Abstract
Background
Heart failure is a public health issue worldwide. However, no comprehensive study on the global burden of heart failure and its contributing causes has been reported. The present study aimed to quantify the burden, trends, and inequalities of heart failure globally.
Methods and Results
Heart failure data were extracted from the Global Burden of Diseases 2019 study. The number of cases, age‐standardized prevalence, and years lived with disability in different locations from 1990 to 2019 were presented and compared. Joinpoint regression analysis was performed to assess trends in heart failure from 1990 to 2019.
In 2019, the global age‐standardized prevalence and years lived with disability rates for heart failure were 711.90 (95% uncertainty interval [UI], 591.15–858.29) and 63.92 (95% UI, 41.49–91.95) per 100 000 population, respectively. In general, the age‐standardized rate decreased globally at an average annual percentage change of 0.3% (95% UI, 0.2–0.3). However, the rate increased at an average annual percentage change of 0.6% (95% UI, 0.4–0.8) from 2017 to 2019. Several nations and territories demonstrated an increased trend from 1990 to 2019, especially in less‐developed countries. Ischemic heart disease and hypertensive heart disease accounted for the highest proportion of heart failure in 2019.
Conclusions
Heart failure remains a major health problem, with increased trends possible in the future. Efforts for prevention and control of heart failure should focus more on less‐developed regions. It is essential to prevent and treat primary diseases such as ischemic heart disease and hypertensive heart disease for the control of heart failure.
Keywords: epidemiology, Global Burden of Diseases, heart failure, prevalence
Subject Categories: Heart Failure
Nonstandard Abbreviations and Acronyms
- AAPC
average annual percentage change
- GBD
Global Burden of Diseases, Injuries, and Risk Factors Study
- SDI
Sociodemographic Index
- UI
uncertainty interval
- YLDs
years lived with disability
Clinical Perspective.
What Is New?
The present study is the first to comprehensively analyze the global burden of heart failure and its contributing causes.
What Are the Clinical Implications?
Heart failure remains a major health problem with a possible increased trend in the future.
It is essential to prevent and treat primary diseases such as ischemic heart disease and hypertensive heart disease for the control of heart failure.
Heart failure (HF), a complex syndrome consisting of cardinal symptoms accompanied by multiple signs and comorbidities, 1 remains a major clinical and public health problem affecting approximately 1% to 2% of adults. 2 , 3 , 4 Because of the aging population, the prevalence of HF tends to increase, 5 reducing the quality of life of patients 6 and increasing the economic burden for both individuals and public health. 7 Estimating the global burden and temporal trends of HF are essential to guide the clinical decision making and improve the prognosis of patients with HF.
The GBD (Global Burden of Diseases, Injuries, and Risk Factors Study) project is a systematic analysis to compare the magnitude of health loss attributable to diseases, injuries, and risk factors by age, sex, and geography for specific points in time. 8 The GBD 2019 study 9 is the newest update of the GBD 2017 study, 10 comprising newly available data sets that enhance method performance and standardization. In the GBD 2019 study, the prevalence and years lived with disability (YLDs) of HF globally is estimated, including 369 diseases and injuries in 204 countries and territories and 21 GBD regions from 1990 to 2019.
Although some previous studies have described the epidemiology of HF, 3 , 11 , 12 , 13 those studies were mostly limited to cohorts in 1 country or region. No comprehensive study on the global burden of HF and its contributing causes was reported. In the present study, we extracted the HF data from the GBD 2019 study and performed a secondary analysis to quantify the burden, trends, and inequalities of HF by location, age, and sex, and to explore the underlying causes of HF.
METHODS
Data Source
We extracted data from the GBD 2019 and performed a secondary analysis of the GBD 2019 in the present study. 9 The GBD 2019 synthesizes a large and growing number of data input sources including surveys, censuses, vital statistics, and other health‐related data sources. The GBD 2019 collaborators explore and provide a systematic scientific estimate of incidence, prevalence, and burden of diseases and injuries globally, including 369 diseases and injuries in 204 countries and territories and 21 GBD regions from 1990 to 2019. 9 All data are available using the GBD results tool (https://ghdx.healthdata.org/gbd‐results‐tool). The institutional review board approval and patient informed consent are waived because the present study is a secondary analysis of published data that can be acquired in the public database.
Definition of HF
The GBD 2019 extended the definition of HF in GBD 2017. 10 HF was diagnosed clinically using the Framingham or European Society of Cardiology criteria, which can be found in a previous study. 10 Briefly, Framingham criteria require patients with HF to fulfill 2 major criteria or 1 major criterion and 2 minor criteria. According to European Society of Cardiology criteria, typical signs and symptoms caused by structural and/or functional cardiac abnormality are necessary. 14 HF was divided into 4 subgroups of varying severity based on clinical symptoms, including treated, mild, moderate, and severe HF.
Data Processing and Modeling
In the GBD 2019, heart failure estimation was modeled using spatiotemporal Gaussian process regression and DisMod–MR. 9 Briefly, spatiotemporal Gaussian process regression is a set of regression methods that allow for smoothing over age, time, and locations. The approach serves as a powerful tool for interpolating nonlinear trends. Unlike classical linear models, spatiotemporal Gaussian process regression assumes that the specific trend of interest follows a Gaussian process, which is defined by a mean function and a covariance function. Random draws of 1000 samples were obtained from the distributions above for every country for a given indicator. The final estimated mean for each country was the mean of the draws. DisMod–MR is a Bayesian metaregression method to evaluate all available data. A Gaussian, log‐Gaussian, Laplace, or log‐Laplace likelihood function was used in the DisMod–MR 2.1. For a given location, country coefficients are calculated by using both data and prior information available for that location. The default value of the minimum coefficient of variation is set as 0.8 to improve coverage and reduce errors based on simulation testing. The process of HF estimation begins with the compilation of data sources from a diverse set of possible sources, which include Global Health Data Exchange data types ranging from scientific literature to survey data to hospital and clinical data. The GBD collaborator network provided data sources for the GBD 2019 study. Overall prevalence of heart failure was estimated in DisMod–MR 2.1 using literature data, hospital data, and claims data. YLDs were estimated as the product of prevalence estimate and a disability weight of HF. Age and sex standardization were performed based on the GBD reference population. More detailed methods can be found in the previous studies. 8 , 9 , 10
Sociodemographic Index
The Sociodemographic Index (SDI) is constructed using Human Development Index methodology, which is an indicator of social and economic conditions that influence health outcomes in each location. In the GBD 2019, SDI comprised the total fertility rates for those <25 years old, mean education for those ≥15 years old, and lag‐distributed income per capita. Values of calculated SDI are multiplied by 100 to report for a scale of 0 to 100 to improve understanding of and broader engagement with the values. Countries with populations <1 million are excluded. According to different SDI levels, all locations are divided into 5 regions, called low SDI, low‐middle SDI, middle SDI, high‐middle SDI, and high SDI. 9
Joinpoint Regression Model
Joinpoint regression analysis was performed to assess trends in HF from 1990 to 2019 using Joinpoint software (version 4.9.0.1, https://surveillance.cancer.gov/joinpoint/). The average annual percentage change (AAPC) represents the weighted average of annual percentage change from the Joinpoint regression analysis. The Monte Carlo permutation test, with 4499 randomly permuted data sets, was used to calculate the AAPCs and their 95% CIs for prevalence attributable to HF. AAPCs are considered significantly different from 0 at the α=0.05 level. If 0 is within the 95% CIs, AAPCs are considered a constant trend. If both limits of the 95% CIs are positive or negative, AAPCs are increasing or decreasing trends.
