Abstract
Objective:
Electroconvulsive therapy (ECT) devices are classified as class II (moderate risk) for the treatment of depressive disorders and catatonia in patients aged 13 and older, but it is unknown how often the treatment is utilized by child and adolescent patients. The aim of this study was to examine the demographics of child and adolescent hospitalizations involving ECT, the medical and psychiatric comorbidities of these hospitalizations, and the overall number of treatments administered per hospitalization.
Method:
The 2019 Kids’ Inpatient Database, a national sample of pediatric discharges from 3,998 acute care hospitals, was analyzed for hospitalizations involving patients aged 19 and younger receiving ECT based on inpatient procedural codes.
Results:
315 (95% confidence interval 275 to 354) discharges among child and adolescent patients, or 0.03% of youth hospitalizations, involved the administration of ECT in the KID in 2019. Hospitalizations in the Northeast, those involving patients residing in ZIP codes in the top income quartile, and those for commercially insured patients had higher odds of ECT administration. Primary discharge diagnoses among ECT recipients were major depressive disorder (143; 46.4%), schizophrenia and other psychotic disorders (71; 23.1%) and bipolar disorder (59; 19.2%). In total 153 (48.6%) of ECT recipients had a coded diagnosis of suicidal ideation. Hospitalizations involved a median of 2 (IQR 1 to 5) ECT treatments before discharge.
Conclusions:
ECT is rarely utilized in the inpatient treatment of child and adolescent patients, but is most often administered to patients with mood and psychotic disorders. Commercial insurance and higher income were associated with higher odds of ECT administration, suggesting that access to care may be limited.
Keywords: electroconvulsive therapy, depressive disorders, cohort studies, adolescent psychiatry, real world evidence
Introduction
Electroconvulsive therapy (ECT) is an evidence-based treatment in young people, with more than 80 years of clinical utilization [1] and clinical guidelines recommending its use in severe pediatric mood disorders and catatonia [2]. Consistent with these recommendations, recent evidence suggests that the efficacy and tolerability of ECT in adolescents is equal to that in adults [3], with the largest individual case series of ECT in patients age 18 and younger finding a response rate of 77% among 107 youth with predominantly mood disorders [4].
While ECT utilization is not tracked uniformly on a national level in the United States, a 1980 estimate based on survey data from inpatient psychiatric facilities suggested only 500 patients age 11–20 were treated with ECT annually, or 1.5% of the total patients in the sample [5]. More recently an analysis of treatment data from 3 states representing 16.5% of the US population found 269 individuals younger than 18 who received ECT in any treatment setting over a variable date range of 10–17 years per state, representing 0.4% of the patients treated in those states [6]. A further analysis of nationally-representative data from community hospitals in the US from 2002 to 2017 found 2,005 hospital discharges among patients aged 18 and younger in which ECT was utilized, or approximately 125 patients per year [7].
Prior studies of pediatric ECT are limited in data source, relying on survey data with imperfect response rates [5], utilizing a subset of US states [6], or focusing on a data source with relatively low (20%) sampling of discharges [7]. Data from a large nationally representative source would allow for better characterization of ECT as it is delivered in ordinary clinical practice, and could point to potential gaps in treatment delivery for pediatric patients. Moreover, such data could provide a starting point for future prospective work, and understanding the present use of ECT is a starting point for potential practice improvement. This study characterizes the demographics of child and adolescent ECT recipients and their medical and psychiatric diagnoses using a nationally representative sample of discharges from community hospitals in the United States.
Methods
Data Source
This study utilized the 2019 version of the Kids’ Inpatient Database (KID). The KID is produced every three years (most recently in 2019) by the Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Research and Quality. The KID provides administrative data on pediatric hospitalizations in the United States. The KID is generated based on billing records from 3,998 non-federal community hospitals in 49 states, with data reported from all payment sources (including government and commercial insurances). This is a subset of the overall 6,090 hospitals, and 5,141 community hospitals in the United States (based on 2019 American Hospital Association data) [8]. Non-newborn discharges from these KID hospitals are then sampled at a depth of 80% without replacement. In order to extrapolate from the sampled hospitals within the KID to the broader universe of overall hospitals, sampled hospitals are stratified on the basis of ownership/control, bed size, teaching status, rural/urban location, U.S. region, and a stratum for freestanding children’s hospitals. The overall number of discharges among KID sample hospitals is then compared to the number of pediatric discharges among overall hospitals, and a weight factor applied to KID hospitalizations by strata to extrapolate to non-sampled hospitals.
Data Elements
KID data elements include patient age, sex, race, as well as the population of the patient’s county of residence and income quartile of the ZIP code in which the patient resides. Additionally, the KID provides data on the region of the hospital in question, whether the hospitalization involved an interfacility transfer at admission or discharge, primary payment source, hospital length of stay, and total hospital charges. The KID likewise includes information on up to 40 discharge diagnoses and up to 25 procedures performed during hospitalization.
