Abstract
Background
European Society of Cardiology (ESC) clinical practice guidelines are currently considered as an essential tool supporting many cardiologists in clinical decision-making not only in Europe but all-over the world. In this study we analyzed these recommendations regarding their class of recommendations (COR) and level of evidence (LOE) to detect how solid is the scientific background behind these recommendations.
Methods
We have abstracted all the current guidelines defined as “the guidelines available on the ESC website by 01 October 2022”. All recommendations were classified according to their COR (Class I, IIa, IIb, or III) and LOE (A, B, or C). As every topic has different number of recommendations, we have used the median values in comparisons between different topics to give all the topics the same weight.
Results
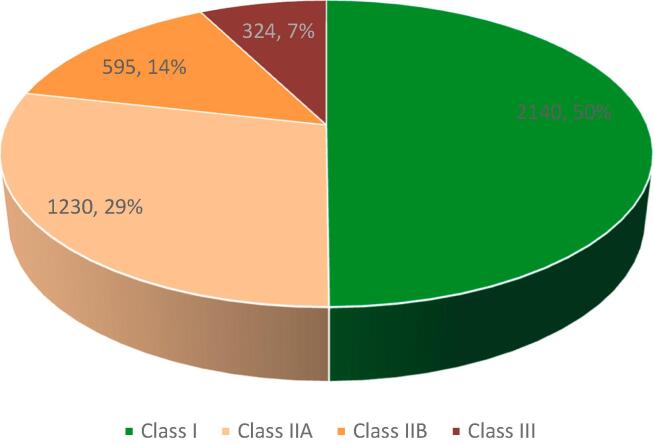
Current ESC guidelines consist of 37 clinical topics including a total of 4289 recommendations. Their distribution was 2140 with a median of 49.9% in Class I, Class II and Class III were 1825 with a median of 42.6% and 324 with a median of 7.5% respectively. LOE A was only present in 667(15.5%) recommendations, 1285(30%) in LOE B, while LOE C was behind the majority of the recommendations, 2337 with a median of 54.5%.
Conclusion
Although ESC guidelines are considered a gold standard for management of cardiovascular diseases, but surprisingly more than half of its recommendations are based on such scientific evidence. Deficiency in clinical trials is not the same across all guideline’s topics, some are needier for clinical research.
Keywords: Clinical Guidelines, Scientific Evidence, European Society of Cardiology
1. Introduction
The European Society of Cardiology (ESC) clinical guidelines are considered one of the most important practice guidelines in cardiovascular medicine. The first ESC guidelines topic was released in 1994 and thereafter more than 100 ESC clinical practice guidelines were published in the European Heart Journal. The ESC has an official body responsible for guidelines production called the guidelines task force, usually a group of 80–100 experts work together for two successive years to produce a set of guidelines according to fixed protocol and review process responsible for the quality of these scientific work. ESC guidelines are popular scientific piece of work for many cardiologists not only in Europe but also in a lot of countries across the world. Moreover, it has a great importance and popularity in most of the developing countries that don’t produce their own guidelines. The ESC guidelines almost cover all the essential topics in cardiovascular medicine with continuous updates according to the best available clinical data. Adherence to its recommendations has become the gold standard of healthcare in many countries and some organizations are using adherence to it in clinical practice as a parameter for measuring quality in hospitals.
The ESC guidelines in each topic consist of several recommendations regarding diagnosis, prevention and management of a certain cardiovascular disease. Each recommendation has a Class of Recommendation (COR) that is distinguished by the writing committee according to the clinical data supporting this recommendation. The COR scheme used in the ESC guidelines consist of four groups as follows [1]:
Class I: conditions for which there is evidence and/or general agreement that a given procedure or treatment is useful and effective.
Class II: conditions for which there is conflicting evidence and/or a divergence of opinion about the usefulness/efficacy of a procedure or treatment.
Class IIa: weight of evidence/opinion is in favor of usefulness/efficacy.
Class IIb: usefulness/efficacy is less well established by evidence/opinion.
Class III: conditions for which there is evidence and/or general agreement that the procedure/treatment is not useful/effective and in some cases may be harmful.
Each recommendation, which is classified either I, IIA, IIB or III has a level of evidence (LOE). This piece of information is very important to know the scientific evidence behind each recommendation. Pierluigi Tricoci et al [2] described the level of evidence as a “classification combines an objective description of the existence and the types of studies supporting the recommendation and expert consensus”. The ESC clinical guidelines across their production process aims to provide physicians with all the relevant data to answer any clinical question within the ESC core curriculum. Level of Evidence is classified into three categories A, B, or C as clarified by Ponikowski P et al [1]:
Level of evidence A: recommendation based on evidence from multiple randomized trials or meta-analyses.
Level of evidence B: recommendation based on evidence from a single randomized trial or non-randomized studies.
Level of evidence C: recommendation based on expert opinion, case studies, or standards of care.
The ESC clinical practice guidelines are considered one of the most appropriate approaches to evidence based medicine which is considering high quality clinical research in the management of different clinical scenarios [3]. Furthermore, there is a significant increase in clinical studies regarding cardiovascular diseases especially with the continuous evolution of new techniques and devices along the last two decades. These elements are supposed to strengthen the scientific background, decrease the gaps in evidence and areas of uncertainty within the ESC clinical guidelines. Accordingly, we performed this study to test this assumption, analyse and evaluate the adequacy of scientific evidence behind the ESC clinical guidelines, determine gaps in evidence and opportunities for improvement.
In 2009, Pierluigi Tricoci et al [2] has published a similar article analysing the scientific evidence behind the American College of Cardiology & American Heart Association (ACC/AHA) guidelines in cardiovascular medicine regarding the distribution of class of recommendations and level of evidence and the change over time in those guidelines. On the other hand, no previous studies were found regarding the analysis of the whole ESC clinical guidelines.
2. Aim of the work
Analyses of the current ESC clinical practice guidelines in all topics from year 2002 till the last quarter in year 2022 and evaluating the adequacy of scientific evidence behind all these guidelines and their recommendations to highlight the areas with gaps in evidence and detect opportunities for improvement.
3. Methods
All the topics of the ESC clinical practice current guidelines were downloaded from the ESC website, these included all current guidelines published from year 2002 till 01 October 2020. Current guidelines are defined as all the guidelines present on the ESC website; https://www.escardio.org/Guidelines by 01 October 2022. The latest and updated version of each topic was included. Current guidelines were analysed at least by two independent reviewers to abstract the number of recommendations within each topic, COR for each recommendation and its LOE. Each recommendation has a clear COR and LOE that is stated within the context of the guidelines. The observer did neither judgments nor classification for the guideline statements.
This analysis identified the distribution of recommendations across different classes of recommendations either I, IIA, IIB, or III and its level of evidence either A, B, or C to detect how these recommendations are bonded to solid scientific evidence. There was no duplication in topics as the ESC website provide the latest updated version for each topic and automatically archives the older one. Thus, we did not provide a clear data about change over time within the same topic. We evaluated the differences between topics; through comparison of the median values within each topic to provide equal weights as the total number of recommendations may vary across different topics. Median values are used to measure the differences between different topics to answer the question; does all CVD topics have similar scientific background and how far is the variability across topics.
