta F., Lanhers C., et al. Prevalence of dry eye disease in visual display terminal workers: a systematic review and meta-analysis. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2015-009675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu N.N., Liu L., Li J., Sun Y.Z. Prevalence of and risk factors for dry eye symptom in mainland China: a systematic review and meta-analysis. J Ophthalmol. 2014;2014 doi: 10.1155/2014/748654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Song P., Xia W., Wang M., Chang X., Wang J., Jin S., et al. Variations of dry eye disease prevalence by age, sex and geographic characteristics in China: a systematic review and meta-analysis. J Glob Health. 2018;8 doi: 10.7189/jogh.08.020503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Uchino M. What we know about the epidemiology of dry eye disease in Japan. Invest Ophthalmol Vis Sci. 2018;59:1–6. doi: 10.1167/iovs.17-23491. [DOI] [PubMed] [Google Scholar]
- 24.Akowuah P.K., Kobia-Acquah E. Prevalence of dry eye disease in Africa: a systematic review and meta-analysis. Optom Vis Sci. 2020;97:1089–1098. doi: 10.1097/OPX.0000000000001610. [DOI] [PubMed] [Google Scholar]
- 25.Asiedu K., Kyei S., Boampong F., Ocansey S. Symptomatic dry eye and its associated factors: a study of university undergraduate students in Ghana. Eye Contact Lens. 2017;43:262–266. doi: 10.1097/ICL.0000000000000256. [DOI] [PubMed] [Google Scholar]
- 26.Caffery B., Srinivasan S., Reaume C.J., Fischer A., Cappadocia D., Siffel C., et al. Prevalence of dry eye disease in Ontario, Canada: a population-based survey. Ocul Surf. 2019;17:526–531. doi: 10.1016/j.jtos.2019.02.011. [DOI] [PubMed] [Google Scholar]
- 27.García-Ayuso D., Di Pierdomenico J., Moya-Rodríguez E., Valiente-Soriano F.J., Galindo-Romero C., Sobrado-Calvo P. Assessment of dry eye symptoms among university students during the COVID-19 pandemic. Clin Exp Optom. 2021:1–7. doi: 10.1080/08164622.2021.1945411. [DOI] [PubMed] [Google Scholar]
- 28.Garza-León M., Valencia-Garza M., Martínez-Leal B., Villarreal-Peña P., Marcos-Abdala H.G., Cortéz-Guajardo A.L., et al. Prevalence of ocular surface disease symptoms and risk factors in group of university students in Monterrey, Mexico. J Ophthalmic Inflamm Infect. 2016;6:44. doi: 10.1186/s12348-016-0114-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hung N., Kang E.Y., Lee T.W., Chen T.H., Shyu Y.C., Sun C.C. The risks of corneal surface damage in aqueous-deficient dry eye disease: a 17-year population-based study in taiwan. Am J Ophthalmol. 2021;227:231–239. doi: 10.1016/j.ajo.2021.03.013. [DOI] [PubMed] [Google Scholar]
- 30.Li S., He J., Chen Q., Zhu J., Zou H., Xu X. Ocular surface health in Shanghai University students: a cross-sectional study. BMC Ophthalmol. 2018;18:245. doi: 10.1186/s12886-018-0825-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Supiyaphun C., Jongkhajornpong P., Rattanasiri S., Lekhanont K. Prevalence and risk factors of dry eye disease among University Students in Bangkok, Thailand. PLoS One. 2021;16 doi: 10.1371/journal.pone.0258217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Uchino M., Dogru M., Uchino Y., Fukagawa K., Shimmura S., Takebayashi T., et al. Japan Ministry of Health study on prevalence of dry eye disease among Japanese high school students. Am J Ophthalmol. 2008;146:925–929. doi: 10.1016/j.ajo.2008.06.030. e2. [DOI] [PubMed] [Google Scholar]
- 33.Yang I., Wakamatsu T., Sacho I.B.I., Fazzi J.H., de Aquino A.C., Ayub G., et al. Prevalence and associated risk factors for dry eye disease among Brazilian undergraduate students. PLoS One. 2021;16 doi: 10.1371/journal.pone.0259399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang Y., Chen H., Wu X. Prevalence and risk factors associated with dry eye syndrome among senior high school students in a county of Shandong Province, China. Ophthalmic Epidemiol. 2012;19:226–230. doi: 10.3109/09286586.2012.670742. [DOI] [PubMed] [Google Scholar]
- 35.Vehof J., Wang B., Kozareva D., Hysi P.G., Snieder H., Hammond C.J. The heritability of dry eye disease in a female twin cohort. Invest Ophthalmol Vis Sci. 2014;55:7278–7283. doi: 10.1167/iovs.14-15200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chhadva P., Goldhardt R., Galor A. Meibomian gland disease: the role of gland dysfunction in dry eye disease. Ophthalmology. 2017;124 doi: 10.1016/j.ophtha.2017.05.031. S20-s6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schaumberg D.A., Nichols J.J., Papas E.B., Tong L., Uchino M., Nichols K.K. The international workshop on meibomian gland dysfunction: report of the subcommittee on the epidemiology of, and associated risk factors for, MGD. Invest Ophthalmol Vis Sci. 2011;52:1994–2005. doi: 10.1167/iovs.10-6997e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li Y., Lu J., Zhou Q., Wang C., Zeng Q., Chen T., et al. Analysis of clinical and regional distribution characteristics of obstructive meibomian gland dysfunction in China: a multicenter study. Curr Eye Res. 2020;45:1373–1379. doi: 10.1080/02713683.2020.1752387. [DOI] [PubMed] [Google Scholar]
- 39.Viso E., Rodríguez-Ares M.T., Abelenda D., Oubiña B., Gude F. Prevalence of asymptomatic and symptomatic meibomian gland dysfunction in the general population of Spain. Invest Ophthalmol Vis Sci. 2012;53:2601–2606. doi: 10.1167/iovs.11-9228. [DOI] [PubMed] [Google Scholar]
- 40.Hassanzadeh S., Varmaghani M., Zarei-Ghanavati S., Heravian Shandiz J., Azimi Khorasani A. Global prevalence of meibomian gland dysfunction: a systematic review and meta-analysis. Ocul Immunol Inflamm. 2021;29:66–75. doi: 10.1080/09273948.2020.1755441. [DOI] [PubMed] [Google Scholar]
- 41.Zhang A.C., Muntz A., Wang M.T.M., Craig J.P., Downie L.E. Ocular Demodex: a systematic review of the clinical literature. Ophthalmic Physiol Opt. 2020;40:389–432. doi: 10.1111/opo.12691. [DOI] [PubMed] [Google Scholar]
- 42.Suzuki T., Kitazawa K., Cho Y., Yoshida M., Okumura T., Sato A., et al. Alteration in meibum lipid composition and subjective symptoms due to aging and meibomian gland dysfunction. Ocul Surf. 2021 doi: 10.1016/j.jtos.2021.10.003. [DOI] [PubMed] [Google Scholar]
- 43.Sullivan B.D., Evans J.E., Dana M.R., Sullivan D.A. Influence of aging on the polar and neutral lipid profiles in human meibomian gland secretions. Arch Ophthalmol. 2006;124:1286–1292. doi: 10.1001/archopht.124.9.1286. [DOI] [PubMed] [Google Scholar]
- 44.Obata H. Anatomy and histopathology of human meibomian gland. Cornea. 2002;21:S70–S74. doi: 10.1097/01.ico.0000263122.45898.09. [DOI] [PubMed] [Google Scholar]
- 45.Akowuah P.K., Kobia-Acquah E., Donkor R., Arthur C., Senanu E.N., Dadzie E.E., et al. Prevalence of meibomian gland dysfunction in Africa: a systematic review and meta-analysis of observational studies. Ophthalmic Epidemiol. 2021:1–10. doi: 10.1080/09286586.2021.1958351. [DOI] [PubMed] [Google Scholar]
- 46.Siak J.J., Tong L., Wong W.L., Cajucom-Uy H., Rosman M., Saw S.M., et al. Prevalence and risk factors of meibomian gland dysfunction: the Singapore Malay eye study. Cornea. 2012;31:1223–1228. doi: 10.1097/ICO.0b013e31823f0977. [DOI] [PubMed] [Google Scholar]
- 47.Hashemi H., Rastad H., Emamian M.H., Fotouhi A. Meibomian gland dysfunction and its determinants in Iranian adults: a population-based study. Contact Lens Anterior Eye. 2017;40:213–216. doi: 10.1016/j.clae.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 48.Gumus K., Pflugfelder S.C. Increasing prevalence and severity of conjunctivochalasis with aging detected by anterior segment optical coherence tomography. Am J Ophthalmol. 2013;155 doi: 10.1016/j.ajo.2012.07.014. 238-42.e2. [DOI] [PubMed] [Google Scholar]
- 49.Marmalidou A., Kheirkhah A., Dana R. Conjunctivochalasis: a systematic review. Surv Ophthalmol. 2018;63:554–564. doi: 10.1016/j.survophthal.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 50.Hashemi H., Rastad H., Emamian M.H., Fotouhi A. Conjunctivochalasis and related factors in an adult population of Iran. Eye Contact Lens. 2018;44(Suppl 1) doi: 10.1097/ICL.0000000000000379. S206-s9. [DOI] [PubMed] [Google Scholar]
- 51.Mimura T., Yamagami S., Usui T., Funatsu H., Mimura Y., Noma H., et al. Changes of conjunctivochalasis with age in a hospital-based study. Am J Ophthalmol. 2009;147:171–177. doi: 10.1016/j.ajo.2008.07.010. e1. [DOI] [PubMed] [Google Scholar]
- 52.Poh S., Lee R., Gao J., Tan C., Gupta P., Sabanayagam C., et al. Factors that influence tear meniscus area and conjunctivochalasis: the Singapore Indian eye study. Ophthalmic Epidemiol. 2018;25:70–78. doi: 10.1080/09286586.2017.1351999. [DOI] [PubMed] [Google Scholar]
- 53.Zhang X., Li Q., Zou H., Peng J., Shi C., Zhou H., et al. Assessing the severity of conjunctivochalasis in a senile population: a community-based epidemiology study in Shanghai, China. BMC Publ Health. 2011;11:198. doi: 10.1186/1471-2458-11-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Le Q., Xiang J., Cui X., Zhou X., Xu J. Prevalence and associated factors of pinguecula in a rural population in Shanghai, Eastern China. Ophthalmic Epidemiol. 2015;22:130–138. doi: 10.3109/09286586.2015.1012269. [DOI] [PubMed] [Google Scholar]
- 55.Liu L., Wu J., Geng J., Yuan Z., Huang D. Geographical prevalence and risk factors for pterygium: a systematic review and meta-analysis. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-003787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rezvan F., Khabazkhoob M., Hooshmand E., Yekta A., Saatchi M., Hashemi H. Prevalence and risk factors of pterygium: a systematic review and meta-analysis. Surv Ophthalmol. 2018;63:719–735. doi: 10.1016/j.survophthal.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 57.Song P., Chang X., Wang M., An L. Variations of pterygium prevalence by age, gender and geographic characteristics in China: a systematic review and meta-analysis. PLoS One. 2017;12 doi: 10.1371/journal.pone.0174587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Modenese A., Gobba F. Occupational exposure to solar radiation at different latitudes and pterygium: a systematic review of the last 10 Years of scientific literature. Int J Environ Res Publ Health. 2017;15 doi: 10.3390/ijerph15010037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bikbov M.M., Zainullin R.M., Kazakbaeva G.M., Gilmanshin T.R., Salavatova V.F., Arslangareeva, et al. Pterygium prevalence and its associations in a Russian population: the ural eye and medical study. Am J Ophthalmol. 2019;205:27–34. doi: 10.1016/j.ajo.2019.02.031. [DOI] [PubMed] [Google Scholar]
- 60.Wang Y., Shan G., Gan L., Qian Y., Chen T., Wang H., et al. Prevalence and associated factors for pterygium in Han and Mongolian adults: a cross-sectional study in inner Mongolian, China. BMC Ophthalmol. 2020;20:45. doi: 10.1186/s12886-020-1324-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rim T.H., Kang M.J., Choi M., Seo K.Y., Kim S.S. The incidence and prevalence of pterygium in South Korea: a 10-year population-based Korean cohort study. PLoS One. 2017;12 doi: 10.1371/journal.pone.0171954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stapleton F. The epidemiology of infectious keratitis. Ocul Surf. 2021 doi: 10.1016/j.jtos.2021.08.007. [DOI] [PubMed] [Google Scholar]
- 63.Arunga S., Kintoki G.M., Gichuhi S., Onyango J., Ayebazibwe B., Newton R., et al. Risk factors of microbial keratitis in Uganda: a case control study. Ophthalmic Epidemiol. 2020;27:98–104. doi: 10.1080/09286586.2019.1682619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Song X., Xie L., Tan X., Wang Z., Yang Y., Yuan Y., et al. A multi-center, cross-sectional study on the burden of infectious keratitis in China. PLoS One. 2014;9 doi: 10.1371/journal.pone.0113843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chidambaram J.D., Venkatesh Prajna N., Srikanthi P., Lanjewar S., Shah M., Elakkiya S., et al. Epidemiology, risk factors, and clinical outcomes in severe microbial keratitis in South India. Ophthalmic Epidemiol. 2018;25:297–305. doi: 10.1080/09286586.2018.1454964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Koh Y.Y., Sun C.C., Hsiao C.H. Epidemiology and the estimated burden of microbial keratitis on the health care system in taiwan: a 14-year population-based study. Am J Ophthalmol. 2020;220:152–159. doi: 10.1016/j.ajo.2020.07.026. [DOI] [PubMed] [Google Scholar]
- 67.Bardach A.E., Palermo C., Alconada T., Sandoval M., Balan D.J., Nieto Guevara J., et al. Herpes zoster epidemiology in Latin America: a systematic review and meta-analysis. PLoS One. 2021;16 doi: 10.1371/journal.pone.0255877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kawai K., Gebremeskel B.G., Acosta C.J. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2014-004833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Patki A., Vora A., Parikh R., Kolhapure S., Agrawal A., Dash R. Herpes zoster in outpatient departments of healthcare centers in India: a review of literature. Hum Vaccines Immunother. 2021;17:4155–4162. doi: 10.1080/21645515.2021.1968737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pinchinat S., Cebrián-Cuenca A.M., Bricout H., Johnson R.W. Similar herpes zoster incidence across Europe: results from a systematic literature review. BMC Infect Dis. 2013;13:170. doi: 10.1186/1471-2334-13-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Forbes H.J., Bhaskaran K., Grint D., Hu V.H., Langan S.M., McDonald H.I., et al. Incidence of acute complications of herpes zoster among immunocompetent adults in England: a matched cohort study using routine health data. Br J Dermatol. 2021;184:1077–1084. doi: 10.1111/bjd.19687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Borkar D.S., Tham V.M., Esterberg E., Ray K.J., Vinoya A.C., Parker J.V., et al. Incidence of herpes zoster ophthalmicus: results from the pacific ocular inflammation study. Ophthalmology. 2013;120:451–456. doi: 10.1016/j.ophtha.2012.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Niederer R.L., Meyer J.J., Liu K., Danesh-Meyer H.V. Herpes zoster ophthalmicus clinical presentation and risk factors for loss of vision. Am J Ophthalmol. 2021;226:83–89. doi: 10.1016/j.ajo.2021.02.002. [DOI] [PubMed] [Google Scholar]
- 74.Ventura M.T., Scichilone N., Paganelli R., Minciullo P.L., Patella V., Bonini M., et al. Allergic diseases in the elderly: biological characteristics and main immunological and non-immunological mechanisms. Clin Mol Allergy. 2017;15:2. doi: 10.1186/s12948-017-0059-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Miyazaki D., Fukagawa K., Okamoto S., Fukushima A., Uchio E., Ebihara N., et al. Epidemiological aspects of allergic conjunctivitis. Allergol Int. 2020;69:487–495. doi: 10.1016/j.alit.2020.06.004. [DOI] [PubMed] [Google Scholar]
- 76.Leonardi A., Piliego F., Castegnaro A., Lazzarini D., La Gloria Valerio A., Mattana P., et al. Allergic conjunctivitis: a cross-sectional study. Clin Exp Allergy. 2015;45:1118–1125. doi: 10.1111/cea.12536. [DOI] [PubMed] [Google Scholar]
- 77.Ventura M.T., D'Amato A., Giannini M., Carretta A., Tummolo R.A., Buquicchio R. Incidence of allergic diseases in an elderly population. Immunopharmacol Immunotoxicol. 2010;32:165–170. doi: 10.3109/08923970903213735. [DOI] [PubMed] [Google Scholar]
- 78.Leonardi A., Castegnaro A., Valerio A.L., Lazzarini D. Epidemiology of allergic conjunctivitis: clinical appearance and treatment patterns in a population-based study. Curr Opin Allergy Clin Immunol. 2015;15:482–488. doi: 10.1097/ACI.0000000000000204. [DOI] [PubMed] [Google Scholar]
- 79.Singh S., Donthineni P.R., Shanbhag S.S., Senthil S., Ong H.S., Dart J.K., et al. Drug induced cicatrizing conjunctivitis: a case series with review of etiopathogenesis, diagnosis and management. Ocul Surf. 2022;24:83–92. doi: 10.1016/j.jtos.2022.02.004. [DOI] [PubMed] [Google Scholar]
- 80.Jung S.J., Mehta J.S., Tong L. Effects of environment pollution on the ocular surface. Ocul Surf. 2018;16:198–205. doi: 10.1016/j.jtos.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 81.Cicinelli M.V., Marchese A., Bandello F., Modorati G. Clinical management of ocular surface squamous neoplasia: a review of the current evidence. Ophthalmol Therap. 2018;7:247–262. doi: 10.1007/s40123-018-0140-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Darwich R., Ghazawi F.M., Le M., Rahme E., Alghazawi N., Zubarev A., et al. Epidemiology of invasive ocular surface squamous neoplasia in Canada during 1992-2010. Br J Ophthalmol. 2020;104:1368–1372. doi: 10.1136/bjophthalmol-2019-314650. [DOI] [PubMed] [Google Scholar]
- 83.Kiire C.A., Stewart R.M.K., Srinivasan S., Heimann H., Kaye S.B., Dhillon B. A prospective study of the incidence, associations and outcomes of ocular surface squamous neoplasia in the United Kingdom. Eye. 2019;33:283–294. doi: 10.1038/s41433-018-0217-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kim B.H., Kim M.K., Wee W.R., Oh J.Y. Clinical and pathological characteristics of ocular surface squamous neoplasia in an Asian population. Graefe’s Arch Clin Exp Ophthalmol. 2013;251:2569–2573. doi: 10.1007/s00417-013-2450-0. [DOI] [PubMed] [Google Scholar]
- 85.Maudgil A., Patel T., Rundle P., Rennie I.G., Mudhar H.S. Ocular surface squamous neoplasia: analysis of 78 cases from a UK ocular oncology centre. Br J Ophthalmol. 2013;97:1520–1524. doi: 10.1136/bjophthalmol-2013-303338. [DOI] [PubMed] [Google Scholar]
- 86.McClellan A.J., McClellan A.L., Pezon C.F., Karp C.L., Feuer W., Galor A. Epidemiology of ocular surface squamous neoplasia in a veterans affairs population. Cornea. 2013;32:1354–1358. doi: 10.1097/ICO.0b013e31829e3c80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ramberg I., Heegaard S., Prause J.U., Sjö N.C., Toft P.B. Squamous cell dysplasia and carcinoma of the conjunctiva. A nationwide, retrospective, epidemiological study of Danish patients. Acta Ophthalmol. 2015;93:663–666. doi: 10.1111/aos.12743. [DOI] [PubMed] [Google Scholar]
- 88.Shields C.L., Alset A.E., Boal N.S., Casey M.G., Knapp A.N., Sugarman J.A., et al. Conjunctival tumors in 5002 cases. Comparative analysis of benign versus malignant counterparts. The 2016 james D. Allen lecture. Am J Ophthalmol. 2017;173:106–133. doi: 10.1016/j.ajo.2016.09.034. [DOI] [PubMed] [Google Scholar]
- 89.Fasina O. Ocular surface squamous neoplasia at a tertiary eye facility, Southwestern Nigeria: a 10-year review. Int Ophthalmol. 2021;41:3325–3331. doi: 10.1007/s10792-021-01894-y. [DOI] [PubMed] [Google Scholar]