Selection of Hospitalizations Involving ECT
Hospitalizations were identified based on the Procedure Coding System from the International Statistical Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM/PCS). ECT was defined by the codes GZB0ZZZ (ECT, unilateral-single seizure), GZB1ZZZ (unilateral-multiple seizures), GZB2ZZZ (ECT bilateral-single seizure), GZB3ZZZ (ECT bilateral-multiple seizures), and GZB4ZZZ (other ECT). Consistent with the World Health Organization definition of childhood and adolescence, hospitalizations were included in the analysis if they involved patients aged 19 or younger at time of admission and who received at least one ECT procedure during hospitalization. Primary diagnoses and comorbidities were identified from the discharge diagnoses, and classified according to the Pediatric Clinical Classification System (PECCS) [9], which groups the 72,446 ICD-10-CM diagnosis codes into 834 clinically distinctive categories for pediatric medical conditions.
Statistical Analysis
As the KID uses a survey design, this produces variance around all reported values for both continuous and categorical variables, which are listed with their respective 95% confidence intervals (CI). As a result of this, and the non-normal distribution of length of stay and total hospital charges, these values are reported as medians with interquartile range (IQR). All analyses were conducted on data weighted according to the appropriate KID discharge weight to obtain national estimates. In the primary statistical model, a logistic regression accounting for the survey design of the KID was conducted among hospitalizations for patients aged 19 and younger and admitted for a primary mental health or substance abuse diagnosis, as classified by the KID (I10_SERVICELINE = 2). In this model, the binary outcome of receipt of ECT (yes/no) was the dependent variable, with hospitalizations not involving the use of ECT as the reference category. Based on consensus of expert clinicians, independent variables were chosen from among KID data fields. For this model age (as a continuous variable), sex (male/female), admission type (elective/non-elective), hospital region (Northeast/Midwest/South/West), household income quartile of the patient’s ZIP code (1st/2nd/3rd/4th), race (Black, Hispanic, Asian or Pacific Islander/Other/white), and primary payor (Medicaid/other/commercial insurance) were the independent variables. As age itself has been associated with ECT access in adults in a non-linear way [10], as a sensitivity model the analysis was repeated with patient age replaced with the Z score of age. Results in this sensitivity model did not differ (data not shown). Analyses were conducted using SPSS (version 29; IBM Software, Inc, Armonk, NY). As the KID is a de-identified dataset this study was determined to be Not Human Subjects Research by the MassGeneral Brigham Institutional Review Board. This study is reported in accordance with the REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement [11].
Results
In the 2019 KID, 315 (95% confidence interval 275 to 354) discharges among children and adolescents involved the administration of ECT. ECT usage increased with age, with only 13 hospitalizations involving ECT patients aged under 14 (Figure 1). In total 138 hospitalizations were for patients younger than age 18 at time of admission. Full demographic information for hospitalizations involving ECT are given in Table 1. In total there were 1,049,655 overall hospitalizations for patients aged 10 to 19 in the KID, meaning that the proportion of youth hospitalizations involving the administration of ECT was 0.03%. ECT was initiated a median of 6.9 days (IQR 3 to 14 days) into hospitalization, and hospitalizations involved a median of 2 (IQR 1 to 5) ECT treatments before discharge. Total hospital length of stay was a median of 20 days (IQR 11.9 to 37.8 days), with a median total hospital charge of $88,778 ($49,571 to $181,860).