4. Results
Current ESC guidelines at 01 October 2022 consist of 37 different clinical cardiovascular topics including a total of 4289 recommendations. The distribution of these recommendations across different classes of recommendations were; 2140 out of 4289 recommendations with a median of 49.9 % in Class I, Class II and Class III were, 1825 recommendations with a median of 42.6 % and 324 recommendations with a median of 7.5 % respectively (Fig. 1).
Fig. 1.
Shows the distributions of COR across the total recommendations.The distribution of these recommendations across different classes of recommendations were; 2140 out of 4289 recommendations with a median of 49.9%, Class IIA, Class IIB and Class III were, 1230 recommendations with a median of 29%, 595 recommendations with a median of 14%, and 324 recommendations with a median of 7.5% respectively.
4.1. Level of evidence
The level of evidence behind the ESC guidelines is presented in Fig. 2, where level of evidence A was only present in 667 recommendations with a median of 15.5 % and 1285 recommendations in level of evidence B with a median of 30 %. While, level of evidence C was behind the majority of the recommendations including 2337 recommendations with a median of 54.5 % of total ESC recommendations.
Fig. 2.
Shows the distributions of loe across the total recommendations), where level of evidence A was only present in 667 recommendations with a median of 15.5% and 1285 recommendations in level of evidence B with a median of 30%. While, level of evidence C was behind the majority of the recommendations including 2337 recommendations with a median of 54.5% of total ESC recommendations.
Level of evidence C was found to be the main body of class II recommendations, 1133 out of 1825 recommendations with a median of 62 % of this class. Moreover, level of evidence C still composite 1028 recommendations with a median of 48 % and 176 recommendations with a median of 54 % of class I and class III recommendations respectively. Fig. 3 shows the detailed distribution of different levels of evidence across each class of recommendations.
Fig. 3.
Shows the distribution of LOE across each COR. This figure shows the detailed distribution of different levels of evidence across each class of recommendations.
Level of evidence A is more concentrated in class I recommendations with 520 out of total 667 recommendations with a median of 78 %, while class II and III nearly show the same share of level of evidence A with medians 13 % and 9 % respectively. Table 1 includes the brief the distribution of class of recommendations and level of evidence in all current topics of the ESC guidelines.
Table 1.
Distribution of level of evidence across different classes of recommendation in each topic.
| Year | Topic/ COR LOE | I A | I B | I C | IIa A | IIa B | IIa C | IIb A | IIb B | IIb C | III A | III B | III C | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2002 | Neonatal ECG[4] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2002 | Chest Pain[5] | 0 | 4 | 7 | 0 | 2 | 0 | 0 | 3 | 1 | 0 | 0 | 0 | 17 |
| 2003 | Separating Science from Economics[6] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2003 | The Score Project[7] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2004 | Beta blockers[8] | 25 | 12 | 8 | 2 | 4 | 11 | 1 | 0 | 2 | 0 | 0 | 0 | 65 |
| 2004 | ACEI[9] | 11 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 14 |
| 2004 | Antiplatelets[10] | 19 | 1 | 2 | 3 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 27 |
| 2007 | Endomyo. Biopsy[11] | 0 | 2 | 0 | 0 | 0 | 6 | 0 | 1 | 4 | 0 | 0 | 1 | 14 |
| 2010 | Device therapy[12] | 2 | 1 | 0 | 0 | 1 | 2 | 0 | 1 | 1 | 0 | 0 | 0 | 8 |
| 2014 | Aortic Disease[13] | 4 | 5 | 59 | 0 | 10 | 25 | 0 | 3 | 11 | 0 | 0 | 4 | 121 |
| 2014 | HCM[14] | 0 | 22 | 31 | 0 | 11 | 35 | 0 | 2 | 26 | 0 | 1 | 2 | 130 |
| 2015 | Infective endocarditis[15] | 1 | 22 | 12 | 0 | 7 | 16 | 0 | 0 | 10 | 0 | 0 | 8 | 76 |
| 2015 | Pericardial disease[16] | 5 | 15 | 52 | 1 | 9 | 28 | 0 | 3 | 9 | 0 | 1 | 10 | 133 |
| 2017 | STEMI[17] | 51 | 39 | 42 | 7 | 12 | 21 | 1 | 6 | 6 | 6 | 17 | 4 | 212 |
| 2017 | DAPT[18] | 18 | 12 | 6 | 1 | 11 | 7 | 3 | 6 | 7 | 2 | 6 | 1 | 80 |
| 2017 | PAD[19] | 26 | 20 | 60 | 3 | 18 | 19 | 1 | 14 | 9 | 6 | 4 | 10 | 190 |
| 2018 | CVD during pregnancy[20] | 2 | 8 | 71 | – | – | 44 | – | 2 | 9 | – | 1 | 12 | 149 |
| 2018 | Hypertension[21] | 41 | 18 | 28 | – | 14 | 7 | 1 | 5 | 8 | 7 | 2 | 4 | 135 |
| 2018 | Revascularization[22] | 40 | 30 | 40 | 8 | 30 | 36 | 8 | 15 | 15 | 4 | 7 | 5 | 238 |
| 2018 | Syncope[23] | 4 | 20 | 22 | – | 18 | 24 | – | 11 | 11 | 1 | 2 | 1 | 114 |
| 2019 | SVT[24] | 2 | 35 | 13 | – | 19 | 27 | – | 7 | 12 | – | 4 | 3 | 122 |
| 2019 | Pulmonary Embolism[25] | 9 | 12 | 9 | 4 | 13 | 14 | – | 2 | 4 | 3 | 2 | 4 | 76 |
| 2019 | Chronic Coronary Syndrome[26] | 37 | 21 | 29 | 4 | 16 | 8 | 1 | 16 | 9 | 3 | 2 | 12 | 158 |
| 2019 | Dyslipidemia[27] | 14 | 4 | 18 | 1 | 5 | 11 | 1 | 4 | 5 | 3 | – | 2 | 68 |
| 2019 | Diabetes[28] | 45 | 16 | 17 | 6 | 8 | 17 | 3 | 5 | 5 | 5 | 7 | 1 | 135 |
| 2020 | Atrial Fibrillation[29] | 16 | 29 | 12 | 2 | 26 | 15 | 1 | 6 | 8 | 4 | 3 | 3 | 125 |
| 2020 | Sports[30] | 12 | 16 | 25 | – | 3 | 41 | – | 1 | 33 | 1 | 3 | 26 | 161 |
| 2020 | NSTEMI[31] | 17 | 32 | 9 | 1 | 27 | 15 | 1 | 6 | 8 | 4 | 3 | 3 | 126 |
| 2020 | Adult Congenital heart disease[32] | 1 | 2 | 56 | 0 | 1 | 51 | 0 | 0 | 18 | 0 | 0 | 6 | 135 |
| 2021 | CVD Prevention[33] | 53 | 27 | 22 | 5 | 25 | 8 | 4 | 14 | 10 | 3 | 2 | 3 | 176 |
| 2021 | Cardiac Pacing & CRT[34] | 9 | 6 | 19 | 2 | 17 | 27 | 0 | 8 | 20 | 2 | 5 | 5 | 120 |
| 2021 | Valvular Heart Disease[35] | 3 | 22 | 30 | 1 | 18 | 27 | 0 | 3 | 11 | 0 | 2 | 2 | 119 |
| 2021 | Heart Failure[36] | 20 | 7 | 25 | 3 | 18 | 16 | 0 | 12 | 14 | 2 | 1 | 3 | 121 |
| 2022 | Cardio-oncology[37] | 5 | 32 | 118 | 2 | 22 | 51 | 0 | 2 | 34 | 0 | 0 | 5 | 271 |
| 2022 | Non-Cardiac Surgery[38] | 12 | 24 | 39 | 2 | 14 | 26 | 2 | 9 | 4 | 1 | 5 | 8 | 146 |
| 2022 | VT & SCD[39] | 10 | 51 | 79 | 1 | 29 | 87 | 0 | 13 | 37 | 1 | 3 | 16 | 327 |
| 2022 | Pulmonary Hypertension[40] | 6 | 24 | 68 | 0 | 9 | 28 | 0 | 5 | 21 | 1 | 6 | 12 | 180 |
| Total | 37 | 520 | 592 | 1028 | 60 | 419 | 751 | 28 | 185 | 382 | 59 | 89 | 176 | 4289 |
4.2. Variability in evidence across different topics
There was a wide variability among different topics regarding the distribution of the level of evidence as shown in Table 2. Level of evidence A was prominent in some topics like, cardiovascular disease (CVD) prevention in clinical practice contains 65 recommendations with LOE A, out of total 176 recommendations contributing to a median of 37 %. Diabetes, pre-diabetes, and cardiovascular diseases contains 59 recommendations with LOE A, out of total 135 recommendations and a median of 44 %. Moreover, B-Adrenergic Receptor Blockers, Angiotensin Converting Enzyme Inhibitors (ACEI) in cardiovascular disease, and Antiplatelet Agents have 28 out of 65, 12 out of 14 and 22 out of 27 recommendations with LOE A respectively. CVD prevention has only 24 % of its recommendations with LOE C and Diabetes has 29 %. B-blockers, ACEI and antiplatelets have 32 %, 7 % and 7 % of their recommendations with LOE C respectively. Accordingly, the recommendations within these topics have strong scientific evidence, with less invasion of scientific evidence “LOE C”.
