Abstract
There is a growing literature on the effects of cancer caregiving on the well-being of informal family caregivers. However, there has been little longitudinal research on caregivers of patients with the complex, rapidly-changing disease of primary malignant brain tumor.
Objective:
Our objective was to model longitudinal relationships between caregiver burden, social support, and distress within caregivers of patients with primary brain tumor.
Methods:
Caregiver participants were recruited from a neuro-oncology clinic. Caregiver questionnaire data, including sociodemographics, social support, depression, anxiety, and caregiving burden, were collected at 4 time points (diagnosis, +4, +8, and +12 mo). Using the stress process model as a guide, we hypothesized that early burden would predict later depression and anxiety, and this would be mediated by social support.
Results:
Using data from 147 participants, we found support for the stress process model in caregivers of patients with primary brain tumor. Greater burden at diagnosis was associated with lower social support at 4 months, and lower social support was related to higher depression and anxiety at 8 months, as well as to changes in anxiety between 8 and 12 months.
Conclusion:
We found evidence of the stress process model in caregivers of primary brain tumor patients unfolding over the course of a year after diagnosis. Our findings emphasize the potential importance of early programs for caregivers to ensure low initial levels of burden, which may have a positive effect on social support, depression, and anxiety.
Keywords: brain tumor, burden, caregiver, distress, longitudinal, oncology, social support
1 |. BACKGROUND
The negative impact of caregiving on health and well-being is increasingly recognized as an important public health issue, especially as the role of informal caregivers in the health care system expands. Patients and families often value and expect family involvement in cancer care, including involvement in decision making and clinical care tasks. However, care provision can be burdensome, especially when there is a high time commitment or when caregivers are responsible for assisting with a higher number of care activities.1
A great deal of research has been conducted on the effects of cancer caregiving burden on the health and well-being of informal family caregivers.2 Much of this research uses the stress process model, developed by Pearlin and colleagues,3 or other similar conceptual models in which the impacts of stress and burden on health and well-being are mediated by appraisal, coping, and/or social support.4 In line with these models, research has shown that a high degree of caregiver burden adversely affects caregiver quality of life and psychological and physical health.5–7 Caregivers who report lower levels perceived burden are more likely to report adequate support from social networks of friends, family, and other acquaintances8,9 and higher levels of well-being.10 However, most research using these models has been cross sectional. More recent model adaptations have been developed to account for longitudinal effects,2 but there is a need for more longitudinal research.
Further, a great deal of caregiver research has been conducted using relatively limited populations of cancer caregivers. One group of caregivers that has received very little attention in the research literature are those caring for patients with malignant primary brain tumor. While research on this population is growing, to date, most studies identified in a recent review are small (ie, median = 27), descriptive studies, often focused on describing caregiver unmet needs.10 These studies have shown that caregivers of patients with primary brain tumor are at particular risk of burden and distress.10–14 Primary brain tumor patients have a comparatively low 5-year survival rate (35% compared to 67% for all cancer sites).15 Primary brain tumor also presents a demanding set of challenges; in addition to significant physical debilitation, brain cancer can cause seizures, impaired judgment, and loss of emotional control and is often associated with cognitive decline as well as personality and behavior changes.12,16,17 Nevertheless, family caregivers may be hesitant to ask for support. Primary brain tumors often progress rapidly; thus, caregivers have little time for adjustment,16,17 leading to uncertainty about the extent and type of support needed.18 For caregivers of patients who require constant monitoring or specialized caregiver skills, such as those at risk for seizure, available support for caregivers may be perceived as inadequate.19 Meanwhile, the symptoms associated with primary brain tumor can compromise the existing relationship between patient and caregiver, removing the patient as a source of support.20
Adding to the complexity of the situation for caregivers of patients with primary brain tumor, burden, social support, and distress are not static. There may be a high perception of available helpful support at diagnosis that tapers off over time.21,22 This change in support may or may not track with a reduced level of need and burden as caregivers learn to navigate their new role, find new avenues for support, find benefit in the experience, or change their expectations.11,23–25 Changes in the caregiver experience may also occur over time; early support has been linked to lower later levels of depression26,27 and higher levels of later post-traumatic growth in breast cancer patients,28 while early depression can predict lowered later perceptions of support.26 Despite the obvious changes that occur in the stressor, resources, and coping, the focus on change over time is a more recent development and is not yet well reflected in all prominent models of caregiver stress. In particular, because of the rapid changes in primary brain tumor and the high demands on caregivers, there is a need to understand how caregiver distress unfolds prospectively over time and to understand when and how to target caregivers for intervention.10 Although the rapid changes in this population contribute to caregiver burden, it also provides a situation where we are able to capture the trajectory of cancer caregiving in a shortened amount of time. Understanding how the stress process works in this population may have implications for both more rapidly-progressing diseases and diseases where the progression and stress process may unfold more slowly.