Figure 1:
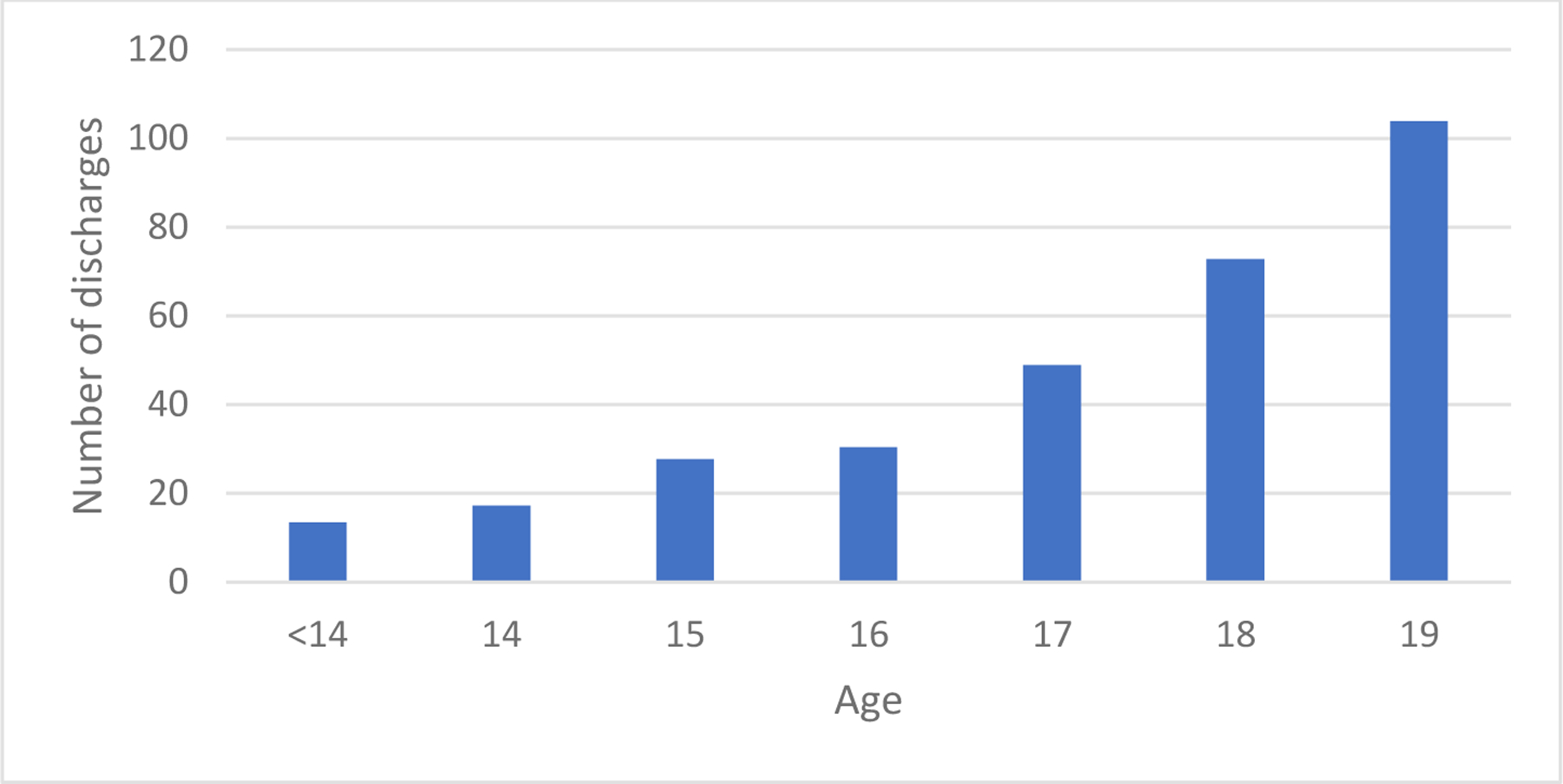
age distribution of child and adolescent patients receiving ECT
Table 1:
demographics of patients aged 19 and younger receiving ECT
| 95% CI | 95% CI | |||||
|---|---|---|---|---|---|---|
| N | Lower | Upper | % | Lower | Upper | |
| Overall sample | 315 | 275 | 354 | |||
| Age (yrs; mean, SD) | 17.2 ± 2.0 | |||||
| Male Sex | 145 | 119 | 170 | 46.0% | 40.5% | 51.5% |
| Race | ||||||
| White | 191 | 165 | 216 | 60.6% | 57.8% | 69.9% |
| Black | 34 | 22 | 46 | 10.9% | 8.1% | 16.1% |
| Hispanic | 33 | 22 | 43 | 10.3% | 8.0% | 14.7% |
| Asian or Pacific Islander | 20 | 9 | 31 | 6.3% | 4.0% | 10.9% |
| Other | 20 | 0 | 0 | 6.3% | 3.4% | 13.5% |
| Hospital Region | ||||||
| Northeast | 112 | 78 | 146 | 35.7% | 28.7% | 43.3% |
| Midwest | 99 | 82 | 117 | 31.6% | 26.5% | 37.1% |
| South | 66 | 60 | 72 | 20.9% | 18.0% | 24.1% |
| West | 37 | 28 | 47 | 11.9% | 9.2% | 15.2% |
| Population of County of Residence | ||||||
| Central metro county >1 million | 109 | 85 | 133 | 34.7% | 29.5% | 40.4% |
| Fringe metro county >1 million | 88 | 64 | 111 | 27.8% | 22.5% | 33.9% |
| Metro Area 250,000–999,999 | 64 | 48 | 80 | 20.3% | 15.7% | 25.9% |
| Metro Area 50,000–249,000 | 22 | 13 | 32 | 7.1% | 4.6% | 10.8% |
| Micropolitan | 20 | 12 | 27 | 6.2% | 4.2% | 9.2% |
| Non-core county | 12 | 6 | 18 | 3.8% | 2.2% | 6.5% |
| Household Income Quartile for Pt ZIP Code | ||||||
| 1 | 42 | 30 | 55 | 13.4% | 9.9% | 18.0% |
| 2 | 60 | 47 | 73 | 19.1% | 15.1% | 23.8% |
| 3 | 93 | 71 | 114 | 29.5% | 24.5% | 35.0% |
| 4 | 119 | 93 | 146 | 38.0% | 32.6% | 43.6% |
| Discharge Quarter | ||||||
| Jan-Mar | 78 | 61 | 94 | 24.7% | 20.1% | 29.8% |
| Apr-Jun | 86 | 65 | 107 | 27.4% | 22.4% | 32.9% |
| Jul-Sep | 71 | 54 | 89 | 22.7% | 18.1% | 28.0% |
| Oct-Dec | 80 | 60 | 99 | 25.3% | 20.6% | 30.7% |
| Admission Type | ||||||
| Elective | 50 | 35 | 65 | 15.8% | 11.7% | 21.0% |
| Non-Elective | 265 | 226 | 304 | 84.2% | 79.0% | 88.3% |
| Primary Payor | ||||||
| Medicaid | 97 | 77 | 117 | 30.8% | 25.9% | 36.2% |
| Commercial Insurance | 201 | 168 | 234 | 64.0% | 58.4% | 69.3% |
| Other | 17 | 6 | 26 | 5.1% | 2.9% | 10.2% |
| Admission Status | ||||||
| Not Transferred In | 200 | 166 | 235 | 63.7% | 58.4% | 69.7% |
| Transferred from Acute Care Hospital | 70 | 53 | 87 | 22.3% | 18.0% | 27.8% |
| Transferred from Another Facility | 41 | 28 | 54 | 13.1% | 9.5% | 18.1% |
| Patient Disposition | ||||||
| Discharged | 281 | 241 | 321 | 89.4% | 84.9% | 92.7% |
| Transferred to Another Facility | 33 | 17 | 50 | 10.8% | 6.4% | 17.6% |
| # of treatments (median, IQR) | 2 (1–5) | |||||
| time to 1st ECT (days; mean, SD) | 6.9 (3, 14) | |||||
| Hospital Length of Stay (median, IQR) | 20.0 (11.9 to 37.8) | |||||
| Total Charges (median, IQR) | $88,778 ($49,571 to $181,860) | |||||