Statistical Analysis
To characterize the global, regional, national, and territorial burden of HF, a descriptive analysis was performed. The number of cases, age‐standardized prevalence (per 100 000 population), and age‐standardized YLDs (per 100 000 population) in different locations from 1990 to 2019 were compared. Because HF was not considered an underlying cause of some deaths in the GBD 2019, years of life lost could not be calculated. Uncertainty was calculated by sampling 1000 draws, and the uncertainty intervals (UIs) were defined as the 25th and 975th values of the 1000 ordered draws.
RESULTS
Global Level
There were 56.19 million (95% UI, 46.45–67.79) prevalent cases of HF around the world, with an age‐standardized rate (ASR) of 711.90 per 100 000 population (95% UI, 591.15–858.29), which is 7.06% lower than that in 1990 (765.99 per 100 000 population [95% UI, 626.29–936.03]) (Figure 1 and Table 1). In general, from 1990 to 2019, ASRs decreased globally at an AAPC of 0.3% (95% UI, 0.2–0.3). However, ASR prevalence of HF increased at an annual percentage change of 0.6% (95% UI, 0.4–0.8) from 2017 to 2019 (Figure 2). In 2019, HF resulted in 5.05 million (95% UI, 3.28–7.26) YLDs across the world, with an ASR of 63.92 per 100 000 population (95% UI, 41.49–91.95), which is 6.83% lower than that in 1990 (68.60 per 100 000 population [95% UI, 44.34–98.68]) (Figure 3 and Table 2).
Figure 1. Global age‐standardized point prevalence rate of heart failure per 100 000 population in 2019.
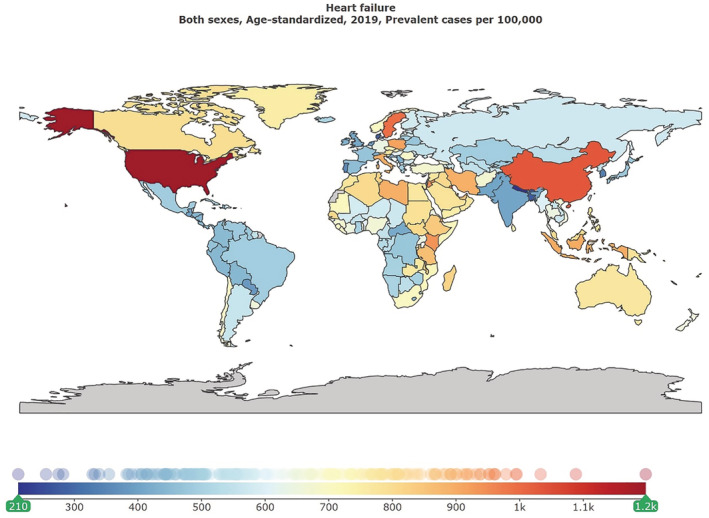
Visualization using the Global Burden of Diseases compare tool (https://www.healthdata.org/data‐visualization/gbd‐compare).
Table 1.
Prevalent Cases and ASRs of Prevalence per 100 000 Population for Heart Failure in 1990 and 2019 Globally and in 21 Global Burden of Diseases Regions
| Regions | 1990, millions | 2019, millions | 1990 | 2019 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | 95% UI | No. | 95% UI | ASRs per 100 000 | 95% UI | ASRs per 100 000 | 95% UI | |||||
| Lower | Upper | Lower | Upper | Lower | Upper | Lower | Upper | |||||
| Global | 27.24 | 22.17 | 33.36 | 56.19 | 46.45 | 67.79 | 765.99 | 626.29 | 936.03 | 711.90 | 591.15 | 858.29 |
| Andean Latin America | 0.09 | 0.07 | 0.11 | 0.25 | 0.19 | 0.31 | 461.95 | 371.11 | 578.14 | 453.01 | 355.22 | 575.83 |
| Australasia | 0.27 | 0.21 | 0.33 | 0.39 | 0.31 | 0.47 | 1161.07 | 929.14 | 1404.29 | 750.24 | 603.56 | 904.89 |
| Caribbean | 0.13 | 0.10 | 0.17 | 0.27 | 0.21 | 0.35 | 542.61 | 424.44 | 694.40 | 521.68 | 405.62 | 672.18 |
| Central Asia | 0.24 | 0.19 | 0.31 | 0.33 | 0.26 | 0.41 | 582.38 | 453.44 | 748.24 | 544.18 | 425.82 | 697.68 |
| Central Europe | 1.07 | 0.84 | 1.34 | 1.59 | 1.32 | 1.91 | 789.04 | 628.59 | 983.55 | 719.85 | 607.69 | 855.24 |
| Central Latin America | 0.41 | 0.33 | 0.50 | 1.07 | 0.86 | 1.33 | 531.55 | 425.65 | 660.74 | 471.07 | 375.38 | 589.79 |
| Central sub‐Saharan Africa | 0.09 | 0.07 | 0.12 | 0.21 | 0.16 | 0.28 | 499.26 | 368.39 | 658.74 | 482.70 | 356.27 | 639.34 |
| East Asia | 7.20 | 5.83 | 9.02 | 18.91 | 15.31 | 23.50 | 1060.30 | 863.37 | 1310.49 | 1014.06 | 830.18 | 1252.95 |
| Eastern Europe | 1.44 | 1.15 | 1.80 | 1.93 | 1.55 | 2.38 | 561.57 | 450.36 | 689.28 | 560.22 | 451.07 | 685.57 |
| Eastern sub‐Saharan Africa | 0.49 | 0.38 | 0.62 | 1.14 | 0.90 | 1.43 | 761.64 | 601.11 | 958.08 | 812.60 | 640.86 | 1019.90 |
| High‐income Asia Pacific | 1.04 | 0.85 | 1.27 | 2.10 | 1.78 | 2.49 | 571.60 | 471.91 | 698.96 | 445.28 | 384.66 | 514.55 |
| High‐income North America | 4.52 | 3.73 | 5.45 | 7.22 | 6.22 | 8.40 | 1278.19 | 1068.01 | 1541.62 | 1154.09 | 1002.16 | 1327.60 |
| North Africa and Middle East | 1.28 | 1.00 | 1.63 | 3.21 | 2.57 | 3.98 | 793.57 | 614.74 | 1004.66 | 784.39 | 628.33 | 976.77 |
| Oceania | 0.02 | 0.01 | 0.02 | 0.05 | 0.04 | 0.06 | 813.81 | 636.97 | 1050.36 | 827.64 | 651.71 | 1060.65 |
| South Asia | 1.64 | 1.33 | 2.03 | 4.69 | 3.79 | 5.83 | 374.17 | 302.18 | 470.48 | 389.97 | 314.38 | 487.19 |
| Southeast Asia | 1.62 | 1.29 | 2.03 | 4.09 | 3.29 | 5.11 | 729.15 | 581.66 | 919.89 | 755.95 | 604.89 | 946.23 |
| Southern Latin America | 0.32 | 0.25 | 0.40 | 0.51 | 0.40 | 0.66 | 721.46 | 572.87 | 908.55 | 604.39 | 473.51 | 771.47 |
| Southern sub‐Saharan Africa | 0.18 | 0.14 | 0.23 | 0.33 | 0.26 | 0.41 | 740.23 | 580.93 | 932.37 | 662.37 | 517.92 | 831.56 |
| Tropical Latin America | 0.43 | 0.35 | 0.52 | 1.13 | 0.92 | 1.40 | 534.24 | 437.41 | 655.11 | 489.56 | 397.55 | 605.66 |
| Western Europe | 4.29 | 3.44 | 5.25 | 5.75 | 4.76 | 6.91 | 732.23 | 597.60 | 886.75 | 581.27 | 483.77 | 690.57 |
| Western sub‐Saharan Africa | 0.45 | 0.36 | 0.57 | 1.02 | 0.81 | 1.27 | 593.12 | 467.71 | 746.63 | 634.53 | 497.17 | 807.21 |
ASRs indicates age‐standardized rates; and UI, uncertainty interval.