- 90.Furahini G., Lewallen S. Epidemiology and management of ocular surface squamous neoplasia in Tanzania. Ophthalmic Epidemiol. 2010;17:171–176. doi: 10.3109/09286581003731544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gichuhi S., Macharia E., Kabiru J., Zindamoyen AMb, Rono H., Ollando E., et al. Risk factors for ocular surface squamous neoplasia in Kenya: a case-control study. Trop Med Int Health. 2016;21:1522–1530. doi: 10.1111/tmi.12792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Meel R., Dhiman R., Vanathi M., Pushker N., Tandon R., Devi S. Clinicodemographic profile and treatment outcome in patients of ocular surface squamous neoplasia. Indian J Ophthalmol. 2017;65:936–941. doi: 10.4103/ijo.IJO_251_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pellerano F., Gil G., Rosario A., Mañon N., Vargas T., Vizcaíno G. Survey of 138 conjunctival tumors in the Dominican republic. Ophthalmic Epidemiol. 2020;27:278–282. doi: 10.1080/09286586.2020.1730912. [DOI] [PubMed] [Google Scholar]
- 94.Tananuvat N., Niparugs M., Wiwatwongwana D., Lertprasertsuk N., Mahanupap P. Ocular surface squamous neoplasia in Northern Thailand: a 16-year review. BMC Ophthalmol. 2022;22:121. doi: 10.1186/s12886-022-02340-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gichuhi S., Macharia E., Kabiru J., Zindamoyen A.M., Rono H., Ollando E., et al. Clinical presentation of ocular surface squamous neoplasia in Kenya. JAMA Ophthalmology. 2015;133:1305–1313. doi: 10.1001/jamaophthalmol.2015.3335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gichuhi S., Sagoo M.S., Weiss H.A., Burton M.J. Epidemiology of ocular surface squamous neoplasia in Africa. Trop Med Int Health. 2013;18:1424–1443. doi: 10.1111/tmi.12203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Carreira H., Coutinho F., Carrilho C., Lunet N. HIV and HPV infections and ocular surface squamous neoplasia: systematic review and meta-analysis. Br J Cancer. 2013;109:1981–1988. doi: 10.1038/bjc.2013.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ramberg I. Human papillomavirus-related neoplasia of the ocular adnexa. Acta Ophthalmol. 2022;100:3–33. doi: 10.1111/aos.15244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hӧllhumer R., Williams S., Michelow P. Observational study of ocular surface squamous neoplasia: risk factors, diagnosis, management and outcomes at a tertiary eye hospital in South Africa. PLoS One. 2020;15 doi: 10.1371/journal.pone.0237453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kaštelan S., Gverović Antunica A., Beketić Orešković L., Salopek Rabatić J., Kasun B., Bakija I. Conjunctival melanoma - epidemiological trends and features. Pathol Oncol Res. 2018;24:787–796. doi: 10.1007/s12253-018-0419-3. [DOI] [PubMed] [Google Scholar]
- 101.Ghazawi F.M., Darwich R., Le M., Jfri A., Rahme E., Burnier J.V., et al. Incidence trends of conjunctival malignant melanoma in Canada. Br J Ophthalmol. 2020;104:23–25. doi: 10.1136/bjophthalmol-2019-313977. [DOI] [PubMed] [Google Scholar]
- 102.Jain P., Finger P.T., Fili M., Damato B., Coupland S.E., Heimann H., et al. Conjunctival melanoma treatment outcomes in 288 patients: a multicentre international data-sharing study. Br J Ophthalmol. 2021;105:1358–1364. doi: 10.1136/bjophthalmol-2020-316293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Larsen A.C. Conjunctival malignant melanoma in Denmark: epidemiology, treatment and prognosis with special emphasis on tumorigenesis and genetic profile. Acta Ophthalmol. 2016;94:1–27. doi: 10.1111/aos.13100. [DOI] [PubMed] [Google Scholar]
- 104.Vaidya S., Dalvin L.A., Yaghy A., Pacheco R., Shields J.A., Lally S.E., et al. Conjunctival melanoma: risk factors for recurrent or new tumor in 540 patients at a single ocular oncology center. Eur J Ophthalmol. 2021;31:2675–2685. doi: 10.1177/1120672120970393. [DOI] [PubMed] [Google Scholar]
- 105.Virgili G., Parravano M., Gatta G., Capocaccia R., Mazzini C., Mallone S., et al. Incidence and survival of patients with conjunctival melanoma in europe. JAMA Ophthalmology. 2020;138:601–608. doi: 10.1001/jamaophthalmol.2020.0531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Dalvin L.A., Yaghy A., Vaidya S., Pacheco R.R., Perez A.L., Lally S.E., et al. Conjunctival melanoma: outcomes based on age at presentation in 629 patients at a single ocular oncology center. Cornea. 2021;40:554–563. doi: 10.1097/ICO.0000000000002449. [DOI] [PubMed] [Google Scholar]
- 107.Kirkegaard M.M., Coupland S.E., Prause J.U., Heegaard S. Malignant lymphoma of the conjunctiva. Surv Ophthalmol. 2015;60:444–458. doi: 10.1016/j.survophthal.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 108.Kirkegaard M.M., Rasmussen P.K., Coupland S.E., Esmaeli B., Finger P.T., Graue G.F., et al. Conjunctival lymphoma—an international multicenter retrospective study. JAMA Ophthalmology. 2016;134:406–414. doi: 10.1001/jamaophthalmol.2015.6122. [DOI] [PubMed] [Google Scholar]
- 109.Sullivan D.A., Rocha E.M., Aragona P., Clayton J.A., Ding J., Golebiowski B., et al. TFOS DEWS II sex, gender, and hormones report. Ocul Surf. 2017;15:284–333. doi: 10.1016/j.jtos.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 110.Aninye I.O., Digre K., Hartnett M.E., Baldonado K., Shriver E.M., Periman L.M., et al. The roles of sex and gender in women's eye health disparities in the United States. Biol Sex Differ. 2021;12:57. doi: 10.1186/s13293-021-00401-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kronzer V.L., Bridges S.L., Jr., Davis J.M., 3rd Why women have more autoimmune diseases than men: an evolutionary perspective. Evolut Appl. 2021;14:629–633. doi: 10.1111/eva.13167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Schaumberg D.A., Sullivan D.A., Buring J.E., Dana M.R. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136:318–326. doi: 10.1016/s0002-9394(03)00218-6. [DOI] [PubMed] [Google Scholar]
- 113.Schaumberg D.A., Dana R., Buring J.E., Sullivan D.A. Prevalence of dry eye disease among US men. Estimates from the physicians' health studies. Arch Ophthalmol. 2009;127:763–768. doi: 10.1001/archophthalmol.2009.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Schein O.D., MuÑOz B., Tielsch J.M., Bandeen-Roche K., West S. Prevalence of dry eye among the elderly. Am J Ophthalmol. 1997;124:723–728. doi: 10.1016/s0002-9394(14)71688-5. [DOI] [PubMed] [Google Scholar]
- 115.Racine M., Tousignant-Laflamme Y., Kloda L.A., Dion D., Dupuis G., Choiniere M. A systematic literature review of 10 years of research on sex/gender and experimental pain perception - part 1: are there really differences between women and men? Pain. 2012;153:602–618. doi: 10.1016/j.pain.2011.11.025. [DOI] [PubMed] [Google Scholar]
- 116.Li W., Lin M.C. Sex disparity in how pain sensitivity influences dry eye symptoms. Cornea. 2019;38:1291–1298. doi: 10.1097/ICO.0000000000002050. [DOI] [PubMed] [Google Scholar]
- 117.Vehof J., Smitt-Kamminga N.S., Nibourg S.A., Hammond C.J. Sex differences in clinical characteristics of dry eye disease. Ocul Surf. 2018;16:242–248. doi: 10.1016/j.jtos.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 118.Uchino M., Dogru M., Yagi Y., Goto E., Tomita M., Kon T., et al. The features of dry eye disease in a Japanese elderly population. Optom Vis Sci. 2006;83:797–802. doi: 10.1097/01.opx.0000232814.39651.fa. [DOI] [PubMed] [Google Scholar]
- 119.Hashemi H., Asharlous A., Aghamirsalim M., Yekta A., Pourmatin R., Sajjadi M., et al. Meibomian gland dysfunction in geriatric population: tehran geriatric eye study. Int Ophthalmol. 2021;41:2539–2546. doi: 10.1007/s10792-021-01812-2. [DOI] [PubMed] [Google Scholar]
- 120.Lomholt J.A., Ehlers N. Graft survival and risk factors of penetrating keratoplasty for microbial keratitis. Acta Ophthalmol Scand. 1997;75:418–422. doi: 10.1111/j.1600-0420.1997.tb00405.x. [DOI] [PubMed] [Google Scholar]
- 121.Magalhaes O.A., Marafon S.B., Ferreira R.C. Gender differences in keratoconus keratoplasty: a 25-year study in Southern Brazil and global perspective. Int Ophthalmol. 2018;38:1627–1633. doi: 10.1007/s10792-017-0634-z. [DOI] [PubMed] [Google Scholar]
- 122.Connor Cgf L.L., Hall C.W. The influence of gender on the ocular surface. J Am Optom Assoc. 1999;70:182–186. [PubMed] [Google Scholar]
- 123.Lahoti S., Weiss M., Johnson D.A., Kheirkhah A. Superior limbic keratoconjunctivitis: a comprehensive review. Surv Ophthalmol. 2022;67:331–341. doi: 10.1016/j.survophthal.2021.05.009. [DOI] [PubMed] [Google Scholar]
- 124.Groessl S.A., Sires B.S., Lemke B.N. An anatomical basis for primary acquired nasolacrimal duct obstruction. Arch Ophthalmol. 1997;115:71–74. doi: 10.1001/archopht.1997.01100150073012. [DOI] [PubMed] [Google Scholar]
- 125.Krishnan T., Prajna N.V., Gronert K., Oldenburg C.E., Ray K.J., Keenan J.D., et al. Gender differences in re-epithelialisation time in fungal corneal ulcers. Br J Ophthalmol. 2012;96:137–138. doi: 10.1136/bjophthalmol-2011-300441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Keita S.O.Y., Kittles R.A., Royal C.D.M., Bonney G.E., Furbert-Harris P., Dunston G.M., et al. Conceptualizing human variation. Nat Genet. 2004;36:S17–S20. doi: 10.1038/ng1455. [DOI] [PubMed] [Google Scholar]
- 127.Hassanzadeh S., Varmaghani M., Zarei-Ghanavati S., Heravian Shandiz J., Azimi Khorasani A. Global prevalence of meibomian gland dysfunction: a systematic review and meta-analysis. Ocul Immunol Inflamm. 2021;29:66–75. doi: 10.1080/09273948.2020.1755441. [DOI] [PubMed] [Google Scholar]
- 128.Craig J.P., Lim J., Han A., Tien L., Xue A.L., Wang M.T.M. Ethnic differences between the Asian and Caucasian ocular surface: a co-located adult migrant population cohort study. Ocul Surf. 2019;17:83–88. doi: 10.1016/j.jtos.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 129.Brown L., Leck A.K., Gichangi M., Burton M.J., Denning D.W. The global incidence and diagnosis of fungal keratitis. Lancet Infect Dis. 2021;21:e49–e57. doi: 10.1016/S1473-3099(20)30448-5. [DOI] [PubMed] [Google Scholar]
- 130.Fernandes A.G., Alves M., Nascimento R.A.E., Valdrighi N.Y., de Almeida R.C., Nakano C.T. Visual impairment and blindness in the xingu indigenous park - Brazil. Int J Equity Health. 2021;20:197. doi: 10.1186/s12939-021-01536-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Furtado J.M., Berezovsky A., Ferraz N.N., Muñoz S., Fernandes A.G., Watanabe S.S., et al. Prevalence and causes of visual impairment and blindness in adults aged 45 Years and older from parintins: the Brazilian amazon region eye survey. Ophthalmic Epidemiol. 2019;26:345–354. doi: 10.1080/09286586.2019.1624783. [DOI] [PubMed] [Google Scholar]
- 132.Quinn E.K., Massey P.D., Speare R. Communicable diseases in rural and remote Australia: the need for improved understanding and action. Rural Rem Health. 2015;15:3371. [PubMed] [Google Scholar]
- 133.Foreman J., Keel S., van Wijngaarden P., Bourne R.A., Wormald R., Crowston J., et al. Prevalence and causes of visual loss among the indigenous peoples of the world: a systematic review. JAMA Ophthalmology. 2018;136:567–580. doi: 10.1001/jamaophthalmol.2018.0597. [DOI] [PubMed] [Google Scholar]
- 134.Ang M., Li X., Wong W., Zheng Y., Chua D., Rahman A., et al. Prevalence of and racial differences in pterygium: a multiethnic population study in Asians. Ophthalmology. 2012;119:1509–1515. doi: 10.1016/j.ophtha.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 135.Na K.S., Mok J.W., Kim J.Y., Joo C.K. Proinflammatory gene polymorphisms are potentially associated with Korean non-Sjogren dry eye patients. Mol Vis. 2011;17:2818–2823. [PMC free article] [PubMed] [Google Scholar]
- 136.He Y., Li X., Bao Y., Sun J., Liu J. [The correlation of polymorphism of estrogen receptor gene to dry eye syndrome in postmenopausal women] Eye Sci. 2006;22:233–236. [PubMed] [Google Scholar]
- 137.Imbert Y., Foulks G.N., Brennan M.D., Jumblatt M.M., John G., Shah H.A., et al. MUC1 and estrogen receptor α gene polymorphisms in dry eye patients. Exp Eye Res. 2009;88:334–338. doi: 10.1016/j.exer.2008.05.019. [DOI] [PubMed] [Google Scholar]
- 138.Imbert Y., Darling D.S., Jumblatt M.M., Foulks G.N., Couzin E.G., Steele P.S., et al. MUC1 splice variants in human ocular surface tissues: possible differences between dry eye patients and normal controls. Exp Eye Res. 2006;83:493–501. doi: 10.1016/j.exer.2006.01.031. [DOI] [PubMed] [Google Scholar]
- 139.Contreras-Ruiz L., Ryan D.S., Sia R.K., Bower K.S., Dartt D.A., Masli S. Polymorphism in THBS1 gene is associated with post-refractive surgery chronic ocular surface inflammation. Ophthalmology. 2014;121:1389–1397. doi: 10.1016/j.ophtha.2014.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lee L., Garrett Q., Flanagan J., Chakrabarti S., Papas E. Genetic factors and molecular mechanisms in dry eye disease. Ocul Surf. 2018;16:206–217. doi: 10.1016/j.jtos.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 141.Portelli M.A., Hodge E., Sayers I. Genetic risk factors for the development of allergic disease identified by genome-wide association. Clin Exp Allergy. 2015;45:21–31. doi: 10.1111/cea.12327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kumar S. Vernal keratoconjunctivitis: a major review. Acta Ophthalmol. 2009;87:133–147. doi: 10.1111/j.1755-3768.2008.01347.x. [DOI] [PubMed] [Google Scholar]
- 143.Guglielmetti S., Dart J.K., Calder V. Atopic keratoconjunctivitis and atopic dermatitis. Curr Opin Allergy Clin Immunol. 2010;10:478–485. doi: 10.1097/ACI.0b013e32833e16e4. [DOI] [PubMed] [Google Scholar]
- 144.Gomez J.A.P. TFOS Lifestyle Report: impact of elective medications and procedures on the ocular surface. Ocul Surf. 2023 doi: 10.1016/j.jtos.2023.04.011. In press. [DOI] [PubMed] [Google Scholar]
- 145.Roh H.C., Lee J.K., Kim M., Oh J.H., Chang M.W., Chuck R.S., et al. Systemic comorbidities of dry eye syndrome: the Korean national health and nutrition examination survey V, 2010 to 2012. Cornea. 2016;35:187–192. doi: 10.1097/ICO.0000000000000657. [DOI] [PubMed] [Google Scholar]
- 146.Wang T.J., Wang I.J., Hu C.C., Lin H.C. Comorbidities of dry eye disease: a nationwide population-based study. Acta Ophthalmol. 2012;90:663–668. doi: 10.1111/j.1755-3768.2010.01993.x. [DOI] [PubMed] [Google Scholar]
- 147.Wolpert L.E., Snieder H., Jansonius N.M., Utheim T.P., Hammond C.J., Vehof J. Medication use and dry eye symptoms: a large, hypothesis-free, population-based study in The Netherlands. Ocul Surf. 2021;22:1–12. doi: 10.1016/j.jtos.2021.06.009. [DOI] [PubMed] [Google Scholar]
- 148.Asbell P.A., Maguire M.G., Peskin E., Bunya V.Y., Kuklinski E.J. Dry eye assessment and management (DREAM©) study: study design and baseline characteristics. Contemp Clin Trials. 2018;71:70–79. doi: 10.1016/j.cct.2018.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Yu K., Bunya V., Maguire M., Asbell P., Ying G.S. Systemic conditions associated with severity of dry eye signs and symptoms in the dry eye assessment and management study. Ophthalmology. 2021;128:1384–1392. doi: 10.1016/j.ophtha.2021.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Psianou K., Panagoulias I., Papanastasiou A.D., de Lastic A.-L., Rodi M., Spantidea P.I., et al. Clinical and immunological parameters of Sjögren's syndrome. Autoimmun Rev. 2018;17:1053–1064. doi: 10.1016/j.autrev.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 151.Knop E., Knop N., Millar T., Obata H., Sullivan D.A. The international workshop on meibomian gland dysfunction: report of the subcommittee on anatomy, physiology, and pathophysiology of the meibomian gland. Invest Ophthalmol Vis Sci. 2011;52:1938–1978. doi: 10.1167/iovs.10-6997c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Fernandez Castro M., Sánchez-Piedra C., Andreu J.L., Martínez Taboada V., Olivé A., Rosas J. Factors associated with severe dry eye in primary Sjögren's syndrome diagnosed patients. Rheumatol Int. 2018;38:1075–1082. doi: 10.1007/s00296-018-4013-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Wallace L.S., Wexler R.K., McDougle L., Miser W.F., Haddox J.D. Voices that may not otherwise be heard: a qualitative exploration into the perspectives of primary care patients living with chronic pain. J Pain Res. 2014;7:291–299. doi: 10.2147/JPR.S62317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Williamson J.F., Huynh K., Weaver M.A., Davis R.M. Perceptions of dry eye disease management in current clinical practice. Eye Contact Lens. 2014;40:111–115. doi: 10.1097/ICL.0000000000000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Galor A., Feuer W., Lee D.J., Florez H., Faler A.L., Zann K.L., et al. Depression, post-traumatic stress disorder, and dry eye syndrome: a study utilizing the national United States Veterans Affairs administrative database. Am J Ophthalmol. 2012;154 doi: 10.1016/j.ajo.2012.02.009. 340-6.e2. [DOI] [PubMed] [Google Scholar]
- 156.Fernandez C.A., Galor A., Arheart K.L., Musselman D.L., Venincasa V.D., Florez H.J., et al. Dry eye syndrome, posttraumatic stress disorder, and depression in an older male veteran population. Invest Ophthalmol Vis Sci. 2013;54:3666–3672. doi: 10.1167/iovs.13-11635. [DOI] [PubMed] [Google Scholar]
- 157.Kawashima M., Yamada M., Shigeyasu C., Suwaki K., Uchino M., Hiratsuka Y., et al. Association of systemic comorbidities with dry eye disease. J Clin Med. 2020;9:2040. doi: 10.3390/jcm9072040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Morthen M.K., Magno M.S., Utheim T.P., Snieder H., Hammond C.J., Vehof J. The physical and mental burden of dry eye disease: a large population-based study investigating the relationship with health-related quality of life and its determinants. Ocul Surf. 2021;21:107–117. doi: 10.1016/j.jtos.2021.05.006. [DOI] [PubMed] [Google Scholar]
- 159.Magno M.S., Utheim T.P., Snieder H., Hammond C.J., Vehof J. The relationship between dry eye and sleep quality. Ocul Surf. 2021;20:13–19. doi: 10.1016/j.jtos.2020.12.009. [DOI] [PubMed] [Google Scholar]
- 160.Galor A., Seiden B.E., Park J.J., Feuer W.J., McClellan A.L., Felix E.R., et al. The association of dry eye symptom severity and comorbid insomnia in US veterans. Eye Contact Lens. 2018;44(Suppl 1) doi: 10.1097/ICL.0000000000000349. S118-s24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Yu X., Guo H., Liu X., Wang G., Min Y., Chen S.S., et al. Dry eye and sleep quality: a large community-based study in Hangzhou. Sleep. 2019;42 doi: 10.1093/sleep/zsz160. [DOI] [PubMed] [Google Scholar]
- 162.Bitar M.S., Olson D.J., Li M., Davis R.M. The correlation between dry eyes, anxiety and depression: the sicca, anxiety and depression study. Cornea. 2019;38:684–689. doi: 10.1097/ICO.0000000000001932. [DOI] [PubMed] [Google Scholar]
- 163.Um S.B., Yeom H., Kim N.H., Kim H.C., Lee H.K., Suh I. Association between dry eye symptoms and suicidal ideation in a Korean adult population. PLoS One. 2018;13 doi: 10.1371/journal.pone.0199131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Stapleton F., Shrestha G.S., Vijay A.K., Carnt N. Epidemiology, microbiology, and genetics of contact lens–related and non–contact lens-related infectious keratitis. Eye Contact Lens. 2022;48:127–133. doi: 10.1097/ICL.0000000000000884. [DOI] [PubMed] [Google Scholar]