In order to explore demographic factors associated with ECT receipt, a logistic regression on the outcome of receiving ECT among hospitalizations involving a principal mental health or substance abuse diagnosis was performed, adjusting for age, sex, admission type (elective vs. non-elective), hospital region, household income quartile of the patient’s ZIP code, race, and primary payor. In this model, older age (aOR 1.46; 95% CI: 1.35 to 1.58), Northeast region (aOR 2.12; 95% CI: 1.13 to 3.98), Asian or Pacific Islander race (aOR 2.28; 95% CI: 1.26 to 4.13), and commercial insurance (aOR 1.70; 95% CI: 1.26 to 2.31) were associated with higher odds of ECT receipt. In contrast, non-elective admission (aOR 0.60; 95% CI: 0.40 to 0.90) and lowest income quartile (aOR 0.32; 95% CI: 0.20 to 0.52) or 2nd income quartile (aOR 0.51; 95% CI: 0.35 to 0.76) were associated with lower odds of ECT receipt, while sex was not significantly associated (Table 2).
Table 2:
logistic regression of the binary outcome of receipt of ECT (yes/no) was the dependent variable, with age, sex, admission type (elective vs. non-elective), hospital region, household income quartile of the patient’s ZIP code, race, and primary payor as independent variables.
| Parameter | aOR | 95% Confidence Interval | |
|---|---|---|---|
| Lower | Upper | ||
| Age | 1.46 | 1.35 | 1.58 |
| Sex | |||
| Male | 1.26 | 0.95 | 1.67 |
| Female | 1.00 | . | . |
| Admission Type | |||
| Non-Elective | 0.60 | 0.40 | 0.90 |
| Elective | 1.00 | . | . |
| Hospital Region | |||
| Northeast | 2.12 | 1.13 | 3.98 |
| Midwest | 1.33 | 0.76 | 2.35 |
| South | 0.71 | 0.39 | 1.29 |
| West | 1.00 | . | . |
| Household Income Quartile for Pt ZIP Code | |||
| 1 | 0.32 | 0.20 | 0.52 |
| 2 | 0.51 | 0.35 | 0.76 |
| 3 | 0.81 | 0.58 | 1.13 |
| 4 | 1.00 | . | . |
| Race | |||
| Black | 0.78 | 0.48 | 1.25 |
| Hispanic | 0.98 | 0.62 | 1.56 |
| Asian or Pacific Islander | 2.28 | 1.26 | 4.13 |
| Other | 1.04 | 0.56 | 1.93 |
| White | 1.00 | . | . |
| Primary Payor | |||
| Commercial Insurance | 1.70 | 1.26 | 2.31 |
| Other | 0.26 | 0.06 | 1.09 |
| Medicaid | 1.00 | . | . |
The most frequent PECCS primary discharge diagnosis category for hospitalizations involving ECT was major depressive disorder (143; 46.4%), with schizophrenia and other psychotic disorders (71; 23.1%) and bipolar disorder (59; 19.2%) as the next most common diagnoses (Table 3; Table S1). The remainder of hospitalizations (35; 11.1%) had a variety of other diagnoses, none of which were individually diagnosed in more than 5 discharges. In total 200 hospitalizations (63.5%) had a primary discharge diagnosis of unipolar depression, bipolar depression, or catatonia (which is counted within the psychotic disorders PECCS category).