The goal of the current analysis is to model the relationships between caregiver burden, social support, and distress within caregivers of patients with primary brain tumor across time. Our overall hypothesis is that, based on the stress process model, burden would predict distress (anxiety and depression) and that this relationship would be mediated by social support.
2 |. METHODS
Data were collected between 2005 and 2012 as part of a larger study (R01CA118711; PI Sherwood). All procedures were approved by the University of Pittsburgh IRB (IRB0704007). Patient-identified primary caregivers were recruited from a neuro-oncology clinic at a NCI-designated Comprehensive Cancer Center. Questionnaire data were collected from caregiver participants at 4 time points during telephone and face-to-face in-home interviews. Time 1 occurred at study enrollment, within 30 days of the patient receiving a diagnosis of a new primary malignant brain tumor. Subsequent questionnaire data were collected at 4, 8, and 12 months (+/−1 mo) after Time 1. Participants who skipped a time point were recontacted at the next time point unless they had formally withdrawn from the study. Caregivers were paid $75 when they completed each data collection session.
In addition to basic caregiver and patient sociodemographic variables collected at baseline, the following measures were assessed at each time point. Social support was measured using the Interpersonal Evaluation List.29 Participants rated the availability of 3 types of social support: appraisal (eg, availability of others to discuss problems), belonging (eg, availability of others to spend time with), and tangible (eg, availability of material aid). Individual items were summed to produce an overall score for each subscale, higher scores indicating more social support. Depressive symptoms were measured using the shortened CES-D.30 Participants indicated how often they experience various symptoms. Individual items were summed to produce an overall score, higher scores indicating higher levels of depressive symptoms. Anxiety was measured using the shortened anxiety subscale of the Profile of Mood States scale.31 Individual items were summed to produce a total score, with higher scores indicating higher levels of anxiety. Caregiver burden was measured via 3 subscales of the Caregiver Reaction Assessment: self-esteem (ie, value/reward of caregiving), schedule (ie, caregiving’s interruption of regular activities), and feelings of abandonment (ie, lack of family support).5 After reversing the self-esteem items, subscale scores were summed to create a total score, with greater caregiver burden indicated by higher scores.32
3 |. ANALYSES
Descriptive analysis was conducted on caregiver demographic information and primary variables of interest, caregiver burden, social support, anxiety, and depression. To model the relationships between caregiver burden, social support, and distress, we used Selig and Preacher’s mediation in latent difference score model approach.33 The advantages of these models are that they allow for information from each of the time points to be included in the analyses, as well as the parameterization of change from adjacent time points for the variables of interest. We conducted a sensitivity analysis by examining the relationships for persons with complete longitudinal data. The parameter estimates were within the 95% CI of those reported here; therefore, we report the model results using all available data.
As seen in Figure 1, our analysis allowed us to determine if burden at diagnosis or change in burden from diagnosis to 4 months predicted anxiety or depression at 8 months or the change in anxiety or depression between 8 and 12 months. We also modeled whether these relationships were mediated by social support at 4 months or change in social support between 4 and 8 months. Two models were tested; anxiety or depression were each used as the “distress” variable in Figure 1.
FIGURE 1.