Table 2.
Distribution of level of evidence in each topic.
| Topic | LOE A N (%) | LOE B N (%) | LOE C N (%) | Total |
|---|---|---|---|---|
| Chest pain [5] | 0 (0 %) | 9 (53 %) | 8 (47 %) | 17 |
| B-Blockers [8] | 28 (43 %) | 16 (25 %) | 21 (32 %) | 65 |
| ACEI [9] | 12 (86 %) | 1 (7 %) | 1 (7 %) | 14 |
| Antiplatelets [10] | 22 (81 %) | 3 (12 %) | 2 (7 %) | 27 |
| Endomyocardial biopsy [11] | 0 (0 %) | 3 (21 %) | 11 (79 %) | 14 |
| Device therapy [12] | 2 (25 %) | 3 (37.5 %) | 3(37.5 %) | 8 |
| Aortic disease [13] | 4 (3 %) | 18 (15 %) | 99 (82 %) | 121 |
| HCM [14] | 0 (0 %) | 36 (28 %) | 94 (72 %) | 130 |
| IE [15] | 1 (1 %) | 29 (38 %) | 46 (61 %) | 76 |
| Pericardial disease [16] | 6 (5 %) | 28 (21 %) | 99 (74 %) | 133 |
| STEMI [17] | 65 (31 %) | 74 (35 %) | 73 (34 %) | 212 |
| DAPT [18] | 24 (30 %) | 35 (44 %) | 21 (26 %) | 80 |
| PAD [19] | 36 (19 %) | 56 (29 %) | 98 (52 %) | 190 |
| CVD during pregnancy [20] | 2 (1.3 %) | 11 (7.4 %) | 136 (91.3 %) | 149 |
| Hypertension [21] | 49 (36.3 %) | 39 (28.9 %) | 47 (34.8 %) | 135 |
| Revascularization [22] | 60 (25.2 %) | 82 (34.5 %) | 96 (40.3 %) | 238 |
| Syncope [23] | 5 (4.4 %) | 51 (44.7 %) | 58 (50.9 %) | 114 |
| SVT [24] | 2 (1.6 %) | 65 (53.3 %) | 55 (45.1 %) | 122 |
| Pulmonary Embolism [25] | 16 (21 %) | 29 (38.2 %) | 31 (40.8 %) | 76 |
| Chronic Coronary Syndrome [26] | 45 (28.5 %) | 55 (34.8 %) | 58 (36.7 %) | 158 |
| Dyslipidemia [27] | 19 (27.9 %) | 13 (19.1 %) | 36 (53 %) | 68 |
| Diabetes [28] | 59 (43.7 %) | 36 (26.7 %) | 40 (29.6 %) | 135 |
| Atrial Fibrillation [29] | 23 (18.4 %) | 64 (51.2 %) | 38 (30.4 %) | 125 |
| Sports [30] | 13 (8.1 %) | 23 (14.3 %) | 125 (77.6 %) | 161 |
| NSTEMI [31] | 23 (18.3) | 68 (54 %) | 35 (27.7 %) | 126 |
| Adult Congenital heart disease [32] | 1 (0.7 %) | 3 (2.2 %) | 131 (97.1 %) | 135 |
| CVD Prevention [33] | 65 (36.9 %) | 68 (38.6 %) | 43 (24.5 %) | 176 |
| Cardiac Pacing & CRT [34] | 13 (10.8 %) | 36 (30 %) | 71 (59.2 %) | 120 |
| Valvular Heart Disease [35] | 4 (3.4 %) | 45 (37.8 %) | 70 (58.8 %) | 119 |
| Heart Failure [36] | 25 (20.7 %) | 38 (31.4 %) | 58 (47.9 %) | 121 |
| Cardio-oncology [37] | 7 (2.6 %) | 56 (20.7 %) | 208 (76.7 %) | 271 |
| Non-Cardiac Surgery [38] | 17 (11.6 %) | 52 (35.6 %) | 77 (52.8 %) | 146 |
| VT & SCD [39] | 12 (3.7 %) | 96 (29.4 %) | 219 (66.9 %) | 327 |
| Pulmonary Hypertension [40] | 7 (3.9 %) | 44 (24.4 %) | 129 (71.7 %) | 180 |
| Total | 667 (15.5 %) | 1285 (30 %) | 2337 (54.5 %) | 4289 |
On the other side, Management of Chest Pain, the Role of Endomyocardial Biopsy in the Management of Cardiovascular Disease, and Hypertrophic Cardiomyopathy have no recommendations with LOE A. Moreover, management of Grown-Up Congenital Heart Disease, cardiovascular diseases in pregnancy, infective endocarditis, aortic diseases, valvular heart diseases and syncope has very limited recommendations with LOE A with median of 0.7 %, 1 %, 1 %, 3 %, 3 % and 4 % respectively as shown in Table 2. These topics most of their recommendations has level of evidence C with median of 97 %, 91 %, 61 %, 82 %, 59 % and 51 % respectively.
5. Discussion
Many studies and surveys have concluded that ESC clinical guidelines are broadly followed in many countries. Maria G el al [41] has reported excellent adherence to the ESC guidelines for the management of heart failure in Spain, the same was found by Jonathan De Blois et al [42] in Norwegian Heart Failure Registry, and this was concordant with Michel Komajda et al [43] who found wide adherence to the ESC guidelines in pan Europe. Michel Komajda et al [43] added that this adherence has improved the patient outcomes by decreasing cardiovascular complications and percentage of rehospitalisation. These better outcomes are related to adherence to the best available evidence-based medicine recommendations, which assumed to be provided by the ESC clinical practice guidelines.