- 165.Sobol E.K., Fargione R.A., Atiya M., Diaz J.D., Powell J.A., Gritz D.C. Case-control study of herpes simplex eye disease: bronx epidemiology of human immunodeficiency virus eye studies. Cornea. 2016;35:801–806. doi: 10.1097/ICO.0000000000000814. [DOI] [PubMed] [Google Scholar]
- 166.Rosenberg C.R., Abazari A., Chou T.Y., Weissbart S.B. Comparison of comorbid associations and ocular complications in herpes simplex and zoster keratitis. Ocul Immunol Inflamm. 2022;30:57–61. doi: 10.1080/09273948.2020.1797115. [DOI] [PubMed] [Google Scholar]
- 167.Jeng B.H., Gritz D.C., Kumar A.B., Holsclaw D.S., Porco T.C., Smith S.D., et al. Epidemiology of ulcerative keratitis in northern California. Arch Ophthalmol. 2010;128:1022–1028. doi: 10.1001/archophthalmol.2010.144. [DOI] [PubMed] [Google Scholar]
- 168.Liu J., Dong Y., Wang Y. Vitamin D deficiency is associated with dry eye syndrome: a systematic review and meta-analysis. Acta Ophthalmol. 2020;98:749–754. doi: 10.1111/aos.14470. [DOI] [PubMed] [Google Scholar]
- 169.Pellegrini M., Senni C., Bernabei F., Cicero A.F.G., Vagge A., Maestri A., et al. The role of nutrition and nutritional supplements in ocular surface diseases. Nutrients. 2020;12 doi: 10.3390/nu12040952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Tokumaru O., Fujita M., Nagai S., Minamikawa Y., Kumatani J. Medical problems and concerns with temporary evacuation shelters after great earthquake disasters in Japan: a systematic review. Disaster Med Public Health Prep. 2021:1–8. doi: 10.1017/dmp.2021.99. [DOI] [PubMed] [Google Scholar]
- 171.An R., Ji M., Zhang S. Global warming and obesity: a systematic review. Obes Rev. 2018;19:150–163. doi: 10.1111/obr.12624. [DOI] [PubMed] [Google Scholar]
- 172.Khor G.L., Sharif Z.M. Dual forms of malnutrition in the same households in Malaysia--a case study among Malay rural households. Asia Pac J Clin Nutr. 2003;12:427–437. [PubMed] [Google Scholar]
- 173.Steyn N.P., Labadarios D., Maunder E., Nel J., Lombard C. Secondary anthropometric data analysis of the National Food Consumption Survey in South Africa: the double burden. Nutrition. 2005;21:4–13. doi: 10.1016/j.nut.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 174.Littlejohn P., Finlay B.B. When a pandemic and an epidemic collide: COVID-19, gut microbiota, and the double burden of malnutrition. BMC Med. 2021;19:31. doi: 10.1186/s12916-021-01910-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Wells J.C., Sawaya A.L., Wibaek R., Mwangome M., Poullas M.S., Yajnik C.S., et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. 2020;395:75–88. doi: 10.1016/S0140-6736(19)32472-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Akhtar S., Ahmed A., Randhawa M.A., Atukorala S., Arlappa N., Ismail T., et al. Prevalence of vitamin A deficiency in South Asia: causes, outcomes, and possible remedies. J Health Popul Nutr. 2013;31:413–423. doi: 10.3329/jhpn.v31i4.19975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Carlier C., Moulia-Pelat J.P., Ceccon J.F., Mourey M.S., Ameline B., Fall M., et al. Prevalence of malnutrition and vitamin A deficiency in the Diourbel, Fatick, and Kaolack regions of Senegal: epidemiological study. Am J Clin Nutr. 1991;53:70–73. doi: 10.1093/ajcn/53.1.70. [DOI] [PubMed] [Google Scholar]
- 178.Hjellbakk V.K., Hailemariam H., Reta F., Engebretsen I.M.S. Diet and nutritional status among hospitalised children in Hawassa, Southern Ethiopia. BMC Pediatr. 2022;22:57. doi: 10.1186/s12887-022-03107-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Adeyeye S.A.O., Ashaolu T.J., Bolaji O.T., Abegunde T.A., Omoyajowo A.O. Africa and the Nexus of poverty, malnutrition and diseases. Crit Rev Food Sci Nutr. 2021:1–16. doi: 10.1080/10408398.2021.1952160. [DOI] [PubMed] [Google Scholar]
- 180.Pirrie M., Harrison L., Angeles R., Marzanek F., Ziesmann A., Agarwal G. Poverty and food insecurity of older adults living in social housing in Ontario: a cross-sectional study. BMC Publ Health. 2020;20:1320. doi: 10.1186/s12889-020-09437-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Jia J., Fung V., Meigs J.B., Thorndike A.N. Food insecurity, dietary quality, and health care utilization in lower-income adults: a cross-sectional study. J Acad Nutr Diet. 2021;121 doi: 10.1016/j.jand.2021.06.001. 2177-86.e3. [DOI] [PubMed] [Google Scholar]
- 182.Azzarri C., Signorelli S. Climate and poverty in Africa south of the Sahara. World Dev. 2020;125 doi: 10.1016/j.worlddev.2019.104691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Soergel B., Kriegler E., Bodirsky B.L., Bauer N., Leimbach M., Popp A. Combining ambitious climate policies with efforts to eradicate poverty. Nat Commun. 2021;12:2342. doi: 10.1038/s41467-021-22315-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Alkire S., Nogales R., Quinn N.N., Suppa N. Global multidimensional poverty and COVID-19: a decade of progress at risk? Soc Sci Med. 2021;291 doi: 10.1016/j.socscimed.2021.114457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Ribeiro-Silva R.C., Pereira M., Campello T., Aragão É., Guimarães J.M.M., Ferreira A.J., et al. Covid-19 pandemic implications for food and nutrition security in Brazil. Ciência Saúde Coletiva. 2020;25:3421–3430. doi: 10.1590/1413-81232020259.22152020. [DOI] [PubMed] [Google Scholar]
- 186.Ribeiro-Silva R.C., Pereira M., Aragão É., Guimarães J.M.M., Ferreira A.J.F., Rocha A.D.S., et al. COVID-19, food insecurity and malnutrition: a multiple burden for Brazil. Front Nutr. 2021;8 doi: 10.3389/fnut.2021.751715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Niles M.T., Bertmann F., Belarmino E.H., Wentworth T., Biehl E., Neff R. The early food insecurity impacts of COVID-19. Nutrients. 2020:12. doi: 10.3390/nu12072096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Pereira M., Oliveira A.M. Poverty and food insecurity may increase as the threat of COVID-19 spreads. Publ Health Nutr. 2020;23:3236–3240. doi: 10.1017/S1368980020003493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.C R., S S., Monk J. Exploring barriers to food security among immigrants: a critical role for public health nutrition. Can J Diet Pract Res. 2022:1–7. doi: 10.3148/cjdpr-2021-032. [DOI] [PubMed] [Google Scholar]
- 190.Jolly A., Thompson J.L. Risk of food insecurity in undocumented migrant households in Birmingham, UK. J Public Health. 2022 doi: 10.1093/pubmed/fdab408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Saeedullah A., Khan M.S., Andrews S.C., Iqbal K., Ul-Haq Z., Qadir S.A., et al. Nutritional status of adolescent Afghan refugees living in peshawar, Pakistan. Nutrients. 2021:13. doi: 10.3390/nu13093072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Cho Y.A., Kim D.Y., Choue R., Lim H. Changes in dietary quality among Vietnamese women immigrants in Korea and comparison with Korean women. Clin Nutr Res. 2018;7:178–188. doi: 10.7762/cnr.2018.7.3.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Harkensee C., Andrew R. Health needs of accompanied refugee and asylum-seeking children in a UK specialist clinic. Acta Paediatr. 2021;110:2396–2404. doi: 10.1111/apa.15861. [DOI] [PubMed] [Google Scholar]
- 194.Moskowitz L., Weiselberg E. Anorexia nervosa/atypical anorexia nervosa. Curr Probl Pediatr Adolesc Health Care. 2017;47:70–84. doi: 10.1016/j.cppeds.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 195.van Eeden A.E., van Hoeken D., Hoek H.W. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatr. 2021;34:515–524. doi: 10.1097/YCO.0000000000000739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Cybulski L., Ashcroft D.M., Carr M.J., Garg S., Chew-Graham C.A., Kapur N., et al. Temporal trends in annual incidence rates for psychiatric disorders and self-harm among children and adolescents in the UK, 2003-2018. BMC Psychiatr. 2021;21:229. doi: 10.1186/s12888-021-03235-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Termorshuizen J.D., Watson H.J., Thornton L.M., Borg S., Flatt R.E., MacDermod C.M., et al. Early impact of COVID-19 on individuals with self-reported eating disorders: a survey of ∼1,000 individuals in the United States and The Netherlands. Int J Eat Disord. 2020;53:1780–1790. doi: 10.1002/eat.23353. [DOI] [PubMed] [Google Scholar]
- 198.Branley-Bell D., Talbot C.V. Exploring the impact of the COVID-19 pandemic and UK lockdown on individuals with experience of eating disorders. J Eat Disord. 2020;8:44. doi: 10.1186/s40337-020-00319-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Dumitrașcu M.C., Șandru F., Carsote M., Petca R.C., Gheorghisan-Galateanu A.A., Petca A., et al. Anorexia nervosa: COVID-19 pandemic period (Review) Exp Ther Med. 2021;22:804. doi: 10.3892/etm.2021.10236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Phillipou A., Woods W., Abel L.A., Rossell S.L., Hughes M.E., Castle D.J., et al. Spontaneous blink rate in anorexia nervosa: implications for dopaminergic activity in anorexia nervosa. Aust N Z J Psychiatr. 2018;52:713–714. doi: 10.1177/0004867417739692. [DOI] [PubMed] [Google Scholar]
- 201.Woodruff P.W., Morton J., Russell G.F. Neuromyopathic complications in a patient with anorexia nervosa and vitamin C deficiency. Int J Eat Disord. 1994;16:205–209. doi: 10.1002/1098-108x(199409)16:2<205::aid-eat2260160212>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 202.Gaudiani J.L., Braverman J.M., Mascolo M., Mehler P.S. Lagophthalmos in severe anorexia nervosa: a case series. Arch Ophthalmol. 2012;130:928–930. doi: 10.1001/archophthalmol.2011.2515. [DOI] [PubMed] [Google Scholar]
- 203.Gilbert J.M., Weiss J.S., Sattler A.L., Koch J.M. Ocular manifestations and impression cytology of anorexia nervosa. Ophthalmology. 1990;97:1001–1007. doi: 10.1016/s0161-6420(90)32473-9. [DOI] [PubMed] [Google Scholar]
- 204.Endalifer M.L., Diress G. Epidemiology, predisposing factors, biomarkers, and prevention mechanism of obesity: a systematic review. J Obes. 2020;2020 doi: 10.1155/2020/6134362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Ng M., Fleming T., Robinson M., Thomson B., Graetz N., Margono C., et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Noubiap J.J., Nansseu J.R., Lontchi-Yimagou E., Nkeck J.R., Nyaga U.F., Ngouo A.T., et al. Global, regional, and country estimates of metabolic syndrome burden in children and adolescents in 2020: a systematic review and modelling analysis. Lancet Child Adolesc Health. 2022 doi: 10.1016/S2352-4642(21)00374-6. [DOI] [PubMed] [Google Scholar]
- 207.Baser G., Yildiz N., Calan M. Evaluation of meibomian gland dysfunction in polycystic ovary syndrome and obesity. Curr Eye Res. 2017;42:661–665. doi: 10.1080/02713683.2016.1233985. [DOI] [PubMed] [Google Scholar]
- 208.Hu J.Y., Liao Y., Huang C.H., Wang S., Liu Z.G. [Association between meibomian gland dysfunction and body mass index in Chinese adults] Zhonghua Yixue Zazhi. 2021;101:2514–2518. doi: 10.3760/cma.j.cn112137-20210223-00466. [DOI] [PubMed] [Google Scholar]
- 209.Gupta P.K., Venkateswaran N., Heinke J., Stinnett S.S. Association of meibomian gland architecture and body mass index in a pediatric population. Ocul Surf. 2020;18:657–662. doi: 10.1016/j.jtos.2020.06.009. [DOI] [PubMed] [Google Scholar]
- 210.Choi H.R., Kim N.H., Lee J.M., Choi D.P., Seo Y., Cho W.K., et al. Risk factors influencing the occurrence and severity of symptomatic dry eye syndrome: a cross-sectional study. Ophthalmic Epidemiol. 2021;28:488–494. doi: 10.1080/09286586.2021.1879172. [DOI] [PubMed] [Google Scholar]
- 211.Mussi N., Haque W., Robertson D.M. The association between risk factors for metabolic syndrome and meibomian gland disease in a dry eye cohort. Clin Ophthalmol. 2021;15:3821–3832. doi: 10.2147/OPTH.S322461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Choi H.R., Lee J.H., Lee H.K., Song J.S., Kim H.C. Association between dyslipidemia and dry eye syndrome among the Korean middle-aged population. Cornea. 2020;39:161–167. doi: 10.1097/ICO.0000000000002133. [DOI] [PubMed] [Google Scholar]
- 213.Tang Y.L., Cheng Y.L., Ren Y.P., Yu X.N., Shentu X.C. Metabolic syndrome risk factors and dry eye syndrome: a Meta-analysis. Int J Ophthalmol. 2016;9:1038–1045. doi: 10.18240/ijo.2016.07.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Kerimoglu H., Ozturk B., Gunduz K., Bozkurt B., Kamis U., Okka M. Effect of altered eating habits and periods during Ramadan fasting on intraocular pressure, tear secretion, corneal and anterior chamber parameters. Eye. 2010;24:97–100. doi: 10.1038/eye.2009.96. [DOI] [PubMed] [Google Scholar]
- 215.Sariri R., Varasteh A., Sajedi R.H. Effect of Ramadan fasting on tear proteins. Acta Med. 2010;53:147–151. doi: 10.14712/18059694.2016.74. [DOI] [PubMed] [Google Scholar]
- 216.Koktekir B.E., Bozkurt B., Gonul S., Gedik S., Okudan S. Effect of religious fasting on tear osmolarity and ocular surface. Eye Contact Lens. 2014;40:239–242. doi: 10.1097/ICL.0000000000000044. [DOI] [PubMed] [Google Scholar]
- 217.Armstrong B.K., Coc I.R., Agarwal P., Smith S., Navon S. Association of Ramadan daytime fasting with ocular surface inflammation and dry eye. Int Ophthalmol. 2019;39:2857–2863. doi: 10.1007/s10792-019-01133-5. [DOI] [PubMed] [Google Scholar]
- 218.Feng J., Zhang S., Li W., Bai T., Liu Y., Chang X. Intermittent fasting to the eye: a new dimension involved in physiological and pathological changes. Front Med. 2022;9 doi: 10.3389/fmed.2022.867624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Varady K.A., Cienfuegos S., Ezpeleta M., Gabel K. Clinical application of intermittent fasting for weight loss: progress and future directions. Nat Rev Endocrinol. 2022;18:309–321. doi: 10.1038/s41574-022-00638-x. [DOI] [PubMed] [Google Scholar]
- 220.Fernandes T.P., Hovis J.K., Almeida N., Souto J.J.S., Bonifacio T.A., Rodrigues S., et al. vol. 14. 2020. (Effects of nicotine gum administration on vision (ENIGMA-Vis): study protocol of a double-blind, randomized, and controlled clinical trial). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Altinors D.D., Akça S., Akova Y.A., Bilezikçi B., Goto E., Dogru M., et al. Smoking associated with damage to the lipid layer of the ocular surface. Am J Ophthalmol. 2006;141:1016–1021. doi: 10.1016/j.ajo.2005.12.047. [DOI] [PubMed] [Google Scholar]
- 222.Miglio F., Naroo S., Zeri F., Tavazzi S., Ponzini E. The effect of active smoking, passive smoking, and e-cigarettes on the tear film: an updated comprehensive review. Exp Eye Res. 2021;210 doi: 10.1016/j.exer.2021.108691. [DOI] [PubMed] [Google Scholar]
- 223.Uchino Y., Uchino M., Yokoi N., Dogru M., Kawashima M., Komuro A., et al. Impact of cigarette smoking on tear function and correlation between conjunctival goblet cells and tear MUC5AC concentration in office workers. Sci Rep. 2016;6 doi: 10.1038/srep27699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Moss S.E., Klein R., Klein B.E.K. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000;118:1264–1268. doi: 10.1001/archopht.118.9.1264. [DOI] [PubMed] [Google Scholar]
- 225.Nita M., Grzybowski A. Smoking and eye pathologies. A systemic review. Part I. Anterior eye segment pathologies. Curr Pharmaceut Des. 2017;23:629–638. doi: 10.2174/1381612822666161129152041. [DOI] [PubMed] [Google Scholar]
- 226.Jafari A., Rajabi A., Gholian-Aval M., Peyman N., Mahdizadeh M., Tehrani H. National, regional, and global prevalence of cigarette smoking among women/females in the general population: a systematic review and meta-analysis. Environ Health Prev Med. 2021;26:5. doi: 10.1186/s12199-020-00924-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Tezera N., Endalamaw A. Current cigarette smoking and its predictors among school-going adolescents in East Africa: a systematic review and meta-analysis. Int J Pediatr. 2019;2019 doi: 10.1155/2019/4769820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Wang J.W., Cao S.S., Hu R.Y. Smoking by family members and friends and electronic-cigarette use in adolescence: a systematic review and meta-analysis. Tob Induc Dis. 2018;16:5. doi: 10.18332/tid/84864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Amiri S. Smoking and alcohol use in unemployed populations: a systematic review and meta-analysis. J Addict Dis. 2021:1–24. doi: 10.1080/10550887.2021.1981124. [DOI] [PubMed] [Google Scholar]
- 230.Casetta B., Videla A.J., Bardach A., Morello P., Soto N., Lee K., et al. Association between cigarette smoking prevalence and income level: a systematic review and meta-analysis. Nicotine Tob Res. 2017;19:1401–1407. doi: 10.1093/ntr/ntw266. [DOI] [PubMed] [Google Scholar]
- 231.Amiri S. Worldwide prevalence of smoking in immigration: a global systematic review and meta-analysis. J Addict Dis. 2020;38:567–579. doi: 10.1080/10550887.2020.1800888. [DOI] [PubMed] [Google Scholar]
- 232.Taylor A.E., Fluharty M.E., Bjørngaard J.H., Gabrielsen M.E., Skorpen F., Marioni R.E., et al. Investigating the possible causal association of smoking with depression and anxiety using Mendelian randomisation meta-analysis: the CARTA consortium. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2014-006141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Fluharty M., Taylor A.E., Grabski M., Munafò M.R. The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine Tob Res. 2017;19:3–13. doi: 10.1093/ntr/ntw140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Mohidin N., Jaafar A.B. Effect of smoking on tear stability and corneal surface. J Curr Ophthalmol. 2020;32:232–237. doi: 10.4103/JOCO.JOCO_70_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Matsumoto Y., Dogru M., Goto E., Sasaki Y., Inoue H., Saito I., et al. Alterations of the tear film and ocular surface health in chronic smokers. Eye. 2008;22:961–968. doi: 10.1038/eye.2008.78. [DOI] [PubMed] [Google Scholar]
- 236.Thomas J., Jacob G.P., Abraham L., Noushad B. The effect of smoking on the ocular surface and the precorneal tear film. Australas Med J. 2012;5:221–226. doi: 10.4066/AMJ.2012.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Khalil H.E., Aboud S., Azzab M. Comparative study between smokers and nonsmokers regarding dry eye. Delta J Ophthalmol. 2018;19:9–13. [Google Scholar]
- 238.Masmali A.M., Al-Shehri A., Alanazi S.A., Abusharaha A., Fagehi R., El-Hiti G.A. Assessment of tear film quality among smokers using tear ferning patterns. J Ophthalmol. 2016;2016 doi: 10.1155/2016/8154315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Aktaş S., Tetikoğlu M., Koçak A., Kocacan M., Aktaş H., Sağdık H.M., et al. Impact of smoking on the ocular surface, tear function, and tear osmolarity. Curr Eye Res. 2017;42:1585–1589. doi: 10.1080/02713683.2017.1362005. [DOI] [PubMed] [Google Scholar]