Figure 2. Joinpoint regression analysis showing annual percentage (APC) change for age‐standardized prevalence rate of heart failure globally from 1990 to 2019.
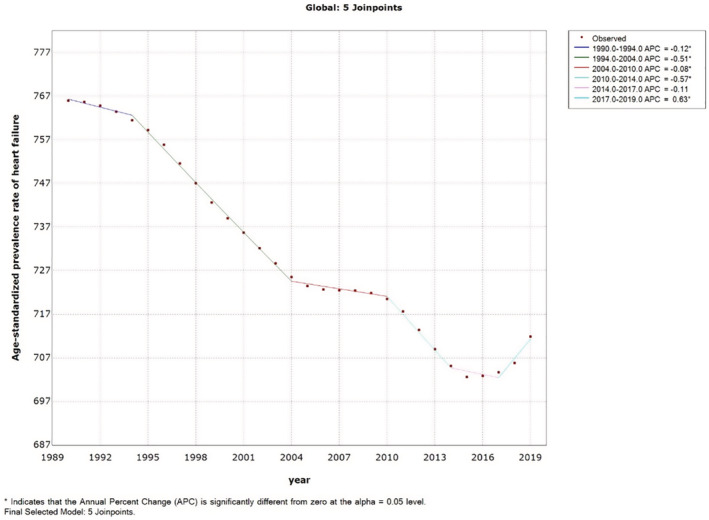
Figure 3. Global age‐standardized years lived with disability (YLDs) of heart failure per 100 000 population in 2019.
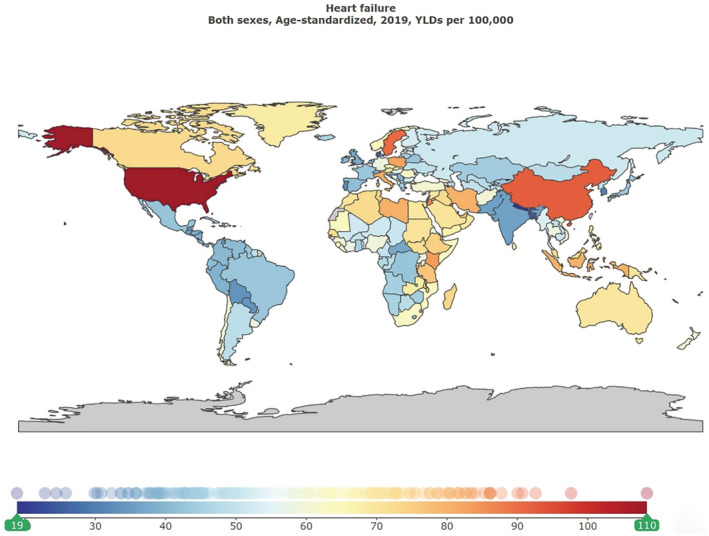
Visualization using the Global Burden of Diseases (GBD) compare tool (https://www.healthdata.org/data‐visualization/gbd‐compare).
Table 2.