Table 3:
primary discharge diagnoses for patients receiving ECT, based on PECCS categories. The category of “bipolar disorder” includes depressed, mixed, and manic diagnoses.
| PECCS Category | n | % | Description |
|---|---|---|---|
| 657003 | 143 | 46.4 | Major depressive disorder |
| 659000 | 71 | 23.1 | Schizophrenia and other psychotic disorders |
| 657002 | 59 | 19.2 | Bipolar disorder |
| Other PECCS categories | 35 | 11.1 | Various |
Expanding the list of diagnoses to all primary and secondary diagnoses reveals a large range of psychiatric, neurologic, and medical comorbidities (Table S2 and S3). Suicidal ideation (153; 48.6%) and personal history of self-harm (83; 26.3%) were the most common secondary diagnoses. Anxiety disorders were next most frequent overall, with a total of 166 diagnoses made for conditions including unspecified anxiety disorder (77; 24.4%), generalized anxiety disorder (51, 16.2%), post-traumatic stress disorder (40; 12.7%), and obsessive-compulsive disorder (32; 10.2%). Autistic disorder was diagnosed in 34 (10.8%). A total of 31 patients (9.8%) had physical restraints applied during hospitalization. Grouping secondary diagnoses into PECCS categories reveals common medical comorbidities in hospitalizations involving ECT (Table S2). These include constipation (45; 14.3%), cardiac dysrhythmias (42; 13.3%), sleep disturbances (41; 13.0%), asthma (37; 11.7%), and obesity (36; 11.4%). An additional 24.1% (76) were diagnosed with substance-related disorders, 11.7% (37) were diagnosed with personality disorders, and 9.5% (30) with developmental disorders.
Discussion
This analysis of the KID, the largest all-payor database of pediatric hospitalizations in the United States, found that ECT remains a rare procedure in child and adolescent hospitalizations, with just 315 discharges in 2019 involving ECT, or 0.03% of the 1,049,655 overall hospitalizations for patients aged 10 to 19. This is comparable to the number of patients aged 11–20 treated with ECT in 1980 in inpatient psychiatric hospitals alone [5], despite the US population growing by 46% in the intervening 40 years.
In total 21 states have legal restrictions of various kinds on the use of ECT in those younger than 18 [12]. Consistent with this variation in legal restriction, there is significant regional variation in ECT utilization, with fewer hospitalizations in the western United States involving ECT treatment relative to those in the Northeast, consistent with patterns observed among adult patients [13]. Additionally, wealthier home ZIP code and commercial insurance were both associated with higher odds of receiving ECT. This observation is difficult to interpret as wealth is heterogeneously distributed over states, but nevertheless the impact of socioeconomic status on access to ECT warrant further investigation in the context of appropriate control for state level factors. Moreover, socioeconomic status may influence not only access to treatment, but also patient understanding of ECT and willingness to consent, which requires further study [14,15].
Hospitalizations involving ECT were costly, with a median total hospital charge of $88,778 ($49,571 to $181,860). This is more than fivefold more expensive than the mean hospitalization for appendicitis with peritonitis ($16,043) and comparable to the cost of hospitalizations for the repair of tetralogy of Fallot ($91,978) [16]. As a result, further research that might reduce the cost of hospitalizations involving ECT, for instance reducing the time between admission and administration of first ECT [17], has the potential for substantial healthcare cost savings.
Two large prospective trials of ECT for the treatment of major depressive disorder in adults have found that the mean number of treatments required to reach remission is 7.3 [18,19]. While there have been no prospective randomized studies of ECT use in children and adolescents, hospitalizations in this sample involved a median of 2 ECT treatments during (IQR 1–5), which is unlikely to be sufficient to achieve remission. Indeed, the largest retrospective study of pediatric ECT found a mean of 10.5 administered treatments [4]. It is possible that patients continued their treatments as outpatients following the index hospitalization (which would not be captured in the KID), or likewise that some of the 33 patients transferred to other facilities following their hospitalization continued treatment in the new facility, but this information is not captured in the KID. Alternatively, if treating physicians failed to code for an accurate number of ECT session this analysis would likewise be confounded. Alternatively, this may represent insufficient treatment of pediatric patients with ECT. The accuracy of ECT billing codes in the KID has not been independently verified using other records (e.g. clinical notes), so we are unable to differentiate among the many possibilities for the low number of observed treatments. The adequacy of inpatient ECT delivery for child and adolescent patients thus requires further study.