Although the ESC guidelines are supposed to have a solid scientific base but still 42.6 % of the whole recommendations are in Class II, this class reflects an area of uncertainty about the clinical benefit of those recommendations. Accordingly, the desired adherence of physicians to the guidelines may be in some situations an adherence to areas of uncertainty and in other situations may reach a degree of harm that has been reported in some studies. As long as there are many recommendations with a scientific background of uncertainty or expert opinions only, there will be differences between different organizations releasing clinical guidelines. Although all writers of guidelines within different organizations are highly selected, but still there are some cognitive biases as observed by Allen F. et al [44]. The bias if often not recognized by the individual leading to decisions with job conditioning, confirmation bias, Maslow’s hammer, or other changes which are affected by professional, financial, and conflicts of interest at intellectual level. These side effects are not confined to the ESC guidelines only but are related to other guidelines. Pierluigi Tricoci et al [2] have said in his systemic review regarding the AHA/ACC guidelines that increasing in class II recommendations could have some drawbacks that have been already reported. He said that in one report in United States 30 % of percutaneous coronary interventions (PCI) were done by a class II indication and another study reported that 39 % of invasive procedures done during the management of acute MI were class II recommendations. So, we need more studies examining the safety and effectiveness of adherence to the ESC clinical guidelines across different countries specially areas of uncertainty. Moreover, physicians should be trained on how to deal cautiously with these areas of uncertainty within the guidelines to avoid the bias of overuse or underuse.
5.1. Level of evidence
LOE C contributes to 54.5 % of the whole recommendations; this evidence is built on expert opinions, small studies, and registries. This means that more than half of the recommendations within the ESC guidelines have weak scientific evidence, these scientific areas need further studies and these recommendations with LOE C should be used properly. ESC clinical guidelines are important for guidance in clinical decision-making but still each patient should be managed according to his special condition with professionalism from highly qualified physicians. Thus, we agree with Jalal K et al [45] who said, “Guidelines are recognized for what they are, guidance for clinicians, not mandates”.
Moreover, Pierluigi Tricoci et al [2] has reported that the LOE C acquired 48 % of the AHA/ACC clinical guidelines which means that the same problem is reported in other organizations producing clinical guidelines but with different degrees, but this comparison is beyond the scope of our study. Accordingly, more care and more quality measures should be directed to expert opinions. This high percentage of recommendations with LOE C highlights that many topics in cardiovascular sciences are waiting more research work and are suffering from shortage of clinical trials.
5.2. Differences across different topics
It is clear that LOE C resembles more than half the recommendations in general, but this is not the situation in every topic solely. LOE shows wide variability across different topics, some topics have most of their recommendations to be in LOE C while on the other hand, some topics have obvious dominance of LOE A. Analysis of the level of evidence within each topic has a great importance to remark the areas that need to be in focus for researchers and need further clinical trials.
We found that topics like ACEI, Antiplatelets, Diabetes and CVD, B-Blockers, and CV prevention are the most topics rich in recommendations with LOE A with a median of 86 %, 81 %, 44 %, 43 %, and 37 % respectively. Accordingly, these topics have sufficient clinical trials more than other ESC guidelines topics. On the other hand, topics like hypertrophic cardiomyopathy, chest pain, grown up congenital heart diseases, and endomyocardial biopsy are topics showing almost complete absence of recommendations with LOE A. Furthermore, topics like CVD in pregnancy, Infective endocarditis, aortic diseases, supraventricular tachycardia and valvular heart disease have scientific presence of LOE A within their recommendations with a median of 1–3 % only. Analysis of these topics has highlighted that topics that are directly related to pharmaceutical medications are richer with clinical trials than other topics that are not directly related to special pharmaceutical product. This observation is prominent and clear in our study when comparing topics like ACEI, B-Blockers, Antiplatelets and diabetes versus hypertrophic cardiomyopathy, congenital heart diseases, CVD in pregnancy and endomyocardial biopsy. We assume that this is due to continuous support and sponsoring of the pharmaceutical companies to clinical trials that are directly related to their products, while other topics that will not affect their business do not gain that much of interest. This was in concordance with Andreas Lundh et al [46] who reported, “Clinical research is increasingly sponsored by companies that make these products, either because the companies directly perform the studies, or fully or partially fund them”.
Accordingly, researchers should give more attention to topics with the clinical trials that are not influenced by pharmaceutical company products. Our study has just highlighted the topics that are in need for more clinical trials but still more studies are needed to analyse in depth each topic within the guidelines to prioritize the areas that are in need for more trials and influence researchers to hit these virgin areas in cardiovascular sciences. Each ESC guideline contains a paragraph with the gaps of evidence.
6. Limitations
We did not study the change over time that occurs within the same topics, our study only included the latest version of every topic “current guidelines”. Accordingly, we cannot measure the progress of the scientific evidence background of the guidelines over time. We analysed only the ESC clinical guidelines and we did not offer a comparison between it and any other societies or organizations guidelines.
7. Conclusion
Although, ESC clinical practice guidelines are considered an important guidance for physicians in clinical decision-making, but still a big proportion of these guidelines are areas of uncertainty that need more studies. Quality of process and methods in guidelines development, especially in planning, conducting and interpreting systematic review results, may provide the most relevant and useful studies regarding the effectiveness of interventions recommended on the basis of low quality of evidence.
Furthermore, more than half of the recommendations are produced through expert opinions, small studies and registries that need training for physicians on how to deal with recommendations carrying this quality of scientific evidence. Deficiency in clinical trials is not the same across all guideline topics, some are more needy for clinical research while others seem satisfactory. The research community should prioritize these areas of deficiency and sponsor the areas with weak evidence especially those away from the pharmaceuticals interest. Finally, we are not against these important guidelines, but we just want to express their limitations to keep them in the area where they are supposed to be used; “For Guidance”.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2023.101175.
Contributor Information
Mahmoud Tantawy, Email: drmtantawy@yahoo.com.
Mohamed Marwan, Email: drm.marwan@gmail.com.
Sherif Hussien, Email: sherif334@gmail.com.
Ahmed Tamara, Email: ahmedtamara@gmail.com.