Years Lived With Disabilities and ASRs of Years Lived With Disabilities per 100 000 Population for Heart Failure in 1990 and 2019 Globally and in 21 Global Burden of Diseases Regions
| Regions | 1990 | 2019 | 1990 | 2019 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | 95% UI | No. | 95% UI | 95% UI | ASRs per 100 000 | 95% UI | ||||||
| Lower | Upper | Lower | Upper | ASRs per 100 000 | Lower | Upper | Lower | Upper | ||||
| Global | 2 447 874.95 | 1 594 510.07 | 3 534 045.71 | 5 050 317.37 | 3 281 008.91 | 7 262 083.90 | 68.60 | 44.34 | 98.68 | 63.92 | 41.49 | 91.95 |
| Andean Latin America | 7226.88 | 4602.80 | 10 328.49 | 21 083.48 | 13 437.91 | 30 314.25 | 37.03 | 23.68 | 52.88 | 38.77 | 24.61 | 55.82 |
| Australasia | 24 209.86 | 15 458.24 | 35 348.94 | 35 467.45 | 22 645.02 | 52 188.64 | 104.93 | 67.59 | 151.55 | 68.00 | 43.74 | 98.90 |
| Caribbean | 12 130.00 | 7757.74 | 17 804.65 | 24 209.94 | 15 516.02 | 35 347.89 | 48.65 | 31.13 | 71.01 | 46.93 | 30.11 | 68.45 |
| Central Asia | 21 971.53 | 14 009.44 | 31 623.22 | 29 401.82 | 18 954.17 | 42 504.91 | 52.15 | 33.17 | 74.95 | 48.81 | 31.19 | 70.00 |
| Central Europe | 96 769.35 | 61 505.54 | 140 850.92 | 143 543.26 | 94 664.15 | 207 061.12 | 71.17 | 45.42 | 102.69 | 65.05 | 43.17 | 93.22 |
| Central Latin America | 34 923.61 | 22 525.24 | 50 238.40 | 92 741.01 | 59 617.60 | 133 984.01 | 45.55 | 29.47 | 65.98 | 40.96 | 26.22 | 59.32 |
| Central sub‐Saharan Africa | 8235.17 | 5170.77 | 12 427.00 | 19 163.66 | 12 030.32 | 28 342.89 | 44.57 | 27.35 | 66.19 | 43.27 | 26.15 | 64.31 |
| East Asia | 646 539.92 | 410 778.64 | 956 726.68 | 1 702 046.98 | 1 086 142.54 | 2 501 819.10 | 94.36 | 61.18 | 136.99 | 90.93 | 58.88 | 132.53 |
| Eastern Europe | 129 802.19 | 85 278.66 | 186 060.86 | 173 924.82 | 113 699.42 | 249 434.93 | 50.45 | 33.26 | 71.77 | 50.40 | 33.17 | 71.93 |
| Eastern sub‐Saharan Africa | 43 744.63 | 28 223.11 | 63 402.33 | 102 810.22 | 66 492.70 | 149 944.60 | 67.60 | 43.42 | 98.36 | 72.45 | 46.11 | 104.58 |
| High‐income Asia Pacific | 94 907.53 | 61 525.06 | 138 108.72 | 190 367.02 | 126 436.20 | 267 005.76 | 51.80 | 33.74 | 74.81 | 40.50 | 27.27 | 57.40 |
| High‐income North America | 409 944.77 | 265 755.91 | 593 839.77 | 652 237.76 | 435 716.08 | 913 955.75 | 116.03 | 77.10 | 166.97 | 104.50 | 70.05 | 146.02 |
| North Africa and Middle East | 116 030.04 | 73 419.48 | 169 481.63 | 290 350.79 | 186 461.95 | 421 310.26 | 71.15 | 44.96 | 103.14 | 70.74 | 45.15 | 101.86 |
| Oceania | 1669.92 | 1073.29 | 2420.96 | 4049.33 | 2598.96 | 5904.76 | 72.49 | 46.56 | 105.45 | 73.85 | 47.33 | 107.03 |
| South Asia | 145 578.36 | 92 926.97 | 209 651.91 | 416 556.10 | 268 503.49 | 603 755.73 | 32.76 | 20.87 | 47.68 | 34.41 | 22.10 | 50.07 |
| Southeast Asia | 145 012.95 | 92 769.70 | 210 104.65 | 367 150.03 | 237 223.16 | 532 655.34 | 64.66 | 41.73 | 93.81 | 67.56 | 43.32 | 97.73 |
| Southern Latin America | 26 097.28 | 16 361.15 | 37 968.46 | 44 562.28 | 28 822.03 | 65 334.32 | 59.91 | 37.73 | 86.84 | 52.62 | 34.19 | 77.17 |
| Southern sub‐Saharan Africa | 16 308.14 | 10 406.04 | 23 743.87 | 29 513.40 | 18 816.44 | 43 354.10 | 65.99 | 42.04 | 97.14 | 59.26 | 37.86 | 86.84 |
| Tropical Latin America | 36 516.04 | 23 861.23 | 53 252.49 | 98 454.98 | 63 169.45 | 144 166.02 | 45.69 | 29.59 | 66.86 | 42.69 | 27.51 | 62.89 |
| Western Europe | 389 736.25 | 249 249.04 | 572 701.06 | 521 001.53 | 338 852.24 | 746 732.32 | 66.47 | 42.73 | 97.06 | 52.83 | 34.27 | 75.91 |
| Western sub‐Saharan Africa | 40 520.53 | 26 155.11 | 58 212.25 | 91 681.53 | 59 703.65 | 132 512.32 | 52.72 | 33.92 | 76.55 | 56.61 | 36.09 | 83.50 |
ASRs indicates age‐standardized rates; and UI, uncertainty interval.
According to the classification of HF severity, there were 20.79 million (95% UI, 16.81–25.37) treated cases, 10.44 million (95% UI, 7.35–14.15) mild cases, 6.78 million (95% UI, 4.75–9.40) moderate cases, and 18.19 million (95% UI, 14.49–22.75) severe cases globally in 2019, with ASRs (per 100 000 population) of 263.35 (95% UI, 214.26–321.08; Figure S1), 132.20 (95% UI, 93.06–178.44; Figure S2), 85.86 (95% UI, 60.11–119.53; Figure S3), and 230.49 (95% UI, 184.89–285.93; Figure S4), which are 7.23%, 7.05%, 6.99%, and 6.90% lower than those in 1990, respectively (Table S1). ASR of prevalence decreased at the AAPC of 0.3% (95% UI, 0.2–0.3) from 1990 to 2019 in all 4 subgroups, whereas it increased at the annual percentage change of 0.6% (95% UI, 0.4–0.8) from 2017 to 2019 (Figures S5 through S8), which is consistent with the general trend. Similarly, the 2019 global YLDs numbers for treated, mild, moderate, and severe HF are 1.00 million (95% UI, 0.58–1.52), 0.42 million (95% UI, 0.23–0.71), 0.47 million (95% UI, 0.27–0.75), and 3.15 million (95% UI, 2.04–4.61), respectively, with ASRs (per 100 000 population) of 12.62 (95% UI, 7.36–19.30), 5.37 (95% UI, 2.92–8.95), 6.00 (95% UI, 3.44–9.50), and 39.93 (95% UI, 25.96–58.21), respectively, which are 7.11%, 6.95%, 6.85%, and 6.71% lower, respectively, than those in 1990 (Table S2).
Association With the SDI
In 1990, the age‐standardized point prevalence of HF (per 100 000 population) was highest in the high SDI location (900.44 [95% UI, 746.49–1079.91]), whereas it was the lowest in the low‐middle SDI location (501.99 [95% UI, 408.07–627.03]). However, in 2019, the middle SDI location replaced the high SDI location as the region with the highest ASRs of prevalence (787.39 [95% UI, 638.97–977.14]). The low‐middle SDI location still had the lowest age‐standardized point prevalence (513.12 [95% UI, 416.96–641.54]) in 2019. From 1990 to 2019, the low and low‐middle SDI locations demonstrated slight increases in ASRs of HF, whereas high, high‐middle, and middle SDI locations showed decreases, with the largest decreases in high SDI locations (Figures S9 through S13).
Regional Level
East Asia, high‐income North America, and Western Europe experienced the largest number of prevalent cases in 1990, which had not changed in 2019 (Table 1). Similarly, those 3 regions had the highest numbers of YLDs attributable to HF both in 1990 and 2019 (Table 2).