Diagnostically most hospitalizations for ECT involved a diagnosis of a mood disorder, with psychotic disorders and other diagnoses occurring less frequently. ECT devices have been classified as Class II (moderate risk) by the FDA for the treatment of depressive disorders (unipolar or bipolar) and catatonia in patients aged 13 or older, and in total 200 hospitalizations (63.5%) had primary diagnoses that are consistent with FDA labeling instructions. Of the remainder, diagnoses included psychotic disorders, and manic or mixed bipolar disorder. Some hospitalizations had primary neurologic or developmental diagnoses including encephalitis, autism, and intractable epilepsy for which there is some evidence for ECT, but none of these was the primary discharge diagnosis in more than 5 patients in 2019.
Analysis of secondary diagnoses shows the diverse medical and psychiatric comorbidities among hospitalizations involving ECT. Nearly half of the sample had suicidal ideation at the time when ECT was conducted, with an additional quarter codes as having a personal history of self-harm. Suicidal ideation is a marker for severe and life-threatening disease, and is thus considered an indication for ECT treatment [20]. As there is no evidence for the pharmacologic treatment of suicidal ideation [21] or self-harm behaviors [22] this patient group presents a therapeutic dilemma. Although we do not know of any evidence for ECT as a treatment of suicidal ideation in children or adolescents, adult data suggest that ECT has efficacy for the reduction of suicidal ideation [23,24]. As such it possible the uses of ECT may be weighted toward suicidal adolescents, who make up a significant fraction of ECT recipients in the sample. Among other comorbidities, both autism (34; 10.8%) and developmental disorders (30; 9.5%) were common. ECT has demonstrated efficacy in self-injurious behaviors and catatonia in patients with autism and intellectual delay [25,26], which may contribute to the prevalence of these patients among ECT recipients. As prior evidence suggests that catatonia is underrecognized in individuals with intellectual delay [27], and overall is rarely recognized in the inpatient setting in children [28], there may be additional hospitalized children who may benefit from ECT administration.
Physical restraints were applied to 31 patients (9.8%) receiving ECT, a rate far higher than the 0.1% physical restraint rate recently reported for pediatric patients in the emergency department [29]. The practice of physical restraints in children, while sometimes medically necessary [30], is traumatic for the child, and rates of restraint use have been found to vary significantly with race and ethnicity [29]. While the KID does not include information about indication for physical restraints, this high rate of restraint utilization is another marker of the severe illness among ECT recipients.
Strengths and limitations of this study are largely those of the KID and observational administrative claims data more broadly. As observational claims data go the KID is particularly strong as it is the largest inpatient database of pediatric hospitalizations in the United States and designed to be nationally representative. Further, because the KID sample includes 80% of pediatric discharges from 3,998 hospitals in 49 states, it increases the likelihood of capturing rare events including comorbidities, complications, and indications. This builds on prior work exploring pediatric ECT using the nationwide inpatient sample [7], which has 20% coverage of pediatric hospital discharges. As a result, the demographics and diagnoses reported here provides a comprehensive description of child and adolescent ECT as its practice in acute care hospitals.
Limitations of observational administrative design claims data are well described and apply here [31,32]. Information about ECT use is based on discharge billing codes, and so any errors in coding would reduce the accuracy of the sample [33]. Likewise, as billing codes only capture discharge diagnoses, they do not specifically indicate the diagnosis that was the primary indication for ECT. Furthermore as the KID counts discharges and not individual patients, if a single patient is admitted multiple times for ECT or receives ECT at more than one facility as a result of a transfer, that patient may appear more than once in the database. This further means that we are unable to assess whether ECT is associated with changes in rehospitalization or total health expenditure for an individual. Finally, the KID does not include rehabilitation hospitals and freestanding psychiatric facilities, and so would not have information about ECT performed in those settings or outpatient ECT at any facilities. It is not known what fraction of ECT is performed in these settings, and so these results do not allow for determination of the overall number of child and adolescent patients treated with ECT nationally.
Conclusion
ECT is a rarely utilized procedure among children and adolescents hospitalized, with 315 discharges (95% confidence interval 275 to 354) utilizing ECT in 2019, representing 0.03% of the 1,049,655 overall hospitalizations for patients aged 10 to 19. Primary diagnoses for ECT hospitalizations were mood and psychotic disorders, and patients also suffered from significant medical and psychiatric comorbidities. Commercial insurance and higher income were associated with higher odds of ECT administration, which invites further study of potential socioeconomic barriers to treatment.