Sameh Mosaad, Email: samehcardio75@gmail.com.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ; et al. (2016). “2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC.”. Eur Heart J. 37 (27): 2129–200. PMID 27206819. doi:10.1093/eurheartj/ehw128. [DOI] [PubMed]
- 2.Pierluigi Tricoci, MD, MHS, PhD; Joseph M. Allen, MA; Judith M. Kramer, MD, MS. Scientific Evidence Underlying the ACC/AHA Clinical Practice Guidelines. JAMA. 2009;301(8):831-841. doi:10.1001/jama.2009.205. [DOI] [PubMed]
- 3.Fanaroff A.C., Califf R.M., Windecker S., Smith S.C., Lopes R.D. Levels of evidence supporting American College of Cardiology/American Heart Association and European Society of Cardiology Guidelines, 2008–2018. JAMA. 2019;321(11):1069–1080. doi: 10.1001/jama.2019.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwartz P.J., Garson A., Jr, Paul T., Stramba-Badiale M., Vetter V.L., Villain E., Wren C. Guidelines for the interpretation of the neonatal electrocardiogram. Eur. Heart J. 2002;23:1329–1344. doi: 10.1053/euhj.2002.3274. [DOI] [PubMed] [Google Scholar]
- 5.Erhardt L., Herlitz J., Bossaert L., Halinen M., Keltai M., Koster R., Marcassa C., Quinn T., van Weert H. Task force on the management of chest pain. Eur. Heart J. 2002;23:1153–1176. doi: 10.1053/euhj.2002.3194. [DOI] [PubMed] [Google Scholar]
- 6.Priori S.G., Klein W., Bassand J.-P. Medical Practice Guidelines Separating science from economics. Eur. Heart J. 2003;24:1962–1964. doi: 10.1016/s0195-668x(03)00438-x. [DOI] [PubMed] [Google Scholar]
- 7.R.M. Conroy, K. Py ¨or ¨al ¨a, A.P. Fitzgerald, S. Sans, A. Menotti, G. De Backer, D. De Bacquer, P. Ducimeti‘ere, P. Jousilahti, U. Keil, I. Njølstad, R.G. Oganov, T. Thomsen, H. Tunstall-Pedoe, A. Tverdal, H. Wedel, P. Whincup, L. Wilhelmsen, I.M. Graham, on behalf of the SCORE project group. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. European Heart Journal (2003) 24, 987–1003. [DOI] [PubMed]
- 8.Task Force Members, Jose Lo pez-Sendo n, Chairperson* (Spain), Karl Swedberg (Sweden), John McMurray (UK), Juan Tamargo (Spain), Aldo P. Maggioni (Italy), Henry Dargie (UK), Michal Tendera (Poland), Finn Waagstein (Sweden), Jan Kjekshus (Norway), Philippe Lechat (France), Christian Torp-Pedersen (Denmark). Expert consensus document on b-adrenergic receptor blockers. The Task Force on Beta-Blockers of the European Society of Cardiology. European Heart Journal (2004) 25, 1341–1362. [DOI] [PubMed]
- 9.Task Force Members, Jose Lo pez-Sendo n, Chairperson* (Spain), Karl Swedberg (Sweden), John McMurray (UK), Juan Tamargo (Spain), Aldo P. Maggioni (Italy), Henry Dargie (UK), Michal Tendera (Poland), Finn Waagstein (Sweden), Jan Kjekshus (Norway), Philippe Lechat (France), Christian Torp-Pedersen (Denmark). Expert consensus document on angiotensin converting enzyme inhibitors in cardiovascular disease. The Task Force on ACE-inhibitors of the European Society of Cardiology. European Heart Journal (2004) 25, 1454–1470. [DOI] [PubMed]
- 10.Carlo Patrono (Chairperson) (Italy), Fedor Bachmann (Switzerland), Colin Baigent (UK), Christopher Bode (Germany), Raffaele De Caterina (Italy), Bernard Charbonnier (France), Desmond Fitzgerald (Ireland), Jack Hirsh (Canada), Steen Husted (Denmark), Jan Kvasnicka (Czech Republic), Gilles Montalescot (France), Luis Alberto Garc ´ıa Rodr ´ıguez (Spain), Freek Verheugt (The Netherlands), Jozef Vermylen (Belgium), Lars Wallentin (Sweden). Expert Consensus Document on the Use of Antiplatelet Agents. The Task Force on the Use of Antiplatelet Agents in Patients with Atherosclerotic Cardiovascular Disease of the European Society of Cardiology. European Heart Journal (2004) 25, 166–181. [DOI] [PubMed]
- 11.Leslie T. Cooper, MD, FAHA, FACC; Kenneth L. Baughman, MD, FAHA, FACC; Arthur M. Feldman, MD, PhD, FAHA, FACC; Andrea Frustaci, MD; Mariell Jessup, MD, FAHA, FACC; Uwe Kuhl, MD; Glenn N. Levine, MD, FAHA, FACC; Jagat Narula, MD, PhD, FAHA; Randall C. Starling, MD, MPH; Jeffrey Towbin, MD, FAHA, FACC; and Renu Virmani, MD, FACC. The role of endomyocardial biopsy in the management of cardiovascular disease. European Heart Journal (2007) 28, 3076–3093 doi:10.1093/eurheartj/ehm456. [DOI] [PubMed]
- 12.Authors/Task Force Members, Kenneth Dickstein (Chairperson) (Norway)*, Panos E. Vardas (Chairperson) (Greece)*, Angelo Auricchio (Switzerland), Jean-Claude Daubert (France), Cecilia Linde (Sweden), John McMurray (UK), Piotr Ponikowski (Poland), Silvia Giuliana Priori (Italy), Richard Sutton (UK), Dirk J. van Veldhuisen (Netherlands). 2010 Focused Update of ESC Guidelines on device therapy in heart failure. European Heart Journal (2010) 31, 2677–2687 doi:10.1093/eurheartj/ehq337. [DOI] [PubMed]
- 13.Authors/Task Force members: Raimund Erbel* (Chairperson) (Germany), Victor Aboyans* (Chairperson) (France), Catherine Boileau (France), Eduardo Bossone (Italy), Roberto Di Bartolomeo (Italy), Holger Eggebrecht (Germany), Arturo Evangelista (Spain), Volkmar Falk (Switzerland), Herbert Frank (Austria), Oliver Gaemperli (Switzerland), Martin Grabenwo ¨ ger (Austria), Axel Haverich (Germany), Bernard Iung (France), Athanasios John Manolis (Greece), Folkert Meijboom (Netherlands), Christoph A. Nienaber (Germany), Marco Roffi (Switzerland), Herve ´ Rousseau (France), Udo Sechtem (Germany), Per Anton Sirnes (Norway), Regula S. von Allmen (Switzerland), Christiaan J.M. Vrints (Belgium). 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases. European Heart Journal (2014) 35, 2873–2926 doi:10.1093/eurheartj/ehu281.
- 14.Authors/Task Force members: Perry M. Elliott* (Chairperson) (UK) Aris Anastasakis (Greece), Michael A. Borger (Germany), Martin Borggrefe (Germany), Franco Cecchi (Italy), Philippe Charron (France), Albert Alain Hagege (France), Antoine Lafont (France), Giuseppe Limongelli (Italy), Heiko Mahrholdt (Germany), William J. McKenna (UK), Jens Mogensen (Denmark), Petros Nihoyannopoulos (UK), Stefano Nistri (Italy), Petronella G. Pieper (Netherlands), Burkert Pieske (Austria), Claudio Rapezzi (Italy), Frans H. Rutten (Netherlands), Christoph Tillmanns (Germany), Hugh Watkins (UK). 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy. European Heart Journal (2014) 35, 2733–2779 doi:10.1093/eurheartj/ehu284. [DOI] [PubMed]
- 15.Authors/Task Force Members: Gilbert Habib* (Chairperson) (France), Patrizio Lancellotti* (co-Chairperson) (Belgium), Manuel J. Antunes (Portugal), Maria Grazia Bongiorni (Italy), Jean-Paul Casalta (France), Francesco Del Zotti (Italy), Raluca Dulgheru (Belgium), Gebrine El Khoury (Belgium), Paola Anna Erbaa (Italy), Bernard Iung (France), Jose M. Mirob (Spain), Barbara J. Mulder (The Netherlands), Edyta Plonska-Gosciniak (Poland), Susanna Price (UK), Jolien Roos-Hesselink (The Netherlands), Ulrika Snygg-Martin (Sweden), Franck Thuny (France), Pilar Tornos Mas (Spain), Isidre Vilacosta (Spain), and Jose Luis Zamorano (Spain). 2015 ESC Guidelines for the management of infective endocarditis. European Heart Journal (2015) 36, 3075–3123 doi:10.1093/eurheartj/ehv319.