- 240.Wang S., Zhao H., Huang C., Li Z., Li W., Zhang X., et al. Impact of chronic smoking on meibomian gland dysfunction. PLoS One. 2016;11 doi: 10.1371/journal.pone.0168763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Nur Amalina I., Koh P.Y., Doraj P. The tear function in electronic cigarette smokers. Optom Vis Sci. 2019;96:678–685. doi: 10.1097/OPX.0000000000001422. [DOI] [PubMed] [Google Scholar]
- 242.D'Isabella N.T., Shkredova D.A., Richardson J.A., Tang A. Effects of exercise on cardiovascular risk factors following stroke or transient ischemic attack: a systematic review and meta-analysis. Clin Rehabil. 2017;31:1561–1572. doi: 10.1177/0269215517709051. [DOI] [PubMed] [Google Scholar]
- 243.Quigley A., MacKay-Lyons M., Eskes G. Effects of exercise on cognitive performance in older adults: a narrative review of the evidence, possible biological mechanisms, and recommendations for exercise prescription. J Aging Res. 2020;2020 doi: 10.1155/2020/1407896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Sano K., Kawashima M., Ito A., Inaba T., Morimoto K., Watanabe M., et al. Aerobic exercise increases tear secretion in type 2 diabetic mice. Invest Ophthalmol Vis Sci. 2014;55:4287–4294. doi: 10.1167/iovs.13-13289. [DOI] [PubMed] [Google Scholar]
- 245.Hanyuda A., Sawada N., Uchino M., Kawashima M., Yuki K., Tsubota K., et al. Physical inactivity, prolonged sedentary behaviors, and use of visual display terminals as potential risk factors for dry eye disease: JPHC-NEXT study. Ocul Surf. 2020;18:56–63. doi: 10.1016/j.jtos.2019.09.007. [DOI] [PubMed] [Google Scholar]
- 246.Mineshita Y., Kim H.K., Chijiki H., Nanba T., Shinto T., Furuhashi S., et al. Screen time duration and timing: effects on obesity, physical activity, dry eyes, and learning ability in elementary school children. BMC Publ Health. 2021;21:422. doi: 10.1186/s12889-021-10484-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Sun C., Chen X., Huang Y., Zou H., Fan W., Yang M., et al. Effects of aerobic exercise on tear secretion and tear film stability in dry eye patients. BMC Ophthalmol. 2022;22:9. doi: 10.1186/s12886-021-02230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Sano K., Kawashima M., Takechi S., Mimura M., Tsubota K. Exercise program improved subjective dry eye symptoms for office workers. Clin Ophthalmol. 2018;12:307–311. doi: 10.2147/OPTH.S149986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Dartt D.A. Neural regulation of lacrimal gland secretory processes: relevance in dry eye diseases. Prog Retin Eye Res. 2009;28:155–177. doi: 10.1016/j.preteyeres.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Cumurcu T., Gunduz A., Cumurcu B.E., Gül I.G., Akpolat N., Karlidag R. The changes in tear film parameters and impression cytology in heavily drinking men. Cornea. 2013;32:237–241. doi: 10.1097/ICO.0b013e31825239d1. [DOI] [PubMed] [Google Scholar]
- 251.Kim J.H., Kim J.H., Nam W.H., Yi K., Choi D.G., Hyon J.Y., et al. Oral alcohol administration disturbs tear film and ocular surface. Ophthalmology. 2012;119:965–971. doi: 10.1016/j.ophtha.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 252.You Y.S., Qu N.B., Yu X.N. Alcohol consumption and dry eye syndrome: a Meta-analysis. Int J Ophthalmol. 2016;9:1487–1492. doi: 10.18240/ijo.2016.10.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Magno M.S., Daniel T., Morthen M.K., Snieder H., Jansonius N., Utheim T.P., et al. The relationship between alcohol consumption and dry eye. Ocul Surf. 2021;21:87–95. doi: 10.1016/j.jtos.2021.05.005. [DOI] [PubMed] [Google Scholar]
- 254.Lieber C.S. Alcohol, liver, and nutrition. J Am Coll Nutr. 1991;10:602–632. doi: 10.1080/07315724.1991.10718182. [DOI] [PubMed] [Google Scholar]
- 255.Karimi S., Arabi A., Shahraki T. Alcohol and the eye. J Ophthalmic Vis Res. 2021;16:260–270. doi: 10.18502/jovr.v16i2.9089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Sommer A. Effects of vitamin A deficiency on the ocular surface. Ophthalmology. 1983;90:592–600. doi: 10.1016/s0161-6420(83)34512-7. [DOI] [PubMed] [Google Scholar]
- 257.Viso E., Rodriguez-Ares M.T., Gude F. Prevalence of and associated factors for dry eye in a Spanish adult population (the Salnes Eye Study) Ophthalmic Epidemiol. 2009;16:15–21. doi: 10.1080/09286580802228509. [DOI] [PubMed] [Google Scholar]
- 258.Xu L., You Q.S., Jonas J.B. Prevalence of alcohol consumption and risk of ocular diseases in a general population: the Beijing Eye Study. Ophthalmology. 2009;116:1872–1879. doi: 10.1016/j.ophtha.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 259.Chia E.M., Mitchell P., Rochtchina E., Lee A.J., Maroun R., Wang J.J. Prevalence and associations of dry eye syndrome in an older population: the Blue Mountains Eye Study. Clin Exp Ophthalmol. 2003;31:229–232. doi: 10.1046/j.1442-9071.2003.00634.x. [DOI] [PubMed] [Google Scholar]
- 260.Zhang Y., Coca A., Casa D.J., Antonio J., Green J.M., Bishop P.A. Caffeine and diuresis during rest and exercise: a meta-analysis. J Sci Med Sport. 2015;18:569–574. doi: 10.1016/j.jsams.2014.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Jeong K.J., Choi J.G., Park E.J., Kim H.E., Yoo S.M., Park S.G. Relationship between dry eye syndrome and frequency of coffee consumption in Korean adults: Korea national health and nutrition examination survey V, 2010-2012. Korean J Fam Med. 2018;39:290–294. doi: 10.4082/kjfm.17.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Magno M.S., Utheim T.P., Morthen M.K., Snieder H., Jansonius N.M., Hammond C.J., et al. The relationship between caffeine intake and dry eye disease. Cornea. 2022;42:186–193. doi: 10.1097/ICO.0000000000002979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Moss S.E., Klein R., Klein B.E. Long-term incidence of dry eye in an older population. Optom Vis Sci. 2008;85:668–674. doi: 10.1097/OPX.0b013e318181a947. [DOI] [PubMed] [Google Scholar]
- 264.Osei K.A., Ovenseri-Ogbomo G., Kyei S., Ntodie M. The effect of caffeine on tear secretion. Optom Vis Sci. 2014;91:171–177. doi: 10.1097/OPX.0000000000000129. [DOI] [PubMed] [Google Scholar]
- 265.Arita R., Yanagi Y., Honda N., Maeda S., Maeda K., Kuchiba A., et al. Caffeine increases tear volume depending on polymorphisms within the adenosine A2a receptor gene and cytochrome P450 1A2. Ophthalmology. 2012;119:972–978. doi: 10.1016/j.ophtha.2011.11.033. [DOI] [PubMed] [Google Scholar]
- 266.Chacko S.M., Thambi P.T., Kuttan R., Nishigaki I. Beneficial effects of green tea: a literature review. Chin Med. 2010;5:13. doi: 10.1186/1749-8546-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Unno K., Noda S., Kawasaki Y., Yamada H., Morita A., Iguchi K., et al. Reduced stress and improved sleep quality caused by green tea are associated with a reduced caffeine content. Nutrients. 2017;9:777. doi: 10.3390/nu9070777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Masmali A.M., Alanazi S.A., Alotaibi A.G., Fagehi R., Abusharaha A., El-Hiti G.A. The acute effect of a single dose of green tea on the quality and quantity of tears in normal eye subjects. Clin Ophthalmol. 2019;13:605–610. doi: 10.2147/OPTH.S201127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Masmali A.M., Purslow C., Murphy P.J. The tear ferning test: a simple clinical technique to evaluate the ocular tear film. Clin Exp Optom. 2014;97:399–406. doi: 10.1111/cxo.12160. [DOI] [PubMed] [Google Scholar]
- 270.Wolffsohn J.S., Arita R., Chalmers R., Djalilian A., Dogru M., Dumbleton K., et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15:539–574. doi: 10.1016/j.jtos.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 271.Nejabat M., Reza S.A., Zadmehr M., Yasemi M., Sobhani Z. Efficacy of green tea extract for treatment of dry eye and meibomian gland dysfunction; A double-blind randomized controlled clinical trial study. J Clin Diagn Res. 2017;11:NC5–NC8. doi: 10.7860/JCDR/2017/23336.9426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Kolomeyer A.M., Yu Y., VanderBeek B.L. Association of opioids with incisional ocular surgery. JAMA Ophthalmology. 2019;137:1283–1291. doi: 10.1001/jamaophthalmol.2019.3694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Dieckmann G., Goyal S., Hamrah P. Neuropathic corneal pain: approaches for management. Ophthalmology. 2017;124:S34–S47. doi: 10.1016/j.ophtha.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Galor A., Levitt R.C., Felix E.R., Martin E.R., Sarantopoulos C.D. Neuropathic ocular pain: an important yet underevaluated feature of dry eye. Eye. 2015;29:301–312. doi: 10.1038/eye.2014.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Ung C., Yonekawa Y., Waljee J.F., Gunaseelan V., Lai Y.L., Woodward M.A. Persistent opioid use after ophthalmic surgery in opioid-naive patients and associated risk factors. Ophthalmology. 2021;128:1266–1273. doi: 10.1016/j.ophtha.2021.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Zöllner C., Mousa S., Klinger A., Förster M., Schäfer M. Topical fentanyl in a randomized, double-blind study in patients with corneal damage. Clin J Pain. 2008;24:690–696. doi: 10.1097/AJP.0b013e318175929e. [DOI] [PubMed] [Google Scholar]
- 277.Peyman G.A., Rahimy M.H., Fernandes M.L. Effects of morphine on corneal sensitivity and epithelial wound healing: implications for topical ophthalmic analgesia. Br J Ophthalmol. 1994;78:138–141. doi: 10.1136/bjo.78.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Degenhardt L., Black E., Breen C., Bruno R., Kinner S., Roxburgh A., et al. Trends in morphine prescriptions, illicit morphine use and associated harms among regular injecting drug users in Australia. Drug Alcohol Rev. 2006;25:403–412. doi: 10.1080/09595230600868504. [DOI] [PubMed] [Google Scholar]
- 279.Gaynes B.I., Barkin R.L. Analgesics in ophthalmic practice: a review of the oral non-narcotic agent tramadol. Optom Vis Sci. 1999;76:455–461. doi: 10.1097/00006324-199907000-00020. [DOI] [PubMed] [Google Scholar]
- 280.Lelescu C.A., Dumitras D.A., Iurian S., Staffieri F., Muresan C. Effects of topical application of tramadol with/without dexmedetomidine and proparacaine on corneal sensitivity in rats. Int Ophthalmol. 2021;41:465–473. doi: 10.1007/s10792-020-01596-x. [DOI] [PubMed] [Google Scholar]
- 281.Apan O., Ozer M., Takir S., Apan A., Sengul D. Effect of topical administration of tramadol on corneal wound healing in rats. Int Ophthalmol. 2016;36 doi: 10.1007/s10792-016-0184-9. [DOI] [PubMed] [Google Scholar]
- 282.Chen H.T., Chen K.H., Hsu W.M. Toxic keratopathy associated with abuse of low-dose anesthetic: a case report. Cornea. 2004;23:527–529. doi: 10.1097/01.ico.0000114127.63670.06. [DOI] [PubMed] [Google Scholar]
- 283.Giannaccare G., Ghelardini C., Mancini A., Scorcia V., Di Cesare Mannelli L. New perspectives in the pathophysiology and treatment of pain in patients with dry eye disease. J Clin Med. 2021:11. doi: 10.3390/jcm11010108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Ruiz T., Peres T., Campos W., Sorte E., Ribeiro A. Effects of tramadol on tear production, intraocular pressure, and pupil size in dogs: clinical study. Ciência Rural. 2015;45:724–729. [Google Scholar]
- 285.Santos P., Pontes K., Pinto R., Rios P., Silva G., Borges A., et al. Comparison of pupil diameter and tear production in dogs treated with acepromazine, tramadol and their combination. Rev Ceres. 2013;60:166–172. [Google Scholar]
- 286.Mouney M.C., Accola P.J., Cremer J., Shepard M.K., Rodriguez Guarin C., Hofmeister E.H. Effects of acepromazine maleate or morphine on tear production before, during, and after sevoflurane anesthesia in dogs. Am J Vet Res. 2011;72:1427–1430. doi: 10.2460/ajvr.72.11.1427. [DOI] [PubMed] [Google Scholar]
- 287.Raušer P., Němečková H., Mrázová M., Václavíková J., Novák L. Influence of fentanyl, ketamine, and lidocaine on tear production in healthy conscious dogs. Topics Comp An Med. 2022;46 doi: 10.1016/j.tcam.2021.100615. [DOI] [PubMed] [Google Scholar]
- 288.Peragallo J., Biousse V., Newman N.J. Ocular manifestations of drug and alcohol abuse. Curr Opin Ophthalmol. 2013;24:566–573. doi: 10.1097/ICU.0b013e3283654db2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Alipour F., Hashemi H., Piri N., Asghari H. Ocular manifestations of transconjunctival heroin abuse: a case report of an unusual route of substance abuse. Cornea. 2010;29:110–112. doi: 10.1097/ICO.0b013e3181a0a220. [DOI] [PubMed] [Google Scholar]
- 290.Marino D., Malandrini A., Rocchi R., Selvi E., Federico A. Transient "sicca syndrome" during phenobarbital treatment. J Neurosci. 2011;300:164. doi: 10.1016/j.jns.2010.09.028. [DOI] [PubMed] [Google Scholar]
- 291.Pontes K., Borges A., Eleotério R., Ferreira P., Duarte T. A comparison of the effects of propofol and thiopental on tear production in dogs. Rev Ceres. 2010;57:757–761. [Google Scholar]
- 292.Galor A., Feuer W., Lee D.J., Florez H., Carter D., Pouyeh B., et al. Prevalence and risk factors of dry eye syndrome in a United States veterans affairs population. Am J Ophthalmol. 2011;152 doi: 10.1016/j.ajo.2011.02.026. 377-84.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Wen W., Wu Y., Chen Y., Gong L., Li M., Chen X., et al. Dry eye disease in patients with depressive and anxiety disorders in Shanghai. Cornea. 2012;31:686–692. doi: 10.1097/ICO.0b013e3182261590. [DOI] [PubMed] [Google Scholar]
- 294.Di Pietro S., Macrì F., Bonarrigo T., Giudice E., Palumbo Piccionello A., Pugliese A. Effects of a medetomidine-ketamine combination on Schirmer tear test I results of clinically normal cats. Am J Vet Res. 2016;77:310–314. doi: 10.2460/ajvr.77.3.310. [DOI] [PubMed] [Google Scholar]
- 295.Elmeligy E., Abdel-hakiem M., Al-lethie A.-L. Effect of xylazine HCl and/or ketamine HCl on the tear production in clinically healthy dogs. Adv Vet Sci. 2019;7:1015–1020. [Google Scholar]
- 296.Volkow N.D., Baler R.D., Compton W.M., Weiss S.R. Adverse health effects of marijuana use. N Engl J Med. 2014;370:2219–2227. doi: 10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Hepler R.S., Frank I.M., Ungerleider J.T. Pupillary constriction after marijuana smoking. Am J Ophthalmol. 1972;74:1185–1190. doi: 10.1016/0002-9394(72)90741-6. [DOI] [PubMed] [Google Scholar]
- 298.Polat N., Cumurcu B., Cumurcu T., Tuncer İ. Corneal endothelial changes in long-term cannabinoid users. Cutan Ocul Toxicol. 2018;37:19–23. doi: 10.1080/15569527.2017.1322098. [DOI] [PubMed] [Google Scholar]
- 299.Thayer A., Murataeva N., Delcroix V., Wager-Miller J., Makarenkova H.P., Straiker A. THC regulates tearing via cannabinoid CB1 receptors. Invest Ophthalmol Vis Sci. 2020;61:48. doi: 10.1167/iovs.61.10.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Fraunfelder F.T., Sciubba J.J., Mathers W.D. The role of medications in causing dry eye. J Ophthalmol. 2012;2012 doi: 10.1155/2012/285851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Kowal M., Hazekamp A., Grotenhermen F. Review on clinical studies with cannabis and cannabinoids 2010-2014. Cannabinoids. 2016;11:1–18. [Google Scholar]
- 302.Mücke M., Phillips T., Radbruch L., Petzke F., Häuser W. Cannabis-based medicines for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2018;3:Cd012182. doi: 10.1002/14651858.CD012182.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Jay W.M., Green K. Multiple-drop study of topically applied 1% delta 9-tetrahydrocannabinol in human eyes. Arch Ophthalmol. 1983;101:591–593. doi: 10.1001/archopht.1983.01040010591012. [DOI] [PubMed] [Google Scholar]
- 304.Lo D., Cobbs L., Chua M., Young J., Haberman I.D., Modi Y. Eye dropping"-A case report of transconjunctival lysergic acid diethylamide drug abuse. Cornea. 2018;37:1324–1325. doi: 10.1097/ICO.0000000000001692. [DOI] [PubMed] [Google Scholar]
- 305.da Silva C.M., de Sousa R.A., Baptista A.M. Assessment of tear amount in subjects under the effect of (inhaled) cocaine. J Psychoact Drugs. 2013;45:195–198. doi: 10.1080/02791072.2013.785857. [DOI] [PubMed] [Google Scholar]
- 306.Mantelli F., Lambiase A., Sacchetti M., Orlandi V., Rosa A., Casella P., et al. Cocaine snorting may induce ocular surface damage through corneal sensitivity impairment. Graefes Arch Clin Exp Ophthalmol. 2015;253:765–772. doi: 10.1007/s00417-015-2938-x. [DOI] [PubMed] [Google Scholar]
- 307.Vasconcelos S.B., Guerra F.M., Morato G.M., Neves N.T., Tzelikis P.F. Acquired anterior staphyloma after corneal ulcer associated with the use of crack. Arq Bras Oftalmol. 2016;79:268–269. doi: 10.5935/0004-2749.20160076. [DOI] [PubMed] [Google Scholar]
- 308.Ravin J.G., Ravin L.C. Blindness due to illicit use of topical cocaine. Ann Ophthalmol. 1979;11:863–864. [PubMed] [Google Scholar]
- 309.Ghosheh F.R., Ehlers J.P., Ayres B.D., Hammersmith K.M., Rapuano C.J., Cohen E.J. Corneal ulcers associated with aerosolized crack cocaine use. Cornea. 2007;26:966–969. doi: 10.1097/ICO.0b013e3180cfe716. [DOI] [PubMed] [Google Scholar]
- 310.Colatrella N., Daniel T.E. Crack eye syndrome. J Am Optom Assoc. 1999;70:193–197. [PubMed] [Google Scholar]
- 311.Pilon A.F., Scheiffle J. Ulcerative keratitis associated with crack-cocaine abuse. Contact Lens Anterior Eye. 2006;29:263–267. doi: 10.1016/j.clae.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 312.Heer J.S., Heavey S., Quesada D., Aguìñiga-Navarrete P., Garrett M.B., Barkataki K. Keratolysis associated with methamphetamine use - incidental diagnosis of corneal melt in a patient with acute methamphetamine intoxication. Clin Prac Emer Med. 2020;4:472–473. doi: 10.5811/cpcem.2020.3.43981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Poulsen E.J., Mannis M.J., Chang S.D. Keratitis in methamphetamine abusers. Cornea. 1996;15:477–482. [PubMed] [Google Scholar]
- 314.Wijaya J., Salu P., Leblanc A., Bervoets S. Acute unilateral visual loss due to a single intranasal methamphetamine abuse. Bull Soc Belge Ophtalmol. 1999;271:19–25. [PubMed] [Google Scholar]
- 315.Al-Ghadeer H., Al-Amry M. Ocular complications resulting from the use of traditional herbal medicine in Central Saudi Arabia: a review. Middle East Afr J Ophthalmol. 2021;28:131–136. doi: 10.4103/meajo.meajo_120_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Diego J.L., Bidikov L., Pedler M.G., Kennedy J.B., Quiroz-Mercado H., Gregory D.G., et al. Effect of human milk as a treatment for dry eye syndrome in a mouse model. Mol Vis. 2016;22:1095–1102. [PMC free article] [PubMed] [Google Scholar]
- 317.Ukponmwan C., Okolo O., Kayoma D.H., Ese-Onakewhor J. Complications of breast milk application to the infected eye. Niger J Ophthalmol. 2009;17 [Google Scholar]
- 318.Prajna N.V., Pillai M.R., Manimegalai T.K., Srinivasan M. Use of Traditional Eye Medicines by corneal ulcer patients presenting to a hospital in South India. Indian J Ophthalmol. 1999;47:15–18. [PubMed] [Google Scholar]