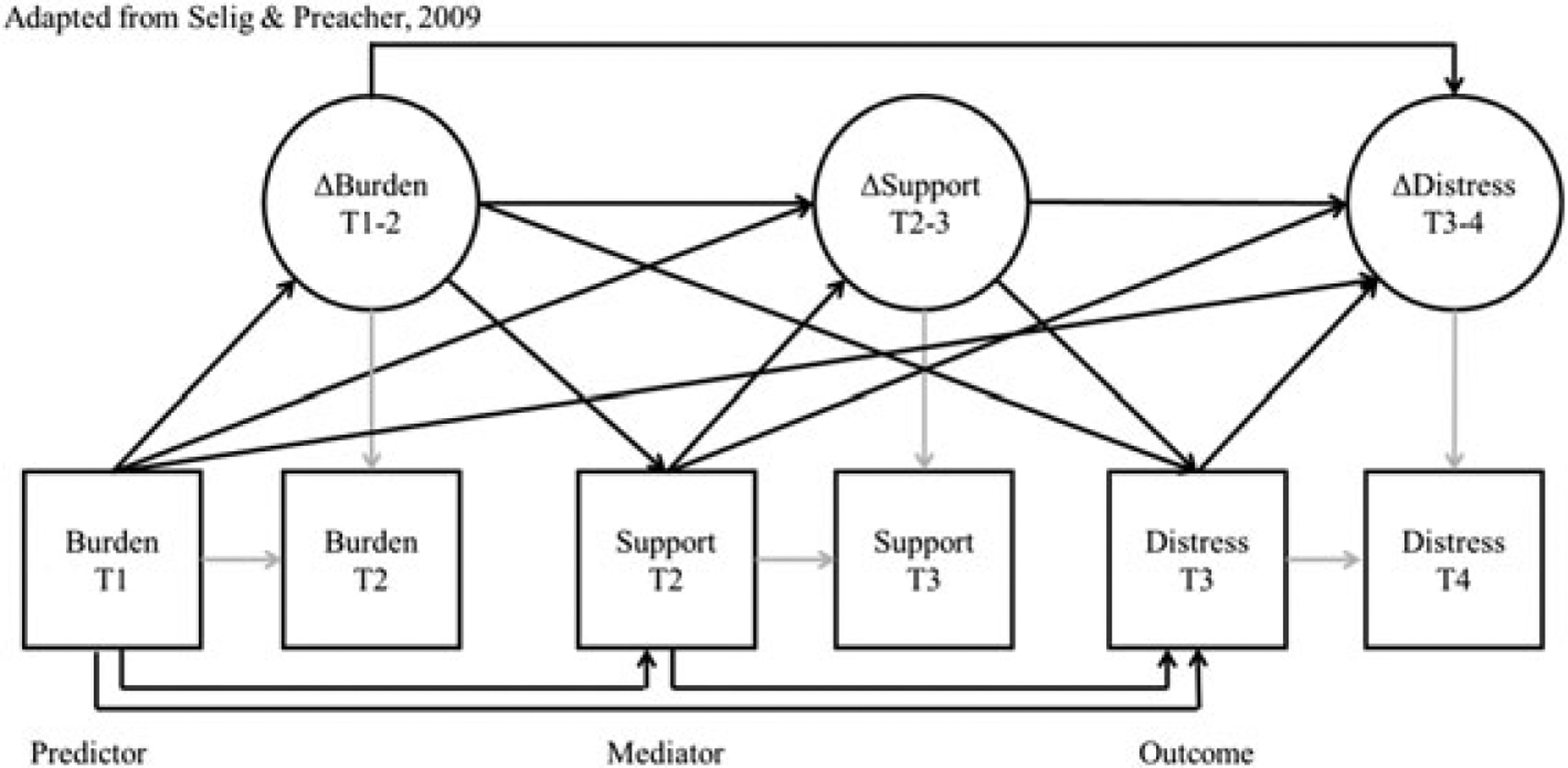
Model schematic
For caregiver burden, social support, and distress, the error variance was constrained to 0 as they were single indicator latent variables, based on scale total scores. MPlus software34 was used to conduct the analysis, which allowed us to use bootstrapping and estimate missing data using maximum likelihood.