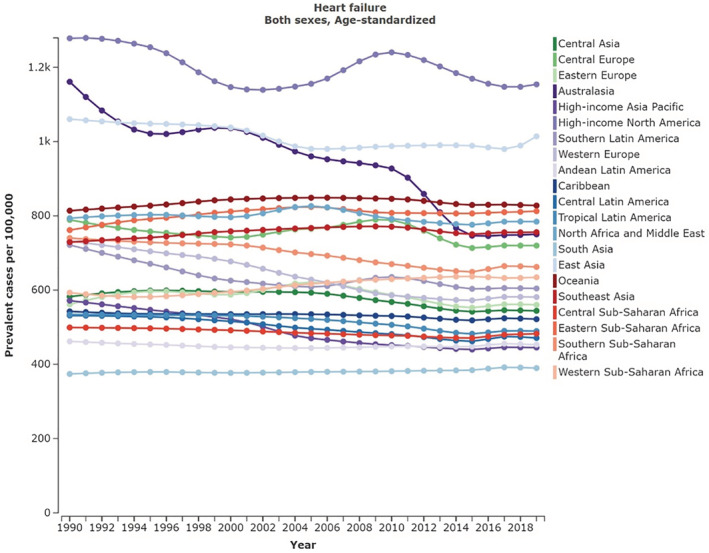
In 2019, the age‐standardized point prevalence of HF (per 100 000 population) was highest in high‐income North America (1154.09 [95% UI, 1002.16–1327.60]), East Asia (1014.06 [95% UI, 830.18–1252.96]), and Oceania (827.64 [95% UI, 651.71–1060.65]). On the contrary, South Asia (389.97 [95% UI, 314.38–487.19]), high‐income Asia Pacific (445.28 [95% UI, 384.66–514.55]), and Andean Latin America (453.01 [95% UI, 355.22–575.83]) had the lowest ASRs (Figure 4 and Table 1).
Figure 4. Age‐standardized point prevalence rate of heart failure per 100 000 population in 21 Global Burden of Diseases (GBD) regions in 2019.
Visualization using the GBD compare tool (https://www.healthdata.org/data‐visualization/gbd‐compare).
High‐income North America (104.50 [95% UI, 70.05–146.02]), East Asia (90.93 [95% UI, 58.88–132.53]), and Oceania (73.85 [95% UI, 47.33–107.03]) had the highest age‐standardized YLDs rates from HF in 2019. The ASRs were lowest for South Asia (34.41 [95% UI, 22.10–50.07]), Andean Latin America (38.77 [95% UI, 24.61–55.82]), and high‐income Asia Pacific (40.50 [95% UI, 27.27–57.40]) (Table 2).
Despite some volatility, a total of 16 GBD regions showed a decrease in the ASRs of HF from 1990 to 2019, with the largest decreases being in Australasia (35.38%), high‐income Asia Pacific (22.10%), and Western Europe (20.62%). On the contrary, only 5 GBD regions showed an increased trend, with the largest increase being in Western sub‐Saharan Africa (6.98%). We also calculated AAPCs of 21 GBD regions (Figures S14 through S34). A total of 5 GBD regions demonstrated increasing AAPCs from 1990 to 2019, including Western sub‐Saharan Africa, Eastern sub‐Saharan Africa, South Asia, Southeast Asia, and Oceania. Eastern Europe, North Africa, and the Middle East showed a constant trend. Other 14 GBD regions showed decreasing trends from 1990 to 2019. Compared with the global level, only 9 GBD regions met or exceeded the global decreasing AAPC. In the same period, a total of 16 GBD regions showed a decrease in the age‐standardized YLDs rates of HF, with the largest decreases being in Australasia (35.19%), high‐income Asia Pacific (21.82%), and Western Europe (20.52%). Another 5 GBD regions show an increased rate.
National and Territorial Level
The national and territorial age‐standardized point prevalence of HF ranged from 211.86 to 1198.06 cases per 100 000 population. The United States (1198.06 [95% UI, 1039.85–1385.34]), Guam (1088.30 [95% UI, 836.55–1411.95]), and China (1032.84 [95% UI, 846.57–1277.46]) had the highest age‐standardized point prevalence rates of HF in 2019. On the contrary, Nepal (211.86 [95% UI, 164.68–276.13]), Bhutan (255.54 [95% UI, 199.01–330.03]), and Bangladesh (275.00 [95% UI, 213.50–355.43]) had the lowest rates (Figure S35).
In 2019, the national and territorial ASRs of YLDs because of HF varied from 18.86 to 108.41 per 100 000 population. Similar to prevalence rates, the highest ASRs of YLDs were calculated in the United States (108.41 [95% UI, 72.39–151.98]), Guam (97.64 [95% UI, 61.69–142.63]), and China (92.59 [95% UI, 59.89–135.06]).
From 1990 to 2019, the percentage change in the age‐standardized point prevalence differed among 204 countries and territories. A total of 94 countries and territories showed increases, whereas others demonstrated decreases during the measurement period.
Over the period of 1990 to 2019, Oman (28.79%), Cameroon (25.71%), and Saudi Arabia (20.97%) showed the largest increases, whereas Canada (47.65%), France (44.78%), and Denmark (44.41%) demonstrated the largest decreases (Figure S36). According to the Joinpoint regression analysis, Oman, Cameroon, and Saudi Arabia showed the largest increases at AAPCs of 0.9%, 0.8%, and 0.7%, respectively (Figures S37 through S39), whereas Canada, France, and Denmark demonstrated the largest decreases from 1990 to 2019 at AAPCs of 2.2%, 2.0%, and 2.0%, respectively (Figures S40 through S42). The percentage change in the ASRs of YLDs is the same as ASRs of prevalence. From 1990 to 2019, Oman (29.57%), Cameroon (26.54%) and Saudi Arabia (22.42%) showed the largest increases, whereas Canada (47.58%), France (44.62%), and Denmark (44.29%) demonstrated the largest decreases.
Sex and Age Differences
The global point prevalence of HF increased with age in 2019 for both men and women, with the highest ASRs of prevalence among those >75 years old (9193.41 [95% UI, 7114.68–11 721.51]; Figure S43). Compared with 1990, ASRs of prevalence had decreased in all age groups except the 50‐ to 55‐year‐old group. The age‐standardized point prevalence in men was higher than that in women in all age groups both in 1990 and 2019. We also explored sex differences in 21 GBD regions (Table S3). In 1990, men demonstrated higher age‐standardized point prevalence in all GBD regions, with the highest male–female ratio of 1.74 in the Caribbean. However, in 2019, the age‐standardized point prevalence for women was slightly higher than for men in East Asia (1001.01 [95% UI, 819.06–1245.62] versus 991.23 [95% UI, 808.02–1228.71]; Figure 5). ASRs of YLDs demonstrated a similar pattern (Table S4).
Figure 5. Sex differences of age‐standardized prevalence rate of heart failure per 100 000 population in 21 Global Burden of Diseases (GBD) regions in 2019.