- 16.Authors/Task Force Members: Yehuda Adler* (Chairperson) (Israel), Philippe Charron* (Chairperson) (France), Massimo Imazio† (Italy), Luigi Badano (Italy), Gonzalo Baro ´ n-Esquivias (Spain), Jan Bogaert (Belgium), Antonio Brucato (Italy), Pascal Gueret (France), Karin Klingel (Germany), Christos Lionis (Greece), Bernhard Maisch (Germany), Bongani Mayosi (South Africa), Alain Pavie (France), Arsen D. Ristic ´ (Serbia), Manel Sabate ´ Tenas (Spain), Petar Seferovic (Serbia), Karl Swedberg (Sweden), and Witold Tomkowski (Poland). 2015 ESC Guidelines for the diagnosis and management of pericardial diseases. European Heart Journal (2015) 36, 2921–2964 doi:10.1093/eurheartj/ehv318.
- 17.Authors/Task Force Members: Borja Ibanez* (Chairperson) (Spain), Stefan James* (Chairperson) (Sweden), Stefan Agewall (Norway), Manuel J. Antunes (Portugal), Chiara Bucciarelli-Ducci (UK), He ´ctor Bueno (Spain), Alida L. P. Caforio (Italy), Filippo Crea (Italy), John A. Goudevenos (Greece), Sigrun Halvorsen (Norway), Gerhard Hindricks (Germany), Adnan Kastrati (Germany), Mattie J. Lenzen (The Netherlands), Eva Prescott (Denmark), Marco Roffi (Switzerland), Marco Valgimigli (Switzerland), Christoph Varenhorst (Sweden), Pascal Vranckx (Belgium), Petr Widimsky (Czech Republic). 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. European Heart Journal (2017) 00, 1–66 doi:10.1093/eurheartj/ehx393.
- 18.Authors/Task Force Members: Marco Valgimigli* (Chairperson) (Switzerland), He ´ ctor Bueno (Spain), Robert A. Byrne (Germany), Jean-Philippe Collet (France), Francesco Costa (Italy), Anders Jeppsson1 (Sweden), Peter Ju ¨ ni (Canada), Adnan Kastrati (Germany), Philippe Kolh (Belgium), Laura Mauri (USA), Gilles Montalescot (France), Franz-Josef Neumann (Germany), Mate Petricevic1 (Croatia), Marco Roffi (Switzerland), Philippe Gabriel Steg (France), Stephan Windecker (Switzerland), and Jose Luis Zamorano (Spain). 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. European Heart Journal (2017) 0, 1–48 doi:10.1093/eurheartj/ehx419.
- 19.Authors/Task Force Members: Victor Aboyans* (ESC Chairperson) (France), Jean-Baptiste Ricco*1 (Co-Chairperson) (France), Marie-Louise E. L. Bartelink (The Netherlands), Martin Bjo ¨ rck1 (Sweden), Marianne Brodmann (Austria), Tina Cohnert1 (Austria), Jean-Philippe Collet (France), Martin Czerny (Germany), Marco De Carlo (Italy), Sebastian Debus1 (Germany), Christine Espinola-Klein (Germany), Thomas Kahan (Sweden), Serge Kownator (France), Lucia Mazzolai (Switzerland), A. Ross Naylor1 (UK), Marco Roffi (Switzerland), Joachim Ro ¨ ther2 (Germany), Muriel Sprynger (Belgium), Michal Tendera (Poland), Gunnar Tepe (Germany), Maarit Venermo1 (Finland), Charalambos Vlachopoulos (Greece), Ileana Desormais (France). 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). European Heart Journal (2017) 00, 1–60 doi:10.1093/eurheartj/ehx095.
- 20.Regitz-Zagrosek V., Roos-Hesselink J.W., Bauersachs J., Blomström-Lundqvist C., Cífková R., De Bonis M., Iung B., Johnson M.R., Kintscher U., Kranke P., Lang I.M., Morais J., Pieper P.G., Presbitero P., Price S., Rosano G.M.C., Seeland U., Simoncini T., Swan L., Warnes C.A. ESC Scientific Document Group. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur. Heart J. 2018 Sep 7;39(34):3165–3241. doi: 10.1093/eurheartj/ehy340. PMID: 30165544. [DOI] [PubMed] [Google Scholar]
- 21.Williams B., Mancia G., Spiering W., Agabiti Rosei E., Azizi M., Burnier M., Clement D.L., Coca A., de Simone G., Dominiczak A., Kahan T., Mahfoud F., Redon J., Ruilope L., Zanchetti A., Kerins M., Kjeldsen S.E., Kreutz R., Laurent S., Lip G.Y.H., McManus R., Narkiewicz K., Ruschitzka F., Schmieder R.E., Shlyakhto E., Tsioufis C., Aboyans V., Desormais I. ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018 Sep 1;39(33):3021–3104. doi: 10.1093/eurheartj/ehy339. Erratum in: Eur Heart J. 2019 Feb 1;40(5):475. PMID: 30165516. [DOI] [PubMed] [Google Scholar]
- 22.Neumann F.J., Sousa-Uva M., Ahlsson A., Alfonso F., Banning A.P., Benedetto U., Byrne R.A., Collet J.P., Falk V., Head S.J., Jüni P., Kastrati A., Koller A., Kristensen S.D., Niebauer J., Richter D.J., Seferovic P.M., Sibbing D., Stefanini G.G., Windecker S., Yadav R., Zembala M.O. ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019 Jan 7;40(2):87–165. doi: 10.1093/eurheartj/ehy394. Erratum in: Eur Heart J. 2019 Oct 1;40(37):3096. PMID: 30165437. [DOI] [PubMed] [Google Scholar]
- 23.Brignole M., Moya A., de Lange F.J., Deharo J.C., Elliott P.M., Fanciulli A., Fedorowski A., Furlan R., Kenny R.A., Martín A., Probst V., Reed M.J., Rice C.P., Sutton R., Ungar A., van Dijk J.G. ESC Scientific Document Group. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur. Heart J. 2018 Jun 1;39(21):1883–1948. doi: 10.1093/eurheartj/ehy037. PMID: 29562304. [DOI] [PubMed] [Google Scholar]
- 24.Kuck KH, Phan HL, Tilz RR. Neue ESC-Leitlinien 2019 zur Behandlung von supraventrikulären Tachykardien [New ESC guidelines 2019 for the treatment of supraventricular tachycardia]. Herz. 2019 Dec;44(8):701-711. German. doi: 10.1007/s00059-019-04866-2. PMID: 31728553. [DOI] [PubMed]
- 25.Konstantinides S.V., Meyer G., Becattini C., Bueno H., Geersing G.J., Harjola V.P., Huisman M.V., Humbert M., Jennings C.S., Jiménez D., Kucher N., Lang I.M., Lankeit M., Lorusso R., Mazzolai L., Meneveau N., Ní Áinle F., Prandoni P., Pruszczyk P., Righini M., Torbicki A., Van Belle E., Zamorano J.L. ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS) Eur. Heart J. 2020 Jan 21;41(4):543–603. doi: 10.1093/eurheartj/ehz405. PMID: 31504429. [DOI] [PubMed] [Google Scholar]
- 26.Knuuti J., Wijns W., Saraste A., Capodanno D., Barbato E., Funck-Brentano C., Prescott E., Storey R.F., Deaton C., Cuisset T., Agewall S., Dickstein K., Edvardsen T., Escaned J., Gersh B.J., Svitil P., Gilard M., Hasdai D., Hatala R., Mahfoud F., Masip J., Muneretto C., Valgimigli M., Achenbach S., Bax J.J. ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020 Jan 14;41(3):407–477. doi: 10.1093/eurheartj/ehz425. Erratum in: Eur Heart J. 2020 Nov 21;41(44):4242. PMID: 31504439. [DOI] [PubMed] [Google Scholar]
- 27.Authors/Task Force Members; ESC Committee for Practice Guidelines (CPG); ESC National Cardiac Societies. 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Atherosclerosis. 2019 Nov;290:140-205. doi: 10.1016/j.atherosclerosis.2019.08.014. Epub 2019 Aug 31. Erratum in: Atherosclerosis. 2020 Jan;292:160-162. Erratum in: Atherosclerosis. 2020 Feb;294:80-82. PMID: 31591002.
