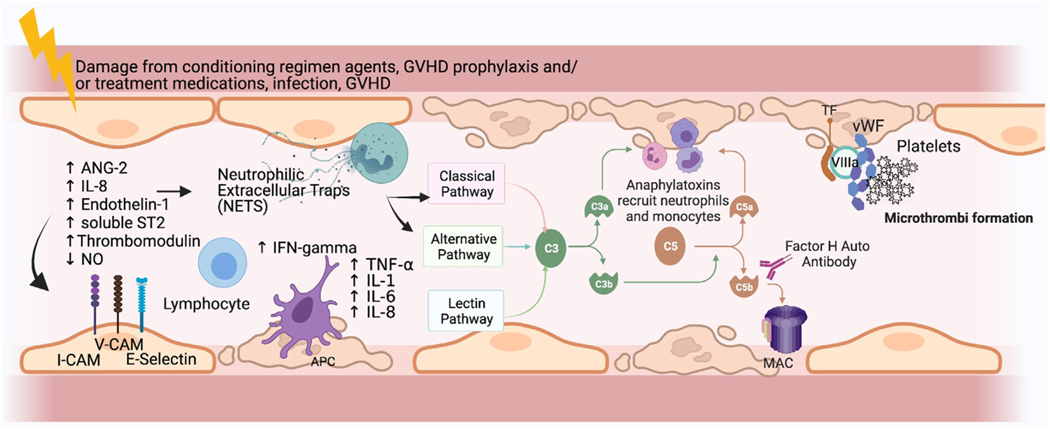
Figure 1.
Proposed pathophysiology of TA-TMA and potential biomarkers. Endothelial cells (ECs) are thought to be damaged by chemotherapy administered as part of the preparative regimen, medications, and complications of BMT. Damaged ECs release ANG-2, leading to vascular destabilization and release of IL-8. Local recruitment of antigen-presenting cells (APCs) and lymphocytes results from the expression of increased adhesion molecules by activated APCs. APCs also express TNF-α and INF-γ, which further activate neutrophils and T cells, which then release neutrophil extracellular traps (NETs). This leads to the activation of a component of the alternative complement pathway, C3b, which binds to the endothelial surface, leading to formation of the membrane activating complex (MAC) on ECs, further contributing to direct ongoing damage of the ECs. The formation of microthrombi ensues next, whereby tissue factor released from the damaged ECs binds factor VIIA and von Willebrand factor (vWF), promoting platelet activation and subsequent thrombus formation. Microthrombi then lead to organ ischemia and end-organ damage (eg, renal failure). Markers of any of these pathways may have diagnostic or prognostic implications in TA-TMA. sC5b-9 and dsDNA (marker of NETs) have been tested for diagnostic utility, but the other markers have not. Potential biomarkers include soluble selectins, markers of endothelial injury, inflammatory cytokines, components of complement cascade other than sC5b-9, and markers of thrombosis. V-CAM indicates vascular cell adhesion molecule; I-CAM, intercellular adhesion molecule (Figure created using Biorender). Figure modified with permission from Schoettler, et al. Current Opinion Hematology, 2021. Schoettler M, Chonat S, Williams K, Lehmann L. Emerging therapeutic and preventive approaches to transplant-associated thrombotic microangiopathy. Curr Opin Hematol. 2021 Nov 1;28 (6):408–416. doi: 10.1097/MOH.0000000000000687. PMID: 34534983.