- 319.Yorston D., Foster A. Traditional eye medicines and corneal ulceration in Tanzania. J Trop Med Hyg. 1994;97:211–214. [PubMed] [Google Scholar]
- 320.Lewallen S., Courtright P. Peripheral corneal ulcers associated with use of African traditional eye medicines. Br J Ophthalmol. 1995;79:343–346. doi: 10.1136/bjo.79.4.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Courtright P., Lewallen S., Kanjaloti S., Divala D.J. Traditional eye medicine use among patients with corneal disease in rural Malawi. Br J Ophthalmol. 1994;78:810–812. doi: 10.1136/bjo.78.11.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Asena L., Suveren E.H., Karabay G., Dursun Altinors D. Human breast milk drops promote corneal epithelial wound healing. Curr Eye Res. 2017;42:506–512. doi: 10.1080/02713683.2016.1223318. [DOI] [PubMed] [Google Scholar]
- 323.Sugimura T., Seo T., Terasaki N., Ozaki Y., Rikitake N., Okabe R., et al. Efficacy and safety of breast milk eye drops in infants with eye discharge. Acta Paedol. 2021;110:1322–1329. doi: 10.1111/apa.15628. [DOI] [PubMed] [Google Scholar]
- 324.Ahmed M., Saeed M., Mahmood M.A. Role of topical human milk in the treatment of neurotrophic corneal opacity. Pakistan J Ophthalmol. 2013;29:225–230. [Google Scholar]
- 325.Tarff A., Drew-Bear L.E., Di Meglio L., Yee R., Vizcaino M.A., Gupta P., et al. Effect of topical bovine colostrum in wound healing of corneal surface after acute ocular alkali burn in mice. Exp Eye Res. 2022;220 doi: 10.1016/j.exer.2022.109093. [DOI] [PubMed] [Google Scholar]
- 326.Sandford E.C., Muntz A., Craig J.P. Therapeutic potential of castor oil in managing blepharitis, meibomian gland dysfunction and dry eye. Clin Exp Optom. 2021;104:315–322. doi: 10.1111/cxo.13148. [DOI] [PubMed] [Google Scholar]
- 327.Al-Mamun M.A., Akter Z., Uddin M.J., Ferdaus K.M., Hoque K.M., Ferdousi Z., et al. Characterization and evaluation of antibacterial and antiproliferative activities of crude protein extracts isolated from the seed of Ricinus communis in Bangladesh. BMC Compl Alternative Med. 2016;16:211. doi: 10.1186/s12906-016-1185-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Goto E., Shimazaki J., Monden Y., Takano Y., Yagi Y., Shimmura S., et al. Low-concentration homogenized castor oil eye drops for noninflamed obstructive meibomian gland dysfunction. Ophthalmology. 2002;109:2030–2035. doi: 10.1016/s0161-6420(02)01262-9. [DOI] [PubMed] [Google Scholar]
- 329.Phong C., Lee V., Yale K., Sung C., Mesinkovska N. Coconut, Castor, and argan oil for hair in skin of color patients: a systematic review. J Drugs Dermatol JDD. 2022;21:751–757. doi: 10.36849/JDD.6972. [DOI] [PubMed] [Google Scholar]
- 330.Courtright P., Lewallen S., Kanjaloti S. Changing patterns of corneal disease and associated vision loss at a rural African hospital following a training programme for traditional healers. Br J Ophthalmol. 1996;80:694–697. doi: 10.1136/bjo.80.8.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Khanduja S., Jain P., Sachdeva S., Phogat J. Cow urine keratopathy: a case report. J Clin Diagn Res. 2017;11:Nd03–nd4. doi: 10.7860/JCDR/2017/24183.9708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Jain N., Gupta V., Garg R., Silawat N. Efficacy of cow urine therapy on various cancer patients in Mandsaur District, India - a survey. Int J Green Pharm. 2010;4 doi: 10.22377/ijgp.v4i1.115. [DOI] [Google Scholar]
- 333.Tabbara K.F. Kermes-induced cicatrization of the conjunctiva. Ann Saudi Med. 1986;6:233–236. [Google Scholar]
- 334.Al-Ghadeer H., Al-Amry M. Corneal thinning induced by self-administered alum substance: a case report and analysis of the active components. Middle East Afr J Ophthalmol. 2020;27:59–61. doi: 10.4103/meajo.MEAJO_215_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Uzodike E., Igwe I.O. Efficacy of garlic (allium sativum) on Staphylococcus aureus conjunctivites. J Nigerian Optometric Ass. 2005;12:20–22. [Google Scholar]
- 336.Craig J.P., Cruzat A., Cheung I.M.Y., Watters G.A., Wang M.T.M. Randomized masked trial of the clinical efficacy of MGO Manuka Honey microemulsion eye cream for the treatment of blepharitis. Ocul Surf. 2020;18:170–177. doi: 10.1016/j.jtos.2019.11.009. [DOI] [PubMed] [Google Scholar]
- 337.Bansal V., Medhi B., Pandhi P. Honey--a remedy rediscovered and its therapeutic utility. Kathmandu Univ Med J. 2005;3:305–309. [PubMed] [Google Scholar]
- 338.Albietz J.M., Schmid K.L. Randomised controlled trial of topical antibacterial Manuka (Leptospermum species) honey for evaporative dry eye due to meibomian gland dysfunction. Clin Exp Optom. 2017;100:603–615. doi: 10.1111/cxo.12524. [DOI] [PubMed] [Google Scholar]
- 339.Tan J., Jia T., Liao R., Stapleton F. Effect of a formulated eye drop with Leptospermum spp. honey on tear film properties. Br J Ophthalmol. 2020;104:1373–1377. doi: 10.1136/bjophthalmol-2019-315160. [DOI] [PubMed] [Google Scholar]
- 340.Salehi A., Jabarzare S., Neurmohamadi M., Kheiri S., Rafieian-Kopaei M. A double blind clinical trial on the efficacy of honey drop in vernal keratoconjunctivitis. Evid base Compl Alternative Med. 2014;2014 doi: 10.1155/2014/287540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Peyman A., Pourazizi M., Peyman M., Kianersi F. Natural honey-induced Acanthamoeba keratitis. Middle East Afr J Ophthalmol. 2019;26:243–245. doi: 10.4103/meajo.MEAJO_56_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Coates P.M., Betz J.M., Blackman M.R., Cragg G.M., Levine M., Moss J., White J.D. second ed. CRC Press; 2015. Encyclopedia of dietary supplements. [Google Scholar]
- 343.Carvalho R.S., Kara-José N., Temporini E.R., Kara-Junior N., Noma-Campos R. Self-medication: initial treatments used by patients seen in an ophthalmologic emergency room. Clinics. 2009;64:735–741. doi: 10.1590/S1807-59322009000800005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Al Ghadeer H., Al Gethami A., Al Sulaiman H., Bukhari T. Corneal toxicity after self-application of calotropis procera (ushaar) latex: case report and analysis of the active components. Middle East Afr J Ophthalmol. 2019;26:40–42. doi: 10.4103/meajo.MEAJO_180_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Yang M., Hu Z., Yue R., Yang L., Zhang B., Chen Y. The efficacy and safety of qiming granule in dry eye disease: protocol for systematic review and meta-analysis. Medicine. 2019;98 doi: 10.1097/MD.0000000000017121. e17121-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Banerjee K., Mathie R.T., Costelloe C.E., Howick J. Homeopathy for allergic rhinitis: a systematic review. J Alternative Compl Med. 2017;23 6:426–444. doi: 10.1089/acm.2016.0310. [DOI] [PubMed] [Google Scholar]
- 347.Miller K.N., Collins C.L., Chounthirath T., Smith G.A. Pediatric sports- and recreation-related eye injuries treated in US emergency departments. Pediatrics. 2018;141 doi: 10.1542/peds.2017-3083. [DOI] [PubMed] [Google Scholar]
- 348.Hoskin A.K., Yardley A.M., Hanman K., Lam G., Mackey D.A. Sports-related eye and adnexal injuries in the Western Australian paediatric population. Acta Ophthalmol. 2016;94:e407–e410. doi: 10.1111/aos.12911. [DOI] [PubMed] [Google Scholar]
- 349.Patel P.A., Gopali R., Reddy A., Patel K.K. Trends in soccer-related ocular injuries within the United States from 2010 through 2019. Semin Ophthalmol. 2021:1–6. doi: 10.1080/08820538.2021.1909077. [DOI] [PubMed] [Google Scholar]
- 350.Murtaugh K. Field hockey injuries. Curr Sports Med Rep. 2009;8:267–272. doi: 10.1249/JSR.0b013e3181b7f1f4. [DOI] [PubMed] [Google Scholar]
- 351.Kriz P.K., Zurakowski D., Almquist J.L., Reynolds J., Ruggieri D., Collins C.L., et al. Eye protection and risk of eye injuries in high school field hockey. Pediatrics. 2015;136:521–527. doi: 10.1542/peds.2015-0216. [DOI] [PubMed] [Google Scholar]
- 352.Haavisto A.K., Sahraravand A., Puska P., Leivo T. Toy gun eye injuries - eye protection needed Helsinki ocular trauma study. Acta Ophthalmol. 2019;97:430–434. doi: 10.1111/aos.13948. [DOI] [PubMed] [Google Scholar]
- 353.Cox C.M.J., Stewart S.A., Hurley K.F. Firearm-related injuries among Canadian children and youth from 2006 to 2013: a CHIRPP study. CJEM. 2019;21:190–194. doi: 10.1017/cem.2018.38. [DOI] [PubMed] [Google Scholar]
- 354.Aziz M., Patel S. BB gun-related open globe injuries. Ophthalmol Retina. 2018;2:1056–1061. doi: 10.1016/j.oret.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 355.Hoskin A.K., Yardley A.-M.E., Mackey D.A. Recreational fishing eye injuries and eye protection. Acta Ophthalmol. 2015;93 doi: 10.1111/aos.12732. e678-e. [DOI] [PubMed] [Google Scholar]
- 356.Alfaro D.V., 3rd, Jablon E.P., Rodriguez Fontal M., Villalba S.J., Morris R.E., Grossman M., et al. Fishing-related ocular trauma. Am J Ophthalmol. 2005;139:488–492. doi: 10.1016/j.ajo.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 357.Hoskin A.K., Low R., de Faber J.T., Mishra C., Susvar P., Pradhan E., et al. Eye injuries from fireworks used during celebrations and associated vision loss: the international globe and adnexal trauma epidemiology study (IGATES) Graefes Arch Clin Exp Ophthalmol. 2022;260:371–383. doi: 10.1007/s00417-021-05284-z. [DOI] [PubMed] [Google Scholar]
- 358.Shiuey E.J., Kolomeyer A.M., Kolomeyer N.N. Assessment of firework-related ocular injury in the US. JAMA Ophthalmology. 2020;138:618–623. doi: 10.1001/jamaophthalmol.2020.0832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Wang F., Lou B., Jiang Z., Yang Y., Ma X., Lin X. Changing trends in firework-related eye injuries in southern China: a 5-year retrospective study of 468 cases. J Ophthalmol. 2020;2020 doi: 10.1155/2020/6194519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.John D., Philip S.S., Mittal R., John S.S., Paul P. Spectrum of ocular firework injuries in children: a 5-year retrospective study during a festive season in Southern India. Indian J Ophthalmol. 2015;63:843–846. doi: 10.4103/0301-4738.171966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Unterlauft J.D., Rehak M., Wiedemann P., Meier P. Firework-related eye trauma in Germany. Curr Eye Res. 2018;43:1522–1528. doi: 10.1080/02713683.2018.1508725. [DOI] [PubMed] [Google Scholar]
- 362.Lenglinger M.A., Zorn M., Pilger D., von Sonnleithner C., Rossel M., Salchow D.J., et al. Firework-inflicted ocular trauma in children and adults in an urban German setting. Eur J Ophthalmol. 2021;31:709–715. doi: 10.1177/1120672120902033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Malla T., Sahu S. Firework-related ocular injuries during festival season: a hospitalbased study in a tertiary eye care center of Nepal. Nepal J Ophthalmol. 2021;13:31–39. doi: 10.3126/nepjoph.v13i1.31246. [DOI] [PubMed] [Google Scholar]
- 364.de Faber J.T., Kivelä T.T., Gabel-Pfisterer A. National studies from The Netherlands and Finland and the impact of regulations on incidences of fireworks-related eye injuries. Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2020;117:36–42. doi: 10.1007/s00347-019-00996-4. [DOI] [PubMed] [Google Scholar]
- 365.Willmann G. Ultraviolet keratitis: from the pathophysiological basis to prevention and clinical management. High Alt Med Biol. 2015;16:277–282. doi: 10.1089/ham.2015.0109. [DOI] [PubMed] [Google Scholar]
- 366.Gilaberte Y., Trullàs C., Granger C., de Troya-Martín M. Photoprotection in outdoor sports: a review of the literature and recommendations to reduce risk among athletes. Dermatol Ther. 2022;12:329–343. doi: 10.1007/s13555-021-00671-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Grupcheva C.N., Radeva M.N., Grupchev D.I., Nikolova S.P. Damage of the ocular surface from indoor suntanning-Insights from in vivo confocal microscopy. Contact Lens Anterior Eye. 2021;44 doi: 10.1016/j.clae.2021.03.005. [DOI] [PubMed] [Google Scholar]
- 368.Clarke A., Rumsey N., Collin J.R., Wyn-Williams M. Psychosocial distress associated with disfiguring eye conditions. Eye. 2003;17:35–40. doi: 10.1038/sj.eye.6700234. [DOI] [PubMed] [Google Scholar]
- 369.James H., Jenkinson E., Harrad R., Ezra D.G., Newman S., Members of Appearance Research C. Appearance concerns in ophthalmic patients. Eye. 2011;25:1039–1044. doi: 10.1038/eye.2011.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Ozates S., Ezerbolat Ozates M., Can C.U., Polat S., Yasar H.H., Taskale B., et al. Improvement in psychiatric symptoms after strabismus surgery in adolescent patients in long-term follow-up. Br J Ophthalmol. 2019;103:966–970. doi: 10.1136/bjophthalmol-2018-312510. [DOI] [PubMed] [Google Scholar]
- 371.Pine N.S., Pine K.R. Depression, anxiety and stress indicators for prosthetic eye wearers. Clin Ophthalmol. 2020;14:1715–1723. doi: 10.2147/OPTH.S254910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Papadopulos N.A., Hodbod M., Henrich G., Kovacs L., Papadopoulos O., Herschbach P., et al. The effect of blepharoplasty on our patient's quality of life, emotional stability, and self-esteem. J Craniofac Surg. 2019;30:377–383. doi: 10.1097/SCS.0000000000005057. [DOI] [PubMed] [Google Scholar]
- 373.Kim H.H., De Paiva C.S., Yen M.T. Effects of upper eyelid blepharoplasty on ocular surface sensation and tear production. Can J Ophthalmol. 2007;42:739–742. doi: 10.3129/i07-141. [DOI] [PubMed] [Google Scholar]
- 374.Yan Y., Zhou Y., Zhang S., Cui C., Song X., Zhu X., et al. Impact of full-incision double-eyelid blepharoplasty on tear film dynamics and dry eye symptoms in young asian females. Aesthetic Plast Surg. 2020;44:2109–2116. doi: 10.1007/s00266-020-01874-0. [DOI] [PubMed] [Google Scholar]
- 375.Shao C., Fu Y., Lu L., Chen J., Shen Q., Zhu H., et al. Dynamic changes of tear fluid after cosmetic transcutaneous lower blepharoplasty measured by optical coherence tomography. Am J Ophthalmol. 2014;158:55–63. doi: 10.1016/j.ajo.2014.03.016. e1. [DOI] [PubMed] [Google Scholar]
- 376.Yong P.T., Arif N., Sharanjeet-Kaur S., Hairol M.I. Double eyelid tape wear affects anterior ocular health among young adult women with single eyelids. Int J Environ Res Publ Health. 2020;17 doi: 10.3390/ijerph17217701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Jones L., Efron N., Bandamwar K., Barnett M., Jacobs D.S., Jalbert I., et al. TFOS Lifestyle: impact of contact lenses on the ocular surface. Ocul Surf. 2023 doi: 10.1016/j.jtos.2023.04.010. [DOI] [PubMed] [Google Scholar]
- 378.Nichols J.J., Sinnott L.T. Tear film, contact lens, and patient-related factors associated with contact lens-related dry eye. Invest Ophthalmol Vis Sci. 2006;47:1319–1328. doi: 10.1167/iovs.05-1392. [DOI] [PubMed] [Google Scholar]
- 379.Cumberland P.M., Chianca A., Rahi J.S., Eyes U.K.B., Vision C. Laser refractive surgery in the UK Biobank study: frequency, distribution by sociodemographic factors, and general health, happiness, and social participation outcomes. J Cataract Refract Surg. 2015;41:2466–2475. doi: 10.1016/j.jcrs.2015.05.040. [DOI] [PubMed] [Google Scholar]
- 380.Gomes J.A.P., Azar D.T., Baudouin C., Efron N., Hirayama M., Horwath-Winter J., et al. TFOS DEWS II iatrogenic report. Ocul Surf. 2017;15:511–538. doi: 10.1016/j.jtos.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 381.Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatr. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Lee Y.B., Kim J.J., Hyon J.Y., Wee W.R., Shin Y.J. Eyelid tattooing induces meibomian gland loss and tear film instability. Cornea. 2015;34:750–755. doi: 10.1097/ICO.0000000000000452. [DOI] [PubMed] [Google Scholar]
- 383.Hurwitz J.J., Brownstein S., Mishkin S.K. Histopathological findings in blepharopigmentation (eyelid tattoo) Can J Ophthalmol. 1988;23:267–269. [PubMed] [Google Scholar]
- 384.Turan H., Okur M., Kaya E., Gun E., Aliagaoglu C. Allergic contact dermatitis to para-phenylenediamine in a tattoo: a case report. Cutan Ocul Toxicol. 2013;32:185–187. doi: 10.3109/15569527.2012.709570. [DOI] [PubMed] [Google Scholar]
- 385.Kind F., Hofmeier K.S., Bircher A.J. Irritant contact dermatitis from a black henna tattoo without sensitization to para-phenylendiamine. Pediatrics. 2013;131:e1974–e1976. doi: 10.1542/peds.2012-2938. [DOI] [PubMed] [Google Scholar]
- 386.Catalano R., Goldman-Mellor S., Saxton K., Margerison-Zilko C., Subbaraman M., LeWinn K., et al. The health effects of economic decline. Annu Rev Publ Health. 2011;32:431–450. doi: 10.1146/annurev-publhealth-031210-101146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Donthineni P.R., Kammari P., Shanbhag S.S., Singh V., Das A.V., Basu S. Incidence, demographics, types and risk factors of dry eye disease in India: electronic medical records driven big data analytics report I. Ocul Surf. 2019;17:250–256. doi: 10.1016/j.jtos.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 388.Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15:288–298. doi: 10.1038/s41574-019-0176-8. [DOI] [PubMed] [Google Scholar]
- 389.Everding J., Marcus J. The effect of unemployment on the smoking behavior of couples. Health Econ. 2020;29:154–170. doi: 10.1002/hec.3961. [DOI] [PubMed] [Google Scholar]
- 390.Walia N., Bhetuwal R., Acosta L., Muddasani S., Kamwal C., Mishra V.D., et al. Employment status and its association with psychological distress and alcohol consumption. Cureus. 2021;13 doi: 10.7759/cureus.16054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Zuelke A.E., Luck T., Schroeter M.L., Witte A.V., Hinz A., Engel C., et al. The association between unemployment and depression-Results from the population-based LIFE-adult-study. J Affect Disord. 2018;235:399–406. doi: 10.1016/j.jad.2018.04.073. [DOI] [PubMed] [Google Scholar]
- 392.Brenner M.H. Unemployment, bankruptcies, and deaths from multiple causes in the COVID-19 recession compared with the 2000‒2018 great recession impact. Am J Publ Health. 2021;111:1950–1959. doi: 10.2105/AJPH.2021.306490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Bazeer S., Jansonius N., Snieder H., Hammond C., Vehof J. The relationship between occupation and dry eye. Ocul Surf. 2019;17:484–490. doi: 10.1016/j.jtos.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 394.Ahmmed A.A., Ting D.S.J., Figueiredo F.C. Epidemiology, economic and humanistic burdens of Ocular Surface Chemical Injury: a narrative review. Ocul Surf. 2021;20:199–211. doi: 10.1016/j.jtos.2021.02.006. [DOI] [PubMed] [Google Scholar]
- 395.Hossain R.R., Papamichael E., Coombes A. East London deliberate corrosive fluid injuries. Eye. 2020;34:733–739. doi: 10.1038/s41433-019-0593-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Anchouche S., Hall N., Bal S., Dana R., Elze T., Miller J.W., et al. Chemical and thermal ocular burns in the United States: an IRIS registry analysis. Ocul Surf. 2021;21:345–347. doi: 10.1016/j.jtos.2021.03.008. [DOI] [PubMed] [Google Scholar]