- 28.Cosentino F., Grant P.J., Aboyans V., Bailey C.J., Ceriello A., Delgado V., Federici M., Filippatos G., Grobbee D.E., Hansen T.B., Huikuri H.V., Johansson I., Jüni P., Lettino M., Marx N., Mellbin L.G., Östgren C.J., Rocca B., Roffi M., Sattar N., Seferović P.M., Sousa-Uva M., Valensi P., Wheeler D.C. ESC Scientific Document Group. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2020 Jan 7;41(2):255–323. doi: 10.1093/eurheartj/ehz486. Erratum in: Eur Heart J. 2020 Dec 1;41(45):4317. PMID: 31497854. [DOI] [PubMed] [Google Scholar]
- 29.Hindricks G., Potpara T., Dagres N., Arbelo E., Bax J.J., Blomström-Lundqvist C., Boriani G., Castella M., Dan G.A., Dilaveris P.E., Fauchier L., Filippatos G., Kalman J.M., La Meir M., Lane D.A., Lebeau J.P., Lettino M., Lip G.Y.H., Pinto F.J., Thomas G.N., Valgimigli M., Van Gelder I.C., Van Putte B.P., Watkins C.L. ESC Scientific Document Group. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021 Feb 1;42(5):373–498. doi: 10.1093/eurheartj/ehaa612. Erratum in: Eur Heart J. 2021 Feb 1;42(5):507. Erratum in: Eur Heart J. 2021 Feb 1;42(5):546-547. Erratum in: Eur Heart J. 2021 Oct 21;42(40):4194. PMID: 32860505. [DOI] [PubMed] [Google Scholar]
- 30.Pelliccia A., Sharma S., Gati S., Bäck M., Börjesson M., Caselli S., Collet J.P., Corrado D., Drezner J.A., Halle M., Hansen D., Heidbuchel H., Myers J., Niebauer J., Papadakis M., Piepoli M.F., Prescott E., Roos-Hesselink J.W., Graham Stuart A., Taylor R.S., Thompson P.D., Tiberi M., Vanhees L., Wilhelm M. ESC Scientific Document Group. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur. Heart J. 2021 Jan 1;42(1):17–96. doi: 10.1093/eurheartj/ehaa605. Erratum in: Eur Heart J. 2021 Feb 1;42(5):548-549. PMID: 32860412. [DOI] [PubMed] [Google Scholar]
- 31.Collet J.P., Thiele H., Barbato E., Barthélémy O., Bauersachs J., Bhatt D.L., Dendale P., Dorobantu M., Edvardsen T., Folliguet T., Gale C.P., Gilard M., Jobs A., Jüni P., Lambrinou E., Lewis B.S., Mehilli J., Meliga E., Merkely B., Mueller C., Roffi M., Rutten F.H., Sibbing D., Siontis G.C.M. ESC Scientific Document Group. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021 Apr 7;42(14):1289–1367. doi: 10.1093/eurheartj/ehaa575. Erratum in: Eur Heart J. 2021 May 14;42(19):1908. Erratum in: Eur Heart J. 2021 May 14;42(19):1925. Erratum in: Eur Heart J. 2021 May 13;: PMID: 32860058. [DOI] [PubMed] [Google Scholar]
- 32.Baumgartner H., De Backer J., Babu-Narayan S.V., Budts W., Chessa M., Diller G.P., Lung B., Kluin J., Lang I.M., Meijboom F., Moons P., Mulder B.J.M., Oechslin E., Roos-Hesselink J.W., Schwerzmann M., Sondergaard L., Zeppenfeld K. ESC Scientific Document Group. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur. Heart J. 2021 Feb 11;42(6):563–645. doi: 10.1093/eurheartj/ehaa554. PMID: 32860028. [DOI] [PubMed] [Google Scholar]
- 33.Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, Benetos A, Biffi A, Boavida JM, Capodanno D, Cosyns B, Crawford C, Davos CH, Desormais I, Di Angelantonio E, Franco OH, Halvorsen S, Hobbs FDR, Hollander M, Jankowska EA, Michal M, Sacco S, Sattar N, Tokgozoglu L, Tonstad S, Tsioufis KP, van Dis I, van Gelder IC, Wanner C, Williams B; ESC National Cardiac Societies; ESC Scientific Document Group. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021 Sep 7;42(34):3227-3337. doi: 10.1093/eurheartj/ehab484. Erratum in: Eur Heart J. 2022 Nov 7;43(42):4468. PMID: 34458905.
- 34.Glikson M, Nielsen JC, Kronborg MB, Michowitz Y, Auricchio A, Barbash IM, Barrabés JA, Boriani G, Braunschweig F, Brignole M, Burri H, Coats AJS, Deharo JC, Delgado V, Diller GP, Israel CW, Keren A, Knops RE, Kotecha D, Leclercq C, Merkely B, Starck C, Thylén I, Tolosana JM; ESC Scientific Document Group. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 2021 Sep 14;42(35):3427-3520. doi: 10.1093/eurheartj/ehab364. Erratum in: Eur Heart J. 2022 May 1;43(17):1651. PMID: 34455430. [DOI] [PubMed]
- 35.Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, Capodanno D, Conradi L, De Bonis M, De Paulis R, Delgado V, Freemantle N, Gilard M, Haugaa KH, Jeppsson A, Jüni P, Pierard L, Prendergast BD, Sádaba JR, Tribouilloy C, Wojakowski W; ESC/EACTS Scientific Document Group. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632. doi: 10.1093/eurheartj/ehab395. Erratum in: Eur Heart J. 2022 Feb 18;: PMID: 34453165.
- 36.McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A; ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-3726. doi: 10.1093/eurheartj/ehab368. Erratum in: Eur Heart J. 2021 Oct 14;: PMID: 34447992.
