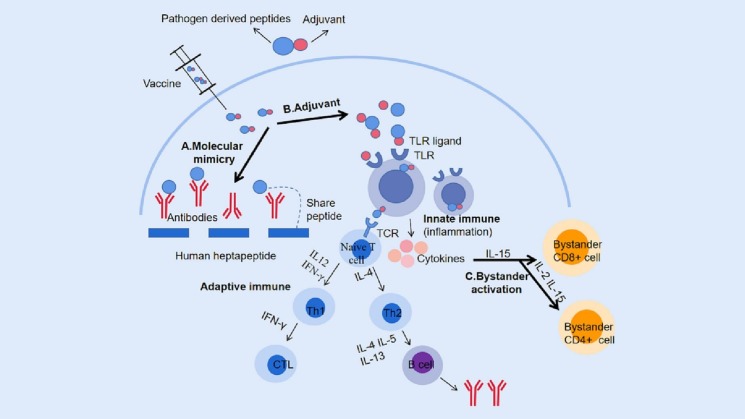
Fig. 1.
Schematic illustration of mechanisms inducing autoimmune diseases following COVID-19 vaccination. A. Following vaccination, vaccine antigens can trigger an immune response in the body. However, due to the presence of a heptapeptide that is shared between the SARS-CoV-2 spike glycoprotein and human proteins, vaccine antigens may also attack human proteins with similar structures via the molecular mimicry pathway. B. Adjuvants in vaccines can act as ligands for pattern recognition receptors (PRRs), such as toll-like receptors (TLR), bind to them to mobilize innate immune cells and secrete massive cytokines, and induce an innate immune response. Additionally, adjuvants also enhance the induction of adaptive immune responses to vaccine antigens. Upon binding to T-cell receptors (TCRs), antigens activate naive T-cells, which differentiate into Th1 or Th2 cells under the influence of different cytokines. Th1 cells primarily stimulate cellular responses, including the production of cytotoxic T lymphocytes (CTLs) that can eliminate infected cells, while Th2 cells promote humoral responses, such as B-cell proliferation, differentiation, and secretion of neutralizing antibodies. C. During the innate immune response following vaccination, the immune system produces a large number of cytokines, which may induce autoimmunity through the bystander activation pathway. This includes the activation of bystander CD8+T cells primarily under the action of IL-15 and the activation of CD4+T cells primarily under the influence of IL-2. PRRs, pattern recognition receptors; TLR, Toll-like receptor; TCR, T cell receptor; CTL, Cytotoxic T lymphocyte.