Supplementary Material
Funding
This work was supported by the National Institute of Mental Health (T32MH112485, JL) and the Avery D. Weisman Fund of the Massachusetts General Hospital Department of Psychiatry. The sponsors had no role in study design, writing of the report, or data collection, analysis, or interpretation.
Conflicts of Interest
JL holds equity in Revival Therapeutics, Inc. THM receives research funding from the Stanley Center at the Broad Institute, the Brain and Behavior Research Foundation, National Institute of Mental Health, National Human Genome Research Institute Home, and Telefonica Alfa. The remaining authors have no disclosures to report.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Hemphill RE, Walter WG. The Treatment of Mental Disorders by Electrically Induced Convulsions. J Ment Sci 1941;87:256–75. 10.1192/bjp.87.367.256. [DOI] [Google Scholar]
- [2].Døssing E, Pagsberg AK. Electroconvulsive Therapy in Children and Adolescents: A Systematic Review of Current Literature and Guidelines. J ECT 2021;37:158–70. 10.1097/YCT.0000000000000761. [DOI] [PubMed] [Google Scholar]
- [3].Luccarelli J, McCoy TH, Uchida M, Green A, Seiner SJ, Henry ME. The Efficacy and Cognitive Effects of Acute Course Electroconvulsive Therapy Are Equal in Adolescents, Transitional Age Youth, and Young Adults. J Child Adolesc Psychopharmacol 2021;31:538–44. 10.1089/cap.2021.0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Pierson MD, Mickey BJ, Gilley LB, Weeks HR. Outcomes of Youth Treated With Electroconvulsive Therapy: A Retrospective Cohort Study. J Clin Psychiatry 2021;82:19m13164. 10.4088/JCP.19m13164. [DOI] [PubMed] [Google Scholar]
- [5].Thompson JW, Blaine JD. Use of ECT in the United States in 1975 and 1980. Am J Psychiatry 1987;144:557–62. 10.1176/ajp.144.5.557. [DOI] [PubMed] [Google Scholar]
- [6].Luccarelli J, Henry ME, McCoy TH. Demographics of Patients Receiving Electroconvulsive Therapy Based on State-Mandated Reporting Data. J ECT 2020;36:229–33. 10.1097/YCT.0000000000000692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Trivedi C, Motiwala F, Mainali P, Mansuri Z, Jain S. Trends for Electroconvulsive Therapy Utilization in Children and Adolescents in the United States From 2002 to 2017: A Nationwide Inpatient Sample Analysis. J ECT 2021;37:100–6. 10.1097/YCT.0000000000000750. [DOI] [PubMed] [Google Scholar]
- [8].American Hospital Association. Fast Facts on U.S. Hospitals, 2021 2021.
- [9].Gill PJ, Anwar MR, Thavam T, Hall M, Rodean J, Mahant S. Pediatric Clinical Classification System for Use in Inpatient Settings. JAMA Pediatr 2021;175:525–7. 10.1001/jamapediatrics.2020.6007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kaster TS, Blumberger DM, Gomes T, Sutradhar R, Dasklakis ZJ, Wijeysundera DN, et al. Patient-level Characteristics and Inequitable Access to Inpatient Electroconvulsive Therapy for Depression: A Population-based Cross-sectional Study: Caractéristiques au niveau du patient et accès inéquitable à la thérapie électroconvulsive pour patients hospitalisés. Can J Psychiatry Rev Can Psychiatr 2021;66:147–58. 10.1177/0706743720935647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLOS Med 2015;12:e1001885. 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Livingston R, Wu C, Mu K, Coffey MJ. Regulation of Electroconvulsive Therapy: A Systematic Review of US State Laws. J ECT 2018;34:60. 10.1097/YCT.0000000000000460. [DOI] [PubMed] [Google Scholar]
- [13].Wilkinson ST, Agbese E, Leslie DL, Rosenheck RA. Identifying Recipients of Electroconvulsive Therapy: Data From Privately Insured Americans. Psychiatr Serv Wash DC 2018;69:542–8. 10.1176/appi.ps.201700364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Yen C-F, Chen C-C, Lee Y, Tang T-C, Ko C-H, Yen J-Y. Insight and correlates among outpatients with depressive disorders. Compr Psychiatry 2005;46:384–9. 10.1016/j.comppsych.2004.11.004. [DOI] [PubMed] [Google Scholar]
- [15].Tsai T-I, Yu W-R, Lee S-YD. Is health literacy associated with greater medical care trust? Int J Qual Health Care 2018;30:514–9. 10.1093/intqhc/mzy043. [DOI] [PubMed] [Google Scholar]