- 37.Lyon AR, López-Fernández T, Couch LS, Asteggiano R, Aznar MC, Bergler-Klein J, Boriani G, Cardinale D, Cordoba R, Cosyns B, Cutter DJ, de Azambuja E, de Boer RA, Dent SF, Farmakis D, Gevaert SA, Gorog DA, Herrmann J, Lenihan D, Moslehi J, Moura B, Salinger SS, Stephens R, Suter TM, Szmit S, Tamargo J, Thavendiranathan P, Tocchetti CG, van der Meer P, van der Pal HJH; ESC Scientific Document Group, Lancellotti P, Thuny F, Abdelhamid M, Aboyans V, Aleman B, Alexandre J, Barac A, Borger MA, Casado-Arroyo R, Cautela J, Čelutkienė J, Cikes M, Cohen-Solal A, Dhiman K, Ederhy S, Edvardsen T, Fauchier L, Fradley M, Grapsa J, Halvorsen S, Heuser M, Humbert M, Jaarsma T, Kahan T, Konradi A, Koskinas KC, Kotecha D, Ky B, Landmesser U, Lewis BS, Linhart A, Lip GYH, Løchen ML, Malaczynska-Rajpold K, Metra M, Mindham R, Moonen M, Neilan TG, Nielsen JC, Petronio AS, Prescott E, Rakisheva A, Salem JE, Savarese G, Sitges M, Ten Berg J, Touyz RM, Tycinska A, Wilhelm M, Zamorano JL. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur Heart J. 2022 Nov 1;43(41):4229-4361. doi: 10.1093/eurheartj/ehac244. PMID: 36017568. [DOI] [PubMed]
- 38.Halvorsen S, Mehilli J, Cassese S, Hall TS, Abdelhamid M, Barbato E, De Hert S, de Laval I, Geisler T, Hinterbuchner L, Ibanez B, Lenarczyk R, Mansmann UR, McGreavy P, Mueller C, Muneretto C, Niessner A, Potpara TS, Ristić A, Sade LE, Schirmer H, Schüpke S, Sillesen H, Skulstad H, Torracca L, Tutarel O, Van Der Meer P, Wojakowski W, Zacharowski K; ESC Scientific Document Group, Knuuti J, Kristensen SD, Aboyans V, Ahrens I, Antoniou S, Asteggiano R, Atar D, Baumbach A, Baumgartner H, Böhm M, Borger MA, Bueno H, Čelutkienė J, Chieffo A, Cikes M, Darius H, Delgado V, Devereaux PJ, Duncker D, Falk V, Fauchier L, Habib G, Hasdai D, Huber K, Iung B, Jaarsma T, Konradi A, Koskinas KC, Kotecha D, Landmesser U, Lewis BS, Linhart A, Løchen ML, Maeng M, Manzo-Silberman S, Mindham R, Neubeck L, Nielsen JC, Petersen SE, Prescott E, Rakisheva A, Saraste A, Sibbing D, Siller-Matula J, Sitges M, Stankovic I, Storey RF, Ten Berg J, Thielmann M, Touyz RM. 2022 ESC Guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery. Eur Heart J. 2022 Oct 14;43(39):3826-3924. doi: 10.1093/eurheartj/ehac270. PMID: 36017553. [DOI] [PubMed]
- 39.Zeppenfeld K, Tfelt-Hansen J, de Riva M, Winkel BG, Behr ER, Blom NA, Charron P, Corrado D, Dagres N, de Chillou C, Eckardt L, Friede T, Haugaa KH, Hocini M, Lambiase PD, Marijon E, Merino JL, Peichl P, Priori SG, Reichlin T, Schulz-Menger J, Sticherling C, Tzeis S, Verstrael A, Volterrani M; ESC Scientific Document Group, Cikes M, Kirchhof P, Abdelhamid M, Aboyans V, Arbelo E, Arribas F, Asteggiano R, Basso C, Bauer A, Bertaglia E, Biering-Sørensen T, Blomström-Lundqvist C, Borger MA, Čelutkienė J, Cosyns B, Falk V, Fauchier L, Gorenek B, Halvorsen S, Hatala R, Heidbuchel H, Kaab S, Konradi A, Koskinas KC, Kotecha D, Landmesser U, Lewis BS, Linhart A, Løchen ML, Lund LH, Metzner A, Mindham R, Nielsen JC, Norekvål TM, Patten M, Prescott E, Rakisheva A, Remme CA, Roca-Luque I, Sarkozy A, Scherr D, Sitges M, Touyz RM, Van Mieghem N, Velagic V, Viskin S, Volders PGA. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2022 Oct 21;43(40):3997-4126. doi: 10.1093/eurheartj/ehac262. PMID: 36017572. [DOI] [PubMed]
- 40.Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, Carlsen J, Coats AJS, Escribano-Subias P, Ferrari P, Ferreira DS, Ghofrani HA, Giannakoulas G, Kiely DG, Mayer E, Meszaros G, Nagavci B, Olsson KM, Pepke-Zaba J, Quint JK, Rådegran G, Simonneau G, Sitbon O, Tonia T, Toshner M, Vachiery JL, Vonk Noordegraaf A, Delcroix M, Rosenkranz S; ESC/ERS Scientific Document Group. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022 Oct 11;43(38):3618-3731. doi: 10.1093/eurheartj/ehac237. PMID: 36017548.
- 41.María G. Crespo-Leiro, Javier Segovia-Cubero, José González-Costello, Antoni Bayes-Genis, Silvia López-Fernández, Eulàlia Roig, Marisa Sanz-Julve, Carla Fernández-Vivancos, Manuel de Mora-Martín, José Manuel García-Pinilla, Alfonso Varela-Román, Luis Almenar-Bonet, Antonio Lara-Padrón, Luis de la Fuente-Galán, Juan Delgado-Jiménez. Adherence to the ESC Heart Failure Treatment Guidelines in Spain: ESC Heart Failure Long-term Registry. Rev Esp Cardiol. 2015;68:785-93 - Vol. 68 Num.09 DOI: 10.1016/j.rec.2015.03.008. [DOI] [PubMed]
- 42.Jonathan De Blois Morten Wang Fagerland Morten Grundtvig Anne Grete Semb Lars Gullestad Arne Westheim Torstein Hole Dan Atar Stefan Agewall. ESC guidelines adherence is associated with improved survival in patients from the Norwegian Heart Failure Registry. European Heart Journal - Cardiovascular Pharmacotherapy, Volume 1, Issue 1, 1 January 2015, Pages 31–36, https://doi.org/10.1093/ehjcvp/pvu010. [DOI] [PubMed]
- 43.Michel Komajda Pablo Lapuerta Nancy Hermans José Ramon Gonzalez-Juanatey Dirk J. van Veldhuisen Erland Erdmann Luigi Tavazzi Philip Poole-Wilson Claude Le Pen. Adherence to guidelines is a predictor of outcome in chronic heart failure: the MAHLER survey. European Heart Journal, Volume 26, Issue 16, 1 August 2005, Pages 1653–1659, https://doi.org/10.1093/eurheartj/ehi251. [DOI] [PubMed]
- 44.Allen F. Shaughnessy, PharmD, MMedEd, Lisa Cosgrove, PhD, and Joel R. Lexchin, MD. The Need to Systematically Evaluate Clinical Practice Guidelines. J Am Board Fam Med 2016;29:644–648. [DOI] [PubMed]
- 45.Jalal K., Ghali M.D., Barry M., Massie M.D., Douglas L., Mann M.D., Michael W., Rich M.D. Guidelines are merely guidelines. J. Cardiac Fail. 2011;17(3):208–209. doi: 10.1016/j.cardfail.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 46.Lundh A., Sismondo S., Lexchin J., Busuioc O.A., Bero L. Industry sponsorship and research outcome. Cochrane Syst. Rev. - Methodology Version Published. 12 December 2012. doi: 10.1002/14651858.MR000033.pub2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.