4 |. RESULTS
Of 230 patients approached, 164 consented to participate (71%), and 147 caregivers provided at least some data. The number of participants providing at least some data for analysis at each time point is shown in Table 1 along with demographic information and descriptive data. The average caregiver age at baseline was 51.82 (SD = 11.61), 70% of caregivers were female, and 96% were Caucasian. Most care-givers were spouse/partners of the patient (n = 110), employed full-or part-time, privately insured (76.8%), and rated themselves as relatively healthy (94% rated at least “good” health). There was a wide range of education and annual household income, but most participants had completed some college and reported an income between $40,000 and $59,999.
TABLE 1.
Demographic information
| Variable | n, % | Variable | n, % |
|---|---|---|---|
| Ethnicity | Gender | ||
| Hispanic | 1 (0.6) | Male | 43 (29.3) |
| Non-Hispanic | 146 (99.3) | Female | 104 (70.7) |
| Race | Relationship to patient | ||
| White/Caucasian | 141 (95.9) | Spouse/partner | 110 (74.8) |
| Black/African American | 3 (2.0) | Parent | 13 (8.8) |
| American Indian | 1 (.7) | Child | 14 (9.5) |
| Asian | 2 (1.4) | Sibling | 2 (1.4) |
| Employment | Other family | 2 (1.4) | |
| Full time | 66 (44.9) | Friend | 6 (4.1) |
| Part time | 20 (13.6) | Education | |
| Unemployed | 15 (10.2) | Less than high school | 7 (4.8) |
| Retired | 18 (19.0) | High school graduate/GED | 36 (24.8) |
| Disabled/unable to work | 3 (2.0) | Some college | 48 (33.1) |
| Homemaker | 9 (6.1) | Bachelor’s degree | 28 (19.3) |
| Student | 1 (0.7) | At least some graduate education | 26 (17.9) |
| Other | 5 (3.4) | Annual household income | |
| Self-reported health | Less than $10,000 | 1 (0.7) | |
| Excellent | 19 (12.9) | $10,000–19,999 | 10 (6.8) |
| Very good | 72 (49.0) | $20,000–39,999 | 33 (22.8) |
| Good | 47 (32.0) | $40,000–59,999 | 54 (37.3) |
| Fair | 9 (6.1) | $50,000–79,999 | 10 (6.8) |
| Primary insurance | $80,000–99,999 | 25 (13.8) | |
| Private | 109 (76.8) | $100,000+ | 24 (16.6) |
| Medicaid | 2 (1.4) | Don’t know/refused | 6 (4.2) |
| Medicare | 13 (9.2) | Variable | M (SD) |
| Self pay | 6 (4.2) | Age | |
| Other (eg, TriCare) | 12 (8.4) | 51.82 (11.61) |
| Variable | T1 n = 147 M (SD) |
T2 n = 119 M (SD) |
T3 n = 102 M (SD) |
T4 n = 106 M (SD) |
|---|---|---|---|---|
| Total support | 34.74 (4.89) | 33.57 (5.55) | 33.81 (6.03) | 33.60 (5.67) |
| Depression | 10.01 (6.93) | 8.07 (6.08) | 7.37 (5.95) | 7.85 (5.95) |
| Anxiety | 9.07 (2.90) | 8.17 (2.67) | 7.94 (2.71) | 7.74 (2.74) |
| Burden | 30.56 (8.45) | 34.16 (9.78) | 33.15 (9.24) | 32.51 (9.45) |
The results from the mediation models for depression or anxiety as outcomes are shown in Table 2. As a guide to the table, the indirect effects indicate whether evidence exists for statistically significant mediation by social support. For caregiver depression as an outcome, only one indirect effect was statistically significant at P < .05; greater burden at diagnosis was associated with lower social support at 4 months, and this was related to increased depressive symptomatology at 8 months. Two trends (P < .10) were apparent in which changes in social support from 4 to 8 months were associated with burden from diagnosis and depression at 8 months, as well as changes in burden from diagnosis to 4 months being associated with social support from 4 months and depression from 8 months, but the indirect effect was not statistically significant. For caregiver anxiety as an outcome, greater burden at diagnosis was associated with lower social support at 4 months, and this was related to increased anxiety at 8 months, as well as less decline in anxiety between 8 and 12 months.