- [16].Gill PJ, Anwar MR, Thavam T, Hall M, Rodean J, Kaiser SV, et al. Identifying Conditions With High Prevalence, Cost, and Variation in Cost in US Children’s Hospitals. JAMA Netw Open 2021;4:e2117816. 10.1001/jamanetworkopen.2021.17816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Patel RS, Sreeram V, Thakur T, Bachu R, Youssef NA. A national study for regional variation of inpatient ECT utilization from 4,411 hospitals across the United States. Ann Clin Psychiatry 2019;31:200–2008. [PubMed] [Google Scholar]
- [18].Kellner CH, Knapp RG, Petrides G, Rummans TA, Husain MM, Rasmussen K, et al. Continuation Electroconvulsive Therapy vs Pharmacotherapy for Relapse Prevention in Major Depression: A Multisite Study From the Consortium for Research in Electroconvulsive Therapy (CORE). Arch Gen Psychiatry 2006;63:1337–44. 10.1001/archpsyc.63.12.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kellner CH, Husain MM, Knapp RG, McCall WV, Petrides G, Rudorfer MV, et al. Right Unilateral Ultrabrief Pulse ECT in Geriatric Depression: Phase 1 of the PRIDE Study. Am J Psychiatry 2016;173:1101–9. 10.1176/appi.ajp.2016.15081101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Espinoza RT, Kellner CH. Electroconvulsive Therapy. N Engl J Med 2022;386:667–72. 10.1056/NEJMra2034954. [DOI] [PubMed] [Google Scholar]
- [21].Kothgassner OD, Robinson K, Goreis A, Ougrin D, Plener PL. Does treatment method matter? A meta-analysis of the past 20 years of research on therapeutic interventions for self-harm and suicidal ideation in adolescents. Borderline Personal Disord Emot Dysregulation 2020;7:9. 10.1186/s40479-020-00123-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Witt KG, Hetrick SE, Rajaram G, Hazell P, Taylor Salisbury TL, Townsend E, et al. Interventions for self-harm in children and adolescents. Cochrane Database Syst Rev 2021;3:CD013667. 10.1002/14651858.CD013667.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kellner CH, Fink M, Knapp R, Petrides G, Husain M, Rummans T, et al. Relief of Expressed Suicidal Intent by ECT: A Consortium for Research in ECT Study. Am J Psychiatry 2005;162:977–82. 10.1176/appi.ajp.162.5.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Fink M, Kellner CH, McCall WV. The Role of ECT in Suicide Prevention. J ECT 2014;30:5–9. 10.1097/YCT.0b013e3182a6ad0d. [DOI] [PubMed] [Google Scholar]
- [25].Wachtel LE. Treatment of catatonia in autism spectrum disorders. Acta Psychiatr Scand 2019;139:46–55. 10.1111/acps.12980. [DOI] [PubMed] [Google Scholar]
- [26].Wachtel LE, Dhossche DM. Challenges of Electroconvulsive Therapy for Catatonia in Youth With Intellectual Disabilities Another Tomato Effect? J Ect 2012;28:151–3. 10.1097/YCT.0b013e31825692e2. [DOI] [PubMed] [Google Scholar]
- [27].Ghaziuddin N, Dhossche D, Marcotte K. Retrospective chart review of catatonia in child and adolescent psychiatric patients. Acta Psychiatr Scand 2012;125:33–8. 10.1111/j.1600-0447.2011.01778.x. [DOI] [PubMed] [Google Scholar]
- [28].Luccarelli J, Kalinich M, Fernandez-Robles C, Fricchione G, Beach SR. The Incidence of Catatonia Diagnosis Among Pediatric Patients Discharged From General Hospitals in the United States: A Kids’ Inpatient Database Study. Front Psychiatry 2022;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Nash KA, Tolliver DG, Taylor RA, Calhoun AJ, Auerbach MA, Venkatesh AK, et al. Racial and Ethnic Disparities in Physical Restraint Use for Pediatric Patients in the Emergency Department. JAMA Pediatr 2021;175:1283–5. 10.1001/jamapediatrics.2021.3348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Preisz A, Preisz P. Restraint in paediatrics: A delicate balance. J Paediatr Child Health 2019;55:1165–9. 10.1111/jpc.14607. [DOI] [PubMed] [Google Scholar]
- [31].Green LW, Allegrante JP. Practice-Based Evidence and the Need for More Diverse Methods and Sources in Epidemiology, Public Health and Health Promotion. Am J Health Promot 2020;34:946–8. 10.1177/0890117120960580b. [DOI] [PubMed] [Google Scholar]
- [32].Johnson EK, Nelson CP. Utility and Pitfalls in the Use of Administrative Databases for Outcomes Assessment. J Urol 2013;190:17–8. 10.1016/j.juro.2013.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Davis KAS, Sudlow CLM, Hotopf M. Can mental health diagnoses in administrative data be used for research? A systematic review of the accuracy of routinely collected diagnoses. BMC Psychiatry 2016;16:263. 10.1186/s12888-016-0963-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