- 397.Jovanovic N., Peek-Asa C., Swanton A., Young T., Alajbegovic-Halimic J., Cavaljuga S., et al. Prevalence and risk factors associated with work-related eye injuries in Bosnia and Herzegovina. Int J Occup Environ Health. 2016;22:325–332. doi: 10.1080/10773525.2016.1243081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Nowrouzi-Kia B., Nadesar N., Sun Y., Gohar B., Casole J., Nowrouzi-Kia B. Types of ocular injury and their antecedent factors: a systematic review and meta-analysis. Am J Ind Med. 2020;63:589–599. doi: 10.1002/ajim.23117. [DOI] [PubMed] [Google Scholar]
- 399.Toh Z.H., Shah S.M., Chua C.H., Hoskin A.K., Agrawal R., Shah M. International globe and adnexal trauma epidemiology study (IGATES): visual outcomes in open globe injuries in rural west India. Eye. 2022;37:88–96. doi: 10.1038/s41433-021-01895-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Echieh C.I., Etim B.A., Echieh C.P., Oyeniyi T., Ajewole J. A comparative assessment of dry eye disease among outdoor street sweepers and indoor office cleaners. BMC Ophthalmol. 2021;21:265. doi: 10.1186/s12886-021-02025-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.Kim Y., Choi Y.H., Kim M.K., Paik H.J., Kim D.H. Different adverse effects of air pollutants on dry eye disease: ozone, PM(2.5), and PM(10) Environ Pollut. 2020;265 doi: 10.1016/j.envpol.2020.115039. [DOI] [PubMed] [Google Scholar]
- 402.Wright C.Y., Norval M. Health risks associated with excessive exposure to solar ultraviolet radiation among outdoor workers in South Africa: an overview. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.678680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Roncone D.P. Environmental droplet keratopathy: a novel approach to nomenclature, classification, treatment and management. Clin Exp Optom. 2022;105:664–666. doi: 10.1080/08164622.2022.2058869. [DOI] [PubMed] [Google Scholar]
- 404.Huang A., Janecki J., Galor A., Rock S., Menendez D., Hackam A.S., et al. Association of the indoor environment with dry eye metrics. JAMA Ophthalmology. 2020;138:867–874. doi: 10.1001/jamaophthalmol.2020.2237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Fjaervoll H., Fjaervoll K., Magno M., Moschowits E., Vehof J., Dartt D.A., et al. The association between visual display terminal use and dry eye: a review. Acta Ophthalmol. 2021;100:357–375. doi: 10.1111/aos.15049. [DOI] [PubMed] [Google Scholar]
- 406.Bernardino C.R., Rapuano C. Ophthalmia nodosa caused by casual handling of a tarantula. CLAO J. 2000;26:111–112. [PubMed] [Google Scholar]
- 407.Hu Y., Xu Y. The optical imaging of tarantula hair corneal injury: one case report and review of the literature. Photodiagnosis Photodyn Ther. 2017;19:352–354. doi: 10.1016/j.pdpdt.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 408.Jalink M.B., Wisse R.P.L. On the dangers of tropical spiders as a pet: a review of ocular symptoms caused by tarantula hairs. Am J Trop Med Hyg. 2021;105:1795–1797. doi: 10.4269/ajtmh.21-0337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Okullo A.T., Low T., Baker L.L. Ocular injury secondary to sheep bile exposure. BMJ Case Rep. 2012;2012 doi: 10.1136/bcr-2012-007439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Vayalambrone D., Butler T. Chemical-biological ocular injury from Turkey bile. Cutan Ocul Toxicol. 2011;30:241–242. doi: 10.3109/15569527.2011.554479. [DOI] [PubMed] [Google Scholar]
- 411.Christoffersen T., Olsen E.G. Injury to the cornea due to fish bile. Scand J Work Environ Health. 1993;19:358–359. doi: 10.5271/sjweh.1462. [DOI] [PubMed] [Google Scholar]
- 412.Bhalerao S.A., Singh P., Rani P.K., Rathi V. The sting of a honey bee: an unusual subconjunctival foreign body. Indian J Ophthalmol. 2017;65:1226–1228. doi: 10.4103/ijo.IJO_533_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Semler-Collery A., Hayek G., Ramadier S., Perone J.M. A case of conjunctival bee sting injury with review of the literature on ocular bee stings. Am J Case Rep. 2019;20:1284–1289. doi: 10.12659/AJCR.917592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Chilibeck C., Wang N., Murphy C. Making a bee-line for the eye: a limbal sting and retained honey bee. Clin Exp Optom. 2021;104:538–540. doi: 10.1080/08164622.2021.1878837. [DOI] [PubMed] [Google Scholar]
- 415.Makateb A., Torabifard H. Dry eye signs and symptoms in night-time workers. J Curr Ophthalmol. 2017;29:270–273. doi: 10.1016/j.joco.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Zhang J., Wu Z., Sun L., Liu X.H. Function and morphology of the meibomian glands using a LipiView interferometer in rotating shift medical staff. J Ophthalmol. 2020;2020 doi: 10.1155/2020/3275143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417.Stocks M.E., Ogden S., Haddad D., Addiss D.G., McGuire C., Freeman M.C. Effect of water, sanitation, and hygiene on the prevention of trachoma: a systematic review and meta-analysis. PLoS Med. 2014;11 doi: 10.1371/journal.pmed.1001605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Abebe T.A., Tucho G.T. The impact of access to water supply and sanitation on the prevalence of active trachoma in Ethiopia: a systematic review and meta-analysis. PLoS Neglected Trop Dis. 2021;15 doi: 10.1371/journal.pntd.0009644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Ahmad S.S. Water related ocular diseases. Saudi J Ophthalmol. 2018;32:227–233. doi: 10.1016/j.sjopt.2017.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Zajacova A., Lawrence E.M. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Publ Health. 2018;39:273–289. doi: 10.1146/annurev-publhealth-031816-044628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.Solomon S.D., Shoge R.Y., Ervin A.M., Contreras M., Harewood J., Aguwa U.T., et al. Improving access to eye care: a systematic review of the literature. Ophthalmology. 2022;129:e114–e126. doi: 10.1016/j.ophtha.2022.07.012. [DOI] [PubMed] [Google Scholar]
- 422.Mitsukura Y., Negishi K., Ayaki M., Santo M., Kawashima M., Tsubota K. Loss of concentration may occur by blink inhibition in DED simulation models. Life. 2020;10:61. doi: 10.3390/life10050061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Al-Mohtaseb Z., Schachter S., Shen Lee B., Garlich J., Trattler W. The relationship between dry eye disease and digital screen use. Clin Ophthalmol. 2021;15:3811–3820. doi: 10.2147/OPTH.S321591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424.Saldanha I., Petris R., Makara M., Channa P., Akpek E. Impact of the COVID-19 pandemic on eye strain and dry eye symptoms. Ocul Surf. 2021;22:38–46. doi: 10.1016/j.jtos.2021.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Elhusseiny A.M., Eleiwa T.K., Yacoub M.S., George J., ElSheikh R.H., Haseeb A., et al. Relationship between screen time and dry eye symptoms in pediatric population during the COVID-19 pandemic. Ocul Surf. 2021;22 doi: 10.1016/j.jtos.2021.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Oh J.H., Yoo H., Park H.K., Do Y.R. Analysis of circadian properties and healthy levels of blue light from smartphones at night. Sci Rep. 2015;5 doi: 10.1038/srep11325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Duarte I.A., Hafner Mde F., Malvestiti A.A. Ultraviolet radiation emitted by lamps, TVs, tablets and computers: are there risks for the population? An Bras Dermatol. 2015;90:595–597. doi: 10.1590/abd1806-4841.20153616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Zhao Z.C., Zhou Y., Tan G., Li J. Research progress about the effect and prevention of blue light on eyes. Int J Ophthalmol. 2018;11:1999–2003. doi: 10.18240/ijo.2018.12.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 429.Sayal A.P., Slomovic J., Bhambra N.S., Popovic M.M., Lichter M. Visual impairment and the prevalence of ocular pathology in homeless children and adults globally: a systematic review. Can J Ophthalmol. 2021:56. doi: 10.1016/j.jcjo.2020.09.023. [DOI] [PubMed] [Google Scholar]
- 430.Lietman T.M., Pinsent A., Liu F., Deiner M., Hollingsworth T.D., Porco T.C. Models of trachoma transmission and their policy implications: from control to elimination. Clin Infect Dis. 2018;66 doi: 10.1093/cid/ciy004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Atik A., Barton K., Azuara-Blanco A., Kerr N.M. Health economic evaluation in ophthalmology. Br J Ophthalmol. 2021;105 doi: 10.1136/bjophthalmol-2020-316880. [DOI] [PubMed] [Google Scholar]
- 432.Sommer A.C., Blumenthal E.Z. Telemedicine in ophthalmology in view of the emerging COVID-19 outbreak. Graefes Arch Clin Exp Ophthalmol. 2020;258:2341–2352. doi: 10.1007/s00417-020-04879-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.Kumar S.D., Kumar S.A., Pattankar J.V., Reddy S.B., Dhar M. Health status of the prisoners in a central jail of south India. Indian J Psychol Med. 2013;35:373–377. doi: 10.4103/0253-7176.122230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Zalwango C., Ayebare P., Mwanja P., Denis E., Kasadhakawo M., Mugerwa M., et al. Prevalence and factors associated with ocular morbidity among prisoners of Luzira prison (Uganda) BMC Ophthalmol. 2021;21:278. doi: 10.1186/s12886-021-02035-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.Mathenge W., Kuper H., Myatt M., Foster A., Gilbert C. Vitamin A deficiency in a Kenyan prison. Trop Med Int Health. 2007;12:269–273. doi: 10.1111/j.1365-3156.2006.01780.x. [DOI] [PubMed] [Google Scholar]
- 436.Osae E.A., Ablordeppey R.K., Horstmann J., Kumah D.B., Steven P. Clinical dry eye and meibomian gland features among dry eye patients in rural and urban Ghana. Clin Ophthalmol. 2020;14:4055–4063. doi: 10.2147/OPTH.S275584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437.Sengupta D., Banerji S. Prevalence of dry eye diseases in a rural and urban population in West Bengal and the role of air pollution. J Env Sci Tox Food Tech. 2014;8:45–50. [Google Scholar]
- 438.Novignon J., Nonvignon J., Mussa R., Chiwaula L.S. Health and vulnerability to poverty in Ghana: evidence from the Ghana living standards survey round 5. Health Econ Rev. 2012;2:11. doi: 10.1186/2191-1991-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Pengpid S., Peltzer K. Hygiene behaviour and health attitudes in African countries. Curr Psychol. 2012;25:149–154. doi: 10.1097/YCO.0b013e32834fda33. [DOI] [PubMed] [Google Scholar]
- 440.Gupta N., Prasad I., Himashree G., D'Souza P. Prevalence of dry eye at high altitude: a case controlled comparative study. High Alt Med Biol. 2008;9:327–334. doi: 10.1089/ham.2007.1055. [DOI] [PubMed] [Google Scholar]
- 441.Kumar N., Feuer W., Lanza N.L., Galor A. Seasonal variation in dry eye. Ophthalmology. 2015;122:1727–1729. doi: 10.1016/j.ophtha.2015.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.McGill J.I., Holgate S.T., Church M.K., Anderson D.F., Bacon A. Allergic eye disease mechanisms. Br J Ophthalmol. 1998;82:1203–1214. doi: 10.1136/bjo.82.10.1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443.Bonini S., Bonini S., Lambiase A., Marchi S., Pasqualetti P., Zuccaro O., et al. Vernal keratoconjunctivitis revisited: a case series of 195 patients with long-term followup. Ophthalmology. 2000;107:1157–1163. doi: 10.1016/s0161-6420(00)00092-0. [DOI] [PubMed] [Google Scholar]
- 444.Bonini S., Coassin M., Aronni S., Lambiase A. Vernal keratoconjunctivitis. Eye. 2004;18:345–351. doi: 10.1038/sj.eye.6700675. [DOI] [PubMed] [Google Scholar]
- 445.Malu K.N. Allergic conjunctivitis in jos-Nigeria. Niger Med J. 2014;55:166–170. doi: 10.4103/0300-1652.129664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 446.Barnes C., Tuck J., Simon S., Pacheco F., Hu F., Portnoy J. Allergenic materials in the house dust of allergy clinic patients. Ann All Asth Immunol. 2001;86:517–523. doi: 10.1016/S1081-1206(10)62899-2. [DOI] [PubMed] [Google Scholar]
- 447.Estopinal C.B., Ewald M.D. Geographic disparities in the etiology of bacterial and fungal keratitis in the United States of America. Semin Ophthalmol. 2016;31:345–352. doi: 10.3109/08820538.2016.1154173. [DOI] [PubMed] [Google Scholar]
- 448.Gorski M., Genis A., Yushvayev S., Awwad A., Lazzaro D.R. Seasonal variation in the presentation of infectious keratitis. Eye Contact Lens. 2016;42:295–297. doi: 10.1097/ICL.0000000000000213. [DOI] [PubMed] [Google Scholar]
- 449.Khalaila S., Coreanu T., Vodonos A., Kloog I., Shtein A., Colwell L.E., et al. Association between ambient temperature, particulate air pollution and emergency room visits for conjunctivitis. BMC Ophthalmol. 2021;21:100. doi: 10.1186/s12886-021-01854-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450.Lee J., Bilonick R.A., Romanowski E.G., Kowalski R.P. Seasonal variation in human adenovirus conjunctivitis: a 30-year observational study. Ophthalmic Epidemiol. 2018;25:451–456. doi: 10.1080/09286586.2018.1509096. [DOI] [PubMed] [Google Scholar]
- 451.Walkden A., Fullwood C., Tan S.Z., Au L., Armstrong M., Brahma A.K., et al. Association between season, temperature and causative organism in microbial keratitis in the UK. Cornea. 2018;37:1555–1560. doi: 10.1097/ICO.0000000000001748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 452.Green M., Apel A., Stapleton F. A longitudinal study of trends in keratitis in Australia. Cornea. 2008;27:33–39. doi: 10.1097/ICO.0b013e318156cb1f. [DOI] [PubMed] [Google Scholar]
- 453.Khoo P., Cabrera-Aguas M., Nguyen V., Lahra M., Watson S. Microbial keratitis in Sydney, Australia: risk factors, patient outcomes, and seasonal variation. Graefes Arch Clin Exp Ophthalmol. 2020;258:1–11. doi: 10.1007/s00417-020-04681-0. [DOI] [PubMed] [Google Scholar]
- 454.McAllum P., Bahar I., Kaiserman I., Srinivasan S., Slomovic A., Rootman D. Temporal and seasonal trends in Acanthamoeba keratitis. Cornea. 2009;28:7–10. doi: 10.1097/ICO.0b013e318181a863. [DOI] [PubMed] [Google Scholar]
- 455.Bharathi M.J., Ramakrishnan R., Meenakshi R., Padmavathy S., Shivakumar C., Srinivasan M. Microbial keratitis in South India: influence of risk factors, climate, and geographical variation. Ophthalmic Epidemiol. 2007;14:61–69. doi: 10.1080/09286580601001347. [DOI] [PubMed] [Google Scholar]
- 456.Lin C.C., Lalitha P., Srinivasan M., Prajna N.V., McLeod S.D., Acharya N.R., et al. Seasonal trends of microbial keratitis in South India. Cornea. 2012;31:1123–1127. doi: 10.1097/ICO.0b013e31825694d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457.Stapleton F., Keay L.J., Sanfilippo P.G., Katiyar S., Edwards K.P., Naduvilath T. Relationship between climate, disease severity, and causative organism for contact lens-associated microbial keratitis in Australia. Am J Ophthalmol. 2007;144:690–698. doi: 10.1016/j.ajo.2007.06.037. [DOI] [PubMed] [Google Scholar]
- 458.Fennell K., Hull M., Jones M., Dollman J. A comparison of barriers to accessing services for mental and physical health conditions in a sample of rural Australian adults. Rural Rem Health. 2018;18:4155. doi: 10.22605/RRH4155. [DOI] [PubMed] [Google Scholar]
- 459.Adio A.O., Alikor A., Awoyesuku E. Survey of pediatric ophthalmic diagnoses in a teaching hospital in Nigeria. Niger J Med. 2011;20:105–108. [PubMed] [Google Scholar]
- 460.Eballe A.O., Bella L.A., Owono D., Mbome S., Mvogo C.E. [Eye disease in children aged 6 to 15 years: a hospital-based study in Yaounde] Sante (Montrouge, France) 2009;19:61–66. doi: 10.1684/san.2009.0158. [DOI] [PubMed] [Google Scholar]
- 461.Hassan M., Olowookere S., Adeleke N., Akinleye C., Adepoju E. Patterns of presentations at a free eye clinic in an urban state hospital. Niger J Clin Pract. 2013;16:145–148. doi: 10.4103/1119-3077.110124. [DOI] [PubMed] [Google Scholar]
- 462.Mehari Z.A. Pattern of childhood ocular morbidity in rural eye hospital, Central Ethiopia. BMC Ophthalmol. 2014;14:50. doi: 10.1186/1471-2415-14-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 463.World Health Organisation. World Report on Vision . 2019. World report on vision (who.int) [Google Scholar]
- 464.Gilson L., Doherty J., Lowenson R., Francis V. Knowledge Network on Health Systems; 2007. Challenging inequity through health systems. Final report. [Google Scholar]
- 465.Misra V., Vashist P., Malhotra S., Gupta S.K. Models for primary eye care services in India. Indian J Community Med. 2015;40:79–84. doi: 10.4103/0970-0218.153868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 466.Khanna R.C., Marmamula S., Rao G.N. International vision care: issues and approaches. Ann Rev Vision Sci. 2017;3:53–68. doi: 10.1146/annurev-vision-102016-061407. [DOI] [PubMed] [Google Scholar]
- 467.Khanna R.C., Sabherwal S., Sil A., Gowth M., Dole K., Kuyyadiyil S., et al. Primary eye care in India - the vision center model. Indian J Ophthalmol. 2020;68:333–339. doi: 10.4103/ijo.IJO_118_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 468.Malhotra R., Uppal Y., Misra A., Taneja D.K., Gupta V.K., Ingle G.K. Increasing access to cataract surgery in a rural area--a support strategy. Indian J Publ Health. 2005;49:63–67. [PubMed] [Google Scholar]
- 469.Nirmalan P.K., Katz J., Robin A.L., Krishnadas R., Ramakrishnan R., Thulasiraj R.D., et al. Utilisation of eye care services in rural south India: the Aravind Comprehensive Eye Survey. Br J Ophthalmol. 2004;88:1237–1241. doi: 10.1136/bjo.2004.042606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 470.Snellingen T., Shrestha B.R., Gharti M.P., Shrestha J.K., Upadhyay M.P., Pokhrel R.P. Socioeconomic barriers to cataract surgery in Nepal: the South Asian cataract management study. Br J Ophthalmol. 1998;82:1424–1428. doi: 10.1136/bjo.82.12.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 471.Turner A.W., Xie J., Arnold A.L., Dunn R.A., Taylor H.R. Eye health service access and utilization in the national indigenous eye health survey. Clin Exp Ophthalmol. 2011;39:598–603. doi: 10.1111/j.1442-9071.2011.02529.x. [DOI] [PubMed] [Google Scholar]
- 472.Cooper-Patrick L., Gallo J.J., Gonzales J.J., Vu H.T., Powe N.R., Nelson C., et al. Race, gender, and partnership in the patient-physician relationship. JAMA Ophthalmology. 1999;282:583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 473.Baunach E., Lines D., Pedwel B., Lange F.D., Cooney R.M., Taylor H.R. The development of culturally safe and relevant health promotion resources for effective trachoma elimination in remote aboriginal communities. Aborig Isl Health Work J. 2012;36:9. [Google Scholar]
- 474.Tanywe A.C., Green H., Fernandez R. JBI evidence synthesis; 2022. Perceptions and practices of community members relating to trachoma in Africa: a qualitative systematic review. [DOI] [PubMed] [Google Scholar]