TABLE 2.
Mediation results
| Depression | a Path B (SE) |
b Path B (SE) |
Indirect Effect B (SE) |
|---|---|---|---|
| Burden T1→ Social Support T2→ Depression T3 | −.375 (.085)*** | −.607 (.165)*** | .228 (.079)** |
| Burden T1→ Social Support T2→ ΔDepressionT3–4 | −.375 (.085)*** | −.061 (.155) | .023 (.056) |
| Burden T1→ ΔSocial Support T2–3→ ΔDepressionT3–4 | −.227 (.093)* | −.025 (.190) | .006 (.047) |
| Burden T1→ ΔSocial Support T2–3→ Depression T3 | −.227 (.093)* | −.473 (.202)* | .108 (.063)τ |
| ΔBurdenT1–2→ ΔSocial Support T2–3→ ΔDepressionT3–4 | −.097 (.133) | −.025 (.190) | .002 (.034) |
| ΔBurdenT1–2→ ΔSocial Support T2–3→ Depression T3 | −.097 (.133) | −.473 (.202)* | .046 (.073) |
| ΔBurdenT1–2→ Social Support T2→ Depression T3 | −.234 (.118)* | −.607 (.165)*** | .142 (.078)τ |
| ΔBurdenT1–2→ Social Support T2→ ΔDepressionT3–4 | −.234 (.118)* | −.061 (.155) | .014 (.041) |
| Anxiety | |||
| Burden T1→ Social Support T2→ Anxiety T3 | −.372 (.084)*** | −.150 (.067)* | .056 (.027)* |
| Burden T1→ Social Support T2→ ΔAnxiety T3–4 | −.372 (.084)*** | −.114 (.050)* | .042 (.021)* |
| Burden T1→ ΔSocial Support T2–3→ ΔAnxiety T3–4 | −.225 (.095)* | −.104 (.080) | .023 (.022) |
| Burden T1→ ΔSocial Support T2–3→ Anxiety T3 | −.225 (.095)* | −.173 (.093)τ | .039 (.031) |
| ΔBurdenT1–2→ ΔSocial Support T2–3→ ΔAnxiety T3–4 | −.073 (.126) | −.104 (.080) | .008 (.017) |
| ΔBurdenT1–2→ ΔSocial Support T2–3→ Anxiety T3 | −.073 (.126) | −.173 (.093)τ | .013 (.027) |
| ΔBurden T1–2→ Social Support T2→ Anxiety T3 | −.228 (.114)* | −.150 (.067)* | .034 (.025) |
| ΔBurden T1–2→ Social Support T2→ ΔAnxiety T3–4 | −.228 (.114)* | −.114 (.050)* | .026 (.018) |
P < .10
P < .05
P < .01
P < .001
5 |. DISCUSSION
The goal of the current study was to assess the stress process model in caregivers of primary brain tumor patients across time. Our analysis found that social support at 4 months significantly mediated the relationship between caregiver burden at diagnosis and distress, conceptualized as anxiety and depression, at 8 months. These results are consistent with other studies suggesting that support may make a difference in the well-being of caregivers of primary brain tumor patients over and above levels of burden.12,13
While research using the stress process model typically uses cross-sectional analysis, our use of the mediation in latent difference score modeling allows for a more nuanced picture regarding change over time. Our findings support a model in which initial levels of burden at diagnosis are associated with later reduced social support and, finally, later increased distress. Interestingly, absolute values of burden and social support appear to be more important for distress than changes over time, which perhaps is protective for those whose burden increases or who lose support as the cancer progresses.