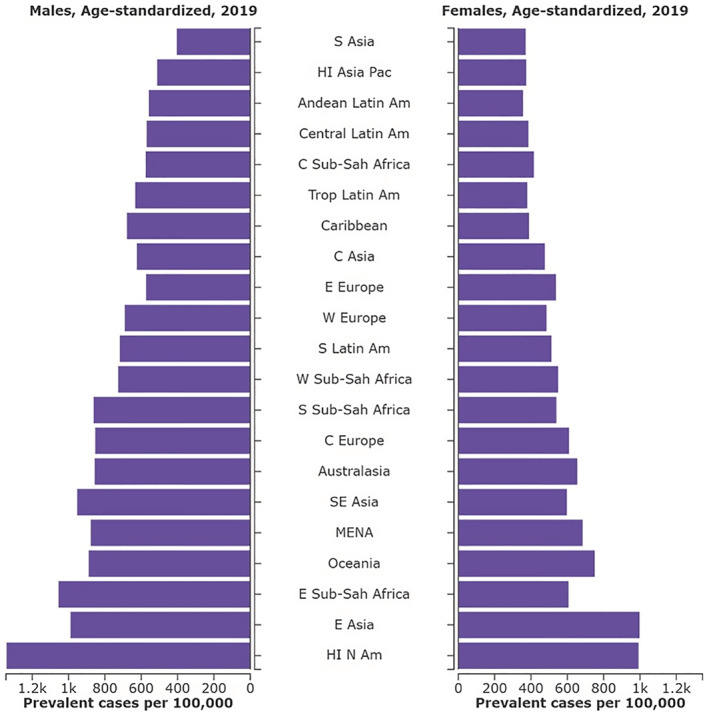
Visualization using the GBD compare tool (https://www.healthdata.org/data‐visualization/gbd‐compare). S indicates south; HI, high‐income; Pac, Pacific; Am, America; C, central; Sub‐Sah, sub‐Saharan; Trop, tropical; E, eastern; W, western; SE, southeast; MENA, Middle East and North Africa; and N, north.
Causes of HF
Although there are sex and regional differences for the causes of HF, the main causes of HF globally are heart diseases. Ischemic heart disease (265.72 [95% UI, 197.23–346.43]) and hypertensive heart disease (233.77 [95% UI, 170.52–312.90]) accounted for the highest proportion of HF both for men and women in 2019. The difference between men and women was that ischemic heart disease took first place in men, whereas hypertensive heart disease led in women. In addition to heart diseases, chronic obstructive pulmonary disease (COPD) (65.64 [95% UI, 45.27–94.08]) is a main cause of HF (Table 3). Over the period 1990 to 2019, the age‐standardized prevalence rate of HF attributable to hypertensive heart disease increased (219.54 [95% UI, 158.77–299.36] versus 233.77 [95% UI, 170.52–312.90]), whereas ASRs of HF from other causes all decreased.
Table 3.
ASRs of Prevalence per 100 000 Population for Heart Failure in 2019 Globally by Causes
| Causes | Men | Women | ||||
|---|---|---|---|---|---|---|
| ASRs per 100 000 | 95% UI | ASRs per 100 000 | 95% UI | |||
| Lower | Upper | Lower | Upper | |||
| Alcoholic cardiomyopathy | 13.33 | 10.32 | 17.25 | 4.13 | 3.18 | 5.36 |
| Asbestosis | 0.07 | 0.05 | 0.09 | 0.01 | 0.01 | 0.01 |
| Chagas disease | 4.67 | 3.20 | 6.35 | 2.27 | 1.29 | 3.60 |
| Chronic obstructive pulmonary disease | 75.55 | 53.22 | 104.32 | 57.51 | 39.01 | 85.02 |
| Coal worker's pneumoconiosis | 0.07 | 0.05 | 0.09 | 0.01 | 0.00 | 0.01 |
| Congenital heart anomalies | 7.04 | 4.97 | 9.87 | 7.55 | 5.39 | 10.49 |
| Endocarditis | 4.29 | 3.51 | 5.32 | 4.82 | 3.96 | 5.97 |
| Endocrine, metabolic, blood, and immune disorders | 2.28 | 1.91 | 2.78 | 2.28 | 1.92 | 2.79 |
| G6PD deficiency | 0.27 | 0.21 | 0.34 | 0.16 | 0.12 | 0.20 |
| Hypertensive heart disease | 241.25 | 176.26 | 324.85 | 224.60 | 162.85 | 302.06 |
| Interstitial lung disease and pulmonary sarcoidosis | 1.45 | 1.06 | 1.92 | 1.19 | 0.86 | 1.60 |
| Ischemic heart disease | 316.12 | 236.51 | 411.40 | 222.48 | 163.75 | 291.22 |
| Myocarditis | 5.54 | 4.50 | 6.73 | 4.76 | 3.85 | 5.79 |
| Nonrheumatic calcific aortic valve disease | 11.17 | 7.00 | 16.91 | 9.07 | 5.70 | 13.88 |
| Nonrheumatic degenerative mitral valve disease | 16.63 | 10.53 | 24.88 | 24.20 | 15.48 | 35.93 |
| Other cardiomyopathy | 56.89 | 44.75 | 71.27 | 39.82 | 30.97 | 51.12 |
| Other hemoglobinopathies and hemolytic anemias | 0.62 | 0.50 | 0.79 | 0.61 | 0.50 | 0.76 |
| Other nonrheumatic valve diseases | 0.25 | 0.20 | 0.34 | 0.41 | 0.32 | 0.53 |
| Other pneumoconiosis | 0.06 | 0.05 | 0.08 | 0.02 | 0.01 | 0.02 |
| Rheumatic heart disease | 20.60 | 15.98 | 26.12 | 31.59 | 24.49 | 40.34 |
| Silicosis | 0.35 | 0.25 | 0.48 | 0.02 | 0.01 | 0.02 |
| Thalassemia | 0.32 | 0.22 | 0.44 | 0.30 | 0.21 | 0.40 |
ASRs indicates age‐standardized rates; UI, uncertainty interval; and G6PD, glucose‐6‐phosphate dehydrogenase.