- 475.Mtuy T.B., Burton M.J., Mwingira U., Ngondi J.M., Seeley J., Lees S. Knowledge, perceptions and experiences of trachoma among Maasai in Tanzania: implications for prevention and control. PLoS Neglected Trop Dis. 2019;13 doi: 10.1371/journal.pntd.0007508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 476.Neyhouser C., Quinn I., Hillgrove T., Chan R., Chhea C., Peou S., et al. A qualitative study on gender barriers to eye care access in Cambodia. BMC Ophthalmol. 2018;18:217. doi: 10.1186/s12886-018-0890-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 477.Burton M.J., Ramke J., Marques A.P., Bourne R.R.A., Congdon N., Jones I., et al. The Lancet global health commission on global eye health: vision beyond 2020. Lancet Global Health. 2021;9:e489–e551. doi: 10.1016/S2214-109X(20)30488-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 478.Courtright P., Lewallen S. Why are we addressing gender issues in vision loss? Community Eye Health. 2009;22:17–19. [PMC free article] [PubMed] [Google Scholar]
- 479.Lewallen S., Mousa A., Bassett K., Courtright P. Cataract surgical coverage remains lower in women. Br J Ophthalmol. 2009;93:295–298. doi: 10.1136/bjo.2008.140301. [DOI] [PubMed] [Google Scholar]
- 480.Bradford J., Reisner S.L., Honnold J.A., Xavier J. Experiences of transgender-related discrimination and implications for health: results from the Virginia Transgender Health Initiative Study. Am J Publ Health. 2013;103:1820–1829. doi: 10.2105/AJPH.2012.300796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 481.Kenagy G.P. Transgender health: findings from two needs assessment studies in Philadelphia. Health Soc Work. 2005;30:19–26. doi: 10.1093/hsw/30.1.19. [DOI] [PubMed] [Google Scholar]
- 482.Kulkarni S., Lawande D.D., Dharmadhikari S., Deshpande C.M. Exploring the barriers for eye care among transgenders and commercial sex workers in Pune. Maharashtra. Indian J Ophthalmol. 2021;69:2277–2281. doi: 10.4103/ijo.IJO_3480_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 483.Erickson S., Sullivan A.G., Abad J.C., Alves M., Barabino S., Craig J.P., et al. TFOS: unique challenges and unmet needs for the management of ocular surface diseases throughout the world. Ocul Surf. 2021;22:242–244. doi: 10.1016/j.jtos.2021.08.014. [DOI] [PubMed] [Google Scholar]
- 484.OECD. Burden of out-of-pocket health expenditure. In Health at a Glance, OECD Indicators, OECD Publishing, Paris. 10.1787/health_glance-2011-54-en. [DOI]
- 485.Banthin J.S., Cunningham P., Bernard D.M. Financial burden of health care, 2001-2004. Health Aff. 2008;27:188–195. doi: 10.1377/hlthaff.27.1.188. [DOI] [PubMed] [Google Scholar]
- 486.Hoffman C., Paradise J. Health insurance and access to health care in the United States. Ann N Y Acad Sci. 2008;1136:149–160. doi: 10.1196/annals.1425.007. [DOI] [PubMed] [Google Scholar]
- 487.Wagstaff A., Eozenou P.H.-V., Smitz M.-D. World Bank; Washington DC: 2019. Out-of-Pocket expenditures on health: a global stocktake. World bank policy research working papers; p. 38. [Google Scholar]
- 488.Selvaraj S., Farooqui H.H., Karan A. Quantifying the financial burden of households' out-of-pocket payments on medicines in India: a repeated cross-sectional analysis of National Sample Survey data, 1994–2014. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2017-018020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 489.Berg E.J., Ying G.S., Maguire M.G., Sheffield P.E., Szczotka-Flynn L.B., Asbell P.A., et al. Climatic and environmental correlates of dry eye disease severity: a report from the dry eye assessment and management (dream) study. Trans Vis Sci Tech. 2020;9:25. doi: 10.1167/tvst.9.5.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 490.Sahai A., Malik P. Dry eye: prevalence and attributable risk factors in a hospital-based population. Indian J Ophthalmol. 2005;53:87–91. doi: 10.4103/0301-4738.16170. [DOI] [PubMed] [Google Scholar]
- 491.Lee K.W., Choi Y.H., Hwang S.H., Paik H.J., Kim M.K., Wee W.R., et al. Outdoor air pollution and pterygium in Korea. J Kor Med Sci. 2017;32:143–150. doi: 10.3346/jkms.2017.32.1.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 492.Ani K., Anyika V., Mutambara E. The impact of climate change on food and human security in Nigeria. Int J Clim Change Strat Manage. 2022;14:148–167. [Google Scholar]
- 493.Parvin G., Ahsan R. Impacts of climate change on food security of rural poor women in Bangladesh. Manage Env Qual. 2013;24 [Google Scholar]
- 494.Kraemer K., Gilbert C. Do vitamin A deficiency and undernutrition still matter? Community Eye Health. 2013;26:61–63. [PMC free article] [PubMed] [Google Scholar]
- 495.Ahmed T., Zounemat-Kermani M., Scholz M. Climate change, water quality and water-related challenges: a review with focus on Pakistan. Int J Environ Res Publ Health. 2020;17 doi: 10.3390/ijerph17228518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 496.Paavola J. Health impacts of climate change and health and social inequalities in the UK. Environ Health. 2017;16:113. doi: 10.1186/s12940-017-0328-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 497.Murthy R.S., Lakshminarayana R. Mental health consequences of war: a brief review of research findings. World Psychiatr. 2006;5:25–30. [PMC free article] [PubMed] [Google Scholar]
- 498.Ahmed M., Whitestone N., Patnaik J.L., Hossain M.A., Husain L., Alauddin M., et al. Burden of eye disease and demand for care in the Bangladesh Rohingya displaced population and host community: a cohort study. PLoS Med. 2020;17 doi: 10.1371/journal.pmed.1003096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 499.Gelaw Y., Abateneh A. Ocular morbidity among refugees in Southwest Ethiopia. Ethiopian J Health Sci. 2014;24:227–234. doi: 10.4314/ejhs.v24i3.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 500.Kawuma M. Eye diseases and blindness in Adjumani refugee settlement camps, Uganda. East Afr Med J. 2000;77:580–582. doi: 10.4314/eamj.v77i11.46724. [DOI] [PubMed] [Google Scholar]
- 501.Kaphle D., Gyawali R., Kandel H., Reading A., Msosa J.M. Vision impairment and ocular morbidity in a refugee population in Malawi. Optom Vis Sci. 2016;93:188–193. doi: 10.1097/OPX.0000000000000775. [DOI] [PubMed] [Google Scholar]
- 502.Ngondi J., Ole-Sempele F., Onsarigo A., Matende I., Baba S., Reacher M., et al. Prevalence and causes of blindness and low vision in southern Sudan. PLoS Med. 2006;3:e477. doi: 10.1371/journal.pmed.0030477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 503.Bin Yameen T.A., Abadeh A., Lichter M. Visual impairment and unmet eye care needs among a Syrian pediatric refugee population in a Canadian city. Can J Ophthalmol. 2019;54:668–673. doi: 10.1016/j.jcjo.2019.03.009. [DOI] [PubMed] [Google Scholar]
- 504.Selvarajah S., Dunt D.R., Marella M., Hewitt A.W., Turner N., Carozzi P., et al. Vision impairment and refractive errors in refugees presenting to community optometry clinics in Victoria, Australia. Clin Exp Optom. 2020;103:668–674. doi: 10.1111/cxo.13010. 20. [DOI] [PubMed] [Google Scholar]
- 505.Bal S., Duckles A., Buttenheim A. Visual health and visual healthcare access in refugees and displaced persons: a systematic review. J Immigr Minority Health. 2019;21:161–174. doi: 10.1007/s10903-018-0766-x. [DOI] [PubMed] [Google Scholar]
- 506.Sherwin J.C., Reacher M.H., Dean W.H., Ngondi J. Epidemiology of vitamin A deficiency and xerophthalmia in at-risk populations. Trans Royal Soc Hyg Trop Med. 2012;106:205–214. doi: 10.1016/j.trstmh.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 507.Seal A.J., Creeke P.I., Mirghani Z., Abdalla F., McBurney R.P., Pratt L.S., et al. Iron and vitamin A deficiency in long-term African refugees. J Nutr. 2005;135:808–813. doi: 10.1093/jn/135.4.808. [DOI] [PubMed] [Google Scholar]
- 508.Elbeyli A., Kurtul B.E. A series of civilian ocular injuries from the Civil war in Syria. Beyoglu Eye J. 2020;5:205–208. doi: 10.14744/bej.2020.58661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 509.Ari A.B. Eye injuries on the battlefields of Iraq and Afghanistan: public health implications. Optometry. 2006;77:329–339. doi: 10.1016/j.optm.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 510.Liu W., Yu B., Bursztyn L., Malvankar-Mehta M.S. Eye injuries sustained during protests due to non-lethal weaponry: a systematic review. Expet Rev Ophthalmol. 2021;16:297–304. [Google Scholar]
- 511.Anon The war on Syrian civilians (Editorial) Lancet. 2014;383:383. doi: 10.1016/S0140-6736(14)60134-3. [DOI] [PubMed] [Google Scholar]
- 512.Lavy T., Asleh S.A. Ocular rubber bullet injuries. Eye. 2003;17:821–824. doi: 10.1038/sj.eye.6700447. [DOI] [PubMed] [Google Scholar]
- 513.Beare J.D. Eye injuries from assault with chemicals. Br J Ophthalmol. 1990;74:514–518. doi: 10.1136/bjo.74.9.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 514.Morgan S.J. Chemical burns of the eye: causes and management. Br J Ophthalmol. 1987;71:854–857. doi: 10.1136/bjo.71.11.854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 515.Sahraravand A., Haavisto A.-K., Holopainen J.M., Leivo T. Ocular traumas in working age adults in Finland – helsinki ocular trauma study. Acta Ophthalmol. 2017;95:288–294. doi: 10.1111/aos.13313. [DOI] [PubMed] [Google Scholar]
- 516.Ghosh S., Salvador-Culla B., Kotagiri A.K., Pushpoth S., Tey A., Johnson Z.K., et al. Acute chemical eye injury and limbal stem cell deficiency: a prospective study in the United Kingdom. Cornea. 2019;38:8–12. doi: 10.1097/ICO.0000000000001739. [DOI] [PubMed] [Google Scholar]
- 517.Merle H., Donnio A., Ayeboua L., Michel F., Thomas F., Ketterle J., et al. Alkali ocular burns in Martinique (French West Indies): evaluation of the use of an amphoteric solution as the rinsing product. Burns. 2005;31:205–211. doi: 10.1016/j.burns.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 518.Ukponmwan C.U. Chemical injuries to the eye in Benin City, Nigeria. W Afr J Med. 2000;19:71–76. [PubMed] [Google Scholar]
- 519.Olaitan P.B., Jiburum B.C. Chemical injuries from assaults: an increasing trend in a developing country. Indian J Plast Surg. 2008;41:20–23. doi: 10.4103/0970-0358.41106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 520.Dua H.S., Ting D.S.J., Al Saadi A., Said D.G. Chemical eye injury: pathophysiology, assessment and management. Eye. 2020;34:2001–2019. doi: 10.1038/s41433-020-1026-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 521.Chau J.P.C., Lee D.T.F., Lo S.H.S. A systematic review of methods of eye irrigation for adults and children with ocular chemical burns. Worldviews Evidence-Based Nurs. 2012;9:129–138. doi: 10.1111/j.1741-6787.2011.00220.x. [DOI] [PubMed] [Google Scholar]
- 522.Eslani M., Baradaran-Rafii A., Movahedan A., Djalilian A.R. The ocular surface chemical burns. J Ophthalmol. 2014;2014 doi: 10.1155/2014/196827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 523.Bouchard C.S., John T. Amniotic membrane transplantation in the management of severe ocular surface disease: indications and outcomes. Ocul Surf. 2004;2:201–211. doi: 10.1016/s1542-0124(12)70062-9. [DOI] [PubMed] [Google Scholar]
- 524.Clare G., Suleman H., Bunce C., Dua H. Amniotic membrane transplantation for acute ocular burns. Cochrane Database Syst Rev. 2012;2012:Cd009379. doi: 10.1002/14651858.CD009379.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 525.Basu S., Ali H., Sangwan V.S. Clinical outcomes of repeat autologous cultivated limbal epithelial transplantation for ocular surface burns. Am J Ophthalmol. 2012;153:643–650. doi: 10.1016/j.ajo.2011.09.016. 50.e1-2. [DOI] [PubMed] [Google Scholar]
- 526.Basu S., Mohamed A., Chaurasia S., Sejpal K., Vemuganti G.K., Sangwan V.S. Clinical outcomes of penetrating keratoplasty after autologous cultivated limbal epithelial transplantation for ocular surface burns. Am J Ophthalmol. 2011;152:917–924. doi: 10.1016/j.ajo.2011.05.019. e1. [DOI] [PubMed] [Google Scholar]
- 527.Klifto K.M., Elhelali A., Gurno C.F., Seal S.M., Asif M., Hultman C.S. Acute surgical vs non-surgical management for ocular and peri-ocular burns: a systematic review and meta-analysis. Burns Trauma. 2019;7:25. doi: 10.1186/s41038-019-0161-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 528.Kim Y.J., Payal A.R., Daly M.K. Effects of tear gases on the eye. Surv Ophthalmol. 2016;61:434–442. doi: 10.1016/j.survophthal.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 529.Cohen A.R., Renner L.M., Shriver E.M. Intimate partner violence in ophthalmology: a global call to action. Curr Opin Ophthalmol. 2017;28:534–538. doi: 10.1097/ICU.0000000000000397. [DOI] [PubMed] [Google Scholar]
- 530.Butchart A., Mikton C., Dahlberg L.L., Krug E.G. Global status report on violence prevention 2014. Inj Prev. 2015;21:213. doi: 10.1136/injuryprev-2015-041640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 531.Kaur N., Kumar A. Vitriolage (vitriolism) - a medico-socio-legal review. Forensic Sci Med Pathol. 2020;16:481–488. doi: 10.1007/s12024-020-00230-7. [DOI] [PubMed] [Google Scholar]
- 532.Walsh D. New York Times; 2012. Years after acid horror, suicide stirs Pakistan.https://www.nytimes.com/2012/04/10/world/asia/hope-in-pakistan-for-curbing-acid-attacks.html [Google Scholar]
- 533.Dhar S. USA Today; 2017. Acid attacks against women in India on the rise; survivors fight back.https://www.usatoday.com/story/news/world/2017/07/27/acid-attacks-women-india-survivors-fight-back/486007001/ [Google Scholar]
- 534.Ahmad N. Weak laws against acid attacks on women: an Indian perspective. J Medico-Legal. 2012;80:110–120. doi: 10.1258/mlj.2012.012020. [DOI] [PubMed] [Google Scholar]
- 535.Kalantry S., Kestenbaum J. Avon global centre for women and justice and dorothea S. Clarke program in feminist jurisprudence. Cornell Law School International Human Rights Clinic and the Virtue Foundation; 2011. Combating acid violence in Bangladesh, India, and Cambodia. [Google Scholar]
- 536.Anon . Kuala Lumpur; Malaysia: 2002. Baseline report: violence against women in Bangladesh. International Women's rights action watch Asia pacific. [Google Scholar]
- 537.Williams H., Bateman D.N., Thomas S.H.L., Thompson J.P., Scott R.A.H., Vale J.A. Exposure to liquid detergent capsules: a study undertaken by the UK National Poisons Information Service. Clin Toxicol. 2012;50:776–780. doi: 10.3109/15563650.2012.709937. [DOI] [PubMed] [Google Scholar]
- 538.Haring R.S., Sheffield I.D., Frattaroli S. Detergent pod–related eye injuries among preschool-aged children. JAMA Ophthalmology. 2017;135:283–284. doi: 10.1001/jamaophthalmol.2016.5694. [DOI] [PubMed] [Google Scholar]
- 539.Breazzano M.P., Day H.R., Tanaka S., Tran U. Prospective analysis of pediatric ocular chemical burns: laundry detergent pods. J AAPOS. 2018;22:426–428. doi: 10.1016/j.jaapos.2018.07.349. [DOI] [PubMed] [Google Scholar]
- 540.Chen A.J., Linakis J.G., Mello M.J., Greenberg P.B. Epidemiology of infant ocular and periocular injuries from consumer products in the United States, 2001-2008. J AAPOS. 2013;17 3:239–242. doi: 10.1016/j.jaapos.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 541.Vajpayee R.B., Shekhar H., Sharma N., Jhanji V. Demographic and clinical profile of ocular chemical injuries in the pediatric age group. Ophthalmology. 2014;121 1:377–380. doi: 10.1016/j.ophtha.2013.06.044. [DOI] [PubMed] [Google Scholar]
- 542.Haring R.S., Sheffield I.D., Channa R., Canner J.K., Schneider E.B. Epidemiologic trends of chemical ocular burns in the United States. JAMA Ophthalmology. 2016;134 10:1119–1124. doi: 10.1001/jamaophthalmol.2016.2645. [DOI] [PubMed] [Google Scholar]
- 543.Jolly R., Arjunan M., Theodorou M., Dahlmann-Noor A.H. Eye injuries in children - incidence and outcomes: an observational study at a dedicated children's eye casualty. Eur J Ophthalmol. 2019;29:499–503. doi: 10.1177/1120672118803512. [DOI] [PubMed] [Google Scholar]
- 544.Baker M.L., Painter G., Hewitt A.W., Islam F.M.A., Szetu J., Qalo M., et al. Profile of ocular trauma in the Solomon Islands. Clin Exp Ophthalmol. 2014;42:440–446. doi: 10.1111/ceo.12256. [DOI] [PubMed] [Google Scholar]
- 545.Bickham D.S., Hswen Y., Rich M. Media use and depression: exposure, household rules, and symptoms among young adolescents in the USA. Int J Public Health. 2015;60:147–155. doi: 10.1007/s00038-014-0647-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 546.Skogen J.C., Hjetland G.J., Boe T., Hella R.T., Knudsen A.K. Through the looking glass of social media. Focus on self-presentation and association with mental health and quality of life. A cross-sectional survey-based study. Int J Environ Res Publ Health. 2021;18 doi: 10.3390/ijerph18063319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 547.Wang K.T., Fu S.H., Hsieh P.L., Lin Y.L., Yang S.Y. Investigating the relationship between media usage, depression, and quality of life among older adults. Healthcare (Basel) 2021;9 doi: 10.3390/healthcare9091154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 548.Wu H.Y., Chiou A.F. Social media usage, social support, intergenerational relationships, and depressive symptoms among older adults. Geriatr Nurs. 2020;41:615–621. doi: 10.1016/j.gerinurse.2020.03.016. [DOI] [PubMed] [Google Scholar]
- 549.Cotten S.R., Anderson W.A., McCullough B.M. Impact of internet use on loneliness and contact with others among older adults: cross-sectional analysis. J Med Internet Res. 2013;15:e39. doi: 10.2196/jmir.2306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 550.Shome D., Vadera S., Male S.R., Kapoor R. Does taking selfies lead to increased desire to undergo cosmetic surgery. J Cosmet Dermatol. 2020;19:2025–2032. doi: 10.1111/jocd.13267. [DOI] [PubMed] [Google Scholar]
- 551.Arab K., Barasain O., Altaweel A., Alkhayyal J., Alshiha L., Barasain R., et al. Influence of social media on the decision to undergo a cosmetic procedure. Plast Reconstr Surg Glob Open. 2019;7:e2333. doi: 10.1097/GOX.0000000000002333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 552.Petrosyan A. Statista Research Department; 2023. Worldwide digital population 2023. Internet and social media users in the world 2023 | Statista. [Google Scholar]
- 553.Fox S., Duggan M. Pew Research Center; 2013. Health Online 2013. One in three American adults have gone online to figure out a medical condition. [Google Scholar]
- 554.Laugesen J., Hassanein K., Yuan Y. The impact of internet health information on patient compliance: a research model and an empirical study. J Med Internet Res. 2015;17:e143. doi: 10.2196/jmir.4333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 555.Shaver J. The state of telehealth before and after the COVID-19 pandemic. PrimaryCare. 2022;10 doi: 10.1016/j.pop.2022.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 556.Donelan K., Barreto E.A., Sossong S., Michael C., Estrada J.J., Cohen A.B., et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care. 2019;25:40–44. [PubMed] [Google Scholar]