Although there is evidence that high levels of support can buffer the relationship between burden and distress,4,9 ensuring low levels of initial caregiver burden is perhaps the simplest way to address long-term distress. Caregivers with higher levels of burden at diagnosis were more likely to report lower levels of support after 4 months and higher levels of distress at 8 months. These findings support other research that suggests that social isolation and lack of support are major issues for caregivers of patients with primary brain tumor.13 This may be due to a sense of obligation as a caregiver to devote one’s time solely to the patient, and/or the reduction in or lack of perceived or available support from friends, family, or health care providers—potential resources that could reduce burden.13,35
5.1 |. Clinical implications
Neuro-oncology clinics should ensure that caregivers are referred to appropriate services, such as support groups or social work, in a timely manner after diagnosis. This is particularly true for high burden caregivers who may be on a trajectory for poor mental health outcomes. To prevent this reduction in support and ensuing high levels of distress, more formal programs are needed to help caregivers navigate changing patient care needs, financial and employment issues, and their own fears.13 Such programs have been recently developed to support caregivers from diagnosis through bereavement,36 but require investment and are not standard. Recent reviews of interventions for caregivers of patients with primary brain tumor suggest that while few rigorous trials exist, psychosocial interventions, such as in-person or online support groups or follow-up calls with health care providers, are desired and may improve caregiver quality of life.10,37 More broadly, interventions for cancer caregivers have been modestly effective; although most interventions focused primarily on education and skills training, elements of some interventions focus on caregiver psychosocial processes.38 Additionally, intervention research is more advanced in dementia caregiving populations. These literatures may provide a foundation for interventions tailored for caregivers of patients with primary brain tumor, although researchers will need to contend with documented challenges in participant burden, recruitment, and retention in this population.10,37
5.2 |. Limitations
While strengths of the current analysis include the unique population and longitudinal assessments, there are several limitations. First, given the relatively small sample and high number of variables, we did not have adequate statistical power to test differences between sociodemographic groups. Factors such as age or income have been linked to caregiver distress10,39 and should be explored as potential moderators to longitudinal caregiver processes in future research. Similarly, more detailed assessments could provide data into why caregivers reported less support, such as stigma, time burdens, or lack of perceived or actual support due to small networks, relocation, or fatigue from support networks. However, more generalized trajectory analysis suggests there may be specific groups who may show unique patterns.8,39 Second, while one strength of the study is its longitudinal nature, more frequent assessments could provide more information about inflection points in the caregiver experience. Finally, the current analysis did not assess patient variables, including their levels of support or distress. Other research has shown that patient and caregiver distress and quality of life are often interdependent.40 A limited number of interventions have targeted both patient and caregiver,37 but more research is needed on the dyadic nature of the stress process in primary brain tumor populations to determine how to address distress and quality of life within the system of patient and caregiver.
5.3 |. Conclusion
This study takes an important step in identifying gaps in current conceptual models to outline a more nuanced view of the experience of caregivers of patients with primary brain tumor. Understanding the trajectory of caregiver experience that can predict distress in this at-risk population is important to develop interventions to improve the caregiving experience for neuro-oncology and other caregivers. More prospective longitudinal research is needed to suggest specifically when to time these interventions. However, our research suggests that early intervention to ensure low caregiver burden at diagnosis may be most beneficial. Additionally, more research is needed to test longitudinal adaptations of established stress and coping theoretical models to determine what factors are important as stresses build and evolve. There are also clinical implications to these findings; more programs and resources need to be available for caregivers early on to protect against distress.
ACKNOWLEDGEMENTS
Research reported in this publication was supported by the American Cancer Society under award number ACS MRSG 13-234-01-PCSM (PI Reblin) and the National Cancer Institute of the National Institutes of Health under award number R01 CA118711 (PI Sherwood). The content is solely the responsibility of the authors and does not necessarily represent the official views of the American Cancer Society or the National Institutes of Health. The authors would like to thank the participants who make this research possible.