DISCUSSION
In the present study, we used HF data from the GBD 2019 study to comprehensively analyze the burden, trends, and inequalities of HF by location, age, and sex from 1990 to 2019. We found that the number of HF cases increased from 1990 to 2019 globally, which might be because of a demographic change, mainly an aging population. In 1990, the population >65 years old accounted for about 6.1% of the global population; this number reached 9.3% in 2019. 15 Despite the enormous efforts of the global public health industry, the trend of an aging population will not be reversed for a period of time, so it is necessary to prepare for the continued increase in the number of people with HF worldwide. The good news is that compared with 1990, the age‐standardized prevalence rate of HF decreased in 2019, albeit modestly. We used the Joinpoint regression model to find that ASRs decreased globally at an AAPC of 0.3% from 1990 to 2019. This might be because with economic development, more patients have received regular treatment. On the other hand, advances in HF treatment options also help reduce the age‐standardized prevalence of HF. 1 , 14 Notably, according to our Joinpoint regression model, the age‐standardized prevalence rate of HF globally increased at an annual percentage change of 0.6% from 2017 to 2019. We speculate that one of the possible reasons for this is because with the development of technology and the promotion of regular physical examinations, some early HF that was not easily detected before was diagnosed. Conrad et al assessed temporal trends in the prevalence of heart failure in the United Kingdom from 2002 to 2014. They found that the standardized incidence of HF decreased from 358 to 332 per 100 000 population, which is consistent with the trends derived from our study. 3 Although the overall trend decreased from 1990 to 2019, given the burden of HF on patients and public health, we must pay attention to this possible increasing trend in recent years.
We also explored the burden of HF in regions with a different SDI. In general, the age‐standardized prevalence rate of HF in regions with a middle or above SDI is significantly higher than low‐middle and low SDI regions. People in high‐level SDI regions have good nutritional status, adequate access to health services, and higher education. Meanwhile, populations that are increasing and aging are more pronounced in high‐level SDI regions. Lack of adequate medical resources for people in low SDI areas may also be a factor. The prevalence of HF in low SDI regions might be underestimated because a subset of the population is underdiagnosed. Similar to our study, socioeconomically deprived individuals were more likely to develop HF than affluent individuals in the United Kingdom. 3
East Asia, high‐income North America, and Western Europe experienced the largest number of prevalent cases both in 1990 and 2019. A total of 5 GBD regions demonstrated increasing AAPCs from 1990 to 2019, including Western sub‐Saharan Africa, Eastern sub‐Saharan Africa, South Asia, Southeast Asia, and Oceania. Several previous studies also support this finding. Compared with Western regions, the prevalence rate in Asia seemed to be higher, ranging from 1.3% to 6.7%. 16 , 17 , 18 , 19 , 20 South Asia accounts for a quarter of the world's population, which is at an increased risk and earlier ages of HF. 21 Compared with the global level, only 9 GBD regions meet or exceed the global decreasing AAPC. This demonstrated clear inequalities between regions, suggesting that we need to strengthen education, improve the quality of health services, and conduct early screening in most parts of Africa and parts of Asia to reduce the prevalence of HF. Oman, Cameroon, and Saudi Arabia showed the largest increases at AAPCs of 0.9%, 0.8%, and 0.7%, respectively. This may be because of a lack of emphasis on HF and inadequate medical resources in these nations. On the contrary, Canada, France, and Denmark demonstrated the largest decreases from 1990 to 2019 at AAPCs of 2.2%, 2.0%, and 2.0%, respectively. Development of abundant economic and medical resources, and regular examinations might contribute to the considerable decreases. It is essential to study the experiences of the countries that have been the most successful at HF control to reverse the increasing prevalence trends of HF in countries such as Oman, Cameroon, and Saudi Arabia. In addition, related international aid is necessary and should be focused on these countries.
Exploring the underlying causes is of great significance for the prevention and treatment of HF. Unsurprisingly, ischemic heart disease and hypertensive heart disease accounted for the highest proportion of HF in 2019. Notably, over the period 1990 to 2019, the age‐standardized prevalence rate of HF attributable to hypertensive heart disease increased, whereas ASRs of HF from rheumatic heart disease decreased. Hypertension is considered a significant risk factor for HF. 22 , 23 , 24 Long‐term elevated blood pressure can lead to structural changes in the myocardium and aggravate the progression of HF. 25 In the present study, we found that the age‐standardized prevalence rate of HF attributable to hypertensive heart disease increased from 1990 to 2019. Considering hypertension is a modifiable risk factor, control of high blood pressure is important to prevent hypertensive HF. In addition to heart diseases, we found that COPD is a main cause of HF. COPD is one of the most prevalent chronic diseases worldwide, which shares various symptoms with HF. 26 COPD and HF also have several common risk factors, including advanced age, smoking, and obesity. 27 Therefore, clinicians must pay more attention to the cardiac function of patients with COPD, and objectively identify HF in patients with COPD at an early stage. Roth and colleagues report that the burden of cardiovascular diseases continues to increase globally, 28 , 29 which is consistent with a potential upward trend in HF worldwide. Despite the consensus on associations between HF and common diseases or factors such as atrial fibrillation and obesity, the GBD 2019 did not identify these factors as underlying causes in HF, which might be improved in a future GBD study. The GBD 2019 study continuously evaluates, improves, and applies statistical methods to achieve reliability and accuracy in the diagnosis of HF. Moreover, the GBD case definition does not allow for remission from heart failure; once diagnosed, all patients remain in 1 of the 4 severity categories. Therefore, it seems that HF treatment advances are not enough to explain the decreases seen in some locations. Prevention or early treatment of underlying causes, such as ischemic heart diseases, hypertensive heart diseases, and COPD, might be plausible reasons.
To the best of our knowledge, this is the first time the global burden of HF and its contributing causes were comprehensively analyzed. The prevalence, trends, and inequalities of HF found in the present study might help guide the development and implementation of interventions for HF. However, our study also has some limitations. First, because of economic underdevelopment in some areas, data collection is limited, and the true prevalence and burden of HF may be underestimated. In this case the results depend on the validity of the GBD predictive model. Although the data processing and modeling methods have been improved in the GBD 2019 study, there is still a need to improve the quality of collected data and strengthen data sharing. Moreover, the prevalence of HF in low SDI regions may be underestimated because of insufficient medical resources and the low priority given to HF, because GBD 2019 counts diagnosed HF. Second, we did not analyze HF subtypes such as HF with preserved ejection fraction, because of the lack of relevant data in the GBD 2019 study. We recommend that data collection on HF subtypes be included in future GBD studies. Third, because HF was not considered an underlying cause of deaths in the GBD 2019 study, disability‐adjusted life‐years could not be evaluated appreciably.
HF remains a major public health problem worldwide, with a possible increased trend in the future. Although the age‐standardized prevalence rate of HF decreased globally from 1990 to 2019 in general, the rate seemed to increase from 2017. Regional inequalities were also found in the burden of HF. Efforts for prevention and control of HF should focus more on less‐developed regions with substantial HF burden. It is essential to prevent and treat primary diseases such as ischemic heart disease and hypertensive heart disease for the control of HF.
Sources of Funding
This work is supported by the General Program of the National Natural Science Foundation of China (number 81770408) and National Key Research and Development Program of China (number 2018YFC1311204).
Disclosures
None.
Supporting information
Tables S1–S4
Figures S1–S43
Acknowledgments
The authors thank the Global Burden of Disease collaborators for their contributions to the GBD 2019 study.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.122.027852
For Sources of Funding and Disclosures, see page 12.