- 557.Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatr. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 558.Richa S., Yazbek J.C. Ocular adverse effects of common psychotropic agents: a review. CNS Drugs. 2010;24 doi: 10.2165/11533180-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 559.Park J.S.Y., Sharma R.A., Sharma V. Ophthalmic adverse effects of lithium. Int Clin Psychopharmacol. 2020;35:69–73. doi: 10.1097/YIC.0000000000000295. [DOI] [PubMed] [Google Scholar]
- 560.2020 COVID-19: les ophtalmologistes s’organisent (Etude SNOF) National Union of Ophthalmologists of France; 2020. [Google Scholar]
- 561.AAO surveys reveal severe effect COVID-19 is having on ophthalmology practices. Eyewire News; 2020. [Google Scholar]
- 562.Hutton D. COVID-19: as patients avoid appointments, vision may be in jeopardy. Ophthalmol Times. 2020 https://ophthalmologytimes.com [Google Scholar]
- 563.Saleem S.M., Pasquale L.R., Sidoti P.A., Tsai J.C. Virtual ophthalmology: telemedicine in a COVID-19 era. Am J Ophthalmol. 2020;216:237–242. doi: 10.1016/j.ajo.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 564.Aziz K., Moon J.Y., Parikh R., Lorch A.C., Friedman D.S., Miller J.B., et al. Association of patient characteristics with delivery of ophthalmic telemedicine during the COVID-19 pandemic. JAMA Ophthalmology. 2021;139:1174–1182. doi: 10.1001/jamaophthalmol.2021.3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 565.Emparan J.P.O., Sardi-Correa C., López-Ulloa J.A., Viteri-Soria J., Penniecook J.A., Jimenez-Román J., et al. COVID-19 and the eye: how much do we really know? A best evidence review. Arq Bras Oftalmol. 2020;83:250–261. doi: 10.5935/0004-2749.20200067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 566.Aggarwal K., Agarwal A., Jaiswal N., Dahiya N., Ahuja A., Mahajan S., et al. Ocular surface manifestations of coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. PLoS One. 2020;15 doi: 10.1371/journal.pone.0241661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 567.Barabino S. A narrative review of current understanding and classification of dry eye disease with new insights on the impact of dry eye during the COVID-19 pandemic. Ophthalmol Ther. 2021;10:495–507. doi: 10.1007/s40123-021-00373-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 568.Inomata T., Kitazawa K., Kuno T., Sung J., Nakamura M., Iwagami M., et al. Clinical and prodromal ocular symptoms in coronavirus disease: a systematic review and meta-analysis. Invest Ophthalmol Vis Sci. 2020;61:29. doi: 10.1167/iovs.61.10.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 569.Jin Y.P., Trope G.E., El-Defrawy S., Liu E.Y., Buys Y.M. Ophthalmology-focused publications and findings on COVID-19: a systematic review. Eur J Ophthalmol. 2021;31:1677–1687. doi: 10.1177/1120672121992949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 570.Koh S., Rhee M.K. COVID-19 and dry eye. Eye Contact Lens. 2021;47:317–322. doi: 10.1097/ICL.0000000000000797. [DOI] [PubMed] [Google Scholar]
- 571.Zhong Y., Wang K., Zhu Y., Lyu D., Yu Y., Li S., et al. Ocular manifestations in COVID-19 patients: a systematic review and meta-analysis. Trav Med Infect Dis. 2021;44 doi: 10.1016/j.tmaid.2021.102191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 572.Wells G., Shea B., O'Connell J. Ottawa Health Research Institute; 2014. The newcastle-ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses.https://oa.mg/work/2612891587 [Google Scholar]
- 573.McKenzie J.E., Brennan S.E. In: Cochrane handbook for systematic reviews of interventions. 6.3 ed. Higgins J.P.T.T.J., Chandler J., Cumpston M., Li T., Page M.J., Welch V.A., editors. Cochrane; 2022. Chapter 12: synthesizing and presenting findings using other methods.https://training.cochrane.org/handbook/current/chapter-12 [Google Scholar]
- 574.Acet Y., Çil B., Kabak M., Vural E. Instability of tear film after novel coronavirus disease: a noninvasive and No contact method by a scheimpflug-placido disc topographer. Klin Monbl Augenheilkd. 2022;239:338–345. doi: 10.1055/a-1585-2239. [DOI] [PubMed] [Google Scholar]
- 575.Bahkir F.A., Grandee S.S. Impact of the COVID-19 lockdown on digital device-related ocular health. Indian J Ophthalmol. 2020;68:2378–2383. doi: 10.4103/ijo.IJO_2306_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 576.Bitirgen G., Korkmaz C., Zamani A., Ozkagnici A., Zengin N., Ponirakis G., et al. Corneal confocal microscopy identifies corneal nerve fibre loss and increased dendritic cells in patients with long COVID. Br J Ophthalmol. 2021;106:1635–1641. doi: 10.1136/bjophthalmol-2021-319450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 577.Boccardo L. Self-reported symptoms of mask-associated dry eye: a survey study of 3,605 people. Contact Lens Anterior Eye. 2022;45 doi: 10.1016/j.clae.2021.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 578.Alabdulkader B. Effect of digital device use during COVID-19 on digital eye strain. Clin Exp Optom. 2021;104:698–704. doi: 10.1080/08164622.2021.1878843. [DOI] [PubMed] [Google Scholar]
- 579.Bozkurt E., Özateş S., Muhafız E., Yılmaz F., Calıskan O. Ocular surface and conjunctival cytology findings in patients with confirmed COVID-19. Eye Contact Lens. 2021;47:168–173. doi: 10.1097/ICL.0000000000000752. [DOI] [PubMed] [Google Scholar]
- 580.Cartes C., Segovia C., Salinas-Toro D., Goya C., Alonso M.J., Lopez-Solis R., et al. Dry eye and visual display terminal-related symptoms among university students during the coronavirus disease pandemic. Ophthalmic Epidemiol. 2022;29:245–251. doi: 10.1080/09286586.2021.1943457. [DOI] [PubMed] [Google Scholar]
- 581.D'Amico Ricci G., Del Turco C., Belcastro E., Palisi M., Romano M.R., Pinna A., et al. Covid-19 and acute conjunctivitis: controversial data from a tertiary refferral Italian center. Eur J Ophthalmol. 2021;31:2910–2913. doi: 10.1177/1120672121991049. [DOI] [PubMed] [Google Scholar]
- 582.Galindo-Romero C., Ruiz-Porras A., García-Ayuso D., Di Pierdomenico J., Sobrado-Calvo P., Valiente-Soriano F.J. Computer vision syndrome in the Spanish population during the COVID-19 lockdown. Optom Vis Sci. 2021;98:1255–1262. doi: 10.1097/OPX.0000000000001794. [DOI] [PubMed] [Google Scholar]
- 583.Gambini G., Savastano M.C., Savastano A., De Vico U., Crincoli E., Cozzupoli G.M., et al. Ocular surface impairment after coronavirus disease 2019: a cohort study. Cornea. 2021;40:477–483. doi: 10.1097/ICO.0000000000002643. [DOI] [PubMed] [Google Scholar]
- 584.Gangaputra S.S., Patel S.N. Ocular symptoms among nonhospitalized patients who underwent COVID-19 testing. Ophthalmology. 2020;127:1425–1427. doi: 10.1016/j.ophtha.2020.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 585.Ganne P., Najeeb S., Chaitanya G., Sharma A., Krishnappa N.C. Digital eye strain epidemic amid COVID-19 pandemic - a cross-sectional survey. Ophthalmic Epidemiol. 2021;28:285–292. doi: 10.1080/09286586.2020.1862243. [DOI] [PubMed] [Google Scholar]
- 586.Krolo I., Blazeka M., Merdzo I., Vrtar I., Sabol I., Petric-Vickovic I. Mask-associated dry eye during COVID-19 pandemic-how face masks contribute to dry eye disease symptoms. Med Arch. 2021;75:144–148. doi: 10.5455/medarh.2021.75.144-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 587.Kuroyedov A.V., Zavadski P.C.H., Brezhnev A.Y.U., Gorodnichii V.V., Gazizova I.R., Seleznev A.V., et al. Influence of personal respiratory and visual protective equipment on the development and progression of dry eye syndrome. Oftalmologiya. 2020;17:519–526. [Google Scholar]
- 588.Lavista Ferres J.M., Meirick T., Lomazow W., Lee C.S., Lee A.Y., Lee M.D. Association of public health measures during the COVID-19 pandemic with the incidence of infectious conjunctivitis. JAMA Ophthalmology. 2022;140:43–49. doi: 10.1001/jamaophthalmol.2021.4852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 589.Long Y., Wang X., Tong Q., Xia J., Shen Y. Investigation of dry eye symptoms of medical staffs working in hospital during 2019 novel coronavirus outbreak. Medicine (Baltim) 2020;99 doi: 10.1097/MD.0000000000021699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 590.Maniaci A., Ferlito S., Bubbico L., Ledda C., Rapisarda V., Iannella G., et al. Comfort rules for face masks among healthcare workers during COVID-19 spread. Ann Ig. 2021;33:615–627. doi: 10.7416/ai.2021.2439. [DOI] [PubMed] [Google Scholar]
- 591.Martin G.C., Le Roux G., Guindolet D., Boulanger E., Hasle D., Morin E., et al. Pediatric eye injuries by hydroalcoholic gel in the context of the coronavirus disease 2019 pandemic. JAMA Ophthalmology. 2021;139:348–351. doi: 10.1001/jamaophthalmol.2020.6346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 592.Martinez-Perez C., Monteiro B., Soares M., Portugues F., Matos S., Ferreira A., et al. Influence of face masks on the use of contact lenses. Int J Environ Res Publ Health. 2021;18:7407. doi: 10.3390/ijerph18147407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 593.Mastropasqua L., Lanzini M., Brescia L., D'Aloisio R., Nubile M., Ciancaglini M., et al. Face mask-related ocular surface modifications during COVID-19 pandemic: a clinical, in vivo confocal microscopy, and immune-cytology study. Trans Vis Sci Tech. 2021;10:22. doi: 10.1167/tvst.10.3.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 594.Mengi E., Kara C.O., Alptürk U., Topuz B. The effect of face mask usage on the allergic rhinitis symptoms in patients with pollen allergy during the covid-19 pandemic. Am J Otolaryngol. 2022;43 doi: 10.1016/j.amjoto.2021.103206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 595.Negishi K., Ayaki M. Presbyopia developed earlier during the COVID-19 pandemic. PLoS One. 2021;16 doi: 10.1371/journal.pone.0259142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 596.Niveditha K.P., Dheepak Sundar M. Digital vision syndrome (DVS) among medical students during COVID-19 pandemic curfew. Int J Res Pharm Sci. 2020;11:1128–1133. [Google Scholar]
- 597.Oruc Y., Aydin S., Akkoc R.F., Gul F.C., Ugur K., Sahin İ., et al. Assessment of the frequency and biochemical parameters of conjunctivitis in COVID-19 and other viral and bacterial conditions. Turk J Biochem. 2020;45:443–449. [Google Scholar]
- 598.Öztürk H., Özen B. The effects of smartphone, tablet and computer overuse on children's eyes during the COVID-19 pandemic. J Ped Res. 2021;8:491–497. [Google Scholar]
- 599.Pardhan S., Vaughan M., Zhang J., Smith L., Chichger H. Sore eyes as the most significant ocular symptom experienced by people with COVID-19: a comparison between pre-COVID-19 and during COVID-19 states. BMJ Open. 2020;5 doi: 10.1136/bmjophth-2020-000632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 600.Pavithra S., Dheepak Sundar M. Assessment of dry eye symptoms and quality of sleep in engineering students during the COVID-19 pandemic. Int J Res Pharm Sci. 2020;11:1202–1207. [Google Scholar]
- 601.Rokohl A.C., Loreck N., Wawer Matos P.A., Zwingelberg S., Augustin M., Dewald F., et al. More than loss of taste and smell: burning watering eyes in coronavirus disease 2019. Clin Microbiol Infect. 2020;26:1560. doi: 10.1016/j.cmi.2020.08.018. e5-e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 602.Sarkar D., Soni D., Nagpal A., Khurram F., Karkhur S., Verma V., et al. Ocular manifestations of RT-PCR-confirmed COVID-19 cases in a large database cross-sectional study. BMJ Open. 2021;6 doi: 10.1136/bmjophth-2021-000775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 603.Scalinci S.Z., Pacella E., Battagliola E.T. Prolonged face mask use might worsen dry eye symptoms. Indian J Ophthalmol. 2021;69:1508–1510. doi: 10.4103/ijo.IJO_2641_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 604.Serban A., Mihai A., Dima A., Balaban D.V., Jinga M., Jurcut C. The impact of the COVID-19 pandemic on patients with primary Sjögren syndrome. Rheumatol Int. 2021;41:1933–1940. doi: 10.1007/s00296-021-04967-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 605.Shah K., Desai S., Lo H., Gadhavi B., Prajapati V., Bhavsar P., et al. COVID 19 and ophthalmic morbidity among college students attending online teaching. Ind J Forensic Med Toxic. 2021;15:413–421. [Google Scholar]
- 606.Silkiss R.Z., Paap M.K., Ugradar S. Increased incidence of chalazion associated with face mask wear during the COVID-19 pandemic. Am J Ophthalmol Case Rep. 2021;22 doi: 10.1016/j.ajoc.2021.101032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 607.Usgaonkar U., Shet Parkar S.R., Shetty A. Impact of the use of digital devices on eyes during the lockdown period of COVID-19 pandemic. Indian J Ophthalmol. 2021;69:1901–1906. doi: 10.4103/ijo.IJO_3500_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 608.Wang L., Wei X., Deng Y. Computer vision syndrome during SARS-CoV-2 outbreak in university students: a comparison between online courses and classroom lectures. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.696036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 609.Wang Y., Lou J., Ji Y., Wang Z. Increased photokeratitis during the coronavirus disease 2019 pandemic: clinical and epidemiological features and preventive measures. Medicine (Baltim) 2021;100 doi: 10.1097/MD.0000000000026343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 610.Li R., Ying B., Qian Y., Chen D., Li X., Zhu H., et al. Prevalence of self-reported symptoms of computer vision syndrome and associated risk factors among school students in China during the COVID-19 pandemic. Ophthalmic Epidemiol. 2022;29:363–373. doi: 10.1080/09286586.2021.1963786. [DOI] [PubMed] [Google Scholar]
- 611.García Lorente M., Zamorano Martín F., Rodríguez Calvo de Mora M., Rocha-de-Lossada C. Impact of the COVID-19 pandemic on ophthalmic emergency services in a tertiary hospital in Spain. Eur J Ophthalmol. 2022;32:NP313–N315. doi: 10.1177/1120672120958324. [DOI] [PubMed] [Google Scholar]
- 612.Cappa C.D., Asadi S., Barreda S., Wexler A.S., Bouvier N.M., Ristenpart W.D. Expiratory aerosol particle escape from surgical masks due to imperfect sealing. Sci Rep. 2021;11 doi: 10.1038/s41598-021-91487-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 613.Hadayer A., Zahavi A., Livny E., Gal-Or O., Gershoni A., Mimouni K., et al. Patients wearing face masks during intravitreal injections may be at a higher risk of endophthalmitis. Retina. 2020;40:1651–1656. doi: 10.1097/IAE.0000000000002919. [DOI] [PubMed] [Google Scholar]
- 614.Moshirfar M., West W.B., Jr., Marx D.P. Face mask-associated ocular irritation and dryness. Ophthalmol Ther. 2020;9:397–400. doi: 10.1007/s40123-020-00282-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 615.Koh S., Tung C., Kottaiyan R., Zavislan J., Yoon G., Aquavella J. Effect of airflow exposure on the tear meniscus. J Ophthalmol. 2012;2012 doi: 10.1155/2012/983182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 616.Chadwick O., Lockington D. Addressing post-operative mask-associated dry eye (MADE) Eye. 2021;35:1543–1544. doi: 10.1038/s41433-020-01280-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 617.Mansour E., Vishinkin R., Rihet S., Saliba W., Fish F., Sarfati P., et al. Measurement of temperature and relative humidity in exhaled breath. Sensor Actuator B Chem. 2019 [Google Scholar]
- 618.Beck D.E.R., Agarwal P. Re: cluster of chalazia in nurses using eye protection while caring for critically ill patients with COVID-19 in intensive care. Occup Environ Med. 2020;77:808. doi: 10.1136/oemed-2020-106871. [Letter)] [DOI] [PubMed] [Google Scholar]
- 619.Mégarbane B., Tadayoni R. Cluster of chalazia in nurses using eye protection while caring for critically ill patients with COVID-19 in intensive care. Occup Environ Med. 2020;77:584–585. doi: 10.1136/oemed-2020-106677. [DOI] [PubMed] [Google Scholar]
- 620.Aiello F., Gallo Afflitto G., Mancino R., Li J.O., Cesareo M., Giannini C., et al. Coronavirus disease 2019 (SARS-CoV-2) and colonization of ocular tissues and secretions: a systematic review. Eye. 2020;34:1206–1211. doi: 10.1038/s41433-020-0926-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 621.Cheong K.X. Systematic review of ocular involvement of SARS-CoV-2 in coronavirus disease 2019. Curr Ophthalmol Rep. 2020;8:185–194. doi: 10.1007/s40135-020-00257-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 622.Jevnikar K., Jaki Mekjavic P., Vidovic Valentincic N., Petrovski G., Globocnik Petrovic M. An update on COVID-19 related ophthalmic manifestations. Ocul Immunol Inflamm. 2021;29:684–689. doi: 10.1080/09273948.2021.1896008. [DOI] [PubMed] [Google Scholar]
- 623.La Distia Nora R., Putera I., Khalisha D.F., Septiana I., Ridwan A.S., Sitompul R. Are eyes the windows to COVID-19? Systematic review and meta-analysis. BMJ Open. 2020;5 doi: 10.1136/bmjophth-2020-000563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 624.Ling X.C., Kang E.Y., Lin J.Y., Chen H.C., Lai C.C., Ma D.H., et al. Ocular manifestation, comorbidities, and detection of severe acute respiratory syndrome-coronavirus 2 from conjunctiva in coronavirus disease 2019: a systematic review and meta-analysis. Taiwan J Ophthalmol. 2020;10:153–166. doi: 10.4103/tjo.tjo_53_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 625.Nasiri N., Sharifi H., Bazrafshan A., Noori A., Karamouzian M., Sharifi A. Ocular manifestations of COVID-19: a systematic review and meta-analysis. J Ophthalmol Vis Res. 2021;16:103–112. doi: 10.18502/jovr.v16i1.8256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 626.Saldanha I.J., Petris R., Makara M., Channa P., Akpek E.K. Impact of the COVID-19 pandemic on eye strain and dry eye symptoms. Ocul Surf. 2021;22:38–46. doi: 10.1016/j.jtos.2021.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 627.Yangzes S., Grewal S., Gailson T., Grewal S.P.S. Hand sanitizer-induced ocular injury: a COVID-19 hazard in children. JAMA Ophthalmology. 2021;139:362–364. doi: 10.1001/jamaophthalmol.2020.6351. [DOI] [PubMed] [Google Scholar]
- 628.Au S.C.L. Hand sanitizer associated ocular chemical injury: a mini-review on its rise under COVID-19. Vis J Emerg Med. 2020;21 doi: 10.1016/j.visj.2020.100881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 629.Redelmeier D.A., Thiruchelvam D. Hand hygiene sprayed into eye. IDCases. 2021;24 doi: 10.1016/j.idcr.2021.e01092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 630.Akbas E., Korkmaz I., Palamar M., Barut Selver O. Shifting trends in demographic features of chemical eye injuries during COVID-19 pandemic. Int Ophthalmol. 2022:1–6. doi: 10.1007/s10792-022-02211-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 631.Craig J.P., Alves M., Wolffsohn J.S., Downie L.E., Efron N., Galor A., et al. TFOS lifestyle: introduction. Ocul Surf. 2023 doi: 10.1016/j.jtos.2023.04.014. In press. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.