Funding information
National Cancer Institute, Grant/Award Number: R01 CA118711; American Cancer Society, Grant/Award Number: ACS MRSG 13-234-01-PCSM
REFERENCES
- 1.Family Caregiver Alliance. Caregiver Statistics: Demographics. San Francisco, CA: Family Caregiver Alliance; 2016. [Google Scholar]
- 2.Fletcher BS, Miaskowski C, Given B, Schumacher K. The cancer family caregiving experience: an updated and expanded conceptual model. Eur J Oncol Nurs. 2012;16(4):387–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30(5):583–594. [DOI] [PubMed] [Google Scholar]
- 4.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. [PubMed] [Google Scholar]
- 5.Given B, Given CW. Patient and family caregiver reaction to new and recurrent breast cancer. J Am Med Womens Assoc. 1992;47(5):201. [PubMed] [Google Scholar]
- 6.Kurtz ME, Given B, Kurtz JC, Given CW. The interaction of age, symptoms, and survival status on physical and mental health of patients with cancer and their families. Cancer. 1994;74(7 Suppl):2071–2078. [DOI] [PubMed] [Google Scholar]
- 7.Robison J, Fortinsky R, Kleppinger A, Shugrue N, Porter M. A broader view of family caregiving: effects of caregiving and caregiver conditions on depressive symptoms, health, work, and social isolation. J Gerontol B Psychol Sci Soc Sci. 2009;64(6):788–798. [DOI] [PubMed] [Google Scholar]
- 8.Newberry A, Kuo J, Donovan H, et al. Identifying family members who are likely to perceive benefits from providing care to a person with a primary malignant brain tumor. Oncol Nurs Forum. 2012;39(3):E226–E232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teixeira RJ, Pereira MG. Psychological morbidity, burden, and the mediating effect of social support in adult children caregivers of oncological patients undergoing chemotherapy. Psychooncology. 2013;22(7):1587–1593. [DOI] [PubMed] [Google Scholar]
- 10.Sherwood PR, Cwiklik M, Donovan HS. Neuro-oncology family caregiving: review and directions for future research. CNS Oncol. 2016;5(1):41–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sherwood PR, Given BA, Doorenbos AZ, Given CW. Forgotten voices: lessons from bereaved caregivers of persons with a brain tumour. Int J Palliat Nurs. 2004;10(2):67–75. discussion 75 [DOI] [PubMed] [Google Scholar]
- 12.Sherwood PR, Given BA, Given CW, et al. Predictors of distress in care-givers of persons with a primary malignant brain tumor. Res Nurs Health. 2006;29(2):105–120. [DOI] [PubMed] [Google Scholar]
- 13.Applebaum AJ, Kryza-Lacombe M, Buthorn J, DeRosa A, Corner G, Diamond EL. Existential distress among caregivers of patients with brain tumors: a review of the literature. Neurooncol Pract. 2016;3(4):232–244. 10.1093/nop/npv060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sherwood PR, Given BA, Donovan H, et al. Guiding research in family care: a new approach to oncology caregiving. Psychooncology. 2008;17(10):986–996. [DOI] [PubMed] [Google Scholar]
- 15.Howlader N, Noone A, Krapcho M, et al. SEER cancer statistics review (CSR) 1975–2011. Bethesda, MD: National Cancer Institute; September 10, 2014. 2014. [Google Scholar]
- 16.Schmer C, Ward-Smith P, Latham S, Salacz M. When a family member has a malignant brain tumor: the caregiver perspective. J Neurosci Nurs. 2008;40(2):78–84. [DOI] [PubMed] [Google Scholar]
- 17.Schubart JR, Kinzie MB, Farace E. Caring for the brain tumor patient: family caregiver burden and unmet needs. Neuro Oncol. 2008;10(1):61–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Skeels MM, Unruh KT, Powell C, Pratt W. Catalyzing social support for breast cancer patients. CHI conference proceedings/Conference on Human Factors in Computing Systems CHI Conference. 2010:173–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McConigley R, Halkett G, Lobb E, Nowak A. Caring for someone with high-grade glioma: a time of rapid change for caregivers. Palliat Med. 2010;24(5):473–479. [DOI] [PubMed] [Google Scholar]
- 20.Gaugler JE, Hanna N, Linder J, et al. Cancer caregiving and subjective stress: a multi-site, multi-dimensional analysis. Psychooncology. 2005;14(9):771–785. [DOI] [PubMed] [Google Scholar]
- 21.Courtens AM, Stevens FCJ,Crebolder HFJM, Philipsen H. Longitudinal study on quality of life and social support in cancer patients. Cancer Nurs. 1996;19(3):162–169. [DOI] [PubMed] [Google Scholar]
- 22.Arora NK, Finney Rutten LJ, Gustafson DH, Moser R, Hawkins RP. Perceived helpfulness and impact of social support provided by family, friends, and health care providers to women newly diagnosed with breast cancer. Psychooncology. 2007;16(5):474–486. [DOI] [PubMed] [Google Scholar]
- 23.Ownsworth T, Goadby E, Chambers SK. Support after brain tumor means different things: family caregivers’ experiences of support and relationship changes. Front Oncol. 2015;5:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hricik A, Donovan H, Bradley SE, et al. Changes in caregiver perceptions over time in response to providing care for a loved one with a primary malignant brain tumor. Oncol Nurs Forum. 2011;38(2):149–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cornwell P, Dicks B, Fleming J, Haines TP, Olson S. Care and support needs of patients and carers early post-discharge following treatment for non-malignant brain tumour: establishing a new reality. Support Care Cancer. 2012;20(10):2595–2610. [DOI] [PubMed] [Google Scholar]
- 26.Talley A, Molix L, Schlegel RJ, Bettencourt A. The influence of breast cancer survivors’ Perceived partner social support and need satisfaction on depressive symptoms: a longitudinal analysis. Psychol Health. 2010;25(4):433–449. [DOI] [PubMed] [Google Scholar]
- 27.Hughes S, Jaremka LM, Alfano CM, et al. Social support predicts inflammation, pain, and depressive symptoms: longitudinal relationships among breast cancer survivors. Psychoneuroendocrinology. 2014;42:38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scrignaro M, Barni S, Magrin ME. The combined contribution of social support and coping strategies in predicting post-traumatic growth: a longitudinal study on cancer patients. Psychooncology. 2011;20(8):823–831. [DOI] [PubMed] [Google Scholar]
- 29.Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Measuring the functional components of social support. In: Sarason IG, Sarason BR, eds. Social Support: Theory Research and Applications. Boston, MA: NATO Scientific Affairs; 1985:73–94. [Google Scholar]
- 30.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Measur. 1977;1(3):385–401. [Google Scholar]
- 31.Usala PD, Hertzog C. Measurement of affective states in adults: evaluation of an adjective rating scale instrument. Res Aging. 1989;11(4):403–426. [DOI] [PubMed] [Google Scholar]
- 32.Grov EK. Anxiety, depression, and quality of life in caregivers of patients with cancer in late palliative phase. Ann Oncol. 2005;16(7):1185–1191. [DOI] [PubMed] [Google Scholar]
- 33.Selig JP, Preacher KJ. Mediation models for longitudinal data in developmental research. Res Hum Dev. 2009;6(2–3):144–164. [Google Scholar]
- 34.Muthen B, Muthen L. Mplus users guide (v. 7.4). Los Angeles, CA: 2016. [Google Scholar]
- 35.Seal K, Murray CD, Seddon L. The experience of being an informal “carer” for a person with cancer: a meta-synthesis of qualitative studies. Palliat Support Care. 2015;13(3):493–504. [DOI] [PubMed] [Google Scholar]
- 36.Page MS, Chang SM. Creating a caregiver program in neuro-oncology. Neuro-Oncology Practice. 2016;116–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Piil K, Juhler M, Jakobsen J, Jarden M. Controlled rehabilitative and supportive care intervention trials in patients with high-grade gliomas and their caregivers: a systematic review. BMJ Support Palliat Care. 2016;6(1):27–34. 10.1136/bmjspcare-2013-000593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Northouse LL, Katapodi M, Song L, Zhang L, Mood DW. Interventions with family caregivers of cancer patients: meta-analysis of randomized trials. CA Cancer J Clin. 2010;60(5):317–339. 10.3322/caac.20081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Choi CW, Stone RA, Kim KH, et al. Group-based trajectory modeling of caregiver psychological distress over time. Ann Behav Med. 2012;44(1):73–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Milbury K, Badr H, Fossella F, Pisters KM, Carmack CL. Longitudinal associations between caregiver burden and patient and spouse distress in couples coping with lung cancer. Support Care Cancer. 2013;2371–2379. [DOI] [PMC free article] [PubMed] [Google Scholar]