Contributor Information
Kai Zhu, Email: zhu.kai1@zs-hospital.sh.cn.
Chunsheng Wang, Email: wangchunsheng@fudan.edu.cn.
Changfa Guo, Email: guo.changfa@zs-hospital.sh.cn.
References
- 1. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599–3726. doi: 10.1093/eurheartj/ehab368 [DOI] [PubMed] [Google Scholar]
- 2. Roger VL. Epidemiology of heart failure: a contemporary perspective. Circ Res. 2021;128:1421–1434. doi: 10.1161/CIRCRESAHA.121.318172 [DOI] [PubMed] [Google Scholar]
- 3. Conrad N, Judge A, Tran J, Mohseni H, Hedgecott D, Crespillo AP, Allison M, Hemingway H, Cleland JG, McMurray JJV, et al. Temporal trends and patterns in heart failure incidence: a population‐based study of 4 million individuals. Lancet. 2018;391:572–580. doi: 10.1016/S0140-6736(17)32520-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Smeets M, Vaes B, Mamouris P, Van Den Akker M, Van Pottelbergh G, Goderis G, Janssens S, Aertgeerts B, Henrard S. Burden of heart failure in Flemish general practices: a registry‐based study in the Intego database. BMJ Open. 2019;9:e022972. doi: 10.1136/bmjopen-2018-022972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dmitrieva NI, Liu D, Wu CO, Boehm M. Middle age serum sodium levels in the upper part of normal range and risk of heart failure. Eur Heart J. 2022;43:3335–3348. doi: 10.1093/eurheartj/ehac138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Roger VL, Weston SA, Redfield MM, Hellermann‐Homan JP, Killian J, Yawn BP, Jacobsen SJ. Trends in heart failure incidence and survival in a community‐based population. JAMA. 2004;292:344–350. doi: 10.1001/jama.292.3.344 [DOI] [PubMed] [Google Scholar]
- 7. Taylor CJ, Ordóñez‐Mena JM, Roalfe AK, Lay‐Flurrie S, Jones NR, Marshall T, Hobbs FDR. Trends in survival after a diagnosis of heart failure in the United Kingdom 2000–2017: population based cohort study. BMJ. 2019;364:l223. doi: 10.1136/bmj.l223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C, Naghavi M, Salomon JA, Shibuya K, Vos T, et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380:2063–2066. doi: 10.1016/S0140-6736(12)61899-6 [DOI] [PubMed] [Google Scholar]
- 9. GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dunlay SM, Roger VL. Understanding the epidemic of heart failure: past, present, and future. Curr Heart Fail Rep. 2014;11:404–415. doi: 10.1007/s11897-014-0220-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, Naghavi M, Mensah GA, Murray CJ. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;372:1333–1341. doi: 10.1056/NEJMoa1406656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017;3:7–11. doi: 10.15420/cfr.2016:25:2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González‐Juanatey JR, Harjola VP, Jankowska EA, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891–975. doi: 10.1002/ejhf.592 [DOI] [PubMed] [Google Scholar]
- 15. GBD 2019 Demographics Collaborators . Global age‐sex‐specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1160–1203. doi: 10.1016/S0140-6736(20)30977-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Raja Shariff RE, Hui Beng K, Mohd Ghazi A. The great Asian mismatch: training versus care in heart failure. J Card Fail. 2022;28:1378–1381. doi: 10.1016/j.cardfail.2022.05.007 [DOI] [PubMed] [Google Scholar]
- 17. Yang YN, Ma YT, Liu F, Huang D, Li XM, Huang Y, Tang Q, Chen BD, Ma X, Xie X, et al. Incidence and distributing feature of chronic heart failure in adult population of Xinjiang. Zhonghua Xin Xue Guan Bing Za Zhi. 2010;38:460–464. [PubMed] [Google Scholar]
- 18. Chong AY, Rajaratnam R, Hussein NR, Lip GY. Heart failure in a multiethnic population in Kuala Lumpur, Malaysia. Eur J Heart Fail. 2003;5:569–574. doi: 10.1016/S1388-9842(03)00013-8 [DOI] [PubMed] [Google Scholar]
- 19. Ng TP, Niti M. Trends and ethnic differences in hospital admissions and mortality for congestive heart failure in the elderly in Singapore, 1991 to 1998. Heart. 2003;89:865–870. doi: 10.1136/heart.89.8.865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Guo Y, Lip GY, Banerjee A. Heart failure in East Asia. Curr Cardiol Rev. 2013;9:112–122. doi: 10.2174/1573403X11309020004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Martinez‐Amezcua P, Haque W, Khera R, Kanaya AM, Sattar N, Lam CSP, Harikrishnan S, Shah SJ, Kandula NR, Jose PO, et al. The upcoming epidemic of heart failure in South Asia. Circ Heart Fail. 2020;13:e7218. doi: 10.1161/CIRCHEARTFAILURE.120.007218 [DOI] [PubMed] [Google Scholar]
- 22. Rismiati H, Lee HY. Hypertensive heart failure in Asia. Pulse (Basel). 2021;9:47–56. doi: 10.1159/000518661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;128:e240–e327. [DOI] [PubMed] [Google Scholar]
- 24. Lloyd‐Jones DM, Larson MG, Leip EP, Beiser A, D'Agostino RB, Kannel WB, Murabito JM, Vasan RS, Benjamin EJ, Levy D, et al. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation. 2002;106:3068–3072. doi: 10.1161/01.CIR.0000039105.49749.6F [DOI] [PubMed] [Google Scholar]
- 25. Kalogeropoulos AP, Goulbourne C, Butler J. Diagnosis and prevention of hypertensive heart failure. Heart Fail Clin. 2019;15:435–445. doi: 10.1016/j.hfc.2019.05.001 [DOI] [PubMed] [Google Scholar]
- 26. MacLeod M, Papi A, Contoli M, Beghé B, Celli BR, Wedzicha JA, Fabbri LM. Chronic obstructive pulmonary disease exacerbation fundamentals: diagnosis, treatment, prevention and disease impact. Respirology. 2021;26:532–551. doi: 10.1111/resp.14041 [DOI] [PubMed] [Google Scholar]
- 27. de Miguel DJ, Chancafe MJ, Jimenez GR. The association between COPD and heart failure risk: a review. Int J Chron Obstruct Pulmon Dis. 2013;8:305–312. doi: 10.2147/COPD.S31236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Roth GA, Mensah GA, Fuster V. The global burden of cardiovascular diseases and risks: a compass for global action. J Am Coll Cardiol. 2020;76:2980–2981. doi: 10.1016/j.jacc.2020.11.021 [DOI] [PubMed] [Google Scholar]
- 29. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021. doi: 10.1016/j.jacc.2020.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S4
Figures S1